An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Am J Pharm Educ
- v.74(8); 2010 Oct 11

Presenting and Evaluating Qualitative Research
The purpose of this paper is to help authors to think about ways to present qualitative research papers in the American Journal of Pharmaceutical Education . It also discusses methods for reviewers to assess the rigour, quality, and usefulness of qualitative research. Examples of different ways to present data from interviews, observations, and focus groups are included. The paper concludes with guidance for publishing qualitative research and a checklist for authors and reviewers.
INTRODUCTION
Policy and practice decisions, including those in education, increasingly are informed by findings from qualitative as well as quantitative research. Qualitative research is useful to policymakers because it often describes the settings in which policies will be implemented. Qualitative research is also useful to both pharmacy practitioners and pharmacy academics who are involved in researching educational issues in both universities and practice and in developing teaching and learning.
Qualitative research involves the collection, analysis, and interpretation of data that are not easily reduced to numbers. These data relate to the social world and the concepts and behaviors of people within it. Qualitative research can be found in all social sciences and in the applied fields that derive from them, for example, research in health services, nursing, and pharmacy. 1 It looks at X in terms of how X varies in different circumstances rather than how big is X or how many Xs are there? 2 Textbooks often subdivide research into qualitative and quantitative approaches, furthering the common assumption that there are fundamental differences between the 2 approaches. With pharmacy educators who have been trained in the natural and clinical sciences, there is often a tendency to embrace quantitative research, perhaps due to familiarity. A growing consensus is emerging that sees both qualitative and quantitative approaches as useful to answering research questions and understanding the world. Increasingly mixed methods research is being carried out where the researcher explicitly combines the quantitative and qualitative aspects of the study. 3 , 4
Like healthcare, education involves complex human interactions that can rarely be studied or explained in simple terms. Complex educational situations demand complex understanding; thus, the scope of educational research can be extended by the use of qualitative methods. Qualitative research can sometimes provide a better understanding of the nature of educational problems and thus add to insights into teaching and learning in a number of contexts. For example, at the University of Nottingham, we conducted in-depth interviews with pharmacists to determine their perceptions of continuing professional development and who had influenced their learning. We also have used a case study approach using observation of practice and in-depth interviews to explore physiotherapists' views of influences on their leaning in practice. We have conducted in-depth interviews with a variety of stakeholders in Malawi, Africa, to explore the issues surrounding pharmacy academic capacity building. A colleague has interviewed and conducted focus groups with students to explore cultural issues as part of a joint Nottingham-Malaysia pharmacy degree program. Another colleague has interviewed pharmacists and patients regarding their expectations before and after clinic appointments and then observed pharmacist-patient communication in clinics and assessed it using the Calgary Cambridge model in order to develop recommendations for communication skills training. 5 We have also performed documentary analysis on curriculum data to compare pharmacist and nurse supplementary prescribing courses in the United Kingdom.
It is important to choose the most appropriate methods for what is being investigated. Qualitative research is not appropriate to answer every research question and researchers need to think carefully about their objectives. Do they wish to study a particular phenomenon in depth (eg, students' perceptions of studying in a different culture)? Or are they more interested in making standardized comparisons and accounting for variance (eg, examining differences in examination grades after changing the way the content of a module is taught). Clearly a quantitative approach would be more appropriate in the last example. As with any research project, a clear research objective has to be identified to know which methods should be applied.
Types of qualitative data include:
- Audio recordings and transcripts from in-depth or semi-structured interviews
- Structured interview questionnaires containing substantial open comments including a substantial number of responses to open comment items.
- Audio recordings and transcripts from focus group sessions.
- Field notes (notes taken by the researcher while in the field [setting] being studied)
- Video recordings (eg, lecture delivery, class assignments, laboratory performance)
- Case study notes
- Documents (reports, meeting minutes, e-mails)
- Diaries, video diaries
- Observation notes
- Press clippings
- Photographs
RIGOUR IN QUALITATIVE RESEARCH
Qualitative research is often criticized as biased, small scale, anecdotal, and/or lacking rigor; however, when it is carried out properly it is unbiased, in depth, valid, reliable, credible and rigorous. In qualitative research, there needs to be a way of assessing the “extent to which claims are supported by convincing evidence.” 1 Although the terms reliability and validity traditionally have been associated with quantitative research, increasingly they are being seen as important concepts in qualitative research as well. Examining the data for reliability and validity assesses both the objectivity and credibility of the research. Validity relates to the honesty and genuineness of the research data, while reliability relates to the reproducibility and stability of the data.
The validity of research findings refers to the extent to which the findings are an accurate representation of the phenomena they are intended to represent. The reliability of a study refers to the reproducibility of the findings. Validity can be substantiated by a number of techniques including triangulation use of contradictory evidence, respondent validation, and constant comparison. Triangulation is using 2 or more methods to study the same phenomenon. Contradictory evidence, often known as deviant cases, must be sought out, examined, and accounted for in the analysis to ensure that researcher bias does not interfere with or alter their perception of the data and any insights offered. Respondent validation, which is allowing participants to read through the data and analyses and provide feedback on the researchers' interpretations of their responses, provides researchers with a method of checking for inconsistencies, challenges the researchers' assumptions, and provides them with an opportunity to re-analyze their data. The use of constant comparison means that one piece of data (for example, an interview) is compared with previous data and not considered on its own, enabling researchers to treat the data as a whole rather than fragmenting it. Constant comparison also enables the researcher to identify emerging/unanticipated themes within the research project.
STRENGTHS AND LIMITATIONS OF QUALITATIVE RESEARCH
Qualitative researchers have been criticized for overusing interviews and focus groups at the expense of other methods such as ethnography, observation, documentary analysis, case studies, and conversational analysis. Qualitative research has numerous strengths when properly conducted.
Strengths of Qualitative Research
- Issues can be examined in detail and in depth.
- Interviews are not restricted to specific questions and can be guided/redirected by the researcher in real time.
- The research framework and direction can be quickly revised as new information emerges.
- The data based on human experience that is obtained is powerful and sometimes more compelling than quantitative data.
- Subtleties and complexities about the research subjects and/or topic are discovered that are often missed by more positivistic enquiries.
- Data usually are collected from a few cases or individuals so findings cannot be generalized to a larger population. Findings can however be transferable to another setting.
Limitations of Qualitative Research
- Research quality is heavily dependent on the individual skills of the researcher and more easily influenced by the researcher's personal biases and idiosyncrasies.
- Rigor is more difficult to maintain, assess, and demonstrate.
- The volume of data makes analysis and interpretation time consuming.
- It is sometimes not as well understood and accepted as quantitative research within the scientific community
- The researcher's presence during data gathering, which is often unavoidable in qualitative research, can affect the subjects' responses.
- Issues of anonymity and confidentiality can present problems when presenting findings
- Findings can be more difficult and time consuming to characterize in a visual way.
PRESENTATION OF QUALITATIVE RESEARCH FINDINGS
The following extracts are examples of how qualitative data might be presented:
Data From an Interview.
The following is an example of how to present and discuss a quote from an interview.
The researcher should select quotes that are poignant and/or most representative of the research findings. Including large portions of an interview in a research paper is not necessary and often tedious for the reader. The setting and speakers should be established in the text at the end of the quote.
The student describes how he had used deep learning in a dispensing module. He was able to draw on learning from a previous module, “I found that while using the e learning programme I was able to apply the knowledge and skills that I had gained in last year's diseases and goals of treatment module.” (interviewee 22, male)
This is an excerpt from an article on curriculum reform that used interviews 5 :
The first question was, “Without the accreditation mandate, how much of this curriculum reform would have been attempted?” According to respondents, accreditation played a significant role in prompting the broad-based curricular change, and their comments revealed a nuanced view. Most indicated that the change would likely have occurred even without the mandate from the accreditation process: “It reflects where the profession wants to be … training a professional who wants to take on more responsibility.” However, they also commented that “if it were not mandated, it could have been a very difficult road.” Or it “would have happened, but much later.” The change would more likely have been incremental, “evolutionary,” or far more limited in its scope. “Accreditation tipped the balance” was the way one person phrased it. “Nobody got serious until the accrediting body said it would no longer accredit programs that did not change.”
Data From Observations
The following example is some data taken from observation of pharmacist patient consultations using the Calgary Cambridge guide. 6 , 7 The data are first presented and a discussion follows:
Pharmacist: We will soon be starting a stop smoking clinic. Patient: Is the interview over now? Pharmacist: No this is part of it. (Laughs) You can't tell me to bog off (sic) yet. (pause) We will be starting a stop smoking service here, Patient: Yes. Pharmacist: with one-to-one and we will be able to help you or try to help you. If you want it. In this example, the pharmacist has picked up from the patient's reaction to the stop smoking clinic that she is not receptive to advice about giving up smoking at this time; in fact she would rather end the consultation. The pharmacist draws on his prior relationship with the patient and makes use of a joke to lighten the tone. He feels his message is important enough to persevere but he presents the information in a succinct and non-pressurised way. His final comment of “If you want it” is important as this makes it clear that he is not putting any pressure on the patient to take up this offer. This extract shows that some patient cues were picked up, and appropriately dealt with, but this was not the case in all examples.
Data From Focus Groups
This excerpt from a study involving 11 focus groups illustrates how findings are presented using representative quotes from focus group participants. 8
Those pharmacists who were initially familiar with CPD endorsed the model for their peers, and suggested it had made a meaningful difference in the way they viewed their own practice. In virtually all focus groups sessions, pharmacists familiar with and supportive of the CPD paradigm had worked in collaborative practice environments such as hospital pharmacy practice. For these pharmacists, the major advantage of CPD was the linking of workplace learning with continuous education. One pharmacist stated, “It's amazing how much I have to learn every day, when I work as a pharmacist. With [the learning portfolio] it helps to show how much learning we all do, every day. It's kind of satisfying to look it over and see how much you accomplish.” Within many of the learning portfolio-sharing sessions, debates emerged regarding the true value of traditional continuing education and its outcome in changing an individual's practice. While participants appreciated the opportunity for social and professional networking inherent in some forms of traditional CE, most eventually conceded that the academic value of most CE programming was limited by the lack of a systematic process for following-up and implementing new learning in the workplace. “Well it's nice to go to these [continuing education] events, but really, I don't know how useful they are. You go, you sit, you listen, but then, well I at least forget.”
The following is an extract from a focus group (conducted by the author) with first-year pharmacy students about community placements. It illustrates how focus groups provide a chance for participants to discuss issues on which they might disagree.
Interviewer: So you are saying that you would prefer health related placements? Student 1: Not exactly so long as I could be developing my communication skill. Student 2: Yes but I still think the more health related the placement is the more I'll gain from it. Student 3: I disagree because other people related skills are useful and you may learn those from taking part in a community project like building a garden. Interviewer: So would you prefer a mixture of health and non health related community placements?
GUIDANCE FOR PUBLISHING QUALITATIVE RESEARCH
Qualitative research is becoming increasingly accepted and published in pharmacy and medical journals. Some journals and publishers have guidelines for presenting qualitative research, for example, the British Medical Journal 9 and Biomedcentral . 10 Medical Education published a useful series of articles on qualitative research. 11 Some of the important issues that should be considered by authors, reviewers and editors when publishing qualitative research are discussed below.
Introduction.
A good introduction provides a brief overview of the manuscript, including the research question and a statement justifying the research question and the reasons for using qualitative research methods. This section also should provide background information, including relevant literature from pharmacy, medicine, and other health professions, as well as literature from the field of education that addresses similar issues. Any specific educational or research terminology used in the manuscript should be defined in the introduction.
The methods section should clearly state and justify why the particular method, for example, face to face semistructured interviews, was chosen. The method should be outlined and illustrated with examples such as the interview questions, focusing exercises, observation criteria, etc. The criteria for selecting the study participants should then be explained and justified. The way in which the participants were recruited and by whom also must be stated. A brief explanation/description should be included of those who were invited to participate but chose not to. It is important to consider “fair dealing,” ie, whether the research design explicitly incorporates a wide range of different perspectives so that the viewpoint of 1 group is never presented as if it represents the sole truth about any situation. The process by which ethical and or research/institutional governance approval was obtained should be described and cited.
The study sample and the research setting should be described. Sampling differs between qualitative and quantitative studies. In quantitative survey studies, it is important to select probability samples so that statistics can be used to provide generalizations to the population from which the sample was drawn. Qualitative research necessitates having a small sample because of the detailed and intensive work required for the study. So sample sizes are not calculated using mathematical rules and probability statistics are not applied. Instead qualitative researchers should describe their sample in terms of characteristics and relevance to the wider population. Purposive sampling is common in qualitative research. Particular individuals are chosen with characteristics relevant to the study who are thought will be most informative. Purposive sampling also may be used to produce maximum variation within a sample. Participants being chosen based for example, on year of study, gender, place of work, etc. Representative samples also may be used, for example, 20 students from each of 6 schools of pharmacy. Convenience samples involve the researcher choosing those who are either most accessible or most willing to take part. This may be fine for exploratory studies; however, this form of sampling may be biased and unrepresentative of the population in question. Theoretical sampling uses insights gained from previous research to inform sample selection for a new study. The method for gaining informed consent from the participants should be described, as well as how anonymity and confidentiality of subjects were guaranteed. The method of recording, eg, audio or video recording, should be noted, along with procedures used for transcribing the data.
Data Analysis.
A description of how the data were analyzed also should be included. Was computer-aided qualitative data analysis software such as NVivo (QSR International, Cambridge, MA) used? Arrival at “data saturation” or the end of data collection should then be described and justified. A good rule when considering how much information to include is that readers should have been given enough information to be able to carry out similar research themselves.
One of the strengths of qualitative research is the recognition that data must always be understood in relation to the context of their production. 1 The analytical approach taken should be described in detail and theoretically justified in light of the research question. If the analysis was repeated by more than 1 researcher to ensure reliability or trustworthiness, this should be stated and methods of resolving any disagreements clearly described. Some researchers ask participants to check the data. If this was done, it should be fully discussed in the paper.
An adequate account of how the findings were produced should be included A description of how the themes and concepts were derived from the data also should be included. Was an inductive or deductive process used? The analysis should not be limited to just those issues that the researcher thinks are important, anticipated themes, but also consider issues that participants raised, ie, emergent themes. Qualitative researchers must be open regarding the data analysis and provide evidence of their thinking, for example, were alternative explanations for the data considered and dismissed, and if so, why were they dismissed? It also is important to present outlying or negative/deviant cases that did not fit with the central interpretation.
The interpretation should usually be grounded in interviewees or respondents' contributions and may be semi-quantified, if this is possible or appropriate, for example, “Half of the respondents said …” “The majority said …” “Three said…” Readers should be presented with data that enable them to “see what the researcher is talking about.” 1 Sufficient data should be presented to allow the reader to clearly see the relationship between the data and the interpretation of the data. Qualitative data conventionally are presented by using illustrative quotes. Quotes are “raw data” and should be compiled and analyzed, not just listed. There should be an explanation of how the quotes were chosen and how they are labeled. For example, have pseudonyms been given to each respondent or are the respondents identified using codes, and if so, how? It is important for the reader to be able to see that a range of participants have contributed to the data and that not all the quotes are drawn from 1 or 2 individuals. There is a tendency for authors to overuse quotes and for papers to be dominated by a series of long quotes with little analysis or discussion. This should be avoided.
Participants do not always state the truth and may say what they think the interviewer wishes to hear. A good qualitative researcher should not only examine what people say but also consider how they structured their responses and how they talked about the subject being discussed, for example, the person's emotions, tone, nonverbal communication, etc. If the research was triangulated with other qualitative or quantitative data, this should be discussed.
Discussion.
The findings should be presented in the context of any similar previous research and or theories. A discussion of the existing literature and how this present research contributes to the area should be included. A consideration must also be made about how transferrable the research would be to other settings. Any particular strengths and limitations of the research also should be discussed. It is common practice to include some discussion within the results section of qualitative research and follow with a concluding discussion.
The author also should reflect on their own influence on the data, including a consideration of how the researcher(s) may have introduced bias to the results. The researcher should critically examine their own influence on the design and development of the research, as well as on data collection and interpretation of the data, eg, were they an experienced teacher who researched teaching methods? If so, they should discuss how this might have influenced their interpretation of the results.
Conclusion.
The conclusion should summarize the main findings from the study and emphasize what the study adds to knowledge in the area being studied. Mays and Pope suggest the researcher ask the following 3 questions to determine whether the conclusions of a qualitative study are valid 12 : How well does this analysis explain why people behave in the way they do? How comprehensible would this explanation be to a thoughtful participant in the setting? How well does the explanation cohere with what we already know?
CHECKLIST FOR QUALITATIVE PAPERS
This paper establishes criteria for judging the quality of qualitative research. It provides guidance for authors and reviewers to prepare and review qualitative research papers for the American Journal of Pharmaceutical Education . A checklist is provided in Appendix 1 to assist both authors and reviewers of qualitative data.
ACKNOWLEDGEMENTS
Thank you to the 3 reviewers whose ideas helped me to shape this paper.
Appendix 1. Checklist for authors and reviewers of qualitative research.
Introduction
- □ Research question is clearly stated.
- □ Research question is justified and related to the existing knowledge base (empirical research, theory, policy).
- □ Any specific research or educational terminology used later in manuscript is defined.
- □ The process by which ethical and or research/institutional governance approval was obtained is described and cited.
- □ Reason for choosing particular research method is stated.
- □ Criteria for selecting study participants are explained and justified.
- □ Recruitment methods are explicitly stated.
- □ Details of who chose not to participate and why are given.
- □ Study sample and research setting used are described.
- □ Method for gaining informed consent from the participants is described.
- □ Maintenance/Preservation of subject anonymity and confidentiality is described.
- □ Method of recording data (eg, audio or video recording) and procedures for transcribing data are described.
- □ Methods are outlined and examples given (eg, interview guide).
- □ Decision to stop data collection is described and justified.
- □ Data analysis and verification are described, including by whom they were performed.
- □ Methods for identifying/extrapolating themes and concepts from the data are discussed.
- □ Sufficient data are presented to allow a reader to assess whether or not the interpretation is supported by the data.
- □ Outlying or negative/deviant cases that do not fit with the central interpretation are presented.
- □ Transferability of research findings to other settings is discussed.
- □ Findings are presented in the context of any similar previous research and social theories.
- □ Discussion often is incorporated into the results in qualitative papers.
- □ A discussion of the existing literature and how this present research contributes to the area is included.
- □ Any particular strengths and limitations of the research are discussed.
- □ Reflection of the influence of the researcher(s) on the data, including a consideration of how the researcher(s) may have introduced bias to the results is included.
Conclusions
- □ The conclusion states the main finings of the study and emphasizes what the study adds to knowledge in the subject area.
- AI Templates
- Get a demo Sign up for free Log in Log in
Buttoning up research: How to present and visualize qualitative data

15 Minute Read

There is no doubt that data visualization is an important part of the qualitative research process. Whether you're preparing a presentation or writing up a report, effective visualizations can help make your findings clear and understandable for your audience.
In this blog post, we'll discuss some tips for creating effective visualizations of qualitative data.
First, let's take a closer look at what exactly qualitative data is.
What is qualitative data?
Qualitative data is information gathered through observation, questionnaires, and interviews. It's often subjective, meaning that the researcher has to interpret it to draw meaningful conclusions from it.
The difference between qualitative data and quantitative data
When researchers use the terms qualitative and quantitative, they're referring to two different types of data. Qualitative data is subjective and descriptive, while quantitative data is objective and numerical.
Qualitative data is often used in research involving psychology or sociology. This is usually where a researcher may be trying to identify patterns or concepts related to people's behavior or attitudes. It may also be used in research involving economics or finance, where the focus is on numerical values such as price points or profit margins.
Before we delve into how best to present and visualize qualitative data, it's important that we highlight how to be gathering this data in the first place.

How best to gather qualitative data
In order to create an effective visualization of qualitative data, ensure that the right kind of information has been gathered.
Here are six ways to gather the most accurate qualitative data:
- Define your research question: What data is being set out to collect? A qualitative research question is a definite or clear statement about a condition to be improved, a project’s area of concern, a troubling question that exists, or a difficulty to be eliminated. It not only defines who the participants will be but guides the data collection methods needed to achieve the most detailed responses.
- Determine the best data collection method(s): The data collected should be appropriate to answer the research question. Some common qualitative data collection methods include interviews, focus groups, observations, or document analysis. Consider the strengths and weaknesses of each option before deciding which one is best suited to answer the research question.
- Develop a cohesive interview guide: Creating an interview guide allows researchers to ask more specific questions and encourages thoughtful responses from participants. It’s important to design questions in such a way that they are centered around the topic of discussion and elicit meaningful insight into the issue at hand. Avoid leading or biased questions that could influence participants’ answers, and be aware of cultural nuances that may affect their answers.
- Stay neutral – let participants share their stories: The goal is to obtain useful information, not to influence the participant’s answer. Allowing participants to express themselves freely will help to gather more honest and detailed responses. It’s important to maintain a neutral tone throughout interviews and avoid judgment or opinions while they are sharing their story.
- Work with at least one additional team member when conducting qualitative research: Participants should always feel comfortable while providing feedback on a topic, so it can be helpful to have an extra team member present during the interview process – particularly if this person is familiar with the topic being discussed. This will ensure that the atmosphere of the interview remains respectful and encourages participants to speak openly and honestly.
- Analyze your findings: Once all of the data has been collected, it’s important to analyze it in order to draw meaningful conclusions. Use tools such as qualitative coding or content analysis to identify patterns or themes in the data, then compare them with prior research or other data sources. This will help to draw more accurate and useful insights from the results.
By following these steps, you will be well-prepared to collect and analyze qualitative data for your research project. Next, let's focus on how best to present the qualitative data that you have gathered and analyzed.

Create your own AI-powered templates for better, faster research synthesis. Discover new customer insights from data instantly.

The top 10 things Notably shipped in 2023 and themes for 2024.
How to visually present qualitative data.
When it comes to how to present qualitative data visually, the goal is to make research findings clear and easy to understand. To do this, use visuals that are both attractive and informative.
Presenting qualitative data visually helps to bring the user’s attention to specific items and draw them into a more in-depth analysis. Visuals provide an efficient way to communicate complex information, making it easier for the audience to comprehend.
Additionally, visuals can help engage an audience by making a presentation more interesting and interactive.
Here are some tips for creating effective visuals from qualitative data:
- Choose the right type of visualization: Consider which type of visual would best convey the story that is being told through the research. For example, bar charts or line graphs might be appropriate for tracking changes over time, while pie charts or word clouds could help show patterns in categorical data.
- Include contextual information: In addition to showing the actual numbers, it's helpful to include any relevant contextual information in order to provide context for the audience. This can include details such as the sample size, any anomalies that occurred during data collection, or other environmental factors.
- Make it easy to understand: Always keep visuals simple and avoid adding too much detail or complexity. This will help ensure that viewers can quickly grasp the main points without getting overwhelmed by all of the information.
- Use color strategically: Color can be used to draw attention to certain elements in your visual and make it easier for viewers to find the most important parts of it. Just be sure not to use too many different colors, as this could create confusion instead of clarity.
- Use charts or whiteboards: Using charts or whiteboards can help to explain the data in more detail and get viewers engaged in a discussion. This type of visual tool can also be used to create storyboards that illustrate the data over time, helping to bring your research to life.

Visualizing qualitative data in Notably
Notably helps researchers visualize their data on a flexible canvas, charts, and evidence based insights. As an all-in-one research platform, Notably enables researchers to collect, analyze and present qualitative data effectively.
Notably provides an intuitive interface for analyzing data from a variety of sources, including interviews, surveys, desk research, and more. Its powerful analytics engine then helps you to quickly identify insights and trends in your data . Finally, the platform makes it easy to create beautiful visuals that will help to communicate research findings with confidence.
Research Frameworks in Analysis
The canvas in Analysis is a multi-dimensional workspace to play with your data spatially to find likeness and tension. Here, you may use a grounded theory approach to drag and drop notes into themes or patterns that emerge in your research. Utilizing the canvas tools such as shapes, lines, and images, allows researchers to build out frameworks such as journey maps, empathy maps, 2x2's, etc. to help synthesize their data.
Going one step further, you may begin to apply various lenses to this data driven canvas. For example, recoloring by sentiment shows where pain points may distributed across your customer journey. Or, recoloring by participant may reveal if one of your participants may be creating a bias towards a particular theme.

Exploring Qualitative Data through a Quantitative Lens
Once you have begun your analysis, you may visualize your qualitative data in a quantitative way through charts. You may choose between a pie chart and or a stacked bar chart to visualize your data. From here, you can segment your data to break down the ‘bar’ in your bar chart and slices in your pie chart one step further.
To segment your data, you can choose between ‘Tag group’, ‘Tag’, ‘Theme’, and ‘Participant'. Each group shows up as its own bar in the bar chart or slice in the pie chart. For example, try grouping data as ‘Participant’ to see the volume of notes assigned to each person. Or, group by ‘Tag group’ to see which of your tag groups have the most notes.
Depending on how you’ve grouped or segmented your charts will affect the options available to color your chart. Charts use colors that are a mix of sentiment, tag, theme, and default colors. Consider color as a way of assigning another layer of meaning to your data. For example, choose a red color for tags or themes that are areas of friction or pain points. Use blue for tags that represent opportunities.

AI Powered Insights and Cover Images
One of the most powerful features in Analysis is the ability to generate insights with AI. Insights combine information, inspiration, and intuition to help bridge the gap between knowledge and wisdom. Even before you have any tags or themes, you may generate an AI Insight from your entire data set. You'll be able to choose one of our AI Insight templates that are inspired by trusted design thinking frameworks to stimulate generative, and divergent thinking. With just the click of a button, you'll get an insight that captures the essence and story of your research. You may experiment with a combination of tags, themes, and different templates or, create your own custom AI template. These insights are all evidence-based, and are centered on the needs of real people. You may package these insights up to present your research by embedding videos, quotes and using AI to generate unique cover image.

You can sign up to run an end to end research project for free and receive tips on how to make the most out of your data. Want to chat about how Notably can help your team do better, faster research? Book some time here for a 1:1 demo with your whole team.

Meet Posty: Your AI Research Assistant for Automatic Analysis

Introducing Notably + Miro Integration: 3 Tips to Analyze Miro Boards with AI in Notably
Give your research synthesis superpowers..
Try Teams for 7 days
Free for 1 project

- UNC Libraries
- HSL Subject Research
- Qualitative Research Resources
- Presenting Qualitative Research
Qualitative Research Resources: Presenting Qualitative Research
Created by health science librarians.

- What is Qualitative Research?
- Qualitative Research Basics
- Special Topics
- Training Opportunities: UNC & Beyond
- Help at UNC
- Qualitative Software for Coding/Analysis
- Software for Audio, Video, Online Surveys
- Finding Qualitative Studies
- Assessing Qualitative Research
- Writing Up Your Research
- Integrating Qualitative Research into Systematic Reviews
- Publishing Qualitative Research
Presenting Qualitative Research, with a focus on posters
- Qualitative & Libraries: a few gems
- Data Repositories
Example posters
- The Meaning of Work for People with MS: a Qualitative Study A good example with quotes
- Fostering Empathy through Design Thinking Among Fourth Graders in Trinidad and Tobago Includes quotes, photos, diagrams, and other artifacts from qualitative study
- Examining the Use and Perception of Harm of JUULs by College Students: A Qualitative Study Another interesting example to consider
- NLM Informationist Supplement Grant: Daring to Dive into Documentation to Determine Impact An example from the Carolina Digital Repository discussed in a class more... less... Allegri, F., Hayes, B., & Renner, B. (2017). NLM Informationist Supplement Grant: Daring to Dive into Documentation to Determine Impact. https://doi.org/10.17615/bk34-p037
- Qualitative Posters in F1000 Research Archive (filtered on "qualitative" in title) Sample qualitative posters
- Qualitative Posters in F1000 Research Archive (filtered on "qualitative" in keywords) Sample qualitative posters
Michelle A. Krieger Blog (example, posts follow an APA convention poster experience with qualitative posters):
- Qualitative Data and Research Posters I
- Qualitative Data and Research Posters II
"Oldies but goodies":
- How to Visualize Qualitative Data: Ann K. Emery, September 25, 2014 Data Visualization / Chart Choosing, Color-Coding by Category, Diagrams, Icons, Photographs, Qualitative, Text, Timelines, Word Clouds more... less... Getting a little older, and a commercial site, but with some good ideas to get you think.
- Russell, C. K., Gregory, D. M., & Gates, M. F. (1996). Aesthetics and Substance in Qualitative Research Posters. Qualitative Health Research, 6(4), 542–552. Older article with much good information. Poster materials section less applicable.Link is for UNC-Chapel Hill affiliated users.
Additional resources
- CDC Coffee Break: Considerations for Presenting Qualitative Data (Mark D. Rivera, March 13, 2018) PDF download of slide presentation. Display formats section begins on slide 10.
- Print Book (Davis Library): Miles, M. B., Huberman, A. M., & Saldaña, J. (2014). Qualitative data analysis: A methods sourcebook, 3rd edition From Paul Mihas, Assistant Director of Education and Qualitative Research at the Odum Institute for Research in Social Science at UNC: Qualitative Data Analysis: A Methods Sourcebook (4th ed.) by Miles, Huberman, and Saldana has a section on Displaying the Data (and a chapter on Designing Matrix, Network, and Graphic Displays) that can help students consider numerous options for visually synthesizing data and findings. Many of the suggestions can be applied to designing posters (April 15, 2021).
- << Previous: Publishing Qualitative Research
- Next: Qualitative & Libraries: a few gems >>
- Last Updated: Jul 28, 2024 4:11 PM
- URL: https://guides.lib.unc.edu/qual
blog @ precision
Presenting your qualitative analysis findings: tables to include in chapter 4.
The earliest stages of developing a doctoral dissertation—most specifically the topic development and literature review stages—require that you immerse yourself in a ton of existing research related to your potential topic. If you have begun writing your dissertation proposal, you have undoubtedly reviewed countless results and findings sections of studies in order to help gain an understanding of what is currently known about your topic.
In this process, we’re guessing that you observed a distinct pattern: Results sections are full of tables. Indeed, the results chapter for your own dissertation will need to be similarly packed with tables. So, if you’re preparing to write up the results of your statistical analysis or qualitative analysis, it will probably help to review your APA editing manual to brush up on your table formatting skills. But, aside from formatting, how should you develop the tables in your results chapter?
In quantitative studies, tables are a handy way of presenting the variety of statistical analysis results in a form that readers can easily process. You’ve probably noticed that quantitative studies present descriptive results like mean, mode, range, standard deviation, etc., as well the inferential results that indicate whether significant relationships or differences were found through the statistical analysis . These are pretty standard tables that you probably learned about in your pre-dissertation statistics courses.
But, what if you are conducting qualitative analysis? What tables are appropriate for this type of study? This is a question we hear often from our dissertation assistance clients, and with good reason. University guidelines for results chapters often contain vague instructions that guide you to include “appropriate tables” without specifying what exactly those are. To help clarify on this point, we asked our qualitative analysis experts to share their recommendations for tables to include in your Chapter 4.
Demographics Tables
As with studies using quantitative methods , presenting an overview of your sample demographics is useful in studies that use qualitative research methods. The standard demographics table in a quantitative study provides aggregate information for what are often large samples. In other words, such tables present totals and percentages for demographic categories within the sample that are relevant to the study (e.g., age, gender, job title).

If conducting qualitative research for your dissertation, however, you will use a smaller sample and obtain richer data from each participant than in quantitative studies. To enhance thick description—a dimension of trustworthiness—it will help to present sample demographics in a table that includes information on each participant. Remember that ethical standards of research require that all participant information be deidentified, so use participant identification numbers or pseudonyms for each participant, and do not present any personal information that would allow others to identify the participant (Blignault & Ritchie, 2009). Table 1 provides participant demographics for a hypothetical qualitative research study exploring the perspectives of persons who were formerly homeless regarding their experiences of transitioning into stable housing and obtaining employment.
Participant Demographics
| Participant ID | Gender | Age | Current Living Situation |
| P1 | Female | 34 | Alone |
| P2 | Male | 27 | With Family |
| P3 | Male | 44 | Alone |
| P4 | Female | 46 | With Roommates |
| P5 | Female | 25 | With Family |
| P6 | Male | 30 | With Roommates |
| P7 | Male | 38 | With Roommates |
| P8 | Male | 51 | Alone |
Tables to Illustrate Initial Codes
Most of our dissertation consulting clients who are conducting qualitative research choose a form of thematic analysis . Qualitative analysis to identify themes in the data typically involves a progression from (a) identifying surface-level codes to (b) developing themes by combining codes based on shared similarities. As this process is inherently subjective, it is important that readers be able to evaluate the correspondence between the data and your findings (Anfara et al., 2002). This supports confirmability, another dimension of trustworthiness .
A great way to illustrate the trustworthiness of your qualitative analysis is to create a table that displays quotes from the data that exemplify each of your initial codes. Providing a sample quote for each of your codes can help the reader to assess whether your coding was faithful to the meanings in the data, and it can also help to create clarity about each code’s meaning and bring the voices of your participants into your work (Blignault & Ritchie, 2009).

Table 2 is an example of how you might present information regarding initial codes. Depending on your preference or your dissertation committee’s preference, you might also present percentages of the sample that expressed each code. Another common piece of information to include is which actual participants expressed each code. Note that if your qualitative analysis yields a high volume of codes, it may be appropriate to present the table as an appendix.
Initial Codes
| Initial code | of participants contributing ( =8) | of transcript excerpts assigned | Sample quote |
|---|---|---|---|
| Daily routine of going to work enhanced sense of identity | 7 | 12 | “It’s just that good feeling of getting up every day like everyone else and going to work, of having that pattern that’s responsible. It makes you feel good about yourself again.” (P3) |
| Experienced discrimination due to previous homelessness | 2 | 3 | “At my last job, I told a couple other people on my shift I used to be homeless, and then, just like that, I get put into a worse job with less pay. The boss made some excuse why they did that, but they didn’t want me handling the money is why. They put me in a lower level job two days after I talk to people about being homeless in my past. That’s no coincidence if you ask me.” (P6) |
| Friends offered shared housing | 3 | 3 | “My friend from way back had a spare room after her kid moved out. She let me stay there until I got back on my feet.” (P4) |
| Mental health services essential in getting into housing | 5 | 7 | “Getting my addiction treated was key. That was a must. My family wasn’t gonna let me stay around their place without it. So that was a big help for getting back into a place.” (P2) |
Tables to Present the Groups of Codes That Form Each Theme
As noted previously, most of our dissertation assistance clients use a thematic analysis approach, which involves multiple phases of qualitative analysis that eventually result in themes that answer the dissertation’s research questions. After initial coding is completed, the analysis process involves (a) examining what different codes have in common and then (b) grouping similar codes together in ways that are meaningful given your research questions. In other words, the common threads that you identify across multiple codes become the theme that holds them all together—and that theme answers one of your research questions.
As with initial coding, grouping codes together into themes involves your own subjective interpretations, even when aided by qualitative analysis software such as NVivo or MAXQDA. In fact, our dissertation assistance clients are often surprised to learn that qualitative analysis software does not complete the analysis in the same ways that statistical analysis software such as SPSS does. While statistical analysis software completes the computations for you, qualitative analysis software does not have such analysis capabilities. Software such as NVivo provides a set of organizational tools that make the qualitative analysis far more convenient, but the analysis itself is still a very human process (Burnard et al., 2008).

Because of the subjective nature of qualitative analysis, it is important to show the underlying logic behind your thematic analysis in tables—such tables help readers to assess the trustworthiness of your analysis. Table 3 provides an example of how to present the codes that were grouped together to create themes, and you can modify the specifics of the table based on your preferences or your dissertation committee’s requirements. For example, this type of table might be presented to illustrate the codes associated with themes that answer each research question.
Grouping of Initial Codes to Form Themes
| Theme Initial codes grouped to form theme | of participants contributing ( =8) | of transcript excerpts assigned |
| Assistance from friends, family, or strangers was instrumental in getting back into stable housing | 6 | 10 |
| Family member assisted them to get into housing | ||
| Friends offered shared housing | ||
| Stranger offered shared housing | ||
| Obtaining professional support was essential for overcoming the cascading effects of poverty and homelessness | 7 | 19 |
| Financial benefits made obtaining housing possible | ||
| Mental health services essential in getting into housing | ||
| Social services helped navigate housing process | ||
| Stigma and concerns about discrimination caused them to feel uncomfortable socializing with coworkers | 6 | 9 |
| Experienced discrimination due to previous homelessness | ||
| Feared negative judgment if others learned of their pasts | ||
| Routine productivity and sense of making a contribution helped to restore self-concept and positive social identity | 8 | 21 |
| Daily routine of going to work enhanced sense of identity | ||
| Feels good to contribute to society/organization | ||
| Seeing products of their efforts was rewarding |
Tables to Illustrate the Themes That Answer Each Research Question
Creating alignment throughout your dissertation is an important objective, and to maintain alignment in your results chapter, the themes you present must clearly answer your research questions. Conducting qualitative analysis is an in-depth process of immersion in the data, and many of our dissertation consulting clients have shared that it’s easy to lose your direction during the process. So, it is important to stay focused on your research questions during the qualitative analysis and also to show the reader exactly which themes—and subthemes, as applicable—answered each of the research questions.

Below, Table 4 provides an example of how to display the thematic findings of your study in table form. Depending on your dissertation committee’s preference or your own, you might present all research questions and all themes and subthemes in a single table. Or, you might provide separate tables to introduce the themes for each research question as you progress through your presentation of the findings in the chapter.
Emergent Themes and Research Questions
| Research question
| Themes that address question
|
| RQ1. How do adults who have previously experienced homelessness describe their transitions to stable housing?
| Theme 1: Assistance from friends, family, or strangers was instrumental in getting back into stable housing Theme 2: Obtaining professional support was essential for overcoming the cascading effects of poverty and homelessness
|
| RQ2. How do adults who have previously experienced homelessness describe returning to paid employment?
| Theme 3: Self-perceived stigma caused them to feel uncomfortable socializing with coworkers Theme 4: Routine productivity and sense of making a contribution helped to restore self-concept and positive social identity |
Bonus Tip! Figures to Spice Up Your Results
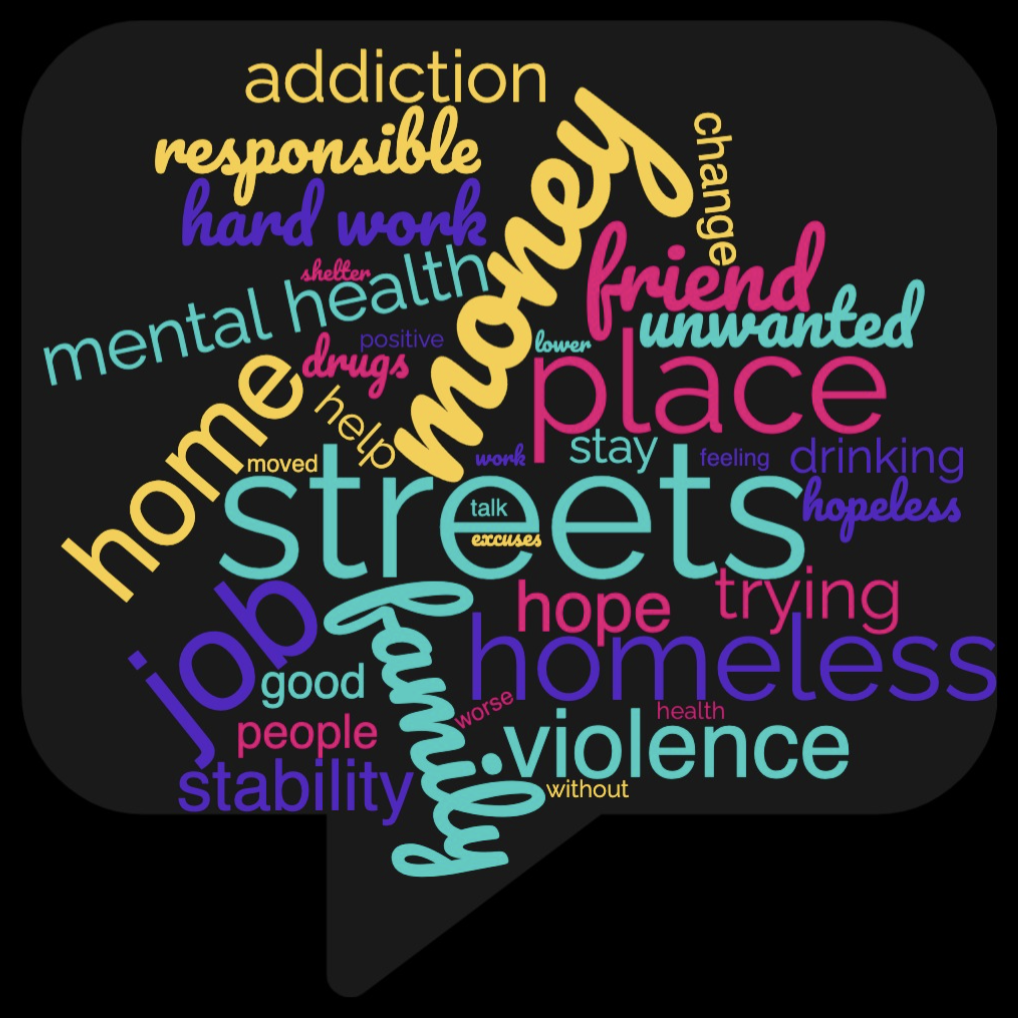
Although dissertation committees most often wish to see tables such as the above in qualitative results chapters, some also like to see figures that illustrate the data. Qualitative software packages such as NVivo offer many options for visualizing your data, such as mind maps, concept maps, charts, and cluster diagrams. A common choice for this type of figure among our dissertation assistance clients is a tree diagram, which shows the connections between specified words and the words or phrases that participants shared most often in the same context. Another common choice of figure is the word cloud, as depicted in Figure 1. The word cloud simply reflects frequencies of words in the data, which may provide an indication of the importance of related concepts for the participants.
As you move forward with your qualitative analysis and development of your results chapter, we hope that this brief overview of useful tables and figures helps you to decide on an ideal presentation to showcase the trustworthiness your findings. Completing a rigorous qualitative analysis for your dissertation requires many hours of careful interpretation of your data, and your end product should be a rich and detailed results presentation that you can be proud of. Reach out if we can help in any way, as our dissertation coaches would be thrilled to assist as you move through this exciting stage of your dissertation journey!
Anfara Jr., V. A., Brown, K. M., & Mangione, T. L. (2002). Qualitative analysis on stage: Making the research process more public. Educational Researcher , 31 (7), 28-38. https://doi.org/10.3102/0013189X031007028
Blignault, I., & Ritchie, J. (2009). Revealing the wood and the trees: Reporting qualitative research. Health Promotion Journal of Australia , 20 (2), 140-145. https://doi.org/10.1071/HE09140
Burnard, P., Gill, P., Stewart, K., Treasure, E., & Chadwick, B. (2008). Analysing and presenting qualitative data. British Dental Journal , 204 (8), 429-432. https://doi.org/10.1038/sj.bdj.2008.292

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Qualitative Data Analysis
23 Presenting the Results of Qualitative Analysis
Mikaila Mariel Lemonik Arthur
Qualitative research is not finished just because you have determined the main findings or conclusions of your study. Indeed, disseminating the results is an essential part of the research process. By sharing your results with others, whether in written form as scholarly paper or an applied report or in some alternative format like an oral presentation, an infographic, or a video, you ensure that your findings become part of the ongoing conversation of scholarship in your field, forming part of the foundation for future researchers. This chapter provides an introduction to writing about qualitative research findings. It will outline how writing continues to contribute to the analysis process, what concerns researchers should keep in mind as they draft their presentations of findings, and how best to organize qualitative research writing
As you move through the research process, it is essential to keep yourself organized. Organizing your data, memos, and notes aids both the analytical and the writing processes. Whether you use electronic or physical, real-world filing and organizational systems, these systems help make sense of the mountains of data you have and assure you focus your attention on the themes and ideas you have determined are important (Warren and Karner 2015). Be sure that you have kept detailed notes on all of the decisions you have made and procedures you have followed in carrying out research design, data collection, and analysis, as these will guide your ultimate write-up.
First and foremost, researchers should keep in mind that writing is in fact a form of thinking. Writing is an excellent way to discover ideas and arguments and to further develop an analysis. As you write, more ideas will occur to you, things that were previously confusing will start to make sense, and arguments will take a clear shape rather than being amorphous and poorly-organized. However, writing-as-thinking cannot be the final version that you share with others. Good-quality writing does not display the workings of your thought process. It is reorganized and revised (more on that later) to present the data and arguments important in a particular piece. And revision is totally normal! No one expects the first draft of a piece of writing to be ready for prime time. So write rough drafts and memos and notes to yourself and use them to think, and then revise them until the piece is the way you want it to be for sharing.
Bergin (2018) lays out a set of key concerns for appropriate writing about research. First, present your results accurately, without exaggerating or misrepresenting. It is very easy to overstate your findings by accident if you are enthusiastic about what you have found, so it is important to take care and use appropriate cautions about the limitations of the research. You also need to work to ensure that you communicate your findings in a way people can understand, using clear and appropriate language that is adjusted to the level of those you are communicating with. And you must be clear and transparent about the methodological strategies employed in the research. Remember, the goal is, as much as possible, to describe your research in a way that would permit others to replicate the study. There are a variety of other concerns and decision points that qualitative researchers must keep in mind, including the extent to which to include quantification in their presentation of results, ethics, considerations of audience and voice, and how to bring the richness of qualitative data to life.
Quantification, as you have learned, refers to the process of turning data into numbers. It can indeed be very useful to count and tabulate quantitative data drawn from qualitative research. For instance, if you were doing a study of dual-earner households and wanted to know how many had an equal division of household labor and how many did not, you might want to count those numbers up and include them as part of the final write-up. However, researchers need to take care when they are writing about quantified qualitative data. Qualitative data is not as generalizable as quantitative data, so quantification can be very misleading. Thus, qualitative researchers should strive to use raw numbers instead of the percentages that are more appropriate for quantitative research. Writing, for instance, “15 of the 20 people I interviewed prefer pancakes to waffles” is a simple description of the data; writing “75% of people prefer pancakes” suggests a generalizable claim that is not likely supported by the data. Note that mixing numbers with qualitative data is really a type of mixed-methods approach. Mixed-methods approaches are good, but sometimes they seduce researchers into focusing on the persuasive power of numbers and tables rather than capitalizing on the inherent richness of their qualitative data.
A variety of issues of scholarly ethics and research integrity are raised by the writing process. Some of these are unique to qualitative research, while others are more universal concerns for all academic and professional writing. For example, it is essential to avoid plagiarism and misuse of sources. All quotations that appear in a text must be properly cited, whether with in-text and bibliographic citations to the source or with an attribution to the research participant (or the participant’s pseudonym or description in order to protect confidentiality) who said those words. Where writers will paraphrase a text or a participant’s words, they need to make sure that the paraphrase they develop accurately reflects the meaning of the original words. Thus, some scholars suggest that participants should have the opportunity to read (or to have read to them, if they cannot read the text themselves) all sections of the text in which they, their words, or their ideas are presented to ensure accuracy and enable participants to maintain control over their lives.
Audience and Voice
When writing, researchers must consider their audience(s) and the effects they want their writing to have on these audiences. The designated audience will dictate the voice used in the writing, or the individual style and personality of a piece of text. Keep in mind that the potential audience for qualitative research is often much more diverse than that for quantitative research because of the accessibility of the data and the extent to which the writing can be accessible and interesting. Yet individual pieces of writing are typically pitched to a more specific subset of the audience.
Let us consider one potential research study, an ethnography involving participant-observation of the same children both when they are at daycare facility and when they are at home with their families to try to understand how daycare might impact behavior and social development. The findings of this study might be of interest to a wide variety of potential audiences: academic peers, whether at your own academic institution, in your broader discipline, or multidisciplinary; people responsible for creating laws and policies; practitioners who run or teach at day care centers; and the general public, including both people who are interested in child development more generally and those who are themselves parents making decisions about child care for their own children. And the way you write for each of these audiences will be somewhat different. Take a moment and think through what some of these differences might look like.
If you are writing to academic audiences, using specialized academic language and working within the typical constraints of scholarly genres, as will be discussed below, can be an important part of convincing others that your work is legitimate and should be taken seriously. Your writing will be formal. Even if you are writing for students and faculty you already know—your classmates, for instance—you are often asked to imitate the style of academic writing that is used in publications, as this is part of learning to become part of the scholarly conversation. When speaking to academic audiences outside your discipline, you may need to be more careful about jargon and specialized language, as disciplines do not always share the same key terms. For instance, in sociology, scholars use the term diffusion to refer to the way new ideas or practices spread from organization to organization. In the field of international relations, scholars often used the term cascade to refer to the way ideas or practices spread from nation to nation. These terms are describing what is fundamentally the same concept, but they are different terms—and a scholar from one field might have no idea what a scholar from a different field is talking about! Therefore, while the formality and academic structure of the text would stay the same, a writer with a multidisciplinary audience might need to pay more attention to defining their terms in the body of the text.
It is not only other academic scholars who expect to see formal writing. Policymakers tend to expect formality when ideas are presented to them, as well. However, the content and style of the writing will be different. Much less academic jargon should be used, and the most important findings and policy implications should be emphasized right from the start rather than initially focusing on prior literature and theoretical models as you might for an academic audience. Long discussions of research methods should also be minimized. Similarly, when you write for practitioners, the findings and implications for practice should be highlighted. The reading level of the text will vary depending on the typical background of the practitioners to whom you are writing—you can make very different assumptions about the general knowledge and reading abilities of a group of hospital medical directors with MDs than you can about a group of case workers who have a post-high-school certificate. Consider the primary language of your audience as well. The fact that someone can get by in spoken English does not mean they have the vocabulary or English reading skills to digest a complex report. But the fact that someone’s vocabulary is limited says little about their intellectual abilities, so try your best to convey the important complexity of the ideas and findings from your research without dumbing them down—even if you must limit your vocabulary usage.
When writing for the general public, you will want to move even further towards emphasizing key findings and policy implications, but you also want to draw on the most interesting aspects of your data. General readers will read sociological texts that are rich with ethnographic or other kinds of detail—it is almost like reality television on a page! And this is a contrast to busy policymakers and practitioners, who probably want to learn the main findings as quickly as possible so they can go about their busy lives. But also keep in mind that there is a wide variation in reading levels. Journalists at publications pegged to the general public are often advised to write at about a tenth-grade reading level, which would leave most of the specialized terminology we develop in our research fields out of reach. If you want to be accessible to even more people, your vocabulary must be even more limited. The excellent exercise of trying to write using the 1,000 most common English words, available at the Up-Goer Five website ( https://www.splasho.com/upgoer5/ ) does a good job of illustrating this challenge (Sanderson n.d.).
Another element of voice is whether to write in the first person. While many students are instructed to avoid the use of the first person in academic writing, this advice needs to be taken with a grain of salt. There are indeed many contexts in which the first person is best avoided, at least as long as writers can find ways to build strong, comprehensible sentences without its use, including most quantitative research writing. However, if the alternative to using the first person is crafting a sentence like “it is proposed that the researcher will conduct interviews,” it is preferable to write “I propose to conduct interviews.” In qualitative research, in fact, the use of the first person is far more common. This is because the researcher is central to the research project. Qualitative researchers can themselves be understood as research instruments, and thus eliminating the use of the first person in writing is in a sense eliminating information about the conduct of the researchers themselves.
But the question really extends beyond the issue of first-person or third-person. Qualitative researchers have choices about how and whether to foreground themselves in their writing, not just in terms of using the first person, but also in terms of whether to emphasize their own subjectivity and reflexivity, their impressions and ideas, and their role in the setting. In contrast, conventional quantitative research in the positivist tradition really tries to eliminate the author from the study—which indeed is exactly why typical quantitative research avoids the use of the first person. Keep in mind that emphasizing researchers’ roles and reflexivity and using the first person does not mean crafting articles that provide overwhelming detail about the author’s thoughts and practices. Readers do not need to hear, and should not be told, which database you used to search for journal articles, how many hours you spent transcribing, or whether the research process was stressful—save these things for the memos you write to yourself. Rather, readers need to hear how you interacted with research participants, how your standpoint may have shaped the findings, and what analytical procedures you carried out.
Making Data Come Alive
One of the most important parts of writing about qualitative research is presenting the data in a way that makes its richness and value accessible to readers. As the discussion of analysis in the prior chapter suggests, there are a variety of ways to do this. Researchers may select key quotes or images to illustrate points, write up specific case studies that exemplify their argument, or develop vignettes (little stories) that illustrate ideas and themes, all drawing directly on the research data. Researchers can also write more lengthy summaries, narratives, and thick descriptions.
Nearly all qualitative work includes quotes from research participants or documents to some extent, though ethnographic work may focus more on thick description than on relaying participants’ own words. When quotes are presented, they must be explained and interpreted—they cannot stand on their own. This is one of the ways in which qualitative research can be distinguished from journalism. Journalism presents what happened, but social science needs to present the “why,” and the why is best explained by the researcher.
So how do authors go about integrating quotes into their written work? Julie Posselt (2017), a sociologist who studies graduate education, provides a set of instructions. First of all, authors need to remain focused on the core questions of their research, and avoid getting distracted by quotes that are interesting or attention-grabbing but not so relevant to the research question. Selecting the right quotes, those that illustrate the ideas and arguments of the paper, is an important part of the writing process. Second, not all quotes should be the same length (just like not all sentences or paragraphs in a paper should be the same length). Include some quotes that are just phrases, others that are a sentence or so, and others that are longer. We call longer quotes, generally those more than about three lines long, block quotes , and they are typically indented on both sides to set them off from the surrounding text. For all quotes, be sure to summarize what the quote should be telling or showing the reader, connect this quote to other quotes that are similar or different, and provide transitions in the discussion to move from quote to quote and from topic to topic. Especially for longer quotes, it is helpful to do some of this writing before the quote to preview what is coming and other writing after the quote to make clear what readers should have come to understand. Remember, it is always the author’s job to interpret the data. Presenting excerpts of the data, like quotes, in a form the reader can access does not minimize the importance of this job. Be sure that you are explaining the meaning of the data you present.
A few more notes about writing with quotes: avoid patchwriting, whether in your literature review or the section of your paper in which quotes from respondents are presented. Patchwriting is a writing practice wherein the author lightly paraphrases original texts but stays so close to those texts that there is little the author has added. Sometimes, this even takes the form of presenting a series of quotes, properly documented, with nothing much in the way of text generated by the author. A patchwriting approach does not build the scholarly conversation forward, as it does not represent any kind of new contribution on the part of the author. It is of course fine to paraphrase quotes, as long as the meaning is not changed. But if you use direct quotes, do not edit the text of the quotes unless how you edit them does not change the meaning and you have made clear through the use of ellipses (…) and brackets ([])what kinds of edits have been made. For example, consider this exchange from Matthew Desmond’s (2012:1317) research on evictions:
The thing was, I wasn’t never gonna let Crystal come and stay with me from the get go. I just told her that to throw her off. And she wasn’t fittin’ to come stay with me with no money…No. Nope. You might as well stay in that shelter.
A paraphrase of this exchange might read “She said that she was going to let Crystal stay with her if Crystal did not have any money.” Paraphrases like that are fine. What is not fine is rewording the statement but treating it like a quote, for instance writing:
The thing was, I was not going to let Crystal come and stay with me from beginning. I just told her that to throw her off. And it was not proper for her to come stay with me without any money…No. Nope. You might as well stay in that shelter.
But as you can see, the change in language and style removes some of the distinct meaning of the original quote. Instead, writers should leave as much of the original language as possible. If some text in the middle of the quote needs to be removed, as in this example, ellipses are used to show that this has occurred. And if a word needs to be added to clarify, it is placed in square brackets to show that it was not part of the original quote.
Data can also be presented through the use of data displays like tables, charts, graphs, diagrams, and infographics created for publication or presentation, as well as through the use of visual material collected during the research process. Note that if visuals are used, the author must have the legal right to use them. Photographs or diagrams created by the author themselves—or by research participants who have signed consent forms for their work to be used, are fine. But photographs, and sometimes even excerpts from archival documents, may be owned by others from whom researchers must get permission in order to use them.
A large percentage of qualitative research does not include any data displays or visualizations. Therefore, researchers should carefully consider whether the use of data displays will help the reader understand the data. One of the most common types of data displays used by qualitative researchers are simple tables. These might include tables summarizing key data about cases included in the study; tables laying out the characteristics of different taxonomic elements or types developed as part of the analysis; tables counting the incidence of various elements; and 2×2 tables (two columns and two rows) illuminating a theory. Basic network or process diagrams are also commonly included. If data displays are used, it is essential that researchers include context and analysis alongside data displays rather than letting them stand by themselves, and it is preferable to continue to present excerpts and examples from the data rather than just relying on summaries in the tables.
If you will be using graphs, infographics, or other data visualizations, it is important that you attend to making them useful and accurate (Bergin 2018). Think about the viewer or user as your audience and ensure the data visualizations will be comprehensible. You may need to include more detail or labels than you might think. Ensure that data visualizations are laid out and labeled clearly and that you make visual choices that enhance viewers’ ability to understand the points you intend to communicate using the visual in question. Finally, given the ease with which it is possible to design visuals that are deceptive or misleading, it is essential to make ethical and responsible choices in the construction of visualization so that viewers will interpret them in accurate ways.
The Genre of Research Writing
As discussed above, the style and format in which results are presented depends on the audience they are intended for. These differences in styles and format are part of the genre of writing. Genre is a term referring to the rules of a specific form of creative or productive work. Thus, the academic journal article—and student papers based on this form—is one genre. A report or policy paper is another. The discussion below will focus on the academic journal article, but note that reports and policy papers follow somewhat different formats. They might begin with an executive summary of one or a few pages, include minimal background, focus on key findings, and conclude with policy implications, shifting methods and details about the data to an appendix. But both academic journal articles and policy papers share some things in common, for instance the necessity for clear writing, a well-organized structure, and the use of headings.
So what factors make up the genre of the academic journal article in sociology? While there is some flexibility, particularly for ethnographic work, academic journal articles tend to follow a fairly standard format. They begin with a “title page” that includes the article title (often witty and involving scholarly inside jokes, but more importantly clearly describing the content of the article); the authors’ names and institutional affiliations, an abstract , and sometimes keywords designed to help others find the article in databases. An abstract is a short summary of the article that appears both at the very beginning of the article and in search databases. Abstracts are designed to aid readers by giving them the opportunity to learn enough about an article that they can determine whether it is worth their time to read the complete text. They are written about the article, and thus not in the first person, and clearly summarize the research question, methodological approach, main findings, and often the implications of the research.
After the abstract comes an “introduction” of a page or two that details the research question, why it matters, and what approach the paper will take. This is followed by a literature review of about a quarter to a third the length of the entire paper. The literature review is often divided, with headings, into topical subsections, and is designed to provide a clear, thorough overview of the prior research literature on which a paper has built—including prior literature the new paper contradicts. At the end of the literature review it should be made clear what researchers know about the research topic and question, what they do not know, and what this new paper aims to do to address what is not known.
The next major section of the paper is the section that describes research design, data collection, and data analysis, often referred to as “research methods” or “methodology.” This section is an essential part of any written or oral presentation of your research. Here, you tell your readers or listeners “how you collected and interpreted your data” (Taylor, Bogdan, and DeVault 2016:215). Taylor, Bogdan, and DeVault suggest that the discussion of your research methods include the following:
- The particular approach to data collection used in the study;
- Any theoretical perspective(s) that shaped your data collection and analytical approach;
- When the study occurred, over how long, and where (concealing identifiable details as needed);
- A description of the setting and participants, including sampling and selection criteria (if an interview-based study, the number of participants should be clearly stated);
- The researcher’s perspective in carrying out the study, including relevant elements of their identity and standpoint, as well as their role (if any) in research settings; and
- The approach to analyzing the data.
After the methods section comes a section, variously titled but often called “data,” that takes readers through the analysis. This section is where the thick description narrative; the quotes, broken up by theme or topic, with their interpretation; the discussions of case studies; most data displays (other than perhaps those outlining a theoretical model or summarizing descriptive data about cases); and other similar material appears. The idea of the data section is to give readers the ability to see the data for themselves and to understand how this data supports the ultimate conclusions. Note that all tables and figures included in formal publications should be titled and numbered.
At the end of the paper come one or two summary sections, often called “discussion” and/or “conclusion.” If there is a separate discussion section, it will focus on exploring the overall themes and findings of the paper. The conclusion clearly and succinctly summarizes the findings and conclusions of the paper, the limitations of the research and analysis, any suggestions for future research building on the paper or addressing these limitations, and implications, be they for scholarship and theory or policy and practice.
After the end of the textual material in the paper comes the bibliography, typically called “works cited” or “references.” The references should appear in a consistent citation style—in sociology, we often use the American Sociological Association format (American Sociological Association 2019), but other formats may be used depending on where the piece will eventually be published. Care should be taken to ensure that in-text citations also reflect the chosen citation style. In some papers, there may be an appendix containing supplemental information such as a list of interview questions or an additional data visualization.
Note that when researchers give presentations to scholarly audiences, the presentations typically follow a format similar to that of scholarly papers, though given time limitations they are compressed. Abstracts and works cited are often not part of the presentation, though in-text citations are still used. The literature review presented will be shortened to only focus on the most important aspects of the prior literature, and only key examples from the discussion of data will be included. For long or complex papers, sometimes only one of several findings is the focus of the presentation. Of course, presentations for other audiences may be constructed differently, with greater attention to interesting elements of the data and findings as well as implications and less to the literature review and methods.
Concluding Your Work
After you have written a complete draft of the paper, be sure you take the time to revise and edit your work. There are several important strategies for revision. First, put your work away for a little while. Even waiting a day to revise is better than nothing, but it is best, if possible, to take much more time away from the text. This helps you forget what your writing looks like and makes it easier to find errors, mistakes, and omissions. Second, show your work to others. Ask them to read your work and critique it, pointing out places where the argument is weak, where you may have overlooked alternative explanations, where the writing could be improved, and what else you need to work on. Finally, read your work out loud to yourself (or, if you really need an audience, try reading to some stuffed animals). Reading out loud helps you catch wrong words, tricky sentences, and many other issues. But as important as revision is, try to avoid perfectionism in writing (Warren and Karner 2015). Writing can always be improved, no matter how much time you spend on it. Those improvements, however, have diminishing returns, and at some point the writing process needs to conclude so the writing can be shared with the world.
Of course, the main goal of writing up the results of a research project is to share with others. Thus, researchers should be considering how they intend to disseminate their results. What conferences might be appropriate? Where can the paper be submitted? Note that if you are an undergraduate student, there are a wide variety of journals that accept and publish research conducted by undergraduates. Some publish across disciplines, while others are specific to disciplines. Other work, such as reports, may be best disseminated by publication online on relevant organizational websites.
After a project is completed, be sure to take some time to organize your research materials and archive them for longer-term storage. Some Institutional Review Board (IRB) protocols require that original data, such as interview recordings, transcripts, and field notes, be preserved for a specific number of years in a protected (locked for paper or password-protected for digital) form and then destroyed, so be sure that your plans adhere to the IRB requirements. Be sure you keep any materials that might be relevant for future related research or for answering questions people may ask later about your project.
And then what? Well, then it is time to move on to your next research project. Research is a long-term endeavor, not a one-time-only activity. We build our skills and our expertise as we continue to pursue research. So keep at it.
- Find a short article that uses qualitative methods. The sociological magazine Contexts is a good place to find such pieces. Write an abstract of the article.
- Choose a sociological journal article on a topic you are interested in that uses some form of qualitative methods and is at least 20 pages long. Rewrite the article as a five-page research summary accessible to non-scholarly audiences.
- Choose a concept or idea you have learned in this course and write an explanation of it using the Up-Goer Five Text Editor ( https://www.splasho.com/upgoer5/ ), a website that restricts your writing to the 1,000 most common English words. What was this experience like? What did it teach you about communicating with people who have a more limited English-language vocabulary—and what did it teach you about the utility of having access to complex academic language?
- Select five or more sociological journal articles that all use the same basic type of qualitative methods (interviewing, ethnography, documents, or visual sociology). Using what you have learned about coding, code the methods sections of each article, and use your coding to figure out what is common in how such articles discuss their research design, data collection, and analysis methods.
- Return to an exercise you completed earlier in this course and revise your work. What did you change? How did revising impact the final product?
- Find a quote from the transcript of an interview, a social media post, or elsewhere that has not yet been interpreted or explained. Write a paragraph that includes the quote along with an explanation of its sociological meaning or significance.
The style or personality of a piece of writing, including such elements as tone, word choice, syntax, and rhythm.
A quotation, usually one of some length, which is set off from the main text by being indented on both sides rather than being placed in quotation marks.
A classification of written or artistic work based on form, content, and style.
A short summary of a text written from the perspective of a reader rather than from the perspective of an author.
Social Data Analysis Copyright © 2021 by Mikaila Mariel Lemonik Arthur is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.

No products in the cart.
Preparing the presentation of qualitative findings: considering your roles and goals

Dr. Philip Adu is a Methodology Expert at The Chicago School of Professional Psychology (TCSPP). In this post he explains the things to consider when presenting your research findings.
This post follows on from his previous blog post “Perfecting the art of qualitative coding” in which he took us through the stages of qualitative coding and, along the way, outlined the features he found most useful.
In my previous blog post, I presented on making good use of the innovative features of NVivo across the three main stages of qualitative analysis. Expounding on the third stage which is the ‘ Post-Coding stage (Presenting your findings) ’, I want to throw light on things to consider when drafting and refining your presentation. The moment you reach a milestone of successfully using NVivo 12 (Version 12.1.249; QSR International Pty Ltd, 2018) to complete the data analysis process, the reality of preparing all of this data so you can present your findings sets in (Adu, 2016). Your methodical review of the qualitative data and development of codes, categories and themes has yielded massive and interesting NVivo outputs. The outcomes include but are not limited to; codes/nodes, categories/themes, Word Clouds, Word Tree, Framework Matrices, Cluster Tree, code-case matrices, and code-attribute matrices (see Figure 1). These findings need to be carefully examined – selecting the ones that will be useful in drafting a meaningful presentation. You can watch the presentation I developed below:

Source: https://www.youtube.com/watch?v=xEyGGFtVQFw
Note, not all of this information (i.e. the outcomes) needs to be presented to your audience (see Adu, 2019 ). Other questions that may arise as you develop your presentation include; what kind of results should you present? How do you engage with your audience when presenting your findings? How would you help your audience to understand and believe your findings?
In this post, I will discuss the three pertinent components a good presentation of qualitative findings should have. They are; background information, data analysis process and main findings.

Figure 1. Presentation of findings
Presenting background information
Participants’ past and current situations influence the information they provide to you. Due to this, there is the need to provide readers a summary of who participants are and any background information which may help them to put the findings into the proper context. Also, as a researcher analyzing qualitative data, there is the likelihood of your own background impacting the data analysis process. In the same way, you need to let readers know who you are, what your background is and how you ‘bracketed’ them from not having an effect on the findings ( Adu, 2019 ).
Presenting the data analysis process
Qualitative analysis doesn’t only involve engaging in subjective development of codes and categories, but also promoting transparency in the coding and categorization process (Greckhamer & Cilesiz, 2014). Due to this, you are expected to describe the main and detailed steps you took to analyze your data to arrive at your findings and their respective outcomes. Addressing the following questions would be great:
- What coding strategy did you use?
- What kinds of codes did you assign to relevant excerpts of the data?
- What are the examples of codes you generated?
- What categorization technique did you use?
- How did you develop categories/themes out of the codes?
Your audience’s aim is not only consuming what you found but also learning more about how you came up with the results.
Presenting main findings
When it comes to the presentation of findings, there are two main structures you could choose from. You could present them based on the themes generated or based on the cases (participants or groups of participants) you have. The decision to either structure depends on the kind of research question(s) or the research purpose you have. For a detailed explanation of the types of presentation formats and how to select an appropriate structure, see Chapter 13 of the book, “ A Step-by-Step Guide to Qualitative Data Coding ”.
Considering your roles and goals
As you plan on how to communicate the above components, make sure you accomplish your goals and carry out your role as a communicator of qualitative data analysis outcomes (See Figure 1). Your roles are; to thoughtfully arrange the data analysis outcomes and to adequately address your research questions.
Liken the presentation of your findings to sharing a puzzle which has been solved. Your goal is to prevent a situation where the burden is put on the audience to piece together the puzzle of findings. In other words, you are expected to present the findings in a meaningful way that would enhance the audience’s understanding of the data analysis outcomes (Adu, 2016 & 2019). By so doing, they are more likely to trust what you found.
Let’s summarize the action items:
- Out of a pool of qualitative analysis outcomes, select the ones that would allow you to address your research questions and meaningfully communicate your findings.
- Decide on how you want to structure the presentation of the findings.
- Irrespective of the presentation format you choose, make sure you include background information, the data analysis process and main findings in your presentation.
- Make sure you are ‘narrating’ participants’ stories or what you found – making the numeric outputs include the tables and charts generated play a supporting role when presenting the main findings.
Adu, P. (2016). Presenting Qualitative Findings Using NVivo Output to Tell the Story. [PowerPoint slides]. SlideShare. Retrieved from https://www.slideshare.net/kontorphilip/presenting-qualitative-findings-using-nvivo-output-to-tell-the-story
QSR International Pty Ltd. (2018). NVivo 12. Version 12.1.249 [Computer software]. Retrieved from https://qsrinternational.com/nvivo-qualitative-data-analysis-software
Adu, P. (2019). A Step-by-Step Guide to Qualitative Data Coding . Oxford: Routledge
Greckhamer, T., & Cilesiz, S. (2014). Rigor, Transparency, Evidence, and Representation in Discourse Analysis: Challenges and Recommendations. International Journal of Qualitative Methods, 13(1), 422-443. doi:10.1177/160940691401300123
ABOUT THE AUTHOR

Dr. Philip Adu is a Methodology Expert at The Chicago School of Professional Psychology (TCSPP). His role is to provide support to dissertating students in TCSPP addressing their methodology related concerns. You could access some of his webinars at the ‘Methodology Related Presentations – TCSPP’ YouTube Channel. He completed his Doctoral degree in Education with a concentration in Learning, Instructional Design and Technology from West Virginia University (WVU). Dr. Adu recently authored a book titled, “A Step-by-Step Guide to Qualitative Data Coding” (available on routledge.com or amazon.com ). You could reach Dr. Adu at [email protected] and @drphilipadu on twitter.
Recent Articles

How To Write The Results/Findings Chapter
For qualitative studies (dissertations & theses).
By: Jenna Crossley (PhD). Expert Reviewed By: Dr. Eunice Rautenbach | August 2021
So, you’ve collected and analysed your qualitative data, and it’s time to write up your results chapter. But where do you start? In this post, we’ll guide you through the qualitative results chapter (also called the findings chapter), step by step.
Overview: Qualitative Results Chapter
- What (exactly) the qualitative results chapter is
- What to include in your results chapter
- How to write up your results chapter
- A few tips and tricks to help you along the way
- Free results chapter template
What exactly is the results chapter?
The results chapter in a dissertation or thesis (or any formal academic research piece) is where you objectively and neutrally present the findings of your qualitative analysis (or analyses if you used multiple qualitative analysis methods ). This chapter can sometimes be combined with the discussion chapter (where you interpret the data and discuss its meaning), depending on your university’s preference. We’ll treat the two chapters as separate, as that’s the most common approach.
In contrast to a quantitative results chapter that presents numbers and statistics, a qualitative results chapter presents data primarily in the form of words . But this doesn’t mean that a qualitative study can’t have quantitative elements – you could, for example, present the number of times a theme or topic pops up in your data, depending on the analysis method(s) you adopt.
Adding a quantitative element to your study can add some rigour, which strengthens your results by providing more evidence for your claims. This is particularly common when using qualitative content analysis. Keep in mind though that qualitative research aims to achieve depth, richness and identify nuances , so don’t get tunnel vision by focusing on the numbers. They’re just cream on top in a qualitative analysis.
So, to recap, the results chapter is where you objectively present the findings of your analysis, without interpreting them (you’ll save that for the discussion chapter). With that out the way, let’s take a look at what you should include in your results chapter.
What should you include in the results chapter?
As we’ve mentioned, your qualitative results chapter should purely present and describe your results , not interpret them in relation to the existing literature or your research questions . Any speculations or discussion about the implications of your findings should be reserved for your discussion chapter.
In your results chapter, you’ll want to talk about your analysis findings and whether or not they support your hypotheses (if you have any). Naturally, the exact contents of your results chapter will depend on which qualitative analysis method (or methods) you use. For example, if you were to use thematic analysis, you’d detail the themes identified in your analysis, using extracts from the transcripts or text to support your claims.
While you do need to present your analysis findings in some detail, you should avoid dumping large amounts of raw data in this chapter. Instead, focus on presenting the key findings and using a handful of select quotes or text extracts to support each finding . The reams of data and analysis can be relegated to your appendices.
While it’s tempting to include every last detail you found in your qualitative analysis, it is important to make sure that you report only that which is relevant to your research aims, objectives and research questions . Always keep these three components, as well as your hypotheses (if you have any) front of mind when writing the chapter and use them as a filter to decide what’s relevant and what’s not.
Need a helping hand?
How do I write the results chapter?
Now that we’ve covered the basics, it’s time to look at how to structure your chapter. Broadly speaking, the results chapter needs to contain three core components – the introduction, the body and the concluding summary. Let’s take a look at each of these.
Section 1: Introduction
The first step is to craft a brief introduction to the chapter. This intro is vital as it provides some context for your findings. In your introduction, you should begin by reiterating your problem statement and research questions and highlight the purpose of your research . Make sure that you spell this out for the reader so that the rest of your chapter is well contextualised.
The next step is to briefly outline the structure of your results chapter. In other words, explain what’s included in the chapter and what the reader can expect. In the results chapter, you want to tell a story that is coherent, flows logically, and is easy to follow , so make sure that you plan your structure out well and convey that structure (at a high level), so that your reader is well oriented.
The introduction section shouldn’t be lengthy. Two or three short paragraphs should be more than adequate. It is merely an introduction and overview, not a summary of the chapter.
Pro Tip – To help you structure your chapter, it can be useful to set up an initial draft with (sub)section headings so that you’re able to easily (re)arrange parts of your chapter. This will also help your reader to follow your results and give your chapter some coherence. Be sure to use level-based heading styles (e.g. Heading 1, 2, 3 styles) to help the reader differentiate between levels visually. You can find these options in Word (example below).
Section 2: Body
Before we get started on what to include in the body of your chapter, it’s vital to remember that a results section should be completely objective and descriptive, not interpretive . So, be careful not to use words such as, “suggests” or “implies”, as these usually accompany some form of interpretation – that’s reserved for your discussion chapter.
The structure of your body section is very important , so make sure that you plan it out well. When planning out your qualitative results chapter, create sections and subsections so that you can maintain the flow of the story you’re trying to tell. Be sure to systematically and consistently describe each portion of results. Try to adopt a standardised structure for each portion so that you achieve a high level of consistency throughout the chapter.
For qualitative studies, results chapters tend to be structured according to themes , which makes it easier for readers to follow. However, keep in mind that not all results chapters have to be structured in this manner. For example, if you’re conducting a longitudinal study, you may want to structure your chapter chronologically. Similarly, you might structure this chapter based on your theoretical framework . The exact structure of your chapter will depend on the nature of your study , especially your research questions.
As you work through the body of your chapter, make sure that you use quotes to substantiate every one of your claims . You can present these quotes in italics to differentiate them from your own words. A general rule of thumb is to use at least two pieces of evidence per claim, and these should be linked directly to your data. Also, remember that you need to include all relevant results , not just the ones that support your assumptions or initial leanings.
In addition to including quotes, you can also link your claims to the data by using appendices , which you should reference throughout your text. When you reference, make sure that you include both the name/number of the appendix , as well as the line(s) from which you drew your data.
As referencing styles can vary greatly, be sure to look up the appendix referencing conventions of your university’s prescribed style (e.g. APA , Harvard, etc) and keep this consistent throughout your chapter.
Section 3: Concluding summary
The concluding summary is very important because it summarises your key findings and lays the foundation for the discussion chapter . Keep in mind that some readers may skip directly to this section (from the introduction section), so make sure that it can be read and understood well in isolation.
In this section, you need to remind the reader of the key findings. That is, the results that directly relate to your research questions and that you will build upon in your discussion chapter. Remember, your reader has digested a lot of information in this chapter, so you need to use this section to remind them of the most important takeaways.
Importantly, the concluding summary should not present any new information and should only describe what you’ve already presented in your chapter. Keep it concise – you’re not summarising the whole chapter, just the essentials.
Tips for writing an A-grade results chapter
Now that you’ve got a clear picture of what the qualitative results chapter is all about, here are some quick tips and reminders to help you craft a high-quality chapter:
- Your results chapter should be written in the past tense . You’ve done the work already, so you want to tell the reader what you found , not what you are currently finding .
- Make sure that you review your work multiple times and check that every claim is adequately backed up by evidence . Aim for at least two examples per claim, and make use of an appendix to reference these.
- When writing up your results, make sure that you stick to only what is relevant . Don’t waste time on data that are not relevant to your research objectives and research questions.
- Use headings and subheadings to create an intuitive, easy to follow piece of writing. Make use of Microsoft Word’s “heading styles” and be sure to use them consistently.
- When referring to numerical data, tables and figures can provide a useful visual aid. When using these, make sure that they can be read and understood independent of your body text (i.e. that they can stand-alone). To this end, use clear, concise labels for each of your tables or figures and make use of colours to code indicate differences or hierarchy.
- Similarly, when you’re writing up your chapter, it can be useful to highlight topics and themes in different colours . This can help you to differentiate between your data if you get a bit overwhelmed and will also help you to ensure that your results flow logically and coherently.
If you have any questions, leave a comment below and we’ll do our best to help. If you’d like 1-on-1 help with your results chapter (or any chapter of your dissertation or thesis), check out our private dissertation coaching service here or book a free initial consultation to discuss how we can help you.

Psst... there’s more!
This post was based on one of our popular Research Bootcamps . If you're working on a research project, you'll definitely want to check this out ...
22 Comments
This was extremely helpful. Thanks a lot guys
Hi, thanks for the great research support platform created by the gradcoach team!
I wanted to ask- While “suggests” or “implies” are interpretive terms, what terms could we use for the results chapter? Could you share some examples of descriptive terms?
I think that instead of saying, ‘The data suggested, or The data implied,’ you can say, ‘The Data showed or revealed, or illustrated or outlined’…If interview data, you may say Jane Doe illuminated or elaborated, or Jane Doe described… or Jane Doe expressed or stated.
I found this article very useful. Thank you very much for the outstanding work you are doing.
What if i have 3 different interviewees answering the same interview questions? Should i then present the results in form of the table with the division on the 3 perspectives or rather give a results in form of the text and highlight who said what?
I think this tabular representation of results is a great idea. I am doing it too along with the text. Thanks
That was helpful was struggling to separate the discussion from the findings
this was very useful, Thank you.
Very helpful, I am confident to write my results chapter now.
It is so helpful! It is a good job. Thank you very much!
Very useful, well explained. Many thanks.
Hello, I appreciate the way you provided a supportive comments about qualitative results presenting tips
I loved this! It explains everything needed, and it has helped me better organize my thoughts. What words should I not use while writing my results section, other than subjective ones.
Thanks a lot, it is really helpful
Thank you so much dear, i really appropriate your nice explanations about this.
Thank you so much for this! I was wondering if anyone could help with how to prproperly integrate quotations (Excerpts) from interviews in the finding chapter in a qualitative research. Please GradCoach, address this issue and provide examples.
what if I’m not doing any interviews myself and all the information is coming from case studies that have already done the research.
Very helpful thank you.
This was very helpful as I was wondering how to structure this part of my dissertation, to include the quotes… Thanks for this explanation
This is very helpful, thanks! I am required to write up my results chapters with the discussion in each of them – any tips and tricks for this strategy?
For qualitative studies, can the findings be structured according to the Research questions? Thank you.
Do I need to include literature/references in my findings chapter?
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly

[Guide] How to Present Qualitative Research Findings in PowerPoint?
By: Author Shrot Katewa
![how to present a qualitative research [Guide] How to Present Qualitative Research Findings in PowerPoint?](https://artofpresentations.com/wp-content/uploads/2020/09/Featured-Image-Present-qualitative-findings-using-Powerpoint.jpg)
As a researcher, it is quite pointless to do the research if we are unable to share the findings with our audience appropriately! Using PowerPoint is one of the best ways to present research outcomes. But, how does one present qualitative research findings using PowerPoint?
In order to present the qualitative research findings using PowerPoint, you need to create a robust structure for your presentation, make it engaging and visually appealing, present the patterns with explanations for it and highlight the conclusion of your research findings.
In this article, we will help you understand the structure of your presentation. Plus, we’ll share some handy tips that will make your qualitative research presentation really effective!
How to Create a Structure for your Qualitative Research Presentation?
Creating the right structure for your presentation is key to ensuring that it is correctly understood by your audience.
The structure of your Research Presentation not only makes it easier for you to create the document, it also makes it simple for the audience to understand what all will be covered in the presentation at the time of presenting it to your audience.
Furthermore, having a robust structure is a great way to ensure that you don’t miss out on any of the points while working on creating the presentation.
But, what structure should one follow?
Creating a good structure can be tricky for some. Thus, I’m sharing what has worked well for me during my previous research projects.
NOTE – It is important to note that although the following structure is highly effective for most research findings presentation, it has been generalized in order to serve a wide range of research projects. You may want to take a look at points that are very specific to the nature of your research project and include them at your discretion.
Here’s my recommended structure to create your Research Findings presentation –
1. Objective of the Research
A great way to start your presentation is to highlight the objective of your research project.
It is important to remember that merely sharing the objective may sometimes not be enough. A short backstory along with the purpose of your research project can pack a powerful punch ! It not only validates the reasoning for your project but also subtly establishes trust with your audience.
However, do make sure that you’re not reading the backstory from the slide. Let it flow naturally when you are delivering the presentation. Keep the presentation as minimalistic as possible.
2. Key Parameters Considered for Measurement
Once you’ve established the objective, the next thing that you may want to do is perhaps share the key parameters considered for the success of your project.
Every research project, including qualitative research, needs to have a few key parameters to measure against the objective of the research.
For example – If the goal of your project is to gather the sentiments of a certain group of people for a particular product, you may need to measure their feelings. Are they happy or unhappy using the product? How do they perceive the branding of the product? Is it affordable?
Make sure that you list down all such key parameters that were considered while conducting the qualitative research.
In general, laying these out before sharing the outcome can help your audience think from your perspective and look at the findings from the correct lens.
3. Research Methodology Adopted
The next thing that you may want to include in your presentation is the methodology that you adopted for conducting the research.
By knowing your approach, the audience can be better prepared for the outcome of your project. Ensure that you provide sound reasoning for the chosen methodology.
This section of your presentation can also showcase some pictures of the research being conducted. If you have captured a video, include that. Doing this provides further validation of your project.
4. Research Outcomes (Presenting Descriptive Analysis)

This is the section that will constitute the bulk of the your presentation.
Use the slides in this section to describe the observations, and the resulting outcomes on each of the key parameters that were considered for the research project.
It is usually a good idea to dedicate at least 1 or more slides for each parameter . Make sure that you present data wherever possible. However, ensure that the data presented can be easily comprehended.
Provide key learnings from the data, highlight any outliers, and possible reasoning for it. Try not to go too in-depth with the stats as this can overwhelm the audience. Remember, a presentation is most helpful when it is used to provide key highlights of the research !
Apart from using the data, make sure that you also include a few quotes from the participants.
5. Summary and Learnings from the Research
Once you’ve taken the audience through the core part of your research findings, it is a good practice to summarize the key learnings from each of the section of your project.
Make sure your touch upon some of the key learnings covered in the research outcome of your presentation.
Furthermore, include any additional observations and key points that you may have had which were previously not covered.
The summary slide also often acts as “Key Takeaways” from the research for your audience. Thus, make sure that you maintain brevity and highlight only the points that you want your audience to remember even after the presentation.
6. Inclusions and Exclusions (if any)
While this can be an optional section for some of the researchers.
However, dedicating a section on inclusions and exclusions in your presentation can be a great value add! This section helps your audience understand the key factors that were excluded (or included) on purpose!
Moreover, it creates a sense of thoroughness in the minds of your audience.
7. Conclusion of the Research
The purpose of the conclusion slide of your research findings presentation is to revisit the objective, and present a conclusion.
A conclusion may simply validate or nullify the objective. It may sometimes do neither. Nevertheless, having a conclusion slide makes your presentation come a full circle. It creates this sense of completion in the minds of your audience.
8. Questions
Finally, since your audience did not spend as much time as you did on the research project, people are bound to have a few questions.
Thus, the last part of your presentation structure should be dedicated to allowing your audience to ask questions.
Tips for Effectively Presenting Qualitative Research Findings using PowerPoint
For a presentation to be effective, it is important that the presentation is not only well structured but also that it is well created and nicely delivered!
While we have already covered the structure, let me share with you some tips that you can help you create and deliver the presentation effectively.
Tip 1 – Use Visuals
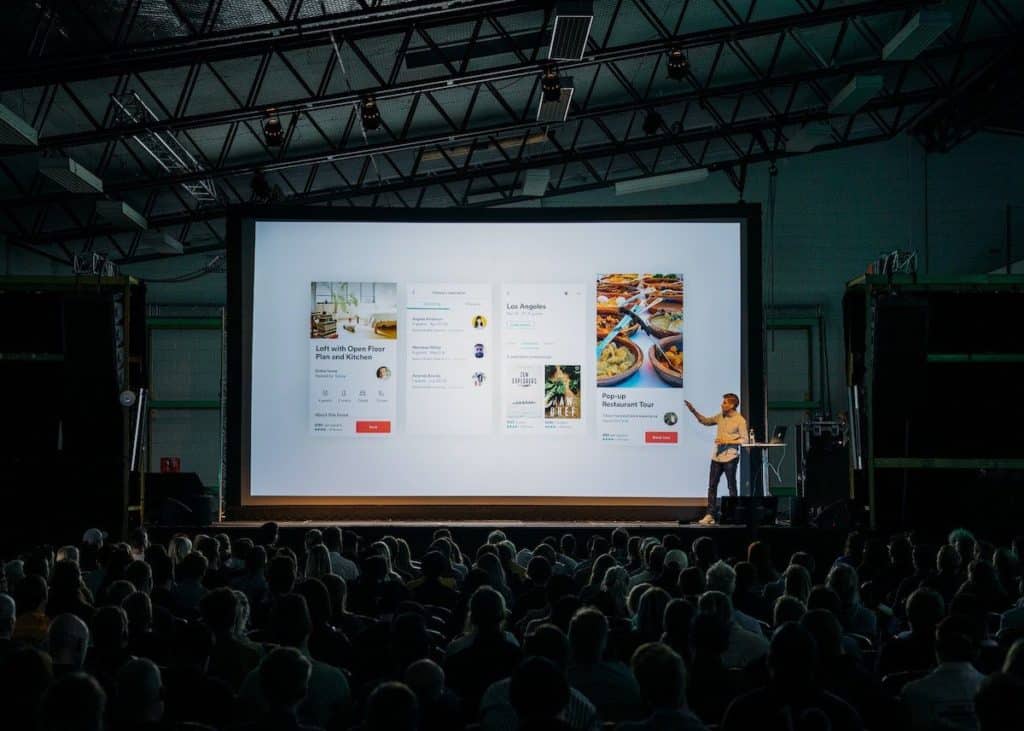
Using visuals in your presentation is a great way to keep the presentations engaging!
Visual aids not only help make the presentation less boring, but it also helps your audience in retaining the information better!
So, use images and videos of the actual research wherever possible. If these do not suffice or do not give a professional feel, there are a number of resources online from where you can source royalty-free images.
My recommendation for high-quality royalty-free images would be either Unsplash or Pexels . Both are really good. The only downside is that they often do not provide the perfect image that can be used. That said, it can get the job done for at least half the time.
If you are unable to find the perfect free image, I recommend checking out Dreamstime . They have a huge library of images and are much cheaper than most of the other image banks. I personally use Dreamstime for my presentation projects!
Tip 2 – Tell a Story (Don’t Show Just Data!)
I cannot stress enough on how important it is to give your presentation a human touch. Delivering a presentation in the form of a story does just that! Furthermore, storytelling is also a great tool for visualization .
Data can be hard-hitting, whereas a touching story can tickle the emotions of your audience on various levels!
One of the best ways to present a story with your research project is to start with the backstory of the objective. We’ve already talked about this in the earlier part of this article.
Start with why is this research project is so important. Follow a story arc that provides an exciting experience of the beginning, the middle, and a progression towards a climax; much like a plot of a soap opera.
Tip 3 – Include Quotes of the Participants
Including quotes of the participants in your research findings presentation not only provides evidence but also demonstrates authenticity!
Quotes function as a platform to include the voice of the target group and provide a peek into the mindset of the target audience.
When using quotes, keep these things in mind –
1. Use Quotes in their Unedited Form
When using quotes in your presentation, make sure that you use them in their raw unedited form.
The need to edit quotes should be only restricted to aid comprehension and sometimes coherence.
Furthermore, when editing the quotes, make sure that you use brackets to insert clarifying words. The standard format for using the brackets is to use square brackets for clarifying words and normal brackets for adding a missing explanation.
2. How to Decide which Quotes to Consider?
It is important to know which quotes to include in your presentation. I use the following 3 criteria when selecting the quote –
- Relevance – Consider the quotes that are relevant, and trying to convey the point that you want to establish.
- Length – an ideal quote should be not more than 1-2 sentences long.
- Choose quotes that are well-expressed and striking in nature.
3. Preserve Identity of the Participant
It is important to preserve and protect the identity of the participant. This can be done by maintaining confidentiality and anonymity.
Thus, refrain from using the name of the participant. An alternative could be using codes, using pseudonyms (made up names) or simply using other general non-identifiable parameters.
Do note, when using pseudonyms, remember to highlight it in the presentation.
If, however, you do need to use the name of the respondent, make sure that the participant is okay with it and you have adequate permissions to use their name.
Tip 4 – Make your Presentation Visually Appealing and Engaging
It is quite obvious for most of us that we need to create a visually appealing presentation. But, making it pleasing to the eye can be a bit challenging.
Fortunately, we wrote a detailed blog post with tips on how to make your presentation attractive. It provides you with easy and effective tips that you can use even as a beginner! Make sure you check that article.
7 EASY tips that ALWAYS make your PPT presentation attractive (even for beginners)
In addition to the tips mentioned in the article, let me share a few things that you can do which are specific to research outcome presentations.
4.1 Use a Simple Color Scheme
Using the right colors are key to make a presentation look good.
One of the most common mistakes that people make is use too many colors in their presentation!
My recommendation would be to go with a monochromatic color scheme in PowerPoint .
4.2 Make the Data Tables Simple and Visually Appealing
When making a presentation on research outcomes, you are bound to present some data.
But, when data is not presented in a proper manner, it can easily and quickly make your presentation look displeasing! The video below can be a good starting point.
Using neat looking tables can simply transform the way your presentation looks. So don’t just dump the data from excel on your PowerPoint presentation. Spend a few minutes on fixing it!
4.3 Use Graphs and Charts (wherever necessary)
When presenting data, my recommendation would be that graphs and charts should be your first preference.
Using graphs or charts make it easier to read the data, takes less time for the audience to comprehend, and it also helps to identify a trend.
However, make sure that the correct chart type is used when representing the data. The last thing that you want is to poorly represent a key piece of information.
4.4 Use Icons instead of Bullet Points
Consider the following example –
This slide could have been created just as easily using bullet points. However, using icons and representing the information in a different format makes the slide pleasing on the eye.
Thus, always try to use icons wherever possible instead of bullet points.
Tip 5 – Include the Outliers
Many times, as a research project manager, we tend to focus on the trends extracted from a data set.
While it is important to identify patterns in the data and provide an adequate explanation for the pattern, it is equally important sometimes to highlight the outliers prominently.
It is easy to forget that there may be hidden learnings even in the outliers. At times, the data trend may be re-iterating the common wisdom. However, upon analyzing the outlier data points, you may get insight into how a few participants are doing things successfully despite not following the common knowledge.
That said, not every outlier will reveal hidden information. So, do verify what to include and what to exclude.
Tip 6 – Take Inspiration from other Presentations
I admit, making any presentation can be a tough ask let alone making a presentation for showcasing qualitative research findings. This is especially hard when we don’t have the necessary skills for creating a presentation.
One quick way to overcome this challenge could be take inspiration from other similar presentations that we may have liked.
There is no shame in being inspired from others. If you don’t have any handy references, you can surely Google it to find a few examples.
One trick that almost always works for me is using Pinterest .
But, don’t just directly search for a research presentation. You will have little to no success with it. The key is to look for specific examples for inspiration. For eg. search for Title Slide examples, or Image Layout Examples in Presentation.
Tip 7 – Ask Others to Critic your Presentation
The last tip that I would want to provide is to make sure that you share the presentation with supportive colleagues or mentors to attain feedback.
This step can be critical to iron out the chinks in the armor. As research project manager, it is common for you to get a bit too involved with the project. This can lead to possibilities wherein you miss out on things.
A good way to overcome this challenge is to get a fresh perspective on your project and the presentation once it has been prepared.
Taking critical feedback before your final presentation can also prepare you to handle tough questions in an adept manner.
Final Thoughts
It is quite important to ensure that we get it right when working on a presentation that showcases the findings of our research project. After all, we don’t want to be in a situation wherein we put in all the hard-work in the project, but we fail to deliver the outcome appropriately.
I hope you will find the aforementioned tips and structure useful, and if you do, make sure that you bookmark this page and spread the word. Wishing you all the very best for your project!
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Presenting and evaluating qualitative research
Affiliation.
- 1 Univeristy of Nottingham, Nottingham, United Kingdom. [email protected]
- PMID: 21179252
- PMCID: PMC2987281
- DOI: 10.5688/aj7408141
The purpose of this paper is to help authors to think about ways to present qualitative research papers in the American Journal of Pharmaceutical Education. It also discusses methods for reviewers to assess the rigour, quality, and usefulness of qualitative research. Examples of different ways to present data from interviews, observations, and focus groups are included. The paper concludes with guidance for publishing qualitative research and a checklist for authors and reviewers.
Keywords: American Journal of Pharmaceutical Education; qualitative research; research papers.
PubMed Disclaimer
Similar articles
- Guidance for Qualitative Research Manuscripts in Pharmacy Education. Kawaguchi-Suzuki M, Blakely ML, Childs-Kean LM, Devraj R, Frenzel JE, Medina MS, Pate AN, Thurston MM, Franks AM. Kawaguchi-Suzuki M, et al. Am J Pharm Educ. 2023 Jul;87(7):100089. doi: 10.1016/j.ajpe.2023.100089. Epub 2023 May 9. Am J Pharm Educ. 2023. PMID: 37380273 Review.
- A Peek Behind the Scenes of the American Journal of Pharmaceutical Education . Schlesselman LS, Romanelli F. Schlesselman LS, et al. Am J Pharm Educ. 2019 Dec;83(10):7877. doi: 10.5688/ajpe7877. Am J Pharm Educ. 2019. PMID: 32001898 Free PMC article. No abstract available.
- Insights, Pearls, and Guidance on Successfully Producing and Publishing Educational Research. Persky AM, Romanelli F. Persky AM, et al. Am J Pharm Educ. 2016 Jun 25;80(5):75. doi: 10.5688/ajpe80575. Am J Pharm Educ. 2016. PMID: 27402978 Free PMC article.
- Building criteria to evaluate qualitative research papers: a tool for peer reviewers. Costa AP, Minayo MCS. Costa AP, et al. Rev Esc Enferm USP. 2019 Mar 28;53:e03448. doi: 10.1590/S1980-220X2018041403448. Rev Esc Enferm USP. 2019. PMID: 30942296
- The Single-Case Reporting Guideline In Behavioural Interventions (SCRIBE) 2016 statement. Tate RL, Perdices M, Rosenkoetter U, Shadish W, Vohra S, Barlow DH, Horner R, Kazdin A, Kratochwill T, McDonald S, Sampson M, Shamseer L, Togher L, Albin R, Backman C, Douglas J, Evans JJ, Gast D, Manolov R, Mitchell G, Nickels L, Nikles J, Ownsworth T, Rose M, Schmid CH, Wilson B. Tate RL, et al. Can J Occup Ther. 2016 Jun;83(3):184-95. doi: 10.1177/0008417416648124. Can J Occup Ther. 2016. PMID: 27231387
- Guidelines to support the design, and selection and appraisal of multimedia teaching aids for microbiology education. Van Beek R, Spijkerman DJC, van der Burgt N, Hermanns B, Barendse S, Sainsbury PD, Timmis KN, Timmis JK. Van Beek R, et al. Microb Biotechnol. 2024 Aug;17(8):e14553. doi: 10.1111/1751-7915.14553. Microb Biotechnol. 2024. PMID: 39163108 Free PMC article.
- Nurses' perception of thirst in patients within palliative home care: a qualitative study. Lythell C, Schaller AS, Jaarsma T, Friedrichsen M. Lythell C, et al. BMC Nurs. 2024 Jul 29;23(1):516. doi: 10.1186/s12912-024-01985-y. BMC Nurs. 2024. PMID: 39075509 Free PMC article.
- Development of the ECLIPSE model of meaningful outcome domains following lower limb amputation and prosthetic rehabilitation, through systematic review and best fit framework synthesis. Ostler C, Dickinson A, Metcalf C, Donovan-Hall M. Ostler C, et al. PLoS One. 2024 Jul 23;19(7):e0307523. doi: 10.1371/journal.pone.0307523. eCollection 2024. PLoS One. 2024. PMID: 39042623 Free PMC article.
- Factors that influence the scope of practice of the chiropractic profession in Australia: a thematic analysis. Wiggins D, Downie A, Engel R, Grace S, Brown BT. Wiggins D, et al. Chiropr Man Therap. 2024 May 27;32(1):18. doi: 10.1186/s12998-024-00535-2. Chiropr Man Therap. 2024. PMID: 38802926 Free PMC article.
- 'Counselling is not just providing information': perceptions of caregivers and stakeholders on the design of nutrition and health counselling interventions for families with young children in rural Kenya. Kihagi GW, Hansen LS, Agure E, Muok EMO, Mank I, Danquah I, Sorgho R. Kihagi GW, et al. BMC Health Serv Res. 2024 May 7;24(1):597. doi: 10.1186/s12913-024-10872-w. BMC Health Serv Res. 2024. PMID: 38715044 Free PMC article.
- Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P. Qualitative research methods in health technology assessment: a review of the literature. Health Technology Assessment 1998; Vol. 2: No. 16. http://www.ncchta.org/fullmono/mon216.pdf Accessed August 31, 2010.
- Pope C, Mays N. Qualitative Research in Healthcare. 3rd ed. Oxford: Wiley Blackwell; 2006.
- Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage; 2006.
- Burke R, Johnson R. Mixed methods research: a research paradigm whose time has come. Educ Res. 2004;33(7):14–26.
- Farris KB, Demb A, Janke KK, Kelley K, Scott SA. Assessment to transform competency-based curricula. Am J Pharm Educ. 2009;73(8) Article 158. - PMC - PubMed
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Elsevier Science
- Europe PubMed Central
- PubMed Central
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Analysing and presenting qualitative data

Related Papers
A Short Guide to Qualitative Studies for Dental Researchers
Faaiz Alhamdani
The goal of medical care is to improve the patient’s quality of life (QOL) by maintaining function and well-being. Consequently, there is an increasing consensus that the patient’s perspective is pivotal in monitoring the outcomes of medical care in general. This is particularly important when management decisions are not clear-cut through a lack of clinical evidence. In such cases, it is imperative to study the health problems from all possible aspects. To achieve this aim we might need to study patients’ experiences and views of a particular disease process. This might optimize management outcomes by improving the clinician’s understanding of patients’ perceptions toward medical intervention. Qualitative studies can offer dental care providers with important aspects of the disease process. Particularly, how does the patient understand a particular oral health problem, and how does this knowledge improve oral health outcomes. This particular aspect cannot be explored using quantitative methods, which is widely used in the medical research field. This short guide tries to shed a light on the use of a qualitative research paradigm through qualitative research methodologies commonly used in medical research. These methodologies are; thematic analysis, phenomenology, interpretive phenomenology, grounded theory, and generic qualitative approaches. These methodologies will be presented in a rather different way from what a medical researcher might expect. This book will use fine art examples as an analogy. The author will use famous artworks to enlighten the main features of each qualitative research methodology.
The goal of medical care is to improve the patient’s quality of life (QOL) by maintaining function and well-being. Consequently, there is an increasing consensus that the patient’s perspective is pivotal in monitoring the outcomes of medical care in general. This is particularly important when management decisions are not clearcut through a lack of clinical evidence. In such cases, it is imperative to study the health problems from all possible aspects. To achieve this aim we might need to study patients’ experiences and views of a particular disease process. This might optimize management outcomes by improving the clinician’s understanding of patients’ perceptions toward medical intervention. Qualitative studies can offer dental care providers with important aspects of the disease process. Particularly, how does the patient understand a particular oral health problem, and how does this knowledge improve oral health outcomes. This particular aspect cannot be explored using quantitative methods, which is widely used in the medical research field. This short guide tries to shed a light on the use of a qualitative research paradigm through qualitative research methodologies commonly used in medical research. These methodologies are; thematic analysis, phenomenology, interpretive phenomenology, grounded theory, and generic qualitative approaches. These methodologies will be presented in a rather different way from what a medical researcher might expect. This book will use fine art examples as an analogy. The author will use famous artworks to enlighten the main features of each qualitative research methodology.
International Journal of Dental Hygiene
Mark Gussy , Virginia Dickson-Swift
Canadian Journal of …
Shafik Dharamsi
Ciência & Saúde Coletiva
Vera L P Alves
Qualitative Health research procedures that are not always applied, mainly in the analysis phase. Our objective is to present a systematized technique of step-by-step procedures for qualitative content analysis in the health field: Clinical-Qualitative Content Analysis. Our proposal consider that the qualitative research applied to the field of health, can acquire a perspective analogous to clinical practice and aims to interpret meanings expressed in reports through individual interviews or statements. This analysis takes part of the Clinical-Qualitative Method. The literature review was realized through: a book chapter, eight original articles and three methodological articles. The Clinical-qualitative Content Analysis technique comprises seven steps: 1) Editing material for analysis; 2) Floating reading; 3) Construction of the units of analysis; 4) Construction of codes of meaning; 5) General refining of the codes and the Construction of categories; 6) Discussion; 7) Validity. Th...
Barry Gibson
Douglas Ezzy
Eleni Mamai-homata
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Nursing & Health Sciences
Hannele Turunen , Terese Bondas
Journal of Evaluation in Clinical Practice
Mary Boulton
Journal of Preventive Medicine and Public Health
CERN European Organization for Nuclear Research - Zenodo
Margaret Zinyama
Journal of advanced nursing
mistir lingerew mehari
British dental journal
Masyita Mamot
Revista Latino-Americana de Enfermagem
Egberto Turato
Indra Lukman
Evidence-Based Nursing
Helen Noble
Online Journal of …
Kalaiselvan Ganapathy
Yanuar Kartika Sari
Catherine Pope
Community Dentistry and Oral Epidemiology
Gill Wright
Evidence Based Nursing
temitope oludoun
BMC Medical Research Methodology
Alexandra Sbaraini
Nurse education today
khamidah zaki
JOURNAL OF NEUROLOGICAL RESEARCH AND THERAPY
Naiya Patel
Brazilian Oral Research
robina shaheen
URNCST Journal
Saqib Shaheen , Umair Majid
Research Methods for Graduate Business and Social Science Students
Crina Damsa
Janine Owens
International Journal of Qualitative Research
Aisha Hadi Ibrahim
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- October 2024: Report Redesign
- November 2024: Powerful Presentations
- December 2024: Dashboard Design
- Self-Paced: Soar Beyond the Dusty Shelf Report
- Full-Day Workshops
- Conference Keynotes
- Shirts & Hoodies
- Chart Templates

12 Comments
Barbara Felver, data visualization specialist in the Research and Data Analysis (RDA) Division of Washington State’s Dept. of Social and Health Services does a great job illustrating a variety of quantitative and qualitative data for research and survey reports. For example, see her work in this year’s foster parents’ survey: http://www.dshs.wa.gov/pdf/ms/rda/research/11/207.pdf
[…] 6 Ideas for Displaying Qualitative Data | Ann’s Blog […]
[…] In her new Blog Post, Ann K. Emery puts forward 6 ideas for displaying qualitative data: […]
Thanks for a great overview of options for displaying qualitative data – and terrific examples. We will expand the options on the BetterEvaluation.org catalogue of options.
Thanks for sharing. To combine pictures and written information makes it easy to cpature even complex data.
HOW DISPLAYING QUALITATIVE DATA WITH NEW MINDSIGHT FROM THOUGHT LEADER for the understanding.
Fantastic Ann! Because qualitative research makes my heart beat fast with joy; I love to see more attention being paid to data vis of such rich information. Thank you, thank you for helping to spread the word that qual is beautiful too!
These are great tips that embrace the “visual learner” among the diverse audience of targeted recipents of qualitive research findings.
Incredibly helpful! I manage focus group feedback and started trying to give a visual to the vast breadth and variety of the qualitative input!
[…] from Nielsen Norman. Awesome tips from CRC colleagues for larger community surveys. Achievable qual visualization ideas from Ann Emery. Some tools for qual analysis and visualization from Tech for […]
[…] Achievable qual visualization ideas from Ann Emery. […]
[…] recently shared six ideas for displaying qualitative data. Later this year, I’ll publish a follow-up post with additional […]
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
How to Visualize Qualitative Data
Are you looking for ways to display your qualitative data? The vast majority of data visualization resources focus on quantitative data. In this article, let’s look at some of your options for qualitative data visualization, like word clouds, photographs, icons, diagrams, and timelines.
I used to conduct qualitative-heavy research projects pretty much all day every day. Key informant interviews, bellwether interviews, document review, focus groups, you name it… So I know from personal experience that 99.9 percent of qualitative reports look like this:
Which is fine, unless you want someone to, ya know, actually read your report.
Here are several ideas for presenting qualitative data for your organization’s reports, presentations, handouts, infographics, and more.
Word Clouds
Data visualization novices love to love word clouds, while data visualization experts love to hate word clouds.
Word Clouds Are Okay for Visualizing One-Word Descriptions, But Not for Visualizing Allllllll Your Qualitative Data
Here’s the most obvious strategy for visualizing text-based data: the word cloud , also known as a tag cloud . Frequent words or phrases are shown in larger, bolder font. Less-frequent words or phrases are shown in a smaller font.
I’m not advocating for run-of-the-mill word clouds where you simply dump your interview transcripts into a word cloud and hope for the best. Simply looking at how often a word or phrase appears in your dataset is not a sufficient way to analyze your data!
Instead, I’m talking about intentional word clouds – when you’ve considered other options, and have purposefully chosen a word cloud as your visualization of choice.
Here’s one example. When I conduct interviews as part of a qualitative research project, I often included a question in the interview protocol such as, “What one word you use to describe _____?” For example, “Mr. Policymaker, what one word would you use to describe public opinion towards poverty in the United States?” or “Mrs. Principal, what one word would you use to describe this new initiative’s effect, if any, on your charter school?”
The rest of the interview is obviously focused on loooooooong responses, and fuller descriptions, and plenty of examples. But for one or two moments during the conversation, it’s nice to pause and throw in a semi-qualitative short question.
Then, you’d visualize those one-word responses in a word cloud, like this one from Students First:

People described their favorite teacher using only one word and the adjectives were visualized in a word cloud shaped like an apple.
Here’s another example from the Pew Research Center , in which they visualized one-word descriptions of Barack Obama with packed bubbles. Packed bubbles are similar to word clouds. In word clouds, word frequency is depicted through font size. In packed bubbles, word frequency is depicted through bubble size.

People described Barack Obama using only one word and the adjectives were visualized in a bubble cloud (and then color-coded by the sentiment or tone of that adjective).
Word Clouds Are Okay for Visualizing Before/After Comparisons
Word clouds are also great for before/after comparisons, like these tweets describing breakups. Does your study involve pre/post tests with a few open-ended questions? Did you interview participants at multiple intervals during the study? You could adapt this technique for nearly any time series design.
What our breakups look like on Twitter http://t.co/yRZ8fBgRxx Before and after: pic.twitter.com/XQg7JKMar5 — Motherboard (@motherboard) September 23, 2014
The Best Software Tools for Creating Word Clouds
There are tons of free and low-cost websites for generating word clouds. The Poll Everywhere blog summarized nine of their favorite tools . My personal favorites are Wordle and Tagxedo.
Wordle is a free website for making word clouds in an oval or rectangular shape. It’s pretty easy to use. You simply copy all of your text (e.g., from your interview transcripts) and paste the text into Wordle. Then, you can customize the word cloud’s fonts, colors, and general shape to your liking. I suggest matching the fonts and colors to your project’s existing branding guidelines so that your word cloud matches the rest of your report or slideshow.
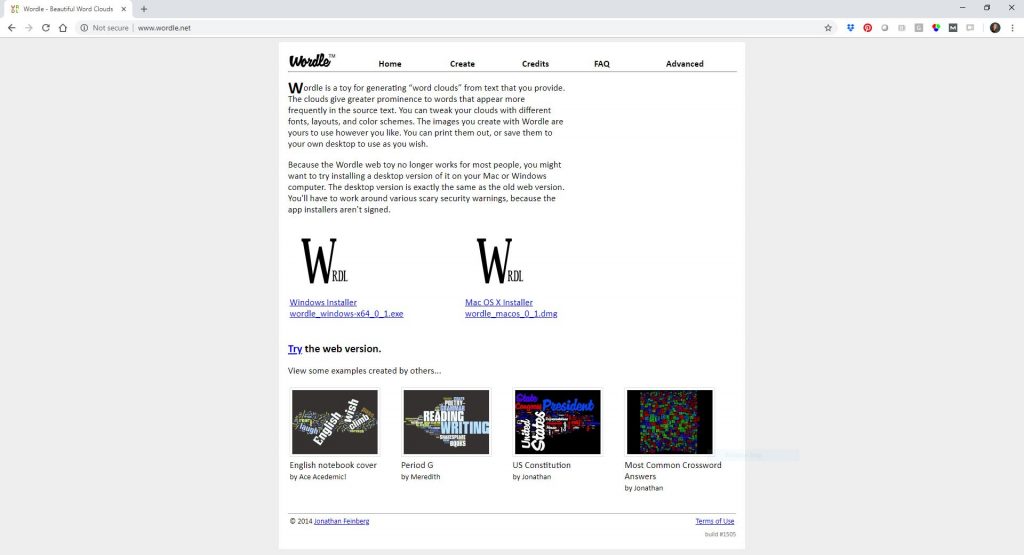
Tagxedo is a free website for making word clouds in fun shapes, like an apple, heart, or outline of the United States. You can pull in qualitative data directly from a website or Twitter feed (you don’t have to copy and paste, so you save a step). And, with Tagxedo, you could even have your word cloud printed on a t-shirt, tote bag, or coffee mug. I see Tagxedo as more of a decorative option than a researchy option.
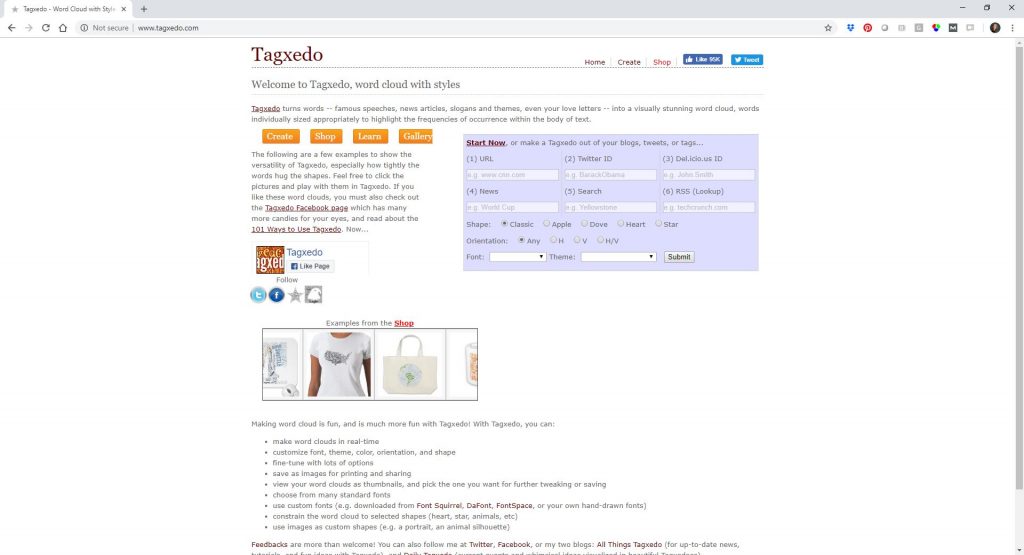
Showcase Open-Ended Survey Data Beside Closed-Ended Data
What’s better than quantitative data? Or better than qualitative data? Quantitative and qualitative data combined!
Use this technique when your survey has both closed-ended and open-ended questions. Tie the responses together in one chart to add much-needed context. In this example, a survey asked nonprofits to describe what it was like to work with an outside consultant. Then, the survey asked them why their experiences were good or bad. Who cares if 33 percent of nonprofits had excellent experiences but we don’t have examples that describe why?
Rather than simply listing out the open-ended responses in your appendix, showcase them beside your stacked column chart.
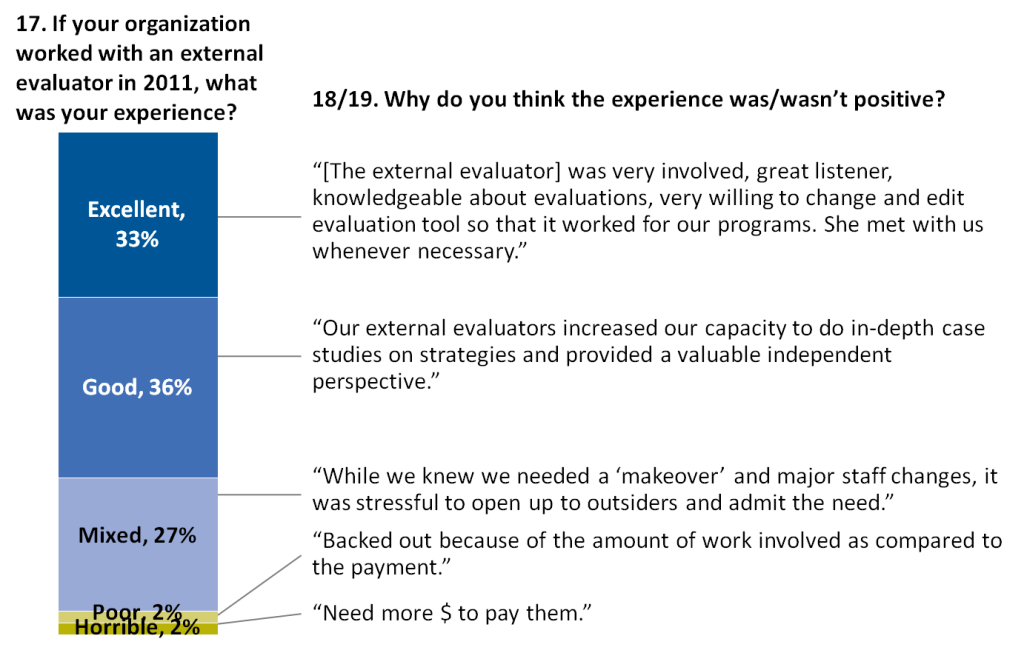
Read more about this technique in this post written by Johanna Morariu and I.
Include Photos Beside Participants’ Responses
For your non-anonymous reporting, how about inserting photos of the interviewees next to their ideas?
Strategies for use of #interpreter services in hospitals http://t.co/EpvPyvNcMZ , from @abtassociates @NHeLP_org &more pic.twitter.com/O8V05h3DoM — Sabriya Rice (@sabriyarice) September 2, 2014
Here’s an example from the New York Times, where they added photographs beside interviewees’ responses :
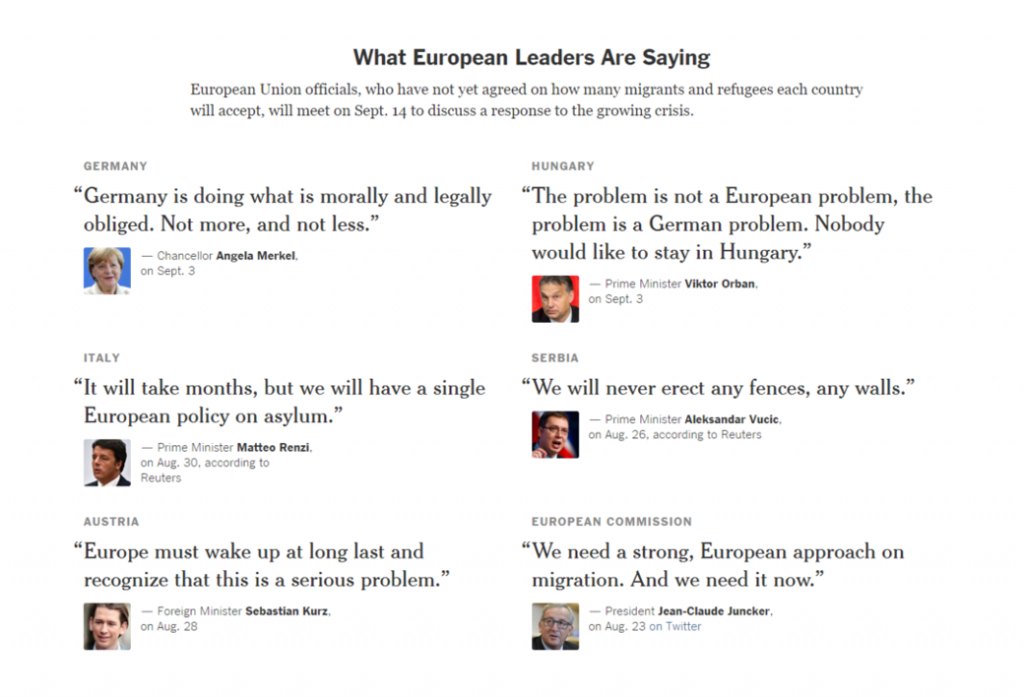
Include Icons Beside Descriptions and Responses
Icons are so easy to use that there’s really no excuse for not using them to break up long sections of text.
Islamic State is one of the world’s richest terror groups. Here’s why: http://t.co/C0DsXqHkfD pic.twitter.com/ikNThUwNhb — Wall Street Journal (@WSJ) August 28, 2014
The Center on Budget and Policy Priorities used icons to visualize how working-family tax credits can help at every stage of life :
And the Center on Budget and Policy Priorities used icons again to help their readers understand how low-wage workers face a cut in tax credits :
Create Diagrams to Explain Complex Concepts and Processes
You can create diagrams for many aspects of your project, like this diagram explaining what type of protective gear is keeping doctors safe from Ebola:
Breaking down the protective gear helping keep doctors safe from Ebola http://t.co/bQUDqFoD1X pic.twitter.com/tDjkiSLFvs — Washington Post (@washingtonpost) September 15, 2014
Graphic Timelines
Regular text-based timelines + diagrams, photos, and other images = graphic timelines. Timelining is especially valuable in situations in which you need to track how a program, initiative, or campaign unfolds over time.
Interactive Timelines
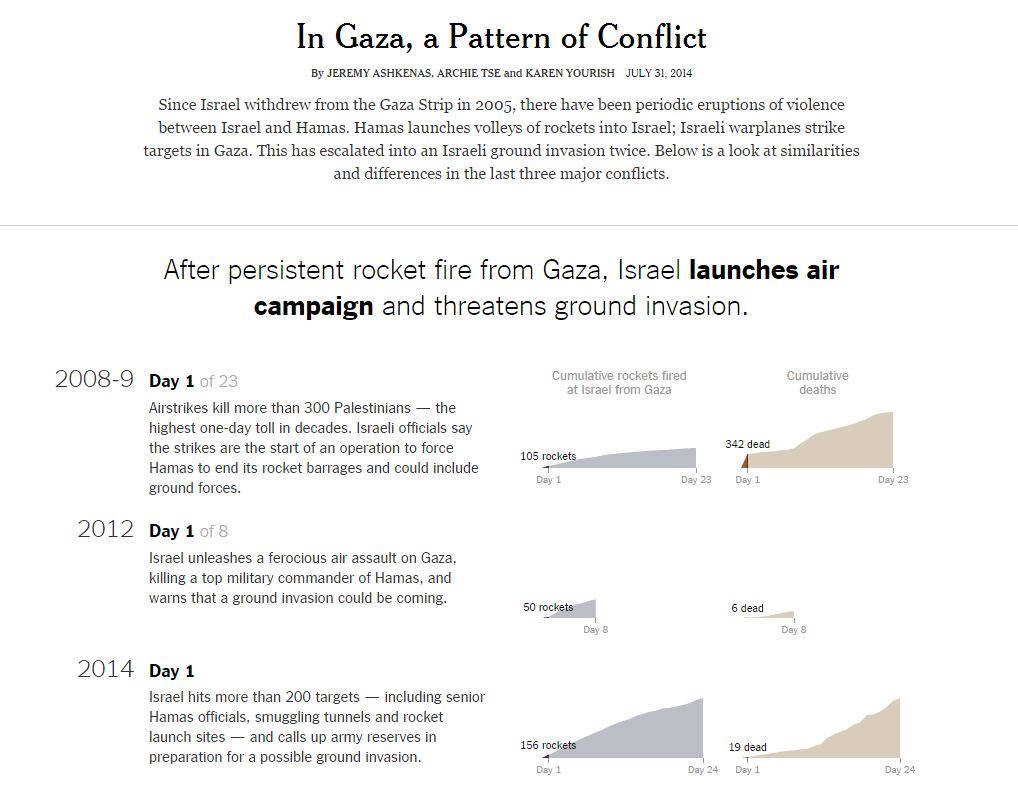
Static Timelines
Maybe you’re not the New York Times, I get it. Anyone can design a static timeline from the comfort of their PowerPoint slide.
A Graphic Timeline of the 21st Century Conservation Service Corps http://t.co/GmpTR3qfqv #21CSC #conservation pic.twitter.com/nGydFtkXkC — The Corps Network (@TheCorpsNetwork) August 12, 2014
Color-Coded Phrases
One of my all-time favorite examples of qualitative data visualization comes from the New York Times’ election coverage in 2016. They compared and contrasted speeches from Donald Trump and Hillary Clinton . First, the New York Times team presented miniature thumbnail images of each nominee’s convention speech. You can even click on the thumbnail images and they’ll expand so that you can read the transcript. I love how the thumbnails provide a birds-eye-view analysis of the qualitative themes from each speech simply by color-coding certain phrases.
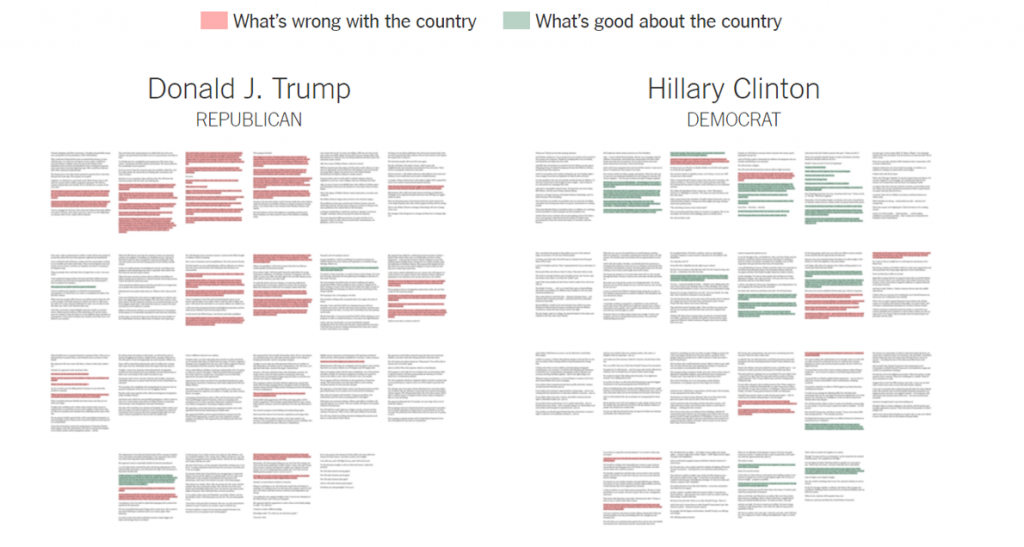
Directly underneath the thumbnails, the New York Times team pulled out a few sample quotes so that readers can get a sense of what was said.
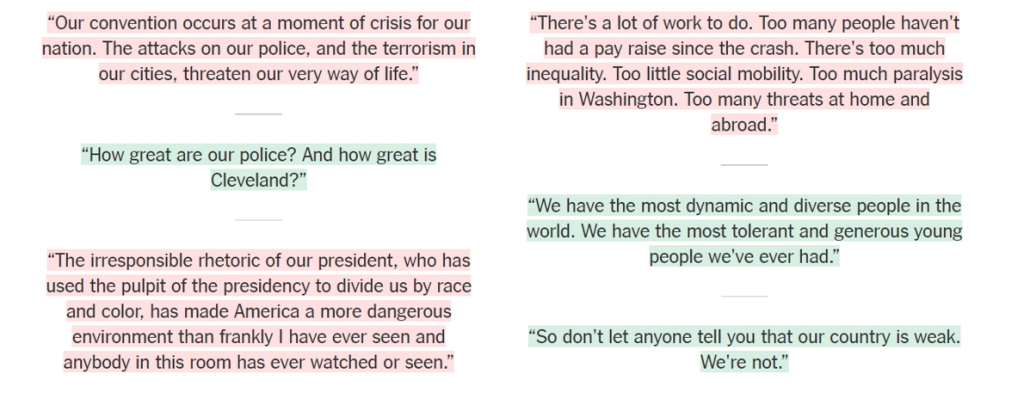
Want to try this technique yourself? Color-coded text is deceptively simple. I suggest highlighting the entire phrase in a light color, as the New York Times has done in this example. Make sure you don’t just color-coded the font itself. It’s challenging for our eyes to read green letters, but it’s pretty easy for our eyes to read black letters against light green background shading.
Comment and Share Your Ideas
How are you visualizing qualitative data interviews, focus groups, surveys, document reviews, and other qualitative data sources? Please link to your favorite resources below. Let’s give virtual high fives to the creators and celebrate a job well done.
You Might Like
Soar beyond the dusty shelf report, unlocking creativity: simple steps for non-designers to build powerful visual frameworks, great graphs.
- First Name *
Enter the URL below into your favorite RSS reader.
What to Do With All Those Open-Ended Responses? Data Visualization Techniques for Survey Researchers
- Citation (BibTeX)

Sorry, something went wrong. Please try again.
If this problem reoccurs, please contact Scholastica Support
Error message:
View more stats
Open-ended survey responses, where respondents provide responses in an unstructured, open-text format instead of defined response categories, are often a successful way to solicit authentic and unexpected feedback, highlight the diversity of responses or nuances in opinions, and capture the “why” that complements quantitative survey data. However, there are many challenges to analyzing and reporting open-ended data. This article draws on visual design best practices, such as Gestalt principles and the authors’ combined experience to demonstrate several visualization strategies that are relatively simple to implement with open-ended data. The application of visualization best practices to open-ended data can increase recall and effective decision-making and can transform findings into a dynamic data story.
Assessing the Problem and Defining Terms
In questionnaire design, close-ended questions (e.g., agree or disagree Likert scales, satisfaction ratings, preference rankings, frequency measures) are best used when a topic or construct is clearly defined, and the responses may be articulated in a few, simple pre-defined options. Open-ended survey questions, on the other hand, are more useful when asking about complex or “fuzzy” constructs—topics that are not well defined or may solicit a variety of responses that cannot be easily captured in one or more closed-ended questions.
Open-ended questions can be used as follow-ups to closed-ended questions, where the respondent is invited to expand on a particular topic or respond to a question in their own words in an unaided, freeform way (e.g., the classic “Please Specify” following selection of the “Other” option in a closed-ended question). They can also stand on their own as primary questions on a topic where closed-ended questions may not capture the information needed. Unlike closed-ended questions, open-ended questions can encourage respondents to share details about their experiences that the researcher did not anticipate, potentially sharing information more openly when the topic is sensitive or relates to personal matters (Allen 2017) . By soliciting authentic feedback and highlighting the diversity of responses, open-ended responses often capture the “why” that complements quantitative results, helping to tell a more nuanced story with the data.
The one commonality of all open-ended questions is that they do not prescribe how the respondent should answer, beyond the specific instructions or question phrasing. There may be character or space limits, but what the respondent shares is up to them. In addition to “Other (Specify)” questions scattered throughout a questionnaire, surveys often place general open-ended questions at the end of a questionnaire as a way to “wrap up” and provide respondents with an opportunity to share any final thoughts. The all-encompassing prompt “Is there anything else you would like to say?” at the end of a structured questionnaire is a common example of this (O’Cathain and Thomas 2004) . While much has been written about how to write quantitative survey questions (e.g., Dillman and Dillman 2000; Fowler 1995; Tourangeau , Rips , and Rainki 2000 ) and report on them (Heeringa , West , and Berglund 2017) , much less has been said in our field about how to ask and analyze open-ended questions. Their place as a qualitative metric in an otherwise quantitative survey often makes them not quite substantial enough for a fully qualitative study, but not quite measurable enough to be useful for quantitative analysis.
Thematic analysis using a coding system to organize information in a way that allows researchers to draw reasonable and meaningful conclusions from the data is a widespread method for qualitative analysis (Suter 2012) . At the same time, quantitative researchers who choose to include open-ended responses in their surveys do not always make full use of the resulting qualitative data, either because they do not have an explicit analytical strategy, or because of limited time, resources or expertise in how to analyze and present the findings (Decorte et al. 2019) . When quantitative researchers do present open-ended data alongside quantitative results, approaches may be perfunctory at best—such as selecting a few quotes to exhibit, or word clouds—and can reduce the value and depth of the information, ultimately devaluing the time and effort respondents may have taken to provide a response (Singer and Couper 2017) . This is not entirely the fault of individual researchers. It is widely acknowledged that techniques for qualitative visualization are less developed than for quantitative analysis (Evergreen 2020) .
Despite potential challenges that researchers may associate with analysis and reporting on open-ended survey responses, our goal is to highlight simple data visualization techniques available through basic software that can transform these data into a visually compelling story. The qualitative data presentations in this article were all created using Microsoft Office products such as PowerPoint and Excel, which have incredibly powerful visualization capabilities that can make visualizing qualitative data more accessible than it once was. The remainder of this article highlights how data visualization can be used as a tool to enhance our understanding of open-ended survey responses and to complement or augment the broader narrative derived from quantitative data.
Simple Methods for Tackling Open-ended Data Analysis
Coding the data.
Open-ended survey responses should be used to enhance, confirm, or refine the story told through quantitative data. For example, if survey respondents generally rate a program favorably, the open-ended feedback may highlight the specific aspects of the program that participants appreciate the most. Similarly, a follow-up open-ended question can add important nuances to the quantitative items that precede it. For example, in a survey related to willingness to receive a new COVID vaccine, open-ended feedback may shed light on why respondents may be willing or unwilling to get vaccinated. Qualitative data may also be used to highlight weaknesses or inconsistencies in the quantitative data itself. Using the vaccine hesitancy example, before COVID vaccines became widely available, many Americans were reluctant to definitively say whether they would or would not get vaccinated, instead reporting that they “didn’t know” or were “unsure.” News reports that focused on the proportions that would get the vaccine thereby showed relatively low levels of acceptance (Neergaard and Fingerhut 2020) strategically-crafted open-ended follow-up question could have shown that most of these respondents simply needed more information (and what kind) or preferred to wait and see. Open-ended data could therefore have reframed the narrative that took hold from the survey results.
The first step in exploring responses from open-ended questions is to review the raw responses and begin the process of preliminary data coding using a combination of deductive codes drawn from the research questions and inductive codes generated by the data. As the coding progresses, the initial codes are grouped into categories while attributes emerge, forming new codes (Saldana 2015) . Throughout this process, patterns in the data begin to take shape, forming the outlines of a story or stories that will add richness to the results.
Specific visual presentations may require that the codes and categories be organized in unique ways, and the process is inherently dynamic. For example, researchers may want to consider the number of codes, the use of primary and secondary codes, or the connections between codes to prepare for different types of visualizations. Importantly, the storytelling approach, subject matter and target audience for both the quantitative and qualitative items in the survey drive the amount of context needed or the level of complexity, and ultimately will inform the choice of visualization.
Assessing Your Toolbox of Visualization Strategies
Data visualization is the practice of translating information into a visual context. The goal of any data visualization is to make the most important findings easier for a viewer to extract, and ideally, to help drive decision-making (Berinato 2016) . According to Gestalt principles for data visualization, there are psychological and perceptual roots to how people perceive visual stimuli and make meaning from it; essentially, how the brain understands visual information (Knaflic 2015) . These principles—proximity, similarity, closure, connection and enclosure—serve as a data visualization “toolbox” (Betzendahl 2020; triva79 2019) . While these principles are most often applied to quantitative data, they can be used to transform qualitative data as well.
Applying Gestalt Principles to Qualitative Data Visualization
Once a survey’s open-ended responses have been thematically coded in some meaningful way, they can be visually represented using the following Gestalt principles:
Color and shape can be used to highlight commonality among respondents or topics. This may include visualizations such as a heat map or a spectrum display. While these are both commonly used for small-sample interviews or focus groups, they can be adapted to qualitative survey data to convey how respondents may be grouped together, for example, highlighting differences in opinions among different demographic groups who completed the survey.
Weight or size can display importance of information or a hierarchy of findings. While word clouds may be the most commonly used version of this (and arguably the least informative or valuable), a packed bubble diagram can be used to highlight notable themes while also displaying a second dimension. For example, in a survey of parents returning to work after COVID-19, the majority may say that they are “uncertain or nervous about their return.” However, open-ended survey responses may highlight differences in the reasons behind this uncertainty between male and female respondents. Each bubble can capture important nuances of the responses; for example, the size of the bubble can convey how frequently the response was selected, the placement can convey how it relates to other responses (such as clustering related responses), and the color can display key demographics such as who was more likely to support that sentiment.
Proximity and connection may be used to highlight the interconnection of ideas such as a process chart or a Venn diagram. In interviews or focus groups, this may be through a description of cause and effect. When it comes to open-ended survey data, proximity may highlight how different themes interrelate, with topics or themes that are closely related placed visually close to each other in the visualization, and loosely or unrelated topics placed further apart.
Examples from Two ICF Data Sets
This section demonstrates the principles discussed previously by applying them to open-ended responses from two surveys conducted by the research and consulting firm ICF. Both used the Surveys on the Go® smartphone-based nonprobability panel to collect quantitative and qualitative data from respondents.
Anti-littering Campaign (New York City): Respondents were asked about their opinions and attitudes about trash and littering, their littering behavior, and reasons why they litter. They were also asked to assess images from an anti-littering campaign, and whether they had seen those images around New York City. The results described in this article are based on 1,000 completed questionnaires collected in 2018. After viewing an image, respondents were asked to provide feedback to the following question: “What do you think the images are telling you to do?” All responses were coded into 10 thematic categories [1] and presented in descending order. [2]
COVID-19 Monitor Survey (US): Using a Census-balanced, national sample of approximately 1,000 adults from the same panel vendor, this survey asked respondents about their experience with and opinions about COVID-19, such as the government’s response to the virus, personal financial impact, and the effect of lockdowns on mental health. [3] The results shown in this article are based on three waves of the study, which fielded in May, June, and July 2020. Respondents who indicated that they were unwilling to receive a COVID vaccine as soon as it became available were asked to identify the reasons why; these freeform statements were then assigned one of 10 categories, after the process of grouping similar codes together.
Figure 1 highlights two versions of the same data gathered as part of the Anti-littering Campaign (n = 786). The first is a traditional table with the counts associated with each category in descending order; the second is a packed bubble chart, created in Excel, which uses the Gestalt principle of size to portray the importance or frequency of each category in relation to the others (i.e., the largest circle was the most common response). By applying a secondary principle, color , the figure also indicates a secondary dimension, in this case the “tone” of the comment. Generally, people responded in one of the following three ways:
They were neutral in their feedback and understood that the image was telling them “not to litter.”
They generally conveyed a positive tone or impact related to community (i.e., a shared responsibility or call to action)
They pointed to the negative impact of littering (e.g., it harms animals or pollutes the environment).
These nuances are incredibly valuable for assessing motivating factors and potentially tapping into these themes for future messages. By effectively using color and size, the open-ended data now adds value to the interpretation of survey results.

Another important principle is that of connection , specifically the way in which multiple layers of meaning within open-ended responses may overlap. Figure 2 presents a sunburst graphic, which illustrates the relationship between the different units of qualitative analysis: the inner circle summarizes the broader category, and the outer circle summarizes any individual codes applied to the data at a more granular level. Each circle should be read like a doughnut plot or pie chart with the amount of space taken up by the “slice” of the donut or pie reflecting the relative frequency or percentage of that concept (i.e., the size principle). While pie and doughnut charts themselves have received well-deserved criticism (e.g., Kosara and Skau 2016; Tufte 2006 ), we find this specific application to be useful for showing the layers of meaning contained in the qualitative data. For example, within the broader category of vaccine safety and effectiveness concerns, the coders identified attributes that appeared to leave the door open to reconsidering the vaccine when more information became available (i.e., it was “too new,” or that the clinical trials were too fast).

If the coding process identifies a hierarchy of concepts, there are ways to display that information in a way that retains this ranking or illustrates how it may change over time. Figure 3 is a dot plot of three waves of data. By applying the principle of proximity, the graphic identifies the change in importance for each of the 10 categories. While the categories that were most substantial (safety/effectiveness of the COVID vaccine) and least substantial (medical condition) remained consistent, the importance of the other eight in impacting the likelihood of getting the vaccine varied across waves. For example, uncertainty generally increased as a factor over time relative to other factors, while the need for more information decreased in importance.

Reflection on Open-ended Data Visualization in Practice
Due to a range of practical considerations (e.g., cost, time, and staff availability), researchers often must pick between quantitative and qualitative data, and fail to recognize the potential of using a few carefully-selected open-ended questions within quantitative instruments. Since respondents have spent time and effort to provide this data, there is often a desire on the part of study team to “do something” with it, but too often, the open-ends fall by the wayside—usually becoming a word cloud or a table in the appendix of a report. We strongly believe that qualitative data, when visualized in creative ways, can provide context and nuance that can enhance and illuminate the quantitative findings, adding depth, rationale, or even just a telltale example to the data-driven narrative. When combined with the quantitative data, open-ended responses can be transformed into dynamic data stories told through simple visualization techniques.
An eleventh category reflected responses that were unrelated or invalid. This was a small fraction of the total responses and is not particularly helpful for analysis.
It is worth noting that some respondents provided an answer that did not directly address the original question. While respondents were asked “What do you think the image is telling you to do?”, many responses were more broadly about “What message do the images convey as to why you should not litter?”
See: https://www.icf.com/insights/health/americans-reluctance-covid-vaccine
Submitted : February 05, 2021 EDT
Accepted : July 06, 2021 EDT
How To Present Qualitative Data In Powerpoint
Are you ready to take your qualitative data presentations to the next level?
From understanding what qualitative data is to tips for engaging your audience, we will cover everything you need to know to create a powerful presentation.
Key Takeaways:
What is qualitative data.
Qualitative data refers to non-numerical information that helps in understanding the ‘why’ and ‘how’ of research findings and analysis.
By looking into the rich layers of qualitative data, researchers can unearth nuanced insights, uncover trends, and make sense of complex phenomena in a way that quantitative data alone cannot capture. Qualitative data often takes the form of interviews, observations, or open-ended survey responses, providing depth and context to research inquiries. Its role in research methodology is crucial, as it allows for a deep exploration of human experiences, perceptions, and behaviors. Through thematic analysis and coding, researchers can identify patterns, themes, and relationships within qualitative data, leading to comprehensive and meaningful interpretations.
Examples of Qualitative Data
Examples of qualitative data include quotes from participants, observational information, and detailed descriptions of outcomes.
Why Use PowerPoint to Present Qualitative Data?
Utilizing PowerPoint for presenting qualitative data offers a structured and visually engaging format that enhances audience comprehension.
One of the key benefits of using PowerPoint for presentations is its user-friendly interface, making it easy to create visually appealing slides that can effectively convey complex data in a simplified manner.
Benefits of Using Powerpoint for Qualitative Data
In the realm of audience engagement, PowerPoint enables presenters to capture and maintain the attention of their viewers through visually appealing slides, engaging animations, and interactive elements. This multimedia approach not only helps in conveying complex information in a simplified manner but also aids in creating a lasting impact on the audience. The clear structure provided by PowerPoint helps in organizing the content logically, ensuring that the message flows seamlessly and is easy to follow.
Preparing Your Data for Presentation
Enhancing the visual appeal of your presentation through color schemes, fonts, and layouts can make your data more engaging and memorable. A visually appealing presentation not only captures attention but also reinforces the key insights you want to communicate.
Organizing Qualitative Data
Organizing qualitative data involves categorizing information based on participants, methodology, and thematic analysis to create a coherent narrative.
Choosing the Right Visuals
Selecting the appropriate visuals such as images and icons can significantly enhance the presentation of qualitative data by making complex information more accessible.
Visual elements play a crucial role in conveying key messages effectively, especially when dealing with qualitative data. Incorporating well-chosen images can evoke emotions and provide context to the data presented, enabling viewers to grasp the underlying insights more easily. Icons, on the other hand, offer a concise way to represent different categories or concepts, aiding in the organization and interpretation of information. By using a combination of these visual elements , presentations become not only visually appealing but also more engaging and memorable for the audience.
Designing Your PowerPoint Slides
When selecting color schemes for your PowerPoint slides, it’s crucial to choose a palette that is visually appealing and enhances the overall message you want to convey. Bold, contrasting colors can help emphasize key points, while subtle tones can create a more professional look. Font choices play a significant role in readability. Opt for clean, easy-to-read fonts, and avoid using too many different styles in one slide.
Integrating text and visuals seamlessly can make your PowerPoint slides more engaging. Use images, charts, and graphs to support your content and reinforce key points. Make sure the visuals are high-quality, and relevant, and add value to the information you’re presenting.
Color and Font Choices
Choosing suitable colors and fonts in PowerPoint design is crucial for conveying information effectively and maintaining visual coherence throughout the presentation.
Layout and Structure
When creating PowerPoint presentations, a well-thought-out layout and structure can make the content more digestible for the audience and enhance overall comprehension. By organizing information into clear sections with headings and subheadings, the presenter can guide viewers through the key points effortlessly.
Incorporating Text and Images
Incorporating a balance of text and images in PowerPoint slides can enrich the presentation by providing visual context and real-world examples to support qualitative data.
Tips for Presenting Qualitative Data Effectively
When presenting qualitative data, it is crucial to understand the audience’s interests and tailor the information to resonate with them. Incorporating real-life examples and anecdotes can make the data more relatable and engaging. Structuring the data sequentially and logically helps in guiding the audience through the insights effectively. Utilizing visual aids such as charts, graphs, and infographics can enhance comprehension and strengthen the impact of the data presentation.
Engaging Your Audience
Using storytelling techniques.
Utilizing storytelling techniques can transform qualitative data into compelling narratives that resonate with the audience and enhance the data’s overall impact.
Interpreting and Explaining the Data
Effectively interpreting and explaining qualitative data involves contextualizing the findings within the research framework and articulating the significance of the outcomes derived from the analysis.
Conclusion: Creating a Powerful Presentation
In conclusion , crafting a powerful presentation of qualitative data involves synthesizing key outcomes, integrating visual elements for impact, and ensuring a cohesive narrative that resonates with the audience.
Weave a compelling narrative around your data, linking the findings together in a meaningful way. This helps create a story that captivates your audience and makes the information more relatable.
Frequently Asked Questions
How do i present qualitative data in powerpoint.
To present qualitative data in PowerPoint, you can use charts, graphs, or tables. You can also use images or screenshots to visually represent the data. Make sure to include a brief explanation or key points for each piece of data.
What kind of charts should I use to present qualitative data in PowerPoint?
Can i customize the design of my qualitative data presentation in powerpoint.
Yes, you can customize the design of your presentation by using different colors, fonts, and styles. You can also add animations or transitions to make your presentation more engaging.
How should I organize my qualitative data in PowerPoint?
Is there a specific format i should follow when presenting qualitative data in powerpoint, how can i make my qualitative data presentation in powerpoint more engaging.
In addition to using visuals and customizing the design as mentioned earlier, you can also include real-life examples or stories to help illustrate the data. You can also incorporate interactive elements such as polls or quizzes to engage your audience and make the presentation more interactive.
Similar Posts
How to add font in powerpoint on mac, how to embed a video in powerpoint from youtube, how to embed a youtube video in powerpoint with start and end time, how to reuse slides in powerpoint, how to use ruler in powerpoint, how to record in powerpoint on ipad.
Integrations
What's new?
In-Product Prompts
Participant Management
Interview Studies
Prototype Testing
Card Sorting
Tree Testing
Live Website Testing
Automated Reports
Templates Gallery
Choose from our library of pre-built mazes to copy, customize, and share with your own users
Browse all templates
Financial Services
Tech & Software
Product Designers
Product Managers
User Researchers
By use case
Concept & Idea Validation
Wireframe & Usability Test
Content & Copy Testing
Feedback & Satisfaction
Content Hub
Educational resources for product, research and design teams
Explore all resources
Question Bank
Maze Research Success Hub
Guides & Reports
Help Center
Future of User Research Report
The Optimal Path Podcast
User Research
Aug 19, 2024 • 17 minutes read
Qualitative research examples: How to unlock, rich, descriptive insights
Qualitative research uncovers in-depth user insights, but what does it look like? Here are seven methods and examples to help you get the data you need.

Armin Tanovic
Behind every what, there’s a why . Qualitative research is how you uncover that why. It enables you to connect with users and understand their thoughts, feelings, wants, needs, and pain points.
There’s many methods for conducting qualitative research, and many objectives it can help you pursue—you might want to explore ways to improve NPS scores, combat reduced customer retention, or understand (and recreate) the success behind a well-received product. The common thread? All these metrics impact your business, and qualitative research can help investigate and improve that impact.
In this article, we’ll take you through seven methods and examples of qualitative research, including when and how to use them.
Qualitative UX research made easy
Conduct qualitative research with Maze, analyze data instantly, and get rich, descriptive insights that drive decision-making.

7 Qualitative research methods: An overview
There are various qualitative UX research methods that can help you get in-depth, descriptive insights. Some are suited to specific phases of the design and development process, while others are more task-oriented.
Here’s our overview of the most common qualitative research methods. Keep reading for their use cases, and detailed examples of how to conduct them.
Method | |||
|---|---|---|---|
User interviews | |||
Focus groups | |||
Ethnographic research | |||
Qualitative observation | |||
Case study research | |||
Secondary research | |||
Open-ended surveys | to extract descriptive insights. |
1. User interviews
A user interview is a one-on-one conversation between a UX researcher, designer or Product Manager and a target user to understand their thoughts, perspectives, and feelings on a product or service. User interviews are a great way to get non-numerical data on individual experiences with your product, to gain a deeper understanding of user perspectives.
Interviews can be structured, semi-structured, or unstructured . Structured interviews follow a strict interview script and can help you get answers to your planned questions, while semi and unstructured interviews are less rigid in their approach and typically lead to more spontaneous, user-centered insights.
When to use user interviews
Interviews are ideal when you want to gain an in-depth understanding of your users’ perspectives on your product or service, and why they feel a certain way.
Interviews can be used at any stage in the product design and development process, being particularly helpful during:
- The discovery phase: To better understand user needs, problems, and the context in which they use your product—revealing the best potential solutions
- The design phase: To get contextual feedback on mockups, wireframes, and prototypes, helping you pinpoint issues and the reasons behind them
- Post-launch: To assess if your product continues to meet users’ shifting expectations and understand why or why not
How to conduct user interviews: The basics
- Draft questions based on your research objectives
- Recruit relevant research participants and schedule interviews
- Conduct the interview and transcribe responses
- Analyze the interview responses to extract insights
- Use your findings to inform design, product, and business decisions
💡 A specialized user interview tool makes interviewing easier. With Maze Interview Studies , you can recruit, host, and analyze interviews all on one platform.
User interviews: A qualitative research example
Let’s say you’ve designed a recruitment platform, called Tech2Talent , that connects employers with tech talent. Before starting the design process, you want to clearly understand the pain points employers experience with existing recruitment tools'.
You draft a list of ten questions for a semi-structured interview for 15 different one-on-one interviews. As it’s semi-structured, you don’t expect to ask all the questions—the script serves as more of a guide.
One key question in your script is: “Have tech recruitment platforms helped you find the talent you need in the past?”
Most respondents answer with a resounding and passionate ‘no’ with one of them expanding:
“For our company, it’s been pretty hit or miss honestly. They let just about anyone make a profile and call themselves tech talent. It’s so hard sifting through serious candidates. I can’t see any of their achievements until I invest time setting up an interview.”
You begin to notice a pattern in your responses: recruitment tools often lack easily accessible details on talent profiles.
You’ve gained contextual feedback on why other recruitment platforms fail to solve user needs.
2. Focus groups
A focus group is a research method that involves gathering a small group of people—around five to ten users—to discuss a specific topic, such as their’ experience with your new product feature. Unlike user interviews, focus groups aim to capture the collective opinion of a wider market segment and encourage discussion among the group.
When to use focus groups
You should use focus groups when you need a deeper understanding of your users’ collective opinions. The dynamic discussion among participants can spark in-depth insights that might not emerge from regular interviews.
Focus groups can be used before, during, and after a product launch. They’re ideal:
- Throughout the problem discovery phase: To understand your user segment’s pain points and expectations, and generate product ideas
- Post-launch: To evaluate and understand the collective opinion of your product’s user experience
- When conducting market research: To grasp usage patterns, consumer perceptions, and market opportunities for your product
How to conduct focus group studies: The basics
- Draft prompts to spark conversation, or a series of questions based on your UX research objectives
- Find a group of five to ten users who are representative of your target audience (or a specific user segment) and schedule your focus group session
- Conduct the focus group by talking and listening to users, then transcribe responses
- Analyze focus group responses and extract insights
- Use your findings to inform design decisions
The number of participants can make it difficult to take notes or do manual transcriptions. We recommend using a transcription or a specialized UX research tool , such as Maze, that can automatically create ready-to-share reports and highlight key user insights.
Focus groups: A qualitative research example
You’re a UX researcher at FitMe , a fitness app that creates customized daily workouts for gym-goers. Unlike many other apps, FitMe takes into account the previous day’s workout and aims to create one that allows users to effectively rest different muscles.
However, FitMe has an issue. Users are generating workouts but not completing them. They’re accessing the app, taking the necessary steps to get a workout for the day, but quitting at the last hurdle.
Time to talk to users.
You organize a focus group to get to the root of the drop-off issue. You invite five existing users, all of whom have dropped off at the exact point you’re investigating, and ask them questions to uncover why.
A dialog develops:
Participant 1: “Sometimes I’ll get a workout that I just don’t want to do. Sure, it’s a good workout—but I just don’t want to physically do it. I just do my own thing when that happens.”
Participant 2: “Same here, some of them are so boring. I go to the gym because I love it. It’s an escape.”
Participant 3: “Right?! I get that the app generates the best one for me on that specific day, but I wish I could get a couple of options.”
Participant 4: “I’m the same, there are some exercises I just refuse to do. I’m not coming to the gym to do things I dislike.”
Conducting the focus groups and reviewing the transcripts, you realize that users want options. A workout that works for one gym-goer doesn’t necessarily work for the next.
A possible solution? Adding the option to generate a new workout (that still considers previous workouts)and the ability to blacklist certain exercises, like burpees.
3. Ethnographic research
Ethnographic research is a research method that involves observing and interacting with users in a real-life environment. By studying users in their natural habitat, you can understand how your product fits into their daily lives.
Ethnographic research can be active or passive. Active ethnographic research entails engaging with users in their natural environment and then following up with methods like interviews. Passive ethnographic research involves letting the user interact with the product while you note your observations.
When to use ethnographic research
Ethnographic research is best suited when you want rich insights into the context and environment in which users interact with your product. Keep in mind that you can conduct ethnographic research throughout the entire product design and development process —from problem discovery to post-launch. However, it’s mostly done early in the process:
- Early concept development: To gain an understanding of your user's day-to-day environment. Observe how they complete tasks and the pain points they encounter. The unique demands of their everyday lives will inform how to design your product.
- Initial design phase: Even if you have a firm grasp of the user’s environment, you still need to put your solution to the test. Conducting ethnographic research with your users interacting with your prototype puts theory into practice.
How to conduct ethnographic research:
- Recruit users who are reflective of your audience
- Meet with them in their natural environment, and tell them to behave as they usually would
- Take down field notes as they interact with your product
- Engage with your users, ask questions, or host an in-depth interview if you’re doing an active ethnographic study
- Collect all your data and analyze it for insights
While ethnographic studies provide a comprehensive view of what potential users actually do, they are resource-intensive and logistically difficult. A common alternative is diary studies. Like ethnographic research, diary studies examine how users interact with your product in their day-to-day, but the data is self-reported by participants.
⚙️ Recruiting participants proving tough and time-consuming? Maze Panel makes it easy, with 400+ filters to find your ideal participants from a pool of 3 million participants.
Ethnographic research: A qualitative research example
You're a UX researcher for a project management platform called ProFlow , and you’re conducting an ethnographic study of the project creation process with key users, including a startup’s COO.
The first thing you notice is that the COO is rushing while navigating the platform. You also take note of the 46 tabs and Zoom calls opened on their monitor. Their attention is divided, and they let out an exasperated sigh as they repeatedly hit “refresh” on your website’s onboarding interface.
You conclude the session with an interview and ask, “How easy or difficult did you find using ProFlow to coordinate a project?”
The COO answers: “Look, the whole reason we turn to project platforms is because we need to be quick on our feet. I’m doing a million things so I need the process to be fast and simple. The actual project management is good, but creating projects and setting up tables is way too complicated.”
You realize that ProFlow ’s project creation process takes way too much time for professionals working in fast-paced, dynamic environments. To solve the issue, propose a quick-create option that enables them to move ahead with the basics instead of requiring in-depth project details.
4. Qualitative observation
Qualitative observation is a similar method to ethnographic research, though not as deep. It involves observing your users in a natural or controlled environment and taking notes as they interact with a product. However, be sure not to interrupt them, as this compromises the integrity of the study and turns it into active ethnographic research.
When to qualitative observation
Qualitative observation is best when you want to record how users interact with your product without anyone interfering. Much like ethnographic research, observation is best done during:
- Early concept development: To help you understand your users' daily lives, how they complete tasks, and the problems they deal with. The observations you collect in these instances will help you define a concept for your product.
- Initial design phase: Observing how users deal with your prototype helps you test if they can easily interact with it in their daily environments
How to conduct qualitative observation:
- Recruit users who regularly use your product
- Meet with users in either their natural environment, such as their office, or within a controlled environment, such as a lab
- Observe them and take down field notes based on what you notice
Qualitative observation: An qualitative research example
You’re conducting UX research for Stackbuilder , an app that connects businesses with tools ideal for their needs and budgets. To determine if your app is easy to use for industry professionals, you decide to conduct an observation study.
Sitting in with the participant, you notice they breeze past the onboarding process, quickly creating an account for their company. Yet, after specifying their company’s budget, they suddenly slow down. They open links to each tool’s individual page, confusingly switching from one tab to another. They let out a sigh as they read through each website.
Conducting your observation study, you realize that users find it difficult to extract information from each tool’s website. Based on your field notes, you suggest including a bullet-point summary of each tool directly on your platform.
5. Case study research
Case studies are a UX research method that provides comprehensive and contextual insights into a real-world case over a long period of time. They typically include a range of other qualitative research methods, like interviews, observations, and ethnographic research. A case study allows you to form an in-depth analysis of how people use your product, helping you uncover nuanced differences between your users.
When to use case studies
Case studies are best when your product involves complex interactions that need to be tracked over a longer period or through in-depth analysis. You can also use case studies when your product is innovative, and there’s little existing data on how users interact with it.
As for specific phases in the product design and development process:
- Initial design phase: Case studies can help you rigorously test for product issues and the reasons behind them, giving you in-depth feedback on everything between user motivations, friction points, and usability issues
- Post-launch phase: Continuing with case studies after launch can give you ongoing feedback on how users interact with the product in their day-to-day lives. These insights ensure you can meet shifting user expectations with product updates and future iterations
How to conduct case studies:
- Outline an objective for your case study such as examining specific user tasks or the overall user journey
- Select qualitative research methods such as interviews, ethnographic studies, or observations
- Collect and analyze your data for comprehensive insights
- Include your findings in a report with proposed solutions

Case study research: A qualitative research example
Your team has recently launched Pulse , a platform that analyzes social media posts to identify rising digital marketing trends. Pulse has been on the market for a year, and you want to better understand how it helps small businesses create successful campaigns.
To conduct your case study, you begin with a series of interviews to understand user expectations, ethnographic research sessions, and focus groups. After sorting responses and observations into common themes you notice a main recurring pattern. Users have trouble interpreting the data from their dashboards, making it difficult to identify which trends to follow.
With your synthesized insights, you create a report with detailed narratives of individual user experiences, common themes and issues, and recommendations for addressing user friction points.
Some of your proposed solutions include creating intuitive graphs and summaries for each trend study. This makes it easier for users to understand trends and implement strategic changes in their campaigns.
6. Secondary research
Secondary research is a research method that involves collecting and analyzing documents, records, and reviews that provide you with contextual data on your topic. You’re not connecting with participants directly, but rather accessing pre-existing available data. For example, you can pull out insights from your UX research repository to reexamine how they apply to your new UX research objective.
Strictly speaking, it can be both qualitative and quantitative—but today we focus on its qualitative application.
When to use secondary research
Record keeping is particularly useful when you need supplemental insights to complement, validate, or compare current research findings. It helps you analyze shifting trends amongst your users across a specific period. Some other scenarios where you need record keeping include:
- Initial discovery or exploration phase: Secondary research can help you quickly gather background information and data to understand the broader context of a market
- Design and development phase: See what solutions are working in other contexts for an idea of how to build yours
Secondary research is especially valuable when your team faces budget constraints, tight deadlines, or limited resources. Through review mining and collecting older findings, you can uncover useful insights that drive decision-making throughout the product design and development process.
How to conduct secondary research:
- Outline your UX research objective
- Identify potential data sources for information on your product, market, or target audience. Some of these sources can include: a. Review websites like Capterra and G2 b. Social media channels c. Customer service logs and disputes d. Website reviews e. Reports and insights from previous research studies f. Industry trends g. Information on competitors
- Analyze your data by identifying recurring patterns and themes for insights
Secondary research: A qualitative research example
SafeSurf is a cybersecurity platform that offers threat detection, security audits, and real-time reports. After conducting multiple rounds of testing, you need a quick and easy way to identify remaining usability issues. Instead of conducting another resource-intensive method, you opt for social listening and data mining for your secondary research.
Browsing through your company’s X, you identify a recurring theme: many users without a background in tech find SafeSurf ’s reports too technical and difficult to read. Users struggle with understanding what to do if their networks are breached.
After checking your other social media channels and review sites, the issue pops up again.
With your gathered insights, your team settles on introducing a simplified version of reports, including clear summaries, takeaways, and step-by-step protocols for ensuring security.
By conducting secondary research, you’ve uncovered a major usability issue—all without spending large amounts of time and resources to connect with your users.
7. Open-ended surveys
Open-ended surveys are a type of unmoderated UX research method that involves asking users to answer a list of qualitative research questions designed to uncover their attitudes, expectations, and needs regarding your service or product. Open-ended surveys allow users to give in-depth, nuanced, and contextual responses.
When to use open-ended surveys
User surveys are an effective qualitative research method for reaching a large number of users. You can use them at any stage of the design and product development process, but they’re particularly useful:
- When you’re conducting generative research : Open-ended surveys allow you to reach a wide range of users, making them especially useful during initial research phases when you need broad insights into user experiences
- When you need to understand customer satisfaction: Open-ended customer satisfaction surveys help you uncover why your users might be dissatisfied with your product, helping you find the root cause of their negative experiences
- In combination with close-ended surveys: Get a combination of numerical, statistical insights and rich descriptive feedback. You��’ll know what a specific percentage of your users think and why they think it.
How to conduct open-ended surveys:
- Design your survey and draft out a list of survey questions
- Distribute your surveys to respondents
- Analyze survey participant responses for key themes and patterns
- Use your findings to inform your design process
Open-ended surveys: A qualitative research example
You're a UX researcher for RouteReader , a comprehensive logistics platform that allows users to conduct shipment tracking and route planning. Recently, you’ve launched a new predictive analytics feature that allows users to quickly identify and prepare for supply chain disruptions.
To better understand if users find the new feature helpful, you create an open-ended, in-app survey.
The questions you ask your users:
- “What has been your experience with our new predictive analytics feature?"
- “Do you find it easy or difficult to rework your routes based on our predictive suggestions?”
- “Does the predictive analytics feature make planning routes easier? Why or why not?”
Most of the responses are positive. Users report using the predictive analytics feature to make last-minute adjustments to their route plans, and some even rely on it regularly. However, a few users find the feature hard to notice, making it difficult to adjust their routes on time.
To ensure users have supply chain insights on time, you integrate the new feature into each interface so users can easily spot important information and adjust their routes accordingly.
💡 Surveys are a lot easier with a quality survey tool. Maze’s Feedback Surveys solution has all you need to ensure your surveys get the insights you need—including AI-powered follow-up and automated reports.
Qualitative research vs. quantitative research: What’s the difference?
Alongside qualitative research approaches, UX teams also use quantitative research methods. Despite the similar names, the two are very different.
Here are some of the key differences between qualitative research and quantitative research .
Research type | ||||
|---|---|---|---|---|
Qualitative research | . | |||
Quantitative research |
Before selecting either qualitative or quantitative methods, first identify what you want to achieve with your UX research project. As a general rule of thumb, think qualitative data collection for in-depth understanding and quantitative studies for measurement and validation.
Conduct qualitative research with Maze
You’ll often find that knowing the what is pointless without understanding the accompanying why . Qualitative research helps you uncover your why.
So, what about how —how do you identify your 'what' and your 'why'?
The answer is with a user research tool like Maze.
Maze is the leading user research platform that lets you organize, conduct, and analyze both qualitative and quantitative research studies—all from one place. Its wide variety of UX research methods and advanced AI capabilities help you get the insights you need to build the right products and experiences faster.
Frequently asked questions about qualitative research examples
What is qualitative research?
Qualitative research is a research method that aims to provide contextual, descriptive, and non-numerical insights on a specific issue. Qualitative research methods like interviews, case studies, and ethnographic studies allow you to uncover the reasoning behind your user’s attitudes and opinions.
Can a study be both qualitative and quantitative?
Absolutely! You can use mixed methods in your research design, which combines qualitative and quantitative approaches to gain both descriptive and statistical insights.
For example, user surveys can have both close-ended and open-ended questions, providing comprehensive data like percentages of user views and descriptive reasoning behind their answers.
Is qualitative or quantitative research better?
The choice between qualitative and quantitative research depends upon your research goals and objectives.
Qualitative research methods are better suited when you want to understand the complexities of your user’s problems and uncover the underlying motives beneath their thoughts, feelings, and behaviors. Quantitative research excels in giving you numerical data, helping you gain a statistical view of your user's attitudes, identifying trends, and making predictions.
What are some approaches to qualitative research?
There are many approaches to qualitative studies. An approach is the underlying theory behind a method, and a method is a way of implementing the approach. Here are some approaches to qualitative research:
- Grounded theory: Researchers study a topic and develop theories inductively
- Phenomenological research: Researchers study a phenomenon through the lived experiences of those involved
- Ethnography: Researchers immerse themselves in organizations to understand how they operate
The 7 most common qualitative slides and how to use them
Table of contents.
Building strategy slide decks isn’t just about fancy charts and data. You also need to understand how to build conceptual or qualitative slides.
Fortunately, you only need to master a handful of conceptual slides. And these will be sufficient for communicating most qualitative insights. These include:
- Process, flow, and journey slides
Driver trees
Ranges and sliders, from-to slides, tables and heatmaps, text slides.
In this article, we break down each type of qualitative slide and teach you exactly when and why to use each.
Processes, flows and journeys
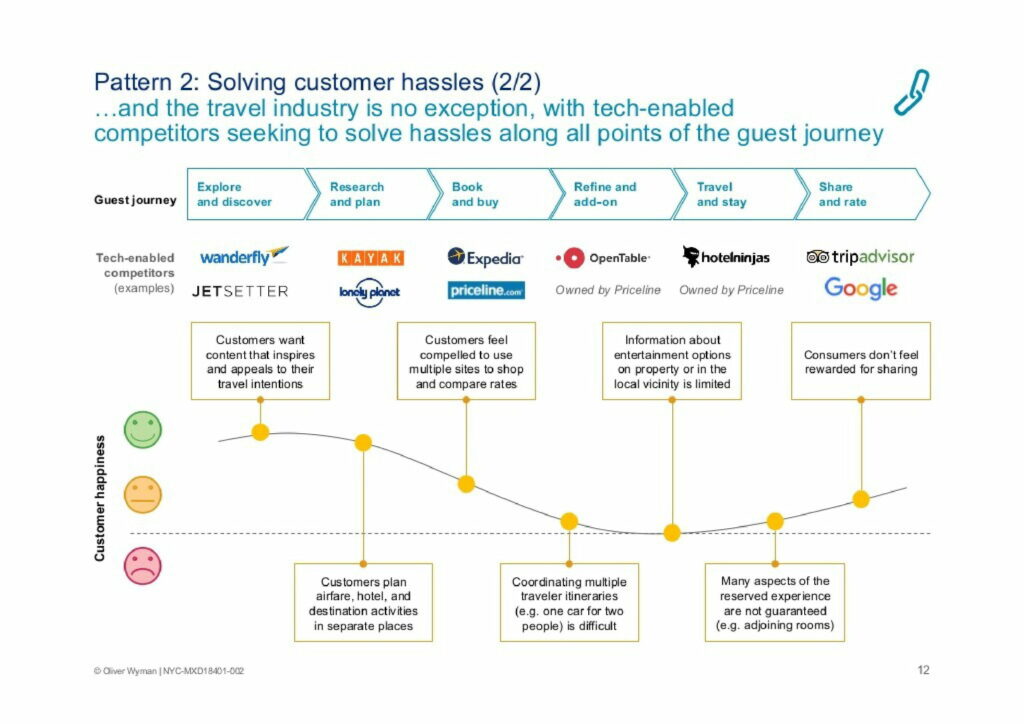
Process slides, flow slides, and journey slides are all used to show the effect of time. If you want to show an insight that has a time dimension, you should consider communicating it with a process, flow or journey.
In the slide above, Oliver Wyman is illustrating a travel guest’s journey from pre-travel research to post-travel review. Underneath, they highlight competitors and customer satisfaction at each stage of the journey.
Other common examples include customer journeys and the marketing funnel. You can see more examples of processes, flows and journeys in our slide library .
Download 120+ strategy consulting presentations for free
Looking for slide inspiration? Download 120+ consulting slide decks from top strategy consulting firms, such as McKinsey, BCG and Bain!
Matrixes are used to show how multiple concepts differ on two dimensions. They are useful because they show a full map of where those concepts could exist, as well as any overlap between the concepts.
For example, in the chart above, BCG are comparing traditional robotics and advanced robotics on the dimensions of task complexity and level of structure.
You can see more examples of matrixes in our slide library .
Driver trees are used to break down an outcome into the drivers or variables that influence it. You can continue to break down those drivers, which builds more and more branches of the tree.
These slides are most commonly used to break down a big, challenging problem into smaller, more manageable chunks. And in later slides, you’ll usually deep dive into each of the drivers in the tree.
In the slide above, you can see how Oliver Wyman broke down RevPARD into its drivers. And you can check out more examples of driver trees in our slide library .
Ranges and sliders show where a particular metric sits on a dimension. They are used when you don’t have a quantitative metric (so you can’t use a chart) but you want to show the ‘relativity’ between different data points.
For example, in the slide above, L.E.K Consulting is comparing a number of metrics on the dimension of coordination. There is no quantitative measure of coordination, so they use a slider.
You can check out more examples of ranges and slides in our slide library .
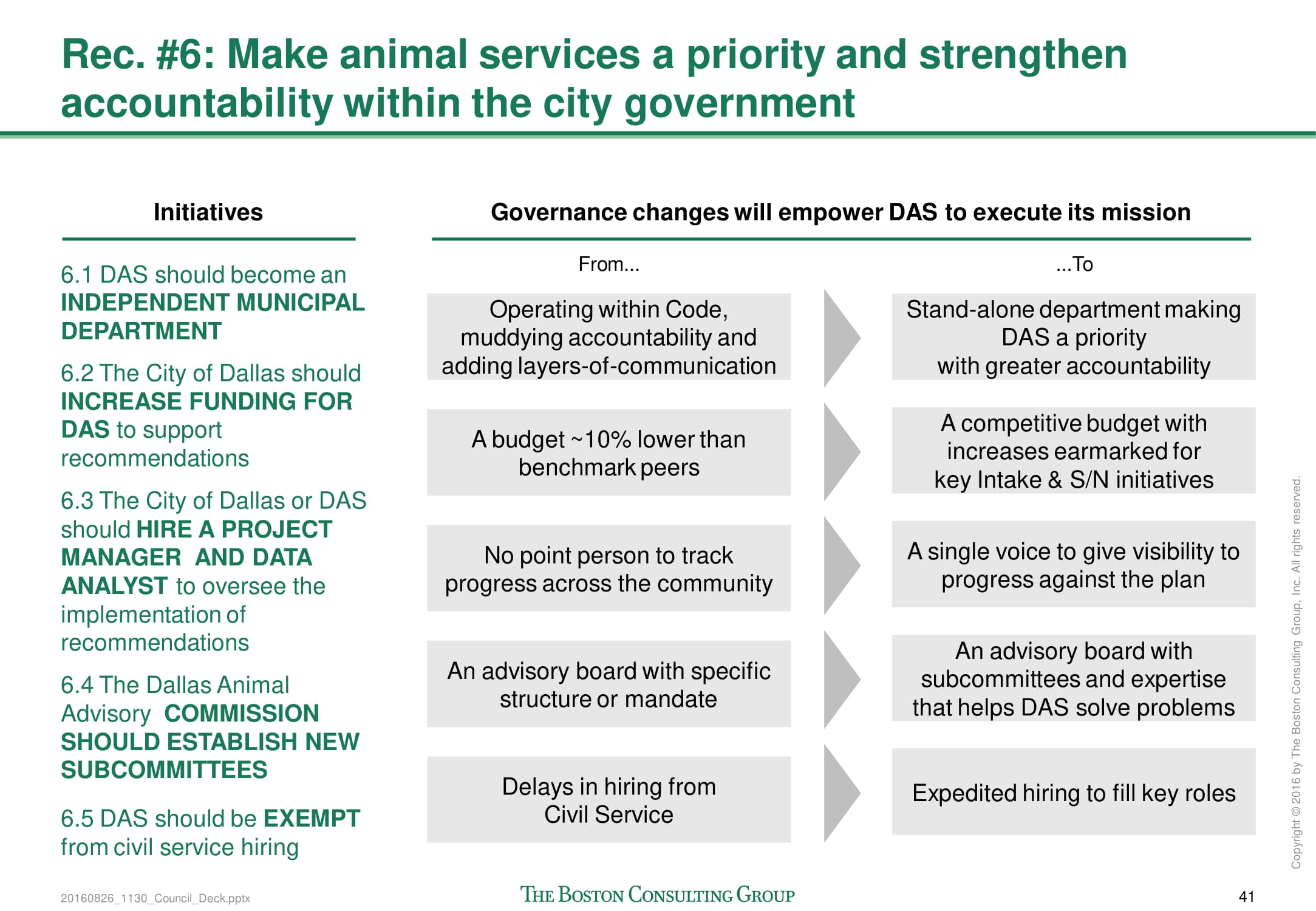
From-to slides are used to show how changes across a number of dimensions using text. First, you need to define a number of categories, then describe the current state, then describe the future state.
There are two common uses for from-to slides:
- You can use them as a context slide and then in later slides you can deep dive into how you’ll achieve the change
- You can use them to summarize the effect of an action or recommendation (like in the BCG example above)
You can check out more examples of from-to slides in our slide library .
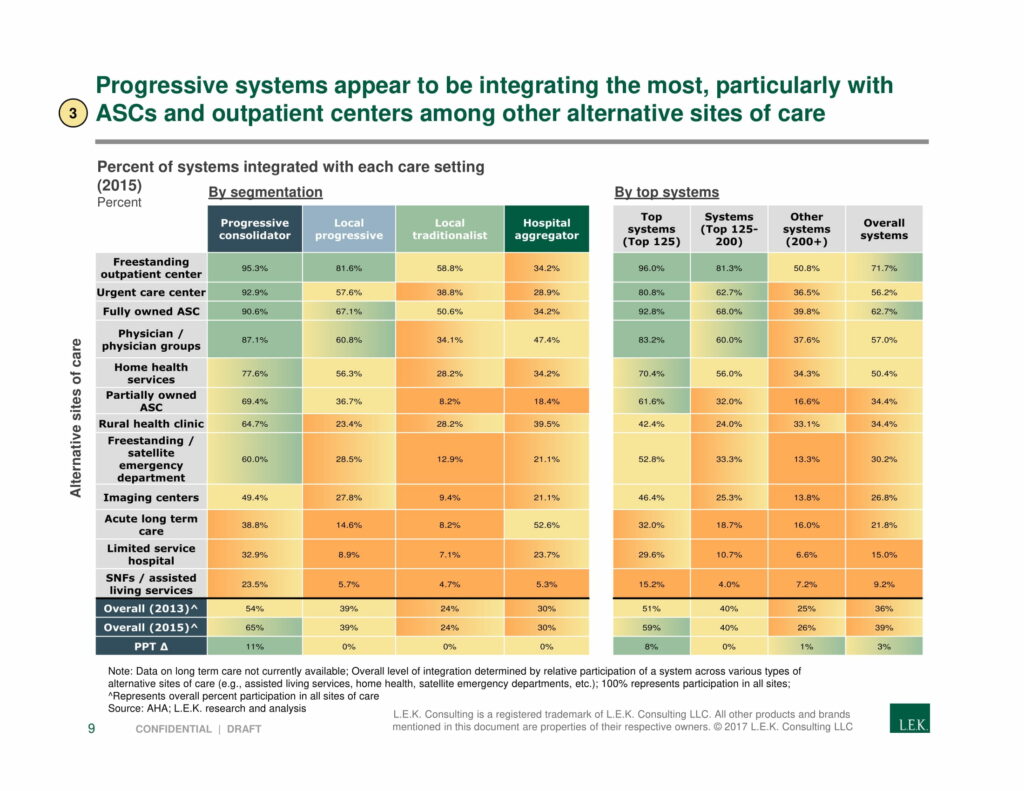
Many people argue that tables are not appropriate in slide decks. But that’s not quite right. Although they are often too dense to belong in the body of the slide, they fit quite well in an appendix.
Tables are a good way to summarize quantitative information. They are most commonly used to break down a calculation or show a complex quantitative output. Plus, you can turn your table into a heatmap by colorizing the cells based on their values.
You can check out more examples of tables and heatmaps in our slide library .
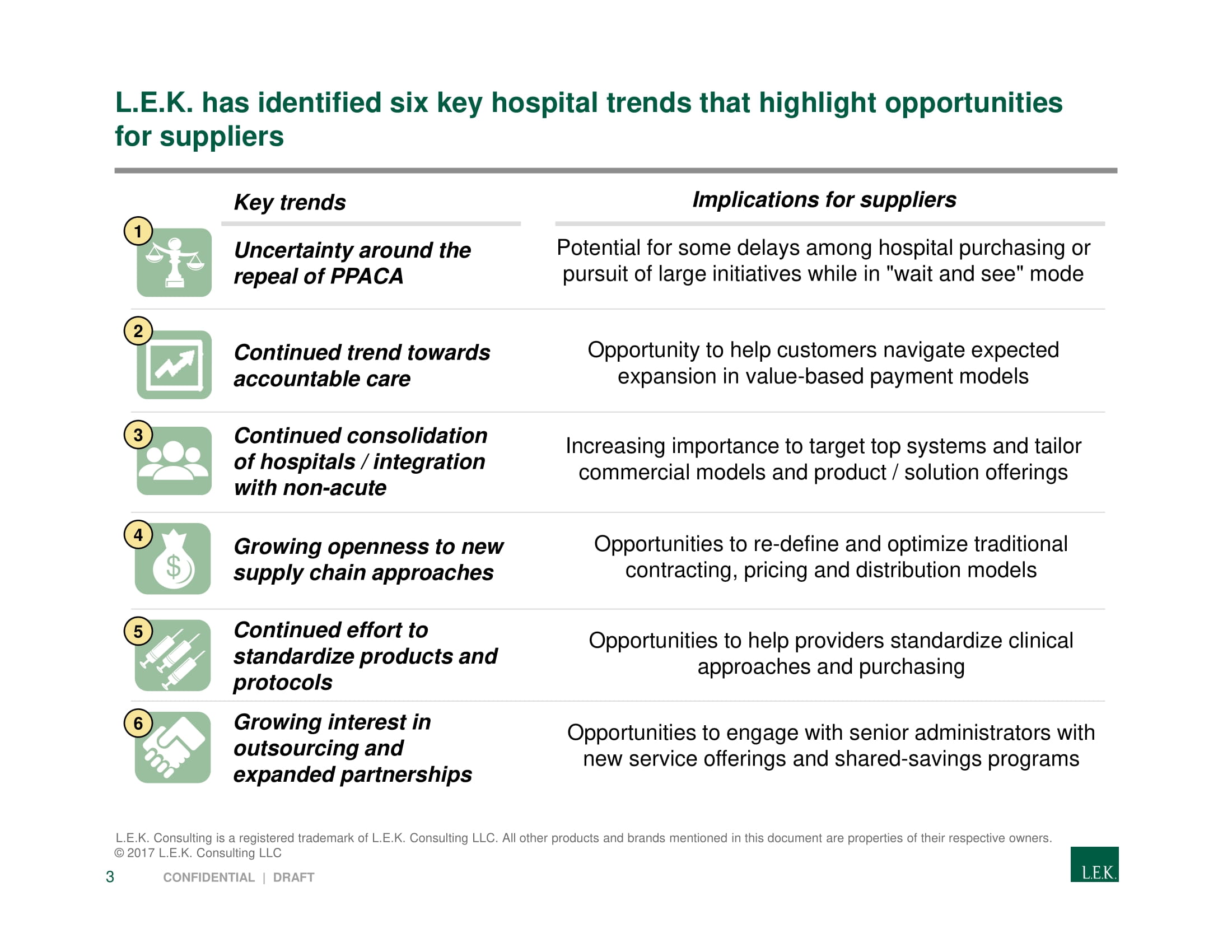
Text slides are simply slides with text on them. But not all text slides are made the same.
The thing that differentiates good text slides from bad text slides is structure. Good text slides are structured in a way that makes it easy for the reader to understand the dense text. So think about how you can break up your text into logical groupings or categories.
For example, in the L.E.K Consulting example above, they’ve categorized six key trends and structured their text into two groups: a description of the trend and the implication of the trend. They’ve also used icons to break up the text.
You can check out more examples of text slides in our slide library .
- Open access
- Published: 26 August 2024
Evaluating panel discussions in ESP classes: an exploration of international medical students’ and ESP instructors’ perspectives through qualitative research
- Elham Nasiri ORCID: orcid.org/0000-0002-0644-1646 1 &
- Laleh Khojasteh ORCID: orcid.org/0000-0002-6393-2759 1
BMC Medical Education volume 24 , Article number: 925 ( 2024 ) Cite this article
15 Accesses
Metrics details
This study investigates the effectiveness of panel discussions, a specific interactive teaching technique where a group of students leads a pre-planned, topic-focused discussion with audience participation, in English for Specific Purposes (ESP) courses for international medical students. This approach aims to simulate professional conference discussions, preparing students for future academic and clinical environments where such skills are crucial. While traditional group presentations foster critical thinking and communication, a gap exists in understanding how medical students perceive the complexities of preparing for and participating in panel discussions within an ESP setting. This qualitative study investigates the perceived advantages and disadvantages of these discussions from the perspectives of both panelists (medical students) and the audience (peers). Additionally, the study explores potential improvements based on insights from ESP instructors. Utilizing a two-phase design involving reflection papers and focus group discussions, data were collected from 46 medical students and three ESP instructors. Thematic analysis revealed that panel discussions offer unique benefits compared to traditional presentations, including enhanced engagement and more dynamic skill development for both panelists and the audience. Panelists reported gains in personal and professional development, including honing critical thinking, communication, and presentation skills. The audience perceived these discussions as engaging learning experiences that fostered critical analysis and information synthesis. However, challenges such as academic workload and concerns about discussion quality were also identified. The study concludes that panel discussions, when implemented effectively, can be a valuable tool for enhancing critical thinking, communication skills, and subject matter knowledge in ESP courses for medical students. These skills are transferable and can benefit students in various academic and professional settings, including future participation in medical conferences. This research provides valuable insights for ESP instructors seeking to integrate panel discussions into their curriculum, ultimately improving student learning outcomes and preparing them for future success in professional communication.
Peer Review reports
Introduction
In the field of medical education, the acquisition and application of effective communication skills are crucial for medical students in today’s global healthcare environment [ 1 ]. This necessitates not only strong English language proficiency but also the ability to present complex medical information clearly and concisely to diverse audiences.
Language courses, especially English for Specific Purposes (ESP) courses for medical students, are highly relevant in today’s globalized healthcare environment [ 2 ]. In non-English speaking countries like Iran, these courses are particularly important as they go beyond mere language instruction to include the development of critical thinking, cultural competence, and professional communication skills [ 3 ]. Proficiency in English is crucial for accessing up-to-date research, participating in international conferences, and communicating with patients and colleagues from diverse backgrounds [ 4 ]. Additionally, ESP courses help medical students understand and use medical terminologies accurately, which is essential for reading technical articles, listening to audio presentations, and giving spoken presentations [ 5 ]. In countries where English is not the primary language, ESP courses ensure that medical professionals can stay current with global advancements and collaborate effectively on an international scale [ 6 ]. Furthermore, these courses support students who may seek to practice medicine abroad, enhancing their career opportunities and professional growth [ 7 ].
Moreover, ESP courses enable medical professionals to communicate effectively with international patients, which is crucial in multicultural societies and for medical tourism, ensuring that patient care is not compromised due to language barriers [ 8 ]. Many medical textbooks, journals, and online resources are available primarily in English, and ESP courses equip medical students with the necessary language skills to access and comprehend these resources, ensuring they are well-informed about the latest medical research and practices [ 9 ].
Additionally, many medical professionals from non-English speaking countries aim to take international certification exams, such as the USMLE or PLAB, which are conducted in English, and ESP courses prepare students for these exams by familiarizing them with the medical terminology and language used in these assessments [ 10 ]. ESP courses also contribute to the professional development of medical students by improving their ability to write research papers, case reports, and other academic documents in English, which is essential for publishing in international journals and contributing to global medical knowledge [ 11 ]. In the increasingly interdisciplinary field of healthcare, collaboration with professionals from other countries is common, and ESP courses facilitate effective communication and collaboration with international colleagues, fostering innovation and the exchange of ideas [ 12 ].
With the rise of telemedicine and online medical consultations, proficiency in English is essential for non-English speaking medical professionals to provide remote healthcare services to international patients, and ESP courses prepare students for these modern medical practices [ 13 ].
Finally, ESP courses often include training on cultural competence, which is crucial for understanding and respecting the cultural backgrounds of patients and colleagues, leading to more empathetic and effective patient care and professional interactions [ 14 ]. Many ESP programs for medical students incorporate group presentations as a vital component of their curriculum, recognizing the positive impact on developing these essential skills [ 15 ].
Group projects in language courses, particularly in ESP for medical students, are highly relevant for several reasons. They provide a collaborative environment that mimics real-world professional settings, where healthcare professionals often work in multidisciplinary teams [ 16 ]. These group activities foster not only language skills but also crucial soft skills such as teamwork, leadership, and interpersonal communication, which are essential in medical practice [ 17 ].
The benefits of group projects over individual projects in language learning are significant. Hartono, Mujiyanto [ 18 ] found that group presentation tasks in ESP courses led to higher self-efficacy development compared to individual tasks. Group projects encourage peer learning, where students can learn from each other’s strengths and compensate for individual weaknesses [ 19 ]. They also provide a supportive environment that can reduce anxiety and increase willingness to communicate in the target language [ 20 ]. However, it is important to note that group projects also come with challenges, such as social loafing and unequal contribution, which need to be managed effectively [ 21 ].
Traditional lecture-based teaching methods, while valuable for knowledge acquisition, may not effectively prepare medical students for the interactive and collaborative nature of real-world healthcare settings [ 22 ]. Panel discussions (hereafter PDs), an interactive teaching technique where a group of students leads a pre-planned, topic-focused discussion with audience participation, are particularly relevant in this context. They simulate professional conference discussions and interdisciplinary team meetings, preparing students for future academic and clinical environments where such skills are crucial [ 23 ].
PDs, also known as moderated discussions or moderated panels, are a specific type of interactive format where a group of experts or stakeholders engage in a facilitated conversation on a particular topic or issue [ 22 ]. In this format, a moderator guides the discussion, encourages active participation from all panelists, and fosters a collaborative environment that promotes constructive dialogue and critical thinking [ 24 ]. The goal is to encourage audience engagement and participation, which can be achieved through various strategies such as asking open-ended questions, encouraging counterpoints and counterarguments, and providing opportunities for audience members to pose questions or share their own experiences [ 25 ]. These discussions can take place in-person or online, and can be designed to accommodate diverse audiences and settings [ 26 ].
In this study, PD is considered a speaking activity where medical students are assigned specific roles to play during the simulation, such as a physician, quality improvement specialist, policymaker, or patient advocate. By taking on these roles, students can gain a better understanding of the diverse perspectives and considerations that come into play in real-world healthcare discussions [ 23 ]. Simulating PDs within ESP courses can be a powerful tool for enhancing medical students’ learning outcomes in multiple areas. This approach improves language proficiency, academic skills, and critical thinking abilities, while also enabling students to communicate effectively with diverse stakeholders in the medical field [ 27 , 28 ].
Theoretical framework
The panel discussions in our study are grounded in the concept of authentic assessment (outlined by Villarroel, Bloxham [ 29 ]), which involves designing tasks that mirror real-life situations and problems. In the context of medical education, this approach is particularly relevant as it prepares students for the complex, multidisciplinary nature of healthcare communication. Realism can be achieved through two means: providing a realistic context that describes and delivers a frame for the problem to be solved and creating tasks that are similar to those faced in real and/or professional life [ 30 ]. In our study, the PDs provide a realistic context by simulating scenarios where medical students are required to discuss and present complex medical topics in a professional setting, mirroring the types of interactions they will encounter in their future careers.
The task of participating in PDs also involves cognitive challenge, as students are required to think critically about complex medical topics, analyze information, and communicate their findings effectively. This type of task aims to generate processes of problem-solving, application of knowledge, and decision-making that correspond to the development of cognitive and metacognitive skills [ 23 ]. For medical students, these skills are crucial in developing clinical reasoning and effective patient communication. The PDs encourage students to go beyond the textual reproduction of fragmented and low-order content and move towards understanding, establishing relationships between new ideas and previous knowledge, linking theoretical concepts with everyday experience, deriving conclusions from the analysis of data, and examining both the logic of the arguments present in the theory and its practical scope [ 24 , 25 , 27 ].
Furthermore, the evaluative judgment aspect of our study is critical in helping students develop criteria and standards about what a good performance means in medical communication. This involves students judging their own performance and regulating their own learning [ 31 ]. In the context of panel discussions, students reflect on their own work, compare it with desired standards, and seek feedback from peers and instructors. By doing so, students can develop a sense of what constitutes good performance in medical communication and what areas need improvement [ 32 ]. Boud, Lawson and Thompson [ 33 ] argue that students need to build a precise judgment about the quality of their work and calibrate these judgments in the light of evidence. This skill is particularly important for future medical professionals who will need to continually assess and improve their communication skills throughout their careers.
The theoretical framework presented above highlights the importance of authentic learning experiences in medical education. By drawing on the benefits of group work and panel discussions, university instructor-researchers aimed to provide medical students with a unique opportunity to engage with complex cases and develop their communication and collaboration skills. As noted by Suryanarayana [ 34 ], authentic learning experiences can lead to deeper learning and improved retention. Considering the advantages of group work in promoting collaborative problem-solving and language development, the instructor-researchers designed a panel discussion task that simulates real-world scenarios, where students can work together to analyze complex cases, share knowledge, and present their findings to a simulated audience.
While previous studies have highlighted the benefits of interactive learning experiences and critical thinking skills in medical education, a research gap remains in understanding how medical students perceive the relevance of PDs in ESP courses. This study aims to address this gap by investigating medical students’ perceptions of PD tasks in ESP courses and how these perceptions relate to their language proficiency, critical thinking skills, and ability to communicate effectively with diverse stakeholders in the medical field. This understanding can inform best practices in medical education, contributing to the development of more effective communication skills for future healthcare professionals worldwide [ 23 ]. The research questions guiding this study are:
What are the perceived advantages of PDs from the perspectives of panelists and the audience?
What are the perceived disadvantages of PDs from the perspectives of panelists and the audience?
How can PDs be improved for panelists and the audience based on the insights of ESP instructors?
Methodology
Aim and design.
For this study, a two-phase qualitative design was employed to gain an understanding of the advantages and disadvantages of PDs from the perspectives of both student panelists and the audience (Phase 1) and to acquire an in-depth understanding of the suggested strategies provided by experts to enhance PPs for future students (Phase 2).
Participants and context of the study
This study was conducted in two phases (Fig. 1 ) at Shiraz University of Medical Sciences (SUMS), Shiraz, Iran.
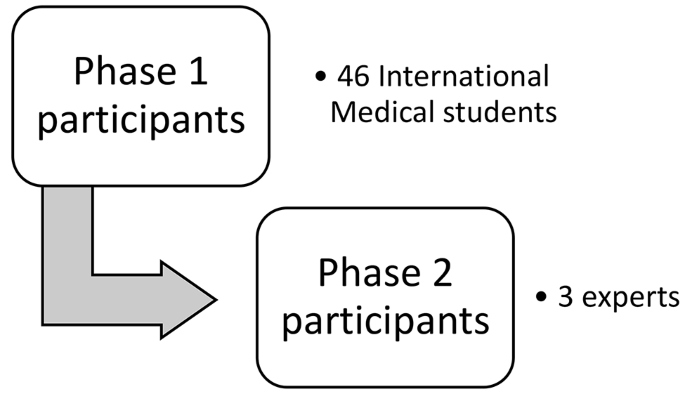
Participants of the study in two phases
In the first phase, the student participants were 46 non-native speakers of English and international students who studied medicine at SUMS. Their demographic characteristics can be seen in Table 1 .
These students were purposefully selected because they were the only SUMS international students who had taken the ESP (English for Specific Purposes) course. The number of international students attending SUMS is indeed limited. Each year, a different batch of international students joins the university. They progress through a sequence of English courses, starting with General English 1 and 2, followed by the ESP course, and concluding with academic writing. At the time of data collection, the students included in the study were the only international students enrolled in the ESP course. This mandatory 3-unit course is designed to enhance their language and communication skills specifically tailored to their profession. As a part of the Medicine major curriculum, this course aims to improve their English language proficiency in areas relevant to medicine, such as understanding medical terminology, comprehending original medicine texts, discussing clinical cases, and communicating with patients, colleagues, and other healthcare professionals.
Throughout the course, students engage in various interactive activities, such as group discussions, role-playing exercises, and case studies, to develop their practical communication skills. In this course, medical students receive four marks out of 20 for their oral presentations, while the remaining marks are allocated to their written midterm and final exams. From the beginning of the course, they are briefed about PDs, and they are shown two YouTube-downloaded videos about PDs at medical conferences, a popular format for discussing and sharing knowledge, research findings, and expert opinions on various medical topics.
For the second phase of the study, a specific group of participants was purposefully selected. This group consisted of three faculty members from SUMS English department who had extensive experience attending numerous conferences at national and international levels, particularly in the medical field, as well as working as translators and interpreters in medical congresses. Over the course of ten years, they also gained considerable experience in PDs. They were invited to discuss strategies helpful for medical students with PDs.
Panel discussion activity design and implementation
When preparing for a PD session, medical students received comprehensive guidance on understanding the roles and responsibilities of each panel member. This guidance was aimed at ensuring that each participant was well-prepared and understood their specific role in the discussion.
Moderators should play a crucial role in steering the conversation. They are responsible for ensuring that all panelists have an opportunity to contribute and that the audience is engaged effectively. Specific tasks include preparing opening remarks, introducing panelists, and crafting transition questions to facilitate smooth topic transitions. The moderators should also manage the time to ensure balanced participation and encourage active audience involvement.
Panelists are expected to be subject matter experts who bring valuable insights and opinions to the discussion. They are advised to conduct thorough research on the topic and prepare concise talking points. Panelists are encouraged to draw from their medical knowledge and relevant experiences, share evidence-based information, and engage with other panelists’ points through active listening and thoughtful responses.
The audience plays an active role in the PDs. They are encouraged to participate by asking questions, sharing relevant experiences, and contributing to the dialogue. To facilitate this, students are advised to take notes during the discussion and think of questions or comments they can contribute during the Q&A segment.
For this special course, medical students were advised to choose topics either from their ESP textbook or consider current medical trends, emerging research, and pressing issues in their field. Examples included breast cancer, COVID-19, and controversies in gene therapy. The selection process involved brainstorming sessions and consultation with the course instructor to ensure relevance and appropriateness.
To accommodate the PD sessions within the course structure, students were allowed to start their PD sessions voluntarily from the second week. However, to maintain a balance between peer-led discussions and regular course content, only one PD was held weekly. This approach enabled the ESP lecturer to deliver comprehensive content while also allowing students to engage in these interactive sessions.
A basic time structure was suggested for each PD (Fig. 2 ):
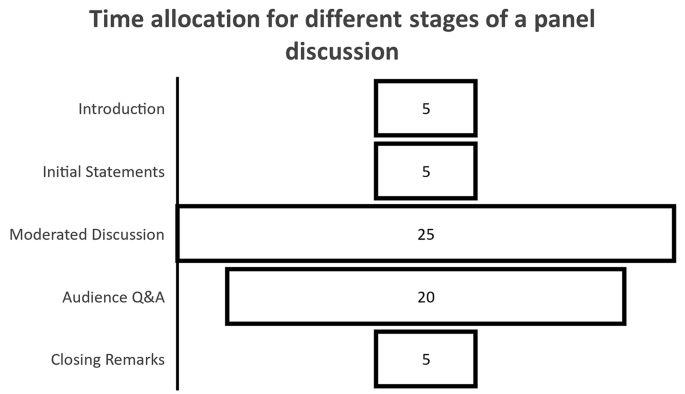
Time allocation for panel discussion stages in minutes
To ensure the smooth running of the course and maintain momentum, students were informed that they could cancel their PD session only once. In such cases, they were required to notify the lecturer and other students via the class Telegram channel to facilitate rescheduling and minimize disruptions. This provision was essential in promoting a sense of community among students and maintaining the course’s continuity.
Research tools and data collection
The study utilized various tools to gather and analyze data from participants and experts, ensuring a comprehensive understanding of the research topic.
Reflection papers
In Phase 1 of the study, 46 medical students detailed their perceptions of the advantages and disadvantages of panel discussions from dual perspectives: as panelists (presenters) and as audience members (peers).
Participants were given clear instructions and a 45-minute time frame to complete the reflection task. With approximately 80% of the international language students being native English speakers and the rest fluent in English, the researchers deemed this time allocation reasonable. The questions and instructions were straightforward, facilitating quick comprehension. It was estimated that native English speakers would need about 30 min to complete the task, while non-native speakers might require an extra 15 min for clarity and expression. This time frame aimed to allow students to respond thoughtfully without feeling rushed. Additionally, students could request more time if needed.
Focus group discussion
In phase 2 of the study, a focus group discussion was conducted with three expert participants. The purpose of the focus group was to gather insights from expert participants, specifically ESP (English for Specific Purposes) instructors, on how presentation dynamics can be improved for both panelists and the audience.
According to Colton and Covert [ 35 ], focus groups are useful for obtaining detailed input from experts. The appropriate size of a focus group is determined by the study’s scope and available resources [ 36 ]. Morgan [ 37 ] suggests that small focus groups are suitable for complex topics where specialist participants might feel frustrated if not allowed to express themselves fully.
The choice of a focus group over individual interviews was based on several factors. First, the exploratory nature of the study made focus groups ideal for interactive discussions, generating new ideas and in-depth insights [ 36 ]. Second, while focus groups usually involve larger groups, they can effectively accommodate a limited number of experts with extensive knowledge [ 37 ]. Third, the focus group format fostered a more open environment for idea exchange, allowing participants to engage dynamically [ 36 ]. Lastly, conducting a focus group was more time- and resource-efficient than scheduling three separate interviews [ 36 ].
Data analysis
The first phase of the study involved a thorough examination of the data related to the research inquiries using thematic analysis. This method was chosen for its effectiveness in uncovering latent patterns from a bottom-up perspective, facilitating a comprehensive understanding of complex educational phenomena [ 38 ]. The researchers first familiarized themselves with the data by repeatedly reviewing the reflection papers written by the medical students. Next, an initial round of coding was independently conducted to identify significant data segments and generate preliminary codes that reflected the students’ perceptions of the advantages and disadvantages of presentation dynamics PDs from both the presenter and audience viewpoints [ 38 ].
The analysis of the reflection papers began with the two researchers coding a subset of five papers independently, adhering to a structured qualitative coding protocol [ 39 ]. They convened afterward to compare their initial codes and address any discrepancies. Through discussion, they reached an agreement on the codes, which were then analyzed, organized into categories and themes, and the frequency of each code was recorded [ 38 ].
After coding the initial five papers, the researchers continued to code the remaining 41 reflection paper transcripts in batches of ten, meeting after each batch to review their coding, resolve any inconsistencies, and refine the coding framework as needed. This iterative process, characterized by independent coding, joint reviews, and consensus-building, helped the researchers establish a robust and reliable coding approach consistently applied to the complete dataset [ 40 ]. Once all 46 reflection paper transcripts were coded, the researchers conducted a final review and discussion to ensure accurate analysis. They extracted relevant excerpts corresponding to the identified themes and sub-themes from the transcripts to provide detailed explanations and support for their findings [ 38 ]. This multi-step approach of separate initial coding, collaborative review, and frequency analysis enhanced the credibility and transparency of the qualitative data analysis.
To ensure the trustworthiness of the data collected in this study, the researchers adhered to the Guba and Lincoln standards of scientific accuracy in qualitative research, which encompass credibility, confirmability, dependability, and transferability [ 41 ] (Table 2 ).
The analysis of the focus group data obtained from experts followed the same rigorous procedure applied to the student participants’ data. Thematic analysis was employed to examine the experts’ perspectives, maintaining consistency in the analytical approach across both phases of the study. The researchers familiarized themselves with the focus group transcript, conducted independent preliminary coding, and then collaboratively refined the codes. These codes were subsequently organized into categories and themes, with the frequency of each code recorded. The researchers engaged in thorough discussions to ensure agreement on the final themes and sub-themes. Relevant excerpts from the focus group transcript were extracted to provide rich, detailed explanations of each theme, thereby ensuring a comprehensive and accurate analysis of the experts’ insights.
1. What are the advantages of PDs from the perspective of panelists and the audience?
The analysis of the advantages of PDs from the perspectives of both panelists and audience members revealed several key themes and categories. Tables 2 and 3 present the frequency and percentage of responses for each code within these categories.
From the panelists’ perspective (Table 3 ), the overarching theme was “Personal and Professional Development.” The most frequently reported advantage was knowledge sharing (93.5%), followed closely by increased confidence (91.3%) and the importance of interaction in presentations (91.3%).
Notably, all categories within this theme had at least one code mentioned by over 80% of participants, indicating a broad range of perceived benefits. The category of “Effective teamwork and communication” was particularly prominent, with collaboration (89.1%) and knowledge sharing (93.5%) being among the most frequently cited advantages. This suggests that PDs are perceived as valuable tools for fostering interpersonal skills and collective learning. In the “Language mastery” category, increased confidence (91.3%) and better retention of key concepts (87.0%) were highlighted, indicating that PDs are seen as effective for both language and content learning.
The audience perspective (Table 4 ), encapsulated under the theme “Enriching Learning Experience,” showed similarly high frequencies across all categories.
The most frequently mentioned advantage was exposure to diverse speakers (93.5%), closely followed by the range of topics covered (91.3%) and increased audience interest (91.3%). The “Broadening perspectives” category was particularly rich, with all codes mentioned by over 70% of participants. This suggests that audience members perceive PDs as valuable opportunities for expanding their knowledge and viewpoints. In the “Language practice” category, the opportunity to practice language skills (89.1%) was the most frequently cited advantage, indicating that even as audience members, students perceive significant language learning benefits.
Comparing the two perspectives reveals several interesting patterns:
High overall engagement: Both panelists and audience members reported high frequencies across all categories, suggesting that PDs are perceived as beneficial regardless of the role played.
Language benefits: While panelists emphasized increased confidence (91.3%) and better retention of concepts (87.0%), audience members highlighted opportunities for language practice (89.1%). This indicates that PDs offer complementary language learning benefits for both roles.
Interactive learning: The importance of interaction was highly rated by panelists (91.3%), while increased audience interest was similarly valued by the audience (91.3%). This suggests that PDs are perceived as an engaging, interactive learning method from both perspectives.
Professional development: Panelists uniquely emphasized professional growth aspects such as experiential learning (84.8%) and real-world application (80.4%). These were not directly mirrored in the audience perspective, suggesting that active participation in PDs may offer additional professional development benefits.
Broadening horizons: Both groups highly valued the diversity aspect of PDs. Panelists appreciated diversity and open-mindedness (80.4%), while audience members valued diverse speakers (93.5%) and a range of topics (91.3%).
2. What are the disadvantages of PDs from the perspective of panelists and the audience?
The analysis of the disadvantages of panel discussions (PDs) from the perspectives of both panelists and audience members revealed several key themes and categories. Tables 4 and 5 present the frequency and percentage of responses for each code within these categories.
From the panelists’ perspective (Table 5 ), the theme “Drawbacks of PDs” was divided into two main categories: “Academic Workload Challenges” and “Coordination Challenges.” The most frequently reported disadvantage was long preparation (87.0%), followed by significant practice needed (82.6%) and the time-consuming nature of PDs (80.4%). These findings suggest that the primary concern for panelists is the additional workload that PDs impose on their already demanding academic schedules. The “Coordination Challenges” category, while less prominent than workload issues, still presented significant concerns. Diverse panel skills (78.3%) and finding suitable panelists (73.9%) were the most frequently cited issues in this category, indicating that team dynamics and composition are notable challenges for panelists.
The audience perspective (Table 6 ), encapsulated under the theme “Drawbacks of PDs,” was divided into two main categories: “Time-related Issues” and “Interaction and Engagement Issues.” In the “Time-related Issues” category, the most frequently mentioned disadvantage was the inefficient use of time (65.2%), followed by the perception of PDs as too long and boring (60.9%). Notably, 56.5% of respondents found PDs stressful due to overwhelming workload from other studies, and 52.2% considered them not very useful during exam time. The “Interaction and Engagement Issues” category revealed more diverse concerns. The most frequently mentioned disadvantage was the repetitive format (82.6%), followed by limited engagement with the audience (78.3%) and the perception of PDs as boring (73.9%). The audience also noted issues related to the panelists’ preparation and coordination, such as “Not practiced and natural” (67.4%) and “Coordination and Interaction Issues” (71.7%), suggesting that the challenges faced by panelists directly impact the audience’s experience.
Workload concerns: Both panelists and audience members highlighted time-related issues. For panelists, this manifested as long preparation times (87.0%) and difficulty balancing with other studies (76.1%). For the audience, it appeared as perceptions of inefficient use of time (65.2%) and stress due to overwhelming workload from other studies (56.5%).
Engagement issues: While panelists focused on preparation and coordination challenges, the audience emphasized the quality of the discussion and engagement. This suggests a potential mismatch between the efforts of panelists and the expectations of the audience.
Boredom and repetition: The audience frequently mentioned boredom (73.9%) and repetitive format (82.6%) as issues, which weren’t directly mirrored in the panelists’ responses. This indicates that while panelists may be focused on content preparation, the audience is more concerned with the delivery and variety of the presentation format.
Coordination challenges: Both groups noted coordination issues, but from different perspectives. Panelists struggled with team dynamics and finding suitable co-presenters, while the audience observed these challenges manifesting as unnatural or unpracticed presentations.
Academic pressure: Both groups acknowledged the strain PDs put on their academic lives, with panelists viewing it as a burden (65.2%) and the audience finding it less useful during exam times (52.2%).
3. How can PDs be improved for panelists and the audience from the experts’ point of view?
The presentation of data for this research question differs from the previous two due to the unique nature of the information gathered. Unlike the quantifiable student responses in earlier questions, this data stems from expert opinions and a reflection discussion session, focusing on qualitative recommendations for improvement rather than frequency of responses (Braun & Clarke, 2006). The complexity and interconnectedness of expert suggestions, coupled with the integration of supporting literature, necessitate a more narrative approach (Creswell & Poth, 2018). This format allows for a richer exploration of the context behind each recommendation and its potential implications (Patton, 2015). Furthermore, the exploratory nature of this question, aimed at generating ideas for improvement rather than measuring prevalence of opinions, is better served by a detailed, descriptive presentation (Merriam & Tisdell, 2016). This approach enables a more nuanced understanding of how PDs can be enhanced, aligning closely with the “how” nature of the research question and providing valuable insights for potential implementation (Yin, 2018).
The experts provided several suggestions to address the challenges faced by students in panel discussions (PDs) and improve the experience for both panelists and the audience. Their recommendations focused on six key areas: time management and workload, preparation and skill development, engagement and interactivity, technological integration, collaboration and communication, and institutional support.
To address the issue of time management and heavy workload, one expert suggested teaching students to “ break down the task to tackle the time-consuming nature of panel discussions and balance it with other studies .” This approach aims to help students manage the extensive preparation time required for PDs without compromising their other academic responsibilities. Another expert emphasized “ enhancing medical students’ abilities to prioritize tasks , allocate resources efficiently , and optimize their workflow to achieve their goals effectively .” These skills were seen as crucial not only for PD preparation but also for overall academic success and future professional practice.
Recognizing the challenges of long preparation times and the perception of PDs being burdensome, an expert proposed “ the implementation of interactive training sessions for panelists .” These sessions were suggested to enhance coordination skills and improve the ability of group presenters to engage with the audience effectively. The expert emphasized that such training could help students view PDs as valuable learning experiences rather than additional burdens, potentially increasing their motivation and engagement in the process.
To combat issues of limited engagement and perceived boredom, experts recommended increasing engagement opportunities for the audience through interactive elements like audience participation and group discussions. They suggested that this could transform PDs from passive listening experiences to active learning opportunities. One expert suggested “ optimizing time management and restructuring the format of panel discussions ” to address inefficiency during sessions. This restructuring could involve shorter presentation segments interspersed with interactive elements to maintain audience attention and engagement.
An innovative solution proposed by one expert was “ using ChatGPT to prepare for PDs by streamlining scenario presentation preparation and role allocation. ” The experts collectively discussed the potential of AI to assist medical students in reducing their workload and saving time in preparing scenario presentations and allocating roles in panel discussions. They noted that AI could help generate initial content drafts, suggest role distributions based on individual strengths, and even provide practice questions for panelists, significantly reducing preparation time while maintaining quality.
Two experts emphasized the importance of enhancing collaboration and communication among panelists to address issues related to diverse panel skills and coordination challenges. They suggested establishing clear communication channels and guidelines to improve coordination and ensure a cohesive presentation. This could involve creating structured team roles, setting clear expectations for each panelist, and implementing regular check-ins during the preparation process to ensure all team members are aligned and progressing.
All experts were in agreement that improving PDs would not be possible “ if nothing is done by the university administration to reduce the ESP class size for international students .” They believed that large class sizes in ESP or EFL classes could negatively influence group oral presentations, hindering language development and leading to uneven participation. The experts suggested that smaller class sizes would allow for more individualized attention, increased speaking opportunities for each student, and more effective feedback mechanisms, all of which are crucial for developing strong presentation skills in a second language.
Research question 1: what are the advantages of PDs from the perspective of panelists and the audience?
The results of this study reveal significant advantages of PDs for both panelists and audience members in the context of medical education. These findings align with and expand upon previous research in the field of educational presentations and language learning.
Personal and professional development for panelists
The high frequency of reported benefits in the “Personal and Professional Development” theme for panelists aligns with several previous studies. The emphasis on language mastery, particularly increased confidence (91.3%) and better retention of key concepts (87.0%), supports the findings of Hartono, Mujiyanto [ 42 ], Gedamu and Gezahegn [ 15 ], Li [ 43 ], who all highlighted the importance of language practice in English oral presentations. However, our results show a more comprehensive range of benefits, including professional growth aspects like experiential learning (84.8%) and real-world application (80.4%), which were not as prominently featured in these earlier studies.
Interestingly, our findings partially contrast with Chou [ 44 ] study, which found that while group oral presentations had the greatest influence on improving students’ speaking ability, individual presentations led to more frequent use of metacognitive, retrieval, and rehearsal strategies. Our results suggest that PDs, despite being group activities, still provide significant benefits in these areas, possibly due to the collaborative nature of preparation and the individual responsibility each panelist bears. The high frequency of knowledge sharing (93.5%) and collaboration (89.1%) in our study supports Harris, Jones and Huffman [ 45 ] emphasis on the importance of group dynamics and varied perspectives in educational settings. However, our study provides more quantitative evidence for these benefits in the specific context of PDs.
Enriching learning experience for the audience
The audience perspective in our study reveals a rich learning experience, with high frequencies across all categories. This aligns with Agustina [ 46 ] findings in business English classes, where presentations led to improvements in all four language skills. However, our study extends these findings by demonstrating that even passive participation as an audience member can lead to significant perceived benefits in language practice (89.1%) and broadening perspectives (93.5% for diverse speakers). The high value placed on diverse speakers (93.5%) and range of topics (91.3%) by the audience supports the notion of PDs as a tool for expanding knowledge and viewpoints. This aligns with the concept of situated learning experiences leading to deeper understanding in EFL classes, as suggested by Li [ 43 ] and others [ 18 , 31 ]. However, our study provides more specific evidence for how this occurs in the context of PDs.
Interactive learning and engagement
Both panelists and audience members in our study highly valued the interactive aspects of PDs, with the importance of interaction rated at 91.3% by panelists and increased audience interest at 91.3% by the audience. This strong emphasis on interactivity aligns with Azizi and Farid Khafaga [ 19 ] study on the benefits of dynamic assessment and dialogic learning contexts. However, our study provides more detailed insights into how this interactivity is perceived and valued by both presenters and audience members in PDs.
Professional growth and real-world application
The emphasis on professional growth through PDs, particularly for panelists, supports Li’s [ 43 ] assertion about the power of oral presentations as situated learning experiences. Our findings provide more specific evidence for how PDs contribute to professional development, with high frequencies reported for experiential learning (84.8%) and real-world application (80.4%). This suggests that PDs may be particularly effective in bridging the gap between academic learning and professional practice in medical education.
Research question 2: what are the disadvantages of pds from the perspective of panelists and the audience?
Academic workload challenges for panelists.
The high frequency of reported challenges in the “Academic Workload Challenges” category for panelists aligns with several previous studies in medical education [ 47 , 48 , 49 ]. The emphasis on long preparation (87.0%), significant practice needed (82.6%), and the time-consuming nature of PDs (80.4%) supports the findings of Johnson et al. [ 24 ], who noted that while learners appreciate debate-style journal clubs in health professional education, they require additional time commitment. This is further corroborated by Nowak, Speed and Vuk [ 50 ], who found that intensive learning activities in medical education, while beneficial, can be time-consuming for students.
Perceived value of pds relative to time investment
While a significant portion of the audience (65.2%) perceived PDs as an inefficient use of time, the high frequency of engagement-related concerns (82.6% for repetitive format, 78.3% for limited engagement) suggests that the perceived lack of value may be more closely tied to the quality of the experience rather than just the time investment. This aligns with Dyhrberg O’Neill [ 27 ] findings on debate-based oral exams, where students perceived value despite the time-intensive nature of the activity. However, our results indicate a more pronounced concern about the return on time investment in PDs. This discrepancy might be addressed through innovative approaches to PD design and implementation, such as those proposed by Almazyad et al. [ 22 ], who suggested using AI tools to enhance expert panel discussions and potentially improve efficiency.
Coordination challenges for panelists
The challenges related to coordination in medical education, such as diverse panel skills (78.3%) and finding suitable panelists (73.9%), align with previous research on teamwork in higher education [ 21 ]. Our findings support the concept of the free-rider effect discussed by Hall and Buzwell [ 21 ], who explored reasons for non-contribution in group projects beyond social loafing. This is further elaborated by Mehmood, Memon and Ali [ 51 ], who proposed that individuals may not contribute their fair share due to various factors including poor communication skills or language barriers, which is particularly relevant in medical education where clear communication is crucial [ 52 ]. Comparing our results to other collaborative learning contexts in medical education, Rodríguez-Sedano, Conde and Fernández-Llamas [ 53 ] measured teamwork competence development in a multidisciplinary project-based learning environment. They found that while teamwork skills improved over time, initial coordination challenges were significant. This aligns with our findings on the difficulties of coordinating diverse panel skills and opinions in medical education settings.
Our results also resonate with Chou’s [ 44 ] study comparing group and individual oral presentations, which found that group presenters often had a limited understanding of the overall content. This is supported by Wilson, Ho and Brookes [ 54 ], who examined student perceptions of teamwork in undergraduate science degrees, highlighting the challenges and benefits of collaborative work, which are equally applicable in medical education [ 52 ].
Quality of discussions and perception for the audience
The audience perspective in our study reveals significant concerns about the quality and engagement of PDs in medical education. The high frequency of issues such as repetitive format (82.6%) and limited engagement with the audience (78.3%) aligns with Parmar and Bickmore [ 55 ] findings on the importance of addressing individual audience members and gathering feedback. This is further supported by Nurakhir et al. [ 25 ], who explored students’ views on classroom debates as a strategy to enhance critical thinking and oral communication skills in nursing education, which shares similarities with medical education. Comparing our results to other interactive learning methods in medical education, Jones et al. [ 26 ] reviewed the use of journal clubs and book clubs in pharmacy education. They found that while these methods enhanced engagement, they also faced challenges in maintaining student interest over time, similar to the boredom issues reported in our study of PDs in medical education. The perception of PDs as boring (73.9%) and not very useful during exam time (52.2%) supports previous research on the stress and pressure experienced by medical students [ 48 , 49 ]. Grieve et al. [ 20 ] specifically examined student fears of oral presentations and public speaking in higher education, which provides context for the anxiety and disengagement observed in our study of medical education. Interestingly, Bhuvaneshwari et al. [ 23 ] found positive impacts of panel discussions in educating medical students on specific modules. This contrasts with our findings and suggests that the effectiveness of PDs in medical education may vary depending on the specific context and implementation.
Comparative analysis and future directions
Our study provides a unique comparative analysis of the challenges faced by both panelists and audience members in medical education. The alignment of concerns around workload and time management between the two groups suggests that these are overarching issues in the implementation of PDs in medical curricula. This is consistent with the findings of Pasandín et al. [ 56 ], who examined cooperative oral presentations in higher education and their impact on both technical and soft skills, which are crucial in medical education [ 52 ]. The mismatch between panelist efforts and audience expectations revealed in our study is a novel finding that warrants further investigation in medical education. This disparity could be related to the self-efficacy beliefs of presenters, as explored by Gedamu and Gezahegn [ 15 ] in their study of TEFL trainees’ attitudes towards academic oral presentations, which may have parallels in medical education. Looking forward, innovative approaches could address some of the challenges identified in medical education. Almazyad et al. [ 22 ] proposed using AI tools like ChatGPT to enhance expert panel discussions in pediatric palliative care, which could potentially address some of the preparation and engagement issues identified in our study of medical education. Additionally, Ragupathi and Lee [ 57 ] discussed the role of rubrics in higher education, which could provide clearer expectations and feedback for both panelists and audience members in PDs within medical education.
Research question 3: how can PDs be improved for panelists and the audience from the experts’ point of view?
The expert suggestions for improving PDs address several key challenges identified in previous research on academic presentations and student workload management. These recommendations align with current trends in educational technology and pedagogical approaches, while also considering the unique needs of medical students.
The emphasis on time management and workload reduction strategies echoes findings from previous studies on medical student stress and academic performance. Nowak, Speed and Vuk [ 50 ] found that medical students often struggle with the fast-paced nature of their courses, which can lead to reduced motivation and superficial learning approaches. The experts’ suggestions for task breakdown and prioritization align with Rabbi and Islam [ 58 ] recommendations for reducing workload stress through effective assignment prioritization. Additionally, Popa et al. [ 59 ] highlight the importance of acceptance and planning in stress management for medical students, supporting the experts’ focus on these areas.
The proposed implementation of interactive training sessions for panelists addresses the need for enhanced presentation skills in professional contexts, a concern highlighted by several researchers [ 17 , 60 ]. This aligns with Grieve et al. [ 20 ] findings on student fears of oral presentations and public speaking in higher education, emphasizing the need for targeted training. The focus on interactive elements and audience engagement also reflects current trends in active learning pedagogies, as demonstrated by Pasandín et al. [ 56 ] in their study on cooperative oral presentations in engineering education.
The innovative suggestion to use AI tools like ChatGPT for PD preparation represents a novel approach to leveraging technology in education. This aligns with recent research on the potential of AI in scientific research, such as the study by Almazyad et al. [ 22 ], which highlighted the benefits of AI in supporting various educational tasks. However, it is important to consider potential ethical implications and ensure that AI use complements rather than replaces critical thinking and creativity.
The experts’ emphasis on enhancing collaboration and communication among panelists addresses issues identified in previous research on teamwork in higher education. Rodríguez-Sedano, Conde and Fernández-Llamas [ 53 ] noted the importance of measuring teamwork competence development in project-based learning environments. The suggested strategies for improving coordination align with best practices in collaborative learning, as demonstrated by Romero-Yesa et al. [ 61 ] in their qualitative assessment of challenge-based learning and teamwork in electronics programs.
The unanimous agreement on the need to reduce ESP class sizes for international students reflects ongoing concerns about the impact of large classes on language learning and student engagement. This aligns with research by Li [ 3 ] on issues in developing EFL learners’ oral English communication skills. Bosco et al. [ 62 ] further highlight the challenges of teaching and learning ESP in mixed classes, supporting the experts’ recommendation for smaller class sizes. Qiao, Xu and bin Ahmad [ 63 ] also emphasize the implementation challenges for ESP formative assessment in large classes, further justifying the need for reduced class sizes.
These expert recommendations provide a comprehensive approach to improving PDs, addressing not only the immediate challenges of preparation and delivery but also broader issues of student engagement, workload management, and institutional support. By implementing these suggestions, universities could potentially transform PDs from perceived burdens into valuable learning experiences that enhance both academic and professional skills. This aligns with Kho and Ting [ 64 ] systematic review on overcoming oral presentation anxiety among tertiary ESL/EFL students, which emphasizes the importance of addressing both challenges and strategies in improving presentation skills.
This study has shed light on the complex challenges associated with PDs in medical education, revealing a nuanced interplay between the experiences of panelists and audience members. The findings underscore the need for a holistic approach to implementing PDs that addresses both the academic workload concerns and the quality of engagement.
Our findings both support and extend previous research on the challenges of oral presentations and group work in medical education settings. The high frequencies of perceived challenges across multiple categories for both panelists and audience members suggest that while PDs may offer benefits, they also present significant obstacles that need to be addressed in medical education. These results highlight the need for careful consideration in the implementation of PDs in medical education, with particular attention to workload management, coordination strategies, and audience engagement techniques. Future research could focus on developing and testing interventions to mitigate these challenges while preserving the potential benefits of PDs in medical education.
Moving forward, medical educators should consider innovative approaches to mitigate these challenges. This may include:
Integrating time management and stress coping strategies into the PD preparation process [ 59 ].
Exploring the use of AI tools to streamline preparation and enhance engagement [ 22 ].
Developing clear rubrics and expectations for both panelists and audience members [ 57 ].
Incorporating interactive elements to maintain audience interest and participation [ 25 ].
Limitations and future research
One limitation of this study is that it focused on a specific population of medical students, which may limit the generalizability of the findings to other student populations. Additionally, the study relied on self-report data from panelists and audience members, which may introduce bias and affect the validity of the results. Future research could explore the effectiveness of PDs in different educational contexts and student populations to provide a more comprehensive understanding of the benefits and challenges of panel discussions.
Future research should focus on evaluating the effectiveness of these interventions and exploring how PDs can be tailored to the unique demands of medical education. By addressing the identified challenges, PDs have the potential to become a more valuable and engaging component of medical curricula, fostering both academic and professional development. Ultimately, the goal should be to transform PDs from perceived burdens into opportunities for meaningful learning and skill development, aligning with the evolving needs of medical education in the 21st century.
Future research could also examine the long-term impact of PDs on panelists’ language skills, teamwork, and communication abilities. Additionally, exploring the effectiveness of different training methods and tools, such as AI technology, in improving coordination skills and reducing workload stress for panelists could provide valuable insights for educators and administrators. Further research could also investigate the role of class size and audience engagement in enhancing the overall effectiveness of PDs in higher education settings. By addressing these gaps in the literature, future research can contribute to the ongoing development and improvement of PDs as a valuable learning tool for students in higher education.
However, it is important to note that implementing these changes may require significant institutional resources and a shift in pedagogical approaches. Future research could focus on piloting these recommendations and evaluating their effectiveness in improving student outcomes and experiences with PDs.
Data availability
We confirm that the data supporting the findings are available within this article. Raw data supporting this study’s findings are available from the corresponding author, upon request.
Abbreviations
Artificial Intelligence
English as a Foreign Language
English for Specific Purposes
Panel Discussion
Shiraz University of Medical Sciences
Harden RM, Laidlaw JM. Essential skills for a medical teacher: an introduction to teaching and learning in medicine. Elsevier Health Sciences; 2020.
Ibrahim Mohamed O, Al Jadaan DO. English for Specific purposes (Esp) Needs Analysis for Health Sciences students: a cross-sectional study at a University in the UAE. English for Specific purposes (Esp) Needs Analysis for Health Sciences Students: A Cross-Sectional Study at a University in the UAE.
Li Y, Heron M. English for general academic purposes or English for specific purposes? Language learning needs of medical students at a Chinese university. Theory Pract Lang Stud. 2021;11(6):621–31.
Article Google Scholar
Chan SMH, Mamat NH, Nadarajah VD. Mind your language: the importance of English language skills in an International Medical Programme (IMP). BMC Med Educ. 2022;22(1):405.
Cortez Faustino BS, Ticas de Córdova CK, de la Hernández DI. Teaching English for specific purposes: contents and methodologies that could be implemented in the English for Medical purposes (EMP) course for the doctor of Medicine Major at the University of El Salvador. Universidad de El Salvador; 2022.
BENYAMINA E-Z BOUKAHLAH. Enhancing Specialty Language learning through content-based instruction: students of Paramedical Institute of Tiaret as a case study. Université IBN KHALDOUN-Tiaret; 2023.
Prikazchikov M. Medical English course for russian-speaking dentists: a needs analysis study. Iowa State University; 2024.
Kim C, Lee SY, Park S-H. Is Korea Ready to be a key player in the Medical Tourism Industry? An English Education Perspective. Iran J Public Health. 2020;49(2):267–73.
Google Scholar
Syakur A, Zainuddin H, Hasan MA. Needs analysis English for specific purposes (esp) for vocational pharmacy students. Budapest International Research and Critics in Linguistics and Education (BirLE). Journal. 2020;3(2):724–33.
Chan S, Taylor L. Comparing writing proficiency assessments used in professional medical registration: a methodology to inform policy and practice. Assess Writ. 2020;46:100493.
Hyland K, Jiang FK. Delivering relevance: the emergence of ESP as a discipline. Engl Specif Purp. 2021;64:13–25.
Maftuna B. The role of English in ESP. Am J Adv Sci Res. 2024;1(2):1–5.
LEON LI, HUMANIZING THE FOREIGN LANGUAGE. COURSE: NEW TEACHING METHODS FOR MEDICAL STUDENTS. Language, Culture and Change. 2022:243.
Dahm MR, Yates L. Rapport, empathy and professional identity: Some challenges for international medical graduates speaking English as a second or foreign language. Multilingual Healthcare: A Global View on Communicative Challenges. 2020:209 – 34.
Gedamu AD, Gezahegn TH. TEFL trainees’ attitude to and self-efficacy beliefs of academic oral presentation. Cogent Educ. 2023;10(1):2163087.
Saliu B, Hajrullai H. Best practices in the English for specific purpose classes at the language center. Procedia-Social Behav Sci. 2016;232:745–9.
Clokie TL, Fourie E. Graduate employability and communication competence: are undergraduates taught relevant skills? Bus Prof Communication Q. 2016;79(4):442–63.
Hartono H, Mujiyanto J, Fitriati SW, Sakhiyya Z, Lotfie MM, Maharani MM. English Presentation Self-Efficacy Development of Indonesian ESP students: the effects of Individual versus Group Presentation tasks. Int J Lang Educ. 2023;7(3):361–76.
Azizi Z, Farid Khafaga A. Scaffolding via Group-dynamic Assessment to positively affect motivation, learning anxiety, and willingness to Communicate: a Case Study of High School Students. J Psycholinguist Res. 2023;52(3):831–51.
Grieve R, Woodley J, Hunt SE, McKay A. Student fears of oral presentations and public speaking in higher education: a qualitative survey. J Furth High Educ. 2021;45(9):1281–93.
Hall D, Buzwell S. The problem of free-riding in group projects: looking beyond social loafing as reason for non-contribution. Act Learn High Educ. 2013;14(1):37–49.
Almazyad M, Aljofan F, Abouammoh NA, Muaygil R, Malki KH, Aljamaan F, et al. Enhancing Expert Panel discussions in Pediatric Palliative Care: innovative scenario development and summarization with ChatGPT-4. Cureus. 2023;15(4):e38249.
Bhuvaneshwari S, Rashmi R, Deepika K, Anirudh VM, Vijayamathy A, Rekha S, Kathiravan R. Impact of panel discussion in educating AETCOM First Module among Undergraduate Medical Students. Latin Am J Pharmacy: Life Sci J. 2023;42(6):407–12.
Johnson BR, Logan LD, Darley A, Stone RH, Smith SE, Osae SP, et al. A scoping review for Debate-Style Journal Clubs in Health Professional Education. Am J Pharm Educ. 2023;87(6):100064.
Nurakhir A, Palupi FN, Langeveld C, Nurmalia D. Students’ views of classroom debates as a strategy to enhance critical thinking and oral communication skills. 2020.
Jones EP, Nelson NR, Thorpe CT, Rodgers PT, Carlson RB. Use of journal clubs and book clubs in pharmacy education: a scoping review. Currents Pharm Teach Learn. 2022;14(1):110–9.
Dyhrberg O’Neill L. Assessment of student debates in support of active learning? Students’ perceptions of a debate-based oral final exam. Act Learn High Educ. 2024.
Dyment JE, O’Connell TS. Assessing the quality of reflection in student journals: a review of the research. Teach High Educ. 2011;16(1):81–97.
Villarroel V, Bloxham S, Bruna D, Bruna C, Herrera-Seda C. Authentic assessment: creating a blueprint for course design. Assess Evaluation High Educ. 2018;43(5):840–54.
Schultz M, Young K, Gunning K, Harvey T. Defining and measuring authentic assessment: a case study in the context of tertiary science. Assess Evaluation High Educ. 2022;47(1):77–94.
Sundrarajun C, Kiely R. The oral presentation as a context for learning and assessment. Innov Lang Learn Teach. 2010;4(2):101–17.
Wyatt-Smith C, Adie L. The development of students’ evaluative expertise: enabling conditions for integrating criteria into pedagogic practice. J Curriculum Stud. 2021;53(4):399–419.
Boud D, Lawson R, Thompson DG. The calibration of student judgement through self-assessment: disruptive effects of assessment patterns. High Educ Res Dev. 2015;34(1):45–59.
A. S. Enhancing Meaningful Learning experiences through Comprehension and Retention by students. Twentyfirst Century Publications Patiala. 2023;49.
Colton D, Covert RW. Designing and constructing instruments for social research and evaluation. Wiley; 2007.
Krueger RA, Casey MA. Focus group interviewing. Handbook of practical program evaluation. 2015:506 – 34.
Morgan DL. Handbook of interview research: Context and method. Oaks, CA, USA: Sage Publications Thousand; 2002.
Braun V, Clarke V. Conceptual and design thinking for thematic analysis. Qualitative Psychol. 2022;9(1):3.
Elliott V. Thinking about the coding process in qualitative data analysis. Qualitative Rep. 2018;23(11).
Syed M, Nelson SC. Guidelines for establishing reliability when coding narrative data. Emerg Adulthood. 2015;3(6):375–87.
Lincoln Y. Naturalistic inquiry: Sage; 1985.
Hartono H, Mujiyanto J, Fitriati SW, Sakhiyya Z, Lotfie MM, Maharani MM. English presentation self-efficacy development of Indonesian ESP students: the effects of Individual versus Group Presentation tasks. Int J Lang Educ. 2023;7(3).
Li X. Teaching English oral presentations as a situated task in an EFL classroom: a quasi-experimental study of the effect of video-assisted self-reflection. Revista Signos. 2018;51(98):359–81.
Chou M-h. The influence of learner strategies on oral presentations: a comparison between group and individual performance. Engl Specif Purp. 2011;30(4):272–85.
Harris A, Jones M, Huffman J. Teachers leading educational reform. The power of. 2017.
Agustina L. Stimulating students to speak up through presentation in business English class. J Appl Stud Lang. 2019;3(1):21–8.
Babal JC, Abraham O, Webber S, Watterson T, Moua P, Chen J. Student pharmacist perspectives on factors that influence wellbeing during pharmacy school. Am J Pharm Educ. 2020;84(9):ajpe7831.
Moir F, Yielder J, Sanson J, Chen Y. Depression in medical students: current insights. Adv Med Educ Pract. 2018;323:33.
Pavlinac Dodig I, Lusic Kalcina L, Demirovic S, Pecotic R, Valic M, Dogas Z. Sleep and lifestyle habits of medical and non-medical students during the COVID-19 lockdown. Behav Sci. 2023;13(5):407.
Nowak G, Speed O, Vuk J. Microlearning activities improve student comprehension of difficult concepts and performance in a biochemistry course. Currents Pharm Teach Learn. 2023;15(1):69–78.
Mehmood K, Memon S, Ali F. Language barriers to Effective Communication in speaking English: a phenomenological study of Pakistan International cricketers. Pakistan Lang Humanit Rev. 2024;8(1):107–14.
Buelow JR, Downs D, Jorgensen K, Karges JR, Nelson D. Building interdisciplinary teamwork among allied health students through live clinical case simulations. J Allied Health. 2008;37(2):e109–23.
Rodríguez-Sedano FJ, Conde M, Fernández-Llamas C, editors. Measuring teamwork competence development in a multidisciplinary project based learning environment. Learning and Collaboration Technologies Design, Development and Technological Innovation: 5th International Conference, LCT 2018, Held as Part of HCI International 2018, Las Vegas, NV, USA, July 15–20, 2018, Proceedings, Part I 5; 2018: Springer.
Wilson L, Ho S, Brookes RH. Student perceptions of teamwork within assessment tasks in undergraduate science degrees. Assess Evaluation High Educ. 2018;43(5):786–99.
Parmar D, Bickmore T. Making it personal: addressing individual audience members in oral presentations using augmented reality. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2020;4(2):1–22.
Pasandín AMR, Pérez IP, Iglesias PO, Díaz JJG. Cooperative oral presentations in higher education to enhance technical and soft skills in engineering students. Int J Continuing Eng Educ Life Long Learn. 2023;33(6):592–607.
Ragupathi K, Lee A. Beyond fairness and consistency in grading: The role of rubrics in higher education. Diversity and inclusion in global higher education: Lessons from across Asia. 2020:73–95.
Rabbi MF, Islam MS. The effect of academic stress and Mental anxiety among the students of Khulna University. Edukasiana: Jurnal Inovasi Pendidikan. 2024;3(3):280–99.
Popa CO, Schenk A, Rus A, Szasz S, Suciu N, Szabo DA, Cojocaru C. The role of acceptance and planning in stress management for medical students. Acta Marisiensis-Seria Med. 2020;66(3):101–5.
Christianson M, Payne S. Helping students develop skills for better presentations: Using the 20x20 format for presentation training. 語学研究. 2012;26:1–15.
Romero-Yesa S, Fonseca D, Aláez M, Amo-Filva D. Qualitative assessment of a challenge-based learning and teamwork applied in electronics program. Heliyon. 2023;9(12).
Bosco TJ, Gabriel B, Florence M, Gilbert N. Towards effective teaching and learning ESP in mixed classes: students’ interest, challenges and remedies. Int J Engl Literature Social Sci. 2020;5(2):506–16.
Qiao L, Xu Y, bin Ahmad N, An Analysis Of Implementation Challenges For English, For Specific Purposes (Esp) Formative Assessment Via Blended Learning Mode At Chinese Vocational Polytechnics. Journal Of Digital Education, Communication, And Arts (DECA). 2023;6(02):64–76.
Kho MG-W, Ting S-H. Overcoming oral presentation anxiety: a systematic review of Tertiary ESL/EFL Students’ challenges and strategies. Qeios. 2023.
Download references
We confirm that no funding was received for this work.
Author information
Authors and affiliations.
Department of English Language, School of Paramedical Sciences, Shiraz University of Medical Sciences, Shiraz, Iran
Elham Nasiri & Laleh Khojasteh
You can also search for this author in PubMed Google Scholar
Contributions
L.KH was involved in writing the proposal, reviewing the text, analyzing the data, and writing the manuscript. E. N was involvedin designing the research and collecting and analyzing the data. Both authors have reviewed and approved the final version of the manuscript.
Corresponding author
Correspondence to Laleh Khojasteh .
Ethics declarations
Ethics approval and consent to participate.
Our study, entitled “Evaluating Panel Discussions in ESP Classes: An Exploration of International Medical Students’ and ESP Instructors’ Perspectives through Qualitative Research,” was reviewed by the Institutional Review Board (IRB) of the School of Paramedical Sciences, Shiraz University of Medical Sciences (SUMS). The IRB reviewed the study on August 14th, 2024, and determined that formal ethics approval or a reference number was not required. This decision was based on the fact that the research posed minimal risk to participants and focused solely on their educational experiences without involving any intervention or the collection of sensitive personal data.
Consent for publication
Not Applicable.
Competing interests
We confirm that there are no known conflicts of interest associated with this publication and that this work did not receive any financial support.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Nasiri, E., Khojasteh, L. Evaluating panel discussions in ESP classes: an exploration of international medical students’ and ESP instructors’ perspectives through qualitative research. BMC Med Educ 24 , 925 (2024). https://doi.org/10.1186/s12909-024-05911-3
Download citation
Received : 08 May 2024
Accepted : 14 August 2024
Published : 26 August 2024
DOI : https://doi.org/10.1186/s12909-024-05911-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Group oral presentations
- Medical students
- Panel discussions
- ESP courses
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
- Open access
- Published: 28 August 2024
Pre-implementation planning for a sepsis intervention in a large learning health system: a qualitative study
- Tara A. Eaton 1 ,
- Marc Kowalkowski 1 , 2 ,
- Ryan Burns 3 ,
- Hazel Tapp 4 ,
- Katherine O’Hare 5 &
- Stephanie P. Taylor 6
BMC Health Services Research volume 24 , Article number: 996 ( 2024 ) Cite this article
Metrics details
Sepsis survivors experience high morbidity and mortality. Though recommended best practices have been established to address the transition and early post hospital needs and promote recovery for sepsis survivors, few patients receive recommended post-sepsis care. Our team developed the Sepsis Transition and Recovery (STAR) program, a multicomponent transition intervention that leverages virtually-connected nurses to coordinate the application of evidence-based recommendations for post-sepsis care with additional clinical support from hospitalist and primary care physicians. In this paper, we present findings from a qualitative pre-implementation study, guided by the Consolidated Framework for Implementation Research (CFIR), of factors to inform successful STAR implementation at a large learning health system prior to effectiveness testing as part of a Type I Hybrid trial.
We conducted semi-structured qualitative interviews ( n = 16) with 8 administrative leaders and 8 clinicians. Interviews were transcribed and analyzed in ATLAS.ti using a combination deductive/inductive strategy based on CFIR domains and constructs and the Constant Comparison Method.
Six facilitators and five implementation barriers were identified spanning all five CFIR domains (Intervention Characteristics, Outer Setting, Inner Setting, Characteristics of Individuals and Process). Facilitators of STAR included alignment with health system goals, fostering stakeholder engagement, sharing STAR outcomes data, good communication between STAR navigators and patient care teams/PCPs, clinician promotion of STAR with patients, and good rapport and effective communication between STAR navigators and patients, caregivers, and family members. Barriers of STAR included competing demands for staff time and resources, insufficient communication and education of STAR’s value and effectiveness, underlying informational and technology gaps among patients, lack of patient access to community resources, and patient distrust of the program and/or health care.
Conclusions
CFIR proved to be a robust framework for examining facilitators and barriers for pre-implementation planning of post-sepsis care programs within diverse hospital and community settings in a large LHS. Conducting a structured pre-implementation evaluation helps researchers design with implementation in mind prior to effectiveness studies and should be considered a key component of Type I hybrid trials when feasible.
Trial registration
Clinicaltrials.gov, NCT04495946 . Registered August 3, 2020.
Peer Review reports
Contributions to literature
This qualitative pre-implementation study of a telehealth nurse navigator-led sepsis transition and recovery (STAR) program demonstrates the Consolidated Framework for Implementation Research (CFIR) is useful to explore contextual conditions of healthcare settings as part of rigorous pre-implementation planning efforts.
This analysis identified actionable facilitators and barriers spanning all five CFIR domains (e.g., inner setting, outer setting) to inform and enhance initial implementation strategies of STAR.
These findings help to close recognized gaps in the literature on post-sepsis survivorship, including how to plan implementation of evidenced-based practices to address transition and early post hospital needs of sepsis survivors and promote recovery.
Sepsis, a common and life-threatening dysregulated response to infection, remains a major cause of morbidity, mortality, and healthcare costs [ 1 , 2 , 3 ]. Although hospital survival has improved in recent years, the increasing number of sepsis survivors are vulnerable to additional health problems [ 4 , 5 , 6 ]. Fewer than one-half of sepsis survivors return to their pre-sepsis health status and many experience new or worsening physical, cognitive, and psychological impairments, along with high rates of rehospitalization and excess mortality for years after sepsis hospitalization [ 7 , 8 , 9 ]. Given increasing recognition of the substantial long-term sequelae and social determinants of health-related needs after sepsis [ 10 ], recommended best practices have been established to address the transition and early post hospital needs and promote recovery for sepsis survivors [ 11 , 12 , 13 ]. However, like the majority of other evidence-based practices (EBPs) that have yet to be successfully adopted into routine practice, few patients receive recommended post-sepsis care [ 14 , 15 ].
To address the transition and early post hospital needs for sepsis survivors, our team developed the Sepsis Transition and Recovery (STAR) program, a multicomponent transition intervention that leverages centrally-located, virtually-connected nurses to coordinate the application of evidence-based recommendations for post-sepsis care with additional clinical support from hospitalist and primary care physicians [ 16 ]. The STAR program, based on the chronic care model [ 17 ], empowers patients and clinicians, via targeted education and coordinated care approaches, and was found to improve mortality and readmission outcomes among sepsis survivors [ 18 ]. There are complex barriers to translation of research findings into real-world post-sepsis care which we sought to identify and mitigate prior to effectiveness testing as part of a Type I Hybrid trial [ 19 ].
Before initiating a large-scale, pragmatic effectiveness evaluation of the STAR program (NCT04495946), we conducted a qualitative pre-implementation study with the aim to identify actionable facilitators and barriers to inform and enhance initial implementation strategies of the program across diverse hospital and community settings in a large Learning Health System (LHS). Qualitative methods are considered an integral component of implementation research and are well-known for being rigorous and efficient in the study of the hows and whys of implementation [ 20 ]. Conducting a robust pre-implementation evaluation was an intentional design choice for the overall project given the critical role of this step in the implementation process [ 21 ]. Through our qualitative investigation, we explored variations in stakeholder perspectives of the program by interviewing both administrators and clinicians.
We guided our study with the Consolidated Framework for Implementation Research (CFIR), due to its breadth, widespread use [ 22 , 23 ], and expert-recommended mapping from CFIR-identified barriers to defined implementation strategies [ 24 ]. As a framework, the CFIR offers a systematic approach well-known for planning, evaluating, and supporting behavioral change for a diverse array of studies [ 25 ], using a consistent language of 39 constructs organized across five domains—Intervention Characteristics, Outer Setting, Inner Setting, Characteristics of Individuals and Process [ 22 ]. It can be used to build implementation knowledge to describe determinants of implementation [ 23 ], as well as tailor pre-implementation strategies to promote intervention success [ 26 , 27 ].
For this pre-implementation study, we conducted a qualitative investigation to identify facilitators and barriers to implementing the STAR program in hospital transition care, and to elaborate and compare key stakeholder perspectives. Instrument development, data collection, analysis, and interpretation of study results were guided by the CFIR. A PhD-level trained qualitative health services researcher (TE) on the study team with experience conducting qualitative research for program evaluations and intervention development led the process of interview instrument design, data collection, and analysis. She was not known to participants of the research prior to undertaking the study. Our study team followed the Standards for Reporting Qualitative Research in the reporting of this work [ 28 ].
Study design
The pre-implementation study was conducted from March through July of 2020 in preparation for the planned implementation of the STAR program intervention in July 2020 at a large LHS. Headquartered in Charlotte, North Carolina, Atrium Health provides not-for-profit healthcare supporting over 14 million patient encounters annually across 40 hospitals and over 1,000 care locations in North Carolina, Georgia, and Alabama. We identified all stakeholders involved with post-sepsis care in this health system according to a framework for stakeholder mapping in health research [ 29 ]. With sepsis survivors and caregivers at the center of our focus for STAR, we identified stakeholder categories relevant to them to determine our recruitment approach for the pre-implementation interviews. By employing an iterative process of delineation between key individuals and groups involved in post-sepsis care at the LHS, we identified key stakeholders.
These stakeholders comprised two main groups: administrative leaders and clinicians. Administrative leaders were chief medical and nursing officers. We selected administrators due to their understanding of outer and inner setting factors and influence on organizational policy. Clinicians were hospitalists and ambulatory care providers representing diverse practice settings. We selected clinicians as representative intervention users with knowledge of intervention characteristics, outer setting, inner setting, characteristics of individuals, and process factors. We purposively sampled potential participants to reflect these organizational roles and responsibilities at the planned intervention sites. We aimed to recruit individuals to sufficiently capture a range of beliefs about post-sepsis care in these practice settings, while limiting redundancy in our data collection.
The final sample included 8 administrators (Chief Medical Officers, Nursing Executives, and a Departmental Chair; representing 7 study hospitals and leadership over post-hospital continuing care and primary care services) and 8 clinicians (with specialty areas in one or more of the following: Hospital Medicine, Internal Medicine, Infectious Disease, Family Medicine and Critical Care; representing individuals with care privileges at 6 study hospitals and primary care responsibilities in the communities served by these hospitals). See Table 1 : Participant Characteristics.
Data collection
We conducted semi-structured qualitative interviews with 16 stakeholders from diverse hospitals and care settings to explore organizational support, culture, workflow processes, needs, and recommendations for STAR’s implementation. Separate and original interview guides were developed for administrator and clinician groups (See Additional file 1: Administrator Interview Guide and Additional file 2: Clinician Interview Guide) in this study, however, both guides included questions about stakeholder roles and work environments, the fit of the STAR program for their facilities which was facilitated using a printed intervention workflow diagram (See Fig. 1 : Patient Trajectory through the STAR Program), and questions about the implementation of STAR. Interview guides intentionally included questions representative of all 5 of the CFIR domains (Intervention Characteristics, Outer Setting, Inner Setting, Characteristics of Individuals and Process) and were initially scripted by adapting questions from the CFIR Interview Guide Tool available at the CFIR website, www.cfguide.org [ 30 ]. Some of the sample questions from the guides are included below:

Patient trajectory through the STAR program
Do you think effectiveness data about the sepsis transition program would be needed to get team buy-in in your facility? (Intervention Characteristics)
How well, would you say, are new ideas (e.g., work processes, new interventions, QI projects, research) embraced and used to make improvements in your facility? (Inner Setting)
What, if any, barriers do you think patients will face to participate in the intervention? (Outer Setting)
What is your role within the organization? (Characteristics of Individuals)
Who would you recommend are the key individuals to speak with to make sure new interventions are successful in your practice or department? (Process)
We pilot tested (field tested) the interview guides in three rounds prior to their administration and iteratively refined the guides based on participant feedback and research team members’ perceptions of the usefulness of the data collection instruments for eliciting information we intended to capture for each stakeholder group (See Fig. 2 : Diagram of Interview Guide Development at Pre-Implementation). Field testing is an established technique in qualitative research for developing interview guides as it provides researchers with the opportunity to practice asking the interview questions and identify weaknesses in the wording and order of questions when spoken aloud [ 31 ]. We then used the refined data collection instruments for the interviews reported here.

Diagram of interview guide development at pre-implementation
Prior to each interview, participants received standardized background information about the study topic and verbal informed consent was obtained. As an adaptation due to research restrictions during the COVID-19 pandemic, interviews were conducted telephonically. Interviews were on average 30 min in duration, which was expected given the number of questions asked of participants (13 questions for the administrators and 15 questions for the clinicians) and what was seen during the pilot testing of the interview guides prior to data collection. Participants were offered a $25 gift card for their participation. Ethical approval for this study was granted by the Advarra IRB Committee.
Data analysis
Interview recordings were transcribed and entered into ATLAS.ti X8 as text documents for thematic coding and analysis. One team member with extensive experience in qualitative research methods (TE) led the analysis of the data set using a combination deductive/inductive strategy based on CFIR domains and constructs and the Constant Comparison Method. The Constant Comparison Method is an inductive approach for developing code structure through the iterative comparison of newly coded text with previously coded text of the same theme until final thematic refinement is achieved [ 32 ]. We referred to the cfirguide.org website’s CFIR Codebook Template [ 33 ], containing domain and construct definitions and guidance for coding qualitative data with the framework and inclusion and exclusion criteria for most constructs, in our application of the framework to our codebook development and analysis. This process included creating a codebook (a complete list of codes and definitions for each code), coding the data set among team members, comparing identified codes, and merging codes when it was necessary based on analytical discussion. Each code was labeled using the following convention: 1) if it was an implementation facilitator or barrier code, 2) a simplified title indicating what the code was, and 3) and a tag of the CFIR domains and constructs that corresponded to the code. E.g., ImplFacilitator_Family support for PT: OUTSET-PT Needs & Res. Throughout the process of analyzing the qualitative interview data, our study team met bi-weekly to discuss the results and engaged with the larger stakeholder group monthly to discuss ideas for overcoming identified barriers.
To promote the reliability of the analysis and prevent interpretive bias, two study team members (TE and RB) completed inter-rater reliability (IRR) coding for 50% of the administrator interviews (n = 4). Three team members (TE, KO, and HT) completed IRR for 50% of the clinician interviews ( n = 4). IRR was conducted by having additional coders (RB, KO, and HT) apart from the principal analyst (TE) apply the codebook to the data set to determine whether they agreed with the original coding of selected interview transcripts. Instances of disagreement were discussed thoroughly and, at times, resulted in the application of additional codes for selected quotations. All identified conflicts in coding were fully resolved, resulting in a final agreement of 100% between coders.
Using a combination deductive/inductive coding strategy, we found 77 codes related to STAR implementation facilitators ( n = 38) and barriers ( n = 39) and labeled those codes with applicable CFIR domains and constructs as appropriate. The STAR implementation facilitators and barriers codes were then aggregated into 11 themes consisting of 6 facilitators (See Table 2 ) and 5 implementation barriers (See Table 3 ). STAR implementation facilitators and barriers, together, spanned all five CFIR domains (Intervention Characteristics, Outer Setting, Inner Setting, Characteristics of Individuals and Process). Administrators and clinicians reported no other sepsis-specific transition programs in their facilities at the time of data collection and indicated the STAR program would be important to address sepsis survivor needs.
Facilitators influencing the implementation of STAR
Our analysis identified six themes pertaining to implementation facilitators. See Table 2 : CFIR-Guided Facilitators of STAR Implementation.
Alignment between STAR and health system goals
Participants reported that STAR’s alignment with other telehealth programs at the LHS, such as virtual hospital care, amidst surge of telehealth care during the COVID-19 pandemic would promote implementation of STAR as indicated in the administrator’s response below:
“I also think it [STAR] would be well received based on the information regarding virtual hospital and what we have been able to achieve with that. And, again with just looking for the bright spots in COVID, there have been a lot of transitions that have taken place in the last couple of months that I think you would have a much easier time implementing this in the new world of healthcare.” (A7)
Beyond virtual care, participants also described other existing infrastructure within the LHS that would align with the STAR program objectives, including sepsis work groups and sepsis champions from physicians, nurses, pharmacy, and case management. These inner setting facilitators combined demonstrate how STAR’s alignment with the implementation climate (compatibility) and structural characteristics of the LHS would influence its adoption.
Fostering engagement with stakeholders
Participants stated that fostering engagement to promote buy-in with stakeholders, including administrators, care teams, patients and caregivers, would facilitate the implementation of STAR. They recommended stakeholders be educated about what STAR is, its benefits, and for organizational stakeholders, how best to integrate STAR into their facility. See the clinician’s response below:
“I think just education [about STAR]. Just tons of education to everyone in the hospital that touches a patient. The nurses. The critical care physicians. The Hospitalists…But I think just educating the patient [about STAR] at the time of admission, just start that process. You know, this is our sepsis program, and let them know that this is going to happen at the time of discharge. And then also provide education to the providers.” (C1)
Participants also emphasized the importance of leaders heading communication about STAR with care teams and STAR navigators establishing a good rapport with clinicians who have patients enrolled in the program. See the clinician’s response below:
“Well, definitely share the information [about STAR] with their [health system leaders] teams. We have a normal leadership structure that provides the mechanism for things like this to be communicated in top down. And for sure, expecting the leaders to disseminate it from Level 2 to Level 3, Level 3 to Level 4 and on down. You know, that would be a minimum expectation…I think they should welcome you all [the STAR study team] at the meetings and give you time on the agenda to share your initiatives, at a minimum.” (C3)
These responses illustrate the relevance of the CFIR outer setting, process, and characteristics of individuals domains for the implementation of STAR, where prioritizing patient needs, attracting and involving appropriate individuals, and individual attitudes about the intervention would be facilitators of its adoption.
Share positive STAR outcomes data
Participants reported sharing positive results or impacts from the program would be helpful. They recommended using STAR performance metrics as motivation for continued buy-in and that leaders share effectiveness data. See the clinician responses below:
“I think readmission data [would be good to provide], like at 90 days, because if you are trying to get people to buy in for 90 days, cause that’s a long time, that’s about three months, I think you need to prove that it is worthwhile. If you’re trying to cut back on that 90-day readmission, because that’s what Medicare looks at, I think that would maybe entice some people to participate.” (C7)
“But, if you want to implement it as a standard process then we are going to have to see some sort of data on it before we say “yep, let’s do it”. Because there are many things that are competing for the resources that we have. So we have to on the basis on which our decisions on where the money goes, where those resources get diverted to is based on how efficiently they affect patient care, rates of readmission, and patient mortality. So we need the data to make an informed decision.” (C2)
Responses pertaining to this theme point to the significance of the CFIR intervention characteristics, inner setting and process domains in STAR’s implementation. Participants’ remarks regarding STAR’s evidence, strength and quality, shared receptivity to STAR within the LHS, and the recommendation to provide quantitative and qualitative feedback for reflecting and evaluating STAR’s quality would be facilitators of its implementation.
Good communication between STAR navigators and patient care teams/PCPs
Participants stated that good communication and recommendation-sharing between the STAR navigator and the patient’s care team and PCP will make STAR’s implementation successful. See the clinician’s response below:
“So, I think, effectively communicating with one another [the STAR navigator and clinician] what is beneficial and helping us ultimately provide for the patient from our end would be helpful. It will be a learning process, but you know, I think once we both communicate what we need from the other to be able to do our jobs, then I think that would be fine if that makes sense.” (C5)
These intervention characteristics and inner setting facilitators demonstrate the importance of intervention design, including how well STAR is bundled, presented and assembled to stakeholders, and navigator-led communication in its implementation.
Clinician promotion of STAR with patients
Our study participants emphasized the importance of clinician promotion of STAR with enrolled patients for implementation success. Specifically, our participants recommended that the LHS show patients their primary care providers and STAR navigators are in alignment to engender patient trust in the program. See the administrator’s response below:
“It always helps if they [patients] feel like it’s their own physicians or their own team that is a part of this. I think it would be important for it not to look like it was some external program that their clinicians were not involved in. So, I think, you know, trust always is important if you feel like people that you trust are endorsing something or believing it’s going to be useful.” (A8)
Similarly, one clinician said:
“I think trust, you know, would be a factor. A lot of times if patients view resources as being disconnected from their Primary Care, they may not be very accepting of them. So, if they view them as being part of “my team”, I think patients are much more likely to participate.” (C3)
Participant responses within this theme underscore the multi-domain influence of outer setting, inner setting and the process of implementation in the success of STAR, where the LHS’s prioritization of patient needs, LHS members’ and structures’ characteristics and behaviors, and the engagement of individuals with STAR would be facilitators of its implementation.
Good rapport and effective communication between STAR navigators and patients, caregivers, and family members
Participants reported that good rapport and effective communication between STAR navigators and enrolled patients and their caregivers/families would be important for implementing STAR. They emphasized the need for STAR navigators to foster a good connection with patients and their caregivers or family members. They also spoke to the integral role caregivers and family members play in patients’ post-sepsis recovery as additional points of contact who are familiar with the program if the patient does not recall what STAR is or if the patient is too ill to speak for themselves. See the clinicians’ responses below:
“I think patients get called a lot about a lot of things and they don’t always know who the person on the phone is. So, I think having that established and really something that the patient is okay with is important. And engaging, if possible, family or support members. I think that reduces barriers if they have support people available.” (C6)
“I think obviously reaching out to the family and support staff and things like that may be helpful. Some of our patients, in general, even at their baseline and at their best day aren’t going to be able to provide you the information that you need, or may not be able to provide an adequate history, or have an appropriate follow-up, and things like that, in place to be able to give you the information you need to help them as well as you would like.” (C5)
Responses within this facilitator theme highlight the importance of intervention characteristics, such as the perceived quality of STAR, and outer setting domains and constructs (patient needs and resources) in STAR navigator communication with patients and their caregivers and family members. Results show how effective navigator communication when presenting STAR to patients and their caregivers/family members, consideration of patient needs and barriers to participation, and the involvement of caregivers or family members would be facilitators of STAR’s implementation.
Barriers influencing the implementation of STAR
Our analysis identified five themes pertaining to implementation barriers. See Table 3 : CFIR-Guided Barriers to STAR Implementation.
Competing demands for staff time and resources
Participants reported that competing demands for staff time and resources, including the busy state of the LHS’ facilities at the time, COVID priorities, other concurrent program implementations, and a lack of time among clinicians to engage with STAR could be barriers to its implementation. See the administrator’s response below:
“So, I think barriers would be too many implementations going on at the same time. It would fail. The other is, right now in COVID time, it’s unlikely to muster enough support or enough interest to do it. I think we need to look at what else is going on, so that there is not information overload for the front-end teammates. And the other thing we look at is, most of these programs become paper intensive or computer intensive. That means, you are just putting things there, and then, if you ask people to do too much, yes, they do too much, but they don’t really do the thing…So just be mindful of that, what you expect them to spend time on.” (A3)
Similarly, one clinician commented:
“Now, from a willingness standpoint, not that people would necessarily disagree with the overall goals and the process of your program, it’s just that if you’re in my field, and in some of my partners, if we are being pulled in ten different directions at one time, you have to prioritize what you can do in a day. So, not willingness from the standpoint of people not wanting to participate, but sometimes people not being able to weight or value that as high as something else that needs to be done.” (C5)
Participants responses pertaining to this barrier theme illustrate the role that the LHS’s inner setting, specifically its implementation climate of decreased organizational capacity to absorb change and a lack of resources dedicated for STAR, would play in hindering the implementation of the program.
Insufficient communication and education of program value and effectiveness
Participants reported that insufficient communication and education of STAR’s value and effectiveness to other clinicians could be barriers to its implementation. See the administrator’s response below:
“To me, it’s always a matter of communication. If there was, if communication didn’t work, people didn’t see it had value, they didn’t want to put any effort into it, you know, those would really be obviously the big things.” (A8)
“So, if it’s not marketed like correctly or appropriately. If we really as attending or residents don’t see the benefit. You know, is this just another checky box, or is this really going to impact our patients in the long term? Will this make a difference in their survival? Or getting them back to a base line or improvements on a base line? I think that’s probably what’s going to help make it successful or not.” (C8)
Responses related to this barrier theme show that the LHS’s inner setting and characteristics of individuals (clinicians) are important implementation domains in the adoption of STAR. Participants identified poor quality communication, and a lack of clinician knowledge and positive beliefs about STAR’s value, would be barriers to the implementation of the program.
Underlying informational and technology gaps among patients
Participants reported several patient-facing factors related to information and technology gaps among patients that could be barriers to implementing STAR. This included a patient’s health literacy or understanding of STAR, a patient’s digital literacy, and a patient’s lack of access to technology when communicating with the STAR telehealth navigator. See the clinician responses below:
“Well, I think a lot of our patients don’t have secure housing. I think our patients’ baseline social determinants of health, like consistent phone numbers, housing, health literacy around that, I think that’s a barrier that a patient would experience [to participate in the intervention].” (C6)
“I think the only barrier is that they [patients] may not understand what is going on. But that’s okay [as if not a big deal], as long as they are receptive to someone talking to them. And like I said, I want to be respectful of our patients, but some of them just do not have the medical literacy or the insight to understand….So, I think a barrier might be that the patient may not understand why you are calling and why you are asking those questions.” (C1)
“Definitely patients have to be capable of doing it uh participating with the Telehealth. At least from the perspective of a lot of my patients and during the Coronavirus pandemic, it has been difficult to get some buy in with Telehealth linkages to care. We have a very rural population and there is some adherence issues with trying to initiate, you know, telephonic or video visits that we have kind of noticed over the last several months. So, patient participation I think in some settings would be challenging.” (C4)
Participant responses within this barrier theme highlight the importance of the outer setting (external to the LHS) in the challenge of implementing STAR, where literacy and technology gaps among patients could be barriers to program enrollees’ participating in the telehealth-based intervention.
Lack of access to community resources for patients
Finally, participants reported that a patient’s lack of access to community resources, including limited primary care, paramedicine, home physical therapy, speech therapy and mental health resources in certain communities (e.g., rural communities), could pose a barrier to the implementation of the STAR program. See the clinicians’ responses below:
“I think that the idea is a good idea [pauses], but it’s just where it would work best based upon the resources of the area. I think that is going to be the major challenge.” (C7)
“Just getting plugged into community resources that can assist with their psycho-social needs as well as their comorbidities” [would be a barrier to patient participation]. (A1)
Participant responses within this theme demonstrate the relevance of intervention characteristics and the outer setting when implementing EBPs for post-sepsis care for patients who lack access to community resources. The extent to which STAR cannot adapt and meet patients’ local needs, especially those of patients who live in areas where there are insufficient resources, will be a barrier to its implementation.
Patient distrust of the program and/or healthcare
Both administrators and clinicians interviewed stated that patient distrust of the program and/or healthcare could be a potential barrier to STAR’s implementation. These reasons included patients being slow to trust a new provider, discomfort when talking with a navigator, feeling skeptical of providers who seem unaffiliated with their primary care, and general distrust of the healthcare system, particularly for patients in rural communities or impoverished areas. See the administrator and clinician responses below:
“You know, people are always a little wary of people they do not know, especially in small and rural communities.” (A1)
“Yeah, I think most of the barriers that are already well known that go with socio economic status or poverty. Trust in the healthcare system. I think those are all going to be barriers.” (C4)
Responses within this theme point to the significance of outer setting factors and the extent to which a patient’s need to trust their provider is accurately known and prioritized by the STAR navigator. Data suggests patient distrust of the STAR program or other providers would be a barrier to implementing EBPs for post-sepsis care.
A foundation of implementation science is that intervention delivery should be tailored to local context to maximize uptake and impact [ 34 , 35 ]. Formative, or pre-implementation, evaluations facilitate initial assessment of the local context and the potential determinants for implementation success within that context. Multiple theoretical frameworks have been applied to pre-implementation evaluations; the Consolidated Framework for Implementation Science (CFIR) is one of the most widely used due to its ability to comprehensively identify implementation facilitators and barriers [ 36 ]. In this study, we utilized qualitative pre-implementation interviews to identify actionable facilitators and barriers to inform and enhance initial implementation strategies of the STAR program across diverse hospital and community settings in a large LHS. From this work, our study offers several contributions to the literature on post-sepsis care.
First, our study successfully leveraged the CFIR to inform and enhance initial implementation strategies of the STAR program across diverse hospital and community settings in a large LHS. This is in line with other studies that similarly applied the CFIR during pre-implementation and found implementation determinants like ours, such as stakeholder involvement being necessary to promote buy-in and the relevance of intervention fit within the organization’s inner setting [ 26 , 37 ]. While some have applied CFIR in the pre-implementation planning of a sepsis management intervention at a single site [ 38 ], to our knowledge, our team is the first to apply the CFIR at pre-implementation to inform the design and dissemination of a sepsis transition and recovery intervention for patients within a large LHS. We decided to guide our interview instrument development and subsequent analysis using the CFIR because we were interested, fundamentally, in the organizational change that will be needed to successfully implement the STAR program. By incorporating the CFIR domains and constructs into our interview instruments and intervention planning, our study was able to identify implementation partners and collect stakeholder input on the potential facilitators and barriers to the STAR program at a large LHS. One benefit of using the CFIR for pre-implementation work is the potential for direct translation to implementation strategies selection using the Expert Recommendations for Implementing Change (ERIC) mapping.
Second, study findings revealed the importance of stakeholder buy-in like other CFIR-guided pre-implementation studies [ 26 , 39 ] across diverse groups, including administrators, care teams, patients, and caregivers. Implementation facilitators related to buy-in that were identified included active engagement with stakeholders, education about STAR, the sharing of positive outcomes data from STAR with clinicians, and promotion of the program’s value throughout implementation. Participants also emphasized the criticality of demonstrating alignment between clinicians and the STAR program. This included the recommendation for clinician support and promotion of STAR with patients to engender patient trust in the program. Conversely, our study found implementation barriers pertaining to lack of stakeholder buy-in as well. These included that a lack of engagement and education about the post-sepsis care program’s value and effectiveness, possible patient distrust of STAR and/or of health care, and patients’ lack of access to community resources could be potential barriers to its implementation. Together these findings point to the necessity of stakeholder buy-in for overcoming inner and outer setting barriers to implementation. They also suggest successful championing of STAR should extend beyond navigator efforts alone and include system and care team participation as well.
Third, our study found the STAR program’s fit with the LHS’s inner setting to be informative for our planning. Participants reported STAR’s compatibility with the structural characteristics and implementation climate of the LHS to likely be important considerations for implementation. At the time of this study, virtual hospital care and other telehealth programs were highly active within the LHS, in part related to the need for such programs during the surge of the COVID-19 pandemic. Additionally, STAR’s alignment with other sepsis-focused work groups and sepsis champions across the LHS was identified as another possible facilitator for implementation success. We found implementation barriers pertaining to the implementation climate of the LHS’s inner setting as well. Despite acknowledging that the program would likely align with current health system goals, participants cautioned STAR would have to compete with demands for staff time and resources. Decreased organizational capacity for a new program was another potential implementation barrier identified. Participants recommended engaging clinicians about the value and effectiveness of the program to promote support and assuage concerns. These facilitators and barriers suggest health system priorities and routine healthcare practice in the inner setting should be identified and considered carefully when making post-sepsis care program implementation decisions. They also underscore how the inner setting is not simply a background of implementation but can rather serve as an important context in implementation success.
Finally, our study findings highlighted the importance of good communication between the STAR navigator and other stakeholders, including clinicians, patients, caregivers, and family members, for successful implementation. Participants recommended clear and reciprocal communication between STAR navigators and clinicians. Similarly, they advised that navigators attempt to establish good rapport with patients, caregivers, and family members by using effective communication. Several potential implementation barriers related to communication were also reported. Participants discussed underlying patient-facing information and technology gaps that could be potential barriers to communicating with STAR navigators related to digital literacy, health literacy, or a lack of access to technology to participate in STAR. These suggest further study may be recommended to identify other patient-facing environmental conditions, such as social determinants of health, affecting sepsis recovery, as proposed in other’s work [ 10 ]. These points underscore the necessity of both effective communication and communication technology to support telehealth-based sepsis transition and recovery intervention implementation.
Study limitations
A limitation of the present research is that it is based on interviews with a small sample of employees at one, albeit large, health system. Although we carefully sampled stakeholders based on their awareness, organizational authority, and involvement in activities related to implementation of a post-sepsis care intervention at study facilities, these perspectives may not necessarily reflect the experience of all facilities within the same LHS or outside of the LHS. A second limitation is that patients were not included as participants at pre-implementation, despite later finding several facilitators and barriers related to patient needs. Third, we deliberately used the CFIR, and included all domains, to inform our approach to data collection and analysis due to its comprehensive assessment of implementation determinants and well-described associations with implementation strategies. However, using CFIR alone may have limited collection of other relevant contextual factors not represented by CFIR or specifically incorporated in our data collection. Our analysis strategy that combined inductive and deductive methods did allow for capture of themes outside of CFIR, if new information emerged from participant responses. Finally, our analysis strategy focused specifically on identifying key individual determinants; thus, additional empirical analyses examining the causal pathways or combinations of contextual factors may be helpful to advance evidence and guide decision making regarding effective implementation strategies tailored to complex determinants.
Our findings demonstrate effective use of the CFIR as a robust framework to examine facilitators and barriers for pre-implementation planning of post-sepsis care programs within diverse hospital and community settings in a large LHS. The comprehensive structure of the framework enabled researchers to identify key implementation determinants across external-, internal-, and program-level domains, plan for organizational change associated with implementation, and engage with relevant stakeholders. Conducting a structured pre-implementation evaluation helps researchers design with implementation in mind prior to effectiveness studies and should be considered a key component of Type I hybrid trials when feasible.
Availability of data and materials
The datasets generated and analyzed during the study are not available due to participant privacy and ethics restrictions, but the codebook and data collection tools may be available from the corresponding author on reasonable request.
Abbreviations
Sepsis transition and recovery
Learning health system
Consolidated framework for implementation research
Evidence-based practices
Buchman T, Simpson SQ, Sciarretta KL, et al. Sepsis among medicare beneficiaries: 1. The burdens of sepsis, 2012–2018*. Crit Care Med. 2020;48(3):276–88. https://doi.org/10.1097/CCM.0000000000004224 . Published Online First: Epub Date.
Article PubMed PubMed Central Google Scholar
Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200–11. https://doi.org/10.1016/S0140-6736(19)32989-7 . Published Online First: Epub Date.
W. MK, Marc R. Most Frequent Principal Diagnoses for Inpatient Stays in U.S. Hospitals, 2018. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs 2021. 2021. https://www.ncbi.nlm.nih.gov/books/NBK573113/ .
Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Crit Care Med. 2018;46(6):997–1000. https://doi.org/10.1097/ccm.0000000000003119 . Published Online First: Epub Date.
Article PubMed Google Scholar
Rhee C, Dantes R, Epstein L, et al. Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009–2014. JAMA. 2017;318(13):1241–9. https://doi.org/10.1001/jama.2017.13836 . Published Online First: Epub Date.
Mostel Z, Perl A, Marck M, et al. Post-sepsis syndrome - an evolving entity that afflicts survivors of sepsis. Molecular medicine (Cambridge, Mass.) 2019;26(1):6. https://doi.org/10.1186/s10020-019-0132-z . Published Online First: Epub Date.
Farrah K, McIntyre L, Doig CJ, et al. Sepsis-associated mortality, resource use, and healthcare costs: a propensity-matched cohort study. Crit Care Med. 2021;49(2):215–27. https://doi.org/10.1097/ccm.0000000000004777 . Published Online First: Epub Date.
Prescott HC, Angus DC. Enhancing recovery from sepsis: a review. JAMA. 2018;319(1):62–75. https://doi.org/10.1001/jama.2017.17687 . Published Online First: Epub Date.
Shankar-Hari M, Saha R, Wilson J, et al. Rate and risk factors for rehospitalisation in sepsis survivors: systematic review and meta-analysis. Intensive Care Med. 2020;46(4):619–36. https://doi.org/10.1007/s00134-019-05908-3 . Published Online First: Epub Date.
Hilton RS, Hauschildt K, Shah M, Kowalkowski M, Taylor S. The assessment of social determinants of health in postsepsis mortality and readmission: a scoping review. Crit Care Explor. 2022;4(8):e0722. https://doi.org/10.1097/cce.0000000000000722 . Published Online First: Epub Date.
Prescott HC, Iwashyna TJ, Blackwood B, et al. Understanding and enhancing sepsis survivorship. Priorities for research and practice. Am J Respir Crit Care Med. 2019;200(8):972–81. https://doi.org/10.1164/rccm.201812-2383CP . Published Online First: Epub Date.
Huang CY, Daniels R, Lembo A, et al. Life after sepsis: an international survey of survivors to understand the post-sepsis syndrome. Int J Qual Health Care. 2019;31(3):191–8. https://doi.org/10.1093/intqhc/mzy137 . Published Online First: Epub Date.
Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–247. https://doi.org/10.1007/s00134-021-06506-y . published Online First: Epub Date.
Taylor SP, Chou SH, Sierra MF, et al. Association between adherence to recommended care and outcomes for adult survivors of sepsis. Ann Am Thorac Soc. 2020;17(1):89–97. https://doi.org/10.1513/AnnalsATS.201907-514OC . published Online First: Epub Date.
Watson MA, Anderson C, Karlic KJ, et al. Receipt of recovery-oriented care practices during hospitalization for sepsis. Crit Care Explor. 2022;4(9):e0766. https://doi.org/10.1097/cce.0000000000000766 . Published Online First: Epub Date.
Taylor SP, Murphy S, Rios A, et al. Effect of a multicomponent sepsis transition and recovery program on mortality and readmissions after sepsis: the improving morbidity during post-acute care transitions for sepsis randomized clinical trial. Crit Care Med. 2022;50(3):469–79. https://doi.org/10.1097/ccm.0000000000005300 . Published Online First: Epub Date.
Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Effective clinical practice : ECP. 1998;1(1):2–4.
CAS PubMed Google Scholar
Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095–107. https://doi.org/10.1001/jamainternmed.2014.1608 . Published Online First: Epub Date.
Kowalkowski M, Eaton T, McWilliams A, et al. Protocol for a two-arm pragmatic stepped-wedge hybrid effectiveness-implementation trial evaluating Engagement and Collaborative Management to Proactively Advance Sepsis Survivorship (ENCOMPASS). BMC Health Serv Res. 2021;21(1):544. https://doi.org/10.1186/s12913-021-06521-1 . Published Online First: Epub Date.
Hamilton AB, Finley EP. Qualitative methods in implementation research: an introduction. Psychiatry Res. 2019;280:112516. https://doi.org/10.1016/j.psychres.2019.112516 . Published Online First: Epub Date.
Alley ZM, Chapman JE, Schaper H, Saldana L. The relative value of Pre-Implementation stages for successful implementation of evidence-informed programs. Implement Sci. 2023;18(1):30. https://doi.org/10.1186/s13012-023-01285-0 . Published Online First: Epub Date.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science : IS. 2009;4:50. https://doi.org/10.1186/1748-5908-4-50
Kirk MA, Kelley C, Yankey N, Birken SA, Abadie B, Damschroder L. A systematic review of the use of the Consolidated Framework for Implementation Research. Implement Sci. 2016;11:72. https://doi.org/10.1186/s13012-016-0437-z . Published Online First: Epub Date.
Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21. https://doi.org/10.1186/s13012-015-0209-1 . Published Online First: Epub Date.
Birken SA, Powell BJ, Presseau J, et al. Combined use of the Consolidated Framework for Implementation Research (CFIR) and the Theoretical Domains Framework (TDF): a systematic review. Implement Sci. 2017;12(1):2. https://doi.org/10.1186/s13012-016-0534-z . Published Online First: Epub Date.
King DK, Shoup JA, Raebel MA, et al. Planning for implementation success using RE-AIM and CFIR Frameworks: a qualitative study. Front Public Health. 2020;8:59. https://doi.org/10.3389/fpubh.2020.00059 . Published Online First: Epub Date.
Dolansky MA, Pohnert A, Ball S, McCormack M, Hughes R, Pino L. Pre-Implementation of the age-friendly health systems evidence-based 4ms framework in a multi-state convenient care practice. Worldviews on evidence-based nursing. 2021;18(2):118–28. https://doi.org/10.1111/wvn.12498 . Published Online First: Epub Date.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51. https://doi.org/10.1097/acm.0000000000000388 . Published Online First: Epub Date.
Schiller C, Winters M, Hanson HM, Ashe MC. A framework for stakeholder identification in concept mapping and health research: a novel process and its application to older adult mobility and the built environment. BMC Public Health. 2013;13:428. https://doi.org/10.1186/1471-2458-13-428 . Published Online First: Epub Date.
Research CRT-CfCM. CFIR Interview guide tool. Secondary CFIR interview guide tool 2019. https://cfirguide.org/guide/app/#/ .
McGrath C, Palmgren PJ, Liljedahl M. Twelve tips for conducting qualitative research interviews. Med Teach. 2019;41(9):1002–6. https://doi.org/10.1080/0142159x.2018.1497149 . Published Online First: Epub Date.
Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health services research. 2007;42(4):1758–72. https://doi.org/10.1111/j.1475-6773.2006.00684.x . Published Online First: Epub Date.
Research CRT-CfCM. CFIR Codebook Template. Secondary CFIR Codebook Template 2019. https://cfirguide.org/tools/tools-and-templates/ .
Baker R, Camosso-Stefinovic J, Gillies C, et al. Tailored interventions to overcome identified barriers to change: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2010;3:Cd005470. https://doi.org/10.1002/14651858.CD005470.pub2 . Published Online First: Epub Date.
Article Google Scholar
Mittman BS. Implementation science in health care. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and implementation research in health: translating science to practice. New York: Oxford; 2012. p. 400–18.
Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implementation Sci. 2022;17(1):75. https://doi.org/10.1186/s13012-022-01245-0 . Published Online First: Epub Date.
Piper KN, Brown LL, Tamler I, Kalokhe AS, Sales JM. Application of the consolidated framework for implementation research to facilitate delivery of trauma-informed HIV care. Ethn Dis. 2021;31(1):109–18. https://doi.org/10.18865/ed.31.1.109 . Published Online First: Epub Date.
Ahmed SI, Khowaja BMH, Barolia R, et al. Adapting the FAST-M maternal sepsis intervention for implementation in Pakistan: a qualitative exploratory study. BMJ Open. 2022;12(9):e059273. https://doi.org/10.1136/bmjopen-2021-73 . eCollection 2022.
Fokuo JK, McCuistian CL, Masson CL, et al. Pre-implementation assessment of tobacco cessation interventions in substance use disorder residential programs in California. Subst Use Misuse. 2022;57(9):1345–55. https://doi.org/10.1080/10826084.2022.2079139 . Published Online First: Epub Date.
Download references
Acknowledgements
The authors would like to thank all of the study participants for sharing their time and insights.
Research reported in this publication was supported by the National Institute Of Nursing Research of the National Institutes of Health under Award Number R01NR018434. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and affiliations.
Center for Health System Sciences, Atrium Health, 1300 Scott Ave, Charlotte, NC, 28203, USA
Tara A. Eaton & Marc Kowalkowski
Department of Internal Medicine, Medical Center Boulevard, Wake Forest University School of Medicine, Winston-Salem, NC, 27157, USA
Marc Kowalkowski
Department of Community Health, Atrium Health, 4135 South Stream Blvd, Charlotte, NC, 28217, USA
Department of Family Medicine, Atrium Health, 2001 Vail Ave., Suite 400B, Charlotte, NC, 28207, USA
Center for Outcomes Research and Evaluation, Yale New Haven Health, 195 Church Street, New Haven, CT, 06510, USA
Katherine O’Hare
Department of Internal Medicine, Taubman Center, University of Michigan, 1500 East Medical Center Drive, 3110SPC 5368, Ann Arbor, MI, 48109-5368, USA
Stephanie P. Taylor
You can also search for this author in PubMed Google Scholar
Contributions
TE, ST, MK, and HT contributed to the design of the study. TE, ST, MK, RB and KO contributed to the acquisition of study data. TE, RB, KO, and HT analyzed the data. TE, ST, and MK contributed to the interpretation of the data. TE, ST, MK, RB, and HT drafted the manuscript. All authors critically revised the intellectual content of the manuscript. All authors approved the final manuscript.
Corresponding author
Correspondence to Tara A. Eaton .
Ethics declarations
Ethics approval and consent to participate.
This study has been approved to be conducted on behalf of all trial sites with a waiver of signed informed consent by the Advarra Institutional Review Board (#Pro00036873) on June 26, 2019. Participants were all given a study information sheet that was reviewed with them prior to their participation. All study methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Eaton, T.A., Kowalkowski, M., Burns, R. et al. Pre-implementation planning for a sepsis intervention in a large learning health system: a qualitative study. BMC Health Serv Res 24 , 996 (2024). https://doi.org/10.1186/s12913-024-11344-x
Download citation
Received : 18 August 2023
Accepted : 23 July 2024
Published : 28 August 2024
DOI : https://doi.org/10.1186/s12913-024-11344-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sepsis (33)
- Pre-Implementation (16)
- Qualitative (10)
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 26 August 2024
Paramedics’ experiences and observations: work-related emotions and well-being resources during the initial months of the COVID-19 pandemic—a qualitative study
- Henna Myrskykari 1 , 2 &
- Hilla Nordquist 3
BMC Emergency Medicine volume 24 , Article number: 152 ( 2024 ) Cite this article
91 Accesses
1 Altmetric
Metrics details
As first responders, paramedics are an extremely important part of the care chain. COVID-19 significantly impacted their working circumstances. We examined, according to the experiences and observations of paramedics, (1) what kinds of emotions the Emergency Medical Service (EMS) personnel experienced in their new working circumstances, and (2) what work-related factors became resources for the well-being of EMS personnel during the initial months of the COVID-19 pandemic.
This qualitative study utilized reflective essay material written by experienced, advanced-level Finnish paramedics ( n = 30). The essays used in this study were written during the fall of 2020 and reflected the period when Finland had declared a state of emergency (on 17.3.2020) and the Emergency Powers Act was implemented. The data was analyzed using an inductive thematic analysis.
The emotions experienced by the EMS personnel in their new working circumstances formed three themes: (1) New concerns arose that were constantly present; (2) Surviving without proper guidance; and (3) Rapidly approaching breaking point. Three themes were formed from work-related factors that were identified as resources for the well-being of the EMS personnel. These were: (1) A high level of organizational efficiency was achieved; (2) Adaptable EMS operations; and (3) Encouraging atmosphere.
Conclusions
Crisis management practices should be more attentive to personnel needs, ensuring that managerial and psychological support is readily available in crisis situations. Preparedness that ensures effective organizational adaptation also supports personnel well-being during sudden changes in working circumstances.
Peer Review reports
At the onset of the COVID-19 pandemic, healthcare personnel across the globe faced unprecedented challenges. As initial responders in emergency healthcare, paramedics were quickly placed at the front lines of the pandemic, dealing with a range of emergencies in unpredictable conditions [ 1 ]. The pandemic greatly changed the everyday nature of work [ 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 ]. Those working on the front line were suddenly forced to adjust to personal protective equipment (PPE) requirements [ 9 , 10 ] and rapidly changing instructions that caused significant adjustments to their job description [ 11 , 12 ]. For instance, it has been reported that during the initial stages of the COVID-19 pandemic, Emergency Medical Services (EMS) personnel, including paramedics working in prehospital emergency care, experienced a significant increase in stress [ 10 , 13 ] due to several reasons, such as the lack of protection and support, increased demands, lack of personnel, fear of exposure to COVID-19 during missions, concerns of spreading the virus to family members, and frustration over quickly changing work policies [ 11 , 14 , 15 ].
With the unprecedented challenges posed by the COVID-19 pandemic, some research has been directed toward identifying available resources that help in coping with such situations. For example, Sangal et al. [ 15 ] underscored the association between effective communication and reduced work stress and burnout, and emphasized the critical need for two-way communication, consistent messaging, and the strategic consolidation of information prior to its dissemination. In parallel, Dickson et al. [ 16 ] highlight the pivotal role of leadership strategies in fostering a healthful work environment. These strategies include being relationally engaging, visibly present, open, and caring for oneself and others, while embodying core values such as compassion, empathy, courage, and authenticity. Moreover, Awais et al. [ 14 ] identify essential measures to reduce mental distress and support EMS personnel’s overall well-being in pandemic conditions, such as by providing accessible mental health and peer support, ensuring a transparent information flow, and the implementation of clear, best-practice protocols and guidelines. As a lesson learned from COVID-19, Kihlström et al. (2022) add that crisis communication, flexible working conditions, compensation, and allowing for mistakes should be part of crisis management. They also emphasize the importance of psychological support for employees. [ 12 ]
Overall, the COVID-19 pandemic had a multifaceted impact on EMS personnel, highlighting the necessity for comprehensive support and resilience strategies to safeguard their well-being [ 11 , 17 , 18 ] alongside organizational functions [ 12 , 19 ]. For example, in Finland, it has been noted in the aftermath of COVID-19 that the availability and well-being of healthcare workers are key vulnerabilities of the resilience of the Finnish health system [ 12 ]. Effective preparedness planning and organizational resilience benefit from learning from past events and gaining a deeper understanding of observations across different organizational levels [ 12 , 19 , 20 ]. For these reasons, it is important to study how the personnel experienced the changing working circumstances and to recognize the resources, even unexpected ones, that supported their well-being during the initial phase of the COVID-19 pandemic [ 12 , 19 ].
The aim of this study was to examine the emotions experienced and the resources identified as supportive of work well-being during the initial months of the COVID-19 pandemic, from the perspective of the paramedics. Our research questions were: According to the experiences and observations of paramedics, (1) what kinds of emotions did the EMS personnel experience in the new working circumstances, and (2) what work-related factors became resources for the well-being of EMS personnel during the initial months of the COVID-19 pandemic? In this study, emotions are understood as complex responses involving psychological, physiological, and behavioral components, triggered by significant events or situations [ 21 ]. Resources are understood as physical, psychological, social, or organizational aspects of the work that help achieve work goals, reduce demands and associated costs [ 22 ].
Materials and methods
This qualitative study utilized reflective essay material written in the fall of 2020 by experienced, advanced-level paramedics who worked in the Finnish EMS during the early phase of the pandemic, when Finland had declared (March 17, 2020 onward) a state of emergency and implemented the Emergency Powers Act. This allowed for new rules and guidelines from the government to ensure the security of healthcare resources. Some work rules for healthcare personnel changed, and non-urgent services were limited.
Data collection procedures
This study is part of a broader, non-project-based research initiative investigating the work well-being of paramedics from various perspectives, and the data was collected for research purposes from this standpoint. The data collection for this study was conducted at the South-Eastern Finland University of Applied Sciences as part of the Current Issues in EMS Management course. The course participants were experienced, advanced-level Finnish paramedics who were students of the master’s degree program in Development and Management of Emergency Medical Services. A similar data collection method has been utilized in other qualitative studies [for example, 23 , 24 ].
The South-Eastern Finland University of Applied Sciences granted research permission for the data collection on August 20, 2020. The learning platform “Learn” (an adapted version of Moodle [ 25 ]) was used to gather the data. A research notice, privacy statement, and essay writing instructions were published on the platform on August 21, 2020. The paramedics were asked to write about their own experiences and observations regarding how the state of emergency impacted the work well-being of EMS personnel. They were instructed not to use references but only their own reflections. Three guiding questions were asked: “What kind of workloads did EMS personnel experience during the state of emergency?” “How has this workload differed from normal conditions?” and “What effects did this workload have on the well-being of the EMS personnel?”. The assignment did not refer solely to paramedics because the EMS field community may also include individuals with other titles (such as EMS field supervisors or firefighters performing prehospital emergency care); hence the term “EMS personnel” was used.
The essay was part of the mandatory course assignments, but submitting it for research purposes was voluntary. The paramedics were informed that their participation in the study would not affect their course evaluations. They had the freedom to decline, remove parts of, or withdraw the essay before analysis. None of the paramedics exercised these options. They were also informed that the last author removes any identifying details (such as names, places, and organizational descriptions that could reveal their workplace) before sharing the data with other, at the time unnamed, researchers. The last author (female) is a senior researcher specializing in EMS and work well-being topics, a principal lecturer of the respective course, and the head of the respective master’s program, and familiar to all of them through their studies. The paramedics were aware that the essays were graded by the last author on a pass/fail scale as part of the course assessment. However, comprehensive and well-reasoned reflections positively influenced the course grade. The evaluation was not part of this study. The paramedics had the opportunity to ask further questions about the study directly from the last author during and after the essay writing process and the course.
The paramedics wrote the essays between August 23, 2020, and November 30, 2020. Thirty-two paramedics (out of 39) returned their essays using the Learn platform during this timeframe. Thus, seven of the course completions were delayed, and the essays written later were no longer appropriate to include in the data due to the time elapsed since the initial months of the COVID-19 pandemic.
All 32 gave their informed consent for their essays to be included in the study. Essays written by paramedics who had not actively participated in EMS field work during exceptional circumstances were excluded from the material ( n = 2), because they wrote the essay from a different perspective, as they could not reflect on their own experiences and observations. Thus, a total of 30 essays were included in the study. The total material was 106 pages long and comprised 32,621 words in Finnish.
Study participants
Thirty advanced-level paramedics from Finland participated in this study. They all had a bachelor’s degree in emergency care or nursing with additional emergency care specialization. At the time of the study, they were pursuing their master’s studies. Thirteen of them were women, and seventeen were men. The average age of the participants was 33.5 years among women and 35.9 years among men. Women had an average of 8.7 years of work experience, and men had 8.8 years. All the participating paramedics worked in EMS in different areas across Finland (except northern Finland) during their studies and the early phase of the pandemic.
Data analysis
The data was analyzed with a thematic analysis following the process detailed by Braun & Clarke [ 26 ]. First, the two researchers thoroughly familiarized themselves with the data, and the refined aim and research questions of the study were formulated inductively in collaboration based on the content of the data (see [ 26 ], page 84). After this, a thorough coding process was mainly carried out by the first author (female), who holds a master’s degree, is an advanced-level paramedic who worked in EMS during the pandemic, and at the time of the analysis was pursuing her doctoral studies in a different subject area related to EMS. Generating the initial codes involved making notes of interesting features of anything that stood out or seemed relevant to the research question systematically across the entire dataset. During this process, the original paragraphs and sentences were copied from the essay material into a table in Microsoft Word, with each research question in separate documents and each paragraph or sentence in its own row. The content of these data extracts was then coded in the adjacent column, carefully preserving the original content but in a more concise form. Then, the content was analyzed, and codes were combined to identify themes. After that, the authors reviewed the themes together by moving back and forth between the original material, the data in the Word documents, and the potential themes. During this process, the authors worked closely and refined the themes, allowing them to be separated and combined into new themes. For example, emotions depicting frustration and a shift to indifference formed their own theme in this kind of process. Finally, the themes were defined into main, major and minor themes and named. In the results, the main themes form the core in response to the research questions and include the most descriptions from the data. The major themes are significant but not as central as the main themes. Major themes provide additional depth and context to the results. One minor theme was formed as the analysis process progressed, and it provided valuable insights and details that deepened the response to the research question. All the coded data was utilized in the formed themes. The full content of the themes is reported in the Results section.
The emotions experienced by the EMS personnel in their new working circumstances formed three themes: New concerns arose that were constantly present (main theme); Surviving without proper guidance (major theme); and Rapidly approaching breaking point (major theme) (Fig. 1 ). Work-related factors identified as resources for the well-being of EMS personnel formed three themes: A high level of organizational efficiency was achieved (main theme); Adaptable EMS operations (major theme); and Encouraging atmosphere (minor theme) (Fig. 2 ).
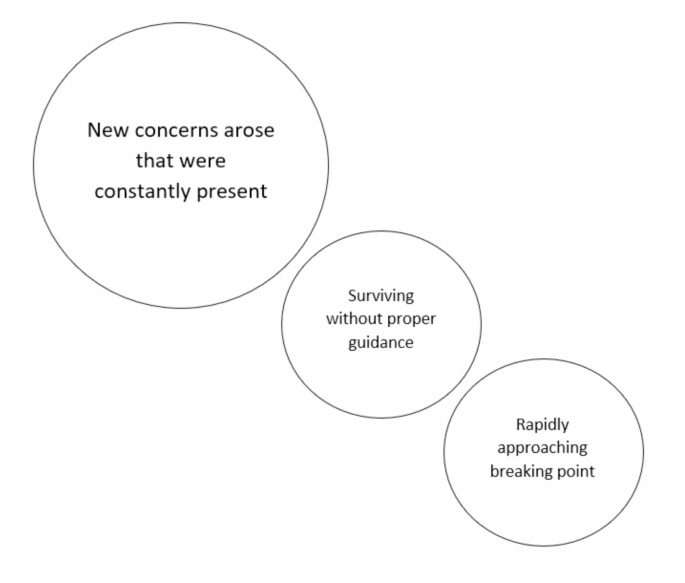
Emotions experienced by the EMS personnel in their new working circumstances
Main theme: New concerns arose that were constantly present
The main theme included several kinds of new concerns. In the beginning, the uncertainty about the virus raised concerns about work safety and the means to prevent the spread of the disease. The initial lack of training and routines led to uncertainty. In addition, the decrease in the number of EMS missions raised fears of units being reduced and unilateral decisions by the management to change the EMS personnel’s work responsibilities. The future was also a source of uncertainty in the early stages. For example, the transition to exceptional circumstances, concerns about management and the supervisors’ familiarity with national guidelines and lack of information related to sickness absence procedures, leave, personal career progression, and even the progress of vaccine development, all contributed to this feeling of uncertainty. The initial uncertainty was described as the most challenging phase, but the uncertainty was also described as long-lasting.
Being on the front line with an unknown, potentially dangerous, and easily transmissible virus caused daily concerns about the personnel’s own health, especially when some patients hid their symptoms. The thought of working without proper PPE was frightening. On the other hand, waiting for a patient’s test result was stressful, as it often resulted in many colleagues being quarantined. A constant concern for the health of loved ones and the fear of contracting the virus and unknowingly bringing it home or transmitting it to colleagues led the EMS personnel to change their behavior by limiting contact.
Being part of a high-risk group , I often wondered , in the case of coronavirus , who would protect me and other paramedics from human vanity and selfishness [of those refusing to follow the public health guidelines]? (Participant 25)
The EMS personnel felt a weight of responsibility to act correctly, especially from the perspective of keeping their skills up to date. The proper selection of PPE and aseptic procedures were significant sources of concern, as making mistakes was feared to lead to quarantine and increase their colleagues’ workloads. At the same time, concerns about the adequacy of PPE weighed on the personnel, and they felt pressure on this matter to avoid wastage of PPEs. The variability in the quality of PPE also caused concerns.
Concerns about acting correctly were also tied to ethical considerations and feelings of inadequacy when the personnel were unable to explain to patients why COVID-19 caused restrictions on healthcare services. The presence of students also provoked such ethical concerns. Recognizing patients’ symptoms correctly also felt distressing due to the immense responsibility. This concern was also closely tied to fear and even made some question their career choices. The EMS personnel were also worried about adequate treatment for the patients and sometimes felt that the patients were left alone at home to cope. A reduction in patient numbers in the early stages of the pandemic raised concerns about whether acutely ill individuals were seeking help. At the same time, the time taken to put on PPE stressed the personnel because it increased delays in providing care. In the early phase of the pandemic, the EMS personnel were stressed that patients were not protected from them.
I’m vexed in the workplace. I felt it was immediately necessary to protect patients from us paramedics as well. It wasn’t specifically called for , mostly it felt like everyone had a strong need to protect themselves. (Participant 30)
All these concerns caused a particularly heavy psychological burden on some personnel. They described feeling more fatigued and irritable than usual. They had to familiarize themselves with new guidelines even during their free time, which was exhausting. The situation felt unjust, and there was a looming fear of the entire healthcare system collapsing. COVID-19 was omnipresent. Even at the base station of the EMS services, movement was restricted and social distancing was mandated. Such segregation, even within the professional community, added to the strain and reduced opportunities for peer support. The EMS personnel felt isolated, and thoughts about changing professions increased.
It was inevitable that the segregation of the work community would affect the community spirit , and a less able work community has a significant impact on the individual level. (Participant 8)
Major theme: Surviving without proper guidance
At the onset of the pandemic, the job description of the EMS personnel underwent changes, and employers could suddenly relocate them to other work. There was not always adequate support for familiarizing oneself with the new roles, leading to a feeling of loss of control. The management was described as commanding and restricting the personnel’s actions. As opportunities to influence one’s work diminished, the sense of job satisfaction and motivation decreased.
Some felt that leadership was inadequate and neglectful, especially when the leaders switched to remote work. The management did not take the situation seriously enough, leaving the EMS personnel feeling abandoned. The lack of consistent leadership and failure to listen to the personnel caused dissatisfaction and reduced occupational endurance. In addition, the reduced contact with colleagues and close ones reduced the amount of peer support. The existing models for psychological support were found to be inadequate.
Particularly in the early stages, guidelines were seen as ambiguous and deficient, causing frustration, irritation, and fear. The guidelines also changed constantly, even daily, and it was felt that the information did not flow properly from the management to the personnel. Changes in protection recommendations also led to skepticism about the correctness of the national guidance, and the lack of consistent guidelines perplexed the personnel. Internalizing the guidelines was not supported adequately, but the necessity to grasp new information was described as immense and cognitively demanding.
At times , it felt like the work was a kind of survival in a jungle of changing instructions , one mission at a time. (Participant 11)
Major theme: Rapidly approaching breaking point
Risking one’s own health at work caused contentious feelings while concurrently feeling angry that management could work remotely. The arrogant behavior of people toward COVID-19 left them frustrated, while the EMS personnel had to limit their contacts and lost their annual leave. There were fears about forced labor.
Incomplete and constantly changing guidelines caused irritation and indifference, as the same tasks had to be performed with different levels of PPE within a short time. Some guidelines were difficult to comply with in practice, which was vexing.
Using a protective mask was described as distressing, especially on long and demanding missions. Communication and operation became more difficult. Some described frustration with cleaning PPE meant for single use.
Ensuring the proper implementation of a work pair’s aseptic and equipment maintenance was burdensome, and explaining and repeating guidelines was exhausting. A feeling of indifference was emphasized toward the end of a long shift.
After the initial stage, many began to slip with the PPE guidelines and found the instructions excessive. COVID-19 information transmitted by the emergency center lost its meaning, and instructions were left unheeded, as there was no energy to believe that the patient would have COVID-19, especially if only a few disease cases had been reported in their area.
It was disheartening to hear personnel being labeled as selfish for demanding higher pay during exceptional circumstances. This lack of recognition eroded professionalism and increased thoughts of changing professions.
However , being a doormat and a human toilet , as well as a lack of appreciation , undermines my professionalism and the prolonged situation has led me to seriously consider a different job , where values other than dedication and constant flexibility carry weight. I have heard similar thoughts from other colleagues. None of us do this for money. (Participant 9)
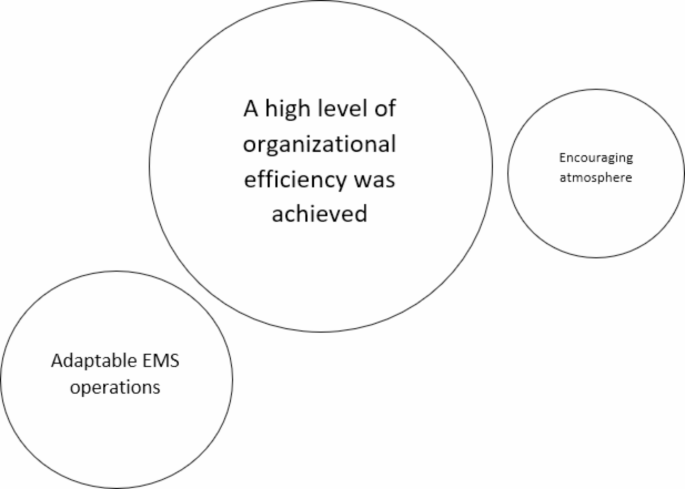
Work-related factors identified as resources for the well-being of EMS personnel
Main theme: A high level of organizational efficiency was achieved
The main theme held several different efficient functions. In the early stages of the pandemic, some felt that the information flow was active. Organizations informed the EMS personnel about the disease, its spread, and its impact on the workplace and emergency care activities.
Some felt that managers were easily accessible during the pandemic, at least remotely. Some managers worked long days to be able to support their personnel.
The response to hate and uncertainty was that one of the supervisors was always present in the morning and evening meetings. Supervisors worked long hours so as to be accessible via remote access. (Participant 26)
The organizations took effective steps to control infections. Quick access to COVID-19 tests, clear guidelines for taking sick leave, and permission to take sick leave with a low threshold were seen as positive things. The consideration of personnel belonging to risk groups by moving them to other work tasks was also perceived as positive. In addition, efforts were made to prevent the emergence of infection chains by isolating EMS personnel in their own social facilities.
Established guidelines, especially on the correct use of protective measures, made it easier to work. Some mentioned that the guidelines were available in ambulances and on phones, allowing the protection guidelines to be checked before going on a mission.
The employers took into account the need for psychological support in a diverse manner. Some organizations provided psychological support such as peer debriefing activities, talking therapy with mental health professionals, actively inquiring about their personnel’s feelings, and training them as support workers. The pandemic situation also caused organizations to create their own standard operating models to decrease mental load.
Fortunately , the problem has now been addressed actively , as a peer-to-peer defusing model was built up at our workplace during the crisis , and group defusing has started , the purpose of which is to lighten the work-related mental load. (Participant 3)
Major theme: Adaptable EMS operations
There were several different resources that clarified mission activities. The amount of protective and cleaning equipment was ramped up, and the treatment equipment was quickly updated to meet the demands brought about by the pandemic and to enable safety distances for the EMS personnel. In addition, various guidelines were amended to reduce exposure. For example, personnel on the dedicated COVID-19 ambulances were separated to work without physical contact with others, and field supervisors joined the EMS missions less often than before. Moreover, people at the scene were contacted by phone in advance to ensure that there would be no exposure risk, which also allowed other occupational safety risks to be identified. New practices resulted from the pandemic, such as cleaning communication equipment during shift changes and regularly using PPE with infected patients. All of these were seen as positive resources for efficient work.
At the end of each shift , all keys , telephones , etc., were cleaned and handed over to the next shift. This practice was not previously established in our area , but this will become a permanent practice in the future and is perceived by everyone in our work community as a positive thing. (Participant 10)
Some stated that access to PPE was sufficient, especially in areas where the number of COVID-19 infections was low. PPE was upgraded to make it easier to wear. Further, organizations acquired a variety of cleaning equipment to speed up the disinfection of ambulances.
Organizations hired more employees to enable leave and the operation of dedicated COVID-19 ambulances. The overall number of ambulances was also increased. Non-urgent missions were handled through enhanced phone services, reducing the unnecessary exposure of EMS personnel to COVID-19.
Five extra holiday substitutes were hired for EMS so that the employer could guarantee the success of agreed leave , even if the Emergency Preparedness Act had given them opportunities to cancel or postpone it. (Participant 12)
Minor theme: Encouraging atmosphere
Peer support from colleagues, a positive, comfortable, pleasant work environment, and open discussion, as well as smooth cooperation with other healthcare employees were felt to be resources for work well-being by reducing the heavy workload experienced. Due to the pandemic, the appreciation of healthcare was felt to increase slightly, which was identified as a resource.
One factor affecting resilience in the healthcare sector is certainly that in exceptional circumstances , visibility and appreciation have somewhat increased. (Participant 23)
This study examined, according to the experiences and observations of paramedics, (1) what kinds of emotions the Emergency Medical Service (EMS) personnel experienced in their new working circumstances, and (2) what work-related factors became resources for the well-being of EMS personnel during the initial months of the COVID-19 pandemic. Each research question was answered with three themes.
Previous studies have shown that the pandemic increased the workload of paramedics, prompting changes in their operating models and the function of EMS to align with new pandemic-related requirements [ 9 , 27 ]. Initially, the paramedics in the current study described facing unclear and deficient guidelines and feeling obligated to follow instructions without adequate support to internalize them. Constantly changing instructions were linked to negative emotions in various ways. Moreover, the overwhelming flood of information was heavily connected to this, although the information flow was also perceived as a resource, especially when it was timely and well-structured. The study by Sangal et al. [ 15 ] has raised similar observations and points out the importance of paying special attention to the personnel working in the frontline, as in EMS, who might be more heavily impacted by too much information and anxiety about it. They also discovered that three factors are crucial for addressing the challenges of information overload and anxiety: consolidating information before distributing it, maintaining consistent communication, and ensuring communication is two-way. McAlearney et al. [ 11 ] found that first responders, including EMS personnel, reported frustration regarding COVID-19 information because of inconsistencies between sources, misinformation on social media, and the impact of politics. A Finnish study also recognized that health systems were not sufficiently prepared for the flood of information in the current media environment [ 12 ]. Based on these previous results and our findings, it can be concluded that proper implementation of crisis communication should be an integral part of organizations’ preparedness in the future, ensuring that communication effectively supports employee actions in real-life situations. Secondly, this topic highlights the need for precise guidelines and their implementation. With better preparedness, similar chaos could be avoided in the future [ 17 ].
Many other factors also caused changes in work. The EMS mission profile changed [ 3 , 4 , 5 , 6 ], where paramedics in this study saw concerns. To prevent infection risk, the number of pre-arrival calls increased [ 7 ], the duration of EMS missions increased [ 8 , 9 ], and the continuous use of PPE and enhanced hygiene standards imposed additional burdens [ 9 , 10 ]. In Finland, there was no preparedness for the levels of PPE usage required in the early stages of the pandemic [ 12 ]. In this study, paramedics described that working with potentially inadequate PPE caused fear and frustration, which was increased by a lack of training, causing them to feel a great deal of responsibility for acting aseptically and caring for patients correctly. Conversely, providing adequate PPE, information and training has been found to increase the willingness to work [ 28 ] and the sense of safety in working in a pandemic situation [ 29 ], meaning that the role of precise training, operating instructions and leadership in the use of PPE is emphasized [ 30 ].
The paramedics in this study described many additional new concerns in their work, affecting their lives comprehensively. It has been similarly described that the pandemic adversely affected the overall well-being of healthcare personnel [ 31 ]. The restrictions implemented also impacted their leisure time [ 32 ], and the virus caused concerns for their own and their families’ health [ 11 , 28 ]. In line with this, the pandemic increased stress, burnout [ 10 , 33 ], and anxiety among EMS personnel and other healthcare personnel working on the frontline [ 11 , 14 , 34 , 35 ]. These kinds of results underscore the need for adequate guidance and support, a lack of which paramedics reported experiencing in the current study.
Personnel play a crucial role in the efficient operation of an organization and comprise the main identified resource in this study. Previous studies and summaries have highlighted that EMS personnel did not receive sufficient support during the COVID-19 pandemic [ 11 , 14 , 17 , 18 ]. Research has also brought to light elements of adequate support related to the pandemic, such as a review by Dickson et al. [ 16 ] that presents six tentative theories for healthful leadership, all of which are intertwined with genuine encounter, preparedness, and information use. In this current study, the results showed numerous factors related to these contexts that were identified as resources, specifically underlined by elements of caring, effective operational change, knowledge-based actions, and present leadership, similarly described in a study by Eaton-Williams & Williams [ 18 ]. Moreover, the paramedics in our study highlighted the importance of encouragement and identified peer support from colleagues as a resource, which is in line with studies in the UK and Finland [ 12 , 23 , 37 ].
In the early stages of the pandemic, it was noted that the EMS personnel lacked adequate training to manage their mental health, and there was a significant shortage of psychosocial support measures [ 14 ], although easy access to support would have been significant [ 18 ]. In the current study, some paramedics felt that mental health support was inadequate and delayed, while others observed an increase in mental health support during the pandemic, seeing it as an incentive for organizations to develop standard operating models for mental support, for example. This awakening was identified as a resource. This is consistent, as providing psychological support to personnel has been highlighted as a core aspect of crisis management in a Finnish study assessing health system resilience related to COVID-19 [ 12 ]. In a comprehensive recommendation commentary, Isakov et al. [ 17 ] suggest developing a national strategy to improve resilience by addressing the mental health consequences of COVID-19 and other occupational stressors for EMS personnel. This concept, applicable beyond the US, supports the view that EMS organizations are becoming increasingly aware of the need to prepare for and invest in this area.
A fundamental factor likely underlying all the described emotions was that changes in the job descriptions of the EMS personnel due to the pandemic were significant and, in part, mandated from above. In this study, paramedics described feelings of concern and frustration related to these many changes and uncertainties. According to Zamoum and Gorpe (2018), efficient crisis management emphasizes the importance of respecting emotions, recognizing rights, and making appropriate decisions. Restoring trust is a significant challenge in a crisis situation, one that cannot be resolved without complete transparency and open communication [ 38 ]. This perspective is crucial to consider in planning for future preparedness. Overall, the perspective of employee rights and obligations in exceptional circumstances has been relatively under-researched, but in Australia, grounding research on this perspective has been conducted with paramedics using various approaches [ 39 , 40 , 41 ]. The researchers conclude that there is a lack of clarity about the concept of professional obligation, specifically regarding its boundaries, and the issue urgently needs to be addressed by developing clear guidelines that outline the obligation to respond, both in normal day-to-day operations and during exceptional circumstances [ 39 ].
Complex adaptive systems (CAS) theory recognizes that in a resilient organization, different levels adapt to changing environments [ 19 , 20 ]. Barasa et al. (2018) note that planned resilience and adaptive resilience are both important [ 19 ]. Kihlström et al. (2022) note that the health system’s resilience was strengthened by a certain expectation of crisis, and they also recognized further study needs on how effectively management is responding to weak signals [ 12 ]. This could be directly related to how personnel can prepare for future changes. The results of this study revealed many negative emotions related to sudden changes, but at the same time, effective organizational adaptation was identified as a resource for the well-being of EMS personnel. Dissecting different elements of system adaptation in a crisis has been recognized as a highly necessary area for further research [ 20 ]. Kihlström et al. (2022) emphasize the importance of ensuring a healthy workforce across the entire health system. These frameworks suggest numerous potential areas for future research, which would also enhance effective preparedness [ 12 ].
Limitations of the study
In this study, we utilized essay material written in the fall of 2020, in which experienced paramedics reflected on the early stages of the COVID-19 pandemic from a work-oriented perspective. The essays were approached inductively, meaning that they were not directly written to answer our research questions, but the aim and the research questions were shaped based on the content [ 26 ]. The essays included extensive descriptions that aligned well with the aim of this study. However, it is important to remember when interpreting the results that asking specifically about this topic, for instance, in an interview, might have yielded different descriptions. It can be assessed that the study achieved a tentative descriptive level, as the detailed examination of complex phenomena such as emotions and resources would require various methods and observations.
Although the essays were mostly profound, well-thought-out, and clearly written, their credibility [ 42 ] may be affected by the fact that several months had passed between the time the essays were written and the events described. Memories may have altered, potentially influencing the content of the writings. Diary-like material from the very onset of the pandemic might have yielded more precise data, and such a data collection method could be considered in future research on exceptional circumstances.
The credibility [ 42 ] could also have been enhanced if the paramedics who wrote the essays had commented on the results and provided additional perspectives on the material and analysis through a multi-phase data collection process. This was not deemed feasible in this study, mainly because there was a 2.5-year gap between data collection and the start of the analysis. However, this also strengthened the overall trustworthiness of the study, as it allowed the first author, who had worked in prehospital emergency care during the initial phase of the pandemic, to maintain a distance from the subject, and enabled a comparison of our own findings with previously published research that investigated the same period in different contexts. The comparison was made when writing the discussion, with the analysis itself being inductive and following the thematic analysis process described by Braun & Clarke [ 26 ].
When evaluating credibility [ 42 ], it should also be noted that the participants who wrote the essays, i.e., the data for the study, were experienced paramedics but also students and one of the researchers was their principal lecturer. This could potentially limit credibility if the students, for some reason, did not want to produce truthful content for their lecturer to read. However, this risk can be considered small because the essays’ topics did not concern the students’ academic progress, the essays’ content was quite consistent, and the results aligned with other studies. As a strength, it can be considered that the students shared their experiences without holding back, as the thoughts were not for workplace use, and they could trust the data privacy statement.
To enhance transferability [ 42 ], the context of the study was described in detail, highlighting the conditions prevailing in Finnish prehospital emergency care during the early stages of the pandemic. Moreover, including a diverse range of perspectives from paramedics working in different regions of Finland (except Northern Finland) contributes to the transferability of the study, indicating that the results may be applicable and relevant to a wider context beyond a single specific region.
Dependability [ 42 ] was reinforced by the close involvement of two researchers from different backgrounds in the analysis of the material, but a limitation is that no separate analyses were conducted. However, the original data was repeatedly revisited during the analysis, which strengthened the dependability. Moreover, the first author kept detailed notes throughout the analysis process, and the last author supervised the progress while also contributing to the analysis and reporting. The research process is also reported in detail.
This study highlighted numerous, mainly negative emotions experienced by EMS personnel during the initial months of the COVID-19 pandemic due to new working circumstances. At the same time, several work-related factors were identified as resources for their well-being. The findings suggest that crisis management practices should be more attentive to personnel needs, ensuring that personnel have the necessary support, both managerial and psychological, readily available in crisis situations. Effective organizational adaptation in a crisis situation also supports personnel well-being, emphasizing the importance of effective preparedness. Future research should particularly focus on considering personnel well-being as part of organizational adaptation during exceptional circumstances and utilize these findings to enhance preparedness.
Data availability
The datasets generated and analyzed during the current study are not publicly available due to the inclusion of sensitive information and the extent of the informed consent provided by the participants.
Abbreviations
Complex Adaptive Systems (theory)
Coronavirus Disease 2019
Emergency Medical Services
Personal Protective Equipment
United Kingdom
Drennan IR, Blanchard IE, Buick JE. Opportunity for change: is it time to redefine the role of paramedics in healthcare? CJEM. 2021;23(2):139–40. https://doi.org/10.1007/s43678-021-00105-y
Boechler L, Cameron C, Smith JC, Ford-Jones P, Suthers P. Impactful approaches to Leadership on the Front lines of the COVID-19 pandemic: lived experiences of Canadian paramedics. Healthc Q. 2021;24(3):42–7. https://doi.org/10.12927/hcq.2021.26620 .
Article PubMed Google Scholar
Lerner EB, Newgard CD, Mann NC. Effect of the Coronavirus Disease 2019 (COVID-19) pandemic on the U.S. Emergency Medical Services System: a preliminary Report. Acad Emerg Med. 2020;27(8):693–9. https://doi.org/10.1111/acem.14051 .
Article PubMed PubMed Central Google Scholar
O’Connor AW, Hannah HA, Burnor EA, Fukutaki KG, Peterson T, Ballard DW, et al. Emergency Medical Service Utilization and response following COVID-19 emergency and stay-at-home policies: an interrupted time-series analysis. Cureus. 2021;21(11). https://doi.org/10.7759/cureus.19794 .
Azbel M, Heinänen M, Lääperi M, Kuisma M. Effects of the COVID-19 pandemic on trauma-related emergency medical service calls: a retrospective cohort study. BMC Emerg Med. 2021;9(1):102. https://doi.org/10.1186/s12873-021-00495-3 .
Article CAS Google Scholar
Lane DJ, Blanchard IE, Buick JE, Shaw M, McRae AD. Changes in presentation, presenting severity and disposition among patients accessing emergency services during the first months of the COVID-19 pandemic in Calgary, Alberta: a descriptive study. CMAJ Open. 2021;9(2):592–601. https://doi.org/10.9778/cmajo.20200313 .
Article Google Scholar
Shukla V, Lau CSM, Towns M, Mayer J, Kalkbrenner K, Beuerlein S, et al. COVID-19 exposure among First Responders in Arizona. J Occup Environ Med. 2020;62(12):981–5. https://doi.org/10.1097/JOM.0000000000002027 .
Article CAS PubMed Google Scholar
Andrew E, Nehme Z, Stephenson M, Walker T, Smith K. The impact of the COVID-19 pandemic on demand for emergency ambulances in Victoria, Australia. Prehosp Emerg Care. 2021;16:1–7. https://doi.org/10.1080/10903127.2021.1944409 .
Eskol JR, Zegers FD, Wittrock D, Lassen AT, Mikkelsen S. Increased ambulance on-scene times but unaffected response times during the first wave of the COVID-19 pandemic in Southern Denmark. BMC Emerg Med. 2022;9(1):61. https://doi.org/10.1186/s12873-022-00623-7 .
Schumann H, Böckelmann I, Thielmann B. Relaxation and strain among emergency medical service personnel and emergency control center dispatchers during the first two waves of the SARS-CoV-2 pandemic. Med Pr. 2023;15(5):353–62. https://doi.org/10.13075/mp.5893.01401 .
McAlearney AS, Gaughan AA, MacEwan SR, Gregory ME, Rush LJ, Volney J, et al. Pandemic experience of first responders: fear, frustration, and stress. Int J Environ Res Public Health. 2022;13(8):4693. https://doi.org/10.3390/ijerph19084693 .
Kihlström L, Huhtakangas M, Karreinen S, Viita-Aho M, Keskimäki I, Tynkkynen LK. Local cooperation has been the cornerstone: facilitators and barriers to resilience in a decentralized health system during COVID-19 in Finland. J Health Organ Manag. 2022. https://doi.org/10.1108/JHOM-02-2022-0069 .
Hendrickson RC, Slevin RA, Hoerster KD, Chang BP, Sano E, McCall CA, et al. The impact of the COVID-19 pandemic on Mental Health, Occupational Functioning, and Professional Retention among Health Care workers and First Responders. J Gen Intern Med. 2022;37(2):397–408. https://doi.org/10.1007/s11606-021-07252-z .
Awais SB, Martins RS, Khan MS. Paramedics in pandemics: protecting the mental wellness of those behind enemy lines. Br J Psychiatry. 2021;218(2):75–6. https://doi.org/10.1192/bjp.2020.193 .
Sangal RB, Bray A, Reid E, Ulrich A, Liebhardt B, Venkatesh AK, et al. Leadership communication, stress, and burnout among frontline emergency department staff amid the COVID-19 pandemic: a mixed methods approach. Healthc (Amst). 2021;9(4):100577. https://doi.org/10.1016/j.hjdsi.2021.100577 .
Dickson CAW, Davies C, McCormack B, Westcott L, Merrell J, Mcilfatrick S, et al. UK nurses’ and midwives’ experiences of healthful leadership practices during the COVID-19 pandemic: a rapid realist review. J Nurs Manag. 2022;30(8):3942–57. https://doi.org/10.1111/jonm.13790 .
Isakov A, Carr M, Munjal KG, Kumar L, Gausche-Hill MEMS. Agenda 2050 meets the COVID-19 pandemic. Health Secur. 2022;20(S1):S97–106. https://doi.org/10.1089/hs.2021.0179 .
Eaton-Williams PJ, Williams J. See us as humans. Speak to us with respect. Listen to us. A qualitative study on UK ambulance staff requirements of leadership while working during the COVID-19 pandemic. BMJ Lead. 2023;7(2):102–7. https://doi.org/10.1136/leader-2022-000622 .
Barasa E, Mbau R, Gilson L. What is resilience and how can it be nurtured? A systematic review of empirical literature on Organizational Resilience. Int J Health Policy Manag. 2018;7(6):491–503. https://doi.org/10.15171/ijhpm.2018.06 .
Coetzee C, Van Niekerk D, Raju E. Disaster resilience and complex adaptive systems theory: finding common grounds for risk reduction. Disaster Prev Manage. 2016;25(2):196–211. https://doi.org/10.1108/DPM-07-2015-0153 .
American Psychological Association. Emotion. APA Dictionary of Psychology. https://dictionary.apa.org/emotion . Accessed on 26.6.2024.
Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499–512.
Ericsson CR, Lindström V, Rudman A, Nordquist H. Paramedics’ perceptions of job demands and resources in Finnish emergency medical services: a qualitative study. BMC Health Serv Res. 2022;22(1):1469. https://doi.org/10.1186/s12913-022-08856-9 .
Rinkinen T, Kinnula M, Nordquist H. Technological development roles and needs in pre-hospital emergency care from the advanced level paramedics’ perspective. Int Emerg Nurs. 2024;73:101406. https://doi.org/10.1016/j.ienj.2024.101406 .
Moodle Pty Ltd. 2020. https://moodle.org/ . Accessed on date 17.6.2024.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:2:77–101. https://doi.org/10.1191/1478088706qp063oa .
Prezant DJ, Lancet EA, Zeig-Owens R, Lai PH, Appel D, Webber MP, et al. System impacts of the COVID-19 pandemic on New York City’s emergency medical services. J Am Coll Emerg Physicians Open. 2020;9(6):1205–13. https://doi.org/10.1002/emp2.12301 .
Alwidyan MT, Oteir AO, Trainor J. Working during pandemic disasters: views and predictors of EMS providers. Disaster Med Public Health Prep. 2022;16(1):116–22. https://doi.org/10.1017/dmp.2020.131 .
Rebmann T, Charney RL, Loux TM, Turner JA, Abbyad YS, Silvestros M. Emergency Medical Services Personnel’s pandemic influenza training received and willingness to work during a future pandemic. Prehosp Emerg Care. 2020;24(5):601–9. https://doi.org/10.1080/10903127.2019.1701158 .
Article CAS PubMed PubMed Central Google Scholar
McCann-Pineo M, Li T, Barbara P, Levinsky B, Berkowitz J. Factors influencing Use of Personal Protective Equipment among Emergency Medical services Responders during the COVID-19 pandemic: a Retrospective Chart Review. West J Emerg Med. 2022;23(3):396–407. https://doi.org/10.5811/westjem.2022.2.55217 .
Vanhaecht K, Seys D, Bruyneel L, Cox B, Kaesemans G, Cloet M, et al. COVID-19 is having a destructive impact on health-care workers’ mental well-being. Int J Qual Health Care. 2021;20(1):mzaa158. https://doi.org/10.1093/intqhc/mzaa158 .
Zolnikov TR, Furio F. First responders and social distancing during the COVID-19 pandemic. J Hum Behav Soc Environ. 2021;31(1–4):244–53. https://doi.org/10.1080/10911359.2020.1811826 .
Spychała A, Piwowarska M, Piekut A. The COVID-19 pandemic as a stress factor in the work of a paramedic. Med Pr. 2023;8(1):9–17. https://doi.org/10.13075/mp.5893.01278 .
Roberts R, Wong A, Jenkins S, Neher A, Sutton C, O’Meara P, et al. Mental health and well-being impacts of COVID-19 on rural paramedics, police, community nurses and child protection workers. Aust J Rural Health. 2021;29(5):753–67. https://doi.org/10.1111/ajr.12804 .
Chang YT, Hu YJ. Burnout and Health issues among Prehospital Personnel in Taiwan Fire Departments during a Sudden Spike in Community COVID-19 cases: a cross-sectional study. Int J Environ Res Public Health. 2022;16(4):2257. https://doi.org/10.3390/ijerph19042257 .
Mausz J, Donnelly EA, Moll S, Harms S, McConnell M. Mental disorder symptoms and the relationship with resilience among paramedics in a single Canadian site. Int J Environ Res Public Health. 2022;17(8):4879. https://doi.org/10.3390/ijerph19084879 .
Phung VH, Sanderson K, Pritchard G, Bell F, Hird K, Wankhade P, et al. The experiences and perceptions of wellbeing provision among English ambulance services staff: a multi-method qualitative study. BMC Health Serv Res. 2022;15(1):1352. https://doi.org/10.1186/s12913-022-08729-1 .
Zamoum K, Gorpe TS. Crisis Management: a historical and conceptual Approach for a better understanding of today’s crises. Crisis Manage - Theory Pract InTech. 2018. https://doi.org/10.5772/intechopen.76198 .
Anderson C, Pooley JA, Mills B, Anderson E, Smith EC. Do paramedics have a Professional Obligation to work during a pandemic? A qualitative exploration of Community Member expectations. Disaster Med Public Health Prep. 2020;14(3):406–12. https://doi.org/10.1017/dmp.2020.212 .
Smith E, Burkle FM, Gebbie K, Ford D, Bensimon C. Acceptable limitations on Paramedic Duty to treat during disaster: a qualitative exploration. Prehosp Disaster Med. 2018;33(5):466–70. https://doi.org/10.1017/S1049023X18000857 .
Smith E, Burkle F, Gebbie K, Ford D, Bensimon C. A qualitative study of paramedic duty to treat during disaster response. Disaster Med Public Health Prep. 2019;13(2):191–6. https://doi.org/10.1017/dmp.2018.15 .
Cypress BS. Rigor or reliability and validity in qualitative research: perspectives, strategies, reconceptualization, and recommendations. Dimens Crit Care Nurs. 2017;36(4):253–63. https://doi.org/10.1097/DCC.0000000000000253 .
TENK. Guidelines for the responsible conduct of research and for handling allegations of misconduct in Finland [Internet]. Helsinki: Finnish National Board on Research Integrity TENK; 2023. https://tenk.fi/sites/default/files/2023-11/RI_Guidelines_2023.pdf . Accessed 13 Jan 2024.
TENK. Ethical review in human sciences [Internet]. Helsinki: Finnish National Board on Research Integrity TENK; 2020. https://tenk.fi/sites/default/files/2021-1/Ethical_review_in_human_sciences_2020.pdf . Accessed 13 Jan 2024.
Download references
Acknowledgements
We want to sincerely thank all the paramedics who participated in this study.
Open access funded by Helsinki University Library.
Open Access funding provided by University of Helsinki (including Helsinki University Central Hospital).
Author information
Authors and affiliations.
Faculty of Medicine, University of Helsinki, Helsinki, Finland
Henna Myrskykari
Emergency Medical Services, University of Turku and Turku University Hospital, Turku, Finland
Department of Healthcare and Emergency Care, South-Eastern Finland University of Applied Sciences, Kotka, Finland
Hilla Nordquist
You can also search for this author in PubMed Google Scholar
Contributions
Study design (HM, HN). Data collection (HN). Methodology (HN). Analysis (HM, HN). Writing (HM, HN). Review and editing (HM, HN). Supervision (HN). Both authors read and approved the final manuscript.
Corresponding author
Correspondence to Henna Myrskykari .
Ethics declarations
Ethics approval and consent to participate.
The study followed the good scientific practice defined by the Finnish National Board on Research Integrity TENK [ 43 ]. The study was conducted in accordance with the Helsinki Declaration and applicable national guidelines. Adhering to the Finnish National Board on Research Integrity (TENK) guidelines on ethical principles of research with human participants and ethical review in the human sciences in Finland, an ethical review statement from a human sciences ethics committee was not required for this type of study. The participants consisted of adult students engaged in regular employment. Their involvement in the research was grounded on informed consent. The study did not involve concerns regarding the participants’ physical integrity, nor were they subjected to exceptionally strong stimuli. The potential for causing mental harm was not beyond what is typically encountered in everyday life, and their participation did not pose any safety risks [ 44 ].
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Myrskykari, H., Nordquist, H. Paramedics’ experiences and observations: work-related emotions and well-being resources during the initial months of the COVID-19 pandemic—a qualitative study. BMC Emerg Med 24 , 152 (2024). https://doi.org/10.1186/s12873-024-01072-0
Download citation
Received : 25 April 2024
Accepted : 13 August 2024
Published : 26 August 2024
DOI : https://doi.org/10.1186/s12873-024-01072-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency medical services
- Health personnel
- Qualitative research
BMC Emergency Medicine
ISSN: 1471-227X
- General enquiries: [email protected]
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Communication challenges for people with chronic aphasia: a systematic qualitative review of barriers and facilitators in local services.

1. Introduction
2.1. search process, 2.2. data extraction and analysis, 3.1. study selection, 3.2. study characteristics, 3.3. methodological quality ratings, 3.4. reported barriers and facilitators, 4. discussion, 4.1. barriers and facilitators, 4.2. what can be done to catalyze the communicational participation of people with aphasia, 5. conclusions, limitations, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
| No. | Item | Guide and Description | Location (Lines) |
|---|---|---|---|
| 1 | Aim | State the research question the synthesis addresses. | 100 |
| 2 | Synthesis methodology | Identify the synthesis methodology or theoretical framework that underpins the synthesis, and describe the rationale for the choice of methodology. | 140–151 |
| 3 | Approach to searching | Indicate whether the search was pre-planned or iterative. | 109 |
| 4 | Inclusion criteria | Specify the inclusion/exclusion criteria. | 109–115 |
| 5 | Data sources | Describe the informational sources used, grey literature databases, relevant organisational websites, experts, information specialists, generic web searches, hand searching, reference lists) and when the searches were conducted; provide the rationale for using the data sources. | 105–108 |
| 6 | Electronic search strategy | Describe the literature search. | 116–118 |
| 7 | Study screening methods | Describe the process of study screening and sifting. | 118–123 |
| 8 | Study characteristics | Present the characteristics of the included studies. | 166–174 |
| 9 | Study selection results | Identify the number of studies screened and provide reasons for study exclusion. | 158–161 |
| 10 | Rationale for appraisal | Describe the rationale and approach used to appraise the included studies or selected findings. | 123–126 |
| 11 | Appraisal items | State the tools, frameworks, and criteria used to appraise the studies or selected findings. | 124–129 |
| 12 | Appraisal process | Indicate whether the appraisal was conducted independently by more than one reviewer and if consensus was required. | 127–129 |
| 13 | Appraisal results | Present the results of the quality assessment and indicate which articles, if any, were weighted/excluded based on the assessment and give the rationale. | 176–180, |
| 14 | Data extraction | Indicate which sections of the primary studies were analyzed and how the data were extracted from the primary studies. | 131–139 |
| 15 | Software | State the computer software used, if any. | No software used for analysis |
| 16 | Number of reviewers | Identify who was involved in coding and analysis. | 132–133 |
| 17 | Coding | Describe the process of the coding of data. | 140–151 |
| 18 | Study comparison | Describe how comparisons were made within and across studies. | 140–151 |
| 19 | Derivation of themes | Explain whether the process of deriving the themes or constructs was inductive or deductive. | 140–151 |
| 20 | Quotations | Provide quotations from the primary studies to illustrate themes/constructs and identify whether the quotations were participant quotations or the author’s interpretation. | and |
| 21 | Synthesis output | Present rich, compelling, and useful results that go beyond a summary of the primary studies. | and , |
| Database | Keywords | Results | |
|---|---|---|---|
| Google Scholar | aphasi *|”aphasic person”|”language disorder”|”communication disorder”|”communication impairment” accessib *|”accessible communication”|”communication access”|”access program”|”access measure”|”universal access”|”universal design *”|”assistive technolog *”|”architectur * access *”|adapt *|signage|”social participation”|accommodat *|independen *|”inclusive society”|inclusi *|barriers|facilitators “public facilit *”|”public space *”|”financial institution *”|store *|shop *|museum *|transportation|restaurant * | 200 first results | |
| CINAHL | In title and in abstract: (aphasi * OR (“language disorders” or “language impairment” or “specific language disorder”) OR “communicati * impairment” OR “acquired language disorder”) AND (accessib * OR communicati * N3 access * OR access * N3 program OR access * N3 measure OR universal access OR universal design OR assistive technolog * OR accomodations OR (barriers or obstacles or challenges) OR facilitators) AND (public facilit * OR public space OR communit * N3 participation OR social N3 participation) Criteria: All adults | 21 | |
| MEDLINE | Searched via Ovid | In title and abstract: (aphasi * or language disorders or language impairment or specific language disorder or communicati * impairment or acquired language disorder) AND (accessib * or (communicati * adj3 access *) or (access * adj3 program) or (access * adj3 measure) or accomodations or barriers or obstacles or facilitators) AND (public facilit * or public space or (communit * adj3 participation) or (social adj3 participation)) | 10 |
| PsycINFO | 22 | ||
| ERIC | 1 | ||
| Web of Science | (aphasi * OR “language disorders” OR “language impairment” OR “specific language disorder” OR “acquired language disorder” OR “communicati * impairment”) AND (accessib * OR “communicati * access *” OR “access * program” OR “access * measure” OR “universal access” OR “universal design” OR “assistive technolog *” OR accomodations OR barriers or obstacles or challenges OR facilitators) AND (“public facilit *” OR “public space” OR “communit * participation” OR “social participation”) Document types: Articles | 57 | |
| Manually added references | 3 | ||
| Total number of references | 314 | ||
| Number of screened references (duplicates removed) | 269 | ||
| Criterion | Ref. No. | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | [ ] | |
| Question/objective sufficiently described? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Study design evident and appropriate? | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 |
| Context for the study clear? | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 |
| Connection to a theoretical framework/wider body of knowledge? | 1 | 2 | 2 | 2 | 0 | 2 | 0 | 1 | 2 |
| Described sampling strategy relevant and justified? | 1 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 |
| Data collection methods clearly described and systematic? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Data analysis clearly described and systematic? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Use of verification procedure(s) to establish credibility? | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Conclusion supported by the results? | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 2 | 2 |
| Reflexivity of the account? | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 |
- Dickey, L.; Kagan, A.; Lindsay, M.P.; Fang, J.; Rowland, A.; Black, S. Incidence and Profile of Inpatient Stroke-Induced Aphasia in Ontario, Canada. Arch. Phys. Med. Rehabil. 2010 , 91 , 196–202. [ Google Scholar ] [ CrossRef ]
- American Speech-Language-Hearing Association Aphasia. Available online: https://www.asha.org/public/speech/disorders/aphasia/ (accessed on 10 June 2024).
- World Health Organization International Classification of Functioning, Disability and Health: ICF. Available online: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health (accessed on 10 June 2024).
- Hall, M.J.; Levant, S.; DeFrances, C.J. NCHS Data Brief No. 95, May 2012 . 95 . 2012. Available online: https://www.scirp.org/reference/referencespapers?referenceid=2334094 (accessed on 10 June 2024).
- Graham, J.R.; Pereira, S.; Teasell, R. Aphasia and Return to Work in Younger Stroke Survivors. Aphasiology 2011 , 25 , 952–960. [ Google Scholar ] [ CrossRef ]
- Roth, E.J.; Lovell, L. Community Skill Performance and Its Association with the Ability to Perform Everyday Tasks by Stroke Survivors One Year Following Rehabilitation Discharge. Top. Stroke Rehabil. 2007 , 14 , 48–56. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hilari, K.; Needle, J.J.; Harrison, K.L. What Are the Important Factors in Health-Related Quality of Life for People with Aphasia? A Systematic Review. Arch. Phys. Med. Rehabil. 2012 , 93 , S86–S95.e4. [ Google Scholar ] [ CrossRef ]
- Alary Gauvreau, C.; Le Dorze, G. Participant Reported Outcomes of a Community of Practice about Social Participation for Speech-Language Pathologists in Aphasia Rehabilitation. Disabil. Rehabil. 2022 , 44 , 231–242. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Howe, T.J.; Worrall, L.E.; Hickson, L.M.H. Interviews with People with Aphasia: Environmental Factors That Influence Their Community Participation. Aphasiology 2008 , 22 , 1092–1120. [ Google Scholar ] [ CrossRef ]
- U.S. Department of Justice Civil Rights Division Americans with Disabilities Act. Available online: https://www.ada.gov/ (accessed on 10 June 2024).
- Disability Discrimination Act; 1992. Available online: https://www.legislation.gov.au/C2004A04426/2018-04-12/text (accessed on 10 June 2024).
- An Act to Ensure a Barrier-Free Canada of 2019 ; 2019; Bill C-81. Available online: https://www.justice.gc.ca/eng/csj-sjc/pl/charter-charte/c81.html (accessed on 10 June 2024).
- Law, J.; van der Gaag, A.; Hardcastle, W.J.; Beckett, D.J.; MacGregor, A.; Plunkett, C. Communication Support Needs: A Review of the Literature ; Scottish Executive Social Research, 2007. Available online: https://eresearch.qmu.ac.uk/bitstream/handle/20.500.12289/2013/communication_support_needs_lit_review_2007.pdf?sequence=1&isAllowed=y (accessed on 10 June 2024).
- Orchardson, R. Aphasia—The Hidden Disability. Dent. Update 2012 , 39 , 168–174. [ Google Scholar ] [ CrossRef ]
- Tierney-Hendricks, C.; Schliep, M.E.; Vallila-Rohter, S. Using an Implementation Framework to Survey Outcome Measurement and Treatment Practices in Aphasia. Am. J. Speech Lang. Pathol. 2022 , 31 , 1133–1162. [ Google Scholar ] [ CrossRef ]
- Tong, A.; Flemming, K.; McInnes, E.; Oliver, S.; Craig, J. Enhancing Transparency in Reporting the Synthesis of Qualitative Research: ENTREQ. BMC Med. Res. Methodol. 2012 , 12 , 181. [ Google Scholar ] [ CrossRef ]
- Haddaway, N.R.; Collins, A.M.; Coughlin, D.; Kirk, S. The Role of Google Scholar in Evidence Reviews and Its Applicability to Grey Literature Searching. PLoS ONE 2015 , 10 , e0138237. [ Google Scholar ] [ CrossRef ]
- Covidence Systematic Review Software 2024. Available online: https://www.covidence.org/ (accessed on 10 June 2024).
- Kmet, L.M.; Lee, R.C.; Cook, L.S. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields. 2004. Available online: https://www.ihe.ca/advanced-search/standard-quality-assessment-criteria-for-evaluating-primary-research-papers-from-a-variety-of-fields (accessed on 10 June 2024).
- Kim, E.S.; Mauriks, K.; Wilson, C.; Auch, L.; Koo, H.; Swensrude, D.; Laccett, J.; Ruelling, A. Barriers and Facilitators to Communication Accessibility as Perceived by People with Aphasia. Top. Lang. Disord. 2023 , 43 , 76–90. [ Google Scholar ] [ CrossRef ]
- Taylor, S.; Wilson, E.; Murfitt, K.; Balandin, S. Communication Access in the Retail Environment for People with Complex Communication Needs. Disabil. Rehabil. 2021 , 43 , 3189–3198. [ Google Scholar ] [ CrossRef ]
- Dalemans, R.J.P.; De Witte, L.; Wade, D.; Van Den Heuvel, W. Social Participation through the Eyes of People with Aphasia. Int. J. Lang. Commun. Disord. 2010 , 45 , 537–550. [ Google Scholar ] [ CrossRef ]
- Blonski, D.C.; Covert, M.; Gauthier, R.; Monas, A.; Murray, D.; O’Brien, K.K.; Mendelson, A.D.; Huijbregts, M. Barriers to and Facilitators of Access and Participation in Community-Based Exercise Programmes from the Perspective of Adults with Post-Stroke Aphasia. Physiother. Can. 2014 , 66 , 367–375. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ashton, C.; Aziz, N.A.; Barwood, C.; French, R.; Savina, E.; Worrall, L. Communicatively Accessible Public Transport for People with Aphasia: A Pilot Study. Aphasiology 2008 , 22 , 305–320. [ Google Scholar ] [ CrossRef ]
- Anglade, C.; Le Dorze, G.; Croteau, C. Service Encounter Interactions of People Living with Moderate-to-Severe Post-Stroke Aphasia in Their Community. Aphasiology 2019 , 33 , 1061–1082. [ Google Scholar ] [ CrossRef ]
- Howe, T.J.; Worrall, L.E.; Hickson, L.M.H. Observing People with Aphasia: Environmental Factors That Influence Their Community Participation. Aphasiology 2008 , 22 , 618–643. [ Google Scholar ] [ CrossRef ]
- Le Dorze, G.; Salois-Bellerose, É.; Alepins, M.; Croteau, C.; Hallé, M.-C. A Description of the Personal and Environmental Determinants of Participation Several Years Post-Stroke According to the Views of People Who Have Aphasia. Aphasiology 2014 , 28 , 421–439. [ Google Scholar ] [ CrossRef ]
- Baylor, C.; Burns, M.; Eadie, T.; Britton, D.; Yorkston, K. A Qualitative Study of Interference with Communicative Participation Across Communication Disorders in Adults. Am. J. Speech Lang. Pathol. 2011 , 20 , 269–287. [ Google Scholar ] [ CrossRef ]
- Nunn, K.; Tilton-Bolowsky, V.; Kershenbaum, A.M. Moving Toward Anti-Ableist Practices in Aphasia Rehabilitation and Research: A Viewpoint. Am. J. Speech Lang. Pathol. 2024 , 1–11. [ Google Scholar ] [ CrossRef ]
- Hagan, T.; Rosenzweig, M.; Zorn, K.; Van Londen, G.J.; Donovan, H. Perspectives on Self-Advocacy: Comparing Perceived Uses, Benefits, and Drawbacks Among Survivors and Providers. Oncol. Nurs. Forum 2017 , 44 , 52–59. [ Google Scholar ] [ CrossRef ]
- Howe, T.; McCarron, E.; Rowe, J. What Helps Confidence in Communication—Perspectives of Adults with Aphasia: “Get Maze…not Stay out It”. J. Commun. Disord. 2023 , 103 , 106334. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Howe, T. Found Opportunities for Social Participation: Facilitating Inclusion of Adults with Aphasia. Top. Lang. Disord. 2017 , 37 , 38–51. [ Google Scholar ] [ CrossRef ]
- Miller, E.L. Negotiating Communicative Access in Practice: A Study of a Memoir Group for People with Aphasia. Writ. Commun. 2019 , 36 , 197–230. [ Google Scholar ] [ CrossRef ]
- Bennington, C.; Shiggins, C.; Isaksen, J.; Beesley, E.; Beesley, K.; Wallace, S.J. What Does It Mean to Be Aphasia Aware? An International Survey of Stakeholder Perspectives and Experiences of Aphasia Awareness. Aphasiology 2024 , 1–24. [ Google Scholar ] [ CrossRef ]
- Aphasia Institute Programs & Services. Available online: https://www.aphasia.ca/programs-services/ (accessed on 10 June 2024).
- Stroke Association Aphasia Awareness and the Communications Access Symbol. Available online: https://www.stroke.org.uk/stroke/effects/aphasia/aphasia-awareness (accessed on 10 June 2024).
- Simmons-Mackie, N.; Worrall, L.; Shiggins, C.; Isaksen, J.; McMenamin, R.; Rose, T.; Guo, Y.E.; Wallace, S.J. Beyond the Statistics: A Research Agenda in Aphasia Awareness. Aphasiology 2020 , 34 , 458–471. [ Google Scholar ] [ CrossRef ]
- Government of Canada Accessibility Standards Canada. Available online: https://accessible.canada.ca/about-us (accessed on 10 June 2024).
Click here to enlarge figure
| Contextual Factors | Contextual Factor Category | Factor Subtype |
|---|---|---|
| Environmental factors | Societal factors | Societal knowledge |
| Services | ||
| Policies (e.g., municipal, governmental) | ||
| Procedures | ||
| Task characteristics (e.g., requiring writing) | ||
| Financial matters | ||
| Transportation | ||
| Service characteristics | ||
| Attitudinal factors | Other people’s actions | |
| Other people’s attitudes | ||
| Other people’s knowledge | ||
| Other people’s characteristics | ||
| Other people’s roles (e.g., caregiver) | ||
| Animals (i.e., presence of animals in the immediate environment) | ||
| Physical factors | Objects’ characteristics | |
| Objects (e.g., phones) | ||
| Acoustic characteristics | ||
| Visual characteristics | ||
| Spatial characteristics | ||
| Physical environment characteristics (e.g., familiarity of the environment) | ||
| Personal factors | Undefined | Undefined |
| Ref. No. | Authors (Year) | Country | Accessibility Context | People with Aphasia | Data Collection Strategy | Methodological Quality [ ] |
|---|---|---|---|---|---|---|
| [ ] | Kim et al. (2023) | Canada | Local businesses | 9 | Interviews | 18/20 |
| [ ] | Taylor et al. (2021) | Australia | Local businesses | 1 | Interview | 20/20 |
| [ ] | Dalemans et al. (2010) | Netherlands | Local businesses | 13 | Interviews | 20/20 |
| [ ] | Howe et al. (2008a) | Australia | Local businesses, public transportation | 25 | Interviews | 20/20 |
| [ ] | Blonski et al. (2014) | Canada | Community centre with exercise programs | 10 | Interviews | 18/20 |
| [ ] | Ashton et al. (2008) | Australia | Public transportation | 7 | Interviews and, observation | 17/20 |
| [ ] | Anglade et al. (2019) | Canada | Local businesses | 6 | Observation | 15/20 |
| [ ] | Howe et al. (2008b) | Australia | Local businesses | 10 | Observation | 19/20 |
| [ ] | Le Dorze et al. (2014) | Canada | Local businesses | 17 | Discussion groups | 20/20 |
| Category of Contextual Factors | Factor Subtype | Barriers | Facilitators |
|---|---|---|---|
| Societal factors | Societal knowledge | , , ]: ] , ] ]“The physical things… seem to get so many stories [in the media], but you hardly ever hear anything about… the brain people.” [ ] | ] ]“Understanding… Education about aphasia is the most important one.” [ ] |
| Services | ]“Finished my speech therapy… devastated at home ‘cause… I didn’t know what to do from here.” [ ] | , ] ] ] ] , ] | |
| Policies | ] | ] | |
| Procedures | , , ] , , , ] ] | ] , ] ] | |
| Task characteristics | ] ] | ] | |
| Financial matters | ] | ] ] | |
| Transportation | ] ] | ||
| Attitudinal factors | Other people’s actions | , , ]; ]; , ]; , ]; ] , , , , ]“Just take time right. Just let me think right.” [ ] | , , , , , , ]; , ]; , , ] ] ] |
| Other people’s attitudes | , , ]: , , ]“Treat you as if I’m stupid,” “Impatience… Number one [barrier],” “Doesn’t give you any respect” [ , , , , , ] | ] , , , , , , ]“Light-hearted attitude… makes you relax more.” [ ] | |
| Other people’s knowledge | , , , , ]: ] | , , ]“Got to the situation where he knew that what I said wasn’t really what I meant.” [ ] | |
| Other people’s characteristics | ] | , , ] | |
| Other people’s roles | ]: ] | , , , , ] ] | |
| Animals | ] | ||
| Physical factors | Objects’ characteristics | , , ] ] ] | , ] |
| Objects | ] | , ] , , ] | |
| Acoustic characteristics | , , ] | , ] | |
| Visual characteristics | ] | ||
| Spatial characteristics | ] ] | , , ] ] | |
| Physical environment characteristics | , ] ] ] |
| Type of Personal Factors | Barriers | Facilitators |
|---|---|---|
| Motivation | , , ] , ] ] ]“if you don’t reach out, you get nothing; you get to stay alone, sitting in your corner.” [ ] | , , ] , , ] , ]: , , ] |
| Physical and psychological conditions | ]: , ] ] , ]“I am embarrassed. People think that I am crazy, and I am not. I don’t dare to talk to strangers. I feel ashamed.” [ ] |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Poirier, S.-È.; Voyer, L.-A.; Poulin, V.; Lamontagne, M.-E.; Monetta, L. Communication Challenges for People with Chronic Aphasia: A Systematic Qualitative Review of Barriers and Facilitators in Local Services. Disabilities 2024 , 4 , 616-631. https://doi.org/10.3390/disabilities4030038
Poirier S-È, Voyer L-A, Poulin V, Lamontagne M-E, Monetta L. Communication Challenges for People with Chronic Aphasia: A Systematic Qualitative Review of Barriers and Facilitators in Local Services. Disabilities . 2024; 4(3):616-631. https://doi.org/10.3390/disabilities4030038
Poirier, Sarah-Ève, Laurie-Anne Voyer, Valérie Poulin, Marie-Eve Lamontagne, and Laura Monetta. 2024. "Communication Challenges for People with Chronic Aphasia: A Systematic Qualitative Review of Barriers and Facilitators in Local Services" Disabilities 4, no. 3: 616-631. https://doi.org/10.3390/disabilities4030038
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Open access
- Published: 27 August 2024
Facilitators and barriers to interprofessional collaboration among health professionals in primary healthcare centers in Qatar: a qualitative exploration using the “Gears” model
- Alla El-Awaisi 1 ,
- Ola Hasan Yakti 2 ,
- Abier Mohamed Elboshra 1 ,
- Kawthar Hasan Jasim 1 ,
- Alzahraa Fathi AboAlward 1 ,
- Raghad Walid Shalfawi 3 ,
- Ahmed Awaisu 1 ,
- Daniel Rainkie 4 ,
- Noora Al Mutawa 3 , 5 &
- Stella Major 6
BMC Primary Care volume 25 , Article number: 316 ( 2024 ) Cite this article
Metrics details
The number of patients seeking medical care is increasing, necessitating more access to primary healthcare services. As several of these patients usually present with complex medical conditions, the need for interprofessional collaboration (IPC) among health professionals in primary care is necessary. IPC is essential for facing the increasing and challenging healthcare demands. Therefore, the facilitators of and the barriers to IPC should be studied in the hope that the results will be used to promote such endeavors.
This study aimed to explore the perspectives of different health professionals regarding the facilitators of and the barriers to IPC in the primary healthcare settings in Qatar.
A qualitative study using focus groups was conducted within the Primary Health Care Corporation (PHCC) in Qatar. Several health professionals were invited to participate in the focus groups. The focus groups were uniprofessional for general practitioners (GPs), nurses, and dentists, while they were interprofessional for the other health professionals. Focus groups were audio-recorded and transcribed verbatim and validated by the research team. The data were analyzed by deductive thematic analysis using the “Gears” Conceptual Model as a coding framework.
Fourteen focus groups were conducted involving 58 participants (including 17 GPs, 12 nurses, 15 pharmacists, 3 dentists, and 11 allied health professionals) working in PHCC in Qatar. The findings revealed a spectrum of factors influencing IPC, categorized into four main domains: Macro, Meso, Micro, and individual levels, with each accompanied by relevant barriers and facilitators. Key challenges identified included a lack of communication skills, insufficient professional competencies, and power imbalances, among others. To address these challenges, recommendations were made to implement dedicated training sessions on IPC, reduce hierarchical barriers among different health professionals, and enhance the effectiveness of existing systems. Conversely, it was emphasized that projects and campaigns focused on IPC, alongside the development of enhanced communication skills and the presence of supportive leadership, as essential for facilitating effective IPC in PHCCs.
The interplay between the meso, macro, micro, and individual levels highlight the significance of a multifaceted approach to interventions, aiming to enhance the successes of IPC. While initiatives like interprofessional education training are underway, numerous challenges persist before achieving improved collaboration and more efficient integration of IPC in the PHCC setting.
Peer Review reports
Introduction
The World Health Organization (WHO) projects a global deficit of health professionals in comparison to the needs, expected to exceed 18 million by 2030, which will impede the provision of optimal healthcare services. In their “Global strategy on human resources for health: Workforce 2030”, they highlighted the need to equip health professionals with the skills needed to practice collaboratively in interprofessional teams [ 1 ]. One of the best solutions to face this strain on the healthcare system and to provide better management of the complex health challenges is to implement and promote the concept of interprofessional collaboration (IPC) as these demands often are beyond the expertise of any single profession [ 2 , 3 , 4 ]. According to the WHO, IPC occurs when “multiple healthcare workers from different professional backgrounds provide comprehensive services by working with patients, their families, caregivers, and communities to deliver the highest quality of care across settings” [ 2 ]. IPC recently has become one of the core demands of accreditors, funding institutions, policymakers, and practicing health professionals, recognizing its potential to improve the quality of care and address the increasing demand for healthcare services [ 5 , 6 , 7 , 8 ].
Research has consistently highlighted the positive impact of IPC on healthcare work processes, patient safety, and patient outcomes across various disease states such as diabetes, heart failure and asthma, which were treated in hospital, primary care, and community settings [ 9 , 10 , 11 ]. Research has concluded that a high degree of IPC has led to better subjective outcomes, including overall satisfaction, treatment success, and willingness to recommend the healthcare institution to others. Additionally, objective outcomes such as reduced mortality rate, readmissions, and hospital length of stay have been noted. Furthermore, collaboration has been associated with improved decision-making and increased innovation [ 12 , 13 ]. It has also been demonstrated that as the relationship and level of connectedness between physicians and other health professionals increase; hospitalization costs and readmission rates decrease [ 14 ].
Primary healthcare is the foundation of any country’s healthcare system. It is not only considered the primary point of contact with the healthcare system, but it also serves as the vehicle for ensuring continuity of care across settings. The increase in the number of people with multiple chronic diseases that are associated with considerable social, functional, and emotional impairment and an increase in the healthcare demand, leading to an increase in the needed services [ 15 , 16 , 17 , 18 ]. Consequently, policymakers on an international scale have persistently advocated for the greater integration of interprofessional team-based care in primary healthcare settings and the development of influencing factors that explicitly acknowledge the value of this collaborative approach [ 19 , 20 ]. Several studies in the literature have highlighted the positive outcomes associated with effective collaboration within primary healthcare settings [ 21 , 22 , 23 ]. This has led to an internationally movement towards team-based primary healthcare, to enhance the integration of services and to emphasize health promotion and chronic disease management [ 19 ]. Ineffective collaboration leads to an increased risk of preventable errors, lack of efficiency, and loss of motivation, resulting in suboptimal patient care based on nurses’ opinions [ 24 ].
While IPC efforts are usually initiated by policymakers, research have demonstrated that health professionals’ play a vital role in providing high-quality IPC. Therefore, it is of crucial importance to consider the perspectives of health professionals working in primary healthcare settings regarding IPC when designing and implementing IPC projects [ 25 ]. Numerous studies have examined IPC across various countries. For example, a systematic review was conducted to explore facilitators and barriers to IPC implementation in primary healthcare settings. This review included studies conducted in Great Britain, the United States, the Netherlands, Australia, Spain, Brazil, Canada, and New Zealand. The findings of this review indicated that allied health professionals generally hold positive perceptions of IPC within primary healthcare contexts [ 26 , 27 ]. However, limited research has been conducted to investigate healthcare IPC practice in Qatar, particularly in primary healthcare settings. Given the recent expansion of scope of practice in primary care in Qatar [ 28 ], it is essential to explore the current practices in primary healthcare in Qatar in terms of IPC facilitators and barriers, and determining the necessary steps to achieve optimal collaboration within the Qatari healthcare system.
This study is a continuation of a previous study that explored the perspective of 1415 health professionals in primary healthcare settings through a self-administered questionnaire [ 28 ]. Results of the study showed that health professionals generally have a positive attitude and readiness toward IPC. Interprofessional differences were noted regarding their readiness to be involved in IPC, where physicians had slightly more positive readiness towards understanding their professional identity compared to other health professionals. Health professionals with previous IPC or interprofessional education (IPE) experiences revealed greater, but non-significant positive attitudes toward IPC compared to those without previous experiences. Participants suggested that facilitators and barriers for IPC in primary healthcare settings are conceptual rather than physical. Facilitators included personal belief in IPC benefit, higher professional satisfaction, interprofessional respect, appreciation of other health professionals’ role, institutional support, and leadership. Barriers identified included lack of time, leadership, support, and limited resources.
In an effort to understand the health professionals’ perception of the facilitators and barriers for IPC in primary healthcare in Qatar, the current study will explore the factors affecting the IPC in primary healthcare in Qatar using the “Gears” conceptual model [ 7 ]. The Gears model offers a taxonomy of factors influencing IPC within Interprofessional Primary Care Teams (IPCTs). These factors are categorized into levels: policymakers (macro gear), organizational managers (meso gear), healthcare teams (micro gear), and health professionals (individual gear). Most of the factors identified by the “Gears model” are within the micro gear, or those affecting the individual. These involve formal processes such as quality audits and group problem-solving; social processes pertained to open communication and supportive colleagues; team attitudes such as feeling part of the team; and team structure such as team size and having a collaboration champion or facilitator. Macro gears/policy factors are those that change less frequently and are pertained to regulations regarding the general scope of practice, funding, etc. Meso gears/ organizational factors are those that change more often and affect more than one team in the organization, those are concerned with the information systems, organizational culture, etc. Individual factors include the individual health professional characteristics such as belief in IPC care and personal flexibility.
The aim of this study is to identify factors facilitating or impeding IPC in primary healthcare in Qatar by exploring the perspectives of health professionals working in primary healthcare qualitatively. These include GPs, nurses, pharmacists, dentists, and allied health professionals (lab technicians, physiotherapists, dieticians, and radiographers). Findings from this study will be used to find ways to enhance and promote collaborative practice in primary healthcare in Qatar.
Study design
In this qualitative study design, data were collected through semi-structured focus groups. A qualitative approach was used to explore comprehensively the lived experiences of health professional’s perspective as it allows for investigating a phenomenon from the people who have experienced it. It gives a deeper insight and answers to what, how, and why questions [ 12 ].
Study setting
The study was conducted among health professionals working in the Primary Health Care Corporation (PHCC) in Qatar. PHCC was established in 1978 to provide comprehensive primary healthcare services and became an independent body in 2012 with full administrative and financial autonomy. At the present time, the PHCC provides PHC through 27 PHC centers distributed across the country. Each center is staffed with health professionals who provide a broad range of services, focusing on health promotion and disease prevention. PHCC has adopted and implemented family medicine model of care and offers a wide range of services, including general medicine, dentistry, ophthalmology, optometry, ENT, dermatology, mental health, preventive and lifestyle services such as wellness, premarital care, cancer screening, gym and geriatric, physiotherapy and radiology services [ 29 ]. In February 2018, a local continuous professional development (CPD) program was initiated by PHCC Workforce Training Department (WFTD) for implementing learning activities across the 27 PHCC health centers using interprofessional and collaborative approaches.
Study participants and sampling
The study comprised 58 participants, including 17 general practitioners, 12 nurses, 3 dentists, 15 pharmacists, and 11 allied health professionals (e.g., laboratory technologists, radiologists, optometrists, and audiologists) working in PHCC in Qatar. A purposive sampling strategy was employed to select health professionals with experience or understanding of IPC, aiming to maximize participant recruitment and ensure representation of the study population’s views [ 16 ]. Sampling continued until thematic saturation was reached, indicating no further emergent ideas from discussions [ 17 ].
Participants’ recruitment
Emails were sent to the health professionals working at PHCC in Qatar inviting them to participate in the study focus groups that were planned to be conducted at Qatar University or PHCC headquarters. Recruitment of participants was facilitated through WFTD which took the responsibility of recruiting and arranging appropriate focus group schedule that can suit study participants. An invitation email was sent with consent form and participant information sheet to participants prior to the focus groups.
Data collection
The topic guide was developed through discussions with the research team, a review of previous literature, and based on phase 1 quantitative results [ 28 ] (please see supplementary file). A pilot interview was conducted with minor adjustments and included a few health professionals working in PHCC. Because no significant changes were made it was included in the final analysis. The focus group were uniprofessional (i.e. homogenous groups) for GPs, nurses and dentist and interprofessional (i.e. heterogeneous groups) for the remaining health professionals and varied in duration between 90 and 120 min. The discussions were audio-recorded and transcribed verbatim.
Data analysis
A deductive thematic analysis was conducted of data, which is an analytical method in which authors use existing themes, categories, or domains to categorize new data under such categories [ 30 ]. Participants’ ideas were categorized under four main domains adapted from the “Gears model” [ 7 ]. The gears model outlines the factors affecting IPC within IPCTs under four main factor domains: macro, meso, micro, and individual factors. AME, AA, KJ, RS reviewed and validated the transcripts. They then independently reviewed couple of transcripts to generate codes in discussion with the lead author (AE). Coding for the rest of the transcripts was validated by one faculty member from the research team. A final discussion took place with all authors to agree on themes and subthemes.
Reflexivity
During the data collection and analysis process, the research team engaged in reflexive practices to mitigate potential biases. The team consisted of various individuals with diverse backgrounds, including faculty members with pharmacy, nursing and medical backgrounds, three of whom were practicing health professionals, along with four pharmacy students and one alumna. The team offered a broad spectrum of perspectives and insights for data generation and analysis. These faculty members had an understanding of IPE and had previously conducted workshops on interprofessional collaboration for health professionals at PHCC. With a background in IPC, participants’ ideas were more easily understood, facilitating deeper engagement, and enabling the comprehension of their perspectives more readily, thus ensuring a comprehensive interpretation of the data. Throughout the research process, attention was paid to the potential influence of professional backgrounds, with reflexive practices employed to mitigate biases and ensure the integrity of the findings.
Data collection were mostly led by the principal investigator, with support from students adhering to a pre-defined topic guide to minimize personal biases. To further enhance trustworthiness of the study, students independently coded the data, which was validated by a faculty member of the research team. The team met several times to review and compare codes and themes, refining the analysis iteratively until consensus was reached. Each stage of the research process was overseen by the principal investigator, ensuring the rigor and robustness of the study.
Fourteen focus groups were conducted between September 2019 and February 2020, involving 58 health professionals working in primary healthcare centers in Qatar (17 general practitioners, 12 nurses 15 pharmacists, 3 dentists, and 11 allied health professionals). The baseline characteristics of the participants are summarized in Table 1 . Four domains, 10 themes, and 14 sub-themes were identified from the focus groups. The domains, themes, and sub-themes are summarized in Table 2 .
Gears domain 1: macro factors
Facilitators, theme 1: the influence of organizational policies on ipc.
Several factors were identified by health professionals pertaining to the policies that can affect IPC. These factors were mainly related to the rules and regulations set by the organization’s managers or government bodies, which typically influence the general scopes of practice, funding mechanisms, and remuneration of providers. Consensus was reached that these regulations play a significant role in fostering IPC among health professionals.
“Actually , we have very well prepared and organized policies. Policies related to teamwork , which align with best-practices and international guidelines. The policies at our PHCC facilitate collaboration… but how to use it? Is everybody aware of its use?” [Laboratory technologist 1].
No major barriers were identified under the macro factors.
Gear’s domain 2: meso factors
Theme 2.1: leveraging technology for enhanced communication.
Participants unanimously agreed that the current health information system, specifically CERNER, serve as a strong facilitator for enhancing communication among health professionals. It enables seamless sharing of patients’ details documented by other health professionals.
“I find the CERNER system software amazing , because you can get to see the history of the patients and previous appointments records. Everything is well documented” [Dentist 3].
Theme 2.2: communication hindered by limitations in healthcare information system utilization
Several participants noted that current system (CERNER) is not fully utilized for documenting and reporting of medical or medication errors which can serve as a barrier. As an example, one participant expressed reluctance to utilize the system and filing an OVA (incidental report) for fear of retaliation in case the reporter is identified.
“If I were to write OVA (incidental report) for him/her , he/she will get angry at me. So , there’s no use. Actually , the purpose is to report in order for others to learn from them , but there is no clear pathway that there will be no consequences for us reporters” [Nurse 2].
Furthermore, another HCP mentioned that the current information system might be a barrier, as not all health professionals have equal access to the system.
“The pharmacist is not allowed to enter a recommendation into the system; they have their own system” [GP 5].
Theme 2.3: barriers in organizational dynamics hindering IPC
Sub-theme 2.3.1: hierarchy hinders collaborative spirit.
One of the primary obstacles to collaboration within the institution is perceived to be the presence of a hierarchical structure. This perception is based not only in the observable existence of a grading system that categorizes health professionals according to their profession and seniority, but also in the benefits associated with higher hierarchical positions.
“The hierarchy is influenced by salary differences” [GP 4].
Participants in the study observed that this hierarchical system leads to disparities, which undermine their willingness to collaborate. As an example, pharmacists expressed feeling of being treated differently compared to GPs, who are routinely offered opportunities to attend international conferences. The lack of such opportunities for pharmacists and other health professionals further reinforces the perception of hierarchy within the institution.
“I have tried to attend a conference; I have a right to enhance my education. Why does this apply to the GP and not to the pharmacist?” [Pharmacist 8]. “He -the GP- thinks that the pharmacist as being of lower status , and he is the only one to have the authority to write and make decisions” [Pharmacist 9].
Sub-theme 2.3.2: blame culture instils apprehension among health professionals
Another significant factor that had a considerable impact on collaborative efforts was the existence of a culture of blame within the PHCC organization. This culture of blame surfaced frequently during discussions among health professionals and was found to hinder effective collaboration among team members. Some perceived the level of blame not to be equitable.
“What if I did a mistake? And what if the mistake was done by the GP? The blame wouldn’t be equal. We would receive more blame” [Nurse 3]. “I still believe that some of us should refrain from perpetuating a blame culture or name-calling. After all , all of us are human beings. We are prone to making errors” [GP 10]. “We need to promote a culture of no blame. When things go wrong or mistakes occur , we should view them as collective challenges rather than assigning fault to individuals and subjecting them to humiliation. This approach will significantly transform the overall attitude within the environment” [GP 2].
Sub-theme 2.3.3: Lack of feedback contributes to the perception that health professionals’ efforts are undervalued
Some health professionals have expressed concerns regarding the lack of feedback on their performance, interventions, and error reports, particularly within Datix, a patient safety software utilized for healthcare risk reporting. This absence of feedback is perceived as a significant impediment to IPC, as it fosters the perception that the efforts of health professionals are not adequately acknowledged or valued.
“The risk management team should gather data and determine the significance of incidents reported through Datix , which is serious or recurring. If a mistake is repeated , they will ask or make an investigation about this issue. However , aside from these instances , no action is taken. No feedback is provided” [Pharmacist 1].
Gears domain 3: micro factor
Theme 3.1: expanding the scope of practice of team members enhances collaboration.
Given that IPC heavily relies on teamwork, the topic of collaborative efforts and teamwork surfaced frequently during focus groups.
“ The most important thing in primary healthcare practice is the teamwork. We underscore its importance , as it permeates our daily operations” [GP 6].
Expanding the scope of practice of healthcare team members has the potential to foster enhanced collaboration between team members. For example, pharmacists who participated in the discussions expressed that the inclusion of a clinical pharmacist within PHCC would enhance collaboration. This is attributed to the direct involvement of the clinical pharmacist with the interprofessional team, which obviates the need for external prompting to initiate collaborative efforts.
Theme 3.2: effective communication channels foster collaboration
Effective collaboration among participants was found to significantly hinge on the establishment of robust communication channels. This encompasses both formal features and tools, ranging from cordial and conversational telephonic exchanges to more structured modes of communication, such as the sharing of electronic patient records. Several participants cited instances of proficient communication that had led to successful collaboration outcomes.
“Every colleague should be encouraged to express their concerns , whether in written form or verbally , as it facilitates communication” [Dentist 3]. “Many doctors respect our opinion and express gratitude , acknowledging that we draw their attention to certain points“ [Pharmacist 9].
The majority of participants highlighted the importance of communication tools provided by the institution, including telephones, the CERNER system, and email platforms. Participants expressed their appreciation for these communication channels, noting that they effectively save time and enable seamless collaboration, even when they are attending to patients in different locations.
“It’s not difficult because we have our colleagues , whom we can contact directly by phone” [Dentist 1].
Theme 3.3: formal team processes have a significant role in facilitating collaboration
Sub-theme 3.3.1: supportive leaders empower team members to collaborate.
Leaders who demonstrate appreciation and dedication play a crucial role in fostering positive experiences of IPC. Regular interprofessional meetings organized by these leaders ensure that the environment is conducive to collaboration, and support empowering health professionals to initiate and engage in collaborative endeavor.
“So , if we have any issues , we talk to our supervisor , who then reports it to the health center manager. She is really supportive” [Pharmacist 3].
Sub-theme 3.3.2: engagement in interprofessional initiatives enhances collaboration among team members
Participants emphasized that their involvement in workplace initiatives, such as projects, campaigns, seminars, and workshops, played a crucial role in promoting IPC. According to health professionals, these initiatives were beneficial as they provided them with diverse professional perspectives, opinions, and ideas, which in turn enhanced their chances of success in their collaborative efforts.
“In our health center , we initiated a project to improve the practice of antibiotic prescribing. We were collaborating with GPs to know from them how to write and put a protocol to lessen the misuse of antibiotic” [Pharmacist 2].
Participants also recognized that engaging in collaborative research activities involving multiple team members was an effective facilitator for enhancing patient safety.
“I conducted research on medication use reviews , actively engaging with general practitioners’ clinics. I would regularly visit these clinics to share information about the study. During these interactions , I explained my criteria , encouraging them to refer eligible patients to the pharmacy” [Pharmacist 6].
Furthermore, vaccination campaigns were considered essential by several pharmacists as they provided opportunities for collaboration with other disciplines including educational outreach events. Several pharmacists reported on their involvement in these campaigns and the subsequent positive impact on collaboration dynamics. Specifically, one pharmacist highlighted a reduction in the uptake of pneumococcal vaccine among eligible patients and assumed a proactive role by gathering information from various GPs regarding the decreased prescription of such vaccines.
“We did a project in collaboration with GPs , regarding vaccinating high risk patients with pneumococcal vaccine” [Pharmacist 4]. “During the immunization week , I held a seminar about immunization. I taught them -nurses- individually how to use each vaccine properly and why we are using it” [Pharmacist 2].
Moreover, participants found case-based discussions and interprofessional training sessions with other health professionals valuable for collaboration. These sessions allowed discussion of each profession’s role and facilitated idea exchange.
“ As part of our interprofessional education efforts , we conduct weekly lectures and brief discussions for an hour… sometimes , new nurses and physiotherapists attend these lectures…… We discuss how we can help promote the collaboration between all of us for better care for the patients” [GP 9].
Sub-theme 3.3.3: optimizing accessible healthcare environments
Experiences related to the impact of the environment on collaboration were generally positively perceived. For instance, the close proximity of a nurse diabetic educator to the pharmacy facilitated direct communication between pharmacists and educators, enabling them to address any concerns more efficiently. Moreover, having practitioners co-located in a single setting, rather than dispersed in various locations within the center, was deemed more advantageous.
“We have it , diabetic educator , clinical pharmacist , and GP all in one place , so they all work together for assessment of patient and education , particularly high-risk patient” [Pharmacist 4].
Theme 3.4: time constraints impede collaboration and affect patient outcomes
Participants identified time constraints as a significant challenge to collaboration, with health professionals struggling to allocate sufficient time for documentation, communication, and knowledge-sharing, potentially impacting patient outcomes.
“We can’t afford the luxury of opening CERNER each time since we are already occupied with other tasks” [Pharmacist 5]. “Even when there is an issue …. we should learn from it. We are not learning. We just want to finish this issue and just move on because there is no time. There is too much work” [Laboratory technologist 1].
Theme: 3.5: lack of clarity in scope of practice leads to misunderstandings and hinders collaboration
A number of health professionals expressed concerns regarding the potential misunderstanding of their scope of practice, leading to requests to perform tasks beyond their designated role which impact the collaborative culture leading to frustration.
“Nurses are responsible for taking vital signs , following the patient’s care plan , and managing medications , but cleaning is not part of their role although some doctors mistakenly believe it to be so” [Nurse 3]. “At times , we notice that some GPs are unaware of the difference between a technician and a radiologist” [Laboratory technologist 1].
Gears domain 4: individual factors
Theme 4.1: prior exposure to ipe enhances appreciation for ipc.
The study observed that health professionals who had prior experience with IPE exhibited a greater appreciation towards collaborative work.
“We learned and practiced IPE during our education. However , in practical settings , there is still a need for a comprehensive understanding of IPE and its implementation. While there are individual efforts to apply it , full implementation has not been achieved yet” [Pharmacist 3].
Theme 4.2: health professionals’ factors
Subtheme 4.2.1: effective communication skills drive enhanced collaboration among health professionals.
Effective communication was deemed crucial by participants in healthcare settings. Nurses felt valued and integral to the team when equipped with proper communication skills, while GPs found direct communication with other health professionals to be advantageous, enhancing their practice.
“Quite a few times , I’ve reached out to the on-site ophthalmologist by phone. When there’s a concern about a patient , whether its suspected cornea issues or the need to rule out certain conditions , a simple phone call often results in them accommodating the patient. The ophthalmologist has consistently been responsive and helpful in these interactions” [GP 6].
Subtheme 4.2.2: positive interpersonal qualities among health professionals enhance collaboration
The collaboration within the team is influenced by health professionals’ interpersonal qualities which was identified as a significant factor, with approachability and friendliness being crucial in facilitating collaboration.
“The difference here is that I find everybody to be approachable and friendly [GP 6]. Very friendly environment. You can approach the nurses , the doctors—everyone is accessible” [GP 10].
Furthermore, respect and trust were highly valued facilitators of IPC and were discussed in conjunction with other facilitators.
“Mutual respect among all health professionals will facilitate smoother and more effective collaboration” [Nurse 3]. “We must respect each other. Just because I am a GP , it doesn’t mean my opinion is the only opinion or the correct one” [GP 3].
Theme 4.3: patient perceptions impact IPC
Patient perceptions were found to exert a considerable impact on the dynamics of collaboration between nurses, GPs, and other health professionals. Participants reported that patients tended to perceive nurses as occupying a subordinate position relative to GPs, and consequently, were less forthcoming in discussing healthcare concerns with them.
“ You are the nurse; you know less than the doctor” [Nurse 4]. “ Patients typically highly value recommendations from physicians. However , when they seek advice or education from nurses or pharmacists , they sometimes may not value it as much as they would if it came from a physician ” [Pharmacist 7].
Additionally, participants believe patients regard GPs as the key health professionals, and preferred to communicate exclusively with them. This perception placed an additional workload on GPs, leading to potential consequences on their capacity to collaborate effectively with other health professionals.
“We need to educate patients more about the roles each team member plays and how we all work together as a team. When a patient comes in , they often see the doctor as the leader but it’s important for them to understand the contributions of all team members” [GP 5].
Theme 4.4: impact of of perceived approachability and ego on IPC
On the other hand, encountered challenges in communicating with GPs, including when they perceived a sense of ego, or if they were less approachable. Nurses expressed reluctancy to approach pharmacists or GPs whom they felt would not respect them.
“ Being approachable is one of the most important things especially when it comes to the team. For example , some of the nurses would know a lot of information about the patient but if you’re not an approachable GP , they will not come and voluntarily divulge the information” [GP 6]. “Ego. When you are dealing with people these things are barriers and the best solution is always communication” [Nurse 6].
Similarly, GPs encountered similar challenges in communicating with other health professionals if they perceived them as unfriendly or unapproachable. However, they differed from the nurses in that they seemed to encounter these challenges within their own field of practice rather than in interactions with other health professionals.
Theme 5: enhancing IPC through equity, training, and support
The study participants put forth several proposals to enhance IPC in their workplace. A key recommendation was to ensure equity among health professionals, such that all members had full and equal access to patient files. This would enable effective IPC by keeping all team members abreast of the patient’s evolving health status and treatment plan. Participants recognized that institutional and leadership support would be necessary to achieve this equity. Additionally, due to the acknowledged limitations posed by workload and time constraints, many participants suggested that the recruitment of additional staff could facilitate IPC processes. Further, the participants proposed the need for more frequent training sessions to improve communication skills, enhance system and documentation writing, and provide IPC disease management, role clarification, and professional competencies education.
“When they send you for training you will be empowered” [Nurse 2].
Finally, health professionals emphasized the importance of a supportive system that offers constructive feedback to identify weaknesses and facilitate continuous improvement of practice. In addition, health professionals remarked on the impact of managerial support on collaboration and performance.
“When we receive support from the health center manager during our practice , we find that collaboration improves , leading to better outcomes” [Pharmacist 2].
This qualitative focus group study explored facilitators of and barriers to IPC as perceived by health professionals (including GPs, nurses, pharmacists, dentists, and allied health professionals) from various backgrounds in primary healthcare in Qatar using the “Gears” conceptual model. Overall, the majority of health professionals who participated in this study have acknowledged and appreciated the importance of IPC work within their institutions, which is consistent with other published studies [ 27 , 31 , 32 ].
Facilitators under the micro-gear domain focused on healthcare teams. Participants agreed that the diversity of health professionals within the same PHCC is a major facilitator for better collaboration. They also agreed that the presence of different communication channels (e.g. telephones, CERNER, etc.) is another facilitator. Supportive leaders in the team were acknowledged to have a positive influence on attitudes toward IPC. IPE activities were identified as positively influencing attitudes towards toward IPE and IPC. These findings are consistent with those of other studies. There was an agreement among several studies regarding the importance of open communication and various communication strategies and tools in facilitating IPC [ 33 , 34 ]. For example, Müller et al. [ 33 ], in their study where authors interviewed several clinical executive managers, found that participants agreed that multilateral communication is one of the enablers for effective IPC. Facilitators within the individual-gear, includes Individual contextual factors contributing to IPC such as previous exposure to IPC, patient related factors, and characteristics of health professionals. Previous exposure to IPC emerged as a significant facilitator for both health professionals and patients. Communication skills were identified as crucial in supporting exposure to IPC. Participants highlighted the importance of accessible communication methods, such as availability by phone or in person conversations, eliminating roadblocks to IPC. Furthermore, the approachability of health professionals, characterized by their openness to information sharing and their trust and respect for the competency, knowledge, and skills of other health professionals was a key facilitator to IPC.
Regarding the meso-gear facilitators, participants valued the importance of receiving ongoing, and timely feedback based on practice experiences to consolidate learning and minimize recurrence of errors. They advocated for utilizing data from platforms such as Datix; an Incident Reporting System (IRS), which is a valuable resource among all team members involved in patient care. Participants recommend a wider use of such data for learning, in interprofessional team meetings. This aligns with evidence from the literature which suggests that critical to the success of any IRS is the quality of the feedback given to reporters to enable learning, encourage reporting, and give reporters evidence that the information they are providing is being used appropriately [ 35 , 36 ]. Space and proximity are reported as excellent opportunity for teams to work together and share perspectives in the care for the patient [ 37 ]. As new PHCC centers are created to serve the growing needs of Qatar’s population, leaders can benefit from including members of the care teams, in the final design discussions, so that space and proximity can continue to remain optimal and facilitate interprofessional practice and team centered patient care.
The least number of factors were identified under the macro-gears. These relate to governance and regulations, which were considered as a major facilitator for better IPC in the primary healthcare setting in Qatar. The participants in this study had reflected on the existing policy and regulatory facilitators that foster collaborative practice in PHC setting in Qatar, but did not discuss barriers to policies and regulations. The study findings reaffirm the potential role and influence of government policies and regulations in facilitating IPC in primary care settings from the perspective of the health professionals. Additionally, organizational-level policies were also perceived as key facilitators. This aligns with the macro-level factors of the Gears conceptual model, which allows the conceptualization of the intricate relationships between this and the other domains of the model from the perspective of the health professionals. Previous studies have documented the influence of policy and regulation in promoting collaborative practice and IPE. One international review has summarized the global policies and legal factors influencing the behaviors of health professionals towards successful implementation of collaborative practice [ 38 ]. These factors largely influence the scope of practice of various health professions and how the different professions work collaboratively, funding mechanisms, and reimbursement systems for health services.
In Qatar, health professions and practices are regulated by the Department of Healthcare Professions under the Ministry of Public Health (MoPH) [ 39 ], which is considered a key aspect of professional practice [ 38 ]. Although there are no umbrella laws to regulate multiple health professions under a single statute, which is a major drawback to an effective and conducive implementation of collaborative practice in various settings, having a unified regulatory and legal structure has been shown to foster a culture of equity among different health professionals [ 40 ]. An important aspect of policy and professional regulation is the scope of practice, which should typically clarify roles and represent specific areas of competence for each particular health profession. Participants indicated the presence of scope of practice for various professions in the State of Qatar. Previous studies and reports have highlighted the importance of restructuring the scope of practice of health professions towards effective IPC and to remove barriers to healthcare provision. This will allow health professionals to practice within the scope of their practices and to the full extent of their professional competence without encroaching other professions’ scope of practice, which will ultimately lead to effective collaborative practice [ 41 , 42 ]. In addition, funding and reimbursement are macro-level aspects that can significantly impact IPC [ 40 , 43 ]. In the present study, there was a consensus that these regulatory factors play a key role in facilitating the IPC among the health professionals in primary care settings in Qatar.
Barriers pertaining to the healthcare teams, or the micro-gear, are the lack of understanding of other professionals’ scope of practice, and the lack of time. This is not different from what is reported in the literature, where lack of time and poor understanding of other health professionals ' roles were considered, besides other barriers, major hinderers for IPC in one review paper that collected multiple articles that studied the enablers and hinderers of IPC [ 34 ]. For the individual-gear barriers, health professionals identified that the hierarchy entrenched within the healthcare system contributed a major barrier to collaboration. Within the studied context, GPs are seen as the pinnacle health professional by patients. Therefore, patients are reluctant to provide information to health professionals other than the GP. This ultimately reduces the effectiveness of the healthcare system as the scope of practice of the remainder of the interprofessional team are constrained to meet patient needs. This might limit other health professionals’ roles, and hence they might be less able to exchange care. This idea might go with the concept of the “patient-doctor dyad” that has been reported in the literature, where authors described that one of the hinderers of IPC is the patient’s desire to be mainly seen and examined by GPs, which is often prioritized over collaborative care [ 44 , 45 , 46 ]. Pharmacists, in this study, described that patients also might ignore pharmacists’ recommendations if it was not aligned with the GPs’ recommendations. While IPC may beget IPC, participants remarked that there was difficulty bringing IPC to life in their PHCC context. Knowledge of IPC must be accompanied by a shift in organizational culture, supported by policies and performance review, led by champions, and guided by exemplars of IPC.
Two subthemes were considered under the meso-factors, which are mainly regarding the information system and the organizational culture. Our results indicate that although a health information system (HIS) is operating within the primary healthcare center (PHCC) system, however, not all members of the team use nor rely on it, to complete their duties in patient care. This fragmentation of data systems poses a threat to team unity and excludes some team members (in this context the pharmacists) from being on the same page as the rest. Efforts to merge all data subunits and enable all team members to access the HIS, can enhance work time efficiency (a micro challenge) that participants reported for pharmacists to require in order to be on the same page as the other care providers in the team and is supported by research which stresses the benefits of a health information system which enables the participation of all staff who are directly concerned with patient care in that setting [ 47 , 48 ].
In the interest of optimizing patient safety, whilst participants in this study valued the opportunity for a shared HIS to serve as a platform where errors could be recorded, our data indicates that health care team members did not feel safe enough to do so. According to Smiley and colleagues [ 49 ] the fear of being fired and subjected to judicial inquiry and prosecution make many nurses conceal errors. This aligns with our participants’ reported concerns about the prevalence of “blame culture” and how this results in individuals feeling personally and professionally vulnerable. Blame culture in health care organizations is mainly associated with the approach used by management when dealing with medical errors and accidents [ 50 , 51 ]. Efforts to embrace a culture that promotes transparency and accountability, and management approach which as described by Catino [ 52 ] relates the causal factors of a given event to the whole organization rather than the individual, are priorities for the PHCC organizational leadership to consider.
Furthermore, hierarchy in privileges, such as varied levels of access to professional development opportunities, threatens team unity, and in turn generates a sense where some professions feel less valued for working in their roles. Educators postulate that if individuals from different professions learn together, they will be able to more effectively work together in teams to achieve desired outcomes [ 53 ]. Integrating CPD in interprofessional decision support with quality improvement and patient safety initiatives will likely enhance the uptake and ability to sustain these educational initiatives [ 54 ]. For instance, the “Schwartz Center Rounds” in the US and UK provide a forum in which professional and nonprofessional staff across healthcare disciplines can discuss challenging psychosocial and emotional aspects of a patient’s care and the impact of these challenges on the care team. These rounds do not focus solely on decision-making, but attendees report significantly enhanced appreciation of colleagues’ roles and contributions, communication, and teamwork [ 55 ]. In this way, the professional learning needs can meet not only the individual profession, but also translate into opportunities for teams to problem solve together and in turn improve safer patient care.
In general, the current study results on facilitators and barriers to IPC align well with those identified by a review study by [ 34 ] that summarized the facilitators and barriers for interprofessional care in primary healthcare. Common facilitators in both studies are the lack of time and training for the health professionals, lack of understanding of others’ roles, and poor communication. It is interesting to note that fears relating to professional identity were identified as a hinderer in the review; however, it was not mentioned by any HCP in the current study. This could be due to the proper understanding of the self-role of the HCP in this study. IPC enablers identified by the review were all reported in this study (i.e. communication tools, co-location of HCP, and recognition of other professionals’ roles and contributions).
Strengths and limitations
One strength of this study is the use of the “Gears model” to understand facilitators and barriers at each level within the IPCTs. Identifying the facilitators and barriers at each level of the work environment makes it easier for decision-makers to identify the gaps and the points that need improvement specific for each level, and hence will help implement appropriate, and probably more efficient, interventions suitable for each level to improve IPC within the PHCC settings. The current study included a high diversity of health professionals and did not focus on certain professions, which aligns with what interprofessional work is all about. This study, as mentioned before, is a continuation of a previous quantitative study done on more than 1400 health professionals to assess their attitude toward IPC. Although the previous study showed that health professionals have a positive attitude toward IPC, which was evident by the survey, the current study examined these quantitative findings from a qualitative lens. This provided a clearer insight to ensure a comprehensive understanding of what shapes these perspectives.
Limitations of the study might include the lack of anonymity in focus groups, which might increase the social desirability. Second, although the study included multiple professions, most participants were GPs, pharmacists, or nurses. Moreover, some HCP were not present (e.g. pharmacy technicians, and physiotherapists), which could limit the generalizability of the current study to these professions.
The interplay between the meso, macro, micro, and individual gears showcases the importance of a multifaceted approach to interventions to amplify the successes of IPC. Policies such as data sharing and collaborative key performance indicators support the interaction between the meso and individual gears. The individual assists the macro and meso gears through communication and trust in the scope of practice of the other team members. Simultaneously, health professionals must advocate for their colleagues to patients. Patients have a direct connection to the micro and individual gears which ultimately affect the care being provided to them.
Data availability
No datasets were generated or analysed during the current study.
World Health Organization. Global strategy on human resources for health: workforce 2030. 2016.
World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva: World Health Organization; 2010.
Google Scholar
Bodenheimer T, Chen E, Bennett HD. Confronting the growing burden of chronic disease: can the U.S. health care workforce do the job? Health affairs. (Project Hope). 2009;28(1):64–74.
Article Google Scholar
Freeth D. Sustaining interprofessional collaboration. J Interprof Care. 2001;15(1):37–46.
Article CAS PubMed Google Scholar
Zwarenstein M, Goldman J, Reeves S. Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):Cd000072.
Tremblay D, Roberge D, Touati N, Maunsell E, Berbiche D. Effects of interdisciplinary teamwork on patient-reported experience of cancer care. BMC Health Serv Res. 2017;17(1):218.
Article PubMed PubMed Central Google Scholar
Mulvale G, Embrett M, Razavi SD. Gearing up’ to improve interprofessional collaboration in primary care: a systematic review and conceptual framework. BMC Fam Pract. 2016;17:83.
Gaboury I, Bujold M, Boon H, Moher D. Interprofessional collaboration within Canadian integrative healthcare clinics: key components. Soc Sci Med. 2009;69(5):707–15.
Article PubMed Google Scholar
Patel PH, Welsh C, Foggs MB. Improved asthma outcomes using a coordinated care approach in a large medical group. Dis Manag. 2004;7(2):102–11.
Renders CM, Valk GD, Griffin S, Wagner EH, Eijk JT, Assendelft WJ. Interventions to improve the management of diabetes mellitus in primary care, outpatient and community settings. Cochrane Database Syst Rev. 2001;2000(1):Cd001481.
PubMed Google Scholar
McAlister FA, Stewart S, Ferrua S, McMurray JJ. Multidisciplinary strategies for the management of heart failure patients at high risk for admission: a systematic review of randomized trials. J Am Coll Cardiol. 2004;44(4):810–9.
Propp KM, Apker J, Zabava Ford WS, Wallace N, Serbenski M, Hofmeister N. Meeting the complex needs of the health care team: identification of nurse-team communication practices perceived to enhance patient outcomes. Qual Health Res. 2010;20(1):15–28.
Pike AW, McHugh M, Canney KC, Miller NE, Reiley P, Seibert CP. A new architecture for quality assurance: nurse-physician collaboration. J Nurs Care Qual. 1993;7(3):1–8.
Uddin S, Hossain L, Kelaher M. Effect of physician collaboration network on hospitalization cost and readmission rate. Eur J Public Health. 2012;22(5):629–33.
Busse R, Scheller-Kreinsen D, Zentner A. Tackling chronic disease in Europe: strategies, interventions and challenges. WHO Regional Office Europe; 2010.
Campbell-Scherer D. Multimorbidity: a challenge for evidence-based medicine. Evid Based Med. 15. England2010. pp. 165-6.
Wijlhuizen GJ, Perenboom RJ, Garre FG, Heerkens YF, van Meeteren N. Impact of multimorbidity on functioning: evaluating the ICF Core Set approach in an empirical study of people with rheumatic diseases. J Rehabil Med. 2012;44(8):664–8.
van Oostrom SH, Picavet HS, de Bruin SR, Stirbu I, Korevaar JC, Schellevis FG, et al. Multimorbidity of chronic diseases and health care utilization in general practice. BMC Fam Pract. 2014;15:61.
Hutchison B, Levesque J-F, Strumpf E, Coyle N. Primary health care in Canada: systems in motion. Milbank Q. 2011;89(2):256–88.
Ontario Ministry of Health and Long-, Term C. Patients first: Action Plan for health care. Ministry of Health and Long-Term Care Toronto, ON; 2015.
Shaffer J, Wexler LF. Reducing low-density lipoprotein cholesterol levels in an ambulatory care system. Results of a multidisciplinary collaborative practice lipid clinic compared with traditional physician-based care. Arch Intern Med. 1995;155(21):2330–5.
Chan DS, Callahan CW, Moreno C. Multidisciplinary education and management program for children with asthma. Am J health-system Pharmacy: AJHP : Official J Am Soc Health-System Pharmacists. 2001;58(15):1413–7.
Article CAS Google Scholar
Gucciardi E, Espin S, Morganti A, Dorado L. Exploring interprofessional collaboration during the integration of diabetes teams into primary care. BMC Fam Pract. 2016;17:12.
Busari JO, Moll FM, Duits AJ. Understanding the impact of interprofessional collaboration on the quality of care: a case report from a small-scale resource limited health care environment. J Multidisciplinary Healthc. 2017;10:227–34.
Schepman S, Bakker D, Batenburg R. The role of health care professionals in collaboration in primary health care. Int J Integr Care. 2019;19:496.
Supper I, Catala O, Lustman M, Chemla C, Bourgueil Y, Letrilliart L. Interprofessional collaboration in primary health care: a review of facilitators and barriers perceived by involved actors. J Public Health. 2015;37(4):716–27.
CAS Google Scholar
Seaton J, Jones A, Johnston C, Francis K. Allied health professionals’ perceptions of interprofessional collaboration in primary health care: an integrative review. J Interprof Care. 2021;35(2):217–28.
El-Awaisi A, Awaisu A, Aboelbaha S, Abedini Z, Johnson J, Al-Abdulla SA. Perspectives of Healthcare Professionals toward Interprofessional Collaboration in primary care settings in a Middle Eastern Country. J Multidiscip Healthc. 2021;14:363–79.
PHCC. Primary Health Care Corporation Corporate Strategic Plan (2019–2023): a healthier future for our families. Primary Health Care Corporation; 2019.
Kyngäs HA, Mikkonen K, Kääriäinen M. The application of content analysis in Nursing Science Research. The application of content analysis in Nursing Science Research; 2020.
Bosch B, Mansell H. Interprofessional collaboration in health care: lessons to be learned from competitive sports. Can Pharmacists J / Revue des Pharmaciens Du Can. 2015;148(4):176–9.
Sangaleti C, Schveitzer MC, Peduzzi M, Zoboli ELCP, Soares CB. Experiences and shared meaning of teamwork and interprofessional collaboration among health care professionals in primary health care settings: a systematic review. JBI Evid Synthesis. 2017;15(11):2723–88.
Müller C, Zimmermann L, Körner M. Förderfaktoren Und Barrieren Interprofessioneller Kooperation in Rehabilitationskliniken – Eine Befragung Von Führungskräften. Rehabilitation (Stuttg). 2014;53(06):390–5.
Rawlinson C, Carron T, Cohidon C, Arditi C, Hong QN, Pluye P, et al. An overview of reviews on Interprofessional Collaboration in primary care: barriers and facilitators. Int J Integr Care. 2021;21(2):32.
Anderson JE, Kodate N, Walters R, Dodds, AJIjfqihc. Can incident reporting improve safety? Healthc Practitioners’ Views Eff Incident Report. 2013;25(2):141–50.
Waring, JJJSs. Medicine. Beyond blame: cultural barriers to medical incident reporting. 2005;60(9):1927–35.
Oandasan IF, Conn LG, Lingard L, Karim A, Jakubovicz D, Whitehead C et al. The impact of space and time on interprofessional teamwork in Canadian primary health care settings: implications for health care reform. 2009;10(2):151–62.
Girard MA. Interprofessional education and collaborative practice policies and law: an international review and reflective questions. Hum Resour Health. 2021;19(1):9.
Ministry of Public Health. Department of Healthcare Professions 2020 [ https://dhp.moph.gov.qa/en/Pages/Home.aspx
San Martín-Rodríguez L, Beaulieu M-D, D’Amour D, Ferrada-Videla, MJJoic. Determinants Success Collaboration: Rev Theoretical Empir Stud. 2005;19(sup1):132–47.
Dower C, Moore J, Langelier MJHA. It is time to restructure health professions scope-of-practice regulations to remove barriers to care. 2013;32(11):1971–6.
Safriet BJJYJoR. Closing the gap between can and may in health-care providers’ scopes of practice: a primer for policymakers. 2002;19:301.
Guindo LA, Wagner M, Baltussen R, Rindress D, van Til J, Kind P et al. From efficacy to equity: literature review of decision criteria for resource allocation and healthcare decisionmaking. 2012;10(1):1–13.
O’Reilly P, Lee SH, O’Sullivan M, Cullen W, Kennedy C, MacFarlane A. Assessing the facilitators and barriers of interdisciplinary team working in primary care using normalisation process theory: an integrative review. PLoS ONE. 2017;12(5):e0177026.
Hills M, Mullett J, Carroll S. Community-based participatory action research: transforming multidisciplinary practice in primary health care. Rev Panam Salud Publica. 2007;21(2–3):125–35.
Shaw A, de Lusignan S, Rowlands G. Do primary care professionals work as a team: a qualitative study. J Interprof Care. 2005;19(4):396–405.
Stavropoulou C, Doherty C, Tosey PJTMQ. How effective are incident-reporting systems for improving patient safety? A systematic literature review. 2015;93(4):826–66.
Herzer KR, Mirrer M, Xie Y, Steppan J, Li M, Jung C et al. Patient safety reporting systems: sustained quality improvement using a multidisciplinary team and good catch awards. 2012;38(8):339–AP1.
Smiley RA, McCarthy CJJNR. A mixed-methods study of gender differences in nurse reporting and nurse discipline. 2016;7(3):33–40.
Edie Brous RN JJJoNL. The criminalization of unintentional error: implications for TAANA. 2008;12(1):5.
Gorini A, Miglioretti M, Pravettoni, GJJoeicp. A new perspective on blame culture: an experimental study. 2012;18(3):671–5.
Catino, MJJoc. management c. A review of literature: individual blame vs. organizational function logics in accident analysis. 2008;16(1):53–62.
Association of American Medical Colleges. Interprofessional Education 2010 [ https://www.aamc.org/what-we-do/mission-areas/medical-education/interprofessional-education
Lown BA, Kryworuchko J, Bieber C, Lillie DM, Kelly C, Berger B et al. Continuing professional development for interprofessional teams supporting patients in healthcare decision making. 2011;25(6):401–8.
Lown BA, Manning CFJAM. The Schwartz Center rounds: evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. 2010;85(6):1073–81.
Download references
Acknowledgements
Thanks to Dr. Jessie Johnson from the University of Calgary-Qatar for her initial support with this project. Also, we would like to thank all health professionals from primary health care who volunteered to participate in this study.
This publication was supported by Qatar University Student Grant [QUST-1-CPH-2020-25]/ [QUST-2-CPH-2019-3]. The findings achieved herein are solely the responsibility of the author[s].
Author information
Authors and affiliations.
Department of Clinical Pharmacy and Practice, College of Pharmacy, QU Health, Qatar University, Doha, Qatar
Alla El-Awaisi, Abier Mohamed Elboshra, Kawthar Hasan Jasim, Alzahraa Fathi AboAlward & Ahmed Awaisu
Hamad Medical Cooperation, Doha, Qatar
Ola Hasan Yakti
Primary Health Care Corporation, Doha, Qatar
Raghad Walid Shalfawi & Noora Al Mutawa
College of Pharmacy, Dalhousie University, Halifax, Canada
Daniel Rainkie
Department of Clinical Academic Education, College of Medicine, QU Health, Qatar University, Doha, Qatar
Noora Al Mutawa
Division of Medical Education, Weill Cornell Medicine – Qatar, Doha, Qatar
Stella Major
You can also search for this author in PubMed Google Scholar
Contributions
AE contributed to the conception of this research idea, study design, data collection, data analysis, and including supporting all stages of this paper. AME, KJ, AAZ, RS accompanied AE in the focus groups. AME, KJ, AAZ, RS, AA, DR, NA, SM supported with the study design, study conceptualization, analysis, and interpretation of findings. OY supported with the data validation, analysis, and interpretation of findings. All authors contributed to drafting the manuscript and reviewed and approved the final version of the manuscript.
Corresponding author
Correspondence to Alla El-Awaisi .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from the PHCC Research Committee (PHCC/RC/18/12/001) and the Qatar University Institutional Review Board (QU-IRB 1084-EA/19). All participants received information leaflet about the study and that their participation in the qualitative study would be voluntarily and will be treated confidentially. All participants signed and dated the written informed consent form. The study was carried out in accordance to the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
El-Awaisi, A., Yakti, O.H., Elboshra, A.M. et al. Facilitators and barriers to interprofessional collaboration among health professionals in primary healthcare centers in Qatar: a qualitative exploration using the “Gears” model. BMC Prim. Care 25 , 316 (2024). https://doi.org/10.1186/s12875-024-02537-8
Download citation
Received : 08 December 2023
Accepted : 22 July 2024
Published : 27 August 2024
DOI : https://doi.org/10.1186/s12875-024-02537-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Interprofesisonal collaboration
- Interprofessional education
- Collaborative practice
- Primary care
- “Gears” Conceptual Model
- Perpsectives
- Qualitative
- Middle East
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
The purpose of this paper is to help authors to think about ways to present qualitative research papers in the American Journal of Pharmaceutical Education. It also discusses methods for reviewers to assess the rigour, quality, and usefulness of qualitative research. Examples of different ways to present data from interviews, observations, and ...
When it comes to how to present qualitative data visually, the goal is to make research findings clear and easy to understand. To do this, use visuals that are both attractive and informative. Presenting qualitative data visually helps to bring the user's attention to specific items and draw them into a more in-depth analysis.
Find sources of qualitative training & support at UNC. How to search for and evaluate qualitative research, integrate qualitative research into systematic reviews, report/publish qualitative research. Includes some Mixed Methods resources. Some examples and thoughts on presenting qualitative research, with a focus on posters
how to best present qualitative research, with rationales and illustrations. The reporting standards for qualitative meta-analyses, which are integrative analy-ses of findings from across primary qualitative research, are presented in Chapter 8. These standards are distinct from the standards for both quantitative meta-analyses and
Open MenuClose Menu. Reporting the findings from a qualitative study in a way that is interesting, meaningful, and trustworthy can be a struggle. Those new to qualitative research often find themselves trying to quantify everything to make it seem more "rigorous," or asking themselves, "Do I really need this much data t.
Tables to Present the Groups of Codes That Form Each Theme. As noted previously, most of our dissertation assistance clients use a thematic analysis approach, which involves multiple phases of qualitative analysis that eventually result in themes that answer the dissertation's research questions. After initial coding is completed, the analysis process involves (a) examining what different ...
In qualitative research, in fact, the use of the first person is far more common. This is because the researcher is central to the research project. ... One of the most important parts of writing about qualitative research is presenting the data in a way that makes its richness and value accessible to readers. As the discussion of analysis in ...
In this video, I'll share five critical areas to consider when presenting qualitative findings: Overview, Demographics, Data Analysis Process, Presentation o...
Preparing the presentation of qualitative findings: considering your roles and goals. Dr. Philip Adu is a Methodology Expert at The Chicago School of Professional Psychology (TCSPP). In this post he explains the things to consider when presenting your research findings. This post follows on from his previous blog post "Perfecting the art of ...
The results chapter in a dissertation or thesis (or any formal academic research piece) is where you objectively and neutrally present the findings of your qualitative analysis (or analyses if you used multiple qualitative analysis methods ). This chapter can sometimes be combined with the discussion chapter (where you interpret the data and ...
Here's my recommended structure to create your Research Findings presentation -. 1. Objective of the Research. A great way to start your presentation is to highlight the objective of your research project. It is important to remember that merely sharing the objective may sometimes not be enough.
Presenting the findings o f a qualitative research p roject is a s ignificant issue as it co uld affect the quality of a manuscript to a great extent. Reay et al. (2019) concentrated on this critical
In this video, I explain how to present and discuss findings in qualitative research. I discuss the use of visual representations (e.g. diagrams, charts, etc...
Qualitative Research*. Reproducibility of Results. United Kingdom. The purpose of this paper is to help authors to think about ways to present qualitative research papers in the American Journal of Pharmaceutical Education. It also discusses methods for reviewers to assess the rigour, quality, and usefulness of qualitative research.
WRITING AND PRESENTING QUALITATIVE RESEARCH There are two main approaches to writing up the fi ndings of qualitative research.20 The first is to simply report key findings under each main theme or category, using appropriate verbatim quotes to illustrate those fi ndings. This is then accompanied by a linking, separate discussion chapter in ...
I used to conduct qualitative-heavy research projects pretty much all day every day. Key informant interviews, bellwether interviews, document review, focus groups, you name it… So I know from personal experience that 99.9 percent of qualitative reports look like this: Which is fine, unless you want someone to, ya know, actually read your report.
Learn how to publish 3+ research papers EVERY year in high-impact Scopus-indexed journals: https://academicenglishnow.com/3papersayear-optin?utm_source=YouTu...
Another important principle is that of connection, specifically the way in which multiple layers of meaning within open-ended responses may overlap.Figure 2 presents a sunburst graphic, which illustrates the relationship between the different units of qualitative analysis: the inner circle summarizes the broader category, and the outer circle summarizes any individual codes applied to the data ...
Qualitative data refers to non-numerical information that helps in understanding the 'why' and 'how' of research findings and analysis. By looking into the rich layers of qualitative data, researchers can unearth nuanced insights, uncover trends, and make sense of complex phenomena in a way that quantitative data alone cannot capture.
Furthermore, qualitative research should be presented with convincing arguments, including enough representative data to support the findings and any alternative explanations (Morse, 1994). Understanding social encounters, which is often the case in qualitative research, calls for an intellectual effort requiring both rigor and diagnostic ...
This article reviews approaches to presenting qualitative comparative analysis and set-theoretic research, with an emphasis on graphic presentation. Although visualization is an important aspect of presenting empirical research, techniques for visualizing qualitative comparative analysis remains underdeveloped.
Qualitative research uncovers the why behind your what. Here are seven qualitative research methods and examples to inspire your next UX research project. ... Open-ended surveys allow users to give in-depth, nuanced, and contextual responses. When to use open-ended surveys. User surveys are an effective qualitative research method for reaching ...
Fortunately, you only need to master a handful of conceptual slides. And these will be sufficient for communicating most qualitative insights. These include: Process, flow, and journey slides. Matrixes. Driver trees. Ranges and sliders. From-to slides. Tables and heatmaps.
The presentation of data for this research question differs from the previous two due to the unique nature of the information gathered. Unlike the quantifiable student responses in earlier questions, this data stems from expert opinions and a reflection discussion session, focusing on qualitative recommendations for improvement rather than ...
In this paper, we present findings from a qualitative pre-implementation study, guided by the Consolidated Framework for Implementation Research (CFIR), of factors to inform successful STAR implementation at a large learning health system prior to effectiveness testing as part of a Type I Hybrid trial.
The emotions experienced by the EMS personnel in their new working circumstances formed three themes: New concerns arose that were constantly present (main theme); Surviving without proper guidance (major theme); and Rapidly approaching breaking point (major theme) (Fig. 1).Work-related factors identified as resources for the well-being of EMS personnel formed three themes: A high level of ...
Following the Enhancing Transparency in Reporting the Synthesis of Qualitative Research guidelines, five databases and Google Scholar were searched for the literature published through April 2024. A total of nine studies were included in the present work. The results highlight that most of the barriers to communicational access to local ...
Background The number of patients seeking medical care is increasing, necessitating more access to primary healthcare services. As several of these patients usually present with complex medical conditions, the need for interprofessional collaboration (IPC) among health professionals in primary care is necessary. IPC is essential for facing the increasing and challenging healthcare demands ...