Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 March 2024

Therapeutic effect and study of human umbilical cord blood mononuclear cells in patients with ischaemic bowel disease
- Xiaoxiao Cai 1 , 3 ,
- Yonghao Li 1 , 3 ,
- Fengyu Gao 1 ,
- Bilal Muhammad 3 , 4 &
- Hongli Yang 2
Scientific Reports volume 14 , Article number: 6121 ( 2024 ) Cite this article
1242 Accesses
Metrics details
- Stem-cell differentiation
Ischaemic bowel disease (ICBD) is a group of intestinal ischaemia syndromes caused by various aetiologies of reduced intestinal blood flow or vascular occlusion. ICBD can present as abdominal pain, bloody stool, and diarrhoea. This disease often occurs in middle-aged and elderly individuals with cardiovascular and cerebrovascular diseases. The incidence of ischaemic bowel disease has been increasing for decades, and it is difficult to diagnose, resulting in rapid disease progression and a high mortality rate. Therefore, fully understanding this disease, improving the diagnosis rate of this disease, and finding appropriate treatment methods are urgently needed to improve the condition and prognosis of patients. Umbilical cord blood stem cells are accessible, have weak immunogenicity, and have various biological functions, such as angiogenesis, inflammation and immune regulation. Many studies have confirmed that cord blood stem cells can relieve ischaemia, and these cells have attracted tremendous amounts of attention in regenerative medicine in recent years. In this paper, we discuss the clinical characteristics of ICBD, analyse the characteristics of human umbilical cord blood mononuclear cells (HUCB-MNCs), and use its to treat ischaemic bowel disease. Additionally, we compare the clinical manifestations and related indicators before and after treatment to evaluate the efficacy and safety of these methods.
Similar content being viewed by others

Mechanism and therapeutic effect of umbilical cord mesenchymal stem cells in inflammatory bowel disease

Effectiveness and safety of normoxic allogenic umbilical cord mesenchymal stem cells administered as adjunctive treatment in patients with severe COVID-19

Mechanisms of mucosal healing: treating inflammatory bowel disease without immunosuppression?
Introduction.
Ischaemic bowel disease (IBD) is a series of intestinal ischaemic syndromes due to an insufficient blood supply to the intestine caused by intestinal ischaemia and hypoxia 1 . The factors leading to this disease can be divided into acute mesenteric ischaemia (AMI), chronic mesenteric ischaemia (CMI) and ischaemic colitis (IC) 2 . The incidence of IC is the highest, reaching 22.9 per 100,000 people 3 , followed by acute mesenteric ischaemia. Several studies have reported that the total incidence of AMI in all patients hospitalized for acute surgery ranges from 0.09 to 0.2% 4 , and the overall incidence of chronic mesenteric ischaemia is approximately 1 per 100,000 people 5 ; therefore, these cases are relatively rare. Elderly individuals with congestive heart failure, arrhythmia, myocardial infarction, diabetes and other diseases are at high risk 6 . The early clinical symptoms of ICBD are not typical, and the onset of abdominal pain, diarrhoea, and bloody stool are common. It is difficult to diagnose, and the misdiagnosis rate is as high as 60% 7 (Fig. 1 ).
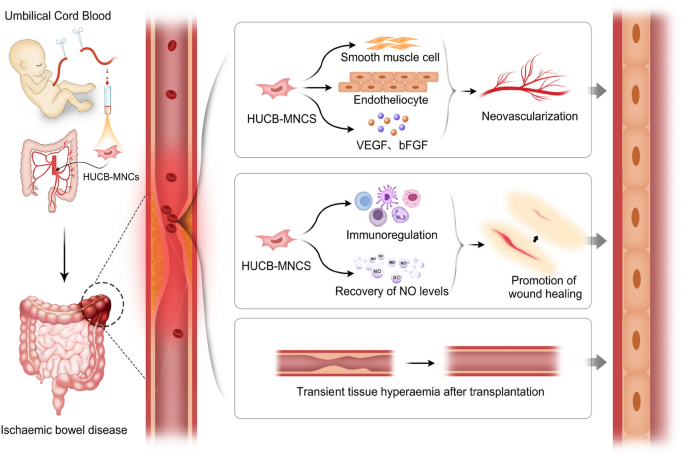
Mechanism of umbilical cord blood mononuclear cells in treatment of ICBD.
At present, this kind of disease is mainly treated by internal medicine. IC is mostly a self-limiting disease, and the symptoms of mild patients can be relieved by rest and diet adjustment and without the need for excessive interventions 8 . However, AMI has long been considered an inevitable and highly fatal disease. Despite the rapid progress in medicine, the incidence of AMI and overall mortality rate are still extremely high. Several reports have shown that the clinical mortality rate of AMI is still as high as 50–80% after active treatment 9 . If CMI is not treated in time, the risk of progressing to AMI is high, and the prognosis is extremely poor. Based on the clinical characteristics of this disease, it is particularly important to make a correct judgement in a timely manner and choose effective treatment methods to quickly relieve the condition and improve the prognosis of patients. The current treatment methods include medical symptomatic treatment, surgery and vascular interventional therapy. The effectiveness of medical treatment is poor, the problem of vascular stenosis cannot be fundamentally solved, and the recurrence rate is high. The surgical risk is high, and the postoperative mortality rate is high. Vascular intervention is a new treatment method that has the advantages of low surgical risk and rapid treatment, but the rate of postoperative intravascular restenosis is high. The incidence of stent restenosis is reportedly as high as 33%, and the mortality rate after acute stent occlusion is 50% 10 . The long-term quality of life of patients is poor, so it is urgent to find an effective treatment for ischaemic bowel disease.
When the body is experiencing ischaemia, compensatory effects mainly depend on the establishment of collateral circulation. Therefore, we investigated how to treat this disease at the cellular level by administering exogenous growth factors and vascular endothelial cells to generate new blood vessels and collateral circulation at the ischaemic site. Stem cells can differentiate into a variety of cells, generate tissues and organs with different functions, and have strong self-renewal ability 11 . Bone marrow, peripheral blood and cord blood contain a variety of stem cells, among which the number of bone marrow and peripheral blood haematopoietic stem cells is low, and the risk of transplantation is high; thus, the clinical application of these cells is relatively limited 12 . However, cord blood stem cells have the advantages of easy access, no harm to the donor, and no immune rejection and have been widely used to treat various difficult and miscellaneous diseases 13 .
Human umbilical cord blood mononuclear cells, which are isolated from the umbilical cord blood of pregnant women after delivery, are mononuclear cells and the largest cells in the human body; these cells include a variety of stem cells, lymphocytes and monocytes 14 . HUCB-MNCs have a variety of biological functions, such as tissue and cell regeneration, anti-inflammatory effects, and immune regulation 14 . Umbilical cord blood mononuclear cells can differentiate into a variety of immune cells as needed and can expand into a large number of highly active immune cells in vitro. When they are reinfused into the human body, they are not susceptible to rejection or side effects 15 , which provides more accurate solutions for many major diseases. At present, many studies have applied umbilical cord blood mononuclear cells to limb ischaemia and cardiovascular and cerebrovascular ischaemia.
Comparison of baseline data before treatment
Comparison of general data and clinical manifestations.
There was no significant difference in the general data or clinical manifestations between the two groups before treatment ( P > 0.05), as shown in Table 1 .
Comparison of laboratory examination between the two groups before and after treatment
There was no significant difference in laboratory test results between the two groups before treatment ( P > 0.05), as shown in Table 2 .
Comparison of therapeutic effects after treatment
Comparison of clinical manifestations and total hospitalization days between the two groups after treatment.
There were significant differences in clinical symptoms between the two groups before and 5 days after treatment ( P < 0.05). The hospitalization time of the experimental group was 9.55 ± 3.12 days, that of the control group was 11.75 ± 3.63 days, and the hospitalization time of the experimental group was significantly shorter than that of the control group ( P < 0.05). The number of patients with abdominal pain, diarrhoea, bloody stool and abdominal tenderness in the experimental group was significantly lower than that before treatment ( P < 0.05). See Table 3 for details.
Comparison of laboratory tests
After treatment, the WBC, NEUT, PCT and DD in the experimental group and the control group had decreased significantly more than those in the control group ( P < 0.05). There was no significant difference in HB or PLT between the two groups.After treatment, WBC, HB, DD and PCT in the experimental group had significantly improved compared with those before treatment ( P < 0.05, showing statistical differences), as detailed in Table 2 .
Comparison of clinical efficacy
In the control group, treatment was markedly effective in 9 patients, effective in 14 patients, and ineffective in 10 patients, for a total effective response rate of 69.7%. In the experimental group, 15 patients had markedly effective treatment, 15 patients had effective treatment, and 3 patients had ineffective treatment, for a total effective rate of 90.9%. The difference was statistically significant ( P < 0.05). See Table 4 for details.
Comparison of clinical symptoms at 1/3/6 months after treatment
One month after treatment, the number of patients with abdominal pain, bloody stool and abdominal tenderness in the experimental group was significantly lower than that in the control group ( P < 0.05). After 3 months of treatment, the number of patients with abdominal pain and bloody stool in the experimental group was significantly greater than that in the control group ( P < 0.05). After 6 months of treatment, the number of patients with abdominal pain, bloody stool and abdominal tenderness improvement in the experimental group was significantly greater than that in the control group ( P < 0.05), as detailed in Table 5 .
Comparison of colonoscopy reexamination after treatment
Within 6 months after treatment, 15 patients in the control group underwent colonoscopy; 8 of them had colonoscopy findings that were better than before, 4 had no significant change, and 2 were worse than before. In the experimental group, 11 patients underwent colonoscopy reexamination; 10 of them had colonscopy findings that were better than before, and 1 was worse than before. There was a significant difference in the effective rate between the two groups ( P < 0.05). Table 6 for details.
Comparison of cord blood mononuclear cells before and after treatment
Comparison map of colonoscopy.
Figure 2 a–d: Before treatment, multiple ulcers in the intestinal tract were observed via endoscopy; these ulcers were distributed along the longitudinal axis and covered with white fur-like material, and the surrounding mucosa was obviously hyperaemic and oedematous. Figure 2 e–h: Colonoscopy reexamination 2 months after HUBC treatment showed smooth intestinal mucosa and clear peripheral vascular texture.
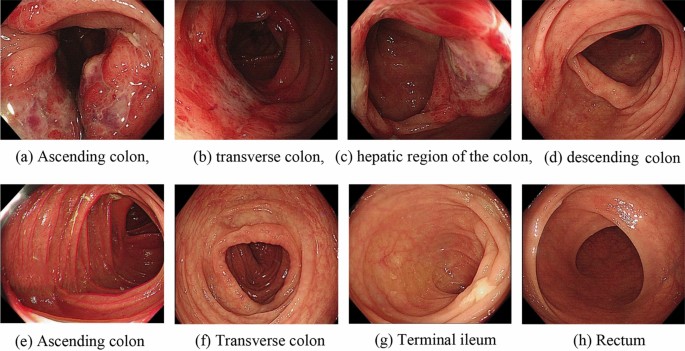
Comparison of colonoscopies before and after cord blood single-cell therapy for ICBD.
Contrast-enhanced mesangial contrast images (Fig. 3 )
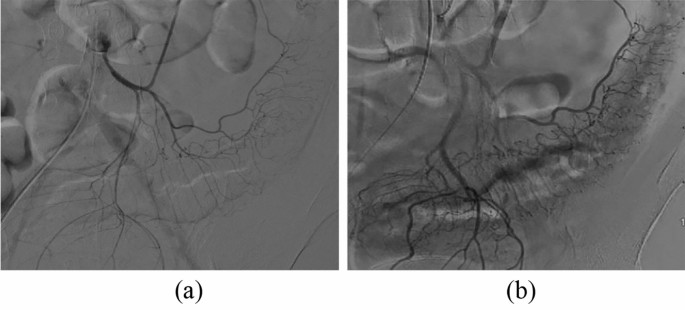
Comparison of inferior mesenteric artery angiography before and after treatment in the experimental group ( a ) Angiography before treatment showed thin and sparse blood vessels throughout the colon. ( b ) Three months after treatment with umbilical cord blood mononuclear cells, angiography showed that the mesenteric vessels were enlarged and that the blood flow had improved. ( a ) Angiography of the inferior mesenteric artery before treatment. ( b ) Posttreatment inferior mesenteric angiography
Adverse reactions
We strictly monitored patients' vital signs, liver and kidney function and electrocardiogram before and after treatment, and used electrocardiogram monitoring during treatment to ensure patients' life safety. There were no treatment-related adverse events, new tumours or deaths in the two groups during the treatment or follow-up.
There are different causes of different types of ischaemic bowel disease. Ischaemia in AMI often occurs in the small intestine, and the most common cause is acute intestinal ischaemia caused by sudden interruption of the blood supply caused by detachment of emboli from the superior mesenteric artery 16 . The majority of CMI cases are caused by a gradual reduction in the intestinal blood supply due to atherosclerosis of the intestinal vessels, and mesenteric vascular ischaemia occurs slowly. The ischaemic site of IC occurs in the colon, and patients often have a vascular nonocclusive ischaemic injury due to vasospasm and contraction that is caused by factors such as hypovolemia or drugs. This type of gastrointestinal injury is the most common form of gastrointestinal ischaemic injury and accounts for more than half of gastrointestinal ischaemic cases 17 . A reduction in blood flow caused by vascular occlusion leads to intestinal ischaemia and hypoxia, intestinal vascular endothelial cell damage, vascular contracture, platelet aggregation, vascular embolism formation and many inflammatory reactions 18 . When intravascular thrombosis occurs, the fibrinolytic system is activated, and fibrin is degraded. The plasma D-dimer concentration is a site of action in the fibrinolysis process, and an increase in D-dimer indicates that the blood is in a hypercoagulable state. At present, many studies at home and abroad have confirmed that the detection of plasma D-dimer has high diagnostic and prognostic value for ischaemic bowel disease 19 . Platelets (PLTs) can undergo coagulation, haemostasis and repair of damaged blood vessels. When the vessel wall is damaged, PLTs quickly adhere to the surface of damaged endothelial cells and undergo a series of complex reactions to repair endothelial cells 20 . When thrombosis or inflammatory reactions occur in the body, the PLT count usually increases. When microcirculation disorders occur in the body, the intestinal blood supply is affected, and tissue ischaemia and hypoxia can result in the production of a large number of oxygen free radicals, which can destroy the intestinal mucosal barrier 21 . At this time, intestinal peristalsis is slowed, which can cause bacterial reproduction and intestinal flora translocation. White blood cells (WBCs) function in chemotaxis and deformation. When invaded by bacteria, WBCs can penetrate the vascular wall and quickly reach the invasion site, engulfing and phagocytosing the bacteria 22 . It has been reported that more than 90% of patients with ischaemic bowel disease have abnormally elevated WBCs 23 . The neutrophil percentage (NEUT) is the proportion of neutrophils among white blood cells, and this ratio is highly important for diagnosing inflammatory infection and determining the degree of infection. When extensive tissue necrosis and severe bacterial infections occur, the percentage of neutrophils is often high 24 . Procalcitonin (PCT) is a known marker of bacterial inflammation, and its concentration in healthy people is very low 25 . PCT has the advantages of a short operation time, good stability, and difficulty in degrading. Its level can well reflect the severity of infection 26 . Therefore, real-time dynamic detection of the PCT concentration in blood is beneficial for observing therapeutic efficacy. Ayten et al. reported that the PCT level in the experimental group was significantly greater than that in the control group when intestinal ischaemia occurred, which was inferred to be related to the inflammatory response caused by intestinal ischaemia 27 . Our findings were also consistent with the related literature. At the same time, bloody stools cause a decrease in haemoglobin, which occurs in some patients. In conclusion, we used the above indicators as the criteria for evaluating whether the treatment was effective when the experiment was designed.
In the early stage of intestinal ischaemia, the intestinal tract in the lesion area still retains a certain extent of vitality. Moreover, if active treatment is performed to improve the intestinal blood supply, further exacerbation of ischaemia can be avoided 28 . Different types of ICBD have different treatment focuses. Patients with clinically suspected ischaemic bowel disease should be fasted, undergo gastrointestinal decompression, and receive oxygen and nutritional support immediately 29 . While actively controlling the primary disease, certain treatments, such as correcting intestinal hypoperfusion caused by hypotension, shock, or cardiac insufficiency and controlling blood pressure and blood glucose, should be initiated 29 . Patients with thrombosis should be treated with anticoagulant and thrombolytic therapy as soon as possible but only after undergoing a bleeding risk assessment. Drug therapy is suitable only for mild patients, and surgical or vascular intervention is often needed for moderate and severe patients 30 . Interventional therapy involves opening occluded blood vessels or removing emboli through guidewires, catheters, balloons, stents and other devices 31 . This treatment has the advantages of safety, less trauma, quick recovery, and fewer complications and has been routinely used to treat ischaemic diseases 32 . However, interventional therapy itself is a kind of trauma to blood vessels and may cause a local inflammatory response in blood vessels after trauma. The incidence of postoperative restenosis is high. Surgical treatment is usually adopted for patients with severe ischaemic bowel disease, especially when the patient has intestinal infarction or acute peritonitis signs requiring immediate laparotomy 33 . The surgical wound area is large, healing is slow, and postoperative mortality is very high. ICBD progresses rapidly, and the existing treatment methods have their own advantages and disadvantages. The improper selection of treatment can easily delay the initiation of appropriate treatment, causing irreversible intestinal injury and critical problems.
Cell therapy, which involves the use of primary cells, cell lines and various stem cells, has been a promising method for the treatment of difficult diseases in recent years 34 . Through transplantation and local infusion of autologous or allogeneic cells, cells and/or biologically active molecules are used to repair or enhance the biological function of damaged tissues 35 . In mammals, stem cells include embryonic stem cells and adult stem cells. Human embryonic stem cells were initially used for reproduction through in vitro fertilization in the 1990s and have since been used to investigate potential roles in regenerative medicine 36 . However, because this process involves the destruction of human embryos, related research is ethically and politically controversial 37 . Umbilical cord blood stem cells are a type of adult stem cell that has unique advantages compared with bone marrow and peripheral blood haematopoietic stem cells: (1) Stem cells in the umbilical cord are easy to collect, harmless to the donor, have less ethical controversy, and have stronger proliferation and differentiation ability 38 . (2) UCB is rich in haematopoietic stem cells, and its concentration and purity are 10–20 times greater than those of bone marrow haematopoietic stem cells 39 . (3) Also, the T and B lymphocytes in cord blood are naive because they have no contact with their own substances, their immune function is not mature, and their antigenicity is low 40 . (4) Umbilical cord blood cells are protected by the placental barrier and are rarely contaminated 41 . (5) Cord blood cells can be cryopreserved for 15 years or more, 60–90% of viable cells can be recovered after resuscitation, and the preparation time for transplantation is short, which is suitable for patients with rapid disease progression 42 . Therefore, cord blood stem cells are an ideal source for stem cell transplantation.
When an ischaemic event occurs, the local microenvironment of ischaemic tissue changes, and “attracts” exogenous stem cells to precisely home toward the ischaemic tissue and interact with vascular endothelial cells in the ischaemic tissue. This cell‒cell interaction is mediated by E-selectin adhesion molecules 43 . In ischaemic tissue, E-selectin is highly expressed on activated endothelial cells and acts as a “docking site” to anchor stem cells expressing corresponding E-selectin ligands in the blood circulation, thereby inducing tissue repair and angiogenesis 44 . For the treatment of ischaemic bowel disease, some research directions include promoting angiogenesis and increasing blood supply at the ischaemic site. Stem cell transplantation can increase blood flow at the ischaemic site by inducing neovascularization and collateral circulation.
Umbilical cord blood mononuclear cells include haematopoietic stem cells (HSCs), mesenchymal stem cells (MSCs), endothelial progenitor cells (EPCs), lymphocytes, and monocytes 45 . HSCs are specialized stem cells and one of the most abundant stem cells in UCB; these cells can differentiate into cells of the blood and immune systems 46 . At present, HSCS are mainly used to treat various refractory haematological diseases.
MSCs can be induced to differentiate into vascular endothelial progenitor cells, vascular smooth muscle cells, nerve cells, cardiomyocytes, osteoblasts and hepatocytes, etc 47 . MSCs have been gradually used in the clinical treatment of cardiovascular and cerebrovascular ischaemia, limb ischaemia, Parkinson's disease, liver cirrhosis and other diseases and have achieved good clinical effects 48 . Intramuscular injection of placental-derived MSCs has been shown to have greater therapeutic efficacy than bone marrow or adipose tissue-derived MSCs in a mouse hindlimb ischaemia model 49 . MSCs can support haematopoiesis, express adhesion molecules, interact with haematopoietic cells, regulate the adhesion between haematopoietic cells and stromal cells, and play an important role in haematopoietic cell implantation and homing 50 . MSCs promote angiogenesis mainly through two pathways. On the one hand, MSCs differentiate into vascular endothelial cells and smooth muscle cells to directly form new blood vessels 51 . On the other hand, through its powerful paracrine effect, microglia secrete angiogenic factors such as basic fibroblast growth factor (bFGF), vascular endothelial growth factor (VEGF) and angiopoietin to indirectly promote angiogenesis 43 , 52 . B-FGF is a polypeptide that can promote angiogenesis. Its role is to promote the mitosis of vascular endothelial cells (VECs) and induce VECs to move to the ischaemic site to produce VEGF 53 . VEGF is a functional glycoprotein with high biological activity that can induce VEC migration, proliferation and differentiation to form new blood vessels 54 . Several studies have confirmed that VEGF levels in the transplanted area are significantly increased after local injection of umbilical cord blood mononuclear cells into an animal model of bilateral lower limb ischaemia 55 , and these results further confirmed the role of MSCs in promoting angiogenesis. In addition, MSCs can also participate in the body’s immune response via two possible mechanisms. One is that they participate in immune regulation by inhibiting the proliferation of T cells and stimulating the proliferation of local endothelial cells to promote intestinal healing in a synergistic manner 56 . On the other hand, changes in the microbiome may be involved. The gut microbiome plays an important role in stimulating intestinal integrity and local immune responses. Recent studies have shown that the diversity of intestinal microbes is also significantly increased in animals treated with MSCs 57 .
EPCs are the precursor cells of VECs. The main functions of EPCs include inhibiting the inflammatory response of the vascular wall, reducing intimal hyperplasia to promote the repair of the injured endothelium, and preventing the narrowing of blood vessels 58 . EPCs play an important role in ischaemic tissue. On the one hand, EPCs differentiate into new VECs by themselves and participate in angiogenesis, and this type of angiogenesis does not rely on the existing vascular system 59 . On the other hand, these cells rely on their own paracrine effect and secrete some growth factors and other proangiogenic substances to indirectly participate in angiogenesis 60 .
In summary, we speculate that the mechanism of cord blood mononuclear cells in the treatment of ischaemic bowel disease may be as follows:
Transient tissue hyperaemia after transplantation. In our study, we found that clinical manifestations such as abdominal pain and abdominal tenderness were significantly relieved 5 days after treatment in most patients after infusion of HUCB-MNCs through the mesenteric artery, but neovascularization and new collateral circulation had not yet formed. This improvement in symptoms may be related to vasodilatation, tissue congestion and temporary blood supply to the ischaemic site after the infusion of cells. Tissue hyperaemia quickly alleviates the symptoms of ischaemia for a short period of time, and the patient’s clinical symptoms are alleviated; however, this tissue response gradually weakens with time after transplantation.
Promotion of angiogenesis. We found that the clinical symptoms of the patients who received umbilical cord blood mononuclear cell transplantation were significantly less common than those of the control group, which was considered to be related to the formation of neovascularization and new collateral circulation.
Promotion of wound healing. The degree of bloody stool in patients treated with HUCB-MNCs was significantly lower than that in the control group and before treatment. On the one hand, these findings were related to the improvement in ischaemia, and on the other hand, they may be related to the mechanism through which HUCB-MNCs promote wound healing. Wound healing is actually achieved by the growth and expansion of some cells whose repair functions involve mainly stem cells from the wound, wound periphery, or blood 61 . Serum nitric oxide (NO) is an antioxidant secreted by vascular endothelial cells and is a key mediator of tissue repair. It can remove superoxide free radicals, regulate vascular tone, relax blood vessels, prevent coagulation and eliminate thrombosis 62 . During ischaemia and hypoxia, the levels of endogenous nitric oxide synthase (NOS) inhibitors increase, and NO synthesis decreases. Treatment with HUCB-MNCs may reduce the level of NOS inhibitors and promote the recovery of NO levels, thereby accelerating wound healing and vasodilation 63 . In this experiment, DD in the experimental group was lower than that in the control group after treatment, which further verified this claim.Collagen is a structural protein of the extracellular matrix that functions to provide strength and integrity to the tissue matrix and plays an extremely important role in wound healing 63 . It has been confirmed that wound contraction and epithelial cell formation occur earlier in the injured areas of skin treated with HUCB-MNCs, and marked vascular and fibrous hyperplasia can be observed around the wound. Moreover, the weight of the granulation tissue increased more obviously 64 . In addition, compared with those of dermal fibroblasts, the collagen synthesis and bFGF and VEGF levels of stem cells are markedly greater, indicating that HUCB-MNCs can also change the tissue microenvironment and promote wound healing and tissue repair by secreting soluble factors 65 .
Regulation of immune and anti-inflammatory effects and reduce inflammatory cell infiltration into the wound. HUCB-MNCs secrete growth factors, such as hepatocyte growth factor, insulin-like growth factor, VEGF, bFGF and anti-inflammatory cytokines, such as IL-10 66 , which have antiapoptotic and antinecroptotic effects on ischaemic and injured cells. McDonald et al. demonstrated that UCB and special types of UCB cells, such as EPCs and monocytes, can regulate peripheral and central immune responses 67 . In this way, the immune inflammatory response around the ischaemic injury site is reduced. Our trial showed that the WBC, NEUT and PCT counts of the experimental group were better than those of the treatment group after treatment, which also indicated that the inflammatory response was inhibited after HUCB-MNCs treatment, which was consistent with the findings of previous reports.
Umbilical cord blood mononuclear cells are involved in compensatory vascular reconstruction in the ischaemic region and can improve and restore blood flow at the ischaemic site. A number of studies have confirmed that umbilical cord blood mononuclear cells are safe and effective in the treatment of ischaemic diseases. Cho et al. 68 found that HUCB-MNC transplantation can activate the angiogenesis signalling pathway mediated by interleukin-8 (IL-8), promote angiogenesis in the injured area, and reduce the area of cerebral infarction. Huang et al. 69 found that intra-arterial infusion of HUCB-MNCs in stroke rats can improve regional intravascular blood flow, vascular reactivity and vascular function and reduce the infarct volume caused by ischemia. In several studies, umbilical cord blood mononuclear cells have been injected into rats with lower limb ischaemic diseases, and the experimental observations revealed that the subjective symptoms and objective indicators of the rats were significantly improved after treatment. A small amount of collateral circulation was found at the transplantation site, and no deaths, tumours, retinal detachments or other sequelae occurred during the study, suggesting that umbilical cord blood mononuclear cells promote angiogenesis. The safety of the treatment is also illustrated.
Umbilical cord blood mononuclear cells have very broad application prospects and have achieved good clinical efficacy in the treatment of lower limb ischaemic diseases. The use of umbilical cord blood mononuclear cells promotes angiogenesis and wound healing, improves blood circulation, improves ischaemia, and opens up new ideas for the treatment of ischaemic diseases. At present, there is no specific treatment for ischaemic bowel disease, and conservative medical treatment alone has a high recurrence rate and mortality. This study used multiple or multiple transplantations of umbilical cord blood mononuclear cells to treat ischaemic bowel disease. The results showed that patients treated with umbilical cord blood mononuclear cells had better clinical symptoms and related auxiliary examinations than did those treated with drugs alone. The clinical remission rate in the experimental group was better than that in the control group, and no treatment-related adverse reactions or complications occurred, which further supports the benefit of umbilical cord blood mononuclear cells in the treatment of ischaemic bowel disease. It was also confirmed that HUCB-MNCs have the advantages of weak immunogenicity and decreased immune rejection. It is relatively easy to obtain umbilical cord blood mononuclear cells. If umbilical cord blood mononuclear cells can be widely used in the improvement and treatment of ischaemic bowel disease under the premise of ensuring safety, this approach will be useful for the majority of patients.
Limitations of this study
First, although the incidence of ischaemic bowel disease is increasing annually, the overall incidence is still low, and the sample size of this study was small. Thus, there is a high possibility of error in the results. If more patients are enrolled from multiple centres, the statistical results will be more convincing. In addition, both the experimental group and the control group were treated in this study. In principle, placebo treatment was more appropriate for the control group, but due to ethical restrictions, both groups were treated. Second, because colonoscopy and mesenteric angiography are invasive procedures and relatively expensive, some patients have a poor compliance toward these two methods. Therefore, this study failed to include comprehensive and regular dynamic follow-up data on the vascular and tissue levels of the two groups of patients, and only the subjective indicators were followed up, which is highly likely to cause errors. Although our results showed that the experimental group was superior to the control group in terms of comprehensive response rate, clinical remission severity and follow-up results, to ensure effectiveness and safety, it is necessary to conduct a relatively comprehensive comparison of patients with umbilical cord blood mononuclear cells before routine clinical treatment for ischaemic bowel disease to further confirm our conclusions.
Sixty-six patients with ischaemic bowel disease diagnosed and hospitalized in our hospital between January 2019 and June 2022 were randomly divided into a control group (n = 33) and an experimental group (n = 33). In both groups, the patients were fasted and given fluid infusion, and medications for haemostasis, anti-infection, vasodilatation, intestinal mucosa repair, intestinal flora regulation and other medical treatments, were also given. In the experimental group, umbilical cord blood mononuclear cells were infused through the superior and/or inferior mesenteric artery, and growth hormone was given to promote stem cell differentiation after the operation. The two groups were reexamined on the 5th day after treatment, and the changes in clinical manifestations and related laboratory indicators before and after the treatment were compared. The adverse reactions related to and during the treatment were recorded, and the efficacy and safety of cord blood stem cell therapy were preliminarily analysed. The patients were followed up at 1, 3, and 6 months after treatment to compare and evaluate the long-term therapeutic effect of the two treatment methods.
Diagnostic criteria
The diagnostic criterion for acute mesenteric ischaemia (AMI) was from the “Acute mesenteric ischaemia: Guidelines of the World Society of Emergency Surgery” 70 . The clinical manifestations were sudden severe abdominal pain, fever, bloody stool, acidosis and organ failure, which are highly suggestive of the disease. Severe abdominal pain is incompatible with mild abdominal signs. CTA generally shows partial or complete obstruction of the mesenteric blood vessels and can be used to diagnose the disease.
The diagnostic criteria for chronic mesenteric ischaemia (CMI) were based on the Chronic Mesenteric Ischaemia Clinical Practice Guideline from the “Chronic Mesenteric Ischaemia Clinical Practice Guideline from the Society for Vascular Surgery Journal of Vascular Surgery (2020)” 31 . The clinical manifestations were recurrent abdominal pain and a non-fixed pain location, and postprandial abdominal pain, fear of eating, and weight loss were typical triad symptoms. CTA was the first diagnostic imaging test, and mesenteric arteriography indicated that vascular stenosis > 70% could be diagnosed.
The diagnostic criteria for ischaemic colitis (IC) were based on the “Ischaemic colitis: Uncertainty in diagnosis, pathophysiology and management” 71 . The clinical manifestations are unexplained abdominal pain, mainly spasmodic pain in the left lower abdomen accompanied by the impulse to defecate, and bloody stool usually occurring within 24 h. The symptoms are not typical, other diseases that may cause intestinal infection should be excluded during diagnosis, and the patient's history, imaging, endoscopic findings and histopathology should be combined.
Inclusion criteria
No age, no sex;
Those who met the above diagnosis;
Patients who were willing to provide signed informed consent for treatment and cooperate with treatment.
Exclusion criteria
Patients with severe necrosis of the intestinal wall caused by severe ischaemic bowel disease requiring surgical treatment;
Patients with other inflammatory bowel diseases;
Patients with serious disease of other organs;
Patients who cannot cooperate and are unwilling to provide informed consent;
Patients who missed visits or had automatic discharge.
Sources of cord blood mononuclear cells
The umbilical cord blood mononuclear cells used in this study were all sourced from Shandong Qilu Cell Therapy Engineering Technology Co., LTD. (Cell size: 20 ml, 2.0 × 10 8 /case, number of live cells ≥ 90%), and all cells were guaranteed to be negative for bacteria, fungi, viruses and bacterial endotoxins.
Procedure of umbilical blood mononuclear cell infusion
The umbilical cord blood mononuclear cells were separated and stored by professionals in special test tubes and placed in standard containers at 2–8 °C, after which a small number of cells were counted, and bacterial culture and various tests were performed.
In the intervention room, the patient's superior and/or lower mesenteric artery angiographs were first recorded and videotaped by senior physicians with more than 5 years of working experience to observe the distribution of the patient's mesenteric blood vessels, after which mononuclear cells were injected. The speed of cell input was not fast, and the control was approximately 2 ml/min. After the operation, the puncture point was compressed to stop bleeding for 8–24 h.
Growth hormone was given via a subcutaneous injection after surgery, the patient’s vital signs were detected, routine medical treatment was continued, and treatment-related adverse reactions were recorded over time.
Observation indicators
Clinical manifestations: abdominal pain, defecation frequency, bloody stool, and abdominal tenderness;
Laboratory indicators: white blood cell (WBC) count, neutrophil percentage (NEUT), haemoglobin (HB), platelet (PLT), D-dimer (DD), and procalcitonin (PCT) count; routine stool test; liver and kidney function; and electrocardiogram.
Colonoscopy findings: mucosal congestion, oedema, ulceration, and clear vascular texture;
Efficacy criteria
The clinical symptoms and signs had disappeared, the results of routine stool examination were negative for occult blood, the frequency of stool was less than 3 times a day, and the laboratory test results were within the normal range.
Compared with previous results, the occult blood test results from a routine stool examination were negative or weakly positive, and the clinical manifestations and laboratory test results had improved.
Ineffective
The clinical manifestations were unchanged or even aggravated compared with before treatment, and the laboratory indices were not improved or even aggravated.
Record of adverse reactions
Anaphylaxis, liver and kidney damage and new electrocardiogram changes were recorded during the treatment.
Statistical analysis
The data were imported into SPSS 27.0 software for statistical analysis. The measurement data were tested for normality and homogeneity of variance. The normally distributed data were tested by two-sample t tests and are presented in \(\overline{x}\) ± s. Nonnormally distributed data were analysed by the nonparametric rank sum test and are expressed as M (P25, P75). Categorical data were analysed by the chi-square test, and count data are expressed as n (%). A difference of 0.05 was considered to indicate statistical significance.
Flowchart of the clinical trial (Fig. 4 )
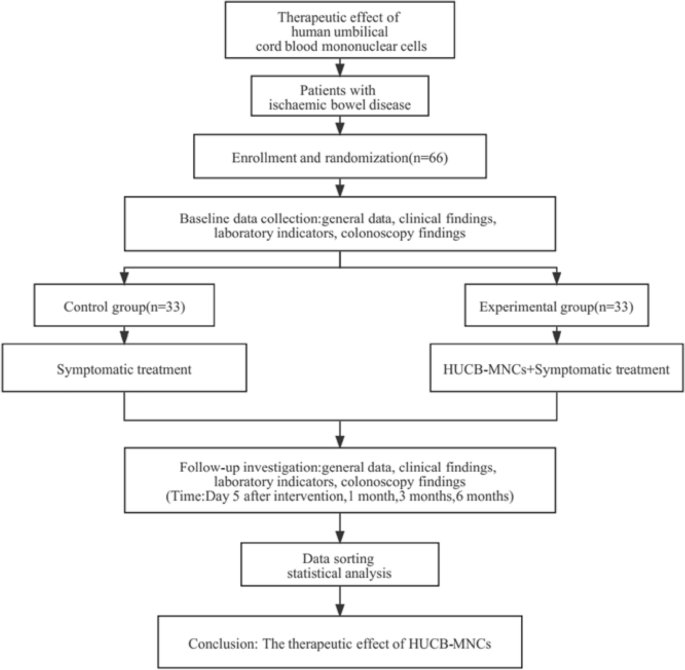
Clinical trial design process.
This study was recognized by the First Affiliated Hospital of Shandong First Medical University, and the licensing committee approved the experiments. All the experiments were performed in accordance with the relevant guidelines and regulations.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Garzelli, L. et al. Insights into acute mesenteric ischaemia: an up-to-date, evidence-based review from a mesenteric stroke centre unit. Br. J. Radiol. 96 , 20230232 (2023).
Article PubMed PubMed Central Google Scholar
Ahmed, M. Ischemic bowel disease in 2021. World J. Gastroenterol. 27 , 4746–4762 (2021).
Article CAS PubMed PubMed Central Google Scholar
Silva, J. A. & White, C. J. Ischemic bowel syndromes. Prim. Care 40 , 153–167 (2013).
Article PubMed Google Scholar
Bala, M. et al. Acute mesenteric ischemia: Guidelines of the world society of emergency surgery. World J. Emerg. Surg. 12 , 38 (2017).
Sardar, P. & White, C. J. Chronic mesenteric ischemia: diagnosis and management. Prog. Cardiovasc. Dis. 65 , 71–75 (2021).
Lawson, R. M. Mesenteric ischemia. Crit. Care Nurs. Clin. N. Am. 30 , 29–39 (2018).
Article Google Scholar
Clair, D. G. & Beach, J. M. Mesenteric ischemia. N. Engl. J. Med. 374 , 959–968 (2016).
Article CAS PubMed Google Scholar
Wang, J. & Metheny, L. Umbilical cord blood derived cellular therapy: Advances in clinical development. Front. Oncol. 13 , 1167266 (2023).
Beaulieu, R. J. et al. Comparison of open and endovascular treatment of acute mesenteric ischemia. J. Vasc. Surg. 59 , 159–164 (2014).
Lundin, N., Lehti, L., Ekberg, O. & Acosta, S. Validation of computed tomography angiography using mean arterial pressure gradient as a reference in stented superior mesenteric artery. Abdom. Radiol. 46 , 792–798 (2021).
Han, Y. et al. Mesenchymal stem cells for regenerative medicine. Cells 8 , 886 (2019).
Singh, K. et al. Evaluation of four methods for processing human cord blood and subsequent study of the expansion of progenitor stem cells isolated using the best method. Cytotherapy 11 , 768–777 (2009).
Rodríguez-Fuentes, D. E. et al. Mesenchymal stem cells current clinical applications: A systematic review. Arch. Med. Res. 52 , 93–101 (2021).
Xi, Y., Yue, G., Gao, S., Ju, R. & Wang, Y. Human umbilical cord blood mononuclear cells transplantation for perinatal brain injury. Stem Cell Res. Ther. 13 , 458 (2022).
Zhang, J. et al. Human umbilical cord blood mononuclear cells ameliorate CCl(4)-induced acute liver injury in mice via inhibiting inflammatory responses and upregulating peripheral interleukin-22. Front. Pharmacol. 13 , 924464 (2022).
Kühn, F., Schiergens, T. S. & Klar, E. Acute mesenteric ischemia. Visc Med. 36 , 256–262 (2020).
Xu, Y., Xiong, L., Li, Y., Jiang, X. & Xiong, Z. Diagnostic methods and drug therapies in patients with ischemic colitis. Int. J. Colorectal Dis. 36 , 47–56 (2021).
Kärkkäinen, J. M., Lehtimäki, T. T., Manninen, H. & Paajanen, H. Acute mesenteric ischemia is a more common cause than expected of acute abdomen in the elderly. J. Gastrointest. Surg. 19 , 1407–1414 (2015).
Sun, D. L. et al. Accuracy of using serum D-dimer for diagnosis of acute intestinal ischemia: a meta-analysis. Medicine 96 , e6380 (2017).
Sang, Y., Roest, M., de Laat, B., de Groot, P. G. & Huskens, D. Interplay between platelets and coagulation. Blood Rev. 46 , 100733 (2021).
Germolec, D. R., Shipkowski, K. A., Frawley, R. P. & Evans, E. Markers of inflammation. Methods Mol. Biol. 1803 , 57–79 (2018).
Foy, B. H., Sundt, T. M., Carlson, J. C. T., Aguirre, A. D. & Higgins, J. M. Human acute inflammatory recovery is defined by co-regulatory dynamics of white blood cell and platelet populations. Nat. Commun. 13 , 4705 (2022).
Article ADS CAS PubMed PubMed Central Google Scholar
Kougias, P. et al. Determinants of mortality and treatment outcome following surgical interventions for acute mesenteric ischemia. J. Vasc. Surg. 46 , 467–474 (2007).
Zhang, H. et al. High neutrophil percentage-to-albumin ratio can predict occurrence of stroke-associated infection. Front. Neurol. 12 , 705790 (2021).
Kamat, I. S., Ramachandran, V., Eswaran, H., Guffey, D. & Musher, D. M. Procalcitonin to distinguish viral from bacterial pneumonia: A systematic review and meta-analysis. Clin. Infect. Dis. 70 , 538–542 (2020).
Cleland, D. A. & Eranki, A. P. Procalcitonin in StatPearls (StatPearls Publishing, 2024).
Papaziogas, B., Anthimidis, G., Koutelidakis, I., Atmatzidis, S. & Atmatzidis, K. Predictive value of procalcitonin for the diagnosis of bowel strangulation. World J. Surg. 32, 1566–1567; author reply 1568 (2008).
Cai, W. et al. Comparison of clinical outcomes of endovascular versus open revascularization for chronic mesenteric ischemia: A meta-analysis. Ann. Vasc. Surg. 29 , 934–940 (2015).
Corcos, O. & Nuzzo, A. Gastro-intestinal vascular emergencies. Best Pract. Res. Clin. Gastroenterol. 27 , 709–725 (2013).
Terlouw, L. G. et al. European guidelines on chronic mesenteric ischaemia - joint United European Gastroenterology, European Association for Gastroenterology, Endoscopy and Nutrition, European Society of Gastrointestinal and Abdominal Radiology, Netherlands Association of Hepatogastroenterologists, Hellenic Society of Gastroenterology, Cardiovascular and Interventional Radiological Society of Europe, and Dutch Mesenteric Ischemia Study group clinical guidelines on the diagnosis and treatment of patients with chronic mesenteric ischaemia. United Eur. Gastroenterol. J. 8 , 371–395 (2020).
Huber, T. S. et al. Chronic mesenteric ischemia: Clinical practice guidelines from the society for vascular surgery. J. Vasc. Surg. 73 , 87s–115s (2021).
Mohr, J. P. et al. Medical management with interventional therapy versus medical management alone for unruptured brain arteriovenous malformations (ARUBA): Final follow-up of a multicentre, non-blinded, randomised controlled trial. Lancet Neurol. 19 , 573–581 (2020).
Char, D. J., Cuadra, S. A., Hines, G. L. & Purtill, W. Surgical intervention for acute intestinal ischemia: Experience in a community teaching hospital. Vasc. Endovasc. Surg. 37 , 245–252 (2003).
Nistor-Cseppentö, D. C., Jurcău, M. C., Jurcău, A., Andronie-Cioară, F. L. & Marcu, F. Stem cell- and cell-based therapies for ischemic stroke. Bioengineering 9 , 717 (2022).
Doster, D. L., Jensen, A. R., Khaneki, S. & Markel, T. A. Mesenchymal stromal cell therapy for the treatment of intestinal ischemia: Defining the optimal cell isolate for maximum therapeutic benefit. Cytotherapy 18 , 1457–1470 (2016).
Alatyyat, S. M., Alasmari, H. M., Aleid, O. A., Abdel-Maksoud, M. S. & Elsherbiny, N. Umbilical cord stem cells: Background, processing and applications. Tissue Cell 65 , 101351 (2020).
Parikh, P. P., Liu, Z. J. & Velazquez, O. C. A molecular and clinical review of stem cell therapy in critical limb ischemia. Stem Cells Int. 2017 , 3750829 (2017).
Ruggeri, L., Aversa, F., Martelli, M. F. & Velardi, A. Allogeneic hematopoietic transplantation and natural killer cell recognition of missing self. Immunol. Rev. 214 , 202–218 (2006).
Berglund, S., Magalhaes, I., Gaballa, A., Vanherberghen, B. & Uhlin, M. Advances in umbilical cord blood cell therapy: The present and the future. Expert Opin. Biol. Ther. 17 , 691–699 (2017).
Galieva, L. R., Mukhamedshina, Y. O., Arkhipova, S. S. & Rizvanov, A. A. Human umbilical cord blood cell transplantation in neuroregenerative strategies. Front. Pharmacol. 8 , 628 (2017).
Bianconi, V. et al. Endothelial and cardiac progenitor cells for cardiovascular repair: A controversial paradigm in cell therapy. Pharmacol. Ther. 181 , 156–168 (2018).
Broxmeyer, H. E. et al. Human umbilical cord blood as a potential source of transplantable hematopoietic stem/progenitor cells. Proc. Natl. Acad. Sci. USA 86 , 3828–3832 (1989).
Liu, Z. J. et al. Identification of E-selectin as a novel target for the regulation of postnatal neovascularization: Implications for diabetic wound healing. Ann. Surg. 252 , 625–634 (2010).
Liu, Z. J. et al. Inhibition of tumor angiogenesis and melanoma growth by targeting vascular E-selectin. Ann. Surg. 254 , 450–456 (2011).
Rallapalli, S. et al. Generation of clinical-grade red blood cells from human umbilical cord blood mononuclear cells. Cell Tissue Res. 375 , 437–449 (2019).
Laurenti, E. & Göttgens, B. From haematopoietic stem cells to complex differentiation landscapes. Nature 553 , 418–426 (2018).
Ankrum, J. A., Ong, J. F. & Karp, J. M. Mesenchymal stem cells: Immune evasive, not immune privileged. Nat. Biotechnol. 32 , 252–260 (2014).
Reyhani, S., Abbaspanah, B. & Mousavi, S. H. Umbilical cord-derived mesenchymal stem cells in neurodegenerative disorders: From literature to clinical practice. Regen. Med. 15 , 1561–1578 (2020).
Jeon, Y. J., Kim, J., Cho, J. H., Chung, H. M. & Chae, J. I. Comparative analysis of human mesenchymal stem cells derived from bone marrow, placenta, and adipose tissue as sources of cell therapy. J. Cell. Biochem. 117 , 1112–1125 (2016).
Bari, S. et al. Expansion and homing of umbilical cord blood hematopoietic stem and progenitor cells for clinical transplantation. Biol. Blood Marrow Transpl. 21 , 1008–1019 (2015).
Galipeau, J. & Sensébé, L. Mesenchymal stromal cells: Clinical challenges and therapeutic opportunities. Cell Stem Cell 22 , 824–833 (2018).
Luttun, A., Carmeliet, G. & Carmeliet, P. Vascular progenitors: From biology to treatment. Trends Cardiovasc. Med. 12 , 88–96 (2002).
Haniffa, M. A., Collin, M. P., Buckley, C. D. & Dazzi, F. Mesenchymal stem cells: the fibroblasts’ new clothes?. Haematologica 94 , 258–263 (2009).
Leask, A. Potential therapeutic targets for cardiac fibrosis: TGFbeta, angiotensin, endothelin, CCN2, and PDGF, partners in fibroblast activation. Circ. Res. 106 , 1675–1680 (2010).
Zhang, J. et al. Umbilical cord mesenchymal stem cells and umbilical cord blood mononuclear cells improve neonatal rat memory after hypoxia-ischemia. Behav. Brain Res. 362 , 56–63 (2019).
Article ADS CAS PubMed Google Scholar
Bian, D., Wu, Y., Song, G., Azizi, R. & Zamani, A. The application of mesenchymal stromal cells (MSCs) and their derivative exosome in skin wound healing: A comprehensive review. Stem Cell Res. Ther. 13 , 24 (2022).
Soontararak, S. et al. Mesenchymal stem cells (MSC) derived from induced pluripotent stem Cells (iPSC) equivalent to adipose-derived MSC in promoting intestinal healing and microbiome normalization in mouse inflammatory bowel disease model. Stem Cells Transl. Med. 7 , 456–467 (2018).
Feugray, G., Miranda, S., Duchez, V. L. C., Bellien, J. & Billoir, P. Endothelial progenitor cells in autoimmune disorders. Stem Cell Rev. Rep. 19 , 2597–2611 (2023).
Lin, R. Z., Dreyzin, A., Aamodt, K., Dudley, A. C. & Melero-Martin, J. M. Functional endothelial progenitor cells from cryopreserved umbilical cord blood. Cell Transpl. 20 , 515–522 (2011).
Yan, F., Li, J. & Zhang, W. Transplantation of endothelial progenitor cells: Summary and prospect. Acta Histochem. 125 , 151990 (2023).
Palma, M. B. et al. Wound healing by allogeneic transplantation of specific subpopulation from human umbilical cord mesenchymal stem cells. Cell Transpl. 30 , 963689721993774 (2021).
Malone-Povolny, M. J., Maloney, S. E. & Schoenfisch, M. H. Nitric oxide therapy for diabetic wound healing. Adv. Healthc. Mater. 8 , e1801210 (2019).
Parmar, K. M., Shende, P. R., Katare, N., Dhobi, M. & Prasad, S. K. Wound healing potential of Solanum xanthocarpum in streptozotocin-induced diabetic rats. J. Pharm. Pharmacol. 70 , 1389–1400 (2018).
Hall, E. D., Yonkers, P. A., Horan, K. L. & Braughler, J. M. Correlation between attenuation of posttraumatic spinal cord ischemia and preservation of tissue vitamin E by the 21-aminosteroid U74006F: Evidence for an in vivo antioxidant mechanism. J. Neurotrauma 6 , 169–176 (1989).
Phinney, D. G. & Prockop, D. J. Concise review: mesenchymal stem/multipotent stromal cells: The state of transdifferentiation and modes of tissue repair–current views. Stem Cells 25 , 2896–2902 (2007).
Zhou, J. et al. Progress in the treatment of neonatal hypoxic-ischemic encephalopathy with umbilical cord blood mononuclear cells. Brain Dev. 45 , 533–546 (2023).
McDonald, C. A. et al. Effects of umbilical cord blood cells, and subtypes, to reduce neuroinflammation following perinatal hypoxic-ischemic brain injury. J. Neuroinflammation 15 , 47 (2018).
Cho, K. H. et al. Therapeutic mechanism of cord blood mononuclear cells via the IL-8-mediated angiogenic pathway in neonatal hypoxic-ischaemic brain injury. Sci. Rep. 10 , 4446 (2020).
Huang, L. et al. Intraarterial transplantation of human umbilical cord blood mononuclear cells in hyperacute stroke improves vascular function. Stem Cell Res. Ther. 8 , 74 (2017).
Chen, C., Li, Y. W., Shi, P. F. & Qian, S. X. Acute mesenteric ischemia in patients with COVID-19: Review of the literature. J. Natl. Med. Assoc. 114 , 47–55 (2022).
PubMed Google Scholar
Nikolic, A. L. & Keck, J. O. Ischaemic colitis: Uncertainty in diagnosis, pathophysiology and management. ANZ J. Surg. 88 , 278–283 (2018).
Download references
Acknowledgements
The authors would like to thank all those who participated in the study.This research was supported by the special fund of Medical Research of Shandong Medical Association. YXH2019ZX005.
Author information
Authors and affiliations.
Shandong Provincial Maternal and Child Health Care Hospital Affiliated to Qingdao University, No. 238 Jingshi East Road, Jinan, Shandong, China
Xiaoxiao Cai, Yonghao Li & Fengyu Gao
Department of Gastroenterology, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, No. 16766 Jingshi Road, Jinan, Shandong, China
Hongli Yang
Graduate Department of Shandong First Medical University & Shandong Academy of Medical Sciences, No. 6699 Qingdao Road, Jinan, Shandong, China
Xiaoxiao Cai, Yonghao Li & Bilal Muhammad
Department of General Surgery, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, No. 16766 Jingshi Road, Jinan, Shandong, China
Bilal Muhammad
You can also search for this author in PubMed Google Scholar
Contributions
X.C and Y.L contributed equally to the work. All authors contributed signifcantly to this work. H.Y. conceived of and designed the study. X.C. collected the data and performed the analyses and wrote the paper, Y.L. helped to shape the research. B.M. and F.G. critically reviewed the paper.

Corresponding author
Correspondence to Hongli Yang .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Cai, X., Li, Y., Gao, F. et al. Therapeutic effect and study of human umbilical cord blood mononuclear cells in patients with ischaemic bowel disease. Sci Rep 14 , 6121 (2024). https://doi.org/10.1038/s41598-024-56720-z
Download citation
Received : 12 December 2023
Accepted : 10 March 2024
Published : 13 March 2024
DOI : https://doi.org/10.1038/s41598-024-56720-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ischaemic bowel disease
- Umbilical cord blood
- Umbilical cord blood mononuclear cells
- Interventional therapy
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Inflamm Regen
- PMC10696687

Umbilical cord blood and cord tissue banking as somatic stem cell resources to support medical cell modalities
Tokiko nagamura-inoue.
1 Department of Cell Processing and Transfusion, Research Hospital, The Institute of Medical Science, The University of Tokyo, 4-6-1 Shirokanedai, Minato-ku, Tokyo, 108-8639 Japan
2 IMSUT CORD, Research Hospital, The Institute of Medical Science, The University of Tokyo, Tokyo, Japan
Fumitaka Nagamura
3 Division of Advanced Medicine Promotion, The Advanced Clinical Center, The Institute of Medical Science, The University of Tokyo, Tokyo, Japan
Associated Data
The review does not include patient data; however, data and materials related to banking are made available. Requests may be sent to [email protected].
Human umbilical cord blood (CB) and umbilical cord tissue (UC) are attractive sources of somatic stem cells for gene and cell therapies. CB and UC can be obtained noninvasively from donors. CB, a known source of hematopoietic stem cells for transplantation, has attracted attention as a new source of immune cells, including universal chimeric antigen receptor-T cell therapy (CAR-T) and, more recently, universal CAR-natural killer cells. UC-derived mesenchymal stromal cells (UC-MSCs) have a higher proliferation potency than those derived from adult tissues and can be used anon-HLA restrictively. UC-MSCs meet the MSC criteria outlined by the International Society of Gene and Cellular Therapy. UC-MSCs are negative for HLA-DR, CD80, and CD86 and have an immunosuppressive ability that mitigates the proliferation of activated lymphocytes through secreting indoleamine 2,3-dioxygenase 1 and prostaglandin E2, and the expression of PD-L2 and PD-L1. We established the off-the-shelf cord blood/cord bank IMSUT CORD to support novel cell therapy modalities, including the CB-derived immune cells, MSCs, MSCs-derived extracellular vesicles, biological carriers loaded with chemotherapy drugs, prodrug, oncolytic viruses, nanoparticles, human artificial chromosome, combinational products with a scaffold, bio3D printing, and so on.
Human umbilical cord blood (CB) has been a well-known source of hematopoietic stem cells (HSCs) for over 25 years. In the present day, CB transplantations are implemented more than 1200 per year in Japan ( http://www.jdchct.or.jp/data/report/2022/ ). However, the number of CB transplantations (CBT) in European countries (EU) is decreasing, instead, the HLA-haploidentical allogeneic HSC transplantation has become popular in the EU rather than CBT. The reason why HLA-haploidentical relatives have become rapidly available sources of HSCs is that prevention methods for acute graft-versus-host disease (aGVHD), mainly post-transplant cyclophosphamide administration, resulting in the removal of alloreactive T cells in the patients [ 1 ]. CB is currently the optimal source for immunotherapy using activated T cells, regulatory T cells, and natural killer (NK) cells, with or without genetic modifications. Additionally, there has been an overwhelming interest in mesenchymal stromal cells (MSCs) for immunotherapy and regenerative medicine, although CBs are limited in volume to obtain an adequate number of MSCs. MSCs can be isolated from any tissue in the body, but currently, the major sources of MSCs include the bone marrow (BM), adipose tissue (AD), and umbilical cord (UC) [ 2 ]. Among these cell sources, human UC has been rapidly utilized as an abundant source of MSCs worldwide due to its ease of collection, noninvasive collection procedure, and categorization as biological waste at birth. Moreover, it is the youngest nonsenescent human tissue except for ES cells. This review focuses on CB- and UC-derived cells as a source of sustainable material for new modalities in gene and cell therapy.
Characteristics and therapeutic potentials of CB and UC-MSCs
CB has been well-investigated and is known to include a relatively high potential of CD34-positive cells to be expanded, more naïve CD45RA-positive T cell ratios, and more potent suppressor function of regulatory T cells than adult peripheral blood [ 3 , 4 ].
UC-MSCs meet the criteria of MSCs defined by The International Society for Gene and Cellular Therapy [ 5 , 6 ]. First, they are plastically adherent when maintained in a standard culture medium supplemented with serum. Second, they are positive for CD105, CD73, and CD90 but negative for CD45, CD34, CD14 or CD11b, CD79α or CD19, and HLA-DR surface molecules. Third, MSCs cannot differentiate into adipocytes, chondrocytes, and osteoblasts in vitro.
Additionally, immunosuppressive abilities and tissue repair are the most important properties of MSCs for clinical use [ 7 ]. However, MSCs are activated to suppress the immune system only upon the inflammatory stimuli, including activated T cells, PHA-L, and IFN-γ. He et al. demonstrated that third-party UC-MSCs suppress the proliferation of CD4 and CD8-positive cells activated by allogeneic dendritic cells or inflammatory reagents [ 8 ]. Secreted factors such as indoleamine 2, 3-dioxygenase 1, and PGE2 are induced in UC-MSCs by the inflammatory environment and play a critical role in controlling excess immune system [ 9 ]. UC-MSCs constitutively express the PD-L2, while PD-L1 is induced in response to IFN-γ [ 10 ]. Furthermore, like BM- and AD-derived MSCs, MSCs are negative for HLA class II expression and the co-stimulatory surface antigens CD80 and CD86, which activate T cells [ 11 ]. UC-MSCs remain negative for HLA-DR even in the presence of IFN-γ, while HLA-DR on BM-MSCs can be induced upon IFN-γ stimuli [ 8 ]. As a result, these cells escape from activated T cells and are utilized in a non-HLA-restricted manner. Because of these anti-inflammatory properties, MSCs may be useful therapeutic candidates for the treatment of inflammatory disorders.
Another important characteristic of UC-MSCs is their ability to repair tissues. Kurtzberg et al. reported that autologous CB may be effective in mitigating the symptoms of cerebral palsy after birth. CD34-positive cells in the CB play a critical role in treating cerebral palsy, and clinical trials using autologous CB for hypoxic–ischemic encephalopathy (HIE) has been performed in Japan [ 12 ]. However, collecting adequate amounts of CB for therapeutic interventions is difficult. Recently, allogeneic UC-MSCs have become an attractive source to overcome the disadvantages of CB collection [ 13 ]. Causes of cerebral palsy include periventricular leukomalacia (PVL), periventricular hemorrhage, and HIE. However, a common mechanism of cerebral palsy is the early phase of inflammation caused by hypoxia, glucose depletion, and microglia dysfunction with reactive oxygen species, followed by neurogenic damage [ 13 ]. The excess inflammation and tissue damage in the pathological cascade are expected to be controlled by MSCs. We previously found that UC-MSCs migrate toward the injured site of the brain after tracking in the lungs, although MSCs do not engraft and disappear after 3 weeks of intravenous injection. UC-MSCs secrete neurotrophic factors such as brain-derived neurotrophic factor and hepatocyte growth factor, and attenuate mice brain injury [ 14 , 15 ]. These characteristics of UC-MSCs described above are expected to contribute to the development of treatments in the fields of immunotherapy and regenerative medicine.
Umbilical cord blood and cord bank
Establishing a stable supply system for CB- and UC-MSCs is critical for implementing regenerative and immunotherapies. For this purpose, The Institute of Medical Science, The University of Tokyo (IMSUT), has established the cord blood/cord bank IMSUT CORD as a new type of public biobank to supply “off-the-shelf” frozen CB, UC tissues, and UC-derived cells. Briefly, the IMSUT CORD collected both CB and UC data after obtaining informed consent from the guardian of the baby (Fig. 1 ). In addition to obtaining informed consent, questionnaires about the medical history, genetic history of the baby donor’s family, and history of the mother’s communicable disease risk behavior were collected. CB and UC were collected, and the mother’s blood was tested for infection. These documentation and tests in CB banks can also be referred to as UC banking, although additional infection-related tests for UC banking are strictly required. The collected CB and UC are transported from the hospitals to the CB/UC bank and the IMSUT CORD cryopreserves UC tissue [ 16 ] until obtaining confirmation that the baby exhibits healthy, normal development and the mother remains free from infection within at least 6 months after delivery.

Overall flow of the off-the-shelf cord blood/cord bank, IMSUT CORD to support the clinical and research use
The IMSUT CORD processes and freezes CB into frozen enriched cells, while freezes the UC tissue and cultures the frozen-thawed UC tissue into master cells, intermediate cell products, or final cell products, according to the physician’s or company’s requirements of cell modalities.
Clinical trials using UC-MSCs for severe acute GVHD and others
Table Table1 1 shows the reports of clinical trials for severe acute graft-versus-host disease (aGVHD) using UC-MSCs [ 10 , 17 ]. Not like BM-MSCs, there are only two studies to treat severe aGVHD using UC-MSCs including the author’s one. Here, we introduce our physician-initiated clinical trial for severe aGVHD using allogeneic UC-MSCs (IMSUT-CORD) manufactured in serum-free medium and cryoprotectant from 2018 to 2020 in Japan [ 10 ]. In a phase I dose-escalation clinical trial, IMSUT-CORD was administered 1 × 10 6 cells/kg or 2 × 10 6 cells /kg intravenously twice per week over 2 cycles. Patients with no adverse effects, partial response (PR), or mixed response (MR) underwent up to two additional cycles. No severe adverse events were observed; at 16 weeks after the initial IMSUT-CORD infusion, one patient showed no response, while one showed MR, two showed PR, and three showed a complete response (CR). The overall response was 71.4% (90% CI 34.1–94.7%), while the overall survival was 85.7% (90% CI 62.2–100%). The continuous CR/PR rate was 100% for > 28 days after CR/PR, while the survival rate was 85.7% on day 100 (90% CI 62.2–100). The overall response rate (ORR) of 70% reported by Soder RP. et al. was similar that of ours. These high ORR and less toxicity show the necessity of conducting further clinical trials. Table Table1 1 shows the reports of clinical trials using UC-MSCs. The overall response rate (ORR) of 70% reported by Soder RP., et al. was similar that of ours. These high ORR and less toxicity show the necessity of conducting further clinical trials.
Clinical trials using allogeneic umbilical cord-derived mesenchymal stromal cells for acute GVHD
| Authors | Disease | Phase | Patients number | Age (range) year | Cell number | Frequency, interval | Results | Adverse event |
|---|---|---|---|---|---|---|---|---|
| Soder RP., et al. [ ] (2020) | Steroid-resistant aGVHD | 1 | 10 | 35–73 | 2 × 10 cells/kg, 10 × 10 cells/kg | Day 0, day 7 | ORR: 70% (4 CR, 3 PR). Day 100/180 survival: 90% /60%, | No AE |
| Nagamura-Inoue, T., et al. [ ] (2022) | Steroid-resistant aGVHD | 1 | 7 | 25–62 | 1 × 10 ells/kg, 2 × 10 /kg | Twice/week, for 2 weeks. 2 additional weeks for PR or MR patients with no SAE | ORR: 71.4% (3 CR, 2PR, 1 MR,1 NR), over 28 days continuous CR/PR: 100% | no SAE |
All MSCs were injected intravenously
Day 0 the first administration day
AE adverse event, aGVHD acute graft-versus-host disease, CR complete response, MR mixed response, NR no response, ORR overall response rate, PR partial response, SAE severe adverse event
Other implementations of clinical trials using IMSUT-CORD include phase I clinical trial for COVID-19-related acute respiratory distress syndrome (ARDS), phase I clinical trial for cerebral palsy, and phase II clinical for post-hematopoietic transplantation non-infectious pulmonary complication in Japan. While all three clinical trials were closed, the results have not been published yet.
In our COVID-19-related ARDS study, there are six publications in the world (Table (Table2) 2 ) [ 18 – 23 ]. Among three phase II clinical trials for COVID-19-related ARDS, one showed an improvement in survival rate significantly [ 19 ], while two did not [ 18 , 20 ].
Clinical trials using allogeneic umbilical cord-derived mesenchymal stromal cells for COVID-19-related ARDS and cerebral palsy
| Authors | Disease | Phase | Patients number | Age (range) year | Cell number | Frequency, interval | Results | Adverse event | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| COVID-19-related ARDS | ||||||||||||
| Monsel A., et al. [ ] (2022) | Moderate to severe COVID-19-related ARDS | 2b | MSC: 21, placebo: 24 | 64 (mean) | 1 × 10 cells/kg | Day 0, day 2 ± 1, day 4 ± 1 | No efficacy of PaO2/FiO2-ratio and mortality | No SAE | ||||
| Dilogo IH., et al. [ ] (2021) | Critically ill COVID-19-related ARDS | 2 | MSC: 20, placebo: 20 | < 40:4, 40–60: 8, > 60: 8 | 1 × 10 cells/kg | One dose | Survival rate in UC-MSCs group was 2.5 times higher ( = .047), that in UC-MSCs group with comorbidities, 4.5 times higher. The length of stay in the intensive care unit and ventilator usage were not statistically significant | No AE | ||||
| Gorman EA., et al. [ ] (2023) | Moderate to severe COVID-19-related ARDS | 2 | MSC: 30, placebo: 29 | 58.4 (mean) | 4 × 10 cells | One dose | Improvement of pulmonary organ dysfunction: no difference | Safe and well tolerated | ||||
| Lanzoni G., et al. [ ] (2021) | Mild to severe COVID-19-related ARDS | 1/2 | MSC: 12, placebo: 12 | 58.6 (mean) | 100 ± 20 × 10 cells | Day 0, day3 | Survival rate at day 28: MSC 91, placebo 42%, = .015), SAE-free survival ( = .008), time to recovery ( = .03) | No SAE, no difference in AEs | ||||
| Farkhad NF., et al. [ ] (2022) | Mild to moderate COVID-19-related ARDS | 1 | MSC:10, control: 10 | 62.0 (mean) | 1 × 10 cells/kg | Day 0, day 2, day 4 | Improvement of patients’ clinical and paraclinical parameters (leukocytosis, lymphopenia, thrombocytopenia, liver enzyme abnormalities) | no SAE | ||||
| Shaz BH., et al. [ ] (2023) | COVID-19-related ARDS | 1 | 10 | 39–79 | 1 × 10 cells/kg, maximum dose 10 cells | Once a day for 3 days | Survival on day 28, 7 (70%) | No SAE | ||||
| Neonatal encephalopathy | ||||||||||||
| Cotten CM., et al. [ ] (2023) | Moderate to severe hypoxic ischemic encephalopathy, treated with hypothermia | 1, pilot | 6 | 36–41 weeks | 1 or 2 doses of 2 × 10 cells/kg/dose | First dose: during hypothermia, second dose: 2 months later | All babies survived, with average to low-average developmental assessment standard scores between 12 and 17 postnatal months | Well tolerated, low titer anti-HLA antibodies by 1 year of age: 5/6 | ||||
AE adverse event, ARDS acute respiratory distress syndrome, COVID-19 coronavirus infectious disease emerged in 2019
In clinical trials for cerebral palsy, there is only one publication of phase I, a pilot study, for moderate to severe hypoxic ischemic encephalopathy (HIE) [ 24 ]. Six neonates with moderate (4) or severe (2) HIE were enrolled and received one dose of UC-MSCs during HIE and 2 received a 2nd dose 2 months later. All babies survived with average to low-average developmental assessment standards scores for ages between 12 and 17 postnatal months. No severe adverse events were reported in all papers, although 5/6 babies developed low titer anti-HLA antibodies.
As for post-hematopoietic transplantation non-infectious pulmonary complication, no report was found.
CB and UC for exploring new cell modalities
Cb and uc-mscs.
Although the use of CB for hematopoietic stem cell transplantation has decreased recently in the world [ 1 ], new technologies have promoted the use of expanded CD34 + cells for HSCT [ 25 ], regulatory T cells to induce tolerance in HSCT [ 26 , 27 ], universal chimeric antigen receptor-T cell therapy (CAR-T) [ 28 ], and universal CAR-NK cells [ 29 – 32 ] for hematological malignancies.
In addition to the clinical trials using UC-MSCs introduced in Tables Tables1 1 and and2, 2 , there are accumulating early-phase clinical trials using UC-MSCs [ 17 , 20 , 23 , 33 – 35 ] for engraftment facilitation in HSCT for aplastic anemia [ 36 ], neurogenic injuries, diabetes mellitus (DM), heart and angioplasty, liver damage including liver cirrhosis, inflammatory bowel diseases such as Crohn’s disease and ulcerative colitis, prevention of acute rejection in renal transplantation, and collagen diseases [ 33 ]. The number of relevant clinical trials on the NIH clinical trial website ( https://00m.in/HHVJP ) has increased up to 95 trials, including complete, recruiting, and not-yet-recruiting status, as of the end of May 2023.
UC-MSCs-derived extracellular vesicles (EVs)
EVs derived from MSCs might be expected to have effects comparable to those of their parental cells. When parental cells exert therapeutic potency, their EVs may carry the key functional molecules by priming [ 37 , 38 ]. EV therapy is an emerging type of next-generation cell therapy, but properly testing the safety and efficacy of EVs is challenging. Recently, Rohde et al. proposed clinical testing for the manufacture and characterization of EVs derived from UC-MSCs [ 39 ]. The number of preclinical proof-of-concept reports using EVs derived from UC-MSCs is increasing. Chu M. et al. reported the result of a phase 1 clinical trial of nebulization of UC-MSCs derived exosome for patients with COVID-19 pneumonia [ 40 ]. The dose of exosome was the same amount of MSCs proportional to the patient’s body weight (1 × 10 6 cells/kg), and the concentration of exosomes for nebulization ranged from 7.66e + 0.8 to 7.00e + 0.7 particles/ml based on NanoSight. Promoted the absorption of pulmonary lesions and reduced the duration of hospitalization for mild cases of COVID-19 pneumonia were observed with no adverse events.
Other clinical trials using exosomes from UC-MSCs listed on Clinicaltrials.gov are summarized in Table Table3. 3 . Target diseases are various, such as COVID-19-related diseases, multiple organ dysfunction syndrome after surgical repair of acute type A aortic dissection liver cirrhosis, and retinitis. Out of six clinical trials, one is in a phase II/III study, and another one is in a phase II study. The exosome therapies may be developed rapidly in the near future.
Clinical trials of exosome listed on ClinicalTrials.gov
| Number | Principal Investigator | Sponsor | Disease | Phase | Patient number | Route of administration | Dose | Frequency, interval |
|---|---|---|---|---|---|---|---|---|
| NCT05808400 | Jihui Du | Huazhong University of Science and Technology, China | chronic cough after COVID-19 | 1 | Exosome: 40, Control: 40 | iv | 1 × 10 particles/ml. × 5 ml | 5 days, twice daily |
| NCT04356300 | Liang-Wan Chen | Fujian Medical University, China | Multiple organ dysfunction syndrome after surgical repair of acute type A aortic dissection | N/A | 60 | iv | 150 mg | Once a day for 14 days |
| NCT05871463 | Behzad Hatami | Research Institute for Gastroenterology and Liver Diseases, Iran | Decompensated liver cirrhosis | 2 | 15 | iv | Final dose of 40 mg | 3 weeks |
| NCT05413148 | Kuddusi Erkılıç | TC Erciyes University, Turkey | Retinitis | 2/3 | 135: MSC vs. exosome vs. placebo | Subtenon’s injection for single eye | Not described | One dose |
| NCT05787288 | Xiaoying Huang | First Affiliated Hospital of Wenzhou Medical University, China | COVID-19 Pneumonia | early phase 1 | 240 (Nebulized extracellular vesicles (EV) vs. saline) | iv | 1 × 10 particles/ml × 5 ml | Twice a day for 5 days |
| NCT05387278 | no information | Vitti Labs, LLC | Severe ARDS associated with COVID-19 | 1 | 20 (Exosome + MSC 10 vs. placebo 10) | iv | No information | No information |
COVID-19 coronavirus infectious disease emerged in 2019
Other modalities
Although UC-MSCs differentiate into osteocytes less frequently than BM-MSCs, tissue engineering with scaffolds such as poly (D, L-lactide-co-glycolide) has been shown to facilitate UC-MSC osteogenesis in a mouse model [ 41 ].
Recently, Ikeguchi et al. reported the first clinical application of a Bio three-dimensional (3D) nerve conduit made from a spheroid of human fibroblasts [ 42 ] using a bio 3D printer to treat peripheral nerve injury [ 43 ], although not yet constructed with UC-MSCs.
UC-MSCs or UC-derived cells can be modified by gene transfer; however, this has not yet been achieved at the clinical level. Meshizuka et al. demonstrated that the CRISPR/Cas9- and AAV-mediated insertion of the beta2 microglobulin-HLA-G fusion gene protected UC-MSCs from allogeneic rejection in a GVHD setting in vitro [ 44 ].
MSCs migrate to the tumor microenvironment (TME) and promote tumor cell generation, mainly through the cross-talk of tumor parenchymal cells, tumor-associated fibroblasts, cytokines, and chemokines in the TME, secreting transforming growth factor-β and VEGF recruiting regulatory T cells. Owing to their accessibility, UC-MSCs may be modified and processed into effective biological carriers for loading with chemotherapy drugs, prodrugs, oncolytic viruses [ 45 – 47 ], nanoparticles, and human artificial chromosomes [ 48 ].
Many studies have been conducted to determine the efficacy of proof-of-concept in treating unmet diseases using CB and UC-MSCs, or their new modality cells.
Conclusions
Both human umbilical CB and UC can serve as effective “off-the-shelf” sustainable sources for gene and cell therapies in immunotherapies and regenerative medicine.
Acknowledgements
We thank the IMSUT CORD staff for working on CB and UC banking. We thank Sugita M. and the staff at NTT Medical Center Hospital (Tokyo, Japan) and Yamaguchi S. and the staff at Yamaguchi Hospital for performing UC tissue and CB collection after obtaining informed consent.
Abbreviations
| AD | Adipose tissue |
| aGVHD | Acute graft-versus-host disease |
| ARDS | Acute respiratory distress syndrome |
| BM | Bone marrow |
| CAR-T | Chimeric antigen receptor-T cell therapy |
| CB | Umbilical cord blood |
| CR | Complete response |
| DM | Diabetes mellitus |
| EVs | Extracellular vesicles |
| HIE | Hypoxic–ischemic encephalopathy |
| HSCs | Hematopoietic stem cells |
| HSCT | Hematopoietic stem cell transplantation |
| IMSUT CORD | The Institute of Medical Science cord blood/cord bank |
| MR | Mixed response |
| MSCs | Mesenchymal stromal cells |
| NK | Natural killer |
| PR | Partial response |
| TME | Tumor microenvironment UC, umbilical cord |
| UC | Umbilical cord tissue |
| UC-MSC | Umbilical cord-derived mesenchymal stromal cells |
Authors’ contributions
TNI and FN wrote the review collecting the papers and references. Both authors read and approved the final manuscript.
This work was supported by the Japan Agency for Medical Research and Development (AMED) (Project Numbers: 21be0804004h0001, 22be0804004h0002,23be0804004h0003).
Availability of data and materials
Declarations.
The collection, storage, and release, including safety and quality management, of CB and UC samples were approved by the Ethics Committee of the Institute of Medical Science, University of Tokyo (IMSUT) Hospital (IRB#35–2).
This manuscript has not been published previously or is not under consideration for publication elsewhere. The authors have read the review manuscript and approved its submission.
This study was partially supported by a joint research study by the University of Tokyo and Human Life Cord Japan Inc. in the development of banking and clinical applications (September 2017). Nagamura-Inoue is a senior medical advisor at Human Life Cord Japan Inc.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
UMBILICAL CORD BLOOD BANKING: A REVIEW
- International Journal Of Advance Research And Innovative Ideas In Education 8(2):284-288
- 8(2):284-288

- Government College of Nursing Baghi Dilawar Khan Srinagar Kashmir

- Islamic University of Science and Technology
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Mary M Herlihy
- Ellen Delpapa
- ACTA OBSTET GYN SCAN
- Stephen Sik Hung Suen

- TRANSFUS APHER SCI

- Simonetta Bottardi
- Paolo Rebulla
- L Z Karagiorgou
- M N Pantazopoulou
- Beloukas Al
- A G Kriebardis
- J PERINAT MED
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Parents' knowledge, awareness and attitudes of cord blood donation and banking options: an integrative review
Affiliations.
- 1 School of Nursing, Midwifery and Paramedicine, University of the Sunshine Coast, Locked Bag 4, Maroochydore DC, QLD, 4558, Australia. [email protected].
- 2 School of Nursing, Midwifery and Paramedicine, University of the Sunshine Coast, Locked Bag 4, Maroochydore DC, QLD, 4558, Australia.
- 3 Sunshine Coast Hospital and Health Service, Maroochydore DC, Queensland, Australia.
- PMID: 30305052
- PMCID: PMC6180365
- DOI: 10.1186/s12884-018-2024-6
Background: For over 25 years cord blood has been used as an alternative to bone marrow for therapeutic use in conditions of the blood, immune system and metabolic disorders. Parents can decide if they would like to privately store their infant's cord blood for later use if needed or to publicly donate it. Parents need to be aware of the options that exist for their infant's cord blood and have access to the relevant information to inform their choice. The aim of this paper is to identify parent's knowledge and awareness of cord blood donation, private banking options and stem cell use, and parent sources and preferred sources of this information.
Methods: An integrative review was conducted using several electronic databases to identify papers on parents' knowledge, attitudes and attitudes towards umbilical cord blood donation and banking. The CASP tool was used to determine validity and quality of the studies included in the review.
Results: The search of the international literature identified 25 papers which met review inclusion criteria. This integrative review identified parents' knowledge of cord banking and/or donation as low, with awareness of cord blood banking options greater than knowledge. Parents were found to have positive attitudes towards cord blood donation including awareness of the value of cord blood and its uses, with the option considered to be an ethical and altruistic choice. Knowledge on cord blood use were mixed; many studies' participants did not correctly identify uses. Information sources for parents on cord blood was found to be varied, fragmented and inconsistent. Health professionals were identified as the preferred source of information on cord blood banking for parents.
Conclusions: This integrative review has identified that further research should focus on identifying information that expectant parents require to assist them to make informed choices around cord blood banking; and identifying barriers present for health professionals providing evidence based information on cord blood use and banking options.
Keywords: Cord blood banking; Cord blood donation; Cord blood stem cells; Expectant parents’ knowledge; Information sources; Women’s knowledge.
PubMed Disclaimer
Conflict of interest statement
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Peer Reviewed Literature Screening and…
Peer Reviewed Literature Screening and Inclusion Process
Similar articles
- Health care professionals' knowledge, attitudes and practices relating to umbilical cord blood banking and donation: an integrative review. Peberdy L, Young J, Kearney L. Peberdy L, et al. BMC Pregnancy Childbirth. 2016 Apr 19;16:81. doi: 10.1186/s12884-016-0863-6. BMC Pregnancy Childbirth. 2016. PMID: 27094796 Free PMC article. Review.
- Australian maternity healthcare professionals' knowledge, attitudes and practices relevant to cord blood banking, donation and clamp timing: A cross-sectional survey. Peberdy L, Young J, Massey D, Kearney L. Peberdy L, et al. Women Birth. 2021 Nov;34(6):e584-e591. doi: 10.1016/j.wombi.2020.11.005. Epub 2020 Dec 11. Women Birth. 2021. PMID: 33309477
- Maternity health professionals' perspectives of cord clamp timing, cord blood banking and cord blood donation: a qualitative study. Peberdy L, Young J, Massey D, Kearney L. Peberdy L, et al. BMC Pregnancy Childbirth. 2020 Jul 16;20(1):410. doi: 10.1186/s12884-020-03102-8. BMC Pregnancy Childbirth. 2020. PMID: 32677904 Free PMC article.
- Umbilical Cord Blood: Counselling, Collection, and Banking. Armson BA, Allan DS, Casper RF. Armson BA, et al. J Obstet Gynaecol Can. 2015 Sep;37(9):832-844. doi: 10.1016/S1701-2163(15)30157-2. J Obstet Gynaecol Can. 2015. PMID: 26605456
- Cord Blood Banking for Potential Future Transplantation. Shearer WT, Lubin BH, Cairo MS, Notarangelo LD; SECTION ON HEMATOLOGY/ONCOLOGY; SECTION ON ALLERGY AND IMMUNOLOGY. Shearer WT, et al. Pediatrics. 2017 Nov;140(5):e20172695. doi: 10.1542/peds.2017-2695. Pediatrics. 2017. PMID: 29084832 Free PMC article. Review.
- Exploring Parental Knowledge, Attitudes, and Factors Influencing Decision-Making in Stem Cell Banking: Rising the Future of Medical Treatment. Alrehaili AA. Alrehaili AA. Cureus. 2024 Apr 16;16(4):e58384. doi: 10.7759/cureus.58384. eCollection 2024 Apr. Cureus. 2024. PMID: 38628380 Free PMC article.
- Peripartum women's perspectives on research study participation in the OneFlorida Clinical Research Consortium during COVID-19 pandemic. Xu K, Hsiao CJ, Ballard H, Chachad N, Reeder CF, Shenkman EA, Flood-Grady E, Louis-Jacques AF, Smith EL, Thompson LA, Krieger J, Francois M, Lemas DJ. Xu K, et al. J Clin Transl Sci. 2022 Oct 10;7(1):e24. doi: 10.1017/cts.2022.476. eCollection 2023. J Clin Transl Sci. 2022. PMID: 36755549 Free PMC article.
- Umbilical Cord Blood Banking: An Update For Childbirth Educators. Waller-Wise R. Waller-Wise R. J Perinat Educ. 2022 Oct 1;31(4):199-205. doi: 10.1891/JPE-2021-0006. J Perinat Educ. 2022. PMID: 36277229 Free PMC article.
- Determinants of the intention to donate umbilical cord blood in pregnant women. Fernandes M, Alessandri G, Abbad R, Grano C. Fernandes M, et al. Vox Sang. 2022 Feb;117(2):169-176. doi: 10.1111/vox.13179. Epub 2021 Jul 14. Vox Sang. 2022. PMID: 34263455 Free PMC article.
- Peddling promise? An analysis of private umbilical cord blood banking company websites in Canada. Marcon AR, Murdoch B, Caulfield T. Marcon AR, et al. Cell Tissue Bank. 2021 Dec;22(4):609-622. doi: 10.1007/s10561-021-09919-7. Epub 2021 Apr 23. Cell Tissue Bank. 2021. PMID: 33890172 Free PMC article.
- Navarrete C, Contreras M. Cord blood banking: a historical perspective. Br J Haematol. 2009;147(2):236–245. doi: 10.1111/j.1365-2141.2009.07827.x. - DOI - PubMed
- Gluckman E. Milestones in umbilical cord blood transplantation. Blood Rev. 2011;25:255–259. doi: 10.1016/j.blre.2011.06.003. - DOI - PubMed
- Ballen KK, Verter F, Kurtzberg J. Umbilical cord blood donation: public or private? Bone Marrow Transplant. 2015:1–8. - PubMed
- Yoder Mervin C. Cord blood banking and transplantation. Current Opinion in Pediatrics. 2014;26(2):163–168. doi: 10.1097/MOP.0000000000000065. - DOI - PubMed
- Waller-Wise R. Umbilical cord blood: information for childbirth educators. J Perinat Educ. 2011;20(1):50–60. doi: 10.1891/1058-1243.20.1.54. - DOI - PMC - PubMed
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

COMMENTS
Studies by several laboratories aimed at understanding the basic biology of cord blood cells demonstrated that UCB is a rich source of HSCs and HPCs.
Webb S. Banking on cord blood stem cells: New research will shed light on claims from commercial banks that cord blood–derived stem cells can be used in diseases beyond hematological disorders. Sarah Webb investigates.
In several studies, umbilical cord blood mononuclear cells have been injected into rats with lower limb ischaemic diseases, and the experimental observations revealed that the subjective...
Cord blood banking often refers to private banking, while donation generally refers to public banking. Research has shown that expectant parents do not have sufficient understanding of the cord blood banking process, umbilical cord stem cell transplants, uses of these cells, or options.
Human umbilical cord blood (CB) and umbilical cord tissue (UC) are attractive sources of somatic stem cells for gene and cell therapies. CB and UC can be obtained noninvasively from donors.
During these 30 years, research in the UCB field has transformed the hematopoietic transplantation arena. Today, scientific and clinical teams are still working on different ways to improve and expand the use of UCB cells. A major effort has been focused on enhancing engraftment to potentially reduce risk of infection and cost.
... Umbilical cord blood (UCB) is a source of hematopoietic stem cells (HSC), which has been successfully used as an alternative to bone marrow or mobilized peripheral blood progenitor cells...
We analysed knowledge, comprehension, opinions, attitudes and choices related to cord blood donation in seven heterogeneous focus groups including pregnant women, future parents, cord...
Results: The search of the international literature identified 25 papers which met review inclusion criteria. This integrative review identified parents' knowledge of cord banking and/or donation as low, with awareness of cord blood banking options greater than knowledge.
Elucidating the role of PCL2 in normal hematopoiesis and leukemogenesis. Developing bioprocesses to expand cord blood hematopoietic stem cells for clinical use. Characterization of the hematopoietic reconstitution enhancing activity of osteoblasts derived from human mesenchymal stromal cells.