
- MJC Library & Learning Center
- Research Guides

Drug Abuse, Addiction, Substance Use Disorder
- Research Drug Abuse
Start Learning About Your Topic
Create research questions to focus your topic, find books in the library catalog, find articles in library databases, find web resources, cite your sources, key search words.
Use the words below to search for useful information in books and articles .
- substance use disorder
- substance abuse
- drug addiction
- substance addiction
- chemical dependency
- war on drugs
- names of specific drugs such as methamphetamine, cocaine, heroin
- opioid crisis
Background Reading:
It's important to begin your research learning something about your subject; in fact, you won't be able to create a focused, manageable thesis unless you already know something about your topic.
This step is important so that you will:
- Begin building your core knowledge about your topic
- Be able to put your topic in context
- Create research questions that drive your search for information
- Create a list of search terms that will help you find relevant information
- Know if the information you’re finding is relevant and useful
If you're working from off campus , you'll be prompted to log in just like you do for your MJC email or Canvas courses.
All of these resources are free for MJC students, faculty, & staff.
- Gale eBooks This link opens in a new window Use this database for preliminary reading as you start your research. Try searching these terms: addiction, substance abuse
Other eBooks from the MJC Library collection:
Use some of the questions below to help you narrow this broad topic. See "substance abuse" in our Developing Research Questions guide for an example of research questions on a focused study of drug abuse.
- In what ways is drug abuse a serious problem?
- What drugs are abused?
- Who abuses drugs?
- What causes people to abuse drugs?
- How do drug abusers' actions affect themselves, their families, and their communities?
- What resources and treatment are available to drug abusers?
- What are the laws pertaining to drug use?
- What are the arguments for legalizing drugs?
- What are the arguments against legalizing drugs?
- Is drug abuse best handled on a personal, local, state or federal level?
- Based on what I have learned from my research what do I think about the issue of drug abuse?
Why Use Books:
Use books to read broad overviews and detailed discussions of your topic. You can also use books to find primary sources , which are often published together in collections.
Where Do I Find Books?
You'll use the library catalog to search for books, ebooks, articles, and more.
What if MJC Doesn't Have What I Need?
If you need materials (books, articles, recordings, videos, etc.) that you cannot find in the library catalog , use our interlibrary loan service .
All of these resources are free for MJC students, faculty, & staff.
- EBSCOhost Databases This link opens in a new window Search 22 databases simultaneously that cover almost any topic you need to research at MJC. EBSCO databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Gale Databases This link opens in a new window Search over 35 databases simultaneously that cover almost any topic you need to research at MJC. Gale databases include articles previously published in journals, magazines, newspapers, books, and other media outlets.
- Psychology and Behavioral Sciences Collection This link opens in a new window Contains articles from nearly 560 scholarly journals, some dating as far back as 1965
- Access World News This link opens in a new window Search the full-text of editions of record for local, regional, and national U.S. newspapers as well as full-text content of key international sources. This is your source for The Modesto Bee from January 1989 to the present. Also includes in-depth special reports and hot topics from around the country. To access The Modesto Bee , limit your search to that publication. more... less... Watch this short video to learn how to find The Modesto Bee .
Use Google Scholar to find scholarly literature on the Web:

Browse Featured Web Sites:
- National Institute on Drug Abuse NIDA's mission is to lead the nation in bringing the power of science to bear on drug abuse and addiction. This charge has two critical components. The first is the strategic support and conduct of research across a broad range of disciplines. The second is ensuring the rapid and effective dissemination and use of the results of that research to significantly improve prevention and treatment and to inform policy as it relates to drug abuse and addiction.
- Drug Free America Foundation Drug Free America Foundation, Inc. is a drug prevention and policy organization committed to developing, promoting and sustaining national and international policies and laws that will reduce illegal drug use and drug addiction.
- Office of National Drug Control Policy A component of the Executive Office of the President, ONDCP was created by the Anti-Drug Abuse Act of 1988. ONDCP advises the President on drug-control issues, coordinates drug-control activities and related funding across the Federal government, and produces the annual National Drug Control Strategy, which outlines Administration efforts to reduce illicit drug use, manufacturing and trafficking, drug-related crime and violence, and drug-related health consequences.
- Drug Policy Alliance The Drug Policy Alliance (DPA) is the nation's leading organization promoting alternatives to current drug policy that are grounded in science, compassion, health and human rights.
Your instructor should tell you which citation style they want you to use. Click on the appropriate link below to learn how to format your paper and cite your sources according to a particular style.
- Chicago Style
- ASA & Other Citation Styles
- Last Updated: Apr 25, 2024 1:28 PM
- URL: https://libguides.mjc.edu/drugabuse
Except where otherwise noted, this work is licensed under CC BY-SA 4.0 and CC BY-NC 4.0 Licenses .
- Open access
- Published: 12 December 2022
School-based harm reduction with adolescents: a pilot study
- Nina Rose Fischer 1
Substance Abuse Treatment, Prevention, and Policy volume 17 , Article number: 79 ( 2022 ) Cite this article
14k Accesses
6 Citations
379 Altmetric
Metrics details
A pilot study of Safety First: Real Drug Education for Teens showed significant results pre to post curriculum with high school freshmen. Negative outcomes of drug education are linked to a failure to engage students because of developmentally inappropriate materials that include activities that have no relevance to real experiences of young people. The few harm reduction studies showed increased student drug related knowledge. Students were less likely to consume substances, and less likely to consume to harmful levels. More studies are necessary to evidence harm reduction efficacy in the classroom. The goal of this study was to measure harm reduction knowledge and behaviors, including drug policy advocacy, before and after Safety First. Data were analyzed using McNemar’s test, ANOVA, linear regression, t -tests and thematic coding. Survey results, corroborated by the qualitative findings, showed a significant increase ( p < .05) in high school freshmen harm reduction knowledge and behaviors in relationship to substance use pre to post Safety First. This increase related to a decrease in overall substance use. Harm reduction is often perceived as a controversial approach to substance use. These findings have implications for further study of what could be a promising harm reduction-based substance use intervention with teens.
Research has shown that common reasons drug education programs for youth have failed were lack of student interest because they were not developmentally appropriate, or because activities did not relate to their actual lives [ 1 , 2 ]. A review of school-based drug education studies [ 1 ] showed that for substance use education programs to be effective they should be based on the real experiences of young people, a harm reduction principle [ 1 , 2 , 3 ]. The study of Drug Policy Alliance’s (DPA) Safety First: Real Drug Education for Teens (hyperlinked) drug education curriculum for health education classes is grounded in harm reduction theory. The objective of the curriculum is to teach substance use harm reduction to support positive outcomes for young people.
Harm reduction theory
Harm reduction theory includes pragmatic strategies aimed at reducing dangers related to substance use. The theory emerged with the discovery of AIDS in 1981. Harm reduction was important for reducing transmission of blood-borne infections and for addressing drug use. Evidence has shown that harm reduction approaches greatly reduce morbidity and mortality associated with risky substance use behaviors [ 4 , 5 , 6 ] but has rarely been used to inform drug education curriculum for teenagers.
Harm reduction is an ecological systems approach, addressing drug use from the micro level, individuals, families and communities to the macro level, local, state, and federal policies and norms [ 3 , 7 , 8 , 9 ]. The theory promotes social justice with an emphasis on users’ rights, health, social and economic development, as opposed to the demonization of drug consumption [ 10 ]. Critical to the practice of harm reduction is recognizing that realities of poverty, class, racism, social isolation, past trauma, sex and gender-based discrimination and other social inequalities affect people’s capacity to address drug-related harm. Aims of this study were to measure student ability to understand and advocate for socially just harm reduction policy pre and post Safety First.
Harm reduction interventions vary according to dynamic needs of individuals and communities. The goals are to meet substance users “where they’re at,” incorporating a spectrum of strategies from abstinence, to managing use, to addressing conditions of use along with use itself. The theory adopts tenets of the trans theoretical stages of change model [ 11 , 12 ] and motivational counseling [ 13 ]. This non-judgmental, amoral approach encourages people to embark on incremental, harm-reducing goals. A harm reduction approach is congruent with what is known about adolescent development and decision-making. However, the most prevalent drug education for teens has been abstinence based, attaching stigma and moral judgment to substance use and users, instead of learning the effects and how to make informed, healthy decisions about use [ 14 , 15 ].
School based harm reduction programs have rarely received the attention of researchers. Limited studies exist about harm reduction drug education with adolescents in the US [ 1 ]. Only a few studies, from Canada, Australia and the UK showed positive results [ 1 , 2 , 16 , 17 ]. Classroom based harm reduction approaches are limited but are gaining traction in school settings because of the mixed or ineffective results from prevention and abstinence-based programs that failed to meet the real needs of youth [ 2 , 18 ]. The small pool of studies showed increase in drug related knowledge. Students were less likely to consume substances and were less likely to consume to harmful levels with themselves and peers [ 1 , 2 , 16 , 17 ]. Harm reduction can potentially address the shortfalls of prevention programs but remains contentious in the context of youth substance use, thus has not been widely studied within this population [ 2 ].
Dr. Marsha Rosenbaum, the founder of Drug Policy Alliance (DPA) developed a pamphlet for parents about harm reduction and teens in 1999 where she defined principles for school drug education and ultimately for the Safety First curriculum, “Parents and teachers are responsible for engaging students, providing them with credible information [to] make responsible decisions, avoid drug abuse, and stay safe. Curricula should be age-specific, emphasize student participation, and provide science-based educational materials.” Harm reduction principles require a non-judgmental, motivational, culturally relevant, actively engaging environment that puts student experience at the center of the curriculum [ 2 ]. Safety first includes these elements.
Safety First teaches students about different types of drugs including the short and long-term effects. Students learn how to identify viable research about drugs and discuss and present their findings in the classroom. Drug beliefs are discussed, myths are dispelled, and facts are validated. Behaviors associated with substance use are studied and discussed to inform student’s future decision making. These key principles make up the operational definition of harm reduction reflected in the Safety First curriculum and measured in the study.
The Safety First curriculum developers trained teachers that participated in the pilot studies for three, 8 hours sessions and coached them weekly for at least an hour in the content and modalities of the curriculum. The developers provided technical assistance for curriculum implementation. All teachers delivered the curriculum one to two times per week, depending on the schedule of their health classes, in each of the schools. The class lasted one semester, up to 14 sessions, at 55 minutes per class. The materials necessary for each class were all easily accessible through free downloads online and physically from the DPA curriculum developer/trainers. “How the curriculum was taught” was the variable that had the most effect on the efficacy of the curriculum and is analyzed below.
The overall goal of the study was to measure harm reduction knowledge and behaviors before and after Safety First. Diverse urban public schools were the foci for the pilots in New York City and San Francisco. Outcomes showed change from pre to post Safety First ( p < .05) in knowledge and behaviors related to substance use. The results corroborated the findings from the few other similar studies [ 1 , 2 , 16 , 17 , 19 ]. This study evidenced need for further implementation of harm reduction based substance use curriculum as part of health education in high schools and for more research to measure the effects of the curriculum with various populations and locales.
The hypotheses of this study were related to the aims of the Safety First: Real Drug Education for Teens curriculum. The curriculum developers hoped to educate freshmen high school students about harm reduction knowledge and behavior. Students will 1) Acquire critical thinking skills to access and evaluate information about alcohol and other drugs [knowledge and behavior]; 2) Understand decision-making and goal setting skills that help students make healthy choices related to substance use [knowledge and behavior]; 3) Develop personal and social strategies to manage the risks, benefits and harms of alcohol and other drug use [behavior]; 4) Know the impact of drug policies on personal and community health [knowledge]; and 5) Learn to advocate for health-oriented drug policies [behaviors]. Thus student knowledge and behavior related to substance use and harm reduction were measured before and after Safety First as part of required health education classes to determine the efficacy of the curriculum.
Data collection
Hypotheses were tested through the collection of data from validated pre/post quantitative surveys (Additional file 1 : Appendix A in the data portal: Appendices A-D can be found in the Data Portal linked here) with items that measured substance use and harm reduction knowledge and behaviors [ 20 , 21 , 22 ] pre/post qualitative focus groups and one on one interviews with semi-structured field-tested guides; and field observation, on a weekly basis in each class with a field tested template. The 14-session (55 minutes/class) curriculum was implemented and studied in four freshmen health education classes at a public school in New York City and five public schools, four classes each, in San Francisco, CA. Researchers committed to different class periods and conducted field observation on different class days weekly to ensure inter-rater reliability [ 23 ].
Demographics (Table 1 )
Participants.
Students were recruited through both purposive and random sampling methods. Drug Police Alliance (DPA) built purposeful relationships with health teachers that wanted to implement Safety First as part of their required substance use unit in New York City. Relationships were built between DPA and San Francisco health teachers through the Adolescent Health Group- a Department of Education arm that oversaw health education curriculum. Students that participated in the pre/post focus groups and interviews were chosen randomly by alternating names on the class rosters.
The total number of freshmen surveyed in the overall pool was 701. Some students did not answer demographic questions which accounted for reduced “ n ” (Table 1 ). The items “What is the definition of abstinence” and “What is the definition of harm reduction” write in examples, were added to the San Francisco survey based on the findings from the initial New York City study. Thus the “ n ” for those items is less. Prior to Safety First most students had not received any drug education (96%). Students were 14 (62%) and 15 years old (31%). Outliers included 13, 16, 17, 18 & 19 years old (7%). Students were males (54%), and female (45.6%). In New York City two identified as “Other” and one as gender non-conforming (0.4%). The largest total ethnic/racial group was Asian (43%), then Latinx (22%), mixed race (12%), white (12%), Black (9%), Middle Eastern (1.8%) and Native American (.02%). In New York City white students were the largest ethnic/racial group, however youth of color made up the majority of the student population. In San Francisco Asian students were the majority student population, then Latinx. Black and white students were next with the same representation. Most New York City students resided in Brooklyn and Manhattan while other students were closely split between Queens and the Bronx. Most San Francisco students lived in Visitacion Valley and Excelsior district. Central Richmond, Outer Sunset and the Mission district vied for second. A small number of students in both cities reported police contact, arrest and/or suspension (Table 1 ). Youth reported substance use as a reason for police involvement.
Sample comparability
The total sample included three higher and three lower achieving schools, all public. The New York City school was unique because students applied and interviewed to be accepted. Pupils were high achieving coming in, average grades were “A’s” and “B’s.” All students planned to attend college and graduate school. Two out of the five San Francisco public schools were like the New York City site in grades and graduation rates but were not admissions based. The remaining three schools had students with lower grade point averages, with more of a range when asked about future plans. All were in politically progressive US coastal cities. All were ethnically diverse, and to an extent reflective of their city’s populations. All schools consisted of students from diverse economic backgrounds. Thus, this body of research from a sample of 701 students in New York City and San Francisco could possibly be extrapolated to students in similar locales with diverse achievement levels, racial and class demographics (Table 1 ).
Data analysis
McNemar’s test was applied to analyze if the harm reduction knowledge and behavior change from before to after Safety First was significant on four critical items (Table 2 ). One-way ANOVA tests were conducted to determine if there was an effect by demographics on substance use knowledge and behavior survey responses (Additional file 1 : Appendix B-D). Linear regression was employed to determine if race or gender were predictive of responses. Qualitative responses were aggregated using thematic codes based on the emergent themes from the “write in” responses on the pre/post surveys, and the interview and focus group transcription and were transformed into quantitative codes to count and compare student responses (Table 2 below, and items 40–44 in Additional file 1 : Appendix A and Appendix B in data portal). Outcomes showed that students learned critical thinking, decision-making and harm reduction strategies. Items that did not show remarkable results, or were null, also informed future implications for Safety First.
The purpose of this pilot study was to determine if DPA’s newly rolled out Safety First: Real Drug education for Teens potentially increased harm reduction knowledge and behaviors for high school freshmen. The findings from the pre and post survey, fortified by the qualitative data, showed a likely increase in student harm reduction knowledge about drug contents and effects, drug research, positive behaviors related to substance use, and drug policies. The results demonstrated that the curriculum most likely influenced overall student substance use knowledge and behavior.
Students showed change in knowledge about, and behaviors related to harm reduction, abstinence, how to detect an opioid overdose, school specific drug policies, and how to advocate for harm reduction based drug policy after Safety First ( p < .001) (Table 2 ). Students were more involved with advocacy activities after Safety First than before ( p < .001). It is likely that learning about activism and advocacy as part of the curriculum contributed to this increase in advocacy activities ( p < .001). More youth advocated for less punitive drug policies after Safety First ( p < .001).
Themes about drug policy advocacy that emerged from the qualitative data collected from the students after the class pointed to “creating systems of support,” “reducing stigma,” and “lessening punishments.” When before Safety First the themes were advocacy for suspension and jail time. Students mentioned passing along what they learned to fellow classmates, family members, and school administrators after the class to help them improve decision-making about drugs and create fairer drug policies.
ANOVA tests revealed that the most influential effect on student response was from the school they attended, indicating that how a specific teacher taught the curriculum most likely mattered (see below and Appendices B-D). Students from specific schools post Safety First showed more understanding of drug policies, how to advocate for harm reduction based initiatives, and how to respond to an opioid overdose (Table 2 ). However, there was remarkable change across all student comprehension despite differences in how the curriculum was taught.
Likert scale pre to post
Paired t- tests were conducted to determine if there was a significant difference between students’ scores on 20 Likert Scale items after the drug education course. The scale was one strongly agree and five strongly disagree. Seventeen were significant from pre to post Safety First ( p < .001) (Additional file 1 : Appendix C). Two of the three items that had no statistical significance, “People do not become dependent upon marijuana,” and “If you overdose on a drug you will die,” still showed a shift towards disagree, the harm reduction response, through means comparison. The item “It is better not to drink water while using MDMA (“molly”)” did not show a significant change. The students agreed more with this statement after Safety First. The harm reduction answer was strongly disagree. More students also agreed that “Alcohol helps you deal with uncomfortable feelings” which showed a significant change from pre to post ( p < .037), producing a null hypothesis. This outcome provides valuable feedback to the Safety First developers. They need to review how Safety First addresses harm reduction related to MDMA and alcohol.
Gender and race
For San Francisco, an Independent Sample t -test showed “Gender” mattered on two items. More males strongly disagreed that “Marijuana is safe because it is all natural,” than females ( p < .001). More females moved to strongly agreeing that “You can die from drinking too much alcohol at one time” after Safety First than males ( p < .001). An independent t -test was administered to measure if gender had an impact on students’ scores on the Likert Scale items. There was a significant difference between males and females on two items in New York City (Additional file 1 : Appendix C). Females were less likely to agree than males that, “People do not become dependent on marijuana,” ( p < .05). Females were also less likely than males to agree that zero tolerance drug policies make schools safer ( p < .05). A linear regression demonstrated that race and gender ( p > .05) were not predictive of significantly different test scores in either city. In San Francisco more males strongly disagreed than females about the item “Marijuana is safe because it is all natural” ( p < .001). On the item “You can die from drinking too much alcohol at one time” females more strongly agreed than males ( p < .001).
An ANOVA test showed that race and religion had an effect on student responses. Asian students were more likely to move towards disagreeing with the statement “Marijuana is safe because it is all natural” which was the harm reduction response, in comparison to Latinx and Black students ( p < .001). Muslim students were more likely to move towards disagreeing with the statement “People do not become dependent upon marijuana,” in comparison to Jewish students ( p = .020). ANOVA tests showed school site had the most influence on student responses to the Likert Scale items from pre to post (Additional file 1 : Appendix C).
Pre to post: substance use behaviors
On the pre/post survey there were questions about amount and likelihood of specific substance use: 1) to understand prevalence of substance use amongst the population; and 2) to see if learning about harm reduction influenced students’ behaviors/decision making. The majority of students did not report smoking or vaping tobacco but the few students that did, smoked a significant amount, this did not change from pre to post. For marijuana, students reported decreased use from pre to post ( p < .001) (see below and Additional file 1 : Appendix D). Marijuana use with a date showed remarkable change from “I would probably not use” to almost completely “I would definitely not use marijuana” ( p < .001). There was a decrease in alcohol use from pre to post ( p < .001). There was also an overall decrease in students reporting prescription drug use ( p < .001) (Additional file 1 : Appendix D).
ANOVA tests were administered to see if the demographic factors had an effect on the substance use behavior outcomes from pre to post Safety First (Additional file 1 : Appendix D). A one-way AVOVA yielded that Asian students were more likely to move towards “I would definitely not take/smoke weed with family” than Black students ( p = .002). An independent sample t -test evidenced that young men were more likely than young women to use prescription drugs with friends ( p = .020). Results evidenced that students learned about harm reduction strategies. Prevalence of substance use amongst the population became clearer; harm reduction influenced students’ substance use behaviors/decision making from pre to post especially in relationship to marijuana and prescription drugs (Additional file 1 : Appendix D).
More students believed that their classmates were using substances after Safety First than before. This change indicated that the class could have made the students more aware of substance use prevalence. This reported prevalence reflected national numbers for this age group [ 24 ]. In 2016 SAMSHA’s comprehensive report on drug abuse and health showed that 7.3 million youth between 12 and 20 reported alcohol use. About 1 in 5 drank alcohol in the past month. An estimated 855,000 adolescents aged 12 to 17 smoked cigarettes in the past month [ 24 ]. An approximated 24.0 million 12 or older in 2016 were current users of marijuana and approximately 1.6 million adolescents used marijuana in the past month. The national study spoke to the prevalence of drug use by 14- and 15-year-old young people shown in the study [ 24 ]. Student receptivity to harm reduction strategies, substantiated collaterally through the overall reduction in student use, validated the potential relevance of this approach with high school students, starting with freshmen.
Overall harm reduction knowledge and behavior change
Thematic qualitative coding was used to identify the most emergent themes in this data. A code was assigned to prevalent themes and counted and compared to determine outcomes (Additional file 1 : Appendix B). Young people demonstrated an understanding of key harm reduction thought processes and strategies solidifying successful aspects of the Safety First curriculum [ 3 ]. Students made change in their ability to describe specific harm reduction strategies possibly due to Safety First ( p < .001). In response to “What would you do to make substance use safer?” More youth responded “1” “Realize and plan for set/setting and limits around goal setting related to substance use,” or understand the “Contents, dose, and dosage” than narrowly, “reduce harm” [ 3 ] after the class (Additional file 1 : Appendix B).
Neighborhood, class and race
Interviews unearthed themes related to a difference in student perceptions about substances based on neighborhood, class and race. Students that lived in lower income neighborhoods that were predominantly black and brown consistently believed that one should not do drugs because of the consequences observed in the community. For example, when asked, “What happens in your community when someone is under the influence of drugs or is found with drugs on them?” A 14-year-old African American young woman from Brownsville Brooklyn responded in the pre and post interview, “Arrest. People get shot. People go to the hospital. People go to jail.”
When asked the same question before the class, a white female student that lived in the Upper Westside of Manhattan stated,
I have to admit that I live in a privileged neighborhood. So the use of drugs actually wouldn’t be that bad. Because it’s not like there’s the strongest police force patrolling my neighborhood, which is a huge part of it, like a part that I have to admit.
When asked the same question after Safety First she answered, “… there’s such a low risk for me to be put in a position where I’m...criminalized. So I don’t have to worry walking down the street if I have weed with me or something.”
When asked, “Are different groups of people treated differently if they have or are using drugs? If so, how?” the same African American young woman above explained the neighborhood, class and race differences:
If you seem like a person from a rich up town neighborhood or family using them [drugs], you would immediately think that they got them from somebody else. And then you will look to someone from a poor community who has them [drugs] and blame them, which is a stereotype that I really hate. I think that most of the times if someone from a rich family gets caught with drugs, they’re not gonna get nothing more than a warning. If someone from a poor community or an African or the Hispanic race gets caught, they are going to jail.
A young white woman from an affluent neighborhood’s pre response corroborated her response through her answer to the same question,
At my middle school there was a situation where a guy, mixed race black and white, bought weed for his friend, a white girl. Then she was high in school with that weed. She didn’t even get into as much trouble as the kid who bought it. Everyone in the school was pointing out, he’s biracial, so he’s black. He had a two-week out of school suspension for buying her the weed off campus and she had nothing.
Her post response to the question, “Are different groups of people treated differently if they have or are using drugs? If so, how?” was informed by the drug policy race and class session,
For sure. Low-income groups, African American communities, people of color in general, are so much quicker to be criminalized and prosecuted for having drugs, especially marijuana. I know now that there’s a disproportionate incarceration rate for men of color caught with marijuana.
Themes from student interviews, focus groups, and “write in” answers about the unequal treatment of people using or selling substances because of race, class and neighborhood reflected class lessons from Safety First about inequality in drug policy implementation. The findings indicated that the class increased student knowledge about critical social justice topics. Social justice is key to the harm reduction approach [ 25 ].
Student evaluation of safety first
The majority of students had a positive evaluation of Safety First. Fifty-five percent ( n = 389) of students reported that they would recommend Safety First. Thirty-nine percent ( n = 274) stated they would recommend Safety First with some changes. Six percent ( n = 45) relayed they would not recommend Safety First. Thus 94% of the students believed Safety First was a worthwhile experience. Quantitative coding of the most prevalent themes from the qualitative data sources informed what the students liked best about Safety First.
Direct quotes exemplified the coded themes: Code “1” learning about harm reduction strategies, including what to do in an overdose, a non-judgmental approach to teaching drug education, and I liked ‘everything’: “I actually learned a lot and didn’t feel like I was just being told that drugs were awful, and trying them makes you an awful person,” “I learned how to be safe and smart;” “High schoolers are more prepared for anything involving drug usage and overdose;” “It was not one of those ‘DARE’ abstinence only curriculums where they try to convince you that weed is a gateway to heroine and you will die if you try molly. I actually felt like I learned something that wasn’t fear based;” and “You seem to have tried really hard to make this curriculum great and it shows.” Code “2” learning about different substances: “I like learning about the different effects different drugs can do to your brain and body.” Code “3” the interactive/engaging activities and liking how the teacher taught the class overall, “I liked the different activities that we did that demonstrated different scenarios and substances, also the teacher explained it very well” and “I liked the part where we drank the Koolaid for a party experiment.” Code “4” videos and mixed media, “The videos including the ASAP science videos,” and “I absolutely love that youtube channel,” “I liked the videos, they were informative.” Code “5” was “Nothing” or “I Don’t Know.” “Learning about specific substances” ( n = 216, 40%) was what the majority of students liked about Safety First. Students wrote “Nothing” or Didn’t Know second ( n = 137, 25%); the interactive and engaging activities third ( n = 87, 16%); learning harm reduction strategies fourth ( n = 81, 15%) and videos were the least mentioned ( n = 18, 3.3%).
“No Judgement,” “Harm Reduction Skills,” and “Real Drug Education” were other themes that emerged in the post evaluation of the curriculum: “I liked that it wasn’t very judgmental and understood that the chance of kids trying drugs is likely. I also liked the harm reduction strategies,” “I liked how the curriculum went in depth about the side effects of drugs and taught us how to research and find correct information about a drug. It was well organized, and I got so much out of it,” and “It did not look down on people who used! Safety First stated facts and was looking out for our well beings; no biased opinions.”
The data illustrated that youth learned about both harm reduction skills and knowledge, appreciated the non-judgmental element of the approach and enjoyed when it was taught using dynamic, interactive teaching modalities with mixed media.
The results demonstrated that after Safety First student harm reduction knowledge and behavior changed after Safety First ( p < .05). Prevalence of substance use amongst this student population became clearer. The issue of prevalence, as described above, is quite critical. Regardless of their moral beliefs parents, teachers, administrators, policy makers and a continuum of social services need to know that 14- and 15-year old’s are using substances, and for some, a remarkable amount daily and weekly (see below and Additional file 1 : Appendix D). Entrenched beliefs by policy makers and institutions that “abstinence-based drug education is more effective” persist even with the preponderance of evidence to expose their inefficacy and actual harm [ 14 , 15 ].
The goals of the Safety First developers did not expressly include reducing substance use. True harm reduction does not stigmatize substance use or assume that it is inevitably “wrong” or “dangerous.” [ 3 ] As a researcher I was curious about whether there would be a collateral effect from the curriculum on student drug use, since institutions that promote drug education often see reduced use and abstinence as a goal. Collateral findings did show a significant relationship ( p < .05) between increased knowledge and skills with reduced substance use over the course of the semester. Teaching students harm reduction influenced students’ substance use behaviors/decision making from pre to post especially in relationship to marijuana and prescription drugs (below and Additional file 1 : Appendix D).
Likert scale items
Seventeen of the Likert scale items on the pre/post survey were significant from pre to post Safety First because students’ answers demonstrated an increase in harm reduction knowledge and behaviors ( p < .001) (Additional file 1 : Appendix C). The item “It is better not to drink water while using MDMA (“molly”)” did not show a significant change. The students agreed more with this statement after Safety First. The harm reduction answer was to “strongly disagree.” More students also agreed that “Alcohol helps you deal with uncomfortable feelings” which showed a significant change from pre to post ( p = .037), producing a null hypothesis. The harm reduction answer was to “strongly disagree.” This outcome provided valuable feedback to the Safety First developers. They need to review how Safety First addresses harm reduction related to MDMA and alcohol.
The teaching effect
ANOVA tests revealed that the most influential effect on student knowledge and behavior change was from the school they attended. How the curriculum was taught was the most influential variable. Teachers need training and coaching about how to implement Safety First. Technical assistance must be available from the purveyor or other trained experts to ensure fidelity. Importantly, there was still remarkable change across all student comprehension despite differences in how the curriculum was taught.
Study limitations with recommendations
The recommendations that stem from the “Discussion” are to include more curricula about MDMA and alcohol; provide coaching, training and technical assistance for teachers to adhere to fidelity of Safety First and to use dynamic, interactive, engaging pedagogical modalities in the classroom.
Abundance of data
An abundance of data points were collected for this study. More explication and discussion of fidelity issues, classroom observations and teacher evaluations are rich fodder for future manuscripts. Further discussion and recommendations could be mined from additional analysis. An article that dives more deeply into solely the qualitative data would give nuanced texture to the unique narrative of the Safety First classroom experience. Ethnography and phenomenology could both be used for the data analysis of interviews, focus groups, field observations and “write in” survey data to produce additional, compelling literature.
Sustainability
Although there have been no longitudinal studies of a high school substance use harm reduction curriculum, research of drug prevention programs over time showed that positive effects last throughout high school but taper off after [ 26 ]. Most schools only require one semester of health. This pilot study showed that in 14 classes students learned advocacy skills to promote creative harm reduction oriented policies. A sustainability recommendation is for drug policy organizations to spearhead advocacy groups on school campuses so students can sustain the harm reduction messages throughout and after high school. Longitudinal studies to measure student behavior and knowledge over time are key to the sustainability of Safety First.
Transportability
Results from public schools in two urban coastal cities showed a remarkable change from pre to post Safety First. This study tested student response across literacy, class and achievement levels. The study population were an integrated, multicultural cohort of 14- and 15-year old’s in urban areas, and these discrete demographic groups- Asian (296), Latinx (141), male (381) and female (311) exceeded 100. A sample must be over 100 to be considered generalizable [ 27 ]. Thus, in order to expand the transportability of the results it is integral to see how Safety First works in suburban, rural or small predominantly white locales; or with predominantly Black youth in smaller towns or large cities [ 23 ]. Lesbian, Bisexual, Trans, Non-Binary and Gay youth should be study participants. Youth in “last chance” schools, on probation, in detention or elite private schools should also be identified. Can Safety First be implemented successfully in a different type of institution? A drug treatment facility or a community-based organization? Does the curriculum work with middle school youth or older teens/young adults? Future research should serve youth of different ages, across similar and new demographic factors, and in environments outside the purview of this study.
Randomized control groups
The scope and scale of this study did not allow for the randomized control groups. These would have allowed a direct comparison of the outcomes for young people that either did not have a substance use component in their health class or had been exposed to a prevention and/or abstinence-based curriculum. Future studies should include randomized control groups across various populations of youth. Albeit, this pre/post study design did show baseline student knowledge and behaviors and the effects of Safety first on students after the curriculum.
The Safety First: Real Drug Education for Teens curriculum had significant effect on a diverse population of freshmen from six public high schools in the United States. Students acquired critical thinking skills to access and evaluate information about alcohol and other drugs; they had a better understanding of decision-making and goal setting skills that increased healthy choices related to substance use; they developed personal and social strategies to manage the risks, benefits and harms of alcohol and other drug use; they knew the impact of drug policies on personal and community health; and students learned to advocate for health-oriented drug policies. Outcomes inform future research. The implications of the results were that Safety First should be tested at comparable and new school sites. Further study should include randomized survey samples and control groups. The generalizability of the results should be measured with similar and different populations, as well as test the same students overtime to show the endurance of the effects.
The results are timely. Student knowledge increase related to the detection and response to an opioid overdose is particularly relevant because of national prevalence [ 28 ]. Student interviews about unequal treatment of people using or selling drugs based on race, class, gender and neighborhood illustrated the importance of understanding the intersection particularly between drug policy, race and class. There are a dearth of studies about harm reduction in the classroom [ 2 , 16 , 19 ]. These pilot findings are seed for future research to support harm reduction education for youth.
Availability of data and materials
Data is included in the Tables below and Additional Tables and Appendices accessible through this link to DropBox .
McBride N. A systematic review of school drug education. Health Educ Res. 2003;18(6):729–42.
Article Google Scholar
Jenkins EK, Slemon A, Haines-Saah RJ. Developing harm reduction in the context of youth substance use: insights from a multi-site qualitative analysis of young people’s harm minimization strategies. Harm Reduct J. 2017:14–53.
Marlatt GA, Larimer ME, Witkiewitz K, editors. Harm reduction pragmatic strategies for managing high risk behaviors. 2nd ed. New York and London: Guildford Press; 2012.
Google Scholar
Langendam MW, van Brussel GH, Coutinho RA, van Ameijden EJ. The impact of harm-reduction-based methadone treatment on mortality among heroin users. Am J Public Health. 2001;91:774–8.
Article CAS Google Scholar
Amundsen EJ. Measuring prevention of HIV among injecting drug users. Addiction. 2006;101:911–2.
Odets W. AIDS education and harm reduction for gay men: psychological approaches for the 21st century. AIDS Public Policy J. 1991;9(1):1–18.
Duncan D, Nicholson T, Cli†ord P, Hawkins W, Petosa R. Harm reduction: an emerging new paradigm for drug education. J Drug Educ. 1994;24:281–90.
Bronfenbrenner U. The ecology of human development. Cambridge: Harvard University Press; 1979.
Moffat BM, Haines-Saah RJ, Johnson JL. From didactic to dialogue: assessing the use of an innovative classroom resource to support decision-making about cannabis use. Drug Educ Prev Policy. 2016;24:85–95.
Roche AM, Evans KR, Stanton WR. Harm reduction: roads less traveled to the holy grail. Addiction. 1997;92:1207–12.
Elovich R, Staying negative. It is not automatic: a harm-reduction approach to substance use and sex. AIDS Public Policy J. 1996;11(2):66–77.
CAS Google Scholar
Prochaska JO, Redding C, Harlow L, Rossi J, Rossi J, Velicer W. The transtheoretical model of change and HIV prevention: a review. Health Educ Q. 1994;21:471–86.
Miller WR, Rollnick S. Motivational interviewing: preparing people to change addictive behavior. New York: Guilford; 1991.
Cima R. DARE: the anti-drug program that never actually worked: Priceonomics; 2016.
Ennett S, Tobler NS, Ringwalt C, Flewelling R. How effective is drug abuse resistance education? a meta-analysis of Project Dare outcome evaluations. Am J Public Health. 1994;84(9):1394–401.
Poulin C, Nicholson J. Should harm minimization as an approach to adolescent substance use be embraced by junior and senior high schools? Empirical evidence from an integrated school- and community-based demonstration intervention addressing drug use among adolescents. Int J Drug Policy. 2005;16(6):403–14.
McKay M, Sumnall H, McBride N, Harvey S. The differential impact of a classroom-based, alcohol harm reduction intervention, on adolescents with different alcohol use experiences: a multi-level growth modeling analysis. J Adolesc. 2014;37:1057–67.
Farrugia A. Assembling the dominant accounts of youth drug use in Australian harm reduction drug education. Int J Drug Policy. 2014;25:663–72.
Ringwalt CL, Clark HK, Hanley S, Shamblen SR, Flewelling RL. Project ALERT: a cluster randomized trial. Arch Pediatr Adolesc Med. 2009;163(7):625–32.
Ringwalt CL, Clark HK, Hanley S, Shamblen SR, Flewelling RL. The effects of project ALERT one year past curriculum completion. Prev Sci. 2010;11(2):172–84.
Kovach HC, Ringwalt CL, Hanley S, Shamblen SR. Project Alert's effects on adolescents' prodrug beliefs: a replication and extension study. Health Educ Behav. 2010;37(3):357–76.
Armstrong D, Gosling A, Weinman J, Marteau T. The place of inter-rater reliability in qualitative research: an empirical study. Sociology. 1997;31(3):597–606.
Ahrnsbrak R, Jonaki B, Hedden SL, Lipari RN, Park-Lee E. Key substance use and mental health indicators in the United States: results from the 2016 National Survey on drug use and health. Originating Office Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration, 2017.
Bernadette P. Harm reduction through a social justice lens. Int J Drug Policy. 2008;19(1):10–7.
Lohrmann DK, Ater R, Greene R, Younoszai T. Long-term impact of a district-wide school/community-based substance abuse prevention initiative on gateway drug use. J Drug Educ. 2005;35(3):233–53.
Burmeister E, Aitken L. Sample size: how many is enough? Australian Critical Quality. Substance Abuse and Mental Health Services Administration, 2012.
Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015:559–74.
Download references
Acknowledgements
Not Applicable.
The Drug Police Alliance awarded funding for this study through the Research Foundation of the City University of New York.
Author information
Authors and affiliations.
John Jay College of Criminal Justice, 524 W. 59th Street Rm. 6.65.09, New York, NY, 91001, USA
Nina Rose Fischer
You can also search for this author in PubMed Google Scholar
Contributions
This author developed the data collection tools, analyzed the data and wrote up the findings. The author(s) read and approved the final manuscript.
Authors’ information
NDr. Nina Rose Fischer is an Associate Professor at City University of New York John Jay College of Criminal Justice in Interdisciplinary Studies where she develops courses about social justice. She is the Co-Director of the prestigious Vera Fellows Program for social justice. She has 25 years experience in harm reduction and youth justice as an organizer, therapist, administrator, policy analyst and researcher. She is currently Principal Investigator on three original research projects 1) youth and police relations; 2) substance use harm reduction; and 3) arrest diversion. She published an article: Interdependent fates: Youth and police—Can they make peace? Peace and Conflict: Journal of Peace Psychology : https://doi.org/10.1037/pac0000466 and a book called The Case for Youth Police Initiative: Interdependent Fates and the Power of Peace, an ethnographic exploration of young people and police relations; as well as recommendations for how law enforcement can benefit from social welfare infrastructure. She is working on creative avenues to disseminate her findings including a docuseries about young people and police in hostile environments envisioning what safety really means. Critical race, class and gender analyses are central to her work as an activist scholar.
Corresponding author
Correspondence to Nina Rose Fischer .
Ethics declarations
Ethics approval and consent to participate.
Institutional Review Board through the Graduate Center City University of New York approval was granted before the study was conducted with human subjects. The reference number is 2017–0746. The date of initial registration was June 29th, 2017, and continued approval has been granted through August 8th, 2022.
Consent for publication
All data collection tools were anonymous. No identifying information was collected. Parental Consent and Adolescent Assent forms were signed by students and parents allowing their adolescent children to participate in the study. Teachers also signed consent forms.
Competing interests
This author declares no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., summary pre and post substance use behaviors.
Tobacco use showed no significant change form pre to post. On average, youth reported being with youth that used tobacco or that they used tobacco themselves monthly or never (3.70) before and after Safety First. On average, youth reported being with youth that used alcohol, or using alcohol themselves monthly or never (3.70) before and after Safety First. Tobacco and alcohol showed no significant change from pre to post. Marijuana was a different story. Students believed that fewer peers used marijuana on average (31%) after Safety First than before the harm reduction unit (43%). Students reported spending more time with students that used marijuana on average from monthly or never (Mean-μ = 3.29) closer to monthly (μ = 3.15). Youth reported marijuana use was monthly or never (μ = 3.80) pre to post.
Marijuana use showed a significant change from “I would probably not use” to almost completely “I would definitely not use” if “...your date is using marijuana” after Safety First. Prescription drug use and alcohol use showed no significant change from pre to post, staying an average between “I would probably not use” to “I would definitely not use.”
Students made a remarkable change from pre to post in their ability to describe specific harm reduction strategies in response to “What would you do to make substance use safer? ” Average youth response moved from “2” just reduce harm (μ = 2.25) to “1” Realize and plan for set/setting and limits around goal setting related to substance use, or Contents, Dose, Dosage including reduction of use (μ = 1.60).
An ANOVA was administered to see if any of the demographic factors had an effect on the substance use behavior outcomes from pre to post Safety First. Race and gender had the only effects. A one-way AVOVA yielded that Asian students were more likely to move towards “I would definitely not take/smoke weed with family” than black students [F(6, 556) = 3.50, p = .002]. An independent sample t -test evidenced that young men were more likely than young women to use prescription drugs with friends (Mean-μ = −.92) to (μ = − 1.31), t(111) = 2.35, p = .020.
The above results evidenced that the curriculum taught the students about harm reduction strategies. Prevalence of substance use amongst the population became more clear; harm reduction seemed to influence students’ substance use behaviors/decision making from pre to post Safety First, especially in relationship to marijuana and prescription drugs; and students clearly demonstrated an increase in knowledge of harm reduction strategies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Fischer, N.R. School-based harm reduction with adolescents: a pilot study. Subst Abuse Treat Prev Policy 17 , 79 (2022). https://doi.org/10.1186/s13011-022-00502-1
Download citation
Accepted : 27 October 2022
Published : 12 December 2022
DOI : https://doi.org/10.1186/s13011-022-00502-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Harm reduction education
- Classroom based substance use curriculum
- Adolescent substance use
- Mixed methods research
Substance Abuse Treatment, Prevention, and Policy
ISSN: 1747-597X
- General enquiries: [email protected]

Grant Writing Academy Newsletter

How to Write a Grant Proposal for Drug Prevention Programs
Craft a winning grant proposal for drug prevention program.

The importance of drug prevention programs cannot be overstated. These programs play a pivotal role in society, acting as a barrier between potential drug abuse and healthy living.

However, funding remains a constant challenge for such initiatives. Securing grants can be a vital lifeline for these programs, but to do so, you need a compelling grant proposal.
Here's how to craft one.
1. Understand Your Funder
Before you begin writing, research potential funders. Understand their priorities, past grants, and their objectives. Aligning your program with the funder’s goals increases the chances of your proposal being accepted.
Example: If a potential funder has previously supported programs focusing on youth drug prevention, emphasize how your initiative targets young individuals, perhaps through school-based campaigns or youth mentorship programs.
2. Executive Summary
This is the first thing potential funders will read. Keep it concise, yet powerful. Introduce the problem, your solution, the amount you’re requesting, and a brief overview of the program's expected outcomes.
Example: “Youth substance abuse in XYZ city has risen by 20% in the past five years. Our organization seeks $50,000 to launch a comprehensive drug prevention initiative targeting schools, aiming to reduce this statistic by 50% within two years.”
3. Introduction to Your Organization
Detail your organization's history, accomplishments, and its experience in drug prevention or related fields. This establishes your credibility.
Example: “Founded in 2010, ABC Foundation has successfully spearheaded 15 community health programs, directly impacting over 10,000 lives.”
4. Needs Statement
Clearly articulate the problem. Use statistics, stories, or case studies to paint a vivid picture of why the program is crucial.
Example: “In XYZ city, one in every five high school students admitted to trying illicit substances. This alarming statistic is compounded by an increase in drug-related crimes and school dropouts.”
5. Program Description
Detail the ins and outs of your drug prevention program. This includes:
Goals and Objectives: Clear, measurable targets your program aims to achieve. Example: “Goal: Reduce youth drug experimentation by 50% within two years. Objective 1: Reach 10,000 students with our school-based program.”
Methods: How you intend to achieve these objectives. Example: “Collaborate with local schools to incorporate drug education into their curriculum.”
Staff/Volunteers: List and describe the key players. Example: “Led by Dr. Jane Doe, a professional with 10 years of experience in drug prevention.”
Timeline: A detailed timeframe of your program’s activities. Example: “January - March: Program design and staff training. April - December: School engagements and community workshops.”
6. Evaluation
Describe how you’ll measure the program’s success. Funders want accountability.
Example: “A quarterly survey will be conducted in participating schools to gauge the program's effectiveness, tracking changes in students' attitudes, knowledge, and behavior concerning drug use.”
Provide a clear, itemized budget. This should include:
Direct Costs: Money that goes straight into the program, like materials, salaries, and equipment.
Indirect Costs: Overhead or administrative expenses.
Income: Potential revenue, like donations or other grants.
Justifications: Explain any costs that might raise questions.
Example: “$10,000 - Educational materials for schools. This ensures up-to-date, high-quality resources that engage students effectively.”
8. Sustainability
Grants often cover only a specific period. Demonstrate how you intend to sustain the program afterward.
Example: “Post-grant, we intend to partner with local businesses for sponsorship, host fundraising events, and integrate a small fee for some services, ensuring the program's continuity.”
9. Conclusion
Reiterate the importance of the program, the difference the grant will make, and express gratitude for the funder’s consideration.
Example: “With the rise of drug abuse in XYZ city, your support can be transformative. Together, we can ensure a brighter, healthier future for our youth. Thank you for considering our proposal.”
10. Supporting Documents
Include any additional materials that strengthen your case: letters of support, organizational charts, endorsements, or relevant news articles.
Example: A letter from the city's mayor, endorsing your program and its importance to the community.
Be clear and concise: Avoid jargon or overly technical language.
Tailor your proposal: Each funder is unique. Modify your proposal to cater to each funder’s priorities.
Follow guidelines: If the funder provides a specific format or guidelines, adhere to them strictly.
Conclusion:
Writing a grant proposal for drug prevention programs requires research, clarity, and a deep understanding of both the issue at hand and the potential funder. By clearly articulating the need, outlining your approach, and demonstrating the potential impact and sustainability, you significantly increase your chances of securing that much-needed grant for your program.
Remember, the goal is not just to secure funds but to bring about tangible, lasting change in the community.
Invitation: Exclusive Live Workshop on Grant Writing in Abuja
We are excited to extend an exclusive invitation to you for our upcoming Live Workshop on Grant Writing , scheduled to be held in the heart of Abuja by the end of November. This is a golden opportunity for individuals and organizations aiming to sharpen their grant-writing skills, gain in-depth insights into the world of grant-making, and increase their chances of securing essential funding.
Virtual Participation: Zoom Into Mastery
Can’t be there in person? No worries. Even if you can’t make it to Abuja physically, you don’t have to miss out on this transformative experience.
Register and make your payment , and we’ll connect you virtually via Zoom, ensuring you receive the same rich content and interactive learning as those attending live. Make payment here.
Event Details:
Date: 27th November, 2023 – 1st December, 2023
Time: 9:00 AM - 3:00 PM
Venue: Abuja, Nigeria
Why Attend?
Expert-Led Sessions: Our panel consists of renowned grant-writing professionals with a track record of securing millions in funds for diverse projects.
Hands-On Training: Dive deep into real-world grant applications, understand the do's and don'ts, and refine your approach with practical exercises.
Networking Opportunities: Rub shoulders with fellow grant writers, and potential collaborators.
Comprehensive Material: Every participant will receive a curated grant-writing toolkit, complete with templates, sample applications, and a list of potential grantors.
Workshop Highlights:
Foundation of Grant Writing: Learn the fundamental principles that set apart winning proposals from the rest.
Narrative Crafting: Uncover the art of storytelling in grant applications, ensuring your project stands out and resonates with funders.
Budgeting & Financial Projections: Understand how to create a robust and transparent financial plan that instills confidence in potential grantors.
Tailoring Applications: Every funder is unique. Gain insights into tailoring your applications to resonate with specific grantors' missions and values.
Feedback & Reviews: Get your past or draft applications reviewed by experts, garner constructive feedback, and learn ways to enhance them.
Registration Details:
Early Bird Fee: N350,000 (Includes workshop materials, lunch, and a certificate of participation.)
Early Bird Offer: Register by November 10th and avail a 10% discount!
How to Make Payment : Click here to make your payment and register or call us at +2348111442950 or email at [email protected] .
Late Registration Fee: N500,000
Note: Seats are limited, and registrations will be on a first-come, first-served basis. So, hurry and secure your spot today!
Join Us & Transform Your Grant Writing Journey!
The world of grant-making is competitive, but with the right skills and approach, you can significantly increase your chances of success. Whether you're a beginner stepping into the realm of grant writing or a seasoned professional looking for advanced strategies, this workshop promises value at every level.
Abuja, with its vibrant community of NGOs, startups, and institutions, is the perfect backdrop for this transformative event.
So, mark your calendars, spread the word, and gear up for a day of learning, networking, and empowerment!
We eagerly look forward to welcoming you and embarking on this enriching journey together.
Essential Reads for Grant Writing Excellence
Grants can unlock vast potentials, but securing them? That's an art and a science. Whether you're new to the field or looking to enhance your skills, these hand-picked titles will elevate your grant-writing game:
1. Advanced Grant Writing
Go Beyond Basics: Dive into strategies and techniques that make proposals irresistible. With insights into a reviewer's mindset, stand out and shine even in fierce competition.
2. Grant Readiness Guide:
Be Grant-Ready: Ensure your organization isn't just applying but is truly ready to manage and utilize grants. Streamline, assess, and position yourself for success from the get-go.
3. Mastering Grant Writing:
From Novice to Pro: Covering the entire spectrum of grant writing, this guide offers invaluable tips, examples, etc.. It's your blueprint to mastering the craft.
4. The Small Business Guide to Winning Grants:
Business-Specific Brilliance: Designed for small businesses, navigate the unique challenges you face. Find, apply, and win grants tailored just for you.
5. Becoming the Grant Guru:
Think, Act, Succeed: More than writing – it's about strategy and mindset. Step into the shoes of a guru, understand funder desires, and become indispensable in the grant world.
Why These Titles?
Securing grants isn't just about paperwork; it's about alignment, narrative, and persuasion. The above titles are your arsenal in this endeavor, carefully crafted to offer actionable insights for every level of expertise.
In a realm where competition is stiff, your edge lies in continuous learning and adaptation.
Grab these books, absorb their wisdom, and position yourself as the top contender in the grant game. Your journey to becoming a grant virtuoso begins with these pages. Dive in!
Unlock Your Grant Success!
Join our email list now for exclusive grant-writing tips and unique grant opportunities delivered straight to your inbox. Click here to Subscribe . Don't miss out!
Ready for more?
- Open access
- Published: 13 November 2021
Risk and protective factors of drug abuse among adolescents: a systematic review
- Azmawati Mohammed Nawi 1 ,
- Rozmi Ismail 2 ,
- Fauziah Ibrahim 2 ,
- Mohd Rohaizat Hassan 1 ,
- Mohd Rizal Abdul Manaf 1 ,
- Noh Amit 3 ,
- Norhayati Ibrahim 3 &
- Nurul Shafini Shafurdin 2
BMC Public Health volume 21 , Article number: 2088 ( 2021 ) Cite this article
148k Accesses
114 Citations
20 Altmetric
Metrics details
Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was adopted for the review which utilized three main journal databases, namely PubMed, EBSCOhost, and Web of Science. Tobacco addiction and alcohol abuse were excluded in this review. Retrieved citations were screened, and the data were extracted based on strict inclusion and exclusion criteria. Inclusion criteria include the article being full text, published from the year 2016 until 2020 and provided via open access resource or subscribed to by the institution. Quality assessment was done using Mixed Methods Appraisal Tools (MMAT) version 2018 to assess the methodological quality of the included studies. Given the heterogeneity of the included studies, a descriptive synthesis of the included studies was undertaken.
Out of 425 articles identified, 22 quantitative articles and one qualitative article were included in the final review. Both the risk and protective factors obtained were categorized into three main domains: individual, family, and community factors. The individual risk factors identified were traits of high impulsivity; rebelliousness; emotional regulation impairment, low religious, pain catastrophic, homework completeness, total screen time and alexithymia; the experience of maltreatment or a negative upbringing; having psychiatric disorders such as conduct problems and major depressive disorder; previous e-cigarette exposure; behavioral addiction; low-perceived risk; high-perceived drug accessibility; and high-attitude to use synthetic drugs. The familial risk factors were prenatal maternal smoking; poor maternal psychological control; low parental education; negligence; poor supervision; uncontrolled pocket money; and the presence of substance-using family members. One community risk factor reported was having peers who abuse drugs. The protective factors determined were individual traits of optimism; a high level of mindfulness; having social phobia; having strong beliefs against substance abuse; the desire to maintain one’s health; high paternal awareness of drug abuse; school connectedness; structured activity and having strong religious beliefs.
The outcomes of this review suggest a complex interaction between a multitude of factors influencing adolescent drug abuse. Therefore, successful adolescent drug abuse prevention programs will require extensive work at all levels of domains.
Peer Review reports
Introduction
Drug abuse is a global problem; 5.6% of the global population aged 15–64 years used drugs at least once during 2016 [ 1 ]. The usage of drugs among younger people has been shown to be higher than that among older people for most drugs. Drug abuse is also on the rise in many ASEAN (Association of Southeast Asian Nations) countries, especially among young males between 15 and 30 years of age. The increased burden due to drug abuse among adolescents and young adults was shown by the Global Burden of Disease (GBD) study in 2013 [ 2 ]. About 14% of the total health burden in young men is caused by alcohol and drug abuse. Younger people are also more likely to die from substance use disorders [ 3 ], and cannabis is the drug of choice among such users [ 4 ].
Adolescents are the group of people most prone to addiction [ 5 ]. The critical age of initiation of drug use begins during the adolescent period, and the maximum usage of drugs occurs among young people aged 18–25 years old [ 1 ]. During this period, adolescents have a strong inclination toward experimentation, curiosity, susceptibility to peer pressure, rebellion against authority, and poor self-worth, which makes such individuals vulnerable to drug abuse [ 2 ]. During adolescence, the basic development process generally involves changing relations between the individual and the multiple levels of the context within which the young person is accustomed. Variation in the substance and timing of these relations promotes diversity in adolescence and represents sources of risk or protective factors across this life period [ 6 ]. All these factors are crucial to helping young people develop their full potential and attain the best health in the transition to adulthood. Abusing drugs impairs the successful transition to adulthood by impairing the development of critical thinking and the learning of crucial cognitive skills [ 7 ]. Adolescents who abuse drugs are also reported to have higher rates of physical and mental illness and reduced overall health and well-being [ 8 ].
The absence of protective factors and the presence of risk factors predispose adolescents to drug abuse. Some of the risk factors are the presence of early mental and behavioral health problems, peer pressure, poorly equipped schools, poverty, poor parental supervision and relationships, a poor family structure, a lack of opportunities, isolation, gender, and accessibility to drugs [ 9 ]. The protective factors include high self-esteem, religiosity, grit, peer factors, self-control, parental monitoring, academic competence, anti-drug use policies, and strong neighborhood attachment [ 10 , 11 , 12 , 13 , 14 , 15 ].
The majority of previous systematic reviews done worldwide on drug usage focused on the mental, psychological, or social consequences of substance abuse [ 16 , 17 , 18 ], while some focused only on risk and protective factors for the non-medical use of prescription drugs among youths [ 19 ]. A few studies focused only on the risk factors of single drug usage among adolescents [ 20 ]. Therefore, the development of the current systematic review is based on the main research question: What is the current risk and protective factors among adolescent on the involvement with drug abuse? To the best of our knowledge, there is limited evidence from systematic reviews that explores the risk and protective factors among the adolescent population involved in drug abuse. Especially among developing countries, such as those in South East Asia, such research on the risk and protective factors for drug abuse is scarce. Furthermore, this review will shed light on the recent trends of risk and protective factors and provide insight into the main focus factors for prevention and control activities program. Additionally, this review will provide information on how these risk and protective factors change throughout various developmental stages. Therefore, the objective of this systematic review was to determine the risk and protective factors of drug abuse among adolescents worldwide. This paper thus fills in the gaps of previous studies and adds to the existing body of knowledge. In addition, this review may benefit certain parties in developing countries like Malaysia, where the national response to drugs is developing in terms of harm reduction, prison sentences, drug treatments, law enforcement responses, and civil society participation.
This systematic review was conducted using three databases, PubMed, EBSCOhost, and Web of Science, considering the easy access and wide coverage of reliable journals, focusing on the risk and protective factors of drug abuse among adolescents from 2016 until December 2020. The search was limited to the last 5 years to focus only on the most recent findings related to risk and protective factors. The search strategy employed was performed in accordance with the Preferred Reporting Items for a Systematic Review and Meta-analysis (PRISMA) checklist.
A preliminary search was conducted to identify appropriate keywords and determine whether this review was feasible. Subsequently, the related keywords were searched using online thesauruses, online dictionaries, and online encyclopedias. These keywords were verified and validated by an academic professor at the National University of Malaysia. The keywords used as shown in Table 1 .
Selection criteria
The systematic review process for searching the articles was carried out via the steps shown in Fig. 1 . Firstly, screening was done to remove duplicate articles from the selected search engines. A total of 240 articles were removed in this stage. Titles and abstracts were screened based on the relevancy of the titles to the inclusion and exclusion criteria and the objectives. The inclusion criteria were full text original articles, open access articles or articles subscribed to by the institution, observation and intervention study design and English language articles. The exclusion criteria in this search were (a) case study articles, (b) systematic and narrative review paper articles, (c) non-adolescent-based analyses, (d) non-English articles, and (e) articles focusing on smoking (nicotine) and alcohol-related issues only. A total of 130 articles were excluded after title and abstract screening, leaving 55 articles to be assessed for eligibility. The full text of each article was obtained, and each full article was checked thoroughly to determine if it would fulfil the inclusion criteria and objectives of this study. Each of the authors compared their list of potentially relevant articles and discussed their selections until a final agreement was obtained. A total of 22 articles were accepted to be included in this review. Most of the excluded articles were excluded because the population was not of the target age range—i.e., featuring subjects with an age > 18 years, a cohort born in 1965–1975, or undergraduate college students; the subject matter was not related to the study objective—i.e., assessing the effects on premature mortality, violent behavior, psychiatric illness, individual traits, and personality; type of article such as narrative review and neuropsychiatry review; and because of our inability to obtain the full article—e.g., forthcoming work in 2021. One qualitative article was added to explain the domain related to risk and the protective factors among the adolescents.
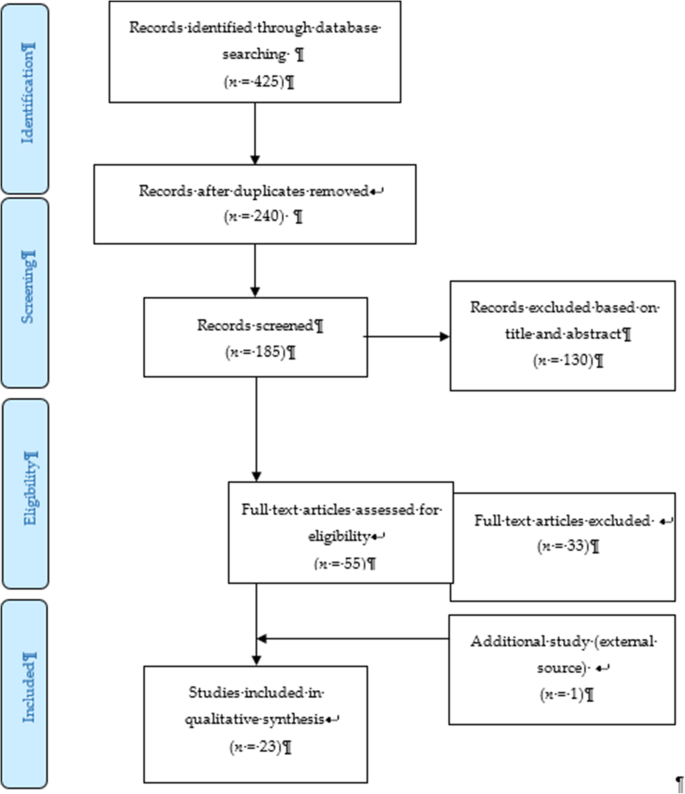
PRISMA flow diagram showing the selection of studies on risk and protective factors for drug abuse among adolescents.2.2. Operational Definition
Drug-related substances in this context refer to narcotics, opioids, psychoactive substances, amphetamines, cannabis, ecstasy, heroin, cocaine, hallucinogens, depressants, and stimulants. Drugs of abuse can be either off-label drugs or drugs that are medically prescribed. The two most commonly abused substances not included in this review are nicotine (tobacco) and alcohol. Accordingly, e-cigarettes and nicotine vape were also not included. Further, “adolescence” in this study refers to members of the population aged between 10 to 18 years [ 21 ].
Data extraction tool
All researchers independently extracted information for each article into an Excel spreadsheet. The data were then customized based on their (a) number; (b) year; (c) author and country; (d) titles; (e) study design; (f) type of substance abuse; (g) results—risks and protective factors; and (h) conclusions. A second reviewer crossed-checked the articles assigned to them and provided comments in the table.
Quality assessment tool
By using the Mixed Method Assessment Tool (MMAT version 2018), all articles were critically appraised for their quality by two independent reviewers. This tool has been shown to be useful in systematic reviews encompassing different study designs [ 22 ]. Articles were only selected if both reviewers agreed upon the articles’ quality. Any disagreement between the assigned reviewers was managed by employing a third independent reviewer. All included studies received a rating of “yes” for the questions in the respective domains of the MMAT checklists. Therefore, none of the articles were removed from this review due to poor quality. The Cohen’s kappa (agreement) between the two reviewers was 0.77, indicating moderate agreement [ 23 ].
The initial search found 425 studies for review, but after removing duplicates and applying the criteria listed above, we narrowed the pool to 22 articles, all of which are quantitative in their study design. The studies include three prospective cohort studies [ 24 , 25 , 26 ], one community trial [ 27 ], one case-control study [ 28 ], and nine cross-sectional studies [ 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ]. After careful discussion, all reviewer panels agreed to add one qualitative study [ 46 ] to help provide reasoning for the quantitative results. The selected qualitative paper was chosen because it discussed almost all domains on the risk and protective factors found in this review.
A summary of all 23 articles is listed in Table 2 . A majority of the studies (13 articles) were from the United States of America (USA) [ 25 , 26 , 27 , 29 , 30 , 31 , 34 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 ], three studies were from the Asia region [ 32 , 33 , 38 ], four studies were from Europe [ 24 , 28 , 40 , 44 ], and one study was from Latin America [ 35 ], Africa [ 43 ] and Mediterranean [ 45 ]. The number of sample participants varied widely between the studies, ranging from 70 samples (minimum) to 700,178 samples (maximum), while the qualitative paper utilized a total of 100 interviewees. There were a wide range of drugs assessed in the quantitative articles, with marijuana being mentioned in 11 studies, cannabis in five studies, and opioid (six studies). There was also large heterogeneity in terms of the study design, type of drug abused, measurements of outcomes, and analysis techniques used. Therefore, the data were presented descriptively.
After thorough discussion and evaluation, all the findings (both risk and protective factors) from the review were categorized into three main domains: individual factors, family factors, and community factors. The conceptual framework is summarized in Fig. 2 .
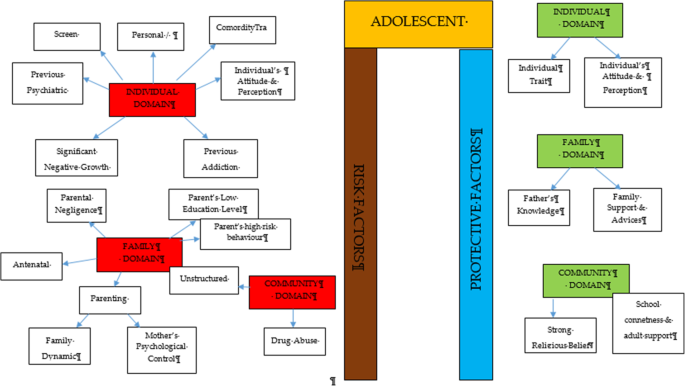
Conceptual framework of risk and protective factors related to adolescent drug abuse
DOMAIN: individual factor
Risk factors.
Almost all the articles highlighted significant findings of individual risk factors for adolescent drug abuse. Therefore, our findings for this domain were further broken down into five more sub-domains consisting of personal/individual traits, significant negative growth exposure, personal psychiatric diagnosis, previous substance history, comorbidity and an individual’s attitude and perception.

Personal/individual traits
Chuang et al. [ 29 ] found that adolescents with high impulsivity traits had a significant positive association with drug addiction. This study also showed that the impulsivity trait alone was an independent risk factor that increased the odds between two to four times for using any drug compared to the non-impulsive group. Another longitudinal study by Guttmannova et al. showed that rebellious traits are positively associated with marijuana drug abuse [ 27 ]. The authors argued that measures of rebelliousness are a good proxy for a youth’s propensity to engage in risky behavior. Nevertheless, Wilson et al. [ 37 ], in a study involving 112 youths undergoing detoxification treatment for opioid abuse, found that a majority of the affected respondents had difficulty in regulating their emotions. The authors found that those with emotional regulation impairment traits became opioid dependent at an earlier age. Apart from that, a case-control study among outpatient youths found that adolescents involved in cannabis abuse had significant alexithymia traits compared to the control population [ 28 ]. Those adolescents scored high in the dimension of Difficulty in Identifying Emotion (DIF), which is one of the key definitions of diagnosing alexithymia. Overall, the adjusted Odds Ratio for DIF in cannabis abuse was 1.11 (95% CI, 1.03–1.20).
Significant negative growth exposure
A history of maltreatment in the past was also shown to have a positive association with adolescent drug abuse. A study found that a history of physical abuse in the past is associated with adolescent drug abuse through a Path Analysis, despite evidence being limited to the female gender [ 25 ]. However, evidence from another study focusing at foster care concluded that any type of maltreatment might result in a prevalence as high as 85.7% for the lifetime use of cannabis and as high as 31.7% for the prevalence of cannabis use within the last 3-months [ 30 ]. The study also found significant latent variables that accounted for drug abuse outcomes, which were chronic physical maltreatment (factor loading of 0.858) and chronic psychological maltreatment (factor loading of 0.825), with an r 2 of 73.6 and 68.1%, respectively. Another study shed light on those living in child welfare service (CWS) [ 35 ]. It was observed through longitudinal measurements that proportions of marijuana usage increased from 9 to 18% after 36 months in CWS. Hence, there is evidence of the possibility of a negative upbringing at such shelters.
Personal psychiatric diagnosis
The robust studies conducted in the USA have deduced that adolescents diagnosed with a conduct problem (CP) have a positive association with marijuana abuse (OR = 1.75 [1.56, 1.96], p < 0.0001). Furthermore, those with a diagnosis of Major Depressive Disorder (MDD) showed a significant positive association with marijuana abuse.
Previous substance and addiction history
Another study found that exposure to e-cigarettes within the past 30 days is related to an increase in the prevalence of marijuana use and prescription drug use by at least four times in the 8th and 10th grades and by at least three times in the 12th grade [ 34 ]. An association between other behavioral addictions and the development of drug abuse was also studied [ 29 ]. Using a 12-item index to assess potential addictive behaviors [ 39 ], significant associations between drug abuse and the groups with two behavioral addictions (OR = 3.19, 95% CI 1.25,9.77) and three behavioral addictions (OR = 3.46, 95% CI 1.25,9.58) were reported.
Comorbidity
The paper by Dash et al. (2020) highlight adolescent with a disease who needs routine medical pain treatment have higher risk of opioid misuse [ 38 ]. The adolescents who have disorder symptoms may have a risk for opioid misuse despite for the pain intensity.
Individual’s attitudes and perceptions
In a study conducted in three Latin America countries (Argentina, Chile, and Uruguay), it was shown that adolescents with low or no perceived risk of taking marijuana had a higher risk of abuse (OR = 8.22 times, 95% CI 7.56, 10.30) [ 35 ]. This finding is in line with another study that investigated 2002 adolescents and concluded that perceiving the drug as harmless was an independent risk factor that could prospectively predict future marijuana abuse [ 27 ]. Moreover, some youth interviewed perceived that they gained benefits from substance use [ 38 ]. The focus group discussion summarized that the youth felt positive personal motivation and could escape from a negative state by taking drugs. Apart from that, adolescents who had high-perceived availability of drugs in their neighborhoods were more likely to increase their usage of marijuana over time (OR = 11.00, 95% CI 9.11, 13.27) [ 35 ]. A cheap price of the substance and the availability of drug dealers around schools were factors for youth accessibility [ 38 ]. Perceived drug accessibility has also been linked with the authorities’ enforcement programs. The youth perception of a lax community enforcement of laws regarding drug use at all-time points predicted an increase in marijuana use in the subsequent assessment period [ 27 ]. Besides perception, a study examining the attitudes towards synthetic drugs based on 8076 probabilistic samples of Macau students found that the odds of the lifetime use of marijuana was almost three times higher among those with a strong attitude towards the use of synthetic drugs [ 32 ]. In addition, total screen time among the adolescent increase the likelihood of frequent cannabis use. Those who reported daily cannabis use have a mean of 12.56 h of total screen time, compared to a mean of 6.93 h among those who reported no cannabis use. Adolescent with more time on internet use, messaging, playing video games and watching TV/movies were significantly associated with more frequent cannabis use [ 44 ].
Protective factors
Individual traits.
Some individual traits have been determined to protect adolescents from developing drug abuse habits. A study by Marin et al. found that youth with an optimistic trait were less likely to become drug dependent [ 33 ]. In this study involving 1104 Iranian students, it was concluded that a higher optimism score (measured using the Children Attributional Style Questionnaire, CASQ) was a protective factor against illicit drug use (OR = 0.90, 95% CI: 0.85–0.95). Another study found that high levels of mindfulness, measured using the 25-item Child Acceptance and Mindfulness Measure, CAMM, lead to a slower progression toward injectable drug abuse among youth with opioid addiction (1.67 years, p = .041) [ 37 ]. In addition, the social phobia trait was found to have a negative association with marijuana use (OR = 0.87, 95% CI 0.77–0.97), as suggested [ 31 ].
According to El Kazdouh et al., individuals with a strong belief against substance use and those with a strong desire to maintain their health were more likely to be protected from involvement in drug abuse [ 46 ].
DOMAIN: family factors
The biological factors underlying drug abuse in adolescents have been reported in several studies. Epigenetic studies are considered important, as they can provide a good outline of the potential pre-natal factors that can be targeted at an earlier stage. Expecting mothers who smoke tobacco and alcohol have an indirect link with adolescent substance abuse in later life [ 24 , 39 ]. Moreover, the dynamic relationship between parents and their children may have some profound effects on the child’s growth. Luk et al. examined the mediator effects between parenting style and substance abuse and found the maternal psychological control dimension to be a significant variable [ 26 ]. The mother’s psychological control was two times higher in influencing her children to be involved in substance abuse compared to the other dimension. Conversely, an indirect risk factor towards youth drug abuse was elaborated in a study in which low parental educational level predicted a greater risk of future drug abuse by reducing the youth’s perception of harm [ 27 , 43 ]. Negligence from a parental perspective could also contribute to this problem. According to El Kazdouh et al. [ 46 ], a lack of parental supervision, uncontrolled pocket money spending among children, and the presence of substance-using family members were the most common negligence factors.
While the maternal factors above were shown to be risk factors, the opposite effect was seen when the paternal figure equipped himself with sufficient knowledge. A study found that fathers with good information and awareness were more likely to protect their adolescent children from drug abuse [ 26 ]. El Kazdouh et al. noted that support and advice could be some of the protective factors in this area [ 46 ].
DOMAIN: community factors
- Risk factor
A study in 2017 showed a positive association between adolescent drug abuse and peers who abuse drugs [ 32 , 39 ]. It was estimated that the odds of becoming a lifetime marijuana user was significantly increased by a factor of 2.5 ( p < 0.001) among peer groups who were taking synthetic drugs. This factor served as peer pressure for youth, who subconsciously had desire to be like the others [ 38 ]. The impact of availability and engagement in structured and unstructured activities also play a role in marijuana use. The findings from Spillane (2000) found that the availability of unstructured activities was associated with increased likelihood of marijuana use [ 42 ].
- Protective factor
Strong religious beliefs integrated into society serve as a crucial protective factor that can prevent adolescents from engaging in drug abuse [ 38 , 45 ]. In addition, the school connectedness and adult support also play a major contribution in the drug use [ 40 ].
The goal of this review was to identify and classify the risks and protective factors that lead adolescents to drug abuse across the three important domains of the individual, family, and community. No findings conflicted with each other, as each of them had their own arguments and justifications. The findings from our review showed that individual factors were the most commonly highlighted. These factors include individual traits, significant negative growth exposure, personal psychiatric diagnosis, previous substance and addiction history, and an individual’s attitude and perception as risk factors.
Within the individual factor domain, nine articles were found to contribute to the subdomain of personal/ individual traits [ 27 , 28 , 29 , 37 , 38 , 39 , 40 , 43 , 44 ]. Despite the heterogeneity of the study designs and the substances under investigation, all of the papers found statistically significant results for the possible risk factors of adolescent drug abuse. The traits of high impulsivity, rebelliousness, difficulty in regulating emotions, and alexithymia can be considered negative characteristic traits. These adolescents suffer from the inability to self-regulate their emotions, so they tend to externalize their behaviors as a way to avoid or suppress the negative feelings that they are experiencing [ 41 , 47 , 48 ]. On the other hand, engaging in such behaviors could plausibly provide a greater sense of positive emotions and make them feel good [ 49 ]. Apart from that, evidence from a neurophysiological point of view also suggests that the compulsive drive toward drug use is complemented by deficits in impulse control and decision making (impulsive trait) [ 50 ]. A person’s ability in self-control will seriously impaired with continuous drug use and will lead to the hallmark of addiction [ 51 ].
On the other hand, there are articles that reported some individual traits to be protective for adolescents from engaging in drug abuse. Youth with the optimistic trait, a high level of mindfulness, and social phobia were less likely to become drug dependent [ 31 , 33 , 37 ]. All of these articles used different psychometric instruments to classify each individual trait and were mutually exclusive. Therefore, each trait measured the chance of engaging in drug abuse on its own and did not reflect the chance at the end of the spectrum. These findings show that individual traits can be either protective or risk factors for the drugs used among adolescents. Therefore, any adolescent with negative personality traits should be monitored closely by providing health education, motivation, counselling, and emotional support since it can be concluded that negative personality traits are correlated with high risk behaviours such as drug abuse [ 52 ].
Our study also found that a history of maltreatment has a positive association with adolescent drug abuse. Those adolescents with episodes of maltreatment were considered to have negative growth exposure, as their childhoods were negatively affected by traumatic events. Some significant associations were found between maltreatment and adolescent drug abuse, although the former factor was limited to the female gender [ 25 , 30 , 36 ]. One possible reason for the contrasting results between genders is the different sample populations, which only covered child welfare centers [ 36 ] and foster care [ 30 ]. Regardless of the place, maltreatment can happen anywhere depending on the presence of the perpetrators. To date, evidence that concretely links maltreatment and substance abuse remains limited. However, a plausible explanation for this link could be the indirect effects of posttraumatic stress (i.e., a history of maltreatment) leading to substance use [ 53 , 54 ]. These findings highlight the importance of continuous monitoring and follow-ups with adolescents who have a history of maltreatment and who have ever attended a welfare center.
Addiction sometimes leads to another addiction, as described by the findings of several studies [ 29 , 34 ]. An initial study focused on the effects of e-cigarettes in the development of other substance abuse disorders, particularly those related to marijuana, alcohol, and commonly prescribed medications [ 34 ]. The authors found that the use of e-cigarettes can lead to more severe substance addiction [ 55 ], possibly through normalization of the behavior. On the other hand, Chuang et al.’s extensive study in 2017 analyzed the combined effects of either multiple addictions alone or a combination of multiple addictions together with the impulsivity trait [ 29 ]. The outcomes reported were intriguing and provide the opportunity for targeted intervention. The synergistic effects of impulsiveness and three other substance addictions (marijuana, tobacco, and alcohol) substantially increased the likelihood for drug abuse from 3.46 (95%CI 1.25, 9.58) to 10.13 (95% CI 3.95, 25.95). Therefore, proper rehabilitation is an important strategy to ensure that one addiction will not lead to another addiction.
The likelihood for drug abuse increases as the population perceives little or no harmful risks associated with the drugs. On the opposite side of the coin, a greater perceived risk remains a protective factor for marijuana abuse [ 56 ]. However, another study noted that a stronger determinant for adolescent drug abuse was the perceived availability of the drug [ 35 , 57 ]. Looking at the bigger picture, both perceptions corroborate each other and may inform drug use. Another study, on the other hand, reported that there was a decreasing trend of perceived drug risk in conjunction with the increasing usage of drugs [ 58 ]. As more people do drugs, youth may inevitably perceive those drugs as an acceptable norm without any harmful consequences [ 59 ].
In addition, the total spent for screen time also contribute to drug abuse among adolescent [ 43 ]. This scenario has been proven by many researchers on the effect of screen time on the mental health [ 60 ] that leads to the substance use among the adolescent due to the ubiquity of pro-substance use content on the internet. Adolescent with comorbidity who needs medical pain management by opioids also tend to misuse in future. A qualitative exploration on the perspectives among general practitioners concerning the risk of opioid misuse in people with pain, showed pain management by opioids is a default treatment and misuse is not a main problem for the them [ 61 ]. A careful decision on the use of opioids as a pain management should be consider among the adolescents and their understanding is needed.
Within the family factor domain, family structures were found to have both positive and negative associations with drug abuse among adolescents. As described in one study, paternal knowledge was consistently found to be a protective factor against substance abuse [ 26 ]. With sufficient knowledge, the father can serve as the guardian of his family to monitor and protect his children from negative influences [ 62 ]. The work by Luk et al. also reported a positive association of maternal psychological association towards drug abuse (IRR 2.41, p < 0.05) [ 26 ]. The authors also observed the same effect of paternal psychological control, although it was statistically insignificant. This construct relates to parenting style, and the authors argued that parenting style might have a profound effect on the outcomes under study. While an earlier literature review [ 63 ] also reported such a relationship, a recent study showed a lesser impact [ 64 ] with regards to neglectful parenting styles leading to poorer substance abuse outcomes. Nevertheless, it was highlighted in another study that the adolescents’ perception of a neglectful parenting style increased their odds (OR 2.14, p = 0.012) of developing alcohol abuse, not the parenting style itself [ 65 ]. Altogether, families play vital roles in adolescents’ risk for engaging in substance abuse [ 66 ]. Therefore, any intervention to impede the initiation of substance use or curb existing substance use among adolescents needs to include parents—especially improving parent–child communication and ensuring that parents monitor their children’s activities.
Finally, the community also contributes to drug abuse among adolescents. As shown by Li et al. [ 32 ] and El Kazdouh et al. [ 46 ], peers exert a certain influence on other teenagers by making them subconsciously want to fit into the group. Peer selection and peer socialization processes might explain why peer pressure serves as a risk factor for drug-abuse among adolescents [ 67 ]. Another study reported that strong religious beliefs integrated into society play a crucial role in preventing adolescents from engaging in drug abuse [ 46 ]. Most religions devalue any actions that can cause harmful health effects, such as substance abuse [ 68 ]. Hence, spiritual beliefs may help protect adolescents. This theme has been well established in many studies [ 60 , 69 , 70 , 71 , 72 ] and, therefore, could be implemented by religious societies as part of interventions to curb the issue of adolescent drug abuse. The connection with school and structured activity did reduce the risk as a study in USA found exposure to media anti-drug messages had an indirect negative effect on substances abuse through school-related activity and social activity [ 73 ]. The school activity should highlight on the importance of developmental perspective when designing and offering school-based prevention programs [75].
Limitations
We adopted a review approach that synthesized existing evidence on the risk and protective factors of adolescents engaging in drug abuse. Although this systematic review builds on the conclusion of a rigorous review of studies in different settings, there are some potential limitations to this work. We may have missed some other important factors, as we only included English articles, and article extraction was only done from the three search engines mentioned. Nonetheless, this review focused on worldwide drug abuse studies, rather than the broader context of substance abuse including alcohol and cigarettes, thereby making this paper more focused.
Conclusions
This review has addressed some recent knowledge related to the individual, familial, and community risk and preventive factors for adolescent drug use. We suggest that more attention should be given to individual factors since most findings were discussed in relation to such factors. With the increasing trend of drug abuse, it will be critical to focus research specifically on this area. Localized studies, especially those related to demographic factors, may be more effective in generating results that are specific to particular areas and thus may be more useful in generating and assessing local control and prevention efforts. Interventions using different theory-based psychotherapies and a recognition of the unique developmental milestones specific to adolescents are among examples that can be used. Relevant holistic approaches should be strengthened not only by relevant government agencies but also by the private sector and non-governmental organizations by promoting protective factors while reducing risk factors in programs involving adolescents from primary school up to adulthood to prevent and control drug abuse. Finally, legal legislation and enforcement against drug abuse should be engaged with regularly as part of our commitment to combat this public health burden.
Data availability and materials
All data generated or analysed during this study are included in this published article.
Nation, U. World Drug Report 2018 (United Nations publication, Sales No. E.18X.XI.9. United Nation publication). 2018. Retrieved from https://www.unodc.org/wdr2018
Google Scholar
Degenhardt L, Stockings E, Patton G, Hall WD, Lynskey M. The increasing global health priority of substance use in young people. Lancet Psychiatry. 2016;3(3):251–64. https://doi.org/10.1016/S2215-0366(15)00508-8 Elsevier Ltd.
Article PubMed Google Scholar
Ritchie H, Roser M. Drug Use - Our World in Data: Global Change Data Lab; 2019. https://ourworldindata.org/drug-use [10 June 2020]
Holm S, Sandberg S, Kolind T, Hesse M. The importance of cannabis culture in young adult cannabis use. J Subst Abus. 2014;19(3):251–6.
Luikinga SJ, Kim JH, Perry CJ. Developmental perspectives on methamphetamine abuse: exploring adolescent vulnerabilities on brain and behavior. Progress Neuro Psychopharmacol Biol Psychiatry. 2018;87(Pt A):78–84. https://doi.org/10.1016/j.pnpbp.2017.11.010 Elsevier Inc.
Article CAS Google Scholar
Ismail R, Ghazalli MN, Ibrahim N. Not all developmental assets can predict negative mental health outcomes of disadvantaged youth: a case of suburban Kuala Lumpur. Mediterr J Soc Sci. 2015;6(1):452–9. https://doi.org/10.5901/mjss.2015.v6n5s1p452 .
Article Google Scholar
Crews F, He J, Hodge C. Adolescent cortical development: a critical period of vulnerability for addiction. Pharmacol Biochem Behav. 2007;86(2):189–99. https://doi.org/10.1016/j.pbb.2006.12.001 .
Article CAS PubMed Google Scholar
Schulte MT, Hser YI. Substance use and associated health conditions throughout the lifespan. Public Health Rev. 2013;35(2). https://doi.org/10.1007/bf03391702 Technosdar Ltd.
Somani, S.; Meghani S. Substance Abuse among Youth: A Harsh Reality 2016. doi: https://doi.org/10.4172/2165-7548.1000330 , 6, 4.
Book Google Scholar
Drabble L, Trocki KF, Klinger JL. Religiosity as a protective factor for hazardous drinking and drug use among sexual minority and heterosexual women: findings from the National Alcohol Survey. Drug Alcohol Depend. 2016;161:127–34. https://doi.org/10.1016/j.drugalcdep.2016.01.022 .
Article PubMed PubMed Central Google Scholar
Goliath V, Pretorius B. Peer risk and protective factors in adolescence: Implications for drug use prevention. Soc Work. 2016;52(1):113–29. https://doi.org/10.15270/52-1-482 .
Guerrero LR, Dudovitz R, Chung PJ, Dosanjh KK, Wong MD. Grit: a potential protective factor against substance use and other risk behaviors among Latino adolescents. Acad Pediatr. 2016;16(3):275–81. https://doi.org/10.1016/j.acap.2015.12.016 .
National Institutes on Drug Abuse. What are risk factors and protective factors? National Institute on Drug Abuse (NIDA); 2003. Retrieved from https://www.drugabuse.gov/publications/preventing-drug-use-among-children-adolescents/chapter-1-risk-factors-protective-factors/what-are-risk-factors
Nguyen NN, Newhill CE. The role of religiosity as a protective factor against marijuana use among African American, White, Asian, and Hispanic adolescents. J Subst Abus. 2016;21(5):547–52. https://doi.org/10.3109/14659891.2015.1093558 .
Schinke S, Schwinn T, Hopkins J, Wahlstrom L. Drug abuse risk and protective factors among Hispanic adolescents. Prev Med Rep. 2016;3:185–8. https://doi.org/10.1016/j.pmedr.2016.01.012 .
Macleod J, Oakes R, Copello A, Crome PI, Egger PM, Hickman M, et al. Psychological and social sequelae of cannabis and other illicit drug use by young people: a systematic review of longitudinal, general population studies. Lancet. 2004;363(9421):1579–88. https://doi.org/10.1016/S0140-6736(04)16200-4 .
Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–28. https://doi.org/10.1016/S0140-6736(07)61162-3 .
Semple DM, McIntosh AM, Lawrie SM. Cannabis as a risk factor for psychosis: systematic review. J Psychopharmacol. 2005;19(2):187–94. https://doi.org/10.1177/0269881105049040 .
Nargiso JE, Ballard EL, Skeer MR. A systematic review of risk and protective factors associated with nonmedical use of prescription drugs among youth in the united states: A social ecological perspective. J Stud Alcohol Drugs. 2015;76(1):5–20. https://doi.org/10.15288/jsad.2015.76.5 .
Guxensa M, Nebot M, Ariza C, Ochoa D. Factors associated with the onset of cannabis use: a systematic review of cohort studies. Gac Sanit. 2007;21(3):252–60. https://doi.org/10.1157/13106811 .
Susan MS, Peter SA, Dakshitha W, George CP. The age of adolescence. Lancet Child Adolesc Health. 2018;2(Issue 3):223–8. https://doi.org/10.1016/S2352-4642(18)30022-1 .
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–91. https://doi.org/10.3233/EFI-180221 .
McHugh ML. Interrater reliability: The kappa statistic. Biochem Med. 2012;22(3):276–82. https://doi.org/10.11613/bm.2012.031 .
Cecil CAM, Walton E, Smith RG, Viding E, McCrory EJ, Relton CL, et al. DNA methylation and substance-use risk: a prospective, genome-wide study spanning gestation to adolescence. Transl Psychiatry. 2016;6(12):e976. https://doi.org/10.1038/tp.2016.247 Nature Publishing Group.
Article CAS PubMed PubMed Central Google Scholar
Kobulsky JM. Gender differences in pathways from physical and sexual abuse to early substance use. Child Youth Serv Rev. 2017;83:25–32. https://doi.org/10.1016/j.childyouth.2017.10.027 .
Luk JW, King KM, McCarty CA, McCauley E, Stoep A. Prospective effects of parenting on substance use and problems across Asian/Pacific islander and European American youth: Tests of moderated mediation. J Stud Alcohol Drugs. 2017;78(4):521–30. https://doi.org/10.15288/jsad.2017.78.521 .
Guttmannova K, Skinner ML, Oesterle S, White HR, Catalano RF, Hawkins JD. The interplay between marijuana-specific risk factors and marijuana use over the course of adolescence. Prev Sci. 2019;20(2):235–45. https://doi.org/10.1007/s11121-018-0882-9 .
Dorard G, Bungener C, Phan O, Edel Y, Corcos M, Berthoz S. Is alexithymia related to cannabis use disorder? Results from a case-control study in outpatient adolescent cannabis abusers. J Psychosom Res. 2017;95:74–80. https://doi.org/10.1016/j.jpsychores.2017.02.012 .
Chuang CWI, Sussman S, Stone MD, Pang RD, Chou CP, Leventhal AM, et al. Impulsivity and history of behavioral addictions are associated with drug use in adolescents. Addict Behav. 2017;74:41–7. https://doi.org/10.1016/j.addbeh.2017.05.021 .
Gabrielli J, Jackson Y, Brown S. Associations between maltreatment history and severity of substance use behavior in youth in Foster Care. Child Maltreat. 2016;21(4):298–307. https://doi.org/10.1177/1077559516669443 .
Khoddam R, Jackson NJ, Leventhal AM. Internalizing symptoms and conduct problems: redundant, incremental, or interactive risk factors for adolescent substance use during the first year of high school? Drug Alcohol Depend. 2016;169:48–55. https://doi.org/10.1016/j.drugalcdep.2016.10.007 .
Li SD, Zhang X, Tang W, Xia Y. Predictors and implications of synthetic drug use among adolescents in the gambling Capital of China. SAGE Open. 2017;7(4):215824401773303. https://doi.org/10.1177/2158244017733031 .
Marin S, Heshmatian E, Nadrian H, Fakhari A, Mohammadpoorasl A. Associations between optimism, tobacco smoking and substance abuse among Iranian high school students. Health Promot Perspect. 2019;9(4):279–84. https://doi.org/10.15171/hpp.2019.38 .
Miech RA, O’Malley PM, Johnston LD, Patrick ME. E-cigarettes and the drug use patterns of adolescents. Nicotine Tob Res. 2015;18(5):654–9. https://doi.org/10.1093/ntr/ntv217 .
Schleimer JP, Rivera-Aguirre AE, Castillo-Carniglia A, Laqueur HS, Rudolph KE, Suárez H, et al. Investigating how perceived risk and availability of marijuana relate to marijuana use among adolescents in Argentina, Chile, and Uruguay over time. Drug Alcohol Depend. 2019;201:115–26. https://doi.org/10.1016/j.drugalcdep.2019.03.029 .
Traube DE, Yarnell LM, Schrager SM. Differences in polysubstance use among youth in the child welfare system: toward a better understanding of the highest-risk teens. Child Abuse Negl. 2016;52:146–57. https://doi.org/10.1016/j.chiabu.2015.11.020 .
Wilson JD, Vo H, Matson P, Adger H, Barnett G, Fishman M. Trait mindfulness and progression to injection use in youth with opioid addiction. Subst Use Misuse. 2017;52(11):1486–93. https://doi.org/10.1080/10826084.2017.1289225 .
Dash GF, Feldstein Ewing SW, Murphy C, Hudson KA, Wilson AC. Contextual risk among adolescents receiving opioid prescriptions for acute pain in pediatric ambulatory care settings. Addict Behav. 2020;104:106314. https://doi.org/10.1016/j.addbeh.2020.106314 Epub 2020 Jan 11. PMID: 31962289; PMCID: PMC7024039.
Osborne V, Serdarevic M, Striley CW, Nixon SJ, Winterstein AG, Cottler LB. Age of first use of prescription opioids and prescription opioid non-medical use among older adolescents. Substance Use Misuse. 2020;55(14):2420–7. https://doi.org/10.1080/10826084.2020.1823420 .
Zuckermann AME, Qian W, Battista K, Jiang Y, de Groh M, Leatherdale ST. Factors influencing the non-medical use of prescription opioids among youth: results from the COMPASS study. J Subst Abus. 2020;25(5):507–14. https://doi.org/10.1080/14659891.2020.1736669 .
De Pedro KT, Esqueda MC, Gilreath TD. School protective factors and substance use among lesbian, gay, and bisexual adolescents in California public schools. LGBT Health. 2017;4(3):210–6. https://doi.org/10.1089/lgbt.2016.0132 .
Spillane NS, Schick MR, Kirk-Provencher KT, Hill DC, Wyatt J, Jackson KM. Structured and unstructured activities and alcohol and marijuana use in middle school: the role of availability and engagement. Substance Use Misuse. 2020;55(11):1765–73. https://doi.org/10.1080/10826084.2020.1762652 .
Ogunsola OO, Fatusi AO. Risk and protective factors for adolescent substance use: a comparative study of secondary school students in rural and urban areas of Osun state, Nigeria. Int J Adolesc Med Health. 2016;29(3). https://doi.org/10.1515/ijamh-2015-0096 .
Doggett A, Qian W, Godin K, De Groh M, Leatherdale ST. Examining the association between exposure to various screen time sedentary behaviours and cannabis use among youth in the COMPASS study. SSM Population Health. 2019;9:100487. https://doi.org/10.1016/j.ssmph.2019.100487 .
Afifi RA, El Asmar K, Bteddini D, Assi M, Yassin N, Bitar S, et al. Bullying victimization and use of substances in high school: does religiosity moderate the association? J Relig Health. 2020;59(1):334–50. https://doi.org/10.1007/s10943-019-00789-8 .
El Kazdouh H, El-Ammari A, Bouftini S, El Fakir S, El Achhab Y. Adolescents, parents and teachers’ perceptions of risk and protective factors of substance use in Moroccan adolescents: a qualitative study. Substance Abuse Treat Prevent Policy. 2018;13(1):–31. https://doi.org/10.1186/s13011-018-0169-y .
Sussman S, Lisha N, Griffiths M. Prevalence of the addictions: a problem of the majority or the minority? Eval Health Prof. 2011;34(1):3–56. https://doi.org/10.1177/0163278710380124 .
Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30(2):217–37. https://doi.org/10.1016/j.cpr.2009.11.004 .
Ricketts T, Macaskill A. Gambling as emotion management: developing a grounded theory of problem gambling. Addict Res Theory. 2003;11(6):383–400. https://doi.org/10.1080/1606635031000062074 .
Williams AD, Grisham JR. Impulsivity, emotion regulation, and mindful attentional focus in compulsive buying. Cogn Ther Res. 2012;36(5):451–7. https://doi.org/10.1007/s10608-011-9384-9 .
National Institutes on Drug Abuse. Drugs, brains, and behavior the science of addiction national institute on drug abuse (nida). 2014. Retrieved from https://www.drugabuse.gov/sites/default/files/soa_2014.pdf
Hokm Abadi ME, Bakhti M, Nazemi M, Sedighi S, Mirzadeh Toroghi E. The relationship between personality traits and drug type among substance abuse. J Res Health. 2018;8(6):531–40.
Longman-Mills S, Haye W, Hamilton H, Brands B, Wright MGM, Cumsille F, et al. Psychological maltreatment and its relationship with substance abuse among university students in Kingston, Jamaica, vol. 24. Florianopolis: Texto Contexto Enferm; 2015. p. 63–8.
Rosenkranz SE, Muller RT, Henderson JL. The role of complex PTSD in mediating childhood maltreatment and substance abuse severity among youth seeking substance abuse treatment. Psychol Trauma Theory Res Pract Policy. 2014;6(1):25–33. https://doi.org/10.1037/a0031920 .
Krishnan-Sarin S, Morean M, Kong G, et al. E-Cigarettes and “dripping” among high-school youth. Pediatrics. 2017;139(3). https://doi.org/10.1542/peds.2016-3224 .
Adinoff B. Neurobiologic processes in drug reward and addiction. Harvard review of psychiatry. NIH Public Access. 2004;12(6):305–20. https://doi.org/10.1080/10673220490910844 .
Kandel D, Kandel E. The gateway hypothesis of substance abuse: developmental, biological and societal perspectives. Acta Paediatrica. 2014;104(2):130–7.
Dempsey RC, McAlaney J, Helmer SM, Pischke CR, Akvardar Y, Bewick BM, et al. Normative perceptions of Cannabis use among European University students: associations of perceived peer use and peer attitudes with personal use and attitudes. J Stud Alcohol Drugs. 2016;77(5):740–8.
Cioffredi L, Kamon J, Turner W. Effects of depression, anxiety and screen use on adolescent substance use. Prevent Med Rep. 2021;22:101362. https://doi.org/10.1016/j.pmedr.2021.101362 .
Luckett T, NewtonJohn T, Phillips J, et al. Risk of opioid misuse in people with cancer and pain and related clinical considerations:a qualitative study of the perspectives of Australian general practitioners. BMJ Open. 2020;10(2):e034363. https://doi.org/10.1136/bmjopen-2019-034363 .
Lipari RN. Trends in Adolescent Substance Use and Perception of Risk from Substance Use. The CBHSQ Report. Substance Abuse Mental Health Serv Admin. 2013; Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/27656743 .
Muchiri BW, dos Santos MML. Family management risk and protective factors for adolescent substance use in South Africa. Substance Abuse. 2018;13(1):24. https://doi.org/10.1186/s13011-018-0163-4 .
Becoña E, Martínez Ú, Calafat A, Juan M, Fernández-Hermida JR, Secades-Villa R. Parental styles and drug use: a review. In: Drugs: Education, Prevention and Policy: Taylor & Francis; 2012. https://doi.org/10.3109/09687637.2011.631060 .
Berge J, Sundel K, Ojehagen A, Hakansson A. Role of parenting styles in adolescent substance use: results from a Swedish longitudinal cohort study. BMJ Open. 2016;6(1):e008979. https://doi.org/10.1136/bmjopen-2015-008979 .
Opara I, Lardier DT, Reid RJ, Garcia-Reid P. “It all starts with the parents”: a qualitative study on protective factors for drug-use prevention among black and Hispanic girls. Affilia J Women Soc Work. 2019;34(2):199–218. https://doi.org/10.1177/0886109918822543 .
Martínez-Loredo V, Fernández-Artamendi S, Weidberg S, Pericot I, López-Núñez C, Fernández-Hermida J, et al. Parenting styles and alcohol use among adolescents: a longitudinal study. Eur J Invest Health Psychol Educ. 2016;6(1):27–36. https://doi.org/10.1989/ejihpe.v6i1.146 .
Baharudin MN, Mohamad M, Karim F. Drug-abuse inmates maqasid shariah quality of lifw: a conceotual paper. Hum Soc Sci Rev. 2020;8(3):1285–94. https://doi.org/10.18510/hssr.2020.83131 .
Henneberger AK, Mushonga DR, Preston AM. Peer influence and adolescent substance use: a systematic review of dynamic social network research. Adolesc Res Rev. 2020;6(1):57–73. https://doi.org/10.1007/s40894-019-00130-0 Springer.
Gomes FC, de Andrade AG, Izbicki R, Almeida AM, de Oliveira LG. Religion as a protective factor against drug use among Brazilian university students: a national survey. Rev Bras Psiquiatr. 2013;35(1):29–37. https://doi.org/10.1016/j.rbp.2012.05.010 .
Kulis S, Hodge DR, Ayers SL, Brown EF, Marsiglia FF. Spirituality and religion: intertwined protective factors for substance use among urban American Indian youth. Am J Drug Alcohol Abuse. 2012;38(5):444–9. https://doi.org/10.3109/00952990.2012.670338 .
Miller L, Davies M, Greenwald S. Religiosity and substance use and abuse among adolescents in the national comorbidity survey. J Am Acad Child Adolesc Psychiatry. 2000;39(9):1190–7. https://doi.org/10.1097/00004583-200009000-00020 .
Moon SS, Rao U. Social activity, school-related activity, and anti-substance use media messages on adolescent tobacco and alcohol use. J Hum Behav Soc Environ. 2011;21(5):475–89. https://doi.org/10.1080/10911359.2011.566456 .
Simone A. Onrust, Roy Otten, Jeroen Lammers, Filip smit, school-based programmes to reduce and prevent substance use in different age groups: what works for whom? Systematic review and meta-regression analysis. Clin Psychol Rev. 2016;44:45–59. https://doi.org/10.1016/j.cpr.2015.11.002 .
Download references
Acknowledgements
The authors acknowledge The Ministry of Higher Education Malaysia and The Universiti Kebangsaan Malaysia, (UKM) for funding this study under the Long-Term Research Grant Scheme-(LGRS/1/2019/UKM-UKM/2/1). We also thank the team for their commitment and tireless efforts in ensuring that manuscript was well executed.
Financial support for this study was obtained from the Ministry of Higher Education, Malaysia through the Long-Term Research Grant Scheme-(LGRS/1/2019/UKM-UKM/2/1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Community Health, Universiti Kebangsaan Malaysia, Cheras, 56000, Kuala Lumpur, Malaysia
Azmawati Mohammed Nawi, Mohd Rohaizat Hassan & Mohd Rizal Abdul Manaf
Centre for Research in Psychology and Human Well-Being (PSiTra), Faculty of Social Sciences and Humanities, Universiti Kebangsaan Malaysia, 43600, Bangi, Selangor, Malaysia
Rozmi Ismail, Fauziah Ibrahim & Nurul Shafini Shafurdin
Clinical Psychology and Behavioural Health Program, Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Noh Amit & Norhayati Ibrahim
You can also search for this author in PubMed Google Scholar
Contributions
Manuscript concept, and drafting AMN and RI; model development, FI, NI and NA.; Editing manuscript MRH, MRAN, NSS,; Critical revision of manuscript for important intellectual content, all authors. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Rozmi Ismail .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of the Secretariat of Research Ethics, Universiti Kebangsaan Malaysia, Faculty of Medicine, Cheras, Kuala Lumpur (Reference no. UKMPPI/111/8/JEP-2020.174(2). Dated 27 Mac 2020.
Consent for publication
Not applicable.
Competing interests
The authors AMN, RI, FI, MRM, MRAM, NA, NI NSS declare that they have no conflict of interest relevant to this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nawi, A.M., Ismail, R., Ibrahim, F. et al. Risk and protective factors of drug abuse among adolescents: a systematic review. BMC Public Health 21 , 2088 (2021). https://doi.org/10.1186/s12889-021-11906-2
Download citation
Received : 10 June 2021
Accepted : 22 September 2021
Published : 13 November 2021
DOI : https://doi.org/10.1186/s12889-021-11906-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Drug abuse, substance, adolescent
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Treating Drug Abuse and Addiction in the Criminal Justice System: Improving Public Health and Safety
Redonna k. chandler.
1 Services Research Branch, National Institute on Drug Abuse, Bethesda, Maryland
Bennett W. Fletcher
Nora d. volkow.
2 National Institute on Drug Abuse, Bethesda, Maryland
Despite increasing evidence that addiction is a treatable disease of the brain, most individuals do not receive treatment. Involvement in the criminal justice system often results from illegal drug-seeking behavior and participation in illegal activities that reflect, in part, disrupted behavior ensuing from brain changes triggered by repeated drug use. Treating drug-involved offenders provides a unique opportunity to decrease substance abuse and reduce associated criminal behavior. Emerging neuroscience has the potential to transform traditional sanction-oriented public safety approaches by providing new therapeutic strategies against addiction that could be used in the criminal justice system. We summarize relevant neuroscientific findings and evidence-based principles of addiction treatment that, if implemented in the criminal justice system, could help improve public heath and reduce criminal behavior.
The past 20 years have seen significant increases in the numbers of individuals incarcerated or under other forms of criminal justice supervision in the United States. These numbers are staggering—approximately 7.1 million adults in the United States are under some form of criminal justice supervision. 1 The large increase in the criminal justice population reflects in part tougher laws and penalties for drug offenses. 2 An estimated one-half of all prisoners (including some sentenced for other than drug offenses) meet the criteria for diagnosis of drug abuse or dependence ( Table 1 ). 3 , 4
Inmate Drug Use, Abuse/Dependence, and Treatment
| No. (%) | ||||
|---|---|---|---|---|
| Drug Use | Drug Abuse or Dependence | |||
| Inmate Type | At Time of Offense | In Month Prior to Offense | Met Criteria | Received Treatment While Incarcerated |
| Local jail inmates , | 128 030 (29) | 242 720 (55) | 245 830 (55) | 16 520 (7) |
| State inmates | 393 610 (32) | 686 670 (56) | 642 500 (53) | 95 090 (15) |
| Federal inmates | 34 140 (26) | 64 910 (50) | 57 200 (46) | 9950 (17) |
During the past 20 years, fundamental advances in the neurobiology of addiction have been made. Molecular and imaging studies have revealed addiction as a brain disorder with a strong genetic component, and this has galvanized research on new pharmacological treatments. However, a large disconnect remains between addiction research and the treatment of addiction in general, particularly within the criminal justice system. This is evidenced in that most prisoners (80%–85%) who could benefit from drug abuse treatment do not receive it. 3 , 4 In addition, drug-using offenders are at high risk for infectious diseases such as human immunodeficiency virus (HIV) and hepatitis C 5 and frequently have co-morbid psychiatric disorders, 6 , 7 which further highlights the dire treatment needs of this population.
Not treating a drug-abusing offender is a missed opportunity to simultaneously improve both public health and safety. Integrating treatment into the criminal justice system would provide treatment to individuals who otherwise would not receive it, improving their medical outcomes and decreasing their rates of reincarceration. 8
Recidivism in the Drug-Abusing Offender
The inadequacy of incarceration by itself in addressing drug abuse or addiction is evident in the statistics. A review of recidivism in 15 states found that one-quarter of individuals released returned to prison within 3 years for technical violations that included, among other things, testing positive for drug use. 9 Illicit drugs are used in jails and prisons despite their highly structured, controlled environments, 10 but even enforced abstinence can mislead criminal justice professionals as well as addicted persons to underestimate the vulnerability to relapse postincarceration. On release from prison or jail, addicted persons will experience challenges to their sobriety through multiple stressors that increase their risk of relapsing to drug use. These include the stigma associated with being labeled an ex-offender, the need for housing and legitimate employment, stresses in re-unifying with family, and multiple requirements for criminal justice supervision. 11 , 12
Returning to neighborhoods associated with preincarceration drug use places the addicted individual in an environment rich in drug cues. As discussed below, these conditioned cues automatically activate the reward/motivational neurocircuitry and can trigger an intense desire to consume drugs (craving). 13 The molecular and neurobiological adaptations resulting from chronic drug use persist for months after drug discontinuation, 14 and evidence exists that compulsive seeking of drugs when addicted individuals are reexposed to drug cues progressively increases after drug withdrawal. 15 This could explain why many drug-addicted individuals rapidly return to drug use following long periods of abstinence during incarceration and highlights the need for ongoing treatment following release.
Drug Abuse Treatment Effectiveness in the Criminal Justice System
Research over the last 2 decades has consistently reported the beneficial effects of treatment for the drug abuser in the criminal justice system. 16 , 17 These interventions include therapeutic alternatives to incarceration, treatment merged with judicial oversight in drug courts, prison- and jail-based treatments, and reentry programs intended to help offenders transition from incarceration back into the community. 8 , 18 Through monitoring, supervision, and threat of legal sanctions, the justice system can provide leverage to encourage drug abusers to enter and remain in treatment.
Behavioral treatments are the most commonly used interventions for addressing substance use disorders. Evidence-based behavioral interventions include cognitive therapies that teach coping and decision-making skills, contingency management therapies that reinforce behavioral changes associated with abstinence, and motivational therapies that enhance the motivation to participate in treatment and in non–drug-related activities. 19 , 20 Many residential treatment programs rely on the creation of a “therapeutic community” based on a social learning model. 21 Medications such as methadone, buprenorphine, and naltrexone are beneficial for the treatment of heroin addiction and naltrexone and topiramate for the treatment of alcoholism. 22 – 24 Self-help programs such as Alcoholics Anonymous or SMART Recovery can be valuable adjuncts to formal drug treatment. 25
Research has consistently shown that community-based drug abuse treatment can reduce drug use and drug-related criminal behavior. 26 A meta-analysis of 78 comparison-group community-based drug treatment studies found treatment to be up to 1.8 times better in reducing drug use than the usual alternatives. 20 In a meta-analysis of 66 incarceration-based treatment evaluations, therapeutic community and counseling approaches were respectively 1.4 and 1.5 times more likely to reduce reoffending. 27 Drug courts combine judicial supervision with drug treatment as an alternative to incarceration; their graduates have rearrest rates about half those of matched comparison samples and much lower than those of drug court dropouts. 28 Individuals who participated in prison-based treatment followed by a community-based program postincarceration were 7 times more likely to be drug free and 3 times less likely to be arrested for criminal behavior than those not receiving treatment. 29 , 30
The benefits of medications for drug treatment were shown in a recent randomized trial in which heroin-dependent inmates began methadone treatment in prison prior to release and continued in the community postrelease. At 1-, 3-, and 6-month follow-up, patients who received methadone plus counseling were significantly less likely to use heroin or engage in criminal activity than those who received only counseling. 31 – 33 The potential exists for immediate adoption of methadone maintenance for incarcerated persons with opioid addictions, but most prison systems have not been receptive to this approach. 34
Economic analyses highlight the cost-effectiveness of treating drug-involved offenders. 35 On average, in- carceration in the United States costs approximately $22 000 per month, 36 and there is little evidence that this strategy reduces drug use or drug-related re-incarceration rates for nonviolent drug offenders. By contrast, the average cost of methadone is $4000 per month, 37 and treatment with methadone has demonstrated effectiveness in reducing drug use and criminal activity following release. 31 Alternatives to incarceration can also defray job productivity losses and the separation from family and social support systems.
The cost of integrating volunteer-led self-help organizations such as Alcoholics Anonymous and Narcotics Anonymous into criminal justice settings is nominal and could provide support to the recovery efforts of addicted persons in the criminal justice system. One dollar spent on drug courts is estimated to save approximately $4 in avoided costs of incarceration and health care, 38 and prison-based treatment saves between $2 to $6. 39 These economic benefits in part reflect reductions in criminal behavior. 40 , 41
Access to Treatment
Drug education—not drug treatment—is the most common service provided to prisoners with drug abuse or addiction problems. 4 , 42 More than one-quarter of state inmates and 1 in 5 federal inmates meeting abuse/dependence criteria participate in self-help groups such as Alcoholics Anonymous while in prison. 4 However, though treatment during and after incarceration has been shown to significantly reduce drug use and drug-related crime, less than 20% of inmates with drug abuse or dependence receive formal treatment ( Table 1 ). 3 , 4
In a recent survey of correctional programs and organizations across the United States, 42 most correctional agencies reported providing sometype of drug abuse treatment services;however, the median percentage of offenders who had access to those services at any given time was low, usually less than 10% ( Table 2 ). 42 Even if a correctional institution does provide treatment, the continuity of treatment postincarceration, which is essential to recovery, 16 is often lacking when the drug-involved offender transitions from incarceration to community supervision. 43 Failure to receive treatment on release increases the risk not only of relapse but also of mortality from drug overdose and other causes. 44
Access to Health, Mental Health, and Substance Abuse Treatment Services in Correctional Facilities a
| Prisons(n = 98) | Jails (n = 57) | Community Corrections (n = 134) | ||||
|---|---|---|---|---|---|---|
| Service Type | Offer Services, % | Access to Services, Median % | Offer Services, % | Access to Services, Median % | Offer Services, % | Access to Services, Median % |
| Physical/mental health services | ||||||
| HIV testing | 89.1 | 68.7 | 73.4 | 22.0 | 42.0 | 12.1 |
| HIV/AIDS counseling | 80.5 | 50.1 | 80.3 | 27.6 | 45.2 | 12.9 |
| Hepatitis C testing | 98.2 | 79.6 | 74.1 | 23.3 | 39.0 | 11.5 |
| Mental health assessment | 99.8 | 86.5 | 94.6 | 39.8 | 63.6 | 19.7 |
| Mental health counseling | 96.3 | 58.9 | 94.5 | 31.1 | 63.9 | 18.6 |
| Pharmacological treatment | ||||||
| Methadone | 8.9 | 31.0 | 54.5 | 1.7 | 1.7 | 31.0 |
| Other medications for substance use disorder | 12.4 | NA | 36.8 | NA | 2.4 | NA |
| Medication for mental illness | 80.3 | NA | 85.4 | NA | 7.8 | NA |
| Substance abuse services | ||||||
| Detoxification | 12.2 | 31.0 | 26.0 | 1.5 | 3.2 | 31.0 |
| Alcohol/drug education | 74.1 | 8.3 | 61.3 | 4.5 | 53.1 | 8.8 |
| Outpatient counseling | ||||||
| ≤4 h/wk | 54.6 | 3.4 | 59.8 | 7.4 | 47.1 | 10.0 |
| ≥5 h/wk | 47.1 | 2.7 | 22.5 | 10.8 | 21.6 | 8.8 |
| Therapeutic community | 26.9 | 6.6 | 26.3 | 3.0 | 5.7 | 11.1 |
Abbreviations: HIV, human immunodeficiency virus; NA, not applicable.
Infectious diseases such as HIV and hepatitis C are associated with illicit drug use and occur at higher rates in correctional populations than in the general population, 5 but treatment for these conditions appears to fall short of need. 45 , 46 It is feasible to implement screening and treatment in correctional settings for HIV 47 , 48 and hepatitis C. 49 , 50 Continuity of treatment for released offenders with infectious disease is crucial not only for the individual’s health 51 , 52 but also for the health of the community. 45 , 53
There are many barriers to treatment for the drug-involved offender, including lack of the resources, infrastructure, and treatment staff (including physicians knowledgeable about addiction medicine) required to meet the drug treatment needs of individuals under their supervision. Addiction remains a stigmatized disease not often regarded by the criminal justice system as a medical condition; as a consequence, treatment is not constitutionally guaranteed as is the treatment of other medical conditions.
Neurobiology of Addiction
Addiction is a chronic brain disease for which genetic factors are believed to contribute 40% to 60% of the vulnerability. 54 Repeated drug exposure in individuals who are vulnerable (because of genetics, or developmental or environmental factors) trigger neuroadaptations in the brain that result in the compulsive drug use and loss of control over drug-related behaviors that characterizes addiction. Molecular and neuroimaging studies have helped illuminate how genes may affect vulnerability to addiction and how repeated use of addictive drugs causes long-lasting disruptions to the structure and function of the brain. 55 Among the genes identified to contribute to the vulnerability for addiction are those that participate in the neuroplastic changes associated with learning. 56 Imaging studies have identified multiple brain circuits that are disrupted in addicted persons 57 ; these include circuits involved in reward and motivation, learning and memory, cognitive control, mood, and interoception (awareness of physiological body signals) ( Figure ). Disruption of these circuits impairs the addicted person’s ability to inhibit intentional actions or to control strong emotions and desires and also increases the likelihood that the individual will have difficulties making adaptive decisions. 60 , 61

Circuits work together and change with experience. Each is linked to an important concept: reward (saliency), motivation (drive), memory (learning associations), inhibitory control (conflict resolution), mood (well-being), 58 and interoception (internal awareness). 59 Size of circuit ovals indicates influence in determining behavioral outcomes. Thicker line weights indicate greater influence on regulation of the circuit. A, In a nonaddicted person the decision to consume a drug (same process pertains for natural rewards) is a function of the balance between the expected pleasure (based on past experience or memory), alternative stimuli (this includes internal states such as mood and interoception but also alternative external rewards), and potential negative outcomes that oppose the motivation to take the drug (inhibitory control exerted by prefrontal cortex) and stop the drug use. B, During addiction, the enhanced value of the drug in the reward, motivation, and memory circuits overcomes the inhibitory control exerted by the prefrontal cortex, thereby favoring a positive feedback loop initiated by the consumption of the drug and perpetuated by enhanced activation of the motivation/drive and memory circuits. Decreased sensitivity to rewards also raises the hedonic threshold, disrupting mood and increasing the saliency values of drugs and behaviors temporarily associated with relief from the dysphoria. Learning and conditioning result in an enhanced interoceptive awareness of discomfort and the associated desire for the drug (craving). Absence of lines from inhibitory control circuit to reward and motivation circuits indicates loss of regulation.
Addiction also decreases sensitivity in the reward and the motivational circuits, which modulate response to positive as well as negative reinforcers. Practically, this suggests that an addicted individual may experience less motivation to pursue activities likely to result in beneficial outcomes and to avoid those that could result in punishment. One can also predict that dysfunction in this neurocircuitry would reduce an addicted person’s motivation to abstain from drug use because alternative reinforcers (natural stimuli) are comparatively weaker and negative consequences (eg, incarceration) are less salient. 62
In parallel, the repeated use of drugs leads to the formation of new linked memories that condition the addicted individual to expect pleasurable responses—not only when exposed to a drug but also when exposed to stimuli associated with the drug. These stimuli trigger automatic responses that frequently drive relapse, even in individuals motivated to stop taking drugs. 63 The enhanced sensitivity to drugs as rewards and the conditioning to associated drug cues increase the interoceptive awareness of discomfort (anxiety and tension) that occurs when the individual is exposed to drug cues and increase the desire to consume the drug. 64 Additionally, repeated drug use also affects brain regions implicated in mood and anxiety, which could explain the high rate of addiction comorbid with dysphoria, depression, or both and the vulnerability of the addicted person to relapse when exposed to social stressors. 65 , 66
Impairment of the neural substrates affected by addiction—particularly those concerned with behavioral inhibition, control of emotions and desires, and decision-making—increase the likelihood that addicted individuals will make choices that appear impulsive. 67 , 68 This idea is supported by research in the emerging area of behavioral economics, which has found that addicted individuals differ from those who do not use drugs in how they make decisions. Addicted individuals tend to have higher levels of temporal discounting than those who do not use drugs; ie, they tend to choose immediate, smaller rewards over future, larger rewards. 69 High temporal discounting is also associated with impulsivity—the inability to delay immediate gratification and to recognize the potential for negative consequences. 70
Many of the neurobiological changes associated with repeated drug use persist for long periods after drug discontinuation. 71 This helps explain why addicted individuals who have ceased drug use are at high risk of relapse and provides neurobiological support for the recognition of addiction as a chronic relapsing disease. 72
What are the implications of neuroscience research for how society and clinicians might regard the addicted offender? There are at least 3 implications for how this emerging knowledge about the neurologic basis of addictive behavior is important.
First, of most importance, neuroscience’s uncovering of new molecular targets implicated in the responses to drugs and of new knowledge on the function of the human brain provides new targets for medication development and behavioral interventions in addiction. Although many of the neurobiological changes associated with repeated drug use persist for long periods after drug discontinuation, 71 research suggests that the impaired brain can regain some of the functions damaged by use of illicit drugs over time. 73
Second, neuroscience establishes a biological framework for understanding aspects of addictive behavior that otherwise seem to defy rational explanation. In the absence of known biological determinants, these behaviors often have been attributed to “moral weakness.” 74 Identifying the neurologic factors underlying addictive behavior can place these moral arguments into a more reasoned context. Addiction does not absolve one of responsibility for use of illicit drugs or for criminal behavior, but understanding how addictive drugs affect behavior through brain mechanisms can inform decisions to provide treatment to addicted individuals. For example, mandated treatment may be useful for drug-involved offenders who would otherwise not engage in the treatment process or make progress toward recovery. The persistence of neurologic deficits provides support for the recognition of addiction as a chronic disease and highlights the need for the same continuity of care so important in treatment of other chronic diseases (eg, asthma, hypertension). 72 It also suggests that agonist medications such as methadone are important treatments for addiction, even for individuals who have been under enforced abstinence during incarceration.
Third, neuroscience may help addicted individuals to better understand their own addiction. Such individuals may become frustrated when their efforts to control their own drug use are unsuccessful, and even with treatment many become frustrated with what is often a slow and tenuous recovery process. The neurobiology of the brain can help the addicted individual put this disease into a more understandable context and thereby facilitate effective treatment. Little research has been conducted in the field of addiction on whether knowing more about the substance use disorder is useful in helping to sustain recovery, and more research is needed. However, the concept of the “expert patient” who serves as his or her own best health advocate in a recovery management paradigm has been promoted for chronic disorders. As with these other illnesses, addiction must be managed by the individual over time to sustain recovery.
Principles of Drug Abuse Treatment for Offenders
Principles of Drug Abuse Treatment for Criminal Justice Populations , 75 published by the National Institute on Drug Abuse, synthesizes research on drug abuse treatment for drug abusers in the criminal justice system. It is intended as a resource for criminal justice professionals and the treatment community working with drug abusers involved with the system. The publication summarizes 20 years of research to provide guidance on evidence-based practices and identifies general principles on how to effectively address the drug abuse problems of populations involved with the criminal justice system ( Box ). 75
Box. NIDA Principles of Drug Abuse Treatment for Criminal Justice Populations
Drug addiction is a chronic brain disease that affects behavior
Recovery from drug addiction requires effective treatment, followed by continued care
Duration of treatment should be sufficiently long to produce stable behavioral changes
Assessment is the first step in treatment
Tailoring services to fit the needs of the individual is an important part of effective drug abuse treatment for criminal justice populations
Drug use during treatment should be carefully monitored
Treatment should target factors associated with criminal behavior
Criminal justice supervision should incorporate treatment planning for drug-abusing offenders, and treatment providers should be aware of correctional supervision requirements
Continuity of care is essential for drug abusers reentering the community
A balance of rewards and sanctions encourages prosocial behavior and treatment participation
Offenders with co-occurring drug abuse and mental health problems often require an integrated treatment approach
Medications are an important part of treatment for many drug-abusing offenders
Treatment planning for drug-abusing offenders living in or reentering the community should include strategies to prevent and treat serious, chronic medical conditions such as human immunodeficiency virus/AIDS, hepatitis B and C, and tuberculosis
NIDA indicates National Institute on Drug Abuse. Principles adapted from Fletcher and Chandler. 75
Implementing the Principles
Effective interventions depend on a coordinated response between criminal justice agencies, drug abuse treatment providers, mental health and physical health care organizations, and social service agencies. Each type of criminal justice agency (eg, jail, drug court, probation, prison) has its own role in sanctioning and supervision and lends itself to specific intervention opportunities. Table 3 provides a simplified overview of the criminal justice system and identifies the points at which intervention is possible.
Intervention Opportunities in Criminal Justice Systems
| Stage | Offender Event | Participants | Intervention Opportunities |
|---|---|---|---|
| Entry | Arrest | Crime victim Police FBI | Screening or referral |
| Prosecution | Court Pretrial release Jail | Crime victim Police FBI Judge | Diversion programs Drug courts Community-based treatment TASC |
| Adjudication | Trial | Prosecutor Defense attorney Defendant Jury Judge | NA |
| Sentencing | Fines Community supervision Incarceration | Jury Judge | Drug court Terms of incarceration Release conditions |
| Corrections | Probation Jail Prison | Probation officers Correctional personnel | Screening and treatment for substance use disorders Screening and treatment for other mental illnesses Screening and treatment for other medical disorders |
| Community reentry | Probation Parole Release | Probation or parole officer Family Community-based providers | Drug treatment Aftercare Housing Employment Mental health Medical care Halfway house TASC |
Abbreviations: FBI, Federal Bureau of Investigation; NA, not applicable; TASC, Treatment Accountability for Safer Communities.
Effective integration of drug treatment interventions into criminal justice settings requires matching the intervention to the organization. For example, since jail stays are usually brief, the interventions best suited to jails may be screening for drug and alcohol abuse, other mental illnesses, and medical conditions (eg, HIV, hepatitis B or C), with referral to community-based treatment providers. Implementing these principles throughout the criminal justice and drug abuse treatment systems also requires that these systems work together to address the addicted individual’s drug use, comorbid mental disorders and medical conditions, if present, and criminal behavior. Treatment professionals should understand the criminal justice process and the supervision requirements of their patients. In addition to addressing drug use behaviors, treatment outcomes improve when antisocial and criminal behaviors are targets of clinical intervention. 76 Criminal justice professionals must develop an understanding of addiction—signs and symptoms, treatment, and relapse—and their role in facilitating recovery.
Substance Abuse Treatment Research in Criminal Justice Settings
Prison environments are inherently coercive, 77 and special safeguards have been developed to ensure that prisoners can choose freely whether to participate in biomedical research without fear of consequence. Beyond mere equipoise, clinical trials must be designed so the research is of benefit to the prisoner participant regardless of the assigned study group. Within these constraints, it is important to conduct research to help improve substance abuse treatment and to assist in the successful transition of the substance abuser to the community. To facilitate research in this area, the National Institute on Drug Abuse created the Criminal Justice Drug Abuse Treatment Studies research cooperative, 78 a network of correctional agencies linked with treatment research centers and community treatment programs.
Opiate agonist medications used for the treatment of heroin addiction such as methadone and buprenorphine are underused in correctional populations. Naltrexone, an opiate antagonist, was developed to treat heroin addiction but also has been approved for treating alcoholism. Naltrexone is likely to be more acceptable in the criminal justice setting than agonist medications. However, the poor compliance with naltrexone has limited its use in the treatment of heroin addiction. The recent development of a long-lasting depot formulation for naltrexone 79 , 80 obviates this limitation, and a multisite clinical trial (NCT00781898) is currently evaluating its effectiveness in heroin-addicted probationers. Another area of research intended to reduce relapse in addicted offenders is the development of vaccines against cocaine, methamphetamine, or heroin.
Several avenues currently exist for providing drug abuse treatment as an alternative to incarceration. Drug courts were intended to provide a bridge between drug treatment and adjudication; from the first drug court established in Miami in 1989, drug courts have increased in number to nearly 2000 today. States such as Arizona, California, and New York have created treatment alternatives to incarceration for first-time drug offenders, juvenile offenders, and others. Many states are coming under political pressure to reduce the costs associated with incarceration by diverting nonviolent drug offenders to treatment.
Conclusions
Punishment alone is a futile and ineffective response to drug abuse, 2 failing as a public safety intervention for offenders whose criminal behavior is directly related to drug use. 81 Addiction is a chronic brain disease with a strong genetic component that in most instances requires treatment. The increase in the number of drug-abusing offenders highlights the urgency to institute treatments for populations involved in the criminal justice system. It also provides a unique opportunity to intervene for individuals who would otherwise not seek treatment.
The challenge of delivering treatment in a criminal setting requires the cooperation and coordination of 2 disparate cultures: the criminal justice system organized to punish the offender and protect society and the drug abuse treatment systems organized to help the addicted individual. Addressing addiction as a disease does not remove the responsibility of the individual, which is the argument frequently used to resist recognizing and treating addiction as an illness. Rather it highlights the personal responsibility of the addicted person to seek and adhere to drug treatment and that of society to ensure that such treatment is available and based on scientific evidence. Only a small percentage of those requiring treatment for drug addiction seek help voluntarily; in light of this, the criminal justice system provides a unique opportunity to intervene and disrupt the cycle of drug use and crime in a cost-effective manner.
Acknowledgments
Funding/Support: This article was written by staff from the National Institute on Drug Abuse and there was no external funding for this work.
Author Contributions: Study concept and design: Chandler, Fletcher, Volkow.
Financial Disclosures: None reported.
Publisher's Disclaimer: Disclaimer: The statements in this article are those of the authors and not necessarily those of the National Institute on Drug Abuse.
Additional Contributions: We thank Faye S. Taxman, PhD, and Matthew Perdoni, MS, both of George Mason University, for data on physical/medical, mental health, and substance use services ( Table 2 ) from the NIDA National Criminal Justice Drug Abuse Treatment Studies (CJ-DATS) National Criminal Justice Treatment Practices Survey. Neither of these individuals received compensation for their contributions.
Analysis and interpretation of data: Fletcher.
Drafting of the manuscript: Chandler, Fletcher.
Critical revision of the manuscript for important intellectual content: Chandler, Fletcher, Volkow.
Administrative, technical, or material support: Chandler, Fletcher, Volkow.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Research Proposal Drug abuse 3

Welcome to TopMarkEssays.blogspot.com, home for academic excellence. This blog is an affiliate of topmarkessays.com. Topmarkessay is among the premier essay writing companies in the world. Since the company was established, it has strived to provide students with the best papers that earn nothing less than top marks. Thousands of students have already benefited from our services and completed their studies passing with flying colors. Our group of highly qualified writers is there to offer you professional academic work that is 100% original. We understand your situation, and we work to give you the best for the price you can afford. We understand you are working or you have other commitment that makes it difficult for you to achieve the best in your academic work, and we offer you the solution. We have built our reputation for providing original quality work; we assure you nothing less than this. Friday, January 14, 2011
Related Papers
Lindsey Jackson
Roohullah Nawandish
saul thorkelson
gideon letaya
Siobhan Slattery
This is a proven fact that truth is the initial stage of progress. However, it is also believed that truth always starts away from the traditions and conventions. Therefore, people consider truths as attacks upon their beliefs, which people are following from ages. Truth also means some new facts that are unknown to us. People do not want to deviate from the facts, which they have learnt from their ancestors, and it is true to say that shedding ones dogmas is often difficult. They feel that it is an attack on their wisdom. If we look at the history of the world, we will find many examples where truth has generated commotions in the society. Different people have different views about the existence of God, life after death and origin of earth etc. For example, people took a long time to accept that the earth is round. Religious leaders and clergymen opposed this idea as it was against what they were teaching. Similarly, when Polish astronomer, Copernicus discovered that the earth goes round the sun and not vice versa, he was opposed by churches for many years. In fact he and his supporters were convicted for their ideas. Hence, it is very difficult to change the traditions that are followed by majority of people. Similarly, when Darwin gave the theory of evolution, and challenged the old ideology, he was resisted by public. Nobody was ready to believe that apes were the ancestors of humankind. However, it is important to accept truths, otherwise it would hinder the growth of mankind. It is important for us to accept new ideas so as to bring out reforms in society and thus adopt new ideologies. It would open doors for various kinds of development. One should not blindly accept and follow old ideas or new truths. There should be enough scientific approach and explanations for everything. However, there might be different reasons for this kind of uncomfortable reactions against truth. The first and the most responsible reason is the human nature. Most people will not prefer to change their ways of life and thinking, as it is accepted and prevalent from time unknown. They believe in what they are doing and experiencing for their whole life. The second factor is that truths often challenge the other persons authority. In order to save their status and honor, authoritarians oppose new ideas and truths. In getting their own way, they provoke the public. Sometimes these reactions go violent also. However, these days, people are becoming more open minded. They are ready to accept new ideas. Our societies all over the world are getting more flexible and open to new truths. Hence, new ideas and truths are accepted peacefully and there are no violent commotions.
Brian L . Ott
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Krista Bonello Rutter Giappone
Lauryn Angel
Hershey Gabi
Maria Cichosz
Oyetola Oniwide
Thường Thích
Michaela Pnacekova
Bradley J Fest
Fields: journal of Huddersfield student research
Helen Lomax
John Daniel Ibembe
Kevin Karpiak
IAEME Publication
Carine CARLET
SUSHRUT JADHAV
Richard Baskas, Ed.D. Candidate
Wendy Van Schalkwyk
Fawwaz Ulaby
Simphiwe Tsawu
corazon morilla , John Biggs
PROFILE Journal
Mary Shorthouse
Behavioral Sciences & The Law
Alan Tomkins
gokulpriya kumar
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
The nih almanac, national institute on drug abuse (nida).
- Important Events
- Legislative Chronology
The National Institute on Drug Abuse (NIDA) is the lead federal agency supporting scientific research on drug use and addiction. NIDA’s mission is to advance science on drug use and addiction and to apply that knowledge to improve individual and public health through:
- Strategically supporting and conducting basic, clinical, and epidemiological research on drug use, its consequences, and the underlying neurobiological, behavioral, and social mechanisms involved.
- Ensuring the effective translation, implementation, and dissemination of scientific research findings to improve the prevention and treatment of SUDs, reduce the harms associated with drug use, guide policies, enhance public awareness of addiction as a chronic but treatable medical illness, and reduce stigma.
In line with this mission, NIDA works to ensure that the following research priorities are addressed across institute programs and initiatives:
- understanding drugs, the brain, and behavior
- developing and testing novel prevention, treatment, harm reduction, and recovery support strategies
- accelerating research on the intersection of substance use, HIV, and related comorbidities
- improving implementation of evidence-based strategies in real-world settings
- translating research into innovative health applications
NIDA also works to ensure that cross-cutting priorities are reflected across institute programs and initiatives, including:
- training the next generation of scientists
- identifying and developing approaches to reduce stigma
- understanding sex, sexual orientation, and gender differences
- identifying and developing approaches to reduce health disparities
- understanding interactions between substance use, HIV, and other comorbidities
- leveraging data science and analytics to understand real-world complexity
- developing personalized interventions informed by people with lived experience
Important Events in NIDA History
1974 — Congress establishes NIDA as the federal focal point for biomedical research on the nature and extent of substance use and substance use disorders.
1975 — NIDA supports the first nationally representative survey of adolescent and young adult substance use and attitudes. The ongoing Monitoring the Future (MTF) Survey tracks trends in past-year, past-month, and lifetime substance use among 12 th graders.
1979 — The NIDA Intramural Research Program (IRP) (formerly the Addiction Research Center) moves to Baltimore’s Johns Hopkins Bayview Medical Center (then, the Francis Scott Key Medical Center) from Lexington, KY.
NIDA-supported scientists identify the brain chemical dynorphin . Its discovery, along with other parts of the natural opioid system in the brain, revolutionizes the addiction field.
1980 — NIDA-supported researchers release data showing caregivers and teachers who receive training in supporting their children’s social and emotional needs (the Raising Healthy Children intervention) raise young people with better behavioral and health outcomes, benefits that are passed to their offspring.
1984 — Nicotine replacement therapy is developed by NIDA-supported researchers
1991 — The Monitoring the Future Survey expands to include 8th and 10th graders.
NIDA researchers clone the dopamine transporter , cocaine's primary site of action in the brain.
1992 — NIDA-supported research isolates anandamide , a chemical in the brain that interacts with the active ingredient in cannabis, delta-9-tetrahydrocannabinol (THC). In addition, the researchers discover that anandamide also plays a role in other brain activities, such as pain relief, sedation, memory, and cognition.
NIDA researchers demonstrate the effectiveness of sublingual buprenorphine for the treatment of opioid use disorder .
NIDA joins the National Institutes of Health (NIH).
1993 — The NIDA Medications Development Program obtains approval from the U.S. Food and Drug Administration (FDA) for levomethadyl acetate (LAAM), the first medication approved in a decade for the treatment of opioid use disorder.
1998 — As part of a team including the Pasteur Institute, Karolinska Institute and Glaxo Wellcome Geneva, a NIDA-supported researcher identifies a brain receptor activated by nicotine use. The finding identifies a potential target for smoking cessation treatment.
Researchers in NIDA's Intramural Research Program discover that the addiction pathway for cocaine is more complicated than previously understood. Researchers tested the theory that dopamine and serotonin were key to the euphoria associated with cocaine use, discovering that other factors may be involved in its rewarding effects.
NIDA scientists identify a chemical known as [D-Ala2,D-leu5]enkephalin (DADLE) that may help reduce long-term nerve damage from methamphetamine use. This has important implications for treating people with substance use disorder and the side effects of long-term substance use.
NIDA research leads to the FDA approval of buproprion for smoking cessation.
1999 — NIDA-supported researchers report the first clinical cases of cannabis withdrawal . Two scientific studies suggest that irritability, stomach pain, and withdrawal from social interactions may be symptoms of quitting cannabis after ongoing use. The findings suggest that effective treatments to alleviate these symptoms are needed. They also suggest that continued use of cannabis may be an effort to alleviate unpleasant withdrawal symptoms.
NIDA awards grants to the first five regional sites under its new Clinical Trials Network (CTN) . The network continues to conduct clinical research into medications for substance use disorders and to bring updated science to communities and healthcare offices.
Using brain scans and tracking cerebral phosphate metabolites, NIDA-supported researchers show that longer term methadone treatment is associated with brain recovery .
Research supported by NIDA identifies a way for scientists to estimate how likely an opioid is to cause tolerance and have the potential to cause addiction. The scale, called relative activity versus endocytosis or RAVE measure , calculates how effective different opioids are regulating the signaling of the opioid receptors they activate in the brain. It assesses the opioid’s ability to trigger cells to remove opioid receptors from the cell membrane, a process called internalization.
NIDA-supported research finds that HIV can survive in used syringes for four weeks or more after use. Specifically, the model estimates that blood containing HIV could survive in the razor-thin space inside the needle of the syringe.
NIDA-supported research identifies brain processes that increase the rewarding effects of cocaine the more a person uses it, a change thought to play an important role in the development of cocaine craving and addiction.
Researchers analyze the health care costs of substance use benefits and find substance use treatment is cost-effective . In this analysis, researchers found that changing even stringent limits on annual substance use benefits had only a small absolute effect on overall insurance costs under managed care, even though a large percentage of substance use patients were affected.
2000 — Researchers demonstrate that contingency management for cocaine use disorder can have long-lasting effects and serve as a valuable role in treating addictions. Patients in this study who received vouchers for having cocaine negative urine tests were more likely to have sustained cocaine abstinence during outpatient treatment than a comparative group that received incentives regardless of urine test results.
In a study partially funded by NIDA, researchers merge technologies from the imaging and genetic fields to discover that the number of brain dopamine D2 receptors an individual has may correlate directly with the amount of euphoria experienced while taking methylphenidate, a mild stimulant.
2001 — NIDA-supported animal research shows a single exposure to cocaine induces changes in brain cells that are very similar to long-term potentiation, a process that plays an important role in associating experiences with feelings and motivations.
2002 — NIDA-supported research leads to the FDA approval of buprenorphine and buprenorphine/naloxone , the first medications for opioid use disorder that can be prescribed in an office setting.
2006 — NIDA-supported research leads to the FDA approval of varenicline for tobacco use disorder
NIDA-supported research demonstrates that methadone is an effective means of reducing heroin use and criminal behavior among opioid-dependent individuals awaiting entry into a comprehensive methadone treatment program.
2008 — NIDA's Monitoring the Future Survey reveals an increased misuse of prescription medications and over-the-counter cough syrups among high school seniors, accounting for 8 of the top 13 drug categories reported by this group.
2009 — NIDA launches a comprehensive Physicians Outreach Initiative, NIDAMED , which gives medical professionals tools and resources to screen their patients for tobacco, alcohol, illicit, and nonmedical prescription drug use, including an interactive online drug use screening tool.
2010 — NIDA launches its first annual National Drug Facts Week (NDFW), a health observance that inspires dialogue about the science of drug use and addiction among youth. It provides an opportunity for scientists, students, educators, healthcare providers, and community partners to help advance addiction science and address youth drug and alcohol use in communities and nationwide.
2011 — The Population Assessment of Tobacco and Health (PATH) Study launches. A joint effort of NIDA and the U.S. Food and Drug Administration, PATH is a national longitudinal study of tobacco use and how it affects the health of people in the United States
2012 — A NIDA-supported seminal study demonstrates that scaling up HIV treatment in people who inject drugs results in reductions in community-level viral load and HIV transmission.
2013 — NIDA, The National Institute on Alcohol Abuse and Alcoholism (NIAAA), and The National Cancer Institute (NCI) form the Collaborative Research on Addiction at NIH (CRAN) . The partnership integrates resources and expertise to advance the science and treatment of substance abuse and addiction.
2014 — NIDA announces the development of an innovative National Drug Early Warning System (NDEWS) to monitor emerging nationwide new and emerging drug trends to help public health experts respond quickly.
2015 — NIDA-supported research leads to FDA approval of the first naloxone nasal spray .
NIDA launches the Adolescent Brain Cognitive Development (ABCD) Study . This study follows more than 11,800 children from ages 9-10 through adolescence into young adulthood. By integrating neuroimaging with genetics, neuropsychological, behavioral, and other health assessments, the study aims to shed light on how substance use and other experiences during adolescence affect brain development and later health outcomes such as drug use and addiction.
2016 — NIDA-supported research leads to FDA approval of a buprenorphine implant to improve treatment retention and reduce burdens associated with frequent dosing.
2017 — NIDA-supported research leads to the development of ReSET-O, the first FDA-approved smartphone app to deliver behavioral treatment for opioid use disorder.
NIDA-supported research develops Flowlytics , a cloud-based data analysis software that allows a health care facility to track its inventory of controlled substances, such as opioids, helping to prevent drug theft (also known as drug diversion). The patented software can detect potential drug diversion incidents earlier than previous methods.
2018 — The Helping to End Addiction Long-Term Initiative® or NIH HEAL Initiative® is launched to speed scientific solutions to stem the national opioid public health crisis. NIDA is leading HEAL-supported research aimed at preventing and treating opioid misuse and addiction.
NIDA-supported research leads to the FDA approval of lofexidine , the first non-opioid treatment for opioid withdrawal.
Researchers develop a biosensor to detect opioid receptor activation. Using this method, researchers are able to show that opioid receptors function in different cell locations depending on the type of opioid.
2019 — Researchers identify a brain receptor with anti-opioid activity, a discovery that opens the door to new way to improve opioid safety.
Through investment in its Small Business Innovation Research (SBIR) and Small Business Technology Transfer (STTR) programs, NIDA supports development of FDA-regulated therapeutic and diagnostic devices, mobile health and general wellness products, research tools, and health IT solutions. These include:
- Prapela ™, a hospital bassinet pad that delivers gentle, random vibrations to treat newborns who were exposed to opioids before birth. The bassinet pad helps improve newborns’ breathing and heart rate.
- OpenBeds , a HIPAA-compliant, cloud-based platform that facilitates referrals and coordination among medical and mental health providers, social services, and substance use programs.
- RelieVRx , the first VR-based therapeutic to receive FDA authorization for chronic lower back pain and the first to obtain a unique HCPS Level II code from the Centers for Medicare and Medicaid Services (CMS).
- SecondChance , which detects changes in a person’s breathing that may indicate a drug overdose or monitor other clinical indications.
- Boulder , a digital platform that delivers comprehensive treatment for OUD.
2020 — A study partially funded by NIDA finds why some people with HIV are able to maintain suppressed viral loads for years without ART. The study is chosen as a runner-up in Science magazine’s 2020 Breakthrough of the Year.
With funding from the HEAL Initiative, NIDA's Clinical Trials Network expands , adding five new nodes across the country.
Monitoring the Future Study and Population Assessment of Tobacco and Health (PATH) study data show that flavored e-cigarette products particularly appeal to youth. The data informs a 2020 U.S. Food and Drug Administration (FDA) policy prioritizing enforcement against certain unauthorized flavored cartridge-based products.
Biobot Analytics , another SBIR grantee, pioneers the commercial application of wastewater technology to monitor the presence of drugs in communities.
The National Drug Early Warning System (NDEWS), a network of 18 sentinel sites that monitors patterns of drug use across the nation, incorporates real-time surveillance and harnesses its network to collect data on substance use-related consequences of COVID-19.
2021 — With partial funding from the Helping to End Addiction Long-term ® Initiative, or NIH HEAL Initiative ® , NIDA launches the HEALthy Brain and Child Development (HBCD) Study to better understand very early brain development and the effects of environmental factors such as maternal substance use during pregnancy.
A study finds that a combination of oral bupropion and injectable naltrexone reduces methamphetamine use and cravings people with methamphetamine use disorder.
SBIR-funded Spark Biomedical develops a wearable treatment technology intended for the relief of opioid withdrawal symptoms.
A meta-analysis of studies shows that medication treatment for opioid use disorder (MOUD) is associated with greater adherence to antiretroviral therapy (ART) and HIV viral suppression.
2022 — NIDA collaborates with the Centers for Disease Control and Prevention and other government agencies for a study that shows the expansion of telehealth services during the COVID-19 pandemic was associated with people staying in treatment longer and reducing their risk of medically treated overdose.
A study finds that people with opioid use disorder who were incarcerated and received a medication approved to treat opioid use disorder, known as buprenorphine, were less likely to face rearrest and reconviction after release than those who did not receive the medication.
NIDA research contributes to a new U.S. Preventive Services Task Force recommendation on pre-exposure prophylaxis (PrEP) for the prevention of HIV for those at increased risk, including people who inject drugs.
2023 — A study under the NIH Heal Initiative shows that initiating buprenorphine treatment in the ER is safe, effective and does not trigger withdrawal in people with opioid use disorder. Clinician concern over this type of withdrawal can be a barrier to using this treatment.
Researchers pinpoint areas in the genome associated with general addiction risk, as well as the risk of specific substance use disorders – namely, alcohol, nicotine, cannabis, and opioid use disorders.
NIDA-supported research leads to FDA approval of nalmefene nasal spray , which can be used to treat fentanyl overdose.
NIDA Legislative Chronology
1966 — P.L. 89-793, the Narcotic Addict Rehabilitation Act, provided for increased Federal efforts in the rehabilitation and treatment of addiction to narcotics (limited to opiates).
1970 — P.L. 91-513, the Comprehensive Drug Abuse Prevention and Control Act, replaced the USPHS Act's definition of "narcotic addict" with a definition of "drug dependent person" to authorize treatment for both narcotic addiction and other drug problems.
1972 — P.L. 92-255, the Drug Abuse Office and Treatment Act, created a Special Action Office for Drug Abuse Prevention (SAODAP) in the Executive Office of the President, and authorized the establishment of NIDA within the Department to become operational in 1974. In cooperation with other Federal agencies, especially the National Institute of Mental Health's (NIMH) Division of Narcotic Addiction and Drug Abuse (DNADA), SAODAP established a national network of multi-modality drug use treatment programs.
1974 — P.L. 93-282, the Comprehensive Alcohol Abuse and Alcoholism Prevention, Treatment, and Rehabilitation Act Amendments, created the Alcohol, Drug Abuse, and Mental Health Administration (ADAMHA), which was charged with supervising and coordinating the functions of NIMH, NIDA, and NIAAA. Programs and responsibilities of DNADA and SAODAP were moved to NIDA. Section 204 of this law, enacted and effective on May 14, 1974, gave NIDA a permanent statutory basis, and established NIDA as a freestanding Institute.
1979 — P.L. 96-181, the Drug Abuse Prevention, Rehabilitation, and Treatment Act, mandated that at least 7% in FY 1980 and 10% in FY 1981 of NIDA's Community Programs budget be spent on prevention.
1981 — P.L. 97-35, the Omnibus Budget Reconciliation Act, repealed NIDA's formula grants and Community Programs project grants and contracts authorities, and established the Alcohol, Drug Abuse, and Mental Health Services (ADMS) Block Grant program, giving more control of treatment and prevention services to the states.
1986 — P.L. 99-570, the Anti-Drug Abuse Act of 1986, increased the Block Grant and created a substance use treatment enhancement. The Act also provided increased funds for all NIDA research, particularly AIDS research.
Executive Order 12564 mandated a drug-free Federal workplace program. NIDA became the lead agency, creating its Office of Workplace Initiatives.
1987 — P.L. 100-71, Supplemental Appropriations Act of 1987, required HHS (NIDA) to publish guidelines in the Federal Register for Federal drug testing.
1988 — P.L. 100-690, the Anti-Drug Abuse Act of 1988, established the Office of National Drug Control Policy (ONDCP) in the Executive Office of the President and authorized funds for Federal, state, and local law enforcement, school-based drug prevention efforts, and drug use treatment with special emphasis on people injecting drugs and at higher risk for acquiring HIV.
1989 and 1990 — P.L. 101-166 and P.L. 101-517, the Departments of Labor, HHS, and Education Appropriations Acts for FY 1990 and 1991, contained identical prohibitions precluding the use of funds provided under these enactments to carry out any program of distributing sterile needles.
1992 — P.L. 102-321, the ADAMHA Reorganization Act, transferred NIDA to NIH; earmarked 15% of the Institute's research appropriation for health services research; established a Medication Development Program within NIDA; provided authority to designate Drug Abuse Research Centers for interdisciplinary research on drug use and related biomedical, behavioral, and social issues; and created an Office on AIDS at NIDA.
P.L. 102-394, the Departments of Labor, HHS, and Education FY 1993 Appropriations Act, provided that up to $2 million of NIDA research funds be available to carry out section 706 of P.L. 102-321, which required the HHS Secretary, acting through NIDA, to request a National Academy of Sciences study of U.S. programs that provide both sterile hypodermic needles and bleach.
1993 — P.L. 103-112, the Department of Labor, HHS and Education FY 1994 Appropriations Act, prohibited the use of funds under the Act for any further implementation of section 706 of P.L. 102-321 (see above) and any program for distributing sterile needles.
1994 and 1996 — P.L. 103-333, the Departments of Labor, HHS, and Education Appropriations Act for FY 1995; P.L. 104-134, the Omnibus Consolidated Rescissions and Appropriations Act for FY 1996; and P.L. 104-208, the Omnibus Consolidated Appropriations Act for FY 1997 — each prohibited use of any funds provided in the enactments to carry out any program of distributing sterile needles.
1997 — P.L. 105-78, the Departments of Labor, HHS, and Education Appropriation Act for FY 1998, continued prior restrictions on needle-exchange programs through March 31, 1998, permitting funding thereafter of those programs meeting certain statutory requirements including criteria of the HHS Secretary.
1998 — P.L. 105-277, the Omnibus Consolidated and Emergency Supplemental Appropriations Act-1999, restored the general prohibition on funds for needle exchange programs; statutorily reestablished ONDCP in the Executive Office of the President with significantly expanded authority over drug control agencies; and required ONDCP to conduct a 4-year (FYs 1999-2002) national anti-drug media campaign aimed at youth.
1999 — P.L. 106-113, the Consolidated Appropriations Act-2000, continued the ban on funding of sterile needle and syringe exchange programs; prohibited use of appropriated funds for promotion of legalization of any Schedule I controlled substance; and postponed termination of NIDA's triennial report until 5/15/2000.
2000 — P.L. 106-554, the Consolidated Appropriations Act-2001, authorized the Director of NIH to negotiate a long-term lease for research facilities at Baltimore's Bayview Campus, and continued prior prohibitions on funding of sterile needle/syringe exchange programs and on promotion of legalization of Schedule I controlled substances.
P.L. 106-310, the Children's Health Act of 2000, repealed the Narcotic Addict Rehabilitation Act of 1966 [P.L. 89-793]; waived certain requirements of the Controlled Substances Act to permit qualified physicians to engage in office-based treatment of opioid addiction; and authorized expansion of NIDA research on methamphetamine and increased emphasis on ecstasy research.
2001 — P.L. 107-116, the Departments of Labor, HHS, and Education FY 2002 Appropriations Act, continued prior prohibitions on funding of sterile needle and syringe exchange programs and on legalization of Schedule I controlled substances.
2002 — Title II of P.L. 107-273, the Drug Abuse Education, Prevention, and Treatment Act of 2002, authorized NIDA expansion of interdisciplinary research and clinical trials with treatment centers of the National Drug Abuse Treatment Clinical Trials Network; and required a NIDA study on development of medications for amphetamine/methamphetamine addiction.
2003 — Division G of P.L. 108-7, the Departments of Labor, HHS, and Education FY 2003 Appropriations Act, continued prior prohibitions on funding of sterile needle and syringe exchange programs and on legalization of Schedule I controlled substances.
2004 — P.L. 108-358, the Anabolic Steroids Control Act of 2004, significantly expanded the list of anabolic steroids classified as controlled substances; required a review of Federal sentencing guidelines; and authorized $15 million, for each of the next fiscal years through 2009, for educational programs in schools to highlight the dangers of steroids, with preference given to programs deemed effective by NIDA.
2005 — P.L. 109-56 amended the Controlled Substances Act to lift the patient limitations imposed on medical practitioners in group practices regarding the prescribing of drug addiction treatments. Section 2013 of P.L. 109-59, the Safe, Accountable, Flexible, Efficient Transportation Equity Act, directed the Secretary of Transportation to advise and coordinate with other Federal agencies to address driving under the influence of controlled substances and, in cooperation with NIH (NIDA), to submit a report to Congress on drug-impaired driving.
2006 — P.L. 109-469, the U.S. Office of National Drug Control Policy (ONDCP) Reauthorization Act of 2006, in section 1102, amended the Controlled Substances Act to further relax the patient limitations on provision of drug addiction treatments, allowing medical practitioners to notify the HHS Secretary of need and intent to treat up to 100 patients. Section 1120 required the ONDCP Director to consult with NIH (NIDA) and the National Academy of Sciences in making policy relating to syringe exchange programs.
2006 — P.L. 109-482 (H.R. 6164) , the National Institutes of Health Reform Act of 2006, reaffirmed certain organizational authorities of the NIH Director including establishing, abolishing, and reorganizing national research institutes. It established the Scientific Management Review Board (SMRB) to advise the NIH Director on the use of these organizational authorities. In 2009, the SMRB began discussions about how to optimize research into substance use, and addiction at the NIH. In 2010, the SMRB voted in favor of recommending to the NIH Director the establishment of a new institute for substance use, and addiction-related research and the dissolution of NIAAA and NIDA.
2008 — P.L. 110-199, Second Chance Act of 2007, reauthorized and rewrote provisions of the 1968 Omnibus Crime Control and Safe Streets Act to expand reentry services for offenders. Required the Attorney General (1) to consult with NIDA (and SAMHSA) regarding performance outcome measures and data collection related to substance use and mental health services [sec.101 (k)]; and (2) in consultation with NIDA to conduct a study on the use and effectiveness of funding aftercare services for offenders completing substance use programs while incarcerated [sec. 102 (c)]. Permitted the U.S. Attorney General in consultation with NIDA to make research grants to evaluate the effectiveness of depot naltrexone for treatment of heroin addiction [sec. 244 (a)].
2009 — P.L. 111-117, the Consolidated Appropriations Act, changed federal law regarding potential funding for syringe exchange programs. The Act states: "None of the funds contained in this Act may be used to distribute any needle or syringe for the purpose of preventing the spread of blood borne pathogens in any location that has been determined by the local public health or local law enforcement authorities to be inappropriate for such distribution."; Thus, syringe exchange for this purpose is allowed unless public health or law enforcement authorities choose, at the local level, to prevent it. This change could result in additional research proposals, and thus funding, for syringe exchange-related research projects.
2010 — P.L. 111-148, The Patient Protection and Affordable Care Act, was signed into Law on March 23, 2010. This landmark legislation includes many of the provisions originally included in The Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act, passed as part of the Emergency Economic Stabilization Act in October of 2008. Implementation of this legislation continues to develop and is designed to help ensure that all Americans have access to mental health and addiction treatment. The parity language prohibits health insurers from placing discriminatory restrictions on such treatment and bars health plans from charging higher copayments, coinsurance, deductibles, and maximum out-of-pocket limits and imposing lower day and visit limits on mental health and addiction care.
2011 — P.L. 112—74, the Consolidated Appropriations Act, rescinded the change made by P.L. 111-117 regarding potential funding for syringe exchange programs. The law now reads, "Notwithstanding any other provision of this Act, no funds appropriated in this Act shall be used to carry out any program of distributing sterile needles or syringes for the hypodermic injection of any illegal drug." It is so far unclear how these changes might affect research in this area.
2015 — The Consolidated Appropriations Act, 2016 changed the rules again for federal funding related to syringe exchange programs. While current law continues the prohibition on the use of federal funds for the actual purchase of syringes or sterile needles, it does allow existing programs in hard-hit communities to access federal funds for other program elements, including substance use counseling and referral to treatment, that support communities in their drive to end the cycle of addiction.
2016 — Comprehensive Addiction and Recovery Act (CARA), enacted on July 22, 2016, aims to address the national epidemic of opioid overdose by creating and expanding federal grant programs to include, but not limited to: expanding access to opioid overdose reversal drugs, by supporting the purchase and distribution of such medications and training for first responders; increasing awareness and educating the public regarding the misuse of prescription opioids; reauthorizing the National All Schedules Prescription Electronic Reporting (NASPER) Act, which provides grants to states to support and improve interoperability of PDMPs; and establishing an HHS-led task force to consolidate federal best practices for pain management.
21 St Century Cures Act was signed into law on December 13, 2016. The legislation provides NIH with critical tools and resources to advance biomedical research across the scientific spectrum, from foundational basic research studies to advanced clinical trials of promising new therapies. Importantly, the Cures Act provides NIH with improved flexibility and resources needed to accomplish its mission to improve the health of Americans. Most notably, the Cures Act implements measures to: alleviate administrative burdens that can prolong the start of clinical trials; improve privacy protections for research volunteers; encourage inclusion of diverse populations represented in clinical research; and open up new NIH funding opportunities for young investigator.
2018 — The “Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act of 2018 (the SUPPORT Act),” became law on October 24, 2018. The legislation included provisions to strengthen the behavioral health workforce through increasing addiction medicine education; standardizing the delivery of addiction medicine; expanding access to high-quality, evidence-based care; and increasing coverage of addiction medicine services in a way that facilitates the delivery of coordinated and comprehensive treatment.
2022 — The Mainstreaming Addiction Treatment (MAT) Act and The Medication Access and Training Expansion (MATE) Act of the Consolidated Appropriations Act, 2023, were signed into law on December 29, 2022. The MAT Act allows any clinician registered to prescribe Schedule III substances the ability to treat opioid use disorder patients with the effective medication buprenorphine, without requiring the additional reporting steps—previously known as the X-waiver—that had been a barrier to provision of this care. The MATE Act requires physicians, including residents and fellows, and other health care professionals who prescribe controlled substances, to complete a one-time-only eight hours of training on the treatment and management of patients with opioid or other substance use disorders.
Biographical Sketch of NIDA Director, Nora D. Volkow, M.D.

Nora D. Volkow, M.D., is Director of the National Institute on Drug Abuse (NIDA) at the National Institutes of Health. NIDA is the world’s largest funder of scientific research on the health aspects of drug use and addiction.
Dr. Volkow's work has been instrumental in demonstrating that drug addiction is a brain disorder. As a research psychiatrist, Dr. Volkow pioneered the use of brain imaging to investigate how substance use affects brain functions. In particular, her studies have documented how changes in the dopamine system affect the functions of brain regions involved with reward and self-control in addiction. She has also made important contributions to the neurobiology of obesity, ADHD, and aging.
Dr. Volkow was born in Mexico and earned her medical degree from the National University of Mexico in Mexico City, where she received the Robins Award for best medical student of her generation. Her psychiatric residency was at New York University, where she earned a Laughlin Fellowship from The American College of Psychiatrists as one of 10 outstanding psychiatric residents in the United States.
Much of her professional career was spent at the Department of Energy’s Brookhaven National Laboratory in Upton, New York, where she held several leadership positions including Director of Nuclear Medicine, Chairman of the Medical Department, and Associate Laboratory Director for Life Sciences. Dr. Volkow was also a professor in the Department of Psychiatry and Associate Dean of the Medical School at The State University of New York at Stony Brook.
Dr. Volkow has published almost a thousand peer-reviewed articles, written 113 book chapters, manuscripts and articles, co-edited "Neuroscience in the 21st Century" and edited four books on neuroscience and brain imaging for mental and substance use disorders.
She received a Nathan Davis Award for Outstanding Government Service, was a Samuel J. Heyman Service to America Medal (Sammies) finalist and is a member of the National Academy of Medicine and the Association of American Physicians. Dr. Volkow received the International Prize from the French Institute of Health and Medical Research for her pioneering work in brain imaging and addiction science; was awarded the Carnegie Prize in Mind and Brain Sciences from Carnegie Mellon University; and was inducted into the Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD) Hall of Fame. She was named one of Time magazine's "Top 100 People Who Shape Our World"; one of "20 People to Watch" by Newsweek magazine; Washingtonian magazine’s "100 Most Powerful Women"; "Innovator of the Year" by U.S. News & World Report; and one of "34 Leaders Who Are Changing Health Care" by Fortune magazine.
NIDA Directors
| Robert L. DuPont | 1973 | 1978 |
| William Pollin | 1979 | 1985 |
| Charles R. Schuster | 1986 | 1992 |
| Richard A. Millstein (Acting) | 1992 | 1994 |
| Alan I. Leshner | 1994 | 2001 |
| Glen R. Hanson (Acting) | 2001 | 2003 |
| Nora D. Volkow | 2003 | Present |
NIDA’s organizational structure comprises the Office of the NIDA Director , the Office of Management , the Office of Science Policy and Communications , the Intramural Research Program , the Division of Extramural Research , and three extramural funding divisions: the Division of Neuroscience and Behavior ; the Division of Therapeutics and Medical Consequences ; and the Division of Epidemiology, Services and Prevention Research . NIDA is also home to the Center for Clinical Trials Network , which manages the National Drug Abuse Treatment Clinical Trials Network ; the Office of Translational Initiatives and Program Innovations , which provides leadership to speed the translation of research discoveries into health applications; and the HIV Research Program , which is responsible for developing, planning, and coordinating high-priority research at the intersection of HIV, substance use, and SUDs. Through a wide range of programs, workshops, and funding mechanisms, the Office of Research Training, Diversity, and Disparities supports researchers at multiple stages of their careers, aims to enhance the diversity of the addiction science workforce, and promotes research to address health inequities.
Through grants and contracts awarded to investigators at research institutions around the country and overseas, as well as through its Intramural Research Program, NIDA addresses the most fundamental and essential questions about substance use. This includes detecting and responding to emerging substance use trends, understanding how drugs work in the brain and body, identifying social determinants of substance use risk and SUDs, and developing and testing new approaches to prevention, treatment, and recovery.
Learn more about NIDA Research Programs and Activities .
This page last reviewed on March 6, 2024
Connect with Us
- More Social Media from NIH
- Open access
- Published: 30 August 2024
Research landscape analysis on dual diagnosis of substance use and mental health disorders: key contributors, research hotspots, and emerging research topics
- Waleed M. Sweileh 1
Annals of General Psychiatry volume 23 , Article number: 32 ( 2024 ) Cite this article
Metrics details
Substance use disorders (SUDs) and mental health disorders (MHDs) are significant public health challenges with far-reaching consequences on individuals and society. Dual diagnosis, the coexistence of SUDs and MHDs, poses unique complexities and impacts treatment outcomes. A research landscape analysis was conducted to explore the growth, active countries, and active journals in this field, identify research hotspots, and emerging research topics.
A systematic research landscape analysis was conducted using Scopus to retrieve articles on dual diagnosis of SUDs and MHDs. Inclusion and exclusion criteria were applied to focus on research articles published in English up to December 2022. Data were processed and mapped using VOSviewer to visualize research trends.
A total of 935 research articles were found. The number of research articles on has been increasing steadily since the mid-1990s, with a peak of publications between 2003 and 2012, followed by a fluctuating steady state from 2013 to 2022. The United States contributed the most articles (62.5%), followed by Canada (9.4%). The Journal of Dual Diagnosis , Journal of Substance Abuse Treatment , and Mental Health and Substance Use Dual Diagnosis were the top active journals in the field. Key research hotspots include the comorbidity of SUDs and MHDs, treatment interventions, quality of life and functioning, epidemiology, and the implications of comorbidity. Emerging research topics include neurobiological and psychosocial aspects, environmental and sociocultural factors, innovative interventions, special populations, and public health implications.
Conclusions
The research landscape analysis provides valuable insights into dual diagnosis research trends, active countries, journals, and emerging topics. Integrated approaches, evidence-based interventions, and targeted policies are crucial for addressing the complex interplay between substance use and mental health disorders and improving patient outcomes.
Introduction
Substance use disorders (SUDs) refer to a range of conditions characterized by problematic use of psychoactive substances, leading to significant impairment in physical, psychological, and social functioning [ 1 ]. These substances may include alcohol, tobacco, illicit drugs (e.g., cocaine, opioids, cannabis), and prescription medications. The global burden of SUDs is substantial, with far-reaching consequences on public health, socio-economic development, and overall well-being. For instance, alcohol abuse accounts for 3 million deaths worldwide annually, while the opioid crisis has escalated to unprecedented levels in certain regions, such as North America, resulting in tens of thousands of overdose deaths per year [ 2 , 3 , 4 ]. Mental health disorders (MHDs) encompass a wide range of conditions that affect mood, thinking, behavior, and emotional well-being [ 5 ]. Examples of MHDs include depression, anxiety disorders, post-traumatic stress disorder (PTSD), bipolar disorder, schizophrenia, and eating disorders. These conditions can significantly impair an individual's ability to function, negatively impacting their quality of life, relationships, and overall productivity [ 6 , 7 , 8 ]. Furthermore, certain MHD such as major depressive disorder and anxiety are often associated with specific affective temperaments, hopelessness, and suicidal behavior and grasping such connections can help in crafting customized interventions to reduce suicide risk [ 9 ]. In addition, a systematic review of 18 studies found that demoralization with somatic or psychiatric disorders is a significant independent risk factor for suicide and negative clinical outcomes across various populations [ 10 ]. The coexistence of SUDs and MHDs, often referred to as dual diagnosis or comorbidity, represents a complex and prevalent phenomenon that significantly impacts affected individuals and healthcare systems [ 11 , 12 , 13 , 14 , 15 ]. For instance, individuals with depression may be more likely to self-medicate with alcohol or drugs to cope with emotional distress [ 16 ]. Similarly, PTSD has been linked to increased rates of substance abuse, as individuals attempt to alleviate the symptoms of trauma [ 17 , 18 ]. Moreover, chronic substance use can lead to changes in brain chemistry, increasing the risk of developing MHDs or exacerbating existing conditions [ 17 , 19 , 20 , 21 ]. The coexistence of SUDs and MHDs presents unique challenges from a medical and clinical standpoint. Dual diagnosis often leads to more severe symptoms, poorer treatment outcomes, increased risk of relapse, and higher rates of hospitalization compared to either disorder alone [ 22 ]. Additionally, diagnosing and treating dual diagnosis cases can be complex due to overlapping symptoms and interactions between substances and psychiatric medications. Integrated treatment approaches that address both conditions simultaneously are essential for successful recovery and improved patient outcomes [ 20 ]. Patients grappling with dual diagnosis encounter a multifaceted web of barriers when attempting to access essential mental health services. These barriers significantly compound the complexity of their clinical presentation. The first barrier pertains to stigma, where societal prejudices surrounding mental health and substance use disorders deter individuals from seeking help, fearing discrimination or social repercussions [ 23 ]. A lack of integrated care, stemming from fragmented healthcare systems, poses another significant hurdle as patients often struggle to navigate separate mental health and addiction treatment systems [ 24 ]. Insurance disparities contribute by limiting coverage for mental health services and imposing strict criteria for reimbursement [ 25 ]. Moreover, there is a shortage of adequately trained professionals equipped to address both substance use and mental health issues, creating a workforce barrier [ 26 ]. Geographical disparities in access further hinder care, particularly in rural areas with limited resources [ 27 ]. These barriers collectively serve to exacerbate the clinical complexity of patients with dual diagnosis, and ultimately contributing to poorer outcomes.
A research landscape analysis involves a systematic review and synthesis of existing literature on a specific topic to identify key trends, knowledge gaps, and research priorities [ 28 , 29 ]. Scientific research landscape analysis, is motivated by various factors. First, the rapid growth of scientific literature poses a challenge for researchers to stay up-to-date with the latest developments in their respective fields. Research landscape analysis provides a structured approach to comprehend the vast body of literature, identifying crucial insights and emerging trends. Additionally, it plays a vital role in identifying knowledge gaps, areas with limited research, or inadequate understanding. This pinpointing allows researchers to focus on critical areas that demand further investigation, fostering more targeted and impactful research efforts [ 30 ]. Furthermore, in the realm of policymaking and resource allocation, evidence-based decision-making is crucial. Policymakers and funding agencies seek reliable information to make informed decisions about research priorities. Research landscape analysis offers a comprehensive view of existing evidence, facilitating evidence-based decision-making processes [ 28 ]. When it comes to the research landscape analysis of dual diagnosis of SUDs and MHDs, there are several compelling justifications to explore this complex comorbidity and gain a comprehensive understanding of its interplay and impact on patient outcomes. Firstly, the complexity of the interplay between SUDs and MHDs demands a comprehensive examination of current research to unravel the intricacies of this comorbidity [ 31 ]. Secondly, dual diagnosis presents unique challenges for treatment and intervention strategies due to the overlapping symptoms and interactions between substances and psychiatric medications. A research landscape analysis can shed light on effective integrated treatment approaches and identify areas for improvement [ 18 ]. Moreover, the public health impact of co-occurring SUDs and MHDs is substantial, resulting in more severe symptoms, poorer treatment outcomes, increased risk of relapse, and higher rates of hospitalization. Understanding the research landscape can inform public health policies and interventions to address this issue more effectively [ 32 ]. Lastly, the holistic approach of research landscape analysis enables a comprehensive understanding of current knowledge, encompassing epidemiological data, risk factors, treatment modalities, and emerging interventions. This integrative approach can lead to more coordinated and effective care for individuals with dual diagnosis [ 22 ]. Based on the above argument, the current study aims to conduct a research landscape analysis of dual diagnosis of SUDs and MHDs. The research landscape analysis bears a lot of significance for individuals and society. First and foremost, it’s a beacon of hope for individuals seeking help. Research isn’t just about dry statistics; it's about finding better ways to treat and support those facing dual diagnosis. By being informed about the latest breakthroughs, healthcare professionals can offer more effective, evidence-backed care, opening the door to improved treatment outcomes and a brighter future for those they serve. Beyond the individual level, this understanding has profound societal implications. It has the power to chip away at the walls of stigma that often surround mental health and substance use issues. Greater awareness and knowledge about the complexities of dual diagnosis can challenge stereotypes and biases, fostering a more compassionate and inclusive society. Additionally, society allocates resources based on research findings. When we understand the prevalence and evolving nature of dual diagnosis, policymakers and healthcare leaders can make informed decisions about where to channel resources most effectively. This ensures that the needs of individuals struggling with co-occurring disorders are not overlooked or under-prioritized. Moreover, research helps identify risk factors and early warning signs related to dual diagnosis. Armed with this information, we can develop prevention strategies and early intervention programs, potentially reducing the incidence of co-occurring disorders and mitigating their impact. Legal and criminal justice systems also stand to benefit. Understanding dual diagnosis trends can inform policies related to diversion programs, treatment alternatives to incarceration, and the rehabilitation of individuals with co-occurring disorders, potentially reducing rates of reoffending. Moreover, dual diagnosis research contributes to public health planning by highlighting the need for integrated mental health and addiction services. This knowledge can guide the development of comprehensive healthcare systems that offer holistic care to individuals with co-occurring disorders. Families and communities, too, are vital players in this narrative. With a grasp of research findings, they can provide informed, empathetic, and effective support to their loved ones, contributing to better outcomes.
The present research landscape analysis of dual diagnosis of SUDs and MHDs was conducted using a systematic approach to retrieve, process, and analyze relevant articles. The following methodology outlines the key steps taken to address the research questions:
Research Design The present study constitutes a thorough and robust analysis of the research landscape concerning the dual diagnosis of SUD and MHD. It's important to note that the research landscape analysis differs from traditional systematic or scoping reviews. In conducting research landscape analysis, we made deliberate methodological choices aimed at achieving both timely completion and unwavering research quality. These choices included a strategic decision to focus our search exclusively on a single comprehensive database, a departure from the customary practice of utilizing multiple databases. Furthermore, we streamlined the quality control process by assigning specific quality checks to a single author, rather than following the conventional dual-reviewer approach. This approach prioritized efficiency and expediency without compromising the rigor of our analysis. To expedite the research process further, we opted for a narrative synthesis instead of a quantitative one, ensuring that we provide a succinct yet highly informative summary of the available evidence. We place a premium on research transparency and, as such, are committed to sharing the detailed search string employed for data retrieval. This commitment underscores our dedication to fostering reproducibility and transparency in research practices.
Ethical considerations Since the research landscape analysis involved the use of existing and publicly available literature, and no human subjects were directly involved, no formal ethical approval was required.
Article retrieval Scopus, a comprehensive bibliographic database, was utilized to retrieve articles related to the dual diagnosis of SUDs and MHDs. Scopus is a multidisciplinary abstract and citation database that covers a wide range of scientific disciplines, including life sciences, physical sciences, social sciences, and health sciences. It includes content from thousands of scholarly journals.
Keywords used To optimize the search process and ensure the inclusion of pertinent articles, a set of relevant keywords and equivalent terms were employed. Keywords for “dual diagnosis” included dual diagnosis, co-occurring disorders, comorbid substance use, comorbid addiction, coexisting substance use, combined substance use, simultaneous substance use, substance use and psychiatric, co-occurring substance use and psychiatric, concurrent substance use and mental, coexisting addiction and mental, combined addiction and mental, simultaneous addiction and mental, substance-related and psychiatric, comorbid mental health and substance use, co-occurring substance use and psychiatric, concurrent mental health and substance use, coexisting mental health and substance use, combined mental health and substance use, simultaneous mental health and substance use, substance-related and coexisting psychiatric, comorbid psychiatric and substance abuse, co-occurring mental health and substance-related, concurrent psychiatric and substance use, coexisting psychiatric and substance abuse, combined psychiatric and substance use, simultaneous psychiatric and substance use, substance-related and concurrent mental, substance abuse comorbidity. Keywords for “Substance use disorders” included substance abuse, substance dependence, drug use disorders, addiction, substance-related disorders, drug abuse, opioid use disorder, cocaine use disorder, alcohol use disorder, substance misuse, substance use disorder, substance-related, substance addiction. Keywords for “Mental health disorders” included psychiatric disorders, mental illnesses, mental disorders, emotional disorders, psychological disorders, schizophrenia, depression, PTSD, ADHD, anxiety, bipolar disorder, eating disorders, personality disorders, mood disorders, psychotic disorders, mood and anxiety disorders, mental health conditions. To narrow down the search to focus specifically on dual diagnosis, we adopted a strategy that involved the simultaneous presence of SUDs and MHDs in the presence of specific keywords in the titles and abstracts such as “dual,” “co-occurring,” “concurrent,” “co-occurring disorders,” “dual disorders,” “dual diagnosis,” “comorbid psychiatric,” “cooccurring psychiatric,” “comorbid*,” and “coexisting”.
Inclusion and exclusion criteria To maintain the study’s focus and relevance, specific inclusion and exclusion criteria were applied. Included articles were required to be research article, written in English, and published in peer-reviewed journals up to December 31, 2022, Articles focusing on animal studies, internet addiction, obesity, pain, and validity of instruments and tools were excluded.
Flow chart of the search strategy Supplement 1 shows the overall search strategy and the number of articles retrieved in each step. The total number of research articles that met the inclusion and exclusion criteria were 935.
Validation of search strategy The effectiveness of our search strategy was rigorously assessed through three distinct methods, collectively demonstrating its ability to retrieve pertinent articles while minimizing false positives. First, to gauge precision, we meticulously examined a sample of 30 retrieved articles, scrutinizing their alignment with our research question and their contributions to the topic of dual diagnosis. This manual review revealed that the majority of the assessed articles were highly relevant to our research focus. Second, for a comprehensive evaluation, we compared the articles obtained through our search strategy with a set of randomly selected articles from another source. This set comprised 10 references sourced from Google Scholar [ 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ], and the aim was to determine if our strategy successfully identified articles selected at random from an alternative database. Impressively, our analysis showed that the search strategy had a notably high success rate in capturing these randomly selected articles. Lastly, to further corroborate the relevance of our retrieved articles, we investigated the research interests of the top 10 active authors and the subject scope of the top 10 active journals. This exploration confirmed that their areas of expertise and the journal scopes were in alignment with the field of mental health and/or substance use disorders. These three validation methods collectively reinforce the reliability of our search strategy, affirming that the vast majority of the retrieved articles are indeed pertinent to our research inquiry.
Data processing and mapping Data extracted from the selected articles were processed and organized using Microsoft Excel. Information on the titles/abstracts/author keywords, year of publication, journal name, authors, institution and country affiliation, and number of citations received by the article were extracted. To visualize and analyze the research landscape, VOSviewer, a bibliometric analysis tool, was employed [ 43 ]. This software enables mapping and clustering of co-occurring terms, authors, and countries, providing a comprehensive overview of the dual diagnosis research domain.
Interpreting VOSviewer maps and generating research topics
We conducted a rigorous analysis and generated a comprehensive research landscape using VOSviewer, a widely acclaimed software tool renowned for its expertise in mapping research domains. We seamlessly integrated pertinent data extracted from the Scopus database, including publication metadata, into VOSviewer to delve into the frequency of author keywords and terminologies. The resulting visualizations provided us with profound insights into the intricate web of interconnected research topics and their relationships within the field. Interpreting VOSviewer maps is akin to navigating a vibrant and interconnected tapestry of knowledge. Each term or keyword in the dataset is depicted as a point on the map, represented by a circle or node. These nodes come in varying sizes and colors and are interconnected by lines of differing thicknesses. The size of a node serves as an indicator of the term’s significance or prevalence within the dataset. Larger nodes denote that a specific term is frequently discussed or plays a pivotal role in the body of research, while smaller nodes signify less commonly mentioned concepts. The colors assigned to these nodes serve a dual purpose. Firstly, they facilitate the categorization of terms into thematic groups, with terms of the same color typically belonging to the same cluster or sharing a common thematic thread. Secondly, they aid in the identification of distinct research clusters or thematic groups within the dataset. For instance, a cluster of blue nodes might indicate that these terms are all associated with a particular area of research. The spatial proximity of nodes on the map reflects their closeness in meaning or concept. Nodes positioned closely together share a robust semantic or contextual connection and are likely to be co-mentioned in research articles or share a similar thematic focus. Conversely, nodes situated farther apart indicate less commonality in terms of their usage in the literature. The lines that link these nodes represent the relationships between terms. The thickness of these lines provides insights into the strength and frequency of these connections. Thick lines indicate that the linked terms are frequently discussed together or exhibit a robust thematic association, while thinner lines imply weaker or less frequent connections. In essence, VOSviewer maps offer a visual narrative of the underlying structure and relationships within your dataset. By examining node size and color, you can pinpoint pivotal terms and thematic clusters. Simultaneously, analyzing the distance between nodes and line thickness unveils the semantic closeness and strength of associations between terms. These visual insights are invaluable for researchers seeking to unearth key concepts, identify research clusters, and track emerging trends within their field of study.
Growth pattern, active countries, and active journals
The growth pattern of the 935 research articles on dual diagnosis of substance use disorders and mental health disorders shows an increasing trend in the number of published articles over the years. Starting from the late 1980s and early 1990s with only a few publications, the research interest gradually picked up momentum, and the number of articles has been consistently rising since the mid-1990s. Table 1 shows the number of articles published in three different periods. The majority of publications (52.2%) were produced between 2003 and 2012, indicating a significant surge in research during that decade. The subsequent period from 2013 to 2022 saw a continued interest in the subject, accounting for 35.5% of the total publications. The number of articles published per year during the period from 2013 to 2022 showed a fluctuating steady state with an average of approximately 33 articles per year. The earliest period from 1983 to 2002 comprised 12.3% of the total publications, reflecting the initial stages of research and the gradual development of interest in the field.
Out of the total 935 publications, the United States contributed the most with 585 publications, accounting for approximately 62.5% of the total research output. Canada follows with 88 publications, making up around 9.4% of the total. The United Kingdom and Australia also made substantial contributions with 70 and 53 publications, accounting for 7.5 and 5.7%, respectively. Table 2 shows the top 10 active countries.
Based on the list of top active journals in the field of dual diagnosis of substance use and mental health disorders, it is evident that there are several reputable and specialized journals that focus on this important area of research (Table 3 ). These journals cover a wide range of topics related to dual diagnosis, including comorbidity, treatment approaches, intervention strategies, and epidemiological studies. The Journal of Dual Diagnosis appears to be a leading and comprehensive platform for research on dual diagnosis. It covers a broad spectrum of studies related to substance use disorders and mental health conditions. The Journal of Substance Abuse Treatment ranked second while the Mental Health and Substance Use Dual Diagnosis journal ranked third and seems to be dedicated specifically to the intersection of substance use disorder and mental health disorders, providing valuable insights and research findings related to comorbidities and integrated treatment approaches.
Most frequent author keywords
Mapping author keywords with a minimum occurrence of five (n = 96) provides insights in research related to dual diagnosis. Figure 1 shows the 96 author keywords and their links with other keywords. The number of occurrences represent the number of times each author keyword appears in the dataset, while the total link strength (TLS) indicates the combined strength of connections between keywords based on their co-occurrence patterns. The most frequent author keywords with high occurrences and TLS represent the key areas of focus in research on the dual diagnosis of substance use and mental health disorders.
“Comorbidity” is the most frequent keyword, with 144 occurrences and a high TLS of 356. This reflects the central theme of exploring the co-occurrence of substance use disorders and mental health conditions and their complex relationship. “Substance use disorder” and “dual diagnosis” are also highly prevalent keywords with 122 and 101 occurrences, respectively. These terms highlight the primary focus on studying individuals with both substance use disorders and mental health disorders, underscoring the significance of dual diagnosis in research. “Co-occurring disorders” and “substance use disorders” are frequently used, indicating a focus on understanding the relationship between different types of disorders and the impact of substance use on mental health. Several specific mental health disorders such as “schizophrenia,” “depression,” “bipolar disorder,” and “PTSD” are prominent keywords, indicating a strong emphasis on exploring the comorbidity of these disorders with substance use. “Mental health” and “mental illness” are relevant keywords, reflecting the broader context of research on mental health conditions and their interaction with substance use. “Treatment” is a significant keyword with 34 occurrences, indicating a focus on investigating effective interventions and treatment approaches for individuals with dual diagnosis. “Addiction” and “recovery” are important keywords, highlighting the interest in understanding the addictive nature of substance use and the potential for recovery in this population. The mention of “veterans” as a keyword suggests a specific focus on the dual diagnosis of substance use and mental health disorders in the veteran population. “Integrated treatment” is an important keyword, indicating an interest in studying treatment approaches that address both substance use and mental health disorders together in an integrated manner.
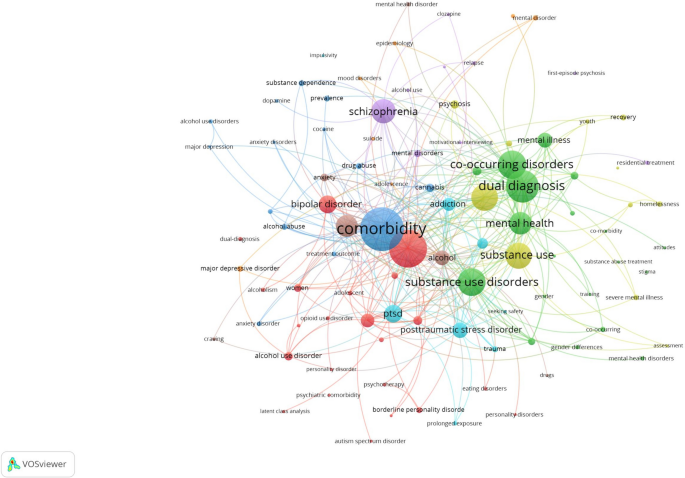
Network visualization map of author keywords with a minimum occurrence of five in the retrieved articles on dual diagnosis of substance use and mental health disorders
Most impactful research topics
To have an insight into the most impactful research topics on dual diagnosis, the top 100 research articles were visualized and the terms with the largest node size and TLS were used to. To come up with the five most common investigated research topics:
Dual diagnosis and comorbidity of SUDs and MHDs: This topic focuses on the co-occurrence of substance use disorders and various mental health conditions, such as schizophrenia, bipolar disorder, PTSD, anxiety disorders, and major depressive disorder. This research topic explored the prevalence, characteristics, and consequences of comorbidity in different populations, including veterans, adolescents, and individuals experiencing homelessness [ 13 , 19 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 ].
Treatment and interventions for co-occurring disorders: This topic involves studies on different treatment approaches and interventions for individuals with dual diagnosis. These interventions may include motivational interviewing, cognitive-behavioral therapy, family intervention, integrated treatment models, assertive community treatment, and prolonged exposure therapy. The goal is to improve treatment outcomes and recovery for individuals with co-occurring substance use and mental health disorders [ 48 , 53 , 54 , 55 , 56 , 57 , 58 , 59 ].
Quality of life and functioning in individuals with dual diagnosis: This research topic explores the impact of dual diagnosis on the quality of life and functioning of affected individuals. It assesses the relationship between dual diagnosis and various aspects of well-being, including social functioning, physical health, and overall quality of life [ 60 , 61 , 62 , 63 , 64 ].
Epidemiology and prevalence of co-occurring disorders: This topic involves population-based studies that investigate the prevalence of comorbid substance use and mental health disorders. It examines the demographic and clinical correlates of dual diagnosis, as well as risk factors associated with the development of co-occurring conditions [ 50 , 52 , 60 , 65 , 66 , 67 ].
Implications and consequences of comorbidity: This research topic explores the consequences of comorbidity between substance use and mental health disorders, such as treatment utilization, service access barriers, criminal recidivism, and the impact on suicidality. It also investigates the implications of comorbidity for treatment outcomes and the potential risks associated with specific comorbidities [ 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 ].
Emerging research topics
Upon scrutinizing the titles, abstracts, author keywords, and a visualization map of the 100 recently published articles, the research themes listed below came to the forefront. It’s worth noting that some of the research themes in the 100 recently published articles were not groundbreaking; rather, they represented a natural progression of ongoing research endeavors, and that is why they were not listed as emerging research themes. For instance, there was a continuation of research into the prevalence and epidemiology of co-occurring mental illnesses and substance use disorders and characteristics of various cases of co-morbid cases of SUDs and MHDs. The list below included such emergent themes. It might seem that certain aspects within these research themes duplicate the initial research topics, but it’s crucial to emphasize that this is not the case. For example, both themes delve into investigations concerning treatment, yet the differentiation lies in the treatment approach adopted.
Neurobiological and psychosocial aspects of dual diagnosis: This research topic focuses on exploring the neurobiological etiology and underlying mechanisms of comorbid substance use and mental health disorders. It investigates brain regions, neurotransmitter systems, hormonal pathways, and other neurobiological factors contributing to the development and maintenance of dual diagnosis. Additionally, this topic may examine psychosocial aspects, such as trauma exposure, adverse childhood experiences, and social support, that interact with neurobiological factors in the context of comorbidity [ 76 ].
Impact of environmental and sociocultural factors on dual diagnosis: This research topic delves into the influence of environmental and sociocultural factors on the occurrence and course of comorbid substance use and mental health disorders. It may explore how cultural norms, socioeconomic status, access to healthcare, and societal attitudes toward mental health and substance use affect the prevalence, treatment outcomes, and quality of life of individuals with dual diagnosis [ 77 , 78 ].
New interventions and treatment approaches for dual diagnosis: This topic involves studies that propose and evaluate innovative interventions and treatment approaches for individuals with dual diagnosis. These interventions may include novel psychotherapeutic techniques, pharmacological treatments, digital health interventions, and integrated care models. The research aims to improve treatment effectiveness, adherence, and long-term recovery outcomes in individuals with comorbid substance use and mental health disorders [ 79 , 80 , 81 , 82 , 83 , 84 ].
Mental health and substance use in special populations with dual diagnosis: This research topic focuses on exploring the prevalence and unique characteristics of comorbid substance use and mental health disorders in specific populations, such as individuals with eating disorders, incarcerated individuals, and people with autism spectrum disorder. It aims to identify the specific needs and challenges faced by these populations and develop tailored interventions to address their dual diagnosis [ 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 ].
Public health implications and policy interventions for dual diagnosis: This topic involves research that addresses the public health implications of dual diagnosis and the need for policy interventions to address this complex issue. It may include studies on the economic burden of comorbidity, the impact on healthcare systems, and the evaluation of policy initiatives aimed at improving prevention, early intervention, and access to integrated care for individuals with dual diagnosis [ 81 , 96 , 97 , 98 , 99 , 100 , 101 ].
Comparison in research topics
The comparison between the most impactful research topics and emerging research topics in the field of dual diagnosis reveals intriguing insights into the evolving landscape of this critical area of study (Table 4 ). In the most impactful research topics, there is a strong emphasis on the epidemiology of dual diagnosis, indicating a well-established foundation in understanding the prevalence, characteristics, and consequences of comorbid SUDs and MHDs. Treatment and interventions also receive considerable attention, highlighting the ongoing efforts to improve outcomes and recovery for individuals with dual diagnosis. Quality of life and medical consequences are additional focal points, reflecting the concern for the holistic well-being of affected individuals and the health-related implications of comorbidity.
On the other hand, emerging research topics signify a shift towards newer methods and interventions. The exploration of neurobiology in the context of dual diagnosis reflects a growing interest in unraveling the underlying neurobiological mechanisms contributing to comorbidity. This shift suggests a deeper understanding of the neural pathways and potential targets for intervention. The consideration of dual diagnosis in special groups underscores a recognition of the unique needs and challenges faced by specific populations, such as individuals with autism spectrum disorder. This tailored approach acknowledges that one size does not fit all in addressing dual diagnosis. Finally, the exploration of environmental and psychosocial contexts highlights the importance of socio-cultural factors, policy interventions, and societal attitudes in shaping the experience of individuals with dual diagnosis, signaling a broader perspective that extends beyond clinical interventions. In summary, while the most impactful research topics have laid a strong foundation in epidemiology, treatment, quality of life, and medical consequences, the emerging research topics point to a promising future with a deeper dive into the neurobiology of dual diagnosis, a focus on special populations, and a broader consideration of the environmental and psychosocial context. This evolution reflects the dynamic nature of dual diagnosis research as it strives to advance our understanding and improve the lives of those affected by comorbid substance use and mental health disorders.
The main hypothesis underlying the study was that dual diagnosis, or the comorbidity of SUDs and MHDs, was historically underrecognized and under-researched. Over time, however, there has been a significant increase in understanding, appreciation, and research into this complex interplay in clinical settings. This was expected to manifest through a growing number of publications, increased attention to integrated treatment approaches, and a heightened recognition of the complexities and public health implications associated with dual diagnosis. The study aims to analyze this progression and its implications through a research landscape analysis, identifying key trends, knowledge gaps, and research priorities. The research landscape analysis of the dual diagnosis of SUDs and MHDs has unveiled a substantial and evolving body of knowledge, with a notable rise in publications since the mid-1990s and a significant surge between 2003 and 2012. This growing research interest underscores the increasing recognition of the importance and complexity of dual diagnosis in clinical and public health contexts. The United States has emerged as the most active contributor, followed by Canada, the United Kingdom, and Australia, with specialized journals such as the Journal of Dual Diagnosis playing a pivotal role in disseminating research findings. Common keywords such as “comorbidity,” “substance use disorder,” “dual diagnosis,” and specific mental health disorders highlight the primary focus areas, with impactful research topics identified as the comorbidity of SUDs and MHDs, treatment and interventions, quality of life, epidemiology, and the implications of comorbidity. Emerging research themes emphasize neurobiological and psychosocial aspects, the impact of environmental and sociocultural factors, innovative treatment approaches, and the needs of special populations with dual diagnosis, reflecting a shift towards a more holistic and nuanced understanding. The study highlights a shift from traditional epidemiological studies towards understanding the underlying mechanisms and broader social determinants of dual diagnosis, with a need for continued research into integrated treatment models, specific needs of diverse populations, and the development of tailored interventions.
The findings of this research landscape analysis have significant implications for clinical practice, public health initiatives, policy development, and future research endeavors. Clinicians and healthcare providers working with individuals with dual diagnosis can benefit from the identified research hotspots, as they highlight crucial aspects that require attention in diagnosis, treatment, and support. The prominence of treatment and intervention topics indicates the need for evidence-based integrated approaches that address both substance use and mental health disorders concurrently [ 102 , 103 , 104 ]. The research on the impact of dual diagnosis on quality of life and functioning underscores the importance of holistic care that addresses psychosocial and functional well-being [ 63 ]. For public health initiatives, understanding the prevalence and epidemiological aspects of dual diagnosis is vital for resource allocation and the development of effective prevention and early intervention programs. Policymakers can use the research landscape analysis to inform policies that promote integrated care, reduce barriers to treatment, and improve access to mental health and substance abuse services [ 15 , 105 ]. Furthermore, the identification of emerging topics offers opportunities for investment in research areas that are gaining momentum and importance.
The present study lays a robust groundwork, serving as a catalyst for the advancement of research initiatives and the formulation of comprehensive policies and programs aimed at elevating the quality of life for individuals grappling with the intricate confluence of SUDs and MHDs. Within the realm of significance, it underscores a critical imperative—the urgent necessity to revolutionize the landscape of tailored mental health services offered to patients harboring this challenging comorbidity. The paper distinctly illuminates the exigency for a heightened quantity of research endeavors that delve deeper into unraveling the temporal intricacies underpinning the relationship between SUDs and MHDs. In so doing, it not only unveils potential risk factors but also delves into the far-reaching consequences of treatment modalities over the extended course of time. This illumination, therefore, not only beckons but virtually ushers in a promising trajectory for prospective research endeavors, a path designed to uncover the intricate and evolving journey of dual diagnosis. A profound implication of this study is the direct applicability of its findings in the corridors of policymaking. By leveraging the insights encapsulated within the paper, policymakers stand uniquely equipped to sculpt policies that unequivocally champion the cause of integrated care. The remarkable emphasis on themes of treatment and intervention, permeating the research's core, emphatically underscores the urgent demand for dismantling barriers obstructing access to mental health and substance abuse services. It is incumbent upon policymakers to heed this call, for policies fostering the integration of care can inexorably elevate the outcomes experienced by patients grappling with dual diagnosis. Furthermore, this study artfully directs policymakers to allocate their resources judiciously by identifying burgeoning areas of research that are surging in prominence and pertinence. These emergent topics, discerned within the study, are not just topics; they are emblematic of windows of opportunity. By investing in these areas, policymakers can tangibly bolster research initiatives that are primed to tackle the multifaceted challenges inherent in the realm of dual diagnosis, addressing both current exigencies and future prospects. Additionally, the paper furnishes the foundational blueprint essential for the development of screening guidelines and clinical practice protocols that truly grasp the complexity of dual diagnosis. Clinical practitioners and healthcare establishments would be remiss not to harness this invaluable information to augment their own practices, thereby delivering more effective and empathetic care to individuals contending with dual diagnosis. In essence, this study serves as the compass guiding the way toward a more compassionate, comprehensive, and efficacious approach to mental health and substance abuse care for those in need.
The current landscape analysis of reveals significant implications and highlights the growing research interest in this field since the late 1980s. This increasing trend underscores the complexities and prevalence of comorbid conditions, which necessitate focused research and intervention strategies. The results can be generalized to guide future research priorities, inform clinical guidelines, shape healthcare policies, and provide a framework for other countries to adapt and build upon in their context.
The key take-home message emphasizes the importance of recognizing the high prevalence and intricate relationship between SUDs and MHDs, necessitating integrated and tailored treatment approaches. Additionally, the study advocates for employing efficient research methodologies to synthesize vast amounts of literature and identify emerging trends, focusing on quality of life, treatment outcomes, and the broader socio-cultural and policy contexts to improve care and support for individuals with dual diagnosis. Finally, the research underscores the critical need for continued focus on dual diagnosis, advocating for comprehensive, integrated, and innovative approaches to research, clinical practice, and policymaking to improve outcomes for affected individuals.
Despite the comprehensive approach adopted in this research landscape analysis, several limitations must be acknowledged. The exclusive reliance on Scopus, while extensive, inherently limits the scope of the analysis, potentially omitting relevant articles indexed in other databases such as the Chinese scientific database, thus not fully representing the entire research landscape on dual diagnosis of SUDs and MHDs. Assigning quality control responsibilities to a single author, rather than employing a dual-reviewer system, may introduce bias and affect the reliability of the quality assessment. Although this approach was chosen to expedite the process, it might have compromised the thoroughness of quality checks. The use of narrative synthesis instead of a quantitative synthesis limits the ability to perform meta-analytical calculations that could provide more robust statistical insights. This choice was made for efficiency, but it may affect the depth of the analysis and the generalizability of the conclusions. The reliance on specific keywords to retrieve articles means that any relevant studies not containing these exact terms in their titles or abstracts may have been overlooked, potentially leading to an incomplete representation of the research domain. The restriction to English-language articles and peer-reviewed journals may exclude significant research published in other languages or in non-peer-reviewed formats, introducing linguistic and publication type bias that could skew the results towards predominantly English-speaking regions and established academic journals. The inclusion of articles up to December 31, 2022, means that any significant research published after this date is not considered, potentially missing the latest developments in the field. The validation of the search strategy using a small sample of 30 articles and a comparison with 10 randomly selected articles from Google Scholar may not be sufficient to comprehensively assess the effectiveness of the search strategy; a larger sample size might provide a more accurate validation. Some of the research topics and findings may be specific to particular populations (e.g., veterans) and might not be generalizable to other groups, highlighting the need for caution when extrapolating the results to broader contexts. Although no formal ethical approval was required due to the use of existing literature, ethical considerations related to the interpretation and application of findings must still be acknowledged, particularly in terms of representing vulnerable populations accurately and sensitively. Acknowledging these limitations is crucial for interpreting the findings of this research landscape analysis and for guiding future research efforts to address these gaps and enhance the robustness and comprehensiveness of studies on the dual diagnosis of SUDs and MHDs.
In conclusion, the research landscape analysis of dual diagnosis of substance abuse and mental health disorders provides valuable insights into the growth, active countries, and active journals in this field. The identification of research hotspots and emerging topics informs the scientific community about prevailing interests and potential areas for future investigation. Addressing research gaps can lead to a more comprehensive understanding of dual diagnosis, while the implications of the findings extend to clinical practice, public health initiatives, policy development, and future research priorities. This comprehensive understanding is crucial in advancing knowledge, improving care, and addressing the multifaceted challenges posed by dual diagnosis to individuals and society.
Availability of data and materials
All data presented in this manuscript are available on the Scopus database using the search query listed in the methodology section.
Hasin DS, O’Brien CP, Auriacombe M, Borges G, Bucholz K, Budney A, et al. DSM-5 criteria for substance use disorders: recommendations and rationale. Am J Psychiatry. 2013;170(8):834–51. https://doi.org/10.1176/appi.ajp.2013.12060782 .
Article PubMed PubMed Central Google Scholar
Collaborators GA. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2018;392(10152):1015–35. https://doi.org/10.1016/s0140-6736(18)31310-2 .
Article Google Scholar
Ayalew M, Tafere M, Asmare Y. Prevalence, trends, and consequences of substance use among university students: implication for intervention. Int Q Community Health Educ. 2018;38(3):169–73. https://doi.org/10.1177/0272684x17749570 .
Article PubMed Google Scholar
Raftery D, Kelly PJ, Deane FP, Baker AL, Ingram I, Goh MCW, et al. Insight in substance use disorder: a systematic review of the literature. Addict Behav. 2020;111:106549. https://doi.org/10.1016/j.addbeh.2020.106549 .
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. https://doi.org/10.1001/archpsyc.62.6.593 .
Hossain MM, Nesa F, Das J, Aggad R, Tasnim S, Bairwa M, et al. Global burden of mental health problems among children and adolescents during COVID-19 pandemic: an umbrella review. Psychiatry Res. 2022;317:114814. https://doi.org/10.1016/j.psychres.2022.114814 .
Article CAS PubMed PubMed Central Google Scholar
Kurdyak P, Patten S. The burden of mental illness and evidence-informed mental health policy development. Can J Psychiatry. 2022;67(2):104–6. https://doi.org/10.1177/07067437211021299 .
Stumbrys D, Jasilionis D, Pūras D. The burden of mental health-related mortality in the Baltic States in 2007–2018. BMC Public Health. 2022;22(1):1776. https://doi.org/10.1186/s12889-022-14175-9 .
Pompili M, Innamorati M, Gonda X, Serafini G, Sarno S, Erbuto D, et al. Affective temperaments and hopelessness as predictors of health and social functioning in mood disorder patients: a prospective follow-up study. J Affect Disord. 2013;150(2):216–22. https://doi.org/10.1016/j.jad.2013.03.026 .
Costanza A, Vasileios C, Ambrosetti J, Shah S, Amerio A, Aguglia A, et al. Demoralization in suicide: a systematic review. J Psychosom Res. 2022;157:110788. https://doi.org/10.1016/j.jpsychores.2022.110788 .
Arias F, Szerman N, Vega P, Mesías B, Basurte I, Rentero D. Bipolar disorder and substance use disorders. Madrid study on the prevalence of dual disorders/pathology. Adicciones. 2017;29(3):186–94. https://doi.org/10.2088/adicciones.782 .
Brewer S, Godley MD, Hulvershorn LA. Treating mental health and substance use disorders in adolescents: what is on the menu? Curr Psychiatry Rep. 2017;19(1):5. https://doi.org/10.1007/s11920-017-0755-0 .
Jones CM, McCance-Katz EF. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend. 2019;197:78–82. https://doi.org/10.1016/j.drugalcdep.2018.12.030 .
Murthy P, Mahadevan J, Chand PK. Treatment of substance use disorders with co-occurring severe mental health disorders. Curr Opin Psychiatry. 2019;32(4):293–9. https://doi.org/10.1097/yco.0000000000000510 .
Saddichha S, Schütz CG, Sinha BN, Manjunatha N. Substance use and dual diagnosis disorders: future epidemiology, determinants, and policies. Biomed Res Int. 2015;2015:145905. https://doi.org/10.1155/2015/145905 .
Hammen C. Adolescent depression: stressful interpersonal contexts and risk for recurrence. Curr Dir Psychol Sci. 2009;18(4):200–4. https://doi.org/10.1111/j.1467-8721.2009.01636.x .
Wolitzky-Taylor K, Bobova L, Zinbarg RE, Mineka S, Craske MG. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addict Behav. 2012;37(8):982–5. https://doi.org/10.1016/j.addbeh.2012.03.026 .
Mueser KT, Drake RE, Wallach MA. Dual diagnosis: a review of etiological theories. Addict Behav. 1998;23(6):717–34.
Article CAS PubMed Google Scholar
Hartz SM, Pato CN, Medeiros H, Cavazos-Rehg P, Sobell JL, Knowles JA, et al. Comorbidity of severe psychotic disorders with measures of substance use. JAMA Psychiat. 2014;71(3):248–54. https://doi.org/10.1001/jamapsychiatry.2013.3726 .
Carroll KM, Kiluk BD, Nich C, Babuscio TA, Brewer JA, Potenza MN, et al. Cognitive function and treatment response in a randomized clinical trial of computer-based training in cognitive-behavioral therapy. Subst Use Misuse. 2011;46(1):23–34. https://doi.org/10.3109/10826084.2011.521069 .
Drake RE, Mueser KT. Psychosocial approaches to dual diagnosis. Schizophr Bull. 2000;26(1):105–18. https://doi.org/10.1093/oxfordjournals.schbul.a033429 .
Ruggeri M, Leese M, Thornicroft G, Bisoffi G, Tansella M. Definition and prevalence of severe and persistent mental illness. Br J Psychiatry. 2000;177:149–55. https://doi.org/10.1192/bjp.177.2.149 .
Reavley NJ, Jorm AF. Stigmatizing attitudes towards people with mental disorders: findings from an Australian national survey of mental health literacy and stigma. Aust N Z J Psychiatry. 2011;45(12):1086–93. https://doi.org/10.3109/00048674.2011.621061 .
Torrey WC, Tepper M, Greenwold J. Implementing integrated services for adults with co-occurring substance use disorders and psychiatric illnesses: a research review. J Dual Diagn. 2011;7(3):150–61. https://doi.org/10.1080/15504263.2011.592769 .
Bouchery EE, Harwood HJ, Dilonardo J, Vandivort-Warren R. Type of health insurance and the substance abuse treatment gap. J Subst Abuse Treat. 2012;42(3):289–300. https://doi.org/10.1016/j.jsat.2011.09.002 .
Abuse S, Administration MHS. National Mental Health Services Survey (N-MHSS): 2014. Data on mental health treatment facilities. Department of Health and Human Services, Substance Abuse and Mental Health …; 2014.
Shiner B, Gottlieb D, Rice K, Forehand JA, Snitkin M, Watts BV. Evaluating policies to improve access to mental health services in rural areas. J Rural Health. 2022;38(4):805–16. https://doi.org/10.1111/jrh.12674 .
Ioannidis JP, Greenland S, Hlatky MA, Khoury MJ, Macleod MR, Moher D, et al. Increasing value and reducing waste in research design, conduct, and analysis. Lancet. 2014;383(9912):166–75. https://doi.org/10.1016/s0140-6736(13)62227-8 .
Bornmann L, Bowman BF, Bauer J, Marx W, Schier H, Palzenberger MJBbHmiosi. (2014): 11 Bibliometric standards for evaluating research institutes in the natural sciences.201.
Hicks D, Wouters P, Waltman L, de Rijcke S, Rafols I. Bibliometrics: the Leiden manifesto for research metrics. Nature. 2015;520(7548):429–31. https://doi.org/10.1038/520429a .
Ziedonis D, Brady K. Dual diagnosis in primary care. Detecting and treating both the addiction and mental illness. Med Clin North Am. 1997;81(4):1017–36. https://doi.org/10.1016/s0025-7125(05)70561-7 .
Kim JI, Kim B, Kim BN, Hong SB, Lee DW, Chung JY, et al. Prevalence of psychiatric disorders, comorbidity patterns, and repeat offending among male juvenile detainees in South Korea: a cross-sectional study. Child Adolesc Psychiatry Ment Health. 2017;11:6. https://doi.org/10.1186/s13034-017-0143-x .
Astals M, Domingo-Salvany A, Buenaventura CC, Tato J, Vazquez JM, Martín-Santos R, et al. Impact of substance dependence and dual diagnosis on the quality of life of heroin users seeking treatment. Subst Use Misuse. 2008;43(5):612–32. https://doi.org/10.1080/10826080701204813 .
Buckley PF. Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. J Clin Psychiatry. 2006;67(Suppl 7):5–9.
PubMed Google Scholar
Buckley PF, Brown ES. Prevalence and consequences of dual diagnosis. J Clin Psychiatry. 2006;67(7):e01. https://doi.org/10.4088/jcp.0706e01 .
Canaway R, Merkes M. Barriers to comorbidity service delivery: the complexities of dual diagnosis and the need to agree on terminology and conceptual frameworks. Aust Health Rev. 2010;34(3):262–8. https://doi.org/10.1071/ah08723 .
Edward KL, Munro I. Nursing considerations for dual diagnosis in mental health. Int J Nurs Pract. 2009;15(2):74–9. https://doi.org/10.1111/j.1440-172X.2009.01731.x .
Healey C, Peters S, Kinderman P, McCracken C, Morriss R. Reasons for substance use in dual diagnosis bipolar disorder and substance use disorders: a qualitative study. J Affect Disord. 2009;113(1–2):118–26. https://doi.org/10.1016/j.jad.2008.05.010 .
Horsfall J, Cleary M, Hunt GE, Walter G. Psychosocial treatments for people with co-occurring severe mental illnesses and substance use disorders (dual diagnosis): a review of empirical evidence. Harv Rev Psychiatry. 2009;17(1):24–34. https://doi.org/10.1080/10673220902724599 .
Kerfoot KE, Petrakis IL, Rosenheck RA. Dual diagnosis in an aging population: prevalence of psychiatric disorders, comorbid substance abuse, and mental health service utilization in the department of veterans affairs. J Dual Diagn. 2011;7(1–2):4–13. https://doi.org/10.1080/15504263.2011.568306 .
Morojele NK, Saban A, Seedat S. Clinical presentations and diagnostic issues in dual diagnosis disorders. Curr Opin Psychiatry. 2012;25(3):181–6. https://doi.org/10.1097/YCO.0b013e328351a429 .
Thylstrup B, Johansen KS. Dual diagnosis and psychosocial interventions–introduction and commentary. Nord J Psychiatry. 2009;63(3):202–8. https://doi.org/10.1080/08039480802571069 .
van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–38. https://doi.org/10.1007/s11192-009-0146-3 .
Arndt S, Tyrrell G, Flaum M, Andreasen NC. Comorbidity of substance abuse and schizophrenia: the role of pre-morbid adjustment. Psychol Med. 1992;22(2):379–88. https://doi.org/10.1017/S0033291700030324 .
Barnes TRE, Mutsatsa SH, Hutton SB, Watt HC, Joyce EM. Comorbid substance use and age at onset of schizophrenia. Br J Psychiatry. 2006;188:237–42. https://doi.org/10.1192/bjp.bp.104.007237 .
Brady KT, Killeen T, Saladin ME, Dansky B, Becker S. Comorbid substance abuse and posttraumatic stress disorder: characteristics of women in treatment. Am J Addict. 1994;3(2):160–4. https://doi.org/10.1111/j.1521-0391.1994.tb00383.x .
Brière FN, Rohde P, Seeley JR, Klein D, Lewinsohn PM. Comorbidity between major depression and alcohol use disorder from adolescence to adulthood. Compr Psychiatry. 2014;55(3):526–33. https://doi.org/10.1016/j.comppsych.2013.10.007 .
Brown PJ, Stout RL, Mueller T. Substance use disorder and posttraumatic stress disorder comorbidity: addiction and psychiatric treatment rates. Psychol Addict Behav. 1999;13(2):115–22. https://doi.org/10.1037/0893-164X.13.2.115 .
Bulik CM, Klump KL, Thornton L, Kaplan AS, Devlin B, Fichter MM, et al. Alcohol use disorder comorbidity in eating disorders: a multicenter study. J Clin Psychiatry. 2004;65(7):1000–6. https://doi.org/10.4088/JCP.v65n0718 .
Compton WM, Conway KP, Stinson FS, Grant BF. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991–1992 and 2001–2002. Am J Psychiatry. 2006;163(12):2141–7. https://doi.org/10.1176/ajp.2006.163.12.2141 .
Green AI, Drake RE, Brunette MF, Noordsy DL. Schizophrenia and co-occurring substance use disorder. Am J Psychiatry. 2007;164(3):402–8. https://doi.org/10.1176/ajp.2007.164.3.402 .
Morgenstern J, Langenbucher J, Labouvie E, Miller KJ. The comorbidity of alcoholism and personality disorders in a clinical population: prevalence rates and relation to alcohol typology variables. J Abnorm Psychol. 1997;106(1):74–84. https://doi.org/10.1037/0021-843X.106.1.74 .
Back SE, Waldrop AE, Brady KT. Treatment challenges associated with comorbid substance use and posttraumatic stress disorder: clinicians’ perspectives. Am J Addict. 2009;18(1):15–20. https://doi.org/10.1080/10550490802545141 .
Brown PJ, Recupero PR, Stout R. PTSD substance abuse comorbidity and treatment utilization. Addict Behav. 1995;20(2):251–4. https://doi.org/10.1016/0306-4603(94)00060-3 .
Harris KM, Edlund MJ. Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatr Serv. 2005;56(8):954–9. https://doi.org/10.1176/appi.ps.56.8.954 .
Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. Am J Psychiatry. 2004;161(8):1426–32. https://doi.org/10.1176/appi.ajp.161.8.1426 .
Manwani SG, Szilagyi KA, Zablotsky B, Hennen J, Griffin ML, Weiss RD. Adherence to pharmacotherapy in bipolar disorder patients with and without co-occurring substance use disorders. J Clin Psychiatry. 2007;68(8):1172–6. https://doi.org/10.4088/JCP.v68n0802 .
Minkoff K. An integrated treatment model for dual diagnosis of psychosis and addiction. Hosp Community Psychiatry. 1989;40(10):1031–6. https://doi.org/10.1176/ps.40.10.1031 .
Smith JP, Book SW. Comorbidity of generalized anxiety disorder and alcohol use disorders among individuals seeking outpatient substance abuse treatment. Addict Behav. 2010;35(1):42–5. https://doi.org/10.1016/j.addbeh.2009.07.002 .
Kamali M, Kelly L, Gervin M, Browne S, Larkin C, O’Callaghan E. The prevalence of comorbid substance misuse and its influence on suicidal ideation among in-patients with schizophrenia. Acta Psychiatr Scand. 2000;101(6):452–6. https://doi.org/10.1034/j.1600-0447.2000.101006452.x .
Padgett DK, Gulcur L, Tsemberis S. Housing first services for people who are homeless with co-occurring serious mental illness and substance abuse. Res Soc Work Pract. 2006;16(1):74–83. https://doi.org/10.1177/1049731505282593 .
Schmidt LM, Hesse M, Lykke J. The impact of substance use disorders on the course of schizophrenia-A 15-year follow-up study. Dual diagnosis over 15 years. Schizophr Res. 2011;130(1–3):228–33. https://doi.org/10.1016/j.schres.2011.04.011 .
Singh J, Mattoo SK, Sharan P, Basu D. Quality of life and its correlates in patients with dual diagnosis of bipolar affective disorder and substance dependence. Bipolar Disord. 2005;7(2):187–91. https://doi.org/10.1111/j.1399-5618.2004.00173.x .
Urboanoski KA, Cairney J, Bassani DG, Rush BR. Perceived unmet need for mental health care for Canadians with co-occurring mental and substance use disorders. Psychiatr Serv. 2008;59(3):283–9. https://doi.org/10.1176/appi.ps.59.3.283 .
Kingston REF, Marel C, Mills KL. A systematic review of the prevalence of comorbid mental health disorders in people presenting for substance use treatment in Australia. Drug Alcohol Rev. 2017;36(4):527–39. https://doi.org/10.1111/dar.12448 .
Klinkenberg WD, Caslyn RJ, Morse GA, Yonker RD, McCudden S, Ketema F, et al. Prevalence of human immunodeficiency virus, hepatitis B, and hepatitis C among homeless persons with co-occurring severe mental illness and substance use disorders. Compr Psychiatry. 2003;44(4):293–302. https://doi.org/10.1016/S0010-440X(03)00094-4 .
Wallace C, Mullen PE, Burgess P. Criminal offending in schizophrenia over a 25-year period marked by deinstitutionalization and increasing prevalence of comorbid substance use disorders. Am J Psychiatry. 2004;161(4):716–27. https://doi.org/10.1176/appi.ajp.161.4.716 .
Bronisch T, Wittchen HU. Suicidal ideation and suicide attempts: comorbidity with depression, anxiety disorders, and substance abuse disorder. Eur Arch Psychiatry Clin Neurosci. 1994;244(2):93–8. https://doi.org/10.1007/BF02193525 .
Hatzenbuehler ML, Keyes KM, Narrow WE, Grant BF, Hasin DS. Racial/ethnic disparities in service utilization for individuals with co-occurring mental health and substance use disorders in the general population: Results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2008;69(7):1112–21. https://doi.org/10.4088/JCP.v69n0711 .
Hodgins S, Tiihonen J, Ross D. The consequences of conduct disorder for males who develop schizophrenia: associations with criminality, aggressive behavior, substance use, and psychiatric services. Schizophr Res. 2005;78(2–3):323–35. https://doi.org/10.1016/j.schres.2005.05.021 .
Hunt GE, Bergen J, Bashir M. Medication compliance and comorbid substance abuse in schizophrenia: impact on community survival 4 years after a relapse. Schizophr Res. 2002;54(3):253–64. https://doi.org/10.1016/S0920-9964(01)00261-4 .
Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38(2):177–90. https://doi.org/10.2307/2955424 .
Priester MA, Browne T, Iachini A, Clone S, DeHart D, Seay KD. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: an integrative literature review. J Subst Abuse Treat. 2016;61:47–59. https://doi.org/10.1016/j.jsat.2015.09.006 .
Talamo A, Centorrino F, Tondo L, Dimitri A, Hennen J, Baldessarini RJ. Comorbid substance-use in schizophrenia: relation to positive and negative symptoms. Schizophr Res. 2006;86(1–3):251–5. https://doi.org/10.1016/j.schres.2006.04.004 .
Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatr Serv. 2005;56(7):823–8. https://doi.org/10.1176/appi.ps.56.7.823 .
Hinckley JD, Danielson CK. Elucidating the neurobiologic etiology of comorbid PTSD and substance use disorders. Brain Sci. 2022. https://doi.org/10.3390/brainsci12091166 .
Jarnecke AM, Saraiya TC, Brown DG, Richardson J, Killeen T, Back SE. Examining the role of social support in treatment for co-occurring substance use disorder and posttraumatic stress disorder. Addict Behav Rep. 2022. https://doi.org/10.1016/j.abrep.2022.100427 .
Kyster NB, Tranberg K, Osler M, Hjorthøj C, Mårtensson S. The influence of childhood aspirations on the risk of developing psychotic disorders, substance use disorders, and dual diagnosis in adulthood based on the Metropolit 1953 Danish male birth cohort. Eur Child Adolesc Psychiatry. 2022. https://doi.org/10.1007/s00787-022-02091-7 .
Cunill R, Castells X, González-Pinto A, Arrojo M, Bernardo M, Sáiz PA, et al. Clinical practice guideline on pharmacological and psychological management of adult patients with attention deficit and hyperactivity disorder and comorbid substance use. Adicciones. 2022;34(2):168–78. https://doi.org/10.2088/adicciones.1569 .
Margolese HC, Boucher M, Therrien F, Clerzius G. Treatment with aripiprazole once-monthly injectable formulation is effective in improving symptoms and global functioning in schizophrenia with and without comorbid substance use—a post hoc analysis of the ReLiAM study. BMC Psychiatry. 2022. https://doi.org/10.1186/s12888-022-04397-x .
Minkoff K, Covell NH. Recommendations for integrated systems and services for people with co-occurring mental health and substance use conditions. Psychiatric Serv. 2022;73(6):686–9. https://doi.org/10.1176/appi.ps.202000839 .
Oliva V, De Prisco M, Pons-Cabrera MT, Guzmán P, Anmella G, Hidalgo-Mazzei D, et al. Machine learning prediction of comorbid substance use disorders among people with bipolar disorder. J Clin Med. 2022. https://doi.org/10.3390/jcm11143935 .
Somohano VC, Kaplan J, Newman AG, O’Neil M, Lovejoy T. Formal mindfulness practice predicts reductions in PTSD symptom severity following a mindfulness-based intervention for women with co-occurring PTSD and substance use disorder. Addict Sci Clin Pract. 2022. https://doi.org/10.1186/s13722-022-00333-2 .
Watkins LE, Patton SC, Drexler K, Rauch SAM, Rothbaum BO. Clinical effectiveness of an intensive outpatient program for integrated treatment of comorbid substance abuse and mental health disorders. Cogn Behav Pract. 2022. https://doi.org/10.1016/j.cbpra.2022.05.005 .
Bertulies-Esposito B, Ouellet-Plamondon C, Jutras-Aswad D, Gagnon J, Abdel-Baki A. The impact of treatment orders for residential treatment of comorbid severe substance use disorders for youth suffering from early psychosis: a case series. Int J Ment Heal Addict. 2021;19(6):2233–44. https://doi.org/10.1007/s11469-020-00317-w .
Butler A, Nicholls T, Samji H, Fabian S, Lavergne MR. Prevalence of mental health needs, substance use, and co-occurring disorders among people admitted to prison. Psychiatric Serv. 2022;73(7):737–44. https://doi.org/10.1176/appi.ps.202000927 .
Henderson JL, Wilkins LK, Hawke LD, Wang W, Sanches M, Brownlie EB, et al. Longitudinal emergence of concurrent mental health and substance use concerns in an ontario school-based sample: the research and action for teens study. J Can Acad Child Adolesc Psychiatry. 2021;30(4):249–63.
PubMed PubMed Central Google Scholar
Huang JS, Yang FC, Chien WC, Yeh TC, Chung CH, Tsai CK, et al. Risk of substance use disorder and its associations with comorbidities and psychotropic agents in patients with autism. JAMA Pediatr. 2021. https://doi.org/10.1001/jamapediatrics.2020.5371 .
Lu W, Muñoz-Laboy M, Sohler N, Goodwin RD. Trends and disparities in treatment for co-occurring major depression and substance use disorders among US adolescents from 2011 to 2019. JAMA Netw Open. 2021. https://doi.org/10.1001/jamanetworkopen.2021.30280 .
Melkonian AJ, Flanagan JC, Calhoun CD, Hogan JN, Back SE. Craving moderates the effects of intranasal oxytocin on anger in response to social stress among veterans with co-occurring posttraumatic stress disorder and alcohol use disorder. J Clin Psychopharmacol. 2021;41(4):465–9. https://doi.org/10.1097/JCP.0000000000001434 .
Otasowie J. Co-occurring mental disorder and substance use disorder in young people: aetiology, assessment and treatment. BJPsych Adv. 2021;27(4):272–81. https://doi.org/10.1192/bja.2020.64 .
Saraiya TC, Badour CL, Jones AC, Jarnecke AM, Brown DG, Flanagan JC, et al. The role of posttraumatic guilt and anger in integrated treatment for PTSD and co-occurring substance use disorders among primarily male veterans. Psychol Trauma: Theory Res Pract Policy. 2022. https://doi.org/10.1037/tra0001204 .
Walhout SJN, Zanten JV, DeFuentes-Merillas L, Sonneborn CKME, Bosma M. Patients with autism spectrum disorder and co-occurring substance use disorder: a clinical intervention study. Subst Abuse: Res Treat. 2022. https://doi.org/10.1177/11782218221085599 .
Walker D, Infante AA, Knight D. Examining the impact of mental health, substance use, and co-occurring disorders on juvenile court outcomes. J Res Crime Delinq. 2022;59(6):820–53. https://doi.org/10.1177/00224278221084981 .
Warfield SC, Pack RP, Degenhardt L, Larney S, Bharat C, Ashrafioun L, et al. The next wave? Mental health comorbidities and patients with substance use disorders in under-resourced and rural areas. J Subst Abuse Treat. 2021. https://doi.org/10.1016/j.jsat.2020.108189 .
Hien DA, Fitzpatrick S, Saavedra LM, Ebrahimi CT, Norman SB, Tripp J, et al. What’s in a name? A data-driven method to identify optimal psychotherapy classifications to advance treatment research on co-occurring PTSD and substance use disorders. Eur J Psychotraumatol. 2022. https://doi.org/10.1080/20008198.2021.2001191 .
Leonhardt M, Brodahl M, Cogan N, Lien L. How did the first COVID-19 lockdown affect persons with concurrent mental health and substance use disorders in Norway? A qualitative study. BMC Psychiatry. 2022. https://doi.org/10.1186/s12888-022-03812-7 .
Leonhardt M, Kyrdalen E, Holstad A, Hurlen-Solbakken H, Chiu MYL, Lien L. Norwegian cross-cultural adaptation of the social and communities opportunities profile-mini for persons with concurrent mental health and substance use disorders. J Psychosoc Rehabil Mental Health. 2022. https://doi.org/10.1007/s40737-022-00309-0 .
Sell L, Lund HL, Johansen KS. Past, present, and future labor market participation among patients admitted to hospital with concurrent substance use and mental health disorder, and what we can learn from it. J Occup Environ Med. 2022;64(12):1041–5. https://doi.org/10.1097/JOM.0000000000002633 .
Sverdlichenko I, Hawke LD, Henderson J. Understanding the service needs of youth with opioid use: a descriptive study of demographics and co-occurring substance use and mental health concerns. J Subst Abuse Treat. 2022. https://doi.org/10.1016/j.jsat.2021.108592 .
Yerriah J, Tomita A, Paruk S. Surviving but not thriving: Burden of care and quality of life for caregivers of patients with schizophrenia spectrum disorders and comorbid substance use in South Africa. Early Interv Psychiatry. 2022;16(2):153–61. https://doi.org/10.1111/eip.13141 .
Murthy P, Chand P. Treatment of dual diagnosis disorders. Curr Opin Psychiatry. 2012;25(3):194–200. https://doi.org/10.1097/YCO.0b013e328351a3e0 .
Schneier M. Better treatment for dual diagnosis patients. Psychiatr Serv. 2000;51(9):1079. https://doi.org/10.1176/appi.ps.51.9.1079 .
Tirado Muñoz J, Farré A, Mestre-Pintó J, Szerman N, Torrens M. Dual diagnosis in depression: treatment recommendations. Adicciones. 2018;30(1):66–76. https://doi.org/10.2088/adicciones.868 .
Carrà G, Clerici M. Dual diagnosis–policy and practice in Italy. Am J Addict. 2006;15(2):125–30. https://doi.org/10.1080/10550490500528340 .
Download references
Acknowledgements
Author information, authors and affiliations.
Department of Physiology and Pharmacology/Toxicology, Division of Biomedical Sciences, College of Medicine and Health Sciences, An-Najah National University, Nablus, Palestine
Waleed M. Sweileh
You can also search for this author in PubMed Google Scholar
Contributions
W.S started the idea, designed the methodology; did the data analysis, graphics, and data interpretation; wrote and submitted the manuscript. This was a single-authored manuscript. W.S wrote and submitted the manuscript.
Corresponding author
Correspondence to Waleed M. Sweileh .
Ethics declarations
Ethics approval and consent to participate.
IRB at An-Najah National University (Palestine) requires no approval for bibliometric studies.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Sweileh, W.M. Research landscape analysis on dual diagnosis of substance use and mental health disorders: key contributors, research hotspots, and emerging research topics. Ann Gen Psychiatry 23 , 32 (2024). https://doi.org/10.1186/s12991-024-00517-x
Download citation
Received : 28 July 2023
Accepted : 21 August 2024
Published : 30 August 2024
DOI : https://doi.org/10.1186/s12991-024-00517-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Substance use disorders
- Mental health disorders
- Dual diagnosis
- Research landscape analysis
- Treatment interventions
- Comorbidity
Annals of General Psychiatry
ISSN: 1744-859X
- Submission enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Abstract. PROPOSAL GENERAL INTRODUCTION Introduction and background to the study The researcher proposed this action research project to increase his junior high school students' achievements in ...
both interventions on illicit drug abuse within the adolescent homeless population. Research Proposal: The Effects of Therapeutic Interventions on Illicit Drug Abuse Among Homeless Adolescents . Alice Baillio, Meghan Stanley, Sarah Kroupa, Rania Ajaj, Paige Rabidoux . Old Dominion University, School of Nursing. Interprofessional Roles ...
abuse of opioids. This issue been exaggerated due to the negative perceptions associated with substance abuse and the lack of medication assisted treatment for individuals. The opioid epidemic affects not only individuals and their family, but the healthcare system, the criminal justice system, and the country's economy as a whole.
Drug and substance abuse have far reaching ramifications, for instance, according. to the survey by NACADA (2012) with a sample of 632 children, it was found out. that 6% have ever engaged in sex while on drugs ( 7.3% for boys and 4.4% for girls).The median age at sexual debut being estimated at 11 years.
Substance or Drug abuse is a serious public health problem affecting usually adolescents and young adults. It affects both males and females and it is. the major source of crimes in youth and ...
See "substance abuse" in our Developing Research Questions guide for an example of research questions on a focused study of drug abuse. In what ways is drug abuse a serious problem? What drugs are abused? Who abuses drugs? What causes people to abuse drugs? How do drug abusers' actions affect themselves, their families, and their communities?
Drug Alcohol Depend, 102(1-3), 78-87. doi: 10.1016/j.drugalcdep.2009.01.012 lived experiences of Resilient substance Abusing Adolescents: A ReseARcH PRoPosAl-by Tara Mariolis Recommended ...
Evidence-Based Prevention Programs. In the following sections, contemporary evidence-based approaches to drug abuse prevention for children and adolescents at the school, family, and community levels are described. Several model preventive intervention programs are reviewed, including universal, selected, and indicated programs for schools and ...
Drug abuse is a global problem; ... The number of sample participants varied widely between the studies, ranging from 70 samples (minimum) to 700,178 samples (maximum), while the qualitative paper utilized a total of 100 interviewees. ... With the increasing trend of drug abuse, it will be critical to focus research specifically on this area ...
This review draws on the peer-reviewed literature on YPAR in the context of youth substance use prevention published from January 1, 1998 through April 30, 2018. We summarize (1) the published evidence regarding YPAR for youth substance use prevention; (2) the level of youth engagement in the research process; (3) the methodologies used in YPAR ...
A pilot study of Safety First: Real Drug Education for Teens showed significant results pre to post curriculum with high school freshmen. Negative outcomes of drug education are linked to a failure to engage students because of developmentally inappropriate materials that include activities that have no relevance to real experiences of young people. The few harm reduction studies showed ...
Here's how to craft one. 1. Understand Your Funder. Before you begin writing, research potential funders. Understand their priorities, past grants, and their objectives. Aligning your program with the funder's goals increases the chances of your proposal being accepted. Example: If a potential funder has previously supported programs focusing ...
Drug Abuse directly influences the economic and social aspects of a country. The young people are mostly addicted to drug. Drug Addiction is commonly defined as the habitual and uncontrollable use of a drug. It is often used interchangeably with other terms such as drug abuse and drug dependence.
into taking drugs by peer pressure. Poor performance is the greatest effect of drug abuse among drug taking students. The researcher recommended that all stakeholders be involved in curriculum review and reform to address drug abuse related issues and guidance and counselling sessions enhanced in changing student behaviour.
Implications and effects on parents and family. Zimic and Jackic (Citation 2012) aver that the impact that substance abuse has on the family and on the individual family members merit attention.Lander et al. (Citation 2013) maintains that family members are affected by the individual's substance abuse; however, each individual is affected differently together with, but not limited to, having ...
these questions clearly suggest that drug abuse prevention interventions have been inconsistent in changing drug abuse and related behaviors. It has been suggested that more is known about what does not work than about what works in preventing drug abuse (Berberian et al. 1976; Goodstadt 1974; Schaps et al. 1981).
18 years; there is a significant relationship between drug abuse and age, use of drugs by other family members and easy access to drugs. A variety of factors contribute to drug abuse with the majority of students citing curiosity, acceptance by peers and ignorance as to the dangers of drug abuse and having a lot of pocket money as the main reasons.
Research Topics. En español. The National Institute on Drug Abuse (NIDA) is the largest supporter of the world's research on substance use and addiction. Part of the National Institutes of Health, NIDA conducts and supports biomedical research to advance the science on substance use and addiction and improve individual and public health.
Drug abuse is detrimental, and excessive drug usage is a worldwide problem. Drug usage typically begins during adolescence. Factors for drug abuse include a variety of protective and risk factors. Hence, this systematic review aimed to determine the risk and protective factors of drug abuse among adolescents worldwide. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA ...
The issue of drugs and substance abuse by the youth is on the increase, and it has called for social concern. Despite the fact and growing appreciation of the need for drugs and substance abuse control, it would appear there is a lack of enough empirical research in Nigeria which explicitly links drugs and substance abuse to youth development.
Drug education—not drug treatment—is the most common service provided to prisoners with drug abuse or addiction problems. 4, 42 More than one-quarter of state inmates and 1 in 5 federal inmates meeting abuse/dependence criteria participate in self-help groups such as Alcoholics Anonymous while in prison. 4 However, though treatment during ...
Friday, January 14, 2011 Sample Research Proposal - Drug Abuse Introduction There have always been people who were unable to restrict their use of mind and body altering substances to culturally prescribed limits, and who have fallen into the trap we know today as addiction. Addiction usually does not happen overnight.
Mission. The National Institute on Drug Abuse (NIDA) is the lead federal agency supporting scientific research on drug use and addiction. NIDA's mission is to advance science on drug use and addiction and to apply that knowledge to improve individual and public health through: Strategically supporting and conducting basic, clinical, and ...
Substance use disorders (SUDs) and mental health disorders (MHDs) are significant public health challenges with far-reaching consequences on individuals and society. Dual diagnosis, the coexistence of SUDs and MHDs, poses unique complexities and impacts treatment outcomes. A research landscape analysis was conducted to explore the growth, active countries, and active journals in this field ...