Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.

Abortion Surveillance — United States, 2019
Surveillance Summaries / November 26, 2021 / 70(9);1–29
Please note: This report has been corrected. An erratum has been published.
Katherine Kortsmit, PhD 1 ; Michele G. Mandel 1 ; Jennifer A. Reeves, MD 1 ; Elizabeth Clark, MD 1 ; H. Pamela Pagano, DrPH 1 ; Antoinette Nguyen, MD 1 ; Emily E. Petersen, MD 1 ; Maura K. Whiteman, PhD 1 ( View author affiliations )
Views: Views equals page views plus PDF downloads
Introduction, limitations, public health implications.
Problem/Condition: CDC conducts abortion surveillance to document the number and characteristics of women obtaining legal induced abortions and number of abortion-related deaths in the United States.
Period Covered: 2019.
Description of System: Each year, CDC requests abortion data from the central health agencies for 50 states, the District of Columbia, and New York City. For 2019, 49 reporting areas voluntarily provided aggregate abortion data to CDC. Of these, 48 reporting areas provided data each year during 2010–2019. Census and natality data were used to calculate abortion rates (number of abortions per 1,000 women aged 15–44 years) and ratios (number of abortions per 1,000 live births), respectively. Abortion-related deaths from 2018 were assessed as part of CDC’s Pregnancy Mortality Surveillance System (PMSS).
Results: A total of 629,898 abortions for 2019 were reported to CDC from 49 reporting areas. Among 48 reporting areas with data each year during 2010–2019, in 2019, a total of 625,346 abortions were reported, the abortion rate was 11.4 abortions per 1,000 women aged 15–44 years, and the abortion ratio was 195 abortions per 1,000 live births. From 2018 to 2019, the total number of abortions increased 2% (from 614,820 total abortions), the abortion rate increased 0.9% (from 11.3 abortions per 1,000 women aged 15–44 years), and the abortion ratio increased 3% (from 189 abortions per 1,000 live births). From 2010 to 2019, the total number of reported abortions, abortion rate, and abortion ratio decreased 18% (from 762,755), 21% (from 14.4 abortions per 1,000 women aged 15–44 years), and 13% (from 225 abortions per 1,000 live births), respectively.
In 2019, women in their 20s accounted for more than half of abortions (56.9%). Women aged 20–24 and 25–29 years accounted for the highest percentages of abortions (27.6% and 29.3%, respectively) and had the highest abortion rates (19.0 and 18.6 abortions per 1,000 women aged 20–24 and 25–29 years, respectively). By contrast, adolescents aged <15 years and women aged ≥40 years accounted for the lowest percentages of abortions (0.2% and 3.7%, respectively) and had the lowest abortion rates (0.4 and 2.7 abortions per 1,000 women aged <15 and ≥40 years, respectively). However, abortion ratios in 2019 were highest among adolescents (aged ≤19 years) and lowest among women aged 25–39 years. Abortion rates decreased from 2010 to 2019 for all women, regardless of age. The decrease in abortion rate was highest among adolescents compared with any other age group. From 2018 to 2019, abortion rates decreased or did not change among women aged ≤24 years; however, the abortion rate increased among those aged ≥25 years. Abortion ratios also decreased or did not change from 2010 to 2019 for all age groups, except adolescents aged <15 years. The decrease in abortion ratio was highest among women aged ≥40 years compared with any other age group. From 2018 to 2019, abortion ratios increased for all age groups, except adolescents aged <15 years. In 2019, 79.3% of abortions were performed at ≤9 weeks’ gestation, and nearly all (92.7%) were performed at ≤13 weeks’ gestation. During 2010–2019, the percentage of abortions performed at >13 weeks’ gestation remained consistently low (≤9.0%). In 2019, the highest proportion of abortions were performed by surgical abortion at ≤13 weeks’ gestation (49.0%), followed by early medical abortion at ≤9 weeks’ gestation (42.3%), surgical abortion at >13 weeks’ gestation (7.2%), and medical abortion at >9 weeks’ gestation (1.4%); all other methods were uncommon (<0.1%). Among those that were eligible (≤9 weeks’ gestation), 53.7% of abortions were early medical abortions. In 2018, the most recent year for which PMSS data were reviewed for pregnancy-related deaths, two women died as a result of complications from legal induced abortion.
Interpretation: Among the 48 areas that reported data continuously during 2010–2019, overall decreases were observed during 2010–2019 in the total number, rate, and ratio of reported abortions; however, from 2018 to 2019, 1%–3% increases were observed across all measures.
Public Health Action: Abortion surveillance can be used to help evaluate programs aimed at promoting equitable access to patient-centered quality contraceptive services in the United States to reduce unintended pregnancies.
This report summarizes data on legal induced abortions for 2019 that were provided voluntarily to CDC by the central health agencies of 49 reporting areas (47 states, the District of Columbia, and New York City, excluding California, Maryland, and New Hampshire) and comparisons over time for the 48 reporting areas that reported each year during 2010–2019 (47 states and New York City). This report also summarizes abortion-related deaths reported voluntarily to CDC for 2018 as part of the Pregnancy Mortality Surveillance System (PMSS).
Since 1969, CDC has conducted abortion surveillance to document the number and characteristics of women obtaining legal induced abortions in the United States. After nationwide legalization of abortion in 1973, the total number, rate (number of abortions per 1,000 women aged 15–44 years), and ratio (number of abortions per 1,000 live births) of reported abortions increased rapidly, reaching the highest levels in the 1980s, before decreasing at a slow yet steady pace ( 1 , 2 ). During 2006–2008, a break occurred in the previously sustained pattern of decrease ( 3 , 4 ), although this break was followed in subsequent years by even greater decreases ( 5 , 6 ). In 2017, the total number, rate, and ratio of reported abortions reached historic lows, followed by 1%–2% increases across all measures from 2017 to 2018 ( 5 ). Nonetheless, despite the overall decreases, abortion incidence and practices have varied over the years and continue to vary across subpopulations ( 7 – 11 ), highlighting the need for continued surveillance.
Description of the Surveillance System
Each year, CDC requests aggregated data from the central health agencies of the 50 states, the District of Columbia, and New York City to document the number and characteristics of women obtaining legal induced abortions in the United States. Not all persons who obtain abortions identify as women; the term “women” has been maintained in this report to be consistent with the collection and reporting of denominator data used to calculate abortion rates and ratios. This report contains data voluntarily reported to CDC as of April 9, 2021. For the purpose of surveillance, legal induced abortion is defined as an intervention performed within the limits of state law by a licensed clinician (e.g., a physician, nurse-midwife, nurse practitioner, or physician assistant) intended to terminate a suspected or known intrauterine pregnancy and that does not result in a live birth. All abortions in this report are considered to be legally induced unless stated otherwise.
In most states and jurisdictions, collection of abortion data is facilitated by a legal requirement for hospitals, facilities, or physicians to report abortions to a central health agency ( 12 ); however, reporting is not complete in all areas, including in some areas with reporting requirements ( 13 ). Because the reporting of abortion data to CDC is voluntary, many reporting areas have developed their own data collection forms and might not collect or provide all the information requested by CDC. As a result, the level of detail reported by CDC on the characteristics of women obtaining abortions might vary from year to year and by reporting area. To encourage uniform collection of data, CDC has collaborated with the National Association for Public Health Statistics and Information Systems to develop reporting standards and provide technical guidance for vital statistics personnel who collect and summarize abortion data within the United States.
Variables and Categorization of Data
Each year, CDC sends a suggested template to central health agencies in the United States for compilation of aggregated abortion data among women obtaining legal induced abortions. Aggregate abortion numbers, without individual-level records, are requested for the following variables:
- Age group in years of women obtaining legal induced abortions (<15, 15–19 [age group and by individual year], 20–24, 25–29, 30–34, 35–39, or ≥40)
- Gestational age of pregnancy in completed weeks at the time of abortion (≤6, 7–20 by individual week, or ≥21)
- Race (Black, White, or other [including Asian, Pacific Islander, other races, and multiple races]), ethnicity (Hispanic or non-Hispanic), and race by ethnicity
- Method type (surgical abortion, intrauterine instillation, medical [nonsurgical] abortion, or hysterectomy/hysterotomy)
- Marital status (married [including currently married or separated] or unmarried [including never married, widowed, or divorced])
- Number of previous live births (zero, one, two, three, or four or more)
- Number of previous induced abortions (zero, one, two, or three or more)
- Residence (the state, jurisdiction, territory, or foreign country in which the women obtaining the abortion lived, or, if additional details are unavailable, in-reporting area versus out-of-reporting area)
In addition, the template provided by CDC requests that aggregate numbers for certain variables be cross-tabulated by a second variable. The cross-tabulations presented in this report include weeks of gestation separately by method type, by age group, and by race/ethnicity.
Beginning with 2014 data, instead of reporting the clinicians’ estimates of gestational age or estimates of gestational age based on last menstrual period, some areas have reported “probable postfertilization age,” “clinician’s estimate of gestation based on date of conception,” and “probable gestational age” to CDC. To ensure consistency between data reported as postfertilization age and the data collection practices for gestational age recommended by CDC’s National Center for Health Statistics ( 14 ), 2 weeks were added to probable postfertilization age. This method was used to account for time after last menstrual period until ovulation in a standard 28-day cycle because fertilization occurs around the time of ovulation ( 15 ). No modifications were made to data reported as clinician’s estimate of gestational age based on date of conception or data reported as probable gestational age.
In this report, medical and surgical abortions are further categorized by gestational age when available in the categories reported by CDC. Early medical abortion is defined as the administration of medications (typically mifepristone followed by misoprostol) to induce an abortion at ≤9 completed weeks’ gestation consistent with the current Food and Drug Administration (FDA) labeling for mifepristone (implemented in 2016) ( 16 ). CDC collects information only on the estimated number of weeks (not days) of gestation and acknowledges the conventional use of completed weeks of gestation to describe pregnancy duration; therefore, CDC’s category of ≤9 weeks’ gestation includes abortions through 9 weeks and 6 days. Medications (typically serial prostaglandins, sometimes administered after mifepristone) may also be used to induce an abortion at >9 weeks’ gestation. Surgical abortions, which include uterine aspiration (i.e., dilation and curettage, aspiration curettage, suction curettage, manual vacuum aspiration, menstrual extraction, or sharp curettage) and dilation and evacuation procedures, are categorized as having been performed at ≤13 weeks’ gestation or at >13 weeks’ gestation because of differences in surgical technique at these gestational ages ( 17 ). Finally, because intrauterine instillations are unlikely to be performed early in gestation ( 18 ), abortions reported to have been performed by intrauterine instillation at ≤12 weeks’ gestation are excluded from calculation of the percentage of abortions by known method type and are grouped with unknown type. The cutoff of ≤12 weeks was selected because this procedure is unlikely to be performed at earlier gestational ages.
Measures of Abortion
Four measures of abortion are presented in this report: 1) the number of abortions in a given population, 2) the percentage of abortions among women by selected characteristics, 3) the abortion rate (number of abortions per 1,000 women within a given population), and 4) the abortion ratio (number of abortions per 1,000 live births within a given population). Abortion rates adjust for differences in population size. Abortion ratios measure the relative number of pregnancies in a population that end in abortion compared with live birth.
The U.S. Census Bureau estimates of the resident female population were used as the denominator for calculating abortion rates ( 19 – 28 ). Overall abortion rates were calculated from the population of women aged 15–44 years living in the reporting areas that provided continuously reported data. For adolescents aged <15 years, abortion rates were calculated using the number of adolescents aged 13–14 years; for women aged ≥40 years, abortion rates were calculated using the number of women aged 40–44 years. For the calculation of abortion ratios, live birth data were obtained from CDC natality files and included births to women of all ages living in the reporting areas that provided abortion data ( 29 , 30 ). For calculation of the total abortion rates and total ratios only, women with unknown data on selected characteristics (e.g., age, race/ethnicity, and marital status) were distributed according to the distribution of abortions among those with known information on the characteristic. For calculation of totals only, abortions for women with an unknown gestational age of pregnancy but known method type were distributed according to the distribution of abortions among those with known information on method type by gestational age to the following categories: surgical, ≤13 weeks’ gestation; surgical, >13 weeks’ gestation; medical ≤9 weeks’ gestation; and medical >9 weeks’ gestation.
Data Presentation and Analysis
This report provides aggregate and reporting area–specific abortion numbers, rates, and ratios for the 49 areas that reported to CDC for 2019, which excluded California, Maryland, and New Hampshire. In addition, this report describes characteristics of women who obtained abortions in 2019. The data in this report are presented by the reporting area in which the abortions were performed.
The completeness and quality of data received vary by year and by variable; this report only describes the characteristics of women obtaining abortions in reporting areas that met CDC reporting standards (i.e., reported at least 20 abortions overall, provided data categorized in accordance with requested variables, and had <15% unknown values for a given characteristic). Cells with a value in the range of 1–4 or cells that would allow for calculation of these values have been suppressed in this report to maintain confidentiality in tables presented by reporting area of occurrence.
Trends in the number, rate, and ratio of reported abortions and annual data are presented for the 48 areas that reported every year during 2010–2019. The percentage change in abortion measures from the most recent past year (2018 to 2019) and during the 10-year period of analysis (2010 to 2019) were calculated for these 48 reporting areas.
Trends are also reported for abortions by age group, weeks of gestation, and early medical abortions (≤9 completed weeks’ gestation). Annual data are presented for areas that met reporting standards every year during 2010–2019; the percentage change was calculated from the beginning to the end of the 10-year period of analysis (2010–2019), in 5-year increments from the beginning to the end of the first and second halves of this period (2010–2014 and 2015–2019), and from the most recent past year (2018 to 2019). Consistent with previous reports ( 5 ), key findings for trends are presented to highlight observed changes over time and differences between groups. Trends for early medical abortions are reported to monitor any changes in clinical practice that might have occurred with the accumulation of evidence on the safety and effectiveness of medical abortion past 63 days of gestation (8 completed weeks’ gestation) ( 31 ), changes in professional practice guidelines published in 2013 and 2014 ( 32 , 33 ), and the 2016 FDA extension of the gestational age limit for the use of mifepristone for early medical abortion from 63 days to 70 days (9 completed weeks’ gestation) ( 34 ). No statistical testing was performed. Comparisons do not imply statistical significance, and lack of comment regarding the difference between values does not imply that no statistically significant difference exists.
Data from reporting areas are not included in trends if the data did not meet reporting standards every year during 2010–2019. As a result, aggregate measures for 2019 in trend analyses might differ from the point estimates reported for 2019.
Abortion Mortality
CDC has reported data on abortion-related deaths periodically since information on abortion mortality first was included in the 1972 abortion surveillance report ( 5 , 35 ). An abortion-related death is defined as a death resulting from a direct complication of an abortion (legal or illegal), an indirect complication caused by a chain of events initiated by an abortion, or an aggravation of a preexisting condition by the physiologic or psychologic effects of abortion ( 36 ). An abortion is categorized as legal when it is performed by a licensed clinician within the limits of state law.
Since 1987, CDC has monitored abortion-related deaths through PMSS ( 37 ). Sources of data to identify abortion-related deaths have included state vital records; media reports, including computerized searches of full-text newspaper and other print media databases; and individual case reports by public health agencies, including maternal mortality review committees, health care providers and provider organizations, private citizens, and citizen groups. For each death that is possibly related to abortion, CDC requests clinical records and autopsy reports. Two medical epidemiologists independently review these reports to determine the cause of death and whether the death was abortion related. Discrepancies are discussed and resolved by consensus. Each death is categorized by abortion type as legal induced, illegal induced, spontaneous, or unknown type.
This report provides PMSS data on induced abortion-related deaths that occurred in 2018, the most recent year for which PMSS data are available. Data on induced abortion-related deaths that occurred during 1972–2017 have been published ( 1 , 5 , 38 ). For 1998–2018, abortion surveillance data reported to CDC cannot be used alone to calculate national case-fatality rates for legal induced abortions (number of legal induced abortion-related deaths per 100,000 reported legal induced abortions in the United States) because eight reporting areas did not report abortion data every year during this period (Alaska, 1998–2000; California, 1998–2018; District of Columbia, 2016; Louisiana, 2005; Maryland, 2007–2018; New Hampshire, 1998–2018; Oklahoma, 1998–1999; and West Virginia, 2003–2004). Thus, denominator data for calculation of national legal induced abortion case-fatality rates were obtained from a published report by the Guttmacher Institute that includes estimated total numbers of abortions in the United States from a national survey of abortion-providing facilities ( 6 ). For 2018, the case-fatality rate was calculated using denominator data for 2017, the most recent year for which data from the Guttmacher Institute are available. Because rates determined on the basis of a numerator of <20 deaths are unstable ( 39 ), national case-fatality rates for legal induced abortion were calculated for consecutive 5-year periods during 1973–2012 and then for a consecutive 6-year period during 2013–2018.
Total Abortions Reported to CDC by Occurrence
Among the 49 reporting areas that provided data for 2019, a total of 629,898 abortions were reported. Of these abortions, 625,346 (99.3%) were from 48 reporting areas that provided data every year during 2010–2019. In 2019, these continuously reporting areas had an abortion rate of 11.4 abortions per 1,000 women aged 15–44 years and an abortion ratio of 195 abortions per 1,000 live births ( Table 1 ). From 2018 to 2019, the total number of reported abortions increased 2% (from 614,820 total abortions), the abortion rate increased 0.9% (from 11.3 abortions per 1,000 women aged 15–44 years), and the abortion ratio increased 3% (from 189 abortions per 1,000 live births). From 2010 to 2019, the total number of reported abortions decreased 18% (from 762,755), the abortion rate decreased 21% (from 14.4 abortions per 1,000 women aged 15–44 years), and the abortion ratio decreased 13% (from 225 abortions per 1,000 live births) ( Figure ).
In 2019, a considerable range existed in abortion rates by reporting area of occurrence (from 0.3 to 27.2 abortions per 1,000 women aged 15–44 years in Wyoming and New York City) and abortion ratios (from 5 to 501 abortions per 1,000 live births in Wyoming and the District of Columbia) ( Table 2 ). The percentage of abortions obtained by out-of-state residents also varied among reporting areas (from 0.5% in Arizona to 68.7% in the District of Columbia). Overall, 0.9% of abortions were reported to CDC with unknown residence.
Age Group, Race/Ethnicity, and Marital Status
Among the 49 areas that reported abortion numbers by women’s age for 2019, women in their 20s accounted for the majority (56.9%) of abortions ( Table 3 ). Women aged 20–24 and 25–29 years accounted for the highest percentages of abortions (27.6% and 29.3%, respectively) and had the highest abortion rates (19.0 and 18.6 abortions per 1,000 women aged 20–24 and 25–29 years, respectively). By contrast, those in the youngest (<15 years) and oldest (≥40 years) age groups accounted for the smallest percentages of abortions (0.2% and 3.7%) and had the lowest abortion rates (0.4 and 2.7 abortions per 1,000 women aged <15 and ≥40 years). However, abortion ratios in 2019 were highest among adolescents (873 and 348 abortions per 1,000 live births among those aged <15 years and 15–19 years) and lowest among women aged 25–39 years (194, 132, and 145 abortions per 1,000 live births among those aged 25–29, 30–34, and 35–39 years, respectively).
Among the 44 reporting areas that provided data each year by women’s age for 2010–2019, this pattern across age groups was stable, with the majority of abortions and the highest abortion rates occurring among women aged 20–29 years and the lowest percentages of abortions and abortion rates occurring among those in the youngest and oldest age groups ( Table 4 ). From 2010 to 2019, abortion rates decreased among all age groups, although the decreases for adolescents (60% and 50% for adolescents aged <15 and 15–19 years) were greater than the decreases for all older age groups. From 2010 to 2014, the abortion rates decreased for all age groups, and from 2015 to 2019, the abortion rates decreased or did not change for all age groups except women aged 30–34 years and ≥40 years. From 2018 to 2019, abortion rates decreased or did not change for women aged ≤24 years; however, the abortion rate increased among those aged ≥25 years. During 2010–2019, abortion ratios decreased or did not change among all age groups, except for adolescents aged <15 years. The abortion ratio decreased for all age groups from 2010 to 2014; however, from 2015 to 2019, abortion ratios only decreased for women aged ≥35 years. From 2018 to 2019, abortion ratios increased for all age groups, except adolescents aged <15 years, for which it decreased.
Among the 47 areas that reported age by individual year among adolescents for 2019, adolescents aged 18–19 years accounted for the majority (70.2%) of adolescent abortions and had the highest adolescent abortion rates (8.6 and 12.2 abortions per 1,000 adolescents aged 18 and 19 years, respectively) ( Table 5 ). Adolescents aged <15 years accounted for the smallest percentage of adolescent abortions (2.6%) and had the lowest adolescent abortion rate (0.4 abortions per 1,000 adolescents aged 13–14 years). In 2019, the abortion ratio for adolescents was highest among adolescents aged <15 years (853 abortions per 1,000 live births) and was lowest among adolescents aged 17–19 years (344, 358, and 294 abortions per 1,000 live births among adolescents aged 17, 18, and 19 years).
Among the 30 areas that reported race by ethnicity data for 2019, non-Hispanic White women and non-Hispanic Black women accounted for the largest percentages of all abortions (33.4% and 38.4%, respectively), and Hispanic women and non-Hispanic women in the other race category accounted for smaller percentages (21.0% and 7.2%, respectively) ( Table 6 ). Non-Hispanic White women had the lowest abortion rate (6.6 abortions per 1,000 women) and ratio (117 abortions per 1,000 live births), and non-Hispanic Black women had the highest abortion rate (23.8 abortions per 1,000 women) and ratio (386 abortions per 1,000 live births).
Among the 42 areas that reported by marital status for 2019, 14.5% of women who obtained an abortion were married, and 85.5% were unmarried ( Table 7 ). The abortion ratio was 46 abortions per 1,000 live births for married women and 394 abortions per 1,000 live births for unmarried women.
Previous Live Births and Previous Induced Abortions
Among the 45 areas that reported the number of previous live births for 2019, 40.2%, 24.5%, 20.0%, 9.2%, and 6.0% of women had zero, one, two, three, or four or more previous live births ( Table 8 ). Among the 44 areas that reported the number of previous induced abortions for 2019, the majority of women (58.2%) had previously had no abortions, 23.8% had previously had one abortion, 10.5% had previously had two abortions, and 7.5% had previously had three or more abortions ( Table 9 ).
Weeks of Gestation and Method Type
Among the 43 areas that reported gestational age at the time of abortion for 2019, 79.3% of abortions were performed at ≤9 weeks’ gestation, and nearly all (92.7%) were performed at ≤13 weeks’ gestation ( Table 10 ). Fewer abortions were performed at 14–20 weeks’ gestation (6.2%) or at ≥21 weeks’ gestation (<1.0%). Among the 34 reporting areas that provided data every year on gestational age for 2010–2019, the percentage of abortions performed at ≤13 weeks’ gestation changed negligibly, from 91.9% to 92.0% ( Table 11 ). However, within this gestational age range, a shift occurred toward earlier gestational ages, with the percentage of abortions performed at ≤6 weeks’ gestation increasing 8% and the percentage of abortions performed at 7–9 weeks’ and 10–13 weeks’ gestation decreasing 0.5% and 14%, respectively.
Among the 47 areas that reported by method type for 2019 and included medical abortion on their reporting form, 49.0% of abortions were surgical abortions at ≤13 weeks’ gestation, 42.3% were early medical abortions (a nonsurgical abortion at ≤9 weeks’ gestation), 7.2% were surgical abortions at >13 weeks’ gestation, and 1.4% were medical abortions at >9 weeks’ gestation; other methods, including intrauterine instillation and hysterectomy/hysterotomy, were both uncommon (<0.1%) ( Table 12 ). During 2010−2019, 35 reporting areas (excludes Alabama, Arizona, California, Delaware, District of Columbia, Florida, Hawaii, Illinois, Louisiana, Maine, Maryland, New Hampshire, New Mexico, Tennessee, Vermont, Wisconsin, and Wyoming) provided continuous data and included medical abortion on their reporting form. Among these 35 areas, use of early medical abortion increased 10% from 2018 to 2019 (from 37.5% of abortions to 41.1%) and 123% from 2010 to 2019 (from 18.4% of abortions to 41.1%).
Among the 42 areas that reported abortions categorized by individual weeks of gestation and method type for 2019, surgical abortion accounted for the largest percentage of abortions within every gestational age category, except ≤6 weeks’ gestation ( Table 13 ). At ≤6 weeks’ gestation, surgical abortion accounted for 41.3% of abortions. Surgical abortion accounted for 52.2% of abortions at 7–9 weeks’ gestation, 93.2% of abortions at 10–13 weeks’ gestation, 96.9%–99.2% of abortions at 14–20 weeks’ gestation, and 87.0% of abortions at ≥21 weeks’ gestation. In contrast, medical abortion accounted for 58.6% of abortions at ≤6 weeks’ gestation, 47.8% of abortions at 7–9 weeks’ gestation, 6.8% of abortions at 10–13 weeks’ gestation, 0.8%–2.3% of abortions at 14–20 weeks’ gestation, and 11.6% of abortions at ≥21 weeks’ gestation. For each gestational age category as applicable, abortions performed by intrauterine instillation or hysterectomy/hysterotomy were rare (<0.1%–1.3% of abortions).
Weeks of Gestation by Age Group and Race/Ethnicity
In selected reporting areas, abortions that were categorized by weeks of gestation were further categorized by age and by race/ethnicity ( Table 14 ). In every subgroup for these characteristics, the largest percentage of abortions occurred at ≤9 weeks’ gestation. In 43 reporting areas, by age, 61.3% of adolescents aged <15 years and 73.6% of adolescents aged 15–19 years obtained an abortion at ≤9 weeks’ gestation, compared with ≥78.6% among women in older age groups. Conversely, 19.8% of adolescents aged <15 years and 9.6% of adolescents aged 15–19 years obtained an abortion after 13 weeks’ gestation, compared with 6.8%–7.5% for women in older age groups. In 29 reporting areas, by race/ethnicity, 76.2% of non-Hispanic Black women obtained an abortion at ≤9 weeks’ gestation, compared with 80.6%–82.4% of women in other racial/ethnic groups. Differences in abortions after 13 weeks’ gestation across race/ethnicity were minimal (7.8% among non-Hispanic Black women, compared with 6.1%–7.7% among women in other racial/ethnic groups).
Using national PMSS data ( 37 ), CDC identified two abortion-related deaths for 2018, the most recent year for which data were reviewed for abortion-related deaths ( Table 15 ). Investigation of these cases indicated that both deaths were related to legal abortion.
The annual number of deaths related to legal induced abortion has fluctuated from year to year since 1973 (Table 15). Because of this variability and the limited number of deaths related to legal induced abortions every year, national case-fatality rates for legal abortion were calculated for consecutive 5-year periods during 1973–2012 and then for a consecutive 6-year period during 2013–2018. The national case-fatality rate for legal induced abortion for 2013–2018 was 0.41 deaths related to legal induced abortions per 100,000 reported legal abortions. This case-fatality rate was lower than the rates for the previous 5-year periods.
For 2019, a total of 629,898 abortions were reported to CDC by 49 areas. Of these reporting areas, 48 submitted data every year for 2010–2019, thus providing the information necessary for consistently reporting trends. Among these 48 areas, for 2019, the abortion rate was 11.4 abortions per 1,000 women aged 15–44 years, and the abortion ratio was 195 abortions per 1,000 live births. From 2018 to 2019, the number of abortions increased 2%, the abortion rate increased 0.9%, and the abortion ratio increased 3%. Although the rate of reported abortions declined overall from 2010 to 2019, after reaching a historic low in 2017, the abortion rates increased overall between 2017 and 2019.
Approximately 18% of all pregnancies in the United States end in induced abortion ( 6 ). Multiple factors influence the incidence of abortion, including access to health care services and contraception ( 40 – 43 ); the availability of abortion providers ( 4 , 6 , 44 – 47 ); state regulations, such as mandatory waiting periods ( 48 – 50 ), parental involvement laws ( 51 , 52 ), and legal restrictions on abortion providers ( 53 – 57 ); and changes in the economy and the resulting impact on family planning decisions and contraceptive use ( 58 ).
Among areas that reported data continuously by age during 2010–2019, women in their 20s accounted for the majority of abortions and had the highest abortion rates, whereas adolescents aged <15 years had the lowest abortion rates, and adolescents aged <15 years and 15−19 years had the highest abortion ratios. During 2010–2019, women aged ≥40 years accounted for a relatively small proportion of reported abortions (3.4%–3.7%). However, the abortion ratio among women aged ≥40 years continues to be higher than among women aged 25–39 years. These data underscore important age differences in abortion measures.
The trends in adolescent abortions described in this report are important for monitoring trends in adolescent pregnancies in the United States. From 2010 to 2019, national birth data indicate that the birth rate for adolescents aged 15–19 years decreased 51% ( 30 ), and the data in this report indicate that the abortion rate for the same age group decreased 50%. These findings highlight that decreases in adolescent births in the United States have been accompanied by large decreases in adolescent abortions ( 30 ).
As in previous years, abortion rates and ratios differ across racial/ethnic groups. For example, in 2019, compared with non-Hispanic White women, abortion rates and ratios were 3.6 and 3.3 times higher among non-Hispanic Black women and 1.8 and 1.5 times higher among Hispanic women. Similar differences have been demonstrated in other U.S.-based studies ( 2 , 7 – 10 , 59 ). The factors leading to higher abortion rates among certain racial/ethnic minority groups are complex. In addition to disparities in rates of unintended pregnancies, structural factors, including unequal access to quality family planning services ( 60 , 61 ), economic disadvantage, and distrust of the medical system ( 62 ), might contribute to observed differences. Strategies are needed to address these broader structural inequities.
In 2019, the majority of abortions occurred early in gestation (≤9 weeks), when the risks for complications are lowest ( 63 – 66 ). In addition, over the past 10 years, approximately three fourths of abortions were performed at ≤9 weeks’ gestation, and this percentage increased from 74.8% in 2010 to 77.4% in 2019. Moreover, among areas that reported abortions at ≤13 weeks’ gestation by individual week, the distribution of abortions by gestational age continued to shift toward earlier weeks of gestation, with the percentage of early abortions performed at ≤6 weeks’ gestation increasing from 34.7% in 2010 to 37.5% in 2019. Previous research indicates that the distribution of abortions by gestational age differs by various sociodemographic characteristics ( 67 – 69 ). In this report, the percentage of adolescents aged ≤19 years who obtained abortions at >13 weeks’ gestation was higher than the percentage of abortions obtained among older age groups. The gestational age when abortions are performed might be influenced by multiple factors, including state abortion restrictions, accurate estimation of gestational age, income level, age, and presence of pregnancy-related health conditions ( 48 , 59 , 66 , 68 – 73 ).
Changes in abortion practices have facilitated the trend of obtaining abortions earlier in pregnancy. Research conducted in the United States during the 1970s indicated that surgical abortion procedures performed at ≤6 weeks’ gestation, compared with 7–12 weeks’ gestation, were less likely to result in successful termination of the pregnancy ( 74 ). However, subsequent advances in technology (e.g., improved transvaginal ultrasonography and sensitivity of pregnancy tests) have allowed very early surgical abortions to be performed with completion rates exceeding 97% ( 75 – 78 ). Likewise, the development of early medical abortion regimens has allowed for abortions to be performed early in gestation, with completion rates for regimens that combine mifepristone and misoprostol reaching 96%–98% ( 78 – 81 ). Among those that were eligible (≤9 weeks’ gestation), 53.7% were reported as early medical abortions. Moreover, among areas that reported by method type and included medical abortion on their reporting form, the percentage of all abortions performed by early medical abortion increased 123% from 2010 to 2019.
Because the annual number of deaths related to legal induced abortion is small and statistically unstable, case-fatality rates were calculated for consecutive 5-year periods during 1973–2012 and then for a consecutive 6-year period during 2013–2018. The national case-fatality rate for legal induced abortion for 2013–2018 was 0.41 deaths per 100,000 abortions; since the late 1970s, all rates for the preceding 5-year periods have been fewer than 1 death per 100,000 abortions, demonstrating the low risk for death associated with legal induced abortion.
The findings in this report are subject to at least four limitations. First, because reporting to CDC is voluntary and reporting requirements vary by the individual reporting areas ( 13 ), CDC is unable to report the total number of abortions performed in the United States. Of the 52 areas from which CDC requested data for 2019, California, Maryland, and New Hampshire did not submit abortion data. In 2017, the most recent year for which data are available through the Guttmacher Institute’s national survey of abortion-providing facilities, abortions performed in these states accounted for approximately 19% of all abortions in the United States ( 6 ). In addition, New Jersey did not have abortion reporting requirements to a centralized health agency during the period covered in this report ( 12 ), which potentially affects the representativeness of data provided to CDC. Some reporting areas (the District of Columbia and Wyoming) implemented new legislation that could improve reporting of 2019 abortion data. Nonetheless, even in reporting areas that legally require clinicians to submit a report for every abortion they perform, enforcement of this requirement varies.
Second, many states use abortion reporting forms that differ from the technical guidance that CDC developed in collaboration with the National Association for Public Health Statistics and Information Systems. Consequently, some reporting areas do not collect all variables requested by CDC (e.g., age and race/ethnicity) or do not report the data in a manner consistent with this guidance (e.g., gestational age). Missing demographic information can reduce the extent to which the statistics in this report represent women who have had abortions. Findings in this report on the age of women seeking abortions were generally similar to previously published data from Guttmacher Institute’s national survey of abortion patients in 2014, although the percentage of abortions among non-Hispanic Black women was lower and among Hispanic women was higher compared with data provided to CDC ( 82 ). Differences might be attributable to the fact that only 30 reporting areas reported race/ethnicity data to CDC that met CDC’s reporting standards. Some areas that either do not report to CDC (e.g., California) or do not report race/ethnicity data (e.g., Illinois) have sufficiently large populations of racial/ethnic minority groups that the absence of data from these areas likely reduces the representativeness of CDC data for these variables. In addition, some areas collect gestational age data that are based on estimated date of conception or probable postfertilization age, which are not consistent with medical conventions for gestational age reporting. Without medical guidance on how to report these data, the validity and reliability of gestational age for these reporting areas is uncertain.
Third, abortion data are compiled and reported to CDC by the central health agency of the reporting area in which the abortion was performed rather than the reporting area in which the person lived. Thus, the available population ( 19 – 28 ) and birth data ( 29 , 30 ), which are organized by the states in which women live, might differ from the population of women who undergo abortions in a given reporting area. This likely results in an overestimation of abortions for reporting areas in which a higher percentage of abortions are obtained by out-of-state residents and an underestimation of abortions for reporting areas where residents more frequently obtain abortions out of state. Limited abortion services, stringent regulatory requirements for obtaining an abortion, or geographic proximity to services in another state might influence where women obtain abortion services ( 83 ).
Finally, CDC reporting of sociodemographic characteristics of women obtaining abortions is limited to data collected on jurisdiction reporting forms. Therefore, examining additional demographic variables (e.g., socioeconomic status) is not possible.
Ongoing surveillance of legal induced abortion is important for several reasons. First, abortion surveillance can be used to help evaluate programs aimed at promoting equitable access to patient-centered contraceptive care in the United States to reduce unintended pregnancies. Cost, inadequate provider reimbursement and training, insufficient patient-centered counseling, lack of youth-friendly services, and low client awareness of available contraceptive methods are reported barriers to accessing contraception ( 40 – 42 , 84 – 90 ). Reducing these barriers might help ensure equitable access to patient-centered contraceptive care and promote equitable reproductive health in the United States ( 91 ).
Second, routine abortion surveillance is needed to assess trends in clinical practice patterns over time. Information in this report on the number of abortions performed through different methods (e.g., medical or surgical) and at different gestational ages provides the denominator data that are necessary for analyses of the relative safety of abortion practices ( 38 ). Finally, information on the number of pregnancies ending in abortion is needed in conjunction with data on births and fetal losses to estimate the number of pregnancies in the United States and determine rates for various outcomes of public health importance (e.g., adolescent pregnancies) ( 11 ).
Corresponding author: Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. E-mail: [email protected] .
1 Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC
Conflicts of Interest
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
- Gamble SB, Strauss LT, Parker WY, Cook DA, Zane SB, Hamdan S; CDC. Abortion surveillance—United States, 2005. MMWR Surveill Summ 2008;57(No. SS-13). PMID:19037196
- Jones RK, Kost K, Singh S, Henshaw SK, Finer LB. Trends in abortion in the United States. Clin Obstet Gynecol 2009;52:119–29. https://doi.org/10.1097/GRF.0b013e3181a2af8f PMID:19407518
- Pazol K, Zane SB, Parker WY, Hall LR, Berg C, Cook DA; CDC. Abortion surveillance—United States, 2008. MMWR Surveill Summ 2011;60(No. SS-15). PMID:22108620
- Jones RK, Kooistra K. Abortion incidence and access to services in the United States, 2008. Perspect Sex Reprod Health 2011;43:41–50. https://doi.org/10.1363/4304111 PMID:21388504
- Kortsmit K, Jatlaoui TC, Mandel MG, et al. Abortion surveillance—United States, 2018. MMWR Surveill Summ 2020;69(No. SS-7). https://doi.org/10.15585/mmwr.ss6907a1 PMID:33237897
- Jones RK, Witwer E, Jerman J. Abortion incidence and service availability in the United States, 2017. New York, NY: Guttmacher Institute; 2019. https://www.guttmacher.org/report/abortion-incidence-service-availability-us-2017
- Henshaw SK, Silverman J. The characteristics and prior contraceptive use of U.S. abortion patients. Fam Plann Perspect 1988;20:158–68. https://doi.org/10.2307/2135791 PMID:3243346
- Jones RK, Darroch JE, Henshaw SK. Patterns in the socioeconomic characteristics of women obtaining abortions in 2000–2001. Perspect Sex Reprod Health 2002;34:226–35. https://doi.org/10.2307/3097821 PMID:12392215
- Jones RK, Kavanaugh ML. Changes in abortion rates between 2000 and 2008 and lifetime incidence of abortion. Obstet Gynecol 2011;117:1358–66. https://doi.org/10.1097/AOG.0b013e31821c405e PMID:21606746
- Jones RK, Jerman J. Population group abortion rates and lifetime incidence of abortion: United States, 2008–2014. Am J Public Health 2017;107:1904–9. https://doi.org/10.2105/AJPH.2017.304042 PMID:29048970
- Maddow-Zimet I, Kost K. Pregnancies, births and abortions in the United States, 1973–2017: national and state trends by age. New York, NY: Guttmacher Institute; 2021. https://www.guttmacher.org/report/pregnancies-births-abortions-in-united-states-1973-2017
- Guttmacher Institute. Abortion reporting requirements. New York, NY: Guttmacher Institute; 2021. https://www.guttmacher.org/state-policy/explore/abortion-reporting-requirements
- Saul R. Abortion reporting in the United States: an examination of the federal-state partnership. Fam Plann Perspect 1998;30:244–7. https://doi.org/10.2307/2991612 PMID:9782049
- National Center for Health Statistics. Guide to completing the facility worksheets for the certificate of live birth and report of fetal death. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2016. https://www.cdc.gov/nchs/data/dvs/GuidetoCompleteFacilityWks.pdf
- Fritz MA, Speroff L. Clinical gynecologic endocrinology and infertility. Philadelphia, PA: Wolters Kluwer Health; 2012.
- Mifeprex (mifepristone) [Package insert]. New York, NY: Danco Laboratories; 2016.
- Paul M, Lichtenberg ES, Borgatta L, Grimes DA, Stubblefield PG, Creinin MD. Management of unintended and abnormal pregnancy: comprehensive abortion care. Oxford, England: Blackwell Publishing Ltd.; 2009.
- Lichtman AS, Brenner P, Mishell DR Jr. Intrauterine administration of prostaglandin F2alpha as an outpatient procedure for termination of early pregnancy. Contraception 1974;9:403–8. https://doi.org/10.1016/0010-7824(74)90083-3 PMID:4442283
- CDC. Bridged-race population estimates, April 1, 2010. [File census_0401_2010.sas7bdat.zip]. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2011. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#april2010
- CDC. Postcensal estimates of the resident population of the United States as of July 1, 2011, by year, state and county, age, bridged race, sex, and Hispanic origin (Vintage 2011). [File pcen_v2011_y11.sas7bdat]. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2012. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#vintage2011
- CDC. Postcensal estimates of the resident population of the United States as of July 1, 2012, by year, state and county, age, bridged race, sex, and Hispanic origin (Vintage 2012) [File pcen_v2012_y12.sas7bdat]. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2013. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#vintage2012
- CDC. Postcensal estimates of the resident population of the United States as of July 1, 2013, by year, state and county, age, bridged race, sex, and Hispanic origin (Vintage 2013) [File pcen_v2013_y13.sas7bdat]. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2014. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#vintage2013
- CDC. Postcensal estimates of the resident population of the United States as of July 1, 2014, by year, state and county, age, bridged race, sex, and Hispanic origin (Vintage 2014). [File pcen_v2014_y14.sas7bdat]. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2015. http://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#vintage2014
- CDC. Postcensal estimates of the resident population of the United States as of July 1, 2015, by year, state and county, age, bridged race, sex, and Hispanic origin (Vintage 2015). [File pcen_v2015_y15.sas7bdat]. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2016. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#vintage2015
- CDC. Postcensal estimates of the resident population of the United States as of July 1, 2016, by year, state and county, age, bridged race, sex, and Hispanic origin (Vintage 2016). [File pcen_v2016_y16.sas7bdat]. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2017. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#Vintage2016
- CDC. Postcensal estimates of the resident population of the United States as of July 1, 2017, by year, state and county, age, bridged race, sex, and Hispanic origin (Vintage 2017). [File pcen_v2017_y17.sas7bdat]. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2018. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#Vintage2017
- CDC. Postcensal estimates of the resident population of the United States as of July 1, 2018, by year, state and county, age, bridged race, sex, and Hispanic origin (Vintage 2018). [File pcen_v2018_y18.sas7bdat]. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2019. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#Vintage2018
- CDC. Postcensal estimates of the resident population of the United States as of July 1, 2019, by year, state and county, age, bridged race, sex, and Hispanic origin (Vintage 2019). [File pcen_v2019_y19.sas7bdat]. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2020. https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm#Vintage2019
- CDC. Natality files. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics. https://wonder.cdc.gov/Natality.html
- Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2019. Natl Vital Stat Rep 2021;70:1–51. PMID:33814033
- Winikoff B, Dzuba IG, Chong E, et al. Extending outpatient medical abortion services through 70 days of gestational age. Obstet Gynecol 2012;120:1070–6. https://doi.org/10.1097/AOG.0b013e31826c315f PMID:23090524
- National Abortion Federation. 2013 clinical policy guidelines. Washington, DC: National Abortion Federation; 2013. https://www.prochoice.org/pubs_research/publications/documents/2013NAFCPGsforweb.pdf
- Creinin M, Grossman DA. Medical management of first-trimester abortion. Contraception 2014;89:148–61. https://doi.org/10.1016/j.contraception.2014.01.016 PMID:24795934
- Food and Drug Administration. Mifeprex (mifepristone) information. Silver Spring, MD: US Department of Health and Human Services, Food and Drug Administration; 2016. https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm111323.htm
- CDC. Abortion surveillance, 1972. Atlanta, GA: US Department of Health, Education, and Welfare, Public Health Service, CDC; 1974.
- CDC. Abortion surveillance, 1977. Atlanta, GA: US Department of Health, Education, and Welfare, Public Health Service, CDC; 1979.
- CDC. Pregnancy Mortality Surveillance System. Atlanta, GA: US Department of Health and Human Services, CDC; 2020. https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm
- Zane S, Creanga AA, Berg CJ, et al. Abortion-related mortality in the United States: 1998–2010. Obstet Gynecol 2015;126:258–65. https://doi.org/10.1097/AOG.0000000000000945 PMID:26241413
- Hoyert DL. Maternal mortality and related concepts. Vital Health Stat 3 2007;33:1–13. PMID:17460868
- Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol 2012;120:1291–7. https://doi.org/10.1097/AOG.0b013e318273eb56 PMID:23168752
- Biggs MA, Rocca CH, Brindis CD, Hirsch H, Grossman D. Did increasing use of highly effective contraception contribute to declining abortions in Iowa? Contraception 2015;91:167–73. https://doi.org/10.1016/j.contraception.2014.10.009 PMID:25465890
- Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health 2014;46:125–32. https://doi.org/10.1363/46e1714 PMID:24961366
- Roth LP, Sanders JN, Simmons RG, Bullock H, Jacobson E, Turok DK. Changes in uptake and cost of long-acting reversible contraceptive devices following the introduction of a new low-cost levonorgestrel IUD in Utah’s Title X clinics: a retrospective review. Contraception 2018;98:63–8. https://doi.org/10.1016/j.contraception.2018.03.029 PMID:29574095
- Jones RK, Jerman J. Abortion incidence and service availability in the United States, 2011. Perspect Sex Reprod Health 2014;46:3–14. https://doi.org/10.1363/46e0414 PMID:24494995
- Finer LB, Henshaw SK. Abortion incidence and services in the United States in 2000. Perspect Sex Reprod Health 2003;35:6–15. https://doi.org/10.1363/3500603 PMID:12602752
- Henshaw SK. Abortion incidence and services in the United States, 1995–1996. Fam Plann Perspect 1998;30:263–70, 287. https://doi.org/10.2307/2991501 PMID:9859016
- Quast T, Gonzalez F, Ziemba R. Abortion facility closings and abortion rates in Texas. Inquiry 2017;54:46958017700944. https://doi.org/10.1177/0046958017700944 PMID:28351188
- Joyce TJ, Henshaw SK, Dennis A, Finer LB, Blanchard K. The impact of state mandatory counseling and waiting period laws on abortion: a literature review. New York, NY: Guttmacher Institute; 2009. https://www.guttmacher.org/pubs/MandatoryCounseling.pdf
- Sanders JN, Conway H, Jacobson J, Torres L, Turok DK. The longest wait: examining the impact of Utah’s 72-hour waiting period for abortion. Womens Health Issues 2016;26:483–7. https://doi.org/10.1016/j.whi.2016.06.004 PMID:27502901
- Ely G, Polmanteer RSR, Caron A. Access to abortion services in Tennessee: does distance traveled and geographic location influence return for a second appointment as required by the mandatory waiting period policy? Health Soc Work 2019;44:13–21. https://doi.org/10.1093/hsw/hly039 PMID:30561624
- Dennis A, Henshaw SK, Joyce TJ, Finer LB, Blanchard K. The impact of laws requiring parental involvement for abortion: a literature review. New York, NY: Guttmacher Institute; 2009. https://www.guttmacher.org/pubs/ParentalInvolvementLaws.pdf
- Ramesh S, Zimmerman L, Patel A. Impact of parental notification on Illinois minors seeking abortion. J Adolesc Health 2016;58:290–4. https://doi.org/10.1016/j.jadohealth.2015.11.004 PMID:26794433
- Grossman D, Baum S, Fuentes L, et al. Change in abortion services after implementation of a restrictive law in Texas. Contraception 2014;90:496–501. https://doi.org/10.1016/j.contraception.2014.07.006 PMID:25128413
- Joyce T. The supply-side economics of abortion. N Engl J Med 2011;365:1466–9. https://doi.org/10.1056/NEJMp1109889 PMID:22010912
- Grossman D, White K, Hopkins K, Potter JE. Change in distance to nearest facility and abortion in Texas, 2012 to 2014. JAMA 2017;317:437–9. https://doi.org/10.1001/jama.2016.17026 PMID:28114666
- White K, Baum SE, Hopkins K, Potter JE, Grossman D. Change in second-trimester abortion after implementation of a restrictive state law. Obstet Gynecol 2019;133:771–9. https://doi.org/10.1097/AOG.0000000000003183 PMID:30870293
- Jones RK, Ingerick M, Jerman J. Differences in abortion service delivery in hostile, middle-ground, and supportive states in 2014. Womens Health Issues 2018;28:212–8. https://doi.org/10.1016/j.whi.2017.12.003 PMID:29339010
- Guttmacher Institute. A real-time look at the impact of the recession on women’s family planning and pregnancy decisions. New York, NY: Guttmacher Institute; 2009. https://www.guttmacher.org/pubs/RecessionFP.pdf
- Jones RK, Jerman J. Characteristics and circumstances of U.S. women who obtain very early and second-trimester abortions. PLoS One 2017;12:e0169969. https://doi.org/10.1371/journal.pone.0169969 PMID:28121999
- Dehlendorf C, Rodriguez MI, Levy K, Borrero S, Steinauer J. Disparities in family planning. Am J Obstet Gynecol 2010;202:214–20. https://doi.org/10.1016/j.ajog.2009.08.022 PMID:20207237
- Pazol K, Robbins CL, Black LI, et al. Receipt of selected preventive health services for women and men of reproductive age—United States, 2011–2013. MMWR Surveill Summ 2017;66(No. SS-20). https://doi.org/10.15585/mmwr.ss6620a1 PMID:29073129
- Dehlendorf C, Harris LH, Weitz TA. Disparities in abortion rates: a public health approach. Am J Public Health 2013;103:1772–9. https://doi.org/10.2105/AJPH.2013.301339 PMID:23948010
- Buehler JW, Schulz KF, Grimes DA, Hogue CJ. The risk of serious complications from induced abortion: do personal characteristics make a difference? Am J Obstet Gynecol 1985;153:14–20. https://doi.org/10.1016/0002-9378(85)90582-4 PMID:4036997
- Ferris LE, McMain-Klein M, Colodny N, Fellows GF, Lamont J. Factors associated with immediate abortion complications. CMAJ 1996;154:1677–85. PMID:8646655
- Bartlett LA, Berg CJ, Shulman HB, et al. Risk factors for legal induced abortion-related mortality in the United States. Obstet Gynecol 2004;103:729–37. https://doi.org/10.1097/01.AOG.0000116260.81570.60 PMID:15051566
- Lichtenberg ES, Paul M; Society of Family Planning. Surgical abortion prior to 7 weeks of gestation. Contraception 2013;88:7–17. https://doi.org/10.1016/j.contraception.2013.02.008 PMID:23574709
- Foster DG, Kimport K. Who seeks abortions at or after 20 weeks? Perspect Sex Reprod Health 2013;45:210–8. https://doi.org/10.1363/4521013 PMID:24188634
- Jones RK, Finer LB. Who has second-trimester abortions in the United States? Contraception 2012;85:544–51. https://doi.org/10.1016/j.contraception.2011.10.012 PMID:22176796
- Kiley JW, Yee LM, Niemi CM, Feinglass JM, Simon MA. Delays in request for pregnancy termination: comparison of patients in the first and second trimesters. Contraception 2010;81:446–51. https://doi.org/10.1016/j.contraception.2009.12.021 PMID:20399953
- Drey EA, Foster DG, Jackson RA, Lee SJ, Cardenas LH, Darney PD. Risk factors associated with presenting for abortion in the second trimester. Obstet Gynecol 2006;107:128–35. https://doi.org/10.1097/01.AOG.0000189095.32382.d0 PMID:16394050
- Finer LB, Frohwirth LF, Dauphinee LA, Singh S, Moore AM. Timing of steps and reasons for delays in obtaining abortions in the United States. Contraception 2006;74:334–44. https://doi.org/10.1016/j.contraception.2006.04.010 PMID:16982236
- Goyal V, Wallace R, Dermish AI, et al. Factors associated with abortion at 12 or more weeks gestation after implementation of a restrictive Texas law. Contraception 2020;102:314–7. https://doi.org/10.1016/j.contraception.2020.06.007 PMID:32592799
- Janiak E, Kawachi I, Goldberg A, Gottlieb B. Abortion barriers and perceptions of gestational age among women seeking abortion care in the latter half of the second trimester. Contraception 2014;89:322–7. https://doi.org/10.1016/j.contraception.2013.11.009 PMID:24332434
- Kaunitz AM, Rovira EZ, Grimes DA, Schulz KF. Abortions that fail. Obstet Gynecol 1985;66:533–7. PMID:4047543
- Creinin MD, Edwards J. Early abortion: surgical and medical options. Curr Probl Obstet Gynecol Fertil 1997;20:1–32.
- Edwards J, Carson SA. New technologies permit safe abortion at less than six weeks’ gestation and provide timely detection of ectopic gestation. Am J Obstet Gynecol 1997;176:1101–6. https://doi.org/10.1016/S0002-9378(97)70410-1 PMID:9166176
- Paul ME, Mitchell CM, Rogers AJ, Fox MC, Lackie EG. Early surgical abortion: efficacy and safety. Am J Obstet Gynecol 2002;187:407–11. https://doi.org/10.1067/mob.2002.123898 PMID:12193934
- Baldwin MK, Bednarek PH, Russo J. Safety and effectiveness of medication and aspiration abortion before or during the sixth week of pregnancy: A retrospective multicenter study. Contraception 2020;102:13–7. https://doi.org/10.1016/j.contraception.2020.04.004 PMID:32298713
- Kapp N, Baldwin MK, Rodriguez MI. Efficacy of medical abortion prior to 6 gestational weeks: a systematic review. Contraception 2018;97:90–9. https://doi.org/10.1016/j.contraception.2017.09.006 PMID:28935220
- Kapp N, Eckersberger E, Lavelanet A, Rodriguez MI. Medical abortion in the late first trimester: a systematic review. Contraception 2019;99:77–86. https://doi.org/10.1016/j.contraception.2018.11.002 PMID:30444970
- Nippita S, Paul M. Abortion. In: Hatcher R, Nelson A, Trussell J, et al., eds. Contraceptive technology. 21st ed. New York, NY: Ayer Company Publishers, Inc.; 2018:779–827.
- Jerman J, Jones RK, Onda T. Characteristics of U.S. abortion patients in 2014 and changes since 2008. New York, NY: Guttmacher Institute; 2016. https://www.guttmacher.org/sites/default/files/report_pdf/characteristics-us-abortion-patients-2014.pdf
- Jerman J, Frohwirth L, Kavanaugh ML, Blades N. Barriers to abortion care and their consequences for patients traveling for services: qualitative findings from two states. Perspect Sex Reprod Health 2017;49:95–102. https://doi.org/10.1363/psrh.12024 PMID:28394463
- Goyal V, Canfield C, Aiken ARA, Dermish A, Potter JE. Postabortion contraceptive use and continuation when long-acting reversible contraception is free. Obstet Gynecol 2017;129:655–62. https://doi.org/10.1097/AOG.0000000000001926 PMID:28277358
- Gyllenberg FK, Saloranta TH, But A, Gissler M, Heikinheimo O. Induced abortion in a population entitled to free-of-charge long-acting reversible contraception. Obstet Gynecol 2018;132:1453–60. https://doi.org/10.1097/AOG.0000000000002966 PMID:30399102
- Biggs MA, Taylor D, Upadhyay UD. Role of insurance coverage in contraceptive use after abortion. Obstet Gynecol 2017;130:1338–46. https://doi.org/10.1097/AOG.0000000000002361 PMID:29112661
- Boulet SL, D’Angelo DV, Morrow B, et al. Contraceptive use among nonpregnant and postpartum women at risk for unintended pregnancy, and female high school students, in the context of Zika preparedness—United States, 2011–2013 and 2015. MMWR Morb Mortal Wkly Rep 2016;65:780–7. https://doi.org/10.15585/mmwr.mm6530e2 PMID:27490117
- Kumar N, Brown JD. Access barriers to long-acting reversible contraceptives for adolescents. J Adolesc Health 2016;59:248–53. https://doi.org/10.1016/j.jadohealth.2016.03.039 PMID:27247239
- Parks C, Peipert JF. Eliminating health disparities in unintended pregnancy with long-acting reversible contraception (LARC). Am J Obstet Gynecol 2016;214:681–8. https://doi.org/10.1016/j.ajog.2016.02.017 PMID:26875950
- Klein DA, Berry-Bibee EN, Keglovitz Baker K, Malcolm NM, Rollison JM, Frederiksen BN. Providing quality family planning services to LGBTQIA individuals: a systematic review. Contraception 2018;97:378–91. https://doi.org/10.1016/j.contraception.2017.12.016 PMID:29309754
- Holt K, Reed R, Crear-Perry J, Scott C, Wulf S, Dehlendorf C. Beyond same-day long-acting reversible contraceptive access: a person-centered framework for advancing high-quality, equitable contraceptive care. Am J Obstet Gynecol 2020;222(4S):878.e1, 878.e6. https://doi.org/10.1016/j.ajog.2019.11.1279 PMID:31809706
| Year | Selected reporting areas | Continuously reporting areas | ||
|---|---|---|---|---|
| No. | No. (%)** | Rate | Ratio | |
| 2010 | 765,651 | 762,755 (99.6) | 14.4 | 225 |
| 2011 | 730,322 | 727,554 (99.6) | 13.7 | 217 |
| 2012 | 699,202 | 696,587 (99.6) | 13.1 | 208 |
| 2013 | 664,435 | 661,874 (99.6) | 12.4 | 198 |
| 2014 | 652,639 | 649,849 (99.6) | 12.1 | 192 |
| 2015 | 638,169 | 636,902 (99.8) | 11.8 | 188 |
| 2016 | 623,471 | 623,471 (100.0) | 11.6 | 186 |
| 2017 | 612,719 | 609,095 (99.4) | 11.2 | 185 |
| 2018 | 619,591 | 614,820 (99.2) | 11.3 | 189 |
| 2019 | 629,898 | 625,346 (99.3) | 11.4 | 195 |
* Number of abortions per 1,000 women aged 15–44 years. † Number of abortions per 1,000 live births. § For each given year, excludes reporting areas that did not report that year’s abortion numbers to CDC: California (2010–2019), District of Columbia (2016), Maryland (2010–2019), and New Hampshire (2010–2019). ¶ For all years, excludes reporting areas that did not report abortion numbers every year during the period of analysis (2010–2019): California, District of Columbia, Maryland, and New Hampshire. ** Abortions from areas that reported every year during 2010–2019 as a percentage of all reported abortions for a given year.
FIGURE . Number, rate,* and ratio † of abortions performed, by year — selected reporting areas, § United States, 2010–2019
* Number of abortions per 1,000 women aged 15–44 years.
† Number of abortions per 1,000 live births.
§ Data are for 48 reporting areas; excludes California, District of Columbia, Maryland, and New Hampshire.
| State/Area | Abortions reported by area of occurrence** | Abortions obtained by out-of-state residents | ||
|---|---|---|---|---|
| No. | Rate | Ratio | No. (%) | |
| Alabama | 6,009 | 6.3 | 103 | 1,040 (17.3) |
| Alaska | 1,270 | 8.8 | 129 | 19 (1.5) |
| Arizona | 13,097 | 9.4 | 165 | 67 (0.5) |
| Arkansas | 2,963 | 5.1 | 81 | 338 (11.4) |
| Colorado | 9,002 | 7.6 | 143 | 946 (10.5) |
| Connecticut | 9,202 | 13.7 | 269 | 334 (3.6) |
| Delaware | 2,042 | 11.3 | 193 | 277 (13.6) |
| District of Columbia | 4,552 | 23.9 | 501 | 3,126 (68.7) |
| Florida | 71,914 | 18.5 | 327 | 2,256 (3.1) |
| Georgia | 36,907 | 16.9 | 292 | 6,500 (17.6) |
| Hawaii | 2,003 | 7.6 | 119 | 49 (2.4) |
| Idaho | 1,513 | 4.4 | 69 | 78 (5.2) |
| Illinois | 46,517 | 18.6 | 332 | 7,534 (16.2) |
| Indiana | 7,637 | 5.8 | 94 | 618 (8.1) |
| Iowa | 3,566 | 6.0 | 95 | 490 (13.7) |
| Kansas | 6,894 | 12.3 | 195 | 3,372 (48.9) |
| Kentucky | 3,664 | 4.3 | 69 | 643 (17.5) |
| Louisiana | 8,144 | 8.8 | 138 | 1,358 (16.7) |
| Maine | 2,021 | 8.7 | 172 | 107 (5.3) |
| Massachusetts | 18,593 | 13.3 | 269 | 631 (3.4) |
| Michigan | 27,339 | 14.6 | 253 | 1,435 (5.2) |
| Minnesota | 9,940 | 9.2 | 151 | 888 (8.9) |
| Mississippi | 3,194 | 5.5 | 87 | 335 (10.5) |
| Missouri | 1,471 | 1.2 | 20 | 128 (8.7) |
| Montana | 1,568 | 8.0 | 142 | 169 (10.8) |
| Nebraska | 2,068 | 5.5 | 84 | 267 (12.9) |
| Nevada | 8,414 | 14.0 | 240 | 434 (5.2) |
| New Jersey | 22,178 | 13.2 | 223 | 1,309 (5.9) |
| New Mexico | 3,942 | 9.9 | 172 | 939 (23.8) |
| New York | 78,587 | 20.3 | 355 | start highlight4,166 (5.3)end highlight |
| New York City | 49,784 | 27.2 | 472 | 4,668 (9.4) |
| New York State | 28,803 | 14.1 | 248 | 2,321 (8.1) |
| North Carolina | 28,450 | 13.8 | 240 | 5,079 (17.9) |
| North Dakota | 1,121 | 7.6 | 107 | 289 (25.8) |
| Ohio | 20,102 | 9.1 | 150 | 1,186 (5.9) |
| Oklahoma | 4,995 | 6.4 | 102 | 407 (8.1) |
| Oregon | 8,688 | 10.5 | 208 | 795 (9.2) |
| Pennsylvania | 31,018 | 13.0 | 231 | 2,222 (7.2) |
| Rhode Island | 2,099 | 10.1 | 206 | 274 (13.1) |
| South Carolina | 5,101 | 5.2 | 89 | 312 (6.1) |
| South Dakota | 414 | 2.6 | 36 | 82 (19.8) |
| Tennessee | 9,719 | 7.3 | 121 | 1,823 (18.8) |
| Texas | 57,275 | 9.5 | 152 | 1,303 (2.3) |
| Utah | 2,922 | 4.2 | 62 | 146 (5.0) |
| Vermont | 1,195 | 10.4 | 223 | 265 (22.2) |
| Virginia | 15,601 | 9.2 | 160 | 867 (5.6) |
| Washington | 17,262 | 11.4 | 203 | 848 (4.9) |
| West Virginia | 1,183 | 3.8 | 65 | 168 (14.2) |
| Wisconsin | 6,511 | 6.0 | 103 | 139 (2.1) |
| Wyoming | 31 | 0.3 | 5 | 5 (16.1) |
Abbreviation: NA = not applicable. * Number of abortions per 1,000 women aged 15–44 years. † Number of abortions per 1,000 live births. § Additional details on the reporting area in which abortions were provided, cross-tabulated by the state/area of residence, are available at https://www.cdc.gov/reproductivehealth/data_stats/Abortion.htm . ¶ Data from 49 reporting areas; excludes three reporting areas (California, Maryland, and New Hampshire) that did not report or did not meet reporting standards. ** The total abortions include those with known and unknown residence status. †† Reporting to the central health agency is not required. Data are requested from hospitals and licensed ambulatory care facilities only.
| State/Area | Age group (yrs) | Total abortions reported by known age | ||||||
|---|---|---|---|---|---|---|---|---|
| <15 | 15–19 | 20–24 | 25–29 | 30–34 | 35–39 | ≥40 | ||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (% of all reported abortions) | |
| Alabama | 23 (0.4) | 526 (8.8) | 1,807 (30.1) | 1,783 (29.7) | 1,119 (18.6) | 565 (9.4) | 183 (3.0) | |
| Alaska | — | 123 (9.7) | 351 (27.6) | 363 (28.6) | 246 (19.4) | 137 (10.8) | — | |
| Arizona | 19 (0.1) | 1,163 (8.9) | 3,932 (30.0) | 3,631 (27.7) | 2,446 (18.7) | 1,420 (10.8) | 482 (3.7) | |
| Arkansas | 10 (0.3) | 294 (9.9) | 892 (30.1) | 901 (30.4) | 513 (17.3) | 260 (8.8) | 90 (3.0) | |
| Colorado | 27 (0.3) | 812 (9.0) | 2,596 (28.9) | 2,557 (28.4) | 1,735 (19.3) | 948 (10.5) | 319 (3.5) | |
| Connecticut | 20 (0.2) | 788 (8.7) | 2,382 (26.3) | 2,600 (28.8) | 1,885 (20.9) | 1,042 (11.5) | 323 (3.6) | |
| Delaware | 8 (0.4) | 240 (11.8) | 575 (28.2) | 574 (28.1) | 388 (19.0) | 209 (10.2) | 48 (2.4) | |
| District of Columbia | 10 (0.2) | 386 (8.5) | 1,262 (27.7) | 1,388 (30.5) | 870 (19.1) | 483 (10.6) | 152 (3.3) | |
| Florida | 118 (0.2) | 5,231 (7.3) | 18,889 (26.5) | 20,741 (29.1) | 15,051 (21.1) | 8,425 (11.8) | 2,907 (4.1) | |
| Georgia | 71 (0.2) | 2,832 (7.7) | 10,185 (27.6) | 11,361 (30.8) | 7,254 (19.7) | 3,932 (10.7) | 1,272 (3.4) | |
| Hawaii | 6 (0.3) | 190 (9.5) | 549 (27.4) | 546 (27.3) | 381 (19.0) | 238 (11.9) | 93 (4.6) | |
| Idaho | — | 187 (12.4) | 477 (31.5) | 378 (25.0) | 252 (16.7) | 161 (10.6) | — | |
| Illinois** | 75 (0.2) | 3,492 (9.1) | 10,960 (28.4) | 11,819 (30.6) | 7,166 (18.6) | 3,813 (9.9) | 1,255 (3.3) | |
| Indiana | 18 (0.2) | 768 (10.1) | 2,324 (30.4) | 2,168 (28.4) | 1,354 (17.7) | 745 (9.8) | 260 (3.4) | |
| Iowa | 12 (0.3) | 357 (10.0) | 957 (26.8) | 1,000 (28.1) | 679 (19.0) | 401 (11.2) | 159 (4.5) | |
| Kansas | 12 (0.2) | 632 (9.2) | 2,148 (31.2) | 1,932 (28.0) | 1,239 (18.0) | 692 (10.0) | 239 (3.5) | |
| Kentucky | 11 (0.3) | 294 (8.0) | 1,071 (29.2) | 1,069 (29.2) | 719 (19.6) | 384 (10.5) | 116 (3.2) | |
| Louisiana | 26 (0.3) | 726 (8.9) | 2,302 (28.3) | 2,521 (31.0) | 1,534 (18.8) | 782 (9.6) | 253 (3.1) | |
| Maine | 5 (0.2) | 198 (9.8) | 585 (29.0) | 534 (26.4) | 381 (18.9) | 254 (12.6) | 63 (3.1) | |
| Massachusetts | 28 (0.2) | 1,306 (7.0) | 4,613 (24.8) | 5,313 (28.6) | 4,028 (21.7) | 2,390 (12.9) | 910 (4.9) | |
| Michigan | 51 (0.2) | 2,328 (8.6) | 7,538 (27.7) | 8,697 (32.0) | 5,201 (19.1) | 2,545 (9.4) | 831 (3.1) | |
| Minnesota | 26 (0.3) | 823 (8.3) | 2,693 (27.1) | 2,837 (28.6) | 2,015 (20.3) | 1,205 (12.1) | 336 (3.4) | |
| Mississippi | 7 (0.2) | 295 (9.2) | 970 (30.4) | 1,003 (31.4) | 574 (18.0) | 276 (8.6) | 69 (2.2) | |
| Missouri | 5 (0.3) | 141 (9.6) | 422 (28.7) | 436 (29.6) | 253 (17.2) | 156 (10.6) | 58 (3.9) | |
| Montana | 5 (0.3) | 157 (10.0) | 458 (29.2) | 454 (29.0) | 269 (17.2) | 161 (10.3) | 64 (4.1) | |
| Nebraska | 7 (0.3) | 187 (9.0) | 625 (30.2) | 534 (25.8) | 400 (19.3) | 234 (11.3) | 81 (3.9) | |
| Nevada | 19 (0.2) | 691 (8.6) | 2,200 (27.2) | 2,257 (27.9) | 1,630 (20.2) | 918 (11.4) | 363 (4.5) | |
| New Jersey | 50 (0.2) | 1,958 (8.8) | 5,648 (25.5) | 6,497 (29.3) | 4,462 (20.1) | 2,604 (11.7) | 959 (4.3) | |
| New Mexico | 22 (0.6) | 507 (13.8) | 1,111 (30.3) | 921 (25.1) | 621 (16.9) | 379 (10.3) | 104 (2.8) | |
| New York | 186 (0.2) | 6,919 (8.8) | 20,238 (25.8) | 22,267 (28.4) | 16,014 (20.4) | 9,438 (12.0) | 3,386 (4.3) | |
| New York City | 109 (0.2) | 4,052 (8.1) | 12,471 (25.1) | 14,159 (28.4) | 10,414 (20.9) | 6,260 (12.6) | 2,318 (4.7) | |
| New York State | 77 (0.3) | 2,867 (10.0) | 7,767 (27.1) | 8,108 (28.3) | 5,600 (19.5) | 3,178 (11.1) | 1,068 (3.7) | |
| North Carolina | 60 (0.2) | 2,252 (8.3) | 7,768 (28.8) | 8,270 (30.6) | 5,095 (18.9) | 2,687 (9.9) | 880 (3.3) | |
| North Dakota | 0 (—) | 121 (10.8) | 349 (31.1) | 326 (29.1) | 189 (16.9) | 107 (9.5) | 29 (2.6) | |
| Ohio | 63 (0.3) | 1,737 (8.6) | 5,887 (29.3) | 6,057 (30.1) | 3,720 (18.5) | 1,983 (9.9) | 655 (3.3) | |
| Oklahoma | 89 (1.8) | 440 (8.8) | 1,517 (30.4) | 1,384 (27.7) | 901 (18.0) | 491 (9.8) | 172 (3.4) | |
| Oregon | 19 (0.2) | 837 (9.6) | 2,373 (27.3) | 2,326 (26.8) | 1,702 (19.6) | 1,049 (12.1) | 382 (4.4) | |
| Pennsylvania | 71 (0.2) | 2,474 (8.0) | 8,435 (27.2) | 9,529 (30.7) | 6,188 (19.9) | 3,244 (10.5) | 1,077 (3.5) | |
| Rhode Island | — | 185 (8.8) | 611 (29.1) | 584 (27.8) | 411 (19.6) | 222 (10.6) | — | |
| South Carolina | 10 (0.2) | 499 (9.8) | 1,403 (27.5) | 1,500 (29.4) | 961 (18.8) | 544 (10.7) | 184 (3.6) | |
| South Dakota | — | — | 129 (31.2) | 117 (28.3) | 61 (14.7) | 45 (10.9) | — | |
| Tennessee | 17 (0.2) | 830 (8.6) | 2,884 (29.8) | 2,982 (30.8) | 1,791 (18.5) | 913 (9.4) | 275 (2.8) | |
| Texas | 106 (0.2) | 5,041 (8.8) | 16,647 (29.1) | 16,327 (28.5) | 10,907 (19.0) | 6,152 (10.7) | 2,095 (3.7) | |
| Utah | 6 (0.2) | 371 (12.7) | 915 (31.3) | 761 (26.0) | 470 (16.1) | 305 (10.4) | 94 (3.2) | |
| Vermont | — | 108 (9.1) | 305 (25.6) | 322 (27.0) | 247 (20.7) | 153 (12.8) | — | |
| Virginia | 25 (0.2) | 1,108 (7.1) | 4,162 (26.7) | 4,626 (29.7) | 3,186 (20.4) | 1,869 (12.0) | 605 (3.9) | |
| Washington | 32 (0.2) | 1,647 (9.6) | 4,598 (26.7) | 4,723 (27.4) | 3,367 (19.5) | 2,095 (12.2) | 765 (4.4) | |
| West Virginia | 8 (0.7) | 115 (9.7) | 377 (31.9) | 320 (27.0) | 194 (16.4) | 136 (11.5) | 33 (2.8) | |
| Wisconsin | 17 (0.3) | 690 (10.6) | 1,917 (29.4) | 1,806 (27.7) | 1,202 (18.5) | 637 (9.8) | 242 (3.7) | |
| Wyoming | — | — | 6 (19.4) | 10 (32.3) | 8 (25.8) | 6 (19.4) | — | |
Abbreviation: NA = not applicable. * Data from 49 reporting areas; excludes three reporting areas (California, Maryland, and New Hampshire) that did not report, did not report by age, or did not meet reporting standards. † Percentages for the individual component categories might not add to 100% because of rounding. § Percentage is calculated as the number of abortions reported by known age divided by the sum of abortions reported by known and unknown age. Values ≥99.95% are rounded to 100.0%. ¶ Cells with a value in the range of 1–4 or cells that would allow for calculation of these small values have been suppressed. ** Includes residents only. †† Reporting to the central health agency is not required. Data are requested from hospitals and licensed ambulatory care facilities only. §§ Percentage based on a total of 622,137 abortions reported among the areas that met reporting standards for age; reporting standards for age were applied to abortions for residents of Illinois only. ¶¶ Number of abortions obtained by women in a given age group per 1,000 women in that same age group. Adolescents aged 13–14 years were used as the denominator for the group of adolescents aged <15 years, and women aged 40–44 years were used as the denominator for the group of women aged ≥40 years. For the total abortion rate only, abortions for women of unknown age were distributed according to the distribution of abortions among women of known age. *** Number of abortions obtained by women in a given age group per 1,000 live births to women in that same age group. For the total abortion ratio only, abortions for women of unknown age were distributed according to the distribution of abortions among women of known age.
| Age group (yrs) | Year | % Change | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2010 to 2014 | 2015 to 2019 | 2018 to 2019 | 2010 to 2019 | |
| <15 | 0.5 | 0.4 | 0.4 | 0.3 | 0.3 | 0.3 | 0.3 | 0.2 | 0.2 | 0.2 | −40.0 | −33.3 | 0.0 | −60.0 |
| 15–19 | 14.6 | 13.5 | 12.2 | 11.4 | 10.4 | 9.8 | 9.4 | 9.1 | 8.8 | 8.7 | −28.8 | −11.2 | −1.1 | −40.4 |
| 20–24 | 32.9 | 32.9 | 32.8 | 32.7 | 32.1 | 31.1 | 30.0 | 29.3 | 28.5 | 27.8 | −2.4 | −10.6 | −2.5 | −15.5 |
| 25–29 | 24.5 | 24.9 | 25.4 | 25.9 | 26.8 | 27.6 | 28.5 | 29.0 | 29.4 | 29.3 | 9.4 | 6.2 | −0.3 | 19.6 |
| 30–34 | 15.3 | 15.8 | 16.4 | 16.8 | 17.2 | 17.7 | 18.0 | 18.3 | 18.8 | 19.4 | 12.4 | 9.6 | 3.2 | 26.8 |
| 35–39 | 8.9 | 8.9 | 9.1 | 9.2 | 9.7 | 10.0 | 10.3 | 10.5 | 10.7 | 10.8 | 9.0 | 8.0 | 0.9 | 21.3 |
| ≥40 | 3.4 | 3.6 | 3.7 | 3.6 | 3.6 | 3.6 | 3.6 | 3.6 | 3.5 | 3.7 | 5.9 | 2.8 | 5.7 | 8.8 |
| <15 | 1.0 | 0.9 | 0.8 | 0.6 | 0.5 | 0.5 | 0.4 | 0.4 | 0.4 | 0.4 | −50.0 | −20.0 | 0.0 | −60.0 |
| 15–19 | 11.7 | 10.5 | 9.2 | 8.2 | 7.3 | 6.7 | 6.2 | 5.9 | 5.8 | 5.8 | −37.6 | −13.4 | 0.0 | −50.4 |
| 20–24 | 26.8 | 25.0 | 23.3 | 21.9 | 20.9 | 19.9 | 19.0 | 18.4 | 18.2 | 18.1 | −22.0 | −9.0 | −0.5 | −32.5 |
| 25–29 | 20.2 | 19.5 | 18.9 | 18.2 | 18.1 | 17.9 | 17.7 | 17.3 | 17.6 | 17.8 | −10.4 | −0.6 | 1.1 | −11.9 |
| 30–34 | 13.2 | 12.7 | 12.4 | 11.8 | 11.7 | 11.7 | 11.6 | 11.5 | 11.9 | 12.3 | −11.4 | 5.1 | 3.4 | −6.8 |
| 35–39 | 7.6 | 7.5 | 7.3 | 7.0 | 7.1 | 7.0 | 6.9 | 6.7 | 6.8 | 7.0 | −6.6 | 0.0 | 2.9 | −7.9 |
| ≥40 | 2.8 | 2.8 | 2.8 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.6 | −10.7 | 4.0 | 4.0 | −7.1 |
| <15 | 848 | 839 | 804 | 791 | 745 | 699 | 729 | 777 | 853 | 851 | −12.1 | 21.7 | −0.2 | 0.4 |
| 15–19 | 332 | 326 | 304 | 300 | 291 | 289 | 295 | 301 | 318 | 332 | −12.3 | 14.9 | 4.4 | 0.0 |
| 20–24 | 291 | 284 | 272 | 262 | 256 | 250 | 249 | 249 | 256 | 260 | −12.0 | 4.0 | 1.6 | −10.7 |
| 25–29 | 184 | 178 | 174 | 169 | 167 | 167 | 169 | 171 | 178 | 183 | −9.2 | 9.6 | 2.8 | −0.5 |
| 30–34 | 138 | 132 | 128 | 122 | 116 | 115 | 113 | 114 | 119 | 124 | −15.9 | 7.8 | 4.2 | −10.1 |
| 35–39 | 171 | 165 | 158 | 148 | 145 | 140 | 136 | 134 | 135 | 137 | −15.2 | −2.1 | 1.5 | −19.9 |
| ≥40 | 274 | 275 | 269 | 245 | 239 | 228 | 218 | 211 | 206 | 213 | −12.8 | −6.6 | 3.4 | −22.3 |
| ** | ||||||||||||||
Abbreviation: NA = not applicable. * Number of abortions obtained by women in a given age group per 1,000 women in that same age group. Adolescents aged 13–14 years were used as the denominator for the group of adolescents aged <15 years, and women aged 40–44 years were used as the denominator for the group of women aged ≥40 years. Abortions for women of unknown age were distributed according to the distribution of abortions among women of known age. † Number of abortions obtained by women in a given age group per 1,000 live births to women in that same age group. Abortions for women of unknown age were distributed according to the distribution of abortions among women of known age. § Data from 44 reporting areas; excludes eight reporting areas (California, District of Columbia, Florida, Maine, Maryland, New Hampshire, Vermont, and Wyoming) that did not report, did not report by age, or did not meet reporting standards for ≥1 year. ¶ By year, the total number of abortions represents 99.4%–99.7% of all abortions reported to CDC among the areas that met reporting standards for age during 2010–2019; reporting standards for age were applied to abortions for residents of Illinois only. ** The total number is different than previously reported because the totals by known age are presented and data for out-of-state residents were subsequently added for Wisconsin.
| State/Area | Age group (yrs) | Total no. | |||||
|---|---|---|---|---|---|---|---|
| <15 | 15 | 16 | 17 | 18 | 19 | ||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | ||
| Alabama | 23 (4.2) | 23 (4.2) | 43 (7.8) | 65 (11.8) | 171 (31.1) | 224 (40.8) | |
| Alaska | — | — | — | — | — | — | |
| Arizona | 19 (1.6) | 40 (3.4) | 79 (6.7) | 150 (12.7) | 367 (31.0) | 527 (44.6) | |
| Arkansas | 10 (3.3) | 22 (7.2) | 33 (10.9) | 36 (11.8) | 87 (28.6) | 116 (38.2) | |
| Colorado | 27 (3.2) | 39 (4.6) | 62 (7.4) | 130 (15.5) | 259 (30.9) | 322 (38.4) | |
| Delaware | 8 (3.2) | 12 (4.8) | 21 (8.5) | 43 (17.3) | 70 (28.2) | 94 (37.9) | |
| District of Columbia | 10 (2.5) | 19 (4.8) | 35 (8.8) | 74 (18.7) | 99 (25.0) | 159 (40.2) | |
| Florida | 118 (2.2) | 199 (3.7) | 402 (7.5) | 689 (12.9) | 1,585 (29.6) | 2,356 (44.0) | |
| Georgia | 71 (2.4) | 115 (4.0) | 209 (7.2) | 383 (13.2) | 860 (29.6) | 1,265 (43.6) | |
| Hawaii | 6 (3.1) | 9 (4.6) | 15 (7.7) | 31 (15.8) | 48 (24.5) | 87 (44.4) | |
| Idaho | — | — | — | — | — | — | |
| Indiana | 18 (2.3) | 35 (4.5) | 67 (8.5) | 103 (13.1) | 234 (29.8) | 329 (41.9) | |
| Iowa | 12 (3.3) | 24 (6.5) | 36 (9.8) | 49 (13.3) | 108 (29.3) | 140 (37.9) | |
| Kansas | 12 (1.9) | 28 (4.3) | 46 (7.1) | 75 (11.6) | 216 (33.5) | 267 (41.5) | |
| Kentucky | 11 (3.6) | 16 (5.2) | 24 (7.9) | 33 (10.8) | 82 (26.9) | 139 (45.6) | |
| Louisiana | 26 (3.5) | 54 (7.2) | 74 (9.8) | 134 (17.8) | 200 (26.6) | 264 (35.1) | |
| Maine | 5 (2.5) | 14 (6.9) | 16 (7.9) | 33 (16.3) | 54 (26.6) | 81 (39.9) | |
| Massachusetts | 28 (2.1) | 43 (3.2) | 100 (7.5) | 169 (12.7) | 383 (28.7) | 611 (45.8) | |
| Michigan | 51 (2.1) | 134 (5.6) | 191 (8.0) | 318 (13.4) | 658 (27.7) | 1,027 (43.2) | |
| Minnesota | 26 (3.1) | 43 (5.1) | 68 (8.0) | 122 (14.4) | 255 (30.0) | 335 (39.5) | |
| Mississippi | 7 (2.3) | 26 (8.6) | 24 (7.9) | 44 (14.6) | 90 (29.8) | 111 (36.8) | |
| Missouri | 5 (3.4) | 15 (10.3) | 12 (8.2) | 27 (18.5) | 37 (25.3) | 50 (34.2) | |
| Montana | 5 (3.1) | 10 (6.2) | 17 (10.5) | 26 (16.0) | 42 (25.9) | 62 (38.3) | |
| Nebraska | 7 (3.6) | 10 (5.2) | 15 (7.7) | 34 (17.5) | 37 (19.1) | 91 (46.9) | |
| Nevada | 19 (2.7) | 37 (5.2) | 62 (8.7) | 101 (14.2) | 219 (30.8) | 272 (38.3) | |
| New Jersey | 50 (2.5) | 84 (4.2) | 206 (10.3) | 344 (17.1) | 539 (26.8) | 785 (39.1) | |
| New Mexico | 22 (4.2) | 34 (6.4) | 65 (12.3) | 93 (17.6) | 120 (22.7) | 195 (36.9) | |
| New York | 186 (2.6) | 316 (4.4) | 657 (9.2) | 1,218 (17.1) | 2,026 (28.5) | 2,702 (38.0) | |
| New York City | 109 (2.6) | 192 (4.6) | 406 (9.8) | 735 (17.7) | 1,170 (28.1) | 1,549 (37.2) | |
| New York State | 77 (2.6) | 124 (4.2) | 251 (8.5) | 483 (16.4) | 856 (29.1) | 1,153 (39.2) | |
| North Carolina | 60 (2.6) | 112 (4.8) | 186 (8.0) | 282 (12.2) | 689 (29.8) | 983 (42.5) | |
| North Dakota | 0 (—) | 6 (5.0) | 13 (10.7) | 16 (13.2) | 33 (27.3) | 53 (43.8) | |
| Ohio | 63 (3.5) | 89 (4.9) | 147 (8.2) | 239 (13.3) | 516 (28.7) | 746 (41.4) | |
| Oklahoma | 89 (16.8) | 19 (3.6) | 29 (5.5) | 67 (12.7) | 145 (27.4) | 180 (34.0) | |
| Oregon | 19 (2.2) | 35 (4.1) | 76 (8.9) | 136 (15.9) | 218 (25.5) | 372 (43.5) | |
| Pennsylvania | 71 (2.8) | 116 (4.6) | 224 (8.8) | 346 (13.6) | 736 (28.9) | 1,052 (41.3) | |
| Rhode Island | — | — | — | — | — | — | |
| South Carolina | 10 (2.0) | 16 (3.1) | 42 (8.3) | 115 (22.6) | 138 (27.1) | 188 (36.9) | |
| South Dakota | — | — | — | — | — | — | |
| Tennessee | 17 (2.0) | 38 (4.5) | 76 (9.0) | 108 (12.8) | 238 (28.1) | 370 (43.7) | |
| Texas | 106 (2.1) | 213 (4.1) | 426 (8.3) | 677 (13.2) | 1,449 (28.2) | 2,276 (44.2) | |
| Utah | 6 (1.6) | 13 (3.4) | 23 (6.1) | 49 (13.0) | 119 (31.6) | 167 (44.3) | |
| Vermont | — | — | — | — | — | — | |
| Virginia | 25 (2.2) | 57 (5.0) | 82 (7.2) | 138 (12.2) | 325 (28.7) | 506 (44.7) | |
| Washington | 32 (1.9) | 74 (4.4) | 145 (8.6) | 277 (16.5) | 477 (28.4) | 674 (40.1) | |
| West Virginia | 8 (6.5) | 5 (4.1) | 7 (5.7) | 19 (15.4) | 35 (28.5) | 49 (39.8) | |
| Wisconsin** | 17 (2.5) | 27 (4.0) | 73 (10.8) | 77 (11.4) | 195 (28.8) | 289 (42.6) | |
| Wyoming | — | — | — | — | — | — | |
Abbreviation: NA = not applicable. * Data from 47 reporting areas; excludes five reporting areas (California, Connecticut, Illinois, Maryland, and New Hampshire) that did not report, did not report age among adolescents by individual year, or did not meet reporting standards. † Percentages for the individual component categories might not add to 100% because of rounding. § Cells with a value in the range of 1–4 or cells that would allow for calculation of these small values have been suppressed. ¶ Reporting to the central health agency is not required. Data are requested from hospitals and licensed ambulatory care facilities only. ** Includes residents only. †† Number of abortions obtained by women in a given age group per 1,000 women in that same age group. Adolescents aged 13–14 years were used as the denominator for the group of adolescents aged <15 years. For the total abortion rate only, abortions for women of unknown age were distributed according to the distribution of abortions among women of known age. §§ Number of abortions obtained by women in a given age group per 1,000 live births to women in that same age group. For the total abortion ratio only, abortions for women of unknown age were distributed according to the distribution of abortions among women of known age.
| State/Area | Non-Hispanic | Hispanic | Total abortions reported by known race/ethnicity | ||
|---|---|---|---|---|---|
| White | Black | Other | |||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (% of all reported abortions) | |
| Alabama | 1,823 (30.4) | 3,717 (61.9) | 142 (2.4) | 323 (5.4) | |
| Alaska | 584 (49.0) | 85 (7.1) | 470 (39.5) | 52 (4.4) | |
| Arizona | 4,821 (38.4) | 1,376 (10.9) | 1,241 (9.9) | 5,130 (40.8) | |
| Arkansas | 1,277 (44.0) | 1,370 (47.2) | 68 (2.3) | 190 (6.5) | |
| Connecticut | 3,122 (37.4) | 2,754 (33.0) | 506 (6.1) | 1,971 (23.6) | |
| Delaware | 863 (42.5) | 850 (41.9) | 72 (3.5) | 244 (12.0) | |
| District of Columbia | 831 (18.8) | 2,365 (53.4) | 517 (11.7) | 717 (16.2) | |
| Florida | 20,576 (30.9) | 23,072 (34.6) | 3,189 (4.8) | 19,829 (29.7) | |
| Georgia | 7,102 (21.2) | 21,709 (64.9) | 1,724 (5.2) | 2,924 (8.7) | |
| Idaho | 939 (67.5) | 39 (2.8) | 68 (4.9) | 346 (24.9) | |
| Indiana | 3,919 (51.6) | 2,404 (31.6) | 583 (7.7) | 691 (9.1) | |
| Kansas | 3,722 (54.0) | 1,631 (23.7) | 534 (7.8) | 1,000 (14.5) | |
| Kentucky | 2,041 (55.7) | 1,236 (33.7) | 133 (3.6) | 253 (6.9) | |
| Michigan | 10,578 (39.9) | 13,687 (51.6) | 1,201 (4.5) | 1,041 (3.9) | |
| Minnesota | 4,310 (46.8) | 2,569 (27.9) | 1,392 (15.1) | 937 (10.2) | |
| Mississippi | 619 (19.5) | 2,352 (74.0) | 114 (3.6) | 95 (3.0) | |
| Montana | 1,293 (82.5) | — | 142 (9.1) | — | |
| Nevada | 2,841 (37.0) | 1,409 (18.4) | 924 (12.0) | 2,497 (32.6) | |
| New Jersey** | 5,133 (26.7) | 7,453 (38.8) | 3,206 (16.7) | 3,427 (17.8) | |
| New Mexico | 930 (27.6) | 160 (4.8) | 380 (11.3) | 1,897 (56.3) | |
| North Carolina | 8,096 (30.7) | 12,968 (49.2) | 1,990 (7.6) | 3,298 (12.5) | |
| South Carolina | 2,481 (48.8) | 1,986 (39.0) | 232 (4.6) | 390 (7.7) | |
| South Dakota | 259 (62.6) | 46 (11.1) | 69 (16.7) | 40 (9.7) | |
| Tennessee | 3,688 (38.9) | 4,842 (51.0) | 363 (3.8) | 595 (6.3) | |
| Texas | 15,066 (26.3) | 15,921 (27.8) | 3,989 (7.0) | 22,217 (38.8) | |
| Utah | 1,721 (60.4) | 133 (4.7) | 214 (7.5) | 779 (27.4) | |
| Vermont | 1,045 (89.7) | 47 (4.0) | 41 (3.5) | 32 (2.7) | |
| Virginia | 4,802 (33.6) | 6,515 (45.5) | 1,512 (10.6) | 1,476 (10.3) | |
| West Virginia | 987 (83.4) | 153 (12.9) | — | — | |
| Wyoming | 17 (60.7) | — | — | 8 (28.6) | |
| *** | |||||
Abbreviation: NA = not applicable. * Data from 30 reporting areas; excludes 22 reporting areas (California, Colorado, Hawaii, Illinois, Iowa, Louisiana, Maine, Maryland, Massachusetts, Missouri, Nebraska, New Hampshire, New York City, New York State, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, Washington, and Wisconsin) that did not report, did not report by race/ethnicity, or did not meet reporting standards. † Percentages for the individual component categories might not add to 100% because of rounding. § Percentage is calculated as the number of abortions reported by known race/ethnicity divided by the sum of abortions reported by known and unknown race/ethnicity. Values ≥99.95% are rounded to 100.0%. ¶ Cells with a value in the range of 1–4 or cells that would allow for calculation of these small values have been suppressed. ** Reporting to the central health agency is not required. Data are requested from hospitals and licensed ambulatory care facilities only. †† Reporting form contains only one question for race/ethnicity; therefore, abortions reported for women of White, Black, and other races (Asian and Native American) are not explicitly identified as non-Hispanic. §§ Percentage based on a total of 366,130 abortions reported among the areas that met reporting standards for race/ethnicity. ¶¶ Number of abortions obtained by women in a given racial/ethnic group per 1,000 women in that same racial/ethnic group. For the total abortion rate only, abortions for women of unknown race/ethnicity were distributed according to the distribution of abortions among women of known race/ethnicity. *** Number of abortions obtained by women in a given racial/ethnic group per 1,000 live births to women in that same racial/ethnic group. For the total abortion ratio only, abortions for women of unknown race/ethnicity were distributed according to the distribution of abortions among women of known race/ethnicity.
| State/Area | Marital status | Total abortions reported by known marital status | |
|---|---|---|---|
| Married | Unmarried | ||
| No. (%) | No. (%) | No. (% of all reported abortions) | |
| Alabama | 663 (11.0) | 5,342 (89.0) | |
| Alaska | 253 (21.1) | 945 (78.9) | |
| Arizona | 1,878 (14.3) | 11,219 (85.7) | |
| Arkansas | 376 (12.7) | 2,575 (87.3) | |
| Colorado | 1,559 (19.1) | 6,596 (80.9) | |
| Connecticut | 939 (11.5) | 7,232 (88.5) | |
| Delaware | 224 (11.0) | 1,818 (89.0) | |
| Florida | 10,136 (16.1) | 52,629 (83.9) | |
| Georgia | 4,410 (12.8) | 30,033 (87.2) | |
| Idaho | 302 (21.6) | 1,094 (78.4) | |
| Illinois | 3,575 (9.5) | 33,868 (90.5) | |
| Indiana | 1,094 (14.3) | 6,543 (85.7) | |
| Iowa | 633 (17.8) | 2,925 (82.2) | |
| Kansas | 1,063 (15.5) | 5,811 (84.5) | |
| Kentucky | 525 (14.3) | 3,139 (85.7) | |
| Louisiana | 828 (10.5) | 7,063 (89.5) | |
| Maine | 308 (16.0) | 1,612 (84.0) | |
| Michigan | 2,660 (10.3) | 23,095 (89.7) | |
| Minnesota | 1,535 (16.2) | 7,959 (83.8) | |
| Mississippi | 290 (9.1) | 2,893 (90.9) | |
| Missouri | 224 (16.0) | 1,179 (84.0) | |
| Montana | 286 (18.2) | 1,282 (81.8) | |
| Nebraska | 306 (15.0) | 1,732 (85.0) | |
| New Jersey** | 2,515 (11.5) | 19,372 (88.5) | |
| New Mexico | 563 (15.3) | 3,128 (84.7) | |
| New York City | 8,269 (18.5) | 36,518 (81.5) | |
| North Carolina | 3,622 (14.4) | 21,547 (85.6) | |
| North Dakota | 162 (14.5) | 958 (85.5) | |
| Ohio | 2,603 (14.0) | 16,027 (86.0) | |
| Oklahoma | 941 (18.9) | 4,043 (81.1) | |
| Oregon | 1,573 (20.3) | 6,193 (79.7) | |
| Pennsylvania | 3,766 (12.2) | 27,221 (87.8) | |
| Rhode Island | 263 (12.9) | 1,782 (87.1) | |
| South Carolina | 726 (14.4) | 4,331 (85.6) | |
| South Dakota | 85 (20.5) | 329 (79.5) | |
| Tennessee | 1,295 (14.0) | 7,985 (86.0) | |
| Texas | 9,784 (17.1) | 47,363 (82.9) | |
| Utah | 724 (24.9) | 2,182 (75.1) | |
| Vermont | 216 (20.3) | 847 (79.7) | |
| Virginia | 2,349 (15.1) | 13,252 (84.9) | |
| West Virginia | 203 (17.2) | 979 (82.8) | |
| Wisconsin | 852 (13.2) | 5,615 (86.8) | |
Abbreviation: NA = not applicable. * Data from 42 reporting areas; excludes 10 reporting areas (California, District of Columbia, Hawaii, Maryland, Massachusetts, Nevada, New Hampshire, New York State, Washington, and Wyoming) that did not report, did not report by marital status, or did not meet reporting standards. † Percentages for the individual component categories might not add to 100% because of rounding. § Percentage is calculated as the number of abortions reported by known marital status divided by the sum of abortions reported by known and unknown marital status. Values ≥99.95% are rounded to 100.0%. ¶ Includes residents only. ** Reporting to the central health agency is not required. Data are requested from hospitals and licensed ambulatory care facilities only. †† Recorded as patient married or not married to father. §§ Percentage based on a total of 542,479 abortions reported among the areas that met reporting standards for marital status; reporting standards for marital status were applied to abortions for residents of Illinois only. ¶¶ Number of abortions obtained by marital status per 1,000 live births to women of the same marital status. For the total abortion ratio only, abortions for women of unknown marital status were distributed according to the distribution of abortions among women of known marital status.
| State/Area | No. of previous live births | Total abortions reported by known number of previous live births | ||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ≥4 | ||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (% of all reported abortions) | |
| Alabama | 2,030 (33.8) | 1,660 (27.6) | 1,369 (22.8) | 602 (10.0) | 348 (5.8) | |
| Alaska | 575 (45.3) | 233 (18.4) | 258 (20.3) | 103 (8.1) | 100 (7.9) | |
| Arizona | 5,707 (44.0) | 2,784 (21.5) | 2,426 (18.7) | 1,195 (9.2) | 846 (6.5) | |
| Arkansas | 1,042 (35.2) | 771 (26.0) | 650 (21.9) | 295 (10.0) | 205 (6.9) | |
| Colorado | 5,167 (57.7) | 1,644 (18.3) | 1,268 (14.1) | 573 (6.4) | 310 (3.5) | |
| Connecticut | 3,731 (40.6) | 2,319 (25.2) | 1,833 (20.0) | 839 (9.1) | 465 (5.1) | |
| Delaware | 849 (42.1) | 501 (24.8) | 390 (19.3) | 159 (7.9) | 118 (5.9) | |
| Florida | 27,510 (38.3) | 18,129 (25.2) | 14,878 (20.7) | 6,660 (9.3) | 4,737 (6.6) | |
| Georgia | 14,313 (38.8) | 9,116 (24.7) | 7,405 (20.1) | 3,646 (9.9) | 2,425 (6.6) | |
| Hawaii | 1,096 (54.8) | 338 (16.9) | 313 (15.7) | 160 (8.0) | 92 (4.6) | |
| Idaho | 694 (46.3) | 316 (21.1) | 277 (18.5) | 130 (8.7) | 83 (5.5) | |
| Indiana | 3,045 (39.9) | 1,831 (24.0) | 1,558 (20.4) | 780 (10.2) | 423 (5.5) | |
| Iowa | 1,430 (40.4) | 781 (22.1) | 705 (19.9) | 356 (10.1) | 268 (7.6) | |
| Kansas | 2,795 (40.5) | 1,686 (24.5) | 1,327 (19.2) | 681 (9.9) | 405 (5.9) | |
| Kentucky | 1,300 (35.5) | 934 (25.5) | 871 (23.8) | 338 (9.2) | 221 (6.0) | |
| Louisiana | 2,627 (32.3) | 2,231 (27.5) | 1,807 (22.2) | 894 (11.0) | 564 (6.9) | |
| Maine | 1,002 (49.7) | 431 (21.4) | 362 (18.0) | 148 (7.3) | 73 (3.6) | |
| Massachusetts | 7,765 (46.2) | 3,910 (23.3) | 3,147 (18.7) | 1,324 (7.9) | 645 (3.8) | |
| Michigan | 9,472 (34.7) | 7,075 (25.9) | 6,209 (22.7) | 2,827 (10.3) | 1,748 (6.4) | |
| Minnesota | 3,954 (40.1) | 2,265 (23.0) | 1,944 (19.7) | 964 (9.8) | 730 (7.4) | |
| Mississippi | 996 (31.2) | 924 (28.9) | 714 (22.4) | 342 (10.7) | 218 (6.8) | |
| Missouri | 561 (38.1) | 353 (24.0) | 301 (20.5) | 146 (9.9) | 110 (7.5) | |
| Montana | 746 (47.6) | 357 (22.8) | 260 (16.6) | 129 (8.2) | 76 (4.8) | |
| Nebraska | 819 (39.6) | 445 (21.5) | 429 (20.8) | 216 (10.4) | 158 (7.6) | |
| Nevada | 3,606 (42.9) | 1,954 (23.2) | 1,496 (17.8) | 790 (9.4) | 567 (6.7) | |
| New Jersey** | 8,148 (36.9) | 6,140 (27.8) | 4,303 (19.5) | 2,105 (9.5) | 1,411 (6.4) | |
| New Mexico | 1,502 (42.6) | 801 (22.7) | 621 (17.6) | 357 (10.1) | 248 (7.0) | |
| New York City | 20,793 (45.8) | 11,596 (25.5) | 8,380 (18.4) | 2,987 (6.6) | 1,680 (3.7) | |
| North Carolina | 9,498 (37.4) | 6,067 (23.9) | 5,016 (19.8) | 2,660 (10.5) | 2,154 (8.5) | |
| North Dakota | 452 (40.3) | 243 (21.7) | 223 (19.9) | 118 (10.5) | 85 (7.6) | |
| Ohio | 7,074 (36.1) | 4,963 (25.3) | 4,176 (21.3) | 2,049 (10.4) | 1,360 (6.9) | |
| Oklahoma | 1,890 (37.9) | 1,208 (24.2) | 1,055 (21.1) | 507 (10.2) | 332 (6.7) | |
| Oregon | 4,366 (50.6) | 1,759 (20.4) | 1,501 (17.4) | 590 (6.8) | 407 (4.7) | |
| Pennsylvania | 11,760 (37.9) | 7,926 (25.6) | 6,367 (20.5) | 3,046 (9.8) | 1,919 (6.2) | |
| Rhode Island | 963 (45.9) | 506 (24.1) | 393 (18.7) | 144 (6.9) | 92 (4.4) | |
| South Carolina | 2,129 (41.7) | 1,294 (25.4) | 1,027 (20.1) | 409 (8.0) | 242 (4.7) | |
| South Dakota | 165 (39.9) | 72 (17.4) | 94 (22.7) | — | — | |
| Tennessee | 3,484 (36.3) | 2,498 (26.0) | 1,974 (20.6) | 940 (9.8) | 695 (7.2) | |
| Texas | 22,862 (39.9) | 13,628 (23.8) | 11,985 (20.9) | 5,483 (9.6) | 3,317 (5.8) | |
| Utah | 1,496 (51.2) | 555 (19.0) | 470 (16.1) | 230 (7.9) | 171 (5.9) | |
| Vermont | 597 (50.0) | 235 (19.7) | 231 (19.3) | 88 (7.4) | 43 (3.6) | |
| Virginia | 5,531 (35.5) | 4,095 (26.2) | 3,326 (21.3) | 1,646 (10.6) | 1,003 (6.4) | |
| Washington | 8,035 (46.7) | 3,845 (22.3) | 3,163 (18.4) | 1,370 (8.0) | 805 (4.7) | |
| West Virginia | 421 (35.6) | 347 (29.4) | 255 (21.6) | 97 (8.2) | 62 (5.2) | |
| Wyoming | 17 (54.8) | 5 (16.1) | 7 (22.6) | — | — | |
* Data from 45 reporting areas; excludes seven reporting areas (California, District of Columbia, Illinois, Maryland, New Hampshire, New York State, and Wisconsin) that did not report, did not report by number of previous live births, or did not meet reporting standards. † Percentages for the individual component categories might not add to 100% because of rounding. § Percentage is calculated as the number of abortions reported by known number of previous live births divided by the sum of abortions reported by known and unknown number of previous live births. Values ≥99.95% are rounded to 100.0%. ¶ Recorded as the number of previous pregnancies carried to term. ** Reporting to the central health agency is not required. Data are requested from hospitals and licensed ambulatory care facilities only. †† Recorded as the number of living children. §§ Cells with a value in the range of 1–4 or cells that would allow for calculation of these small values have been suppressed. ¶¶ Percentage based on a total of 543,515 abortions reported among the areas that met reporting standards for the number of previous live births.
| State/Area | No. of previous induced abortions | Total abortions reported by known number of previous induced abortions | |||
|---|---|---|---|---|---|
| 0 | 1 | 2 | ≥3 | ||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (% of all reported abortions) | |
| Alabama | 4,008 (66.7) | 1,332 (22.2) | 443 (7.4) | 226 (3.8) | |
| Alaska | 819 (64.5) | 271 (21.4) | 109 (8.6) | 70 (5.5) | |
| Arizona | 8,472 (65.6) | 3,047 (23.6) | 955 (7.4) | 445 (3.4) | |
| Arkansas | 1,915 (64.6) | 587 (19.8) | 233 (7.9) | 228 (7.7) | |
| Colorado | 6,287 (69.9) | 1,852 (20.6) | 601 (6.7) | 251 (2.8) | |
| Connecticut | 4,883 (53.2) | 2,163 (23.5) | 1,123 (12.2) | 1,018 (11.1) | |
| Delaware | 1,244 (61.5) | 472 (23.3) | 197 (9.7) | 109 (5.4) | |
| Florida | 41,693 (58.0) | 17,171 (23.9) | 7,405 (10.3) | 5,645 (7.8) | |
| Georgia | 22,534 (61.1) | 8,778 (23.8) | 3,605 (9.8) | 1,990 (5.4) | |
| Hawaii | 1,244 (62.2) | 452 (22.6) | 178 (8.9) | 125 (6.3) | |
| Idaho | 1,228 (81.8) | 209 (13.9) | 44 (2.9) | 21 (1.4) | |
| Indiana | 5,160 (67.6) | 1,712 (22.4) | 539 (7.1) | 226 (3.0) | |
| Iowa | 2,675 (75.6) | 565 (16.0) | 186 (5.3) | 114 (3.2) | |
| Kansas | 4,647 (67.4) | 1,467 (21.3) | 499 (7.2) | 281 (4.1) | |
| Kentucky | 2,324 (63.4) | 866 (23.6) | 293 (8.0) | 181 (4.9) | |
| Louisiana | 5,098 (62.7) | 2,006 (24.7) | 732 (9.0) | 291 (3.6) | |
| Maine | 1,314 (65.1) | 455 (22.6) | 153 (7.6) | 95 (4.7) | |
| Massachusetts | 9,507 (52.6) | 4,868 (26.9) | 2,240 (12.4) | 1,466 (8.1) | |
| Michigan | 14,134 (51.7) | 6,797 (24.9) | 3,684 (13.5) | 2,712 (9.9) | |
| Minnesota | 6,030 (61.1) | 2,197 (22.3) | 937 (9.5) | 708 (7.2) | |
| Mississippi | 2,159 (67.6) | 685 (21.4) | 249 (7.8) | 101 (3.2) | |
| Missouri | 882 (60.0) | 367 (24.9) | 141 (9.6) | 81 (5.5) | |
| Montana | 643 (41.0) | 622 (39.7) | 199 (12.7) | 104 (6.6) | |
| Nebraska | 1,429 (69.1) | 430 (20.8) | 142 (6.9) | 67 (3.2) | |
| Nevada | 5,281 (62.8) | 1,874 (22.3) | 744 (8.8) | 512 (6.1) | |
| New Jersey | 13,486 (60.9) | 4,195 (18.9) | 2,251 (10.2) | 2,223 (10.0) | |
| New York City | 16,911 (37.9) | 11,024 (24.7) | 8,392 (18.8) | 8,244 (18.5) | |
| North Carolina | 15,400 (61.4) | 5,874 (23.4) | 2,474 (9.9) | 1,329 (5.3) | |
| North Dakota | 778 (70.7) | 200 (18.2) | 92 (8.4) | 31 (2.8) | |
| Ohio | 11,689 (59.7) | 4,727 (24.2) | 1,915 (9.8) | 1,242 (6.3) | |
| Oklahoma | 3,558 (71.3) | 975 (19.5) | 304 (6.1) | 155 (3.1) | |
| Oregon | 5,182 (60.1) | 2,064 (23.9) | 809 (9.4) | 574 (6.7) | |
| Pennsylvania | 16,327 (52.6) | 7,699 (24.8) | 3,829 (12.3) | 3,163 (10.2) | |
| Rhode Island | 1,286 (61.4) | 480 (22.9) | 218 (10.4) | 110 (5.3) | |
| South Carolina | 3,320 (65.1) | 1,160 (22.7) | 414 (8.1) | 207 (4.1) | |
| South Dakota | 285 (68.8) | 88 (21.3) | —** | —** | |
| Tennessee | 6,230 (64.7) | 2,326 (24.2) | 724 (7.5) | 348 (3.6) | |
| Texas | 35,902 (62.7) | 14,039 (24.5) | 4,874 (8.5) | 2,460 (4.3) | |
| Utah | 2,251 (77.0) | 506 (17.3) | 114 (3.9) | 51 (1.7) | |
| Vermont | 746 (62.5) | 266 (22.3) | 111 (9.3) | 70 (5.9) | |
| Virginia | 8,520 (54.6) | 4,322 (27.7) | 1,670 (10.7) | 1,089 (7.0) | |
| Washington | 9,911 (57.6) | 4,219 (24.5) | 1,713 (10.0) | 1,363 (7.9) | |
| West Virginia | 728 (61.5) | 298 (25.2) | 106 (9.0) | 51 (4.3) | |
| Wyoming | 20 (64.5) | 9 (29.0) | —** | —** | |
* Data from 44 reporting areas; excludes eight reporting areas (California, District of Columbia, Illinois, Maryland, New Hampshire, New Mexico, New York State, and Wisconsin) that did not report, did not report by number of previous induced abortions, or did not meet reporting standards. † Percentages for the individual component categories might not add to 100% because of rounding. § Percentage is calculated as the number of abortions reported by known number of previous induced abortions divided by the sum of abortions reported by known and unknown number of previous induced abortions. Values ≥99.95% are rounded to 100.0%. ¶ Reporting to the central health agency is not required. Data are requested from hospitals and licensed ambulatory care facilities only. ** Cells with a value in the range of 1–4 or cells that would allow for calculation of these small values have been suppressed. †† Percentage based on a total of 539,573 abortions reported among the areas that met reporting standards for the number of previous induced abortions.
| State/Area | Weeks of gestation | Total abortions reported by known gestational age | ||||||
|---|---|---|---|---|---|---|---|---|
| ≤6 | 7–9 | 10–13 | 14–15 | 16–17 | 18–20 | ≥21 | ||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (% of all reported abortions) | |
| Alabama** | 1,280 (21.3) | 2,807 (46.8) | 1,257 (20.9) | 317 (5.3) | 163 (2.7) | 133 (2.2) | 46 (0.8) | |
| Alaska | 292 (23.0) | 639 (50.4) | 271 (21.4) | 64 (5.0) | — | — | 0 (—) | |
| Arizona | 3,863 (29.5) | 5,985 (45.7) | 2,079 (15.9) | 496 (3.8) | 261 (2.0) | 245 (1.9) | 168 (1.3) | |
| Arkansas** | 479 (16.2) | 1,265 (42.7) | 862 (29.1) | 150 (5.1) | 82 (2.8) | 97 (3.3) | 28 (0.9) | |
| Colorado | 3,639 (40.4) | 3,666 (40.7) | 1,062 (11.8) | 198 (2.2) | 150 (1.7) | 110 (1.2) | 173 (1.9) | |
| Connecticut | 4,046 (45.7) | 3,155 (35.7) | 947 (10.7) | 263 (3.0) | 175 (2.0) | 164 (1.9) | 95 (1.1) | |
| Delaware | 536 (26.3) | 1,071 (52.5) | 328 (16.1) | 73 (3.6) | 16 (0.8) | 6 (0.3) | 9 (0.4) | |
| Florida | 52,850 (73.5) | 11,641 (16.2) | 4,843 (6.7) | 973 (1.4) | 691 (1.0) | 699 (1.0) | 217 (0.3) | |
| Georgia | 16,086 (43.6) | 13,864 (37.6) | 4,396 (11.9) | 927 (2.5) | 653 (1.8) | 752 (2.0) | 229 (0.6) | |
| Hawaii | 678 (33.9) | 861 (43.0) | 268 (13.4) | 80 (4.0) | 43 (2.1) | 49 (2.4) | 22 (1.1) | |
| Idaho | 493 (32.9) | 707 (47.1) | 257 (17.1) | 37 (2.5) | — | — | — | |
| Indiana | 1,924 (25.2) | 4,055 (53.1) | 1,618 (21.2) | 9 (0.1) | 8 (0.1) | 17 (0.2) | 6 (0.1) | |
| Iowa | 1,652 (46.3) | 1,305 (36.6) | 412 (11.6) | 68 (1.9) | 58 (1.6) | 54 (1.5) | 17 (0.5) | |
| Kansas | 2,761 (40.0) | 2,722 (39.5) | 921 (13.4) | 195 (2.8) | 121 (1.8) | 137 (2.0) | 37 (0.5) | |
| Kentucky | 1,302 (35.5) | 1,493 (40.7) | 550 (15.0) | 116 (3.2) | 65 (1.8) | 109 (3.0) | 29 (0.8) | |
| Louisiana | 2,815 (34.6) | 3,567 (43.8) | 1,274 (15.7) | 273 (3.4) | 173 (2.1) | 38 (0.5) | 0 (—) | |
| Maine | 595 (29.5) | 996 (49.3) | 317 (15.7) | 48 (2.4) | 33 (1.6) | 31 (1.5) | 0 (—) | |
| Michigan | 9,016 (33.0) | 11,496 (42.1) | 4,055 (14.9) | 1,110 (4.1) | 667 (2.4) | 584 (2.1) | 353 (1.3) | |
| Minnesota | 3,597 (36.7) | 3,845 (39.2) | 1,381 (14.1) | 379 (3.9) | 194 (2.0) | 216 (2.2) | 187 (1.9) | |
| Mississippi | 1,117 (35.0) | 1,421 (44.5) | 468 (14.7) | 171 (5.4) | 16 (0.5) | — | — | |
| Missouri | 86 (5.8) | 496 (33.7) | 505 (34.3) | 130 (8.8) | 87 (5.9) | 112 (7.6) | 55 (3.7) | |
| Montana | 599 (38.2) | 628 (40.1) | 211 (13.5) | 51 (3.3) | 34 (2.2) | 34 (2.2) | 11 (0.7) | |
| Nebraska | 976 (47.2) | 683 (33.0) | 284 (13.7) | 62 (3.0) | 46 (2.2) | 16 (0.8) | 0 (—) | |
| Nevada | 3,214 (38.6) | 3,510 (42.1) | 1,078 (12.9) | 250 (3.0) | 142 (1.7) | 89 (1.1) | 52 (0.6) | |
| New Jersey | 8,513 (39.3) | 7,499 (34.6) | 2,923 (13.5) | 961 (4.4) | 638 (2.9) | 613 (2.8) | 514 (2.4) | |
| New Mexico | 1,487 (42.7) | 957 (27.5) | 381 (10.9) | 80 (2.3) | 73 (2.1) | 101 (2.9) | 406 (11.6) | |
| New York City | 22,364 (44.9) | 17,579 (35.3) | 5,579 (11.2) | 1,335 (2.7) | 897 (1.8) | 934 (1.9) | 1,096 (2.2) | |
| North Carolina | 9,598 (33.9) | 12,098 (42.8) | 4,432 (15.7) | 982 (3.5) | 672 (2.4) | 484 (1.7) | 15 (0.1) | |
| North Dakota | 435 (38.8) | 447 (39.9) | 180 (16.1) | 42 (3.7) | 17 (1.5) | 0 (—) | 0 (—) | |
| Ohio | 5,523 (27.5) | 9,070 (45.1) | 3,558 (17.7) | 848 (4.2) | 531 (2.6) | 477 (2.4) | 95 (0.5) | |
| Oklahoma | 2,177 (43.6) | 1,835 (36.8) | 710 (14.2) | 125 (2.5) | 64 (1.3) | 64 (1.3) | 16 (0.3) | |
| Oregon | 4,064 (47.2) | 2,924 (33.9) | 949 (11.0) | 241 (2.8) | 129 (1.5) | 149 (1.7) | 160 (1.9) | |
| Rhode Island | 929 (44.4) | 705 (33.7) | 270 (12.9) | 90 (4.3) | 52 (2.5) | 32 (1.5) | 13 (0.6) | |
| South Carolina** | 1,063 (20.8) | 1,970 (38.6) | 1,740 (34.1) | 298 (5.8) | 8 (0.2) | 13 (0.3) | 9 (0.2) | |
| South Dakota | 64 (15.6) | 224 (54.8) | — | — | 0 (—) | — | 7 (1.7) | |
| Tennessee | 1,836 (18.9) | 4,939 (50.9) | 2,188 (22.5) | 436 (4.5) | 176 (1.8) | 119 (1.2) | 9 (0.1) | |
| Texas** | 22,356 (39.0) | 22,721 (39.7) | 8,232 (14.4) | 1,870 (3.3) | 957 (1.7) | 838 (1.5) | 301 (0.5) | |
| Utah | 1,018 (34.8) | 1,185 (40.6) | 478 (16.4) | 92 (3.1) | 51 (1.7) | 67 (2.3) | 31 (1.1) | |
| Vermont | 550 (46.0) | 423 (35.4) | 129 (10.8) | 32 (2.7) | 21 (1.8) | 22 (1.8) | 18 (1.5) | |
| Virginia | 7,917 (50.8) | 5,215 (33.5) | 1,938 (12.4) | 121 (0.8) | 131 (0.8) | 170 (1.1) | 90 (0.6) | |
| Washington | 7,046 (41.0) | 6,768 (39.4) | 2,061 (12.0) | 420 (2.4) | 265 (1.5) | 273 (1.6) | 363 (2.1) | |
| West Virginia | 325 (27.5) | 536 (45.3) | 235 (19.9) | 58 (4.9) | 18 (1.5) | — | — | |
| Wyoming | 18 (58.1) | 12 (38.7) | — | — | 0 (—) | 0 (—) | 0 (—) | |
* Gestational age based on clinician’s estimate (Alaska, Arizona, Colorado, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Indiana, Iowa, Kansas, Kentucky, Louisiana, Maine, Michigan, Minnesota, Mississippi, Missouri, Montana, Nebraska, Nevada, New Jersey, New Mexico, New York City, North Carolina, North Dakota, Ohio, Oregon, Rhode Island, South Dakota, Tennessee, Vermont, Washington, West Virginia, and Wyoming); gestational age calculated from the last normal menstrual period (Oklahoma and Utah); clinician’s estimate of gestation based on estimated date of conception (Virginia); probable postfertilization age (Alabama, Arkansas, South Carolina, and Texas). † Data from 43 reporting areas; excludes nine reporting areas (California, District of Columbia, Illinois, Maryland, Massachusetts, New Hampshire, New York State, Pennsylvania, and Wisconsin) that did not report, did not report by gestational age, or did not meet reporting standards. § Percentages for the individual component categories might not add to 100% because of rounding. ¶ Percentage is calculated as the number of abortions reported by known gestational age divided by the sum of abortions reported by known and unknown gestational age. Values ≥99.95% are rounded to 100.0%. ** Two weeks were added to the probable postfertilization age to provide a corresponding measure to gestational age based on the clinician’s estimate. †† Cells with a value in the range of 1–4 or cells that would allow for calculation of these small values have been suppressed. §§ Reporting to the central health agency is not required. Data are requested from hospitals and licensed ambulatory care facilities only. ¶¶ Percentage based on a total of 493,904 abortions reported among the areas that met reporting standards for gestational age.
| Weeks of gestation | Year | % Change | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2010 to 2014 | 2015 to 2019 | 2018 to 2019 | 2010 to 2019 | |
| ≤6 | 34.7 | 34.3 | 35.1 | 34.7 | 33.8 | 34.3 | 34.2 | 35.1 | 36.2 | 37.5 | −2.6 | 9.3 | 3.6 | 8.1 |
| 7–9 | 40.1 | 40.1 | 39.4 | 39.9 | 40.0 | 40.0 | 40.3 | 40.4 | 40.0 | 39.9 | −0.2 | −0.3 | −0.3 | −0.5 |
| 10–13 | 17.0 | 17.1 | 16.9 | 17.0 | 17.2 | 16.7 | 16.4 | 15.7 | 15.2 | 14.6 | 1.2 | −12.6 | −3.9 | −14.1 |
| 14–15 | 3.3 | 3.4 | 3.5 | 3.4 | 3.5 | 3.5 | 3.6 | 3.4 | 3.4 | 3.2 | 6.1 | −8.6 | −5.9 | −3.0 |
| 16–17 | 1.8 | 1.9 | 1.9 | 1.9 | 2.2 | 2.1 | 2.1 | 2.2 | 2.1 | 1.9 | 22.2 | −9.5 | −9.5 | 5.6 |
| 18–20 | 1.8 | 1.9 | 1.9 | 1.8 | 1.9 | 2.0 | 2.0 | 2.0 | 1.9 | 1.8 | 5.6 | −10.0 | −5.3 | 0.0 |
| ≥21 | 1.2 | 1.4 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.2 | 1.1 | 8.3 | −15.4 | −8.3 | −8.3 |
Abbreviation: NA = not applicable. * Data from 34 reporting areas; excludes 18 areas (California, Connecticut, Delaware, District of Columbia, Florida, Illinois, Maine, Maryland, Massachusetts, Mississippi, Nebraska, New Hampshire, New York State, Pennsylvania, Rhode Island, Vermont, Wisconsin, and Wyoming) that did not report, did not report by weeks of gestation, or did not meet reporting standards for ≥1 year. † Percentages for the individual component categories might not add to 100% because of rounding. § By year, the total number of abortions represents 74.6%–98.2% of all abortions reported to CDC among the areas that met reporting standards for gestational age during 2010–2019.
| State/Area | Surgical | Medical | Intrauterine instillation | Hysterectomy/ Hysterotomy | Total abortions reported by known method type | ||||
|---|---|---|---|---|---|---|---|---|---|
| Surgical, ≤13 weeks’ gestation | Surgical, >13 weeks’ gestation | Surgical, unknown gestational age | Medical, ≤9 weeks’ gestation | Medical, >9 weeks’ gestation | Medical, unknown gestational age | ||||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (% of all reported abortions)** | |
| Alabama | 3,257 (54.2) | 653 (10.9) | — | 2,030 (33.8) | 58 (1.0) | — | 0 (—) | 0 (—) | |
| Alaska | 895 (70.5) | 65 (5.1) | 0 (—) | 305 (24.0) | — | — | — | 0 (—) | |
| Arizona | 6,768 (51.7) | 992 (7.6) | 0 (—) | 5,031 (38.4) | 159 (1.2) | 0 (—) | 137 (1.0) | 0 (—) | |
| Arkansas | 1,369 (46.2) | 356 (12.0) | 0 (—) | 829 (28.0) | 408 (13.8) | 0 (—) | 0 (—) | 0 (—) | |
| Colorado | 2,989 (35.9) | 400 (4.8) | — | 4,819 (57.8) | 120 (1.4) | 0 (—) | — | 0 (—) | |
| Connecticut | 3,747 (41.0) | 687 (7.5) | 136 (1.5) | 4,367 (47.8) | 25 (0.3) | 173 (1.9) | 0 (—) | 0 (—) | |
| Delaware | 722 (36.0) | 101 (5.0) | — | 1,136 (56.6) | 46 (2.3) | — | 0 (—) | 0 (—) | |
| District of Columbia | 2,170 (47.7) | 382 (8.4) | 0 (—) | NA | NA | 2,000 (43.9) | 0 (—) | 0 (—) | |
| Florida | 32,315 (47.1) | 2,505 (3.7) | 0 (—) | 33,428 (48.7) | 352 (0.5) | 0 (—) | 0 (—) | 8 (0.0) | |
| Georgia | 15,801 (42.8) | 2,555 (6.9) | 0 (—) | 18,240 (49.4) | 309 (0.8) | 0 (—) | 0 (—) | 0 (—) | |
| Hawaii | 1,030 (51.4) | 194 (9.7) | — | 776 (38.8) | — | 0 (—) | 0 (—) | 0 (—) | |
| Idaho | 826 (54.7) | 42 (2.8) | 10 (0.7) | 621 (41.1) | 8 (0.5) | — | — | 0 (—) | |
| Indiana | 4,241 (55.5) | 36 (0.5) | 0 (—) | 3,297 (43.2) | 62 (0.8) | 0 (—) | 0 (—) | 0 (—) | |
| Iowa | 948 (26.8) | 190 (5.4) | 0 (—) | 2,364 (66.7) | 40 (1.1) | 0 (—) | 0 (—) | 0 (—) | |
| Kansas | 1,959 (28.4) | 486 (7.1) | 0 (—) | 4,364 (63.3) | 82 (1.2) | 0 (—) | 0 (—) | 0 (—) | |
| Kentucky | 1,512 (41.3) | 306 (8.4) | 0 (—) | 1,828 (49.9) | 18 (0.5) | 0 (—) | 0 (—) | 0 (—) | |
| Maine | 888 (44.0) | 106 (5.3) | — | 960 (47.6) | 63 (3.1) | — | 0 (—) | 0 (—) | |
| Massachusetts*** | NA | NA | 10,377 (56.4) | NA | NA | 7,958 (43.2) | 67 (0.4) | 0 (—) | |
| Michigan | 12,984 (47.6) | 2,649 (9.7) | 42 (0.2) | 11,213 (41.1) | 386 (1.4) | 10 (0.0) | 0 (—) | 0 (—) | |
| Minnesota | 5,187 (52.2) | 958 (9.6) | 54 (0.5) | 3,589 (36.1) | 61 (0.6) | 87 (0.9) | — | — | |
| Mississippi | 725 (22.7) | 186 (5.8) | 0 (—) | 2,228 (69.8) | 55 (1.7) | 0 (—) | 0 (—) | 0 (—) | |
| Missouri | 1,076 (73.5) | 367 (25.1) | 0 (—) | 5 (0.3) | 10 (0.7) | 0 (—) | — | — | |
| Montana | 524 (33.4) | 128 (8.2) | 0 (—) | 900 (57.4) | 16 (1.0) | 0 (—) | 0 (—) | 0 (—) | |
| Nebraska | 686 (33.2) | 122 (5.9) | 0 (—) | 1,245 (60.2) | 13 (0.6) | — | 0 (—) | — | |
| Nevada | 4,599 (55.0) | 527 (6.3) | 38 (0.5) | 3,113 (37.2) | 51 (0.6) | 37 (0.4) | — | — | |
| New Jersey | 12,938 (58.3) | 2,692 (12.1) | 481 (2.2) | 5,896 (26.6) | 134 (0.6) | 35 (0.2) | 0 (—) | 0 (—) | |
| New Mexico | 1,394 (39.9) | 301 (8.6) | 58 (1.7) | 1,332 (38.2) | 338 (9.7) | 65 (1.9) | — | — | |
| New York | 40,495 (52.9) | 6,130 (8.0) | 1,399 (1.8) | 23,809 (31.1) | 2,125 (2.8) | 2,555 (3.3) | 24 (0.0) | 32 (0.0) | |
| New York City | 29,516 (59.4) | 4,113 (8.3) | 0 (—) | 15,505 (31.2) | 525 (1.1) | 0 (—) | 9 (0.0) | 32 (0.1) | |
| New York State | 10,979 (40.9) | 2,017 (7.5) | 1,399 (5.2) | 8,304 (30.9) | 1,600 (6.0) | 2,555 (9.5) | 15 (0.1) | 0 (—) | |
| North Carolina | 12,295 (45.9) | 1,992 (7.4) | 32 (0.1) | 12,209 (45.6) | 190 (0.7) | 36 (0.1) | 0 (—) | 12 (0.0) | |
| North Dakota | 698 (62.3) | 59 (5.3) | — | 361 (32.2) | — | 0 (—) | 0 (—) | 0 (—) | |
| Ohio | 10,350 (51.5) | 1,937 (9.6) | — | 7,716 (38.4) | 91 (0.5) | 0 (—) | 0 (—) | — | |
| Oklahoma | 2,152 (43.8) | 263 (5.4) | — | 2,460 (50.1) | 33 (0.7) | — | — | 0 (—) | |
| Oregon | 3,494 (40.2) | 646 (7.4) | 21 (0.2) | 4,337 (49.9) | 133 (1.5) | 51 (0.6) | — | — | |
| Pennsylvania | NA | NA | 17,159 (55.3) | NA | NA | 13,845 (44.6) | — | — | |
| Rhode Island | 1,010 (48.3) | 179 (8.6) | 7 (0.3) | 884 (42.2) | 12 (0.6) | — | — | 0 (—) | |
| South Carolina | 1,676 (32.9) | 319 (6.3) | — | 2,334 (45.8) | 766 (15.0) | 0 (—) | 5 (0.1) | — | |
| South Dakota | 272 (65.7) | 0 (—) | — | 124 (30.0) | 13 (3.1) | — | 0 (—) | 0 (—) | |
| Tennessee | 4,034 (41.5) | 716 (7.4) | 8 (0.1) | 4,765 (49.0) | 183 (1.9) | 8 (0.1) | 0 (—) | 5 (0.1) | |
| Texas | 30,824 (53.8) | 3,906 (6.8) | 0 (—) | 22,234 (38.8) | 305 (0.5) | 0 (—) | — | — | |
| Utah | 1,455 (49.8) | 229 (7.8) | 0 (—) | 1,223 (41.9) | 11 (0.4) | 0 (—) | — | — | |
| Vermont | 394 (33.1) | 87 (7.3) | — | 683 (57.4) | 25 (2.1) | 0 (—) | — | 0 (—) | |
| Virginia | 9,252 (59.3) | 500 (3.2) | 15 (0.1) | 5,744 (36.8) | 74 (0.5) | — | — | 0 (—) | |
| Washington | 7,491 (43.4) | 1,317 (7.6) | 30 (0.2) | 8,320 (48.2) | 56 (0.3) | 36 (0.2) | 0 (—) | 0 (—) | |
| West Virginia | 617 (52.2) | 77 (6.5) | 0 (—) | 454 (38.4) | 35 (3.0) | 0 (—) | 0 (—) | 0 (—) | |
| Wisconsin*** | NA | NA | 4,207 (66.0) | NA | NA | 2,165 (34.0) | 0 (—) | 0 (—) | |
| Wyoming | 0 (—) | 0 (—) | — | 30 (96.8) | — | 0 (—) | 0 (—) | 0 (—) | |
Abbreviation: NA = not available. * Data from 47 reporting areas; excludes five reporting areas (California, Illinois, Louisiana, Maryland, and New Hampshire) that did not report, did not report by method type, or did not meet reporting standards. Areas reporting by method type with unknown gestational age or gestational age reported was not compatible with categorizations presented in this table are included. † Includes uterine aspiration (might also be called dilation and curettage, aspiration curettage, suction curettage, manual vacuum aspiration, menstrual extraction, sharp curettage) and dilation and evacuation procedures. § Intrauterine instillations reported at ≤12 weeks’ gestation were considered as unknown for method type. ¶ Percentages for the individual component categories might not add to 100% because of rounding. ** Percentage is calculated as the number of abortions reported by known method type divided by the sum of abortions reported by known and unknown method type. Values ≥99.95% are rounded to 100.0%. †† Two weeks were added to the probable postfertilization age to provide a corresponding measure to gestational age based on the clinician’s estimate. §§ Cells with a value in the range of 1–4 or cells that would allow for calculation of these small values have been suppressed. ¶¶ Numbers for medical abortions at ≤9 weeks versus >9 weeks are not presented because gestational age reported was not compatible with these categorizations. *** Numbers for surgical abortions at ≤13 weeks versus >13 weeks and for medical abortions at ≤9 weeks versus >9 weeks are not presented because gestational age data were not provided by method type. ††† Reporting to the central health agency is not required. Data are requested from hospitals and licensed ambulatory care facilities only. §§§ Numbers for surgical abortions ≤13 weeks and >13 weeks and medical abortions ≤9 weeks versus >9 weeks are not presented as gestational age reported was not compatible with these categorizations. ¶¶¶ Includes residents only. Wisconsin reports as surgical, unspecified and does not differentiate surgical abortions from hysterectomy/hysterotomy. All abortions were reported as surgical or chemically induced. For this report, all surgical abortions were classified as surgical and all chemical abortions as medical. **** For the total only, surgical abortions reported without a gestational age were distributed among the surgical abortion categories according to the distribution of surgical abortions at known gestational age. †††† For the total only, medical abortions reported without a gestational age were distributed among the medical abortion categories according to the distribution of medical abortions at known gestational age. §§§§ Percentage based on a total of 575,098 abortions reported among the areas that met reporting standards for method type.
| Method type | Weeks of gestation | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| ≤6 | 7–9 | 10–13 | 14–15 | 16–17 | 18–20 | ≥21 | ||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |
| ≤13 weeks’ gestation | 84,850 (41.3) | 90,714 (52.2) | 59,346 (93.2) | NA | NA | NA | NA | |
| >13 weeks’ gestation | NA | NA | NA | 13,965 (99.2) | 8,199 (98.3) | 7,686 (96.9) | 4,094 (87.0) | |
| ≤9 weeks’ gestation | 120,333 (58.6) | 82,966 (47.8) | NA | NA | NA | NA | NA | |
| >9 weeks’ gestation | NA | NA | 4,339 (6.8) | 109 (0.8) | 94 (1.1) | 185 (2.3) | 545 (11.6) | |
| —** | —** | 1 (0.0) | 2 (0.0) | 48 (0.6) | 58 (0.7) | 60 (1.3) | ||
| 19 (0.0) | 28 (0.0) | 5 (0.0) | 4 (0.0) | 3 (0.0) | 6 (0.1) | 7 (0.1) | ||
Abbreviation : NA = not applicable. * Data from 42 reporting areas; excludes 10 reporting areas (California, District of Columbia, Illinois, Louisiana, Maryland, Massachusetts, New Hampshire, New York State, Pennsylvania, and Wisconsin) that did not report, did not report by weeks of gestation, did not meet reporting standards, or did not have medical abortion as a specific category on their reporting form. † For each gestational age category, percentages of all method types might not add to 100% because of rounding. § Includes uterine aspiration (might also be called dilation and curettage, aspiration curettage, suction curettage, manual vacuum aspiration, menstrual extraction, sharp curettage) and dilation and evacuation procedures. ¶ The administration of medication or medications to induce an abortion; at ≤9 weeks’ gestation, typically involves the use of mifepristone and misoprostol, and at >9 weeks’ gestation, typically involves the use of vaginal prostaglandins. ** Intrauterine instillations reported at ≤12 weeks’ gestation have not been included with known values.
| Characteristic | Weeks of gestation | Total | ||||||
|---|---|---|---|---|---|---|---|---|
| ≤6 | 7–9 | 10–13 | 14–15 | 16–17 | 18–20 | ≥21 | ||
| No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | No. (%) | |
| <15 | 306 (27.2) | 384 (34.1) | 214 (19.0) | 73 (6.5) | 53 (4.7) | 47 (4.2) | 50 (4.4) | |
| 15–19 | 14,886 (35.7) | 15,785 (37.9) | 7,007 (16.8) | 1,536 (3.7) | 948 (2.3) | 962 (2.3) | 561 (1.3) | |
| 20–24 | 56,003 (41.3) | 50,599 (37.3) | 19,052 (14.1) | 4,179 (3.1) | 2,398 (1.8) | 2,142 (1.6) | 1,226 (0.9) | |
| 25–29 | 61,791 (43.3) | 52,298 (36.7) | 18,882 (13.2) | 3,925 (2.8) | 2,294 (1.6) | 2,189 (1.5) | 1,242 (0.9) | |
| 30–34 | 43,257 (45.1) | 34,165 (35.6) | 11,747 (12.3) | 2,654 (2.8) | 1,523 (1.6) | 1,473 (1.5) | 1,022 (1.1) | |
| 35–39 | 24,816 (46.1) | 18,652 (34.7) | 6,425 (11.9) | 1,501 (2.8) | 960 (1.8) | 880 (1.6) | 588 (1.1) | |
| ≥40 | 9,053 (49.4) | 5,919 (32.3) | 1,990 (10.9) | 523 (2.9) | 344 (1.9) | 334 (1.8) | 165 (0.9) | |
| Non-Hispanic | ||||||||
| White | 51,748 (45.4) | 40,580 (35.6) | 14,205 (12.5) | 2,978 (2.6) | 1,741 (1.5) | 1,767 (1.6) | 963 (0.8) | |
| Black | 49,644 (38.1) | 49,659 (38.1) | 20,818 (16.0) | 4,464 (3.4) | 2,543 (2.0) | 2,190 (1.7) | 903 (0.7) | |
| Other | 11,606 (47.6) | 8,047 (33.0) | 2,861 (11.7) | 697 (2.9) | 409 (1.7) | 477 (2.0) | 279 (1.1) | |
| Hispanic | 35,358 (49.5) | 23,471 (32.9) | 8,211 (11.5) | 1,897 (2.7) | 1,020 (1.4) | 962 (1.3) | 499 (0.7) | |
* Percentages for the individual component categories might not add to 100% because of rounding. † Data from 43 reporting areas; excludes nine reporting areas (California, District of Columbia, Illinois, Maryland, Massachusetts, New Hampshire, New York State, Pennsylvania, and Wisconsin) that did not report, did not report weeks of gestation by age, or did not meet reporting standards. § Data from 29 reporting areas; excludes 23 reporting areas (California, Colorado, District of Columbia, Hawaii, Illinois, Iowa, Louisiana, Maine, Maryland, Massachusetts, Missouri, Nebraska, New Hampshire, New York City, New York State, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, Washington, and Wisconsin) that did not report, did not report weeks of gestation by race/ethnicity, or did not meet reporting standards.
| Year | Type of abortion | CFR per 100,000 legal abortions | |||
|---|---|---|---|---|---|
| Induced | Unknown** | Total | |||
| Legal | Illegal | ||||
| 1973 | 25 | 19 | 3 | ||
| 1974 | 26 | 6 | 1 | ||
| 1975 | 29 | 4 | 1 | ||
| 1976 | 11 | 2 | 1 | ||
| 1977 | 17 | 4 | 0 | ||
| 1978 | 9 | 7 | 0 | ||
| 1979 | 22 | 0 | 0 | ||
| 1980 | 9 | 1 | 2 | ||
| 1981 | 8 | 1 | 0 | ||
| 1982 | 11 | 1 | 0 | ||
| 1983 | 11 | 1 | 0 | ||
| 1984 | 12 | 0 | 0 | ||
| 1985 | 11 | 1 | 1 | ||
| 1986 | 11 | 0 | 2 | ||
| 1987 | 7 | 2 | 0 | ||
| 1988 | 16 | 0 | 0 | ||
| 1989 | 12 | 1 | 0 | ||
| 1990 | 9 | 0 | 0 | ||
| 1991 | 11 | 1 | 0 | ||
| 1992 | 10 | 0 | 0 | ||
| 1993 | 6 | 1 | 2 | ||
| 1994 | 10 | 2 | 0 | ||
| 1995 | 4 | 0 | 0 | ||
| 1996 | 9 | 0 | 0 | ||
| 1997 | 7 | 0 | 0 | ||
| 1998 | 9 | 0 | 0 | ||
| 1999 | 4 | 0 | 0 | ||
| 2000 | 11 | 0 | 0 | ||
| 2001 | 7 | 1 | 0 | ||
| 2002 | 10 | 0 | 0 | ||
| 2003 | 10 | 0 | 0 | ||
| 2004 | 7 | 1 | 0 | ||
| 2005 | 7 | 0 | 0 | ||
| 2006 | 7 | 0 | 0 | ||
| 2007 | 6 | 0 | 0 | ||
| 2008 | 12 | 0 | 0 | ||
| 2009 | 8 | 0 | 0 | ||
| 2010 | 10 | 0 | 0 | ||
| 2011 | 2 | 0 | 0 | ||
| 2012 | 4 | 0 | 0 | ||
| 2013 | 4 | 0 | 0 | ||
| 2014 | 6 | 0 | 0 | ||
| 2015 | 2 | 0 | 1 | ||
| 2016 | 6 | 1 | 1 | ||
| 2017 | 2 | 0 | 0 | ||
| 2018 | 2 | 0 | 0 | ||
Abbreviation: CFR = case-fatality rate. * Number of legal induced abortion-related deaths per 100,000 reported legal induced abortions. Because a substantial number of legal induced abortions occurred outside reporting areas that provided data to CDC, national CFRs (i.e., number of legal induced abortion-related deaths per 100,000 reported legal induced abortions in the United States) were calculated with denominator data from the Guttmacher Institute’s national survey of abortion-providing facilities; for 2018, the CFR was calculated using denominator data for 2017, the most recent year for which data are available. Case-fatality rates were computed for consecutive 5-year periods during 1973–2012 and then for a consecutive 6-year period during 2013–2018 because rates based on <20 cases might be unstable. † Certain numbers might differ from those in reports published previously because additional information has been supplied to CDC subsequent to publication. § An abortion is defined as legal if it was performed by a licensed clinician within the limits of state law. ¶ An abortion is defined as illegal if it was performed by any person other than a licensed clinician. ** Unknown whether abortion was induced or spontaneous.
Suggested citation for this article: Kortsmit K, Mandel MG, Reeves JA, et al. Abortion Surveillance — United States, 2019. MMWR Surveill Summ 2021;70(No. SS-9):1–29. DOI: http://dx.doi.org/10.15585/mmwr.ss7009a1 .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
- ACOG Clinical
- Green Journal
- For Patients
- For Parents
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Addressing a Crisis in Abortion Access
A case study in advocacy.
Lynch, Beatrice BS; Mallow, Michaela MPH; Bodde, Katharine E. S. MEd, JD; Castaldi-Micca, Danielle BA; Yanow, Susan MSW; Nádas, Marisa MD, MPH
Albert Einstein College of Medicine, The Bronx, New York; NYC Health + Hospitals; the New York Civil Liberties Union; the National Institute for Reproductive Health, New York, New York; the Later Abortion Initiative, Ibis Reproductive Health, Cambridge, Massachusetts.
Corresponding author: Marisa Nádas, MD, MPH, NYC Health + Hospitals, Jacobi Medical Center, The Bronx, New York; email: [email protected] .
Financial Disclosure The authors did not report any potential conflicts of interest.
The authors acknowledge the continuous efforts of clinicians who provide abortion and their supporters in New York.
Each author has confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at https://links.lww.com/AOG/C746 .
This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-NC-ND) , where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially without permission from the journal.
As restrictions on abortion increase nationwide, it is critical to ensure ongoing access to abortion care throughout pregnancy. People may seek abortions later in pregnancy as a result of financial or legal barriers that delay care or because of changing circumstances, such as the status of their partner, the health of other children, employment, or a new fetal diagnosis. New York State has been a beacon for abortion access since 1970. Yet, after Roe v Wade was decided, New York State abortion law was not in compliance with federal law, and risk-averse medical institutions hesitated to provide later abortions, forcing patients out of state for care. After years of advocacy, the Reproductive Health Act was passed in 2019. Clinicians and advocates collaborated to translate policy into expanded practice at NYC Health + Hospitals, the largest public health care system in the United States. NYC Health + Hospitals conducted an internal review, identified barriers to abortion care, and addressed these through improvements in public and internal communication, strengthening of procedural skills, and a better referral system. As a result, abortion services have become visible and the system’s capacity and gestational age limit have expanded. The example of NYC Health + Hospitals is an instructive model to ensure that abortion care is provided to the most vulnerable patients, including those who need care later in pregnancy. Given the ongoing threat to reproductive rights, this example of expanded access is particularly timely.
Health care systems can ensure that high-quality abortion care is available to all by identifying and removing barriers to services in collaboration with local advocates.
On December 1, 2021, the U.S. Supreme Court heard arguments in a Mississippi case, Dobbs v Jackson . 1 Experts who listened to the arguments and questions from the Justices agree that the current federal protections for abortion established by Roe v Wade (hereinafter “ Roe ”) 2 will be significantly weakened. Access will be particularly restricted for people who need abortions later in pregnancy. 3 In 2021 alone, there have been 108 abortion restrictions enacted in 19 states, the highest total in any year since the 1973 Roe decision, 4 most of which dramatically reduce the upper gestational age for abortion care.
Prohibiting abortion does not remove the need for abortion, but instead exacerbates the economic stratification between who can and cannot access care. 5 People need later abortions for many of the same reasons people need abortions earlier in pregnancy. Studies show that many of those who seek abortion care after 20 weeks of gestation wanted an earlier abortion but faced financial hurdles and legal barriers, including the need to travel for care. 6 For others, new information such as a fetal diagnosis may arise later in pregnancy. 7 And for others still, circumstances change and a wanted pregnancy becomes untenable, for example when a partner leaves or dies, a young child develops a serious illness, or someone in the family loses their job or health insurance. In all of these circumstances, the ability to access later care is essential and yet has constricted over the past decade. 8 It is anticipated that at least 22 states will quickly restrict abortion if the Supreme Court weakens federal protections, either following Texas’ example of banning abortion after an early point in pregnancy or falling in step with a currently enjoined Alabama law banning all abortions. These bans will result in people from these states traveling long distances to access services and will place a burden on clinicians who provide abortion in neighboring states, particularly for later abortion care. 9
It is critical that facilities expand their capacity to provide abortion care to those who will travel for care wherever possible. This article highlights the effort of the public health care system in New York City to expand access to later abortion care.
New York State has historically been considered a beacon for abortion access. New York State permitted abortion in 1970, 3 years before Roe . However, after Roe was decided in 1973, New York State law fell short of constitutional protections with respect to later care. The 1970 state law criminalized care after 24 weeks from the commencement of pregnancy unless a person’s life was at risk. 10 This meant that, even though Roe and subsequent cases protected care later in pregnancy when a pregnant person’s health or life is at risk or a fetus is not viable, risk-averse medical institutions in New York State were reluctant to provide later care in those instances. As a result, pregnant people and their families were forced to travel to distant states such as New Mexico and Colorado to seek later abortion care, far from the support of family, friends, and familiar physicians and at great financial cost, stress, and additional health risks. 11
Despite the legal challenges, over the past decades, advocates and health care professionals in New York City and New York State worked to expand access to care. This included interviewing health care professionals to better understand access points and needs, convening physician roundtables, and strengthening referral networks. Furthermore, attention was given to creating residency training initiatives, 12 seeking legal opinions from the New York State Attorney General to clarify health care professionals’ scope, and creating the first-in-the-nation direct municipal funding to individuals for abortion care. 13 However, access to later care did not improve, as evidenced in an informal New York City physician survey done by advocates in 2015, which revealed that hospitals were not providing care after 24 weeks of gestation, except for specific maternal or fetal indications, and only one ambulatory facility was providing care up to 26 weeks of gestation. Finally, after more than a decade of advocacy, in 2019, New York State passed the Reproductive Health Act. 14
The Reproductive Health Act made three principal changes to New York State’s abortion law. It 1) removed abortion from the criminal code; 2) clarified that advanced practice clinicians such as physician assistants, nurse practitioners, and licensed midwives may provide abortion care within their scope of practice; and 3) created protections that allow for abortion up to 24 weeks from the commencement of pregnancy and throughout pregnancy when the patient’s life or health is at risk or in cases of fetal nonviability. Advocates and clinicians have been working with the New York State Department of Health to create guidance interpreting the Reproductive Health Act’s parameters. The guidance was newly released on May 6, 2022 in the form of a letter from the Commissioner of Health, and it aligns with federal policy (eg, 45 CFR § 46.102) and the “ReVITALize: Gynecology Data Definitions” endorsed by the American College of Obstetricians and Gynecologists and numerous other respected national organizations, placing the “commencement of pregnancy” at implantation of a fertilized egg. 15 This will have a significant effect on clinical practice, placing “24 weeks from the commencement of pregnancy” at 27–28 weeks from the last menstrual period, as opposed to the previous interpretation of 26 weeks from the last menstrual period. Furthermore, this guidance aligns with the Supreme Court’s broad definition of health, 16 which supports individualized decision making between patient and health care team throughout pregnancy.
However, policy and legal changes do not automatically result in changes to medical practice. Determined New York City advocates worked closely with hospital and ambulatory clinicians who provide abortion to mobilize expanded services allowed under the Reproductive Health Act. One example of this successful collaboration is the expansion of abortion care within NYC Health + Hospitals.
CASE STUDY: NYC HEALTH + HOSPITALS
NYC Health + Hospitals is the largest public health care system in the United States, comprised of 11 hospitals (see Box 1), five long-term care facilities, a certified home health agency, and more than 100 community health centers. Its mission is to deliver high-quality comprehensive health care services to all with compassion, dignity, and respect. The health care system provides essential inpatient, outpatient, and home-based services to more than 1 million New Yorkers annually. NYC Health + Hospitals recognizes abortion as an essential and necessary component of comprehensive care, and abortion care is available at all of the hospitals; however, these services have expanded and contracted over the years, largely as a result of staffing changes, loss of institutional knowledge, competing priorities, and the evolving political landscape. Interpretations of New York State’s previous abortion law allowed for abortion care for any indication up to 26 weeks of gestation; yet, by 2019, when the Reproductive Health Act was passed, many staff were unaware of the existing legal parameters that regulated abortion, and few health care professionals had the clinical experience to provide care beyond 24 weeks of gestation, leaving a gap in care beyond that point. Furthermore, each hospital had its own organizational politics related to historical practices, unique patient communities, and current leadership views. However, NYC Health + Hospitals clinician–advocates identified strong supporters of reproductive rights at the systemwide leadership level and, with their endorsement, moved forward on expanding abortion access. Supported by policy advocates, these clinicians assessed existing barriers to care and created a strategic plan around communication, skill-building, and accessibility to expand abortion services to more fully align with the Reproductive Health Act.
NYC Health + Hospitals Acute Care Facilities
- NYC Health + Hospitals/Jacobi
- NYC Health + Hospitals/Lincoln
- NYC Health + Hospitals/North Central Bronx
- NYC Health + Hospitals/Coney Island
- NYC Health + Hospitals/Kings County
- NYC Health + Hospitals/Woodhull
- NYC Health + Hospitals/Bellevue
- NYC Health + Hospitals/Harlem
- NYC Health + Hospitals/Metropolitan
- NYC Health + Hospitals/Elmhurst
- NYC Health + Hospitals/Queens
COMMUNICATION
The first critical barrier identified was a lack of knowledge among patients and physicians about the abortion care NYC Health + Hospitals provided. Patients often went elsewhere for abortion care. Owing to communication challenges within the vast health care system, there was also low clinician awareness about abortion services. To improve patient awareness, clinician–advocates worked with the hospital communications team to edit patient materials to provide clear and accessible information about abortion on all websites, social media, and printed materials. To target awareness on the provider side, clinician–advocates provide ongoing presentations to give real-time clarification to clinicians and staff regarding what the Reproductive Health Act means for patient care. Additionally, the systemwide policy on abortion later in pregnancy, which was first written in 2003, was revised by a working group comprised of family planning directors from several hospitals. It was updated to align with the Reproductive Health Act and then approved by hospital legal counsel. It is being circulated to physician and nursing leadership to bring people up to date on current New York State law.
ENHANCING PROCEDURAL SKILLS
NYC Health + Hospitals clinicians also identified gaps in procedural skills that needed to be filled to expand services. Training for later abortion care is limited by the small volume of cases, the narrow specialization of care, and the misinformation and stigma about these services that exists within the medical community. To build clinician skills and participation, two educational projects are underway. The first is the development and implementation of training for physicians on administering feticidal injections. Although inducing fetal death is part of the clinical process for abortions after 24 weeks of gestation in NYC Health + Hospitals, the injection procedure is not a standard part of obstetrics and gynecology residency or family planning fellowship training. Abortion services historically have relied on maternal–fetal medicine specialists to perform this procedure; however, this depends on these specialists being comfortable participating in later abortion care. Training physicians who provide abortion services in the injection procedure will reduce the reliance on outside specialists. The second project focuses on the expansion of surgical skills needed to provide later abortion care. To facilitate training, physicians have been credentialed at multiple sites, allowing practitioners who are the sole providers of later abortion care at their facilities to find support for skill expansion outside their home institutions. Building a cadre of trained clinicians who provide abortion services who are able to administer injections and perform abortions across the pregnancy spectrum will solidify access to later abortion care within the health care system.
ACCESSIBILITY
Abortion is a time-sensitive service that requires appropriate and timely referral. The clinician–advocate team identified several obstacles within the existing referral network. There was no effective communication pathway to support timely referrals, nor a central, identifiable referral pathway for external health care professionals. In addition, because care can be cost-prohibitive for patients, seamless connections to sources of financial support such as abortion funds are a critical part of the referral system, but they were absent. To improve accessibility, NYC Health + Hospitals created a new, nimble referral system that can reduce logistical barriers to care. This referral system was built by a team comprised of physicians, administrators, members of the electronic medical record team, and data analysts. This new system integrates a patient’s geographic preference and gestational age to ensure an appropriate and timely referral. The health care system is also liaising with abortion funds to facilitate financial support for patients who face financial barriers to care.
Additionally, NYC Health + Hospitals created a new position of “Client Navigator,” following a successful model that was created in Massachusetts. 17 The Client Navigator’s primary role will be to accompany patients who need logistic or financial support through their abortion care experience, linking them to necessary resources and ensuring timely access to care. The Client Navigator will also support health care professionals both inside and outside the public health care system who are seeking referrals for their patients. This position has been filled and onboarding is underway.
In the past 6 years, NYC Health + Hospitals has successfully made abortion services more visible to the public by citing them in public speeches, clearly explaining them on their website, and adding information about these services in patient materials. The health care system added two institutions to the list of hospitals providing abortions at more than 20 weeks of gestation and expanded systemwide capacity to provide abortion care up to 26 weeks of gestation. The number of clinicians who provide abortion care has grown with internal training and changes in hiring priorities, resulting in 10 new providers. Further, there is now a strong network of health care professionals across institutions involved in a systemwide Reproductive Health Working Group, which creates policies and cross-institutional support. This working group consists of family planning leaders from several institutions within the system and serves as a team of experts that sets medical standards for the system and liaises with individual institutions. The group has created systemwide guidance for medication abortion, later abortion, and long-acting reversible contraception. Each institution has expanded access in an individualized way depending on local politics. Future systemwide goals include expansion of abortion services to include the option of induction termination and expanding beyond 26 weeks of gestation. With this measurable progress, NYC Health + Hospitals is increasing access to abortion care for people in New York City who need this critical service.
Replication of this model in other hospital systems where allowed by law is urgent. Given the ongoing threat to abortion access stemming from the Supreme Court and state legislatures that continue to pass restrictions aiming to eliminate care, it will take a national movement of health care professionals to create sustainable abortion access. The internal advocacy by NYC Health + Hospitals clinicians, supported by state-based advocates who helped to clear legislative and regulatory barriers, is a clear example of how to provide and expand abortion care for the most vulnerable patients, including those in need of care later in pregnancy. To ensure that the right to abortion does not become a hollow promise, health care systems must evaluate and address barriers, review and expand policies, and build coalitions with local advocates, supportive lawmakers, and abortion funds so that high-quality abortion care is a reality for all our communities.

Supplemental Digital Content
- AOG_140_1_2022_04_27_TPRLYNCH_22-285_SDC1.pdf; [PDF] (430 KB)
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Abortion as essential health care and the critical role your practice can play..., dobbs v jackson women\'s health organization</em> decision on obstetrics and gynecology graduating residents\' practice plans', 'woodcock alexandra l. md; carter, gentry ms; baayd, jami msph; turok, david k. md, mph; turk, jema phd, ma; sanders, jessica n. phd; pangasa, misha md; gawron, lori m. md, mph; kaiser, jennifer e. md, msci', 'obstetrics & gynecology', 'november 2023', '142', '5' , 'p 1105-1111');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link">effects of the dobbs v jackson women's health organization decision on..., instructions for authors—july 2021, pregnancy at age 35 years or older: acog obstetric care consensus no. 11, obstetrics & gynecology</em>', 'kaimal anjali j. md', 'obstetrics & gynecology', 'november 2023', '142', '5' , 'p 997');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link">new editor selected for obstetrics & gynecology.
- About the Hub
- Announcements
- Faculty Experts Guide
- Subscribe to the newsletter
Explore by Topic
- Arts+Culture
- Politics+Society
- Science+Technology
- Student Life
- University News
- Voices+Opinion
- About Hub at Work
- Gazette Archive
- Benefits+Perks
- Health+Well-Being
- Current Issue
- About the Magazine
- Past Issues
- Support Johns Hopkins Magazine
- Subscribe to the Magazine
You are using an outdated browser. Please upgrade your browser to improve your experience.

Credit: Wikimedia Commons
The public health case for abortion rights
Joanne rosen from the johns hopkins center for law and the public's health discusses dobbs v. jackson women's health organization, which heads to the supreme court dec. 1.
By Annalies Winny, Alissa Zhu, and Lindsay Smith Rogers
This article is adapted from a special episode of the Public Health On Call podcast called Public Health in the Field. Hear the full episode online .
Editor's note: The terms "woman" and "women" are used throughout this article because that is how the CDC and other sources record related data.
A potentially landmark battle is in play over abortion rights, and it's headed to the U.S. Supreme Court on Dec. 1.
In 2018, the Mississippi legislature passed and the governor signed House Bill 1510, known as the Gestational Age Act, which bans abortions after 15 weeks. There are exceptions if the life of the fetus or parent is at risk—but not in cases of rape or incest. The law violated Roe v. Wade, the 1973 Supreme Court decision that legalized abortion nationwide and protects the right to abortion prior to "viability" of the fetus, which is at around 24 weeks. House Bill 1510 was quickly blocked by lower federal courts but now the law's fate is up to the Supreme Court.
The outcome of this case—Dobbs v. Jackson Women's Health Organization—has implications for abortion rights far beyond Mississippi: A decision that previability bans are not unconstitutional could upend longstanding protections established by Roe v. Wade.
The conversation about abortion rights in the U.S. is a noisy one involving politics, precedents, and personal beliefs. What often gets short shrift, however, is the public health reality that restricting access to abortion frequently results in erosion of the health of women, especially low-income women and women of color. This is why abortion is so much more than a legal battle.
According to The Turnaway Study , a 10-year study that followed nearly 1,000 women who either had or were denied abortions, any women who were denied wanted abortions had higher levels of household poverty, debt, evictions, and other economic hardships and instabilities, says Joanne Rosen , associate director of the Johns Hopkins Center for Law and the Public's Health.
"The study also found that women who were seeking but unable to obtain abortions endured higher levels of physical violence from the men who had fathered these children," Rosen says. "And people who were turned away when seeking abortions endured more health problems than women who were able to obtain [them], as well as more serious health problems. That gives you a sense of the ways in which being unable to obtain abortions had really long lasting impacts on these peoples' lives."
A 2020 study in the American Journal of Preventive Medicine found that women living in states with less restrictive reproductive health policies were less likely to give birth to low-weight babies. Other research published in The Lancet found that restrictive abortion laws actually mean a higher rate of abortion-related maternal deaths.
Restrictive abortion laws affect more than just the health of individuals and families—they affect the economy, too. Research from The Lancet found that "ensuring women's access to safe abortion services does lower medical costs for health systems."
The Institute for Women's Policy Research has a host of data around how reproductive health restrictions impact women's earning potential, including an interactive map tool, Total Economic Losses Due to State-level Abortion Restrictions. In Mississippi, for example, the data indicate that removing restrictions to abortion would translate to a 1.8% increase of Black women in the labor force, over 2% for Hispanic women, and a leap of more than 2.6% for women who identify as Asian-Pacific Islander. This same tool calculates that removing restrictions on abortion access would translate to an estimated $13.4 million in increased earnings at the state level for Black women alone.
Abortion restrictions disproportionately affect people of color and those with low-incomes. According to data from the CDC, Black women are five times more likely to have an abortion than white women, and Latinx women are two times as likely as whites. Seventy-five percent of people who have abortions are low-income or poor.
Mississippi, Texas, and the Supreme Court
On Dec. 1, the Supreme Court will hear Dobbs v. Jackson Women's Health Organization and Rosen thinks it's unlikely the court would agree to hear the case if they were just going to affirm the status quo.
The case isn't the only one on the docket, however. Texas' Senate Bill 8, which bans abortion after six weeks of pregnancy, made headlines earlier this month and may impact the court's ultimate decision on the Mississippi case. The high-profile law came before the Supreme Court in November 2021 and Rosen said the important thing to note is that the justices didn't actually address whether the six-week ban is constitutional. Rather, they examined the unusual enforcement scheme of the law—where, when, and by whom the Texas law could be challenged.
Rosen says that the justices may compare the Texas law with the Mississippi law and, when considering a six-week abortion ban, a 15-week ban may seem less extreme. In this way, the Texas case could give the court some cover to uphold Mississippi's 15-week ban.
It's likely to be months before an opinion is released; Rosen says the court typically releases its decisions on high-stakes or controversial cases in June. And high stakes this is: for the future of abortion, for reproductive health rights, and for public health.
Posted in Health , Politics+Society
Tagged supreme court , reproductive health , abortion
Related Content

The invisible women

A case for OTC contraception
You might also like, news network.
- Johns Hopkins Magazine
- Get Email Updates
- Submit an Announcement
- Submit an Event
- Privacy Statement
- Accessibility
Discover JHU
- About the University
- Schools & Divisions
- Academic Programs
- Plan a Visit
- my.JohnsHopkins.edu
- © 2024 Johns Hopkins University . All rights reserved.
- University Communications
- 3910 Keswick Rd., Suite N2600, Baltimore, MD
- X Facebook LinkedIn YouTube Instagram
Watch CBS News
Abortion at "historic low" by all measures, new CDC study says
By Kate Smith
November 27, 2019 / 1:44 PM EST / CBS News
All statistics measuring abortion in the U.S. — the rate, the ratio to live births, and the absolute number — reached a "historic low" in 2016, according to new data released Wednesday from the Centers for Disease Control and Prevention.
In 2016, the most recent year available, the government agency reported 623,471 abortions, the lowest number the CDC has ever seen since it began tracking the procedure in 1969, according to the study. That's a 2.3% decline from 2015, when the CDC recorded 638,169 instances of the procedure.
During the same time period, the abortion rate dropped to 11.6 abortions per 1,000 women of reproductive age and the ratio fell to 186 abortions per 1,000 live births, according to the CDC's data. The agency compiled data from 48 reporting areas — 47 states plus New York City. (California, Washington D.C., Maryland and New Hampshire did not report data.)
The government agency's data were similar to results released earlier this year from the Guttmacher Institute, a research organization that supports abortion rights. According to Guttmacher, the abortion rate was 13.5 abortions per 1,000 women aged 15 to 44 in 2017, the lowest rate recorded since Roe v. Wade, the 1973 Supreme Court decision that legalized abortion nationwide. That's an 8% decline from 2014, the last time Guttmacher calculated the United States' abortion rate, and 54% lower than when the group recorded the peak rate in 1980.
Guttmacher attributed the decline to two factors: a declining pregnancy rate and a growing disparity between abortion access in liberal and conservative states. That divide stems largely from laws targeting the operations of clinics that provide abortions, a style of regulation known as a Targeted Regulation of Abortion Provider, or TRAP, law.
With a newly conservative Supreme Court, access to abortion has come under fire across the South and Midwest, where state lawmakers have raced to pass laws that ban the procedure in hopes of overturning Roe v. Wade.
In 2019, state politicians have introduced 300 bills restricting access to abortion , according to data compiled by the Guttmacher Institute. Twelve states have passed abortion bans, none of which are currently in effect .
In Wednesday's CDC study, the agency reported that 59% of people who received an abortion in 2016 already had at least one child. Additionally, the CDC reported just under two-thirds of abortions in 2016 occurred at or before eight weeks into a pregnancy, and 91% of all abortions happened at or before 13 weeks into a pregnancy. Nearly 28% of the 2016 abortions involved use of medication , rather than surgery.
More from CBS News
Nearly 50% of insured in U.S. get surprise medical bills, poll says

How to get the best home equity loan rate this August, according to experts

Mortgage rates tumble to lowest since April 2023 after weak jobs report

Stocks dive as investors fret over signs of U.S. economic slowdown
- Open access
- Published: 09 April 2022
Determinants of induced abortion among women received maternal health care services in public hospitals of Arba Minch and Wolayita Sodo town, southern Ethiopia: unmatched case–control study
- Mesfin Abebe 1 ,
- Abera Mersha 2 ,
- Nega Degefa 2 ,
- Feleke Gebremeskel 3 ,
- Etenesh Kefelew 3 &
- Wondwosen Molla 1
BMC Women's Health volume 22 , Article number: 107 ( 2022 ) Cite this article
4856 Accesses
4 Citations
6 Altmetric
Metrics details
About 210 million women become pregnant per year, with one out of every ten pregnancies terminating unsafely worldwide. In developing countries, unsafe induced abortion is a leading cause of maternal mortality and morbidity. In addition, the burden of public health is also greatest in developing regions. In Ethiopia, abortion was responsible for 8.6% of maternal deaths. Despite the problem's significance, little is known about the factors that lead to women terminating their pregnancies. Therefore, this study aims to identify the factors associated with having induced abortion in public hospitals of Arba Minch and Wolayita Sodo town, Southern Ethiopia.
An institutional-based unmatched case–control study was conducted among 413 women from 15th April to 15th June 2021 in selected public hospitals of Arba Minch and Wolayita Sodo town, Southern Ethiopia. Cases were women who received induced abortion care services or who received post-abortion care services after being presented to the selected public hospital with an attempt of induced abortion whereas controls were women who came for maternal health care (antenatal or postnatal care) services in selected public hospitals and never had history of induced abortion. The data were collected by pretested and structured questionnaires with face-to-face interviews via Kobo Collect v3.1 mobile tools and analyzed by STATA version14. Logistic regression model was used to identify factors associated with induced abortion. In this study P -value less than 0.05 with 95% CI was declared a result as statistically significant.
In this study, 103 cases and 309 controls were participated. Urban residence (AOR = 2.33, 95%CI:1.26, 4.32), encountered first sex at age of 20–24 years (AOR = 0.51, 95%CI:0.27,0.97), multiple sexual partner (AOR = 5.47, 95%CI: 2.98,10.03), women who had one child (AOR = 0.32, 95%CI: 0.10, 0.99), and good knowledge of contraceptives (AOR = 0.12, 95%CI: 0.03, 0.46) were identified as determinants of induced abortion.
Conclusions
Interventions focusing on those identified factors could probably reduce the burden and consequences of induced abortion. Sexual and reproductive health education and family planning programs would target urban dwellers, women who start sexual intercourse between the ages of 15 and 19, women with more than one sexual partner, women with a desire to limit childbearing, and women with poor contraceptive knowledge in order to reduce induced abortion.
Peer Review reports
Abortion is the termination of a pregnancy before the 28th week of gestation after the last normal menstrual period or birth weight less than 1000gm [ 1 ]. Induced abortion is described as intentional medical or surgical termination of a live fetus before it is viable, and spontaneous abortions generally referred to as miscarriages, occur when an embryo or fetus is lost due to natural causes [ 2 ]. Globally, from 2015 to 2019, approximately 73.3 million induced abortions were performed annually, with 45% of these abortions being performed unsafely. Almost half of these unsafe abortions occurred in developing countries, including Ethiopia. Developing countries accounted for more than 98% of all unsafe abortions [ 3 , 4 ]. About 210 million women become pregnant per year, with one out of every ten pregnancies ending in an unsafely induced abortion worldwide [ 5 , 6 ]. Every year, an estimated 68,000 women die as a result of unsafe abortions around the world, with another 5.3 million suffering temporary or permanent disability. In developing countries, unsafe abortion is a leading cause of maternal mortality and morbidity. In addition to this, the public health burden is greatest in the developing world [ 7 ].
In Africa, unsafe abortion complications account for almost half of all maternal deaths [ 8 ]. Abortion-related maternal deaths account for 13% of all maternal deaths worldwide, most of which are caused by unsafe abortions [ 9 ]. In sub-Saharan Africa, more than 77% of induced abortions are terminated in unsafe conditions and account for 50% of maternal deaths, with the abortion rate in sub-Saharan Africa almost doubling from 4.3 million to 8.0 million between 1995–1999 and 2015–2019 [ 10 , 11 ]. In East Africa, the annual abortion rate for all women of reproductive age is 34 per 1,000. Ethiopia has the world's fifth-highest rate of maternal mortality, with one in every twenty-seven women dying each year from pregnancy and childbirth complications [ 12 ]. Ethiopia is one of the low-income countries in sub-Sahara Africa with the highest maternal morbidity and mortality rates. The maternal mortality rate in Ethiopia was 412 maternal deaths per 100,000 live births, according to the 2016 Ethiopia Demographic and Health Survey (2016 EDHS) [ 13 ].
Around 3.27 million women became pregnant each year in Ethiopia, of which approximately half-million ends by abortion and the rate of abortion is highest in the urban area of Ethiopia, which is 92 per 1000 in Addis Ababa and 78 per 1000 in smaller regions like Harari and Dire Dewa [ 12 , 14 ]. Previous studies in different parts of Ethiopia found that the prevalence of induced abortion was 42.7%, 18.8%, 12.3%, and 4% in the Harari region, Southwest Ethiopia, Guraghe Zone, and Gondar Town, respectively [ 6 , 12 , 14 , 15 ]. In Ethiopia, abortion was responsible for 8.6% of maternal deaths [ 16 ]. Ethiopia made some strides in 2005 by revising the abortion law, which previously only allowed procedures to save a woman's life, and making safe abortion available to many women. Following that, abortion is legal whether the pregnancy is the result of rape or incest, the continuation of the pregnancy risks the mother's or child's health, the fetal disability is severe or incurable, and the woman is in a minority that is physically and mentally unprepared for childbirth [ 17 ].
Despite the presence of technological advancement in health care, unsafe abortion remains essentially unchanged globally as well as Ethiopian women are suffering from an increased risk of abortion-related complications, due to various reasons for example unmet family planning method need, rape, early sexual practice, etc. [ 18 , 19 ]. Women seek induced abortion for a variety of reasons, depending on their circumstances. According to a study conducted in Denmark and Uganda, the strongest determinant of women's decision to have an abortion is being single, followed by being under the age of 19, having two or more children, being a student, or being unemployed [ 20 , 21 ]. In Ethiopia, similar findings were revealed that unwanted pregnancy, single marital status, young age, low income, occupational status, the mother's level of education, is the major contributing factors to induced abortion [ 6 , 14 , 22 ].
Several efforts have been made to improve abortion-related services, including the construction of more health centers and the training of more mid-level healthcare providers, the expansion of abortion services to primary healthcare units, and the development and dissemination of national guidelines for providing legal and safe abortion services [ 23 ]. In 2014, the guideline was revised to update the gestational age limits for medication abortion and to make second-trimester abortion services more available [ 24 ]. As a result of these efforts, unintended pregnancy decreased to 38% in 2014 from 42% in 2008, abortion in health facilities increased to 53% in 2014 from 27% in 2008, and induced abortion and post-abortion care provided by mid-level providers increased to 53% in 2014 from 27% in 2008 [ 25 ].
Even with numerous initiatives and attempts to increase access to safe abortion facilities, nearly six out of ten abortions in Ethiopia are still conducted in a risky manner [ 26 ]. Despite the problem's significance, little is known about the factors that lead to women terminating their pregnancies. A further enhancement is still needed; so assessing its risk factors is important for tracking progress toward sustainable development goals. As a result, this study aims to identify determinants of induced abortion among women who received maternal health care services in public hospitals of Arba Minch and Wolayita Sodo town, southern Ethiopia, 2021.
Study setting, and period
This study was conducted at selected public hospitals of Arba Minch and Sodo town, Southern Ethiopia from April 15th–June 15th, 2021. Arba Minch and Wolayita Sodo are town found in the South Nations, Nationalities and Peoples’ Region (SNNPR) of Ethiopia. In the towns of Arba Minch and Wolayita Sodo, there are four hospitals, but the study was conducted in selected two public hospitals (Arba Minch General Hospital and Wolayita Sodo University Teaching & Referral Hospital). The total population of the Arba Minch town 112,724 among them 50.2% are females whereas Wolayita Sodo 250,521 among them 79,871 (52%) males, and 73,650 (48%) females. There are four public health facilities (one general hospital, one primary hospital and two health centers), thirty-two private medium and higher clinic, one Marie Stopes clinic, twelve drug stores, and two community pharmacies in Arba Minch town [ 27 ]. According to the medical director's report for the fiscal year 2020, Arba Minch General Hospital provides 100 comprehensive abortion care services, 195 antenatal care services, and 180 postnatal care services per month on average. There are two (one government and one private) hospital, three health centers, one Marie Stopes clinic and thirty private medium and higher clinics in Wolayita Sodo town [ 28 ]. According to the medical director's report for the fiscal year 2020, Wolayita Sodo teaching and referral Hospital provides 150 comprehensive abortion care services, 250 antenatal care services, and 210 postnatal care services per month on average. per month on average.
Study design
An institutional based unmatched case–control study was conducted.
Source population
All women who received maternal health care services in the public hospitals of Arba Minch and Wolayita Sodo town.
Study population
All women who received comprehensive abortion care and those who visited maternal and child health (MCH) units for antenatal or postnatal care services in selected public hospitals of Arba Minch and Wolayita Sodo town during the data collection period.
Selection of cases and controls
Cases: women who received induced abortion care services in selected public hospitals during the data collection period or who received post-abortion care services after being presented to the selected public hospital with an attempt of induced abortion.
Controls: women who had at least one pregnancy history in the last 12 months, and who came for maternal health care (antenatal or postnatal care) services in selected public hospitals and never had history of induced abortion.
Exclusion criteria
Women presented to the selected public hospitals for spontaneous abortion care after diagnosed by physician and unable to communicate or seriously ill until the end of the data collection period were excluded.
Sample size determination
For a case–control study, the sample size for this study was determined by using the Stat Cal application of Epi- Info version 7 software and two population proportion formulas. The following assumptions were considered: 95% level of confidence, 80% of power, the ratio of case to control 1:3 and percent of case exposed 8.2% and percent of control with exposure 21%. The percentages of cases and controls of exposure variable were taken from study conducted in Addis Ababa that the most determinate variables for induced abortion were monthly income [ 29 ]. Based on the above assumptions, the minimum estimated sample size for this study was 94 cases and 281 controls. After considering 10% of non-response rate, the final sample size for this study was 103 cases and 310 controls.
Sampling technique and procedures
In this study, Arba Minch general hospital and Wolayita Sodo University teaching & referral Hospital were included. By reviewing the previous year's two-month report in a data collection period, in Arba Minch General hospital, and Wolayita Sodo University teaching & referral hospital on average of 40, and 80 women received induced abortion care and 295 & 340 women received maternal health care services respectively. The proportional allocation method was used to include 413 women in the sample. The cases were selected using a consecutive sampling technique until the required sample size was reached. Controls were selected using a systematic random sampling technique. The lottery method was used to select the first control and then every second controls was interview until the required sample size was reached (Fig. 1 ).
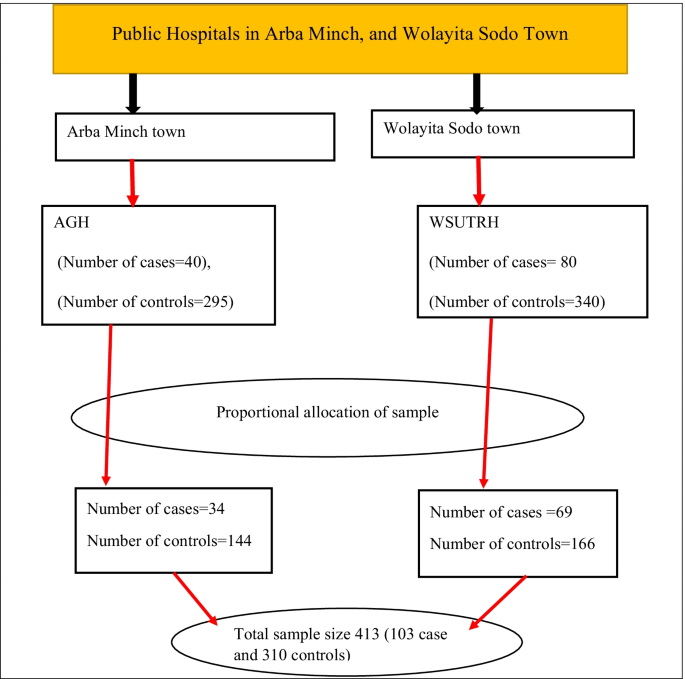
Schematic presentation of sampling procedures to identify the determinants of induced abortion among women received maternal health care services in public hospitals of Arba Minch and Wolayita Sodo town, Southern Ethiopia, 2021. Whereas AGH Arbaminch General Hospital, WSUTRH Wolayita Sodo University Teaching and Referral Hospital
Study variables
Induced abortion was the dependent variable for this study. The independent variables were socio-demographic and economic factors (age, residence, marital status, occupational status, educational status, monthly income), reproductive and maternal health related factors (age at first marriage, age at first sexual encounter, multiple sexual partner, number of pregnancy, number of living children, pregnancy status), and contraceptive related factors (use, and knowledge).
Operational definition and measurements
Induced abortion : intentional termination of pregnancy, by any means or person other than spontaneous [ 30 ]. Contraceptive use : the percentage of women who used any modern contraceptive methods prior to current pregnancy [ 31 ]. Contraceptive knowledge : based on bloom cut of point women who answered 75–100%, 50–74%, and < 50% correctly on six knowledge-assessment questions were considered to have good knowledge, moderate knowledge, and poor knowledge, respectively [ 32 ].
Data collection tools and procedures
Data were collected using a standardized and pretested interviewer-administered questionnaire, which was adapted from previous related studies [ 22 , 29 , 31 , 33 ]. The questionnaires contain three sections: Sociodemographic characteristics, reproductive and maternal health related, and contraceptive related factors (Additional file 1 ). Six BSc holder midwives were recruited to collect the data. In addition to this two supervisors who have MSc degree holders were recruited for supervisory activities. The principal investigator gave three days of theoretical and practical training to data collectors and supervisors on data collection tools, interview techniques, information confidentiality, and the objective and relevance of the study. The Kobo collect version 3.1 application was installed on the data collector's Android mobile, and the blank form was downloaded from the Kobo toolbox server. Two weeks before the actual data collection, the tool was pre-tested on 20 women (5 cases and 15 controls) in Chencha and Bodti primary hospitals. After obtaining respondent informed consent, an exit face-to-face interview and record review were used to collect data. Supervisors communicated on a regular basis with data collectors to ensure that the data collection procedure was followed. To avoid misclassification questionnaires gave a code for cases and controls (1 = cases, 0 = controls) and the women seeking maternal health care services were asked about a history of previous induced abortions and their medical records were reviewed to ensure they are true controls. Finally, on a weekly basis, the data collectors sent the filled questionnaire forms to the Kobo toolbox server.
Data quality management
The questionnaire initially prepared in English and translated to the Amharic language, and then translated back to English by the expert to check the consistency. Data collectors and supervisors were trained for two days to become familiar with all types of data, tools, and data collection methods and objectives, as well as one day of practical sessions on Kobo Collect. A pre-test was conducted on 5% of the participants in Chencha and Bodti primary hospital, and any ambiguity, as well as the missed points, were added into the final version of the questionnaire. The supervisors checked completed questionnaires for key contents before uploading them from the Android mobile phone to the Kobo toolbox server to ensure data quality. All data were collected on-site using Android mobile devices and uploaded to the Kobo server on a weekly basis using Kobo collect version 3.1. The principal investigator also checked the sent files from each data collector on a regular basis for consistency and completeness.
Data processing and analysis
The Kobo server data were downloaded as an excel file and exported to SPSS V.25 for cleaning, coding, ensuring completeness and accuracy, and then to Stata V.14 software for further analysis. A descriptive analysis was done to describe the pertinent characteristics of the study participants. After that, simple frequencies, percentages, and summary measures were computed. Both bivariate and multivariable analyses were used to assess the association between each independent variable and the outcome variable by using binary logistic regression. The goodness of fit was checked by Hosmer and Lemeshow test. Variables with a 95% confidence interval and P-value < 0.25 during the bivariate analysis were included in the multivariable logistic regression analysis in order to control all potential confounding variables. In addition, even if the above parameters were not being met, variables that were significant in previous studies and from a contextual viewpoint were included in the final model. Multi co-linearity was checked by co-linearity diagnostic statistics via variance inflation factors and tolerance test. Adjusted odds ratios with a 95% confidence interval were calculated and P-value less than 0.05 was considered as statistically significant. Finally, data were being presented using tables, graphs, and texts.

Sociodemographic and economic characteristics
Out of 413 participants, 412 women completed the face-to-face interview with a response rate of 100% for cases and 99.7% for controls. The report encompasses 412 women of which 103 (25%) were cases while 309 (74.8%) were controls and it was unmatched case–control study.
The mean and standard deviation of respondents age were 25.7 ± 5 years (cases 24 ± 6.2 and controls 26.2 ± 4.5). The minimum age of cases was 15 years old and maximum age was 38 years old whereas the minimum and maximum age of controls was 16 and 40 years old respectively. Among the study participants, 28(27.18%) of the cases and 140(45.31%) of controls age ranges from 25 to 29 years. Of the respondents, 52(50.49%) cases and 155(50.16%) controls were Wolayita ethnicity. Seventy-six (73.79%) of the cases and 175 (56.63%) of controls were urban residents. Regarding marital status, around 41 (39.8%) of the cases and 306(99%) controls were married and 45(43.69%) of the cases and 151(48.87%) of controls were protestant religion followers.
Regarding educational status of women, 43(41.75%) of the cases and 90(29.13%) controls had secondary educational level. The overall median and interquartile range of monthly income was 62.5 (25 to 100) USD and 37.5 (interquartile range 12.5 to 90 USD) for cases whereas 62.5(30 to 107.5 USD) for controls. Out of the respondents, 62(60.19%) for cases and 130(42%) for controls were earned less than 50 USD per month. Related to the occupational status of respondents, 13(12.62%) of the cases and 106(34.3%) controls were housewife (Table 1 ).
Reproductive and maternal health characteristics
Fourteen (25.9%) of the cases and 64 (20.78%) of the controls were married before the age of 18. The overall mean and standard deviation of women age at first marriage was 21 ± 3.1 (cases 21.29 ± 3.6 and controls 21 ± 3). The minimum age at first marriage among cases was 16 years old and maximum age was 34 years old whereas the minimum and maximum age of first marriage among controls was 15 and 33 years old respectively.
Sixty-five (63.1%) of the cases and 118 (38.19%) of the controls age ranges from 15 to 19 at the time sexual debut. The mean and standard deviation of women age at first sexual encounter was 20 ± 2.99 years (cases 18.87 ± 3.2 and controls 20 ± 2.8). In both cases and controls, the minimum and maximum age at first sex were 15 and 28 years old, respectively. Forty-two (40.78%) of cases and 48 (15.53%) of controls had more than one sexual partners in past 12 months. Out of respondents, 42 (40.78%) of cases and 76 (24.6%) of controls had at least one pregnancy during their lifetime. Fifty-one (49.51%) of the cases and 61(19.74%) of controls had no history of delivery. Regarding number of alive children, 15(14.56%) of the cases and 130(42%) of the controls had one alive child.
About 72 (69.9%) of cases and 33 (10.68%) of controls reported their last pregnancy was unplanned and Partner pressure (33.33%) and contraceptive failure (27.78%) were the most common reasons for unplanned pregnancy among cases. Whereas contraceptive failure was reported by more than half (54.55%) of the controls as the main reason for unplanned pregnancy. In terms of abortion complications, 43 (41.75%) of the cases and 164 (53.07%) of the controls had awareness about abortion-related complications. Of those who knew abortion complications, 31(30%) of cases and 106(34.3%) of controls were aware of at least two or more complications of induced abortion. Out of respondents, 35(33.98%) for cases and 100(32.36%) for controls had information about Ethiopian abortion law (Table 2 ). In the current studies, 44(42.72%) cases stated that their reason for termination was an unplanned pregnancy. Approximately 9.71% of cases terminated their pregnancy because the mother's life would be threatened if the pregnancy continued (Fig. 2 ).
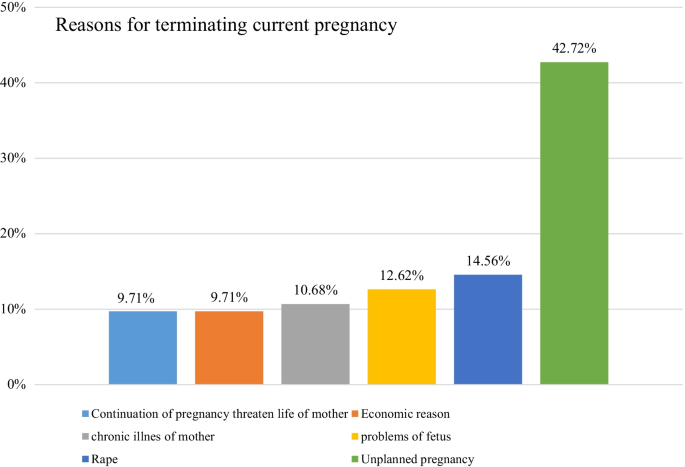
The reason for termination of current pregnancy among cases who received maternal health care services in public hospitals of Arba Minch and Wolayita Sodo town, southern Ethiopia, 2021
Contraceptive related characteristics
Eighty-seven (84.47%) of cases and 301 controls (97.41%) had heard about family planning methods. Regarding the source of information, 47(54%) of the cases and 183(60.8%) controls (60.8%), 29(33.33%) of cases and 58(19.27%) controls, & 11(12.64%) of cases and 60(19.93%) controls were heard from health facilities, mass media/printed materials, and family/friends respectively. Eighty-six (83.5%) of the cases and 297 (96.12%) of the controls were aware of at least one type of modern contraceptive. As a result, oral contraceptive pills 60 (69.77%) and Nexplanon 252 (84.85%) were the most commonly mentioned contraceptive methods by cases and controls, respectively. Eighty-two (79.61%) of the cases and 303 (98.06%) of the controls were aware of contraceptive methods used to prevent unwanted pregnancy, with the majority of 84 cases (84.55%) and 305 controls (98.7%) were aware of contraceptive methods used to space & a limited number of children. Eighty-one (78.64%) of cases & 291(94.17%) of controls had good knowledge about contraceptive methods (Table 3 ).
Determinants of induced abortion
In binary logistics regression analysis, age, residence, educational status, monthly income, age at first intercourse, multiple sexual partners, number of alive children, and knowledge on contraceptives were found to be candidate variables for final multivariable logistics regression analysis model.
In the multivariable analysis, residence, age at first sex, multiple sexual partners, number of children, and knowledge of contraceptives were statistically associated with induced abortion. The odds of having an induced abortion were 2.33 times higher in women who lived in an urban area than women living in rural areas (AOR = 2.33, 95%CI: 1.26, 4.32). A woman who had encountered first sex at age of 20–24 years was 49% less likely to have an induced abortion as compared to women who encounter first sex at age of 15–19 years (AOR = 0.51, 95% CI:0.27,0.97). The odds of induced abortion were 5.47 times higher among women who had more than one sexual partner than those who had a single sexual partner (AOR = 5.47, 95%CI: 2.98, 10.03). Women who had one child were 68% less likely to have an induced abortion than those who had three or more children (AOR = 0.32, 95%CI: 0.10, 0.99). The odds of induced abortion were 88% less likely among women who had good knowledge of contraceptives than those who had poor knowledge of contraceptives (AOR = 0.12, 95%CI: 0.03, 0.46) (Table 4 ).
Inducing abortion is one of the major public health concerns in the world today. Maternal mortality and morbidity continue to be alarmingly high. Sub-Saharan Africa has the highest estimated proportion of induced abortions, and women are more likely to die as a result of abortion than any other region of the world [ 10 ]. Identifying the determinants of induced abortion is crucial for many sub-Saharan African countries like Ethiopia. Thus, this study revealed a facility-based case–control study to identify factors associated with induced abortion in the study settings. Among characteristics assessed in this study; residence, age at first sex, multiple sexual partners, number of children, and contraceptive knowledge had a significant association with induced abortion.
This study showed that urban residents were more likely to report having an induced abortion compared with those who were rural residents. This finding was supported by studies done in different parts of Ethiopia [ 15 , 34 , 35 , 36 ]. This finding was also consistent with a study conducted in Ghana [ 37 ]. This may be due to the fact that women who live in urban are exposed to a variety of factors (like peer pressure, drinking too much alcohol, unprotected sex) that make them vulnerable to risky sexual behaviors that result in an unwanted pregnancy. Another possible explanation is that women in urban areas have more access to abortion services than women in rural areas. Similarly, those living in urban areas are more likely to have premarital sex, which can lead to unintended pregnancy and induced abortion. The finding of this study is supported by the findings of the 2016 EDHS, which revealed that urban residents have a higher rate of premarital sex than their rural counterparts [ 38 ].
As indicated in this study, women who had their first sex start between the ages of 15 and 19 were more likely to have induced abortion than those who had their first sexual intercourse at the age of 20 or later. Similarly, other studies from Ethiopia [ 29 ], and Chile [ 39 ] have found that women who had their sexual debut at a younger age are more likely to have an induced abortion. This could be due to adolescents having unstable marital relationships, not completing their education, and lack of knowledge about safe sex practices, including how to prevent unintended pregnancy and other reproductive health problems. Another possibility is that women who had their first sexual encounter at a younger age may have limited knowledge on how to use family planning. Multiple sexual partners were found to be significant determinants of induced abortion in this study. Women who had more than one sexual partner were found to have increased odds of having an induced abortion than women who had a single sexual partner. This finding was consistent with studies done in Ethiopia [ 35 , 36 ], and Cambodia [ 40 ]. This could be due to the fact that having multiple sexual partners leads to women being in unstable marital relationships, which leads to irregular contraceptive use that also leads to contraceptive failure and unwanted pregnancy.
In this study, women who had one child were less likely to report having an induced abortion as compared with women who had three or more children. This finding was supported by studies done in Ethiopia [ 6 , 29 ], Nepal [ 41 ], and Iran [ 42 , 43 ]. This is obvious that women who had several pregnancies would have the tendency not to have additional children so they may induce their current pregnancy to avoid unwanted pregnancies.
Women who had good knowledge of contraceptives were less likely to have an induced abortion than those who had poor knowledge of contraceptives. This finding was congruent with studies done in Ethiopia [ 44 ], Ghana [ 31 ], and Tanzania [ 45 ]. This could be due to the fact that women who have inadequate knowledge of contraceptives are unable to prevent themselves from unintended pregnancies and thus seek induced abortion to avoid having unwanted children.
The strength of this study was used primary data by directly interviewing study participants, and incident cases were used to reduce the problem of establishing a temporal relationship. Since this study was conducted at a general and teaching hospital with an experienced obstetrician and gynecologist, there was no misclassification between spontaneous and induced abortion among cases. The cases were included in this study after being diagnosed by a physician.
Limitation of the study
However, the study has some limitations. There is a concern of information bias because women's history of induced abortion was self-reported, so some controls may have had abortions in the past but wanted to give responses. The medical records of controls were cross-checked to ensure they had not obtained an abortion. Secondly, this study was also prone to recall bias, as respondents may not have been able to recall past events accurately. Thirdly, non-governmental and private health care facilities were not included in this study. Finally, because the study was conducted in a health facility, the findings may not be generalizable to the general population of women.
Women with urban residents, early sexual initiation, having multiple sexual partners, poor knowledge of contraceptives and those with a higher number of children in the household were independently associated factors with induced abortion. As a result, interventions focusing on those identified factors by the concerned bodies could probably reduce the burden and consequences of induced abortion. Sexual and reproductive health education and family planning programs should target community-based outreach programs regularly to raise community awareness of contraception by involving adolescents and the prevention of unintended pregnancy to reduce induced abortion.
Availability of data and materials
The datasets generated and /or analyzed during the current study are not publicly available due to preserving participant anonymity but are available from the corresponding author on reasonable request (Mesfin Abebe, [email protected]).
Abbreviations
Coronavirus Disease 2019
Ethiopian Demographic and Health Survey
Intra-uterine contraceptive device
Maternal and child health
Arbaminch General Hospital
Wolayita Sodo University Teaching and Referral Hospital
Health FD. Technical and procedural guidelines for safe abortion services in Ethiopia second edition. 2013, FDRE-FHD Addis Ababa.
Cunningham, F., et al., Williams obstetrics, 24e. 2014: Mcgraw-hill New York, NY, USA.
Gebremedhin M, et al. Unsafe abortion and associated factors among reproductive aged women in Sub-Saharan Africa: a protocol for a systematic review and meta-analysis. Syst Rev. 2018;7(1):1–5.
Article Google Scholar
Bearak J, et al. Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019. Lancet Glob Health. 2020;8(9):e1152–61.
Article PubMed Google Scholar
Organization WH. Safe and unsafe induced abortion: global and regional levels in 2008, and trends during 1995–2008. 2012, World Health Organization.
Tesfaye G, Hambisa MT, Semahegn A. Induced abortion and associated factors in health facilities of Guraghe zone, southern Ethiopia. Journal of pregnancy, 2014. 2014.
Warriner I, Shah I. Preventing unsafe abortion and its consequences: priorities for research and action. 2006. New York, NY. 10017: p. 1–6.
Hord C, Wolf M. Breaking the cycle of unsafe abortion in Africa. Afr J Reprod Health, 2004;29–36.
Siraneh Y, Workneh A. Determinants and Outcome of Safe Second Trimester Medical Abortion at Jimma University Medical Center, Southwest Ethiopia. J Pregnancy, 2019. 2019.
Bankole A, et al. From unsafe to safe abortion in Sub-Saharan Africa: slow but steady progress;2020.
Mizana BA, Woyecha T, Abdu S. Delay in decision and determinants for safe abortion among women at health facilities in south West Ethiopia: facility based cross sectional study. Int J Equity Health. 2020;19(1):1–6.
Oumer M, Manaye A. Prevalence and associated factors of induced abortion among women of reproductive age group in Gondar Town, Northwest Ethiopia. Int J Public Health. 2019;7(3):66.
Google Scholar
CSA I. Central Statistical Agency. Ethiopia demographic and health survey, 2016.
Jamie AH, Abdosh MZ. Prevalence of induced abortion and associated factors among women of reproductive age in Harari region, Ethiopia. Public Health Indonesia. 2020;6(2):35–40.
Nigussie T, et al. Prevalence of induced abortion and its associated factors among female students of health science in South West Ethiopia. Open Nurs J 2020;14(1).
Mekonnen W, Gebremariam A. Causes of maternal death in Ethiopia between 1990 and 2016: systematic review with meta-analysis. Ethiopian Journal of Health Development, 2018;32(4).
Holcombe SJ. Medical society engagement in contentious policy reform: the Ethiopian Society for Obstetricians and Gynecologists (ESOG) and Ethiopia’s 2005 reform of its penal code on abortion. Health Policy Plan. 2018;33(4):583–91.
Article PubMed PubMed Central Google Scholar
Gebremedhin M, et al. Unsafe abortion and associated factors among reproductive aged women in Sub-Saharan Africa: a protocol for a systematic review and meta-analysis. Syst Rev. 2018;7(1):130.
Amhare AF, Alemayehu DG, Bogale AA. Factors associated with unsafe induced abortion among women who attended Fitche Hospital, Oromia, Ethiopia: Cross-sectional study. 2019.
Rasch V, et al. Induced abortion in Denmark: effect of socio-economic situation and country of birth. Eur J Public Health. 2008;18(2):144–9.
Kaye DK, et al. Domestic violence as risk factor for unwanted pregnancy and induced abortion in Mulago Hospital, Kampala, Uganda. Trop Med Int Health. 2006;11(1):90–101.
Tilahun F, Dadi AF, Shiferaw G. Determinants of abortion among clients coming for abortion service at felegehiwot referral hospital, northwest Ethiopia: a case control study. Contracept Reprod Med. 2017;2(1):1–6.
Health FD. Health Sector Development Program IV: 2010/11–2014/15. 2010, Ministry of Health Addis Ababa.
Holcombe SJ, Berhe A, Cherie A. Personal beliefs and professional responsibilities: Ethiopian midwives’ attitudes toward providing abortion services after legal reform. Stud Fam Plann. 2015;46(1):73–95.
Moore AM, et al. The estimated incidence of induced abortion in Ethiopia, 2014: changes in the provision of services since 2008. Int Perspect Sex Reprod Health. 2016;42(3):111.
Bridgman-Packer D, Kidanemariam S. The implementation of safe abortion services in Ethiopia. Int J Gynecol Obstet. 2018;143:19–24.
in The Gamo zone health Department 2021.
The Wolayita Zone Health Department. 2021.
Megersa BS, et al. Factors associated with induced abortion among women of reproductive age attending selected health facilities in Addis Ababa, Ethiopia: a case control study. BMC Womens Health. 2020;20(1):1–11.
Behulu GK, Fenta EA, Aynalem GL. Repeat induced abortion and associated factors among reproductive age women who seek abortion services in Debre Berhan town health institutions, Central Ethiopia, 2019. BMC Res Notes. 2019;12(1):1–5.
Klutsey EE, Ankomah A. Factors associated with induced abortion at selected hospitals in the Volta Region, Ghana. Int J Women’s Health. 2014;6:809.
Adane AA, et al. Modern contraceptive utilization and associated factors among married Gumuz Women in Metekel Zone North West Ethiopia. BioMed Res Int, 2020. 2020.
Bonnen KI, Tuijje DN, Rasch V. Determinants of first and second trimester induced abortion-results from a cross-sectional study taken place 7 years after abortion law revisions in Ethiopia. BMC Pregnancy Childbirth. 2014;14(1):1–9.
Senbeto E, et al. Prevalence and associated risk factoprs of Induced Abortion in Northwet Ethiopia. Ethiopian J Health Dev. 2005;19(1):37–44.
Waktola MI, et al. Repeat induced abortion and associated factors among women seeking abortion care services at Debre Markos town health institutions, Amhara regional state, Ethiopia, 2017. BMC Res Notes. 2020;13(1):1–6.
Mekie M, et al. The level and deriving factors of repeat-induced abortion in Ethiopia: a systematic review and meta-analysis. Heliyon 2021; 7 (1): e05984.
Mote CV, Otupiri, E, Hindin MJ. Factors associated with induced abortion among women in Hohoe, Ghana. Afr J Reprod Health 2010;14(4).
Ethiopia CSA, Macro O. Ethiopia demographic and health survey. Addis Ababa: Central Statistical Agency, 2016.
Huneeus A, et al. Induced abortion according to socioeconomic status in Chile. J Pediatr Adolescent Gynecol 2020; 33 (4):415–420. e1.
Yi S, et al. Factors associated with induced abortion among female entertainment workers: a cross-sectional study in Cambodia. BMJ Open, 2015;5(7): e007947.
Mehata S, et al. RETRACTED ARTICLE: Factors associated with induced abortion in Nepal: data from a nationally representative population-based cross-sectional survey. Reprod Health. 2019;16(1):1–8.
Ranji A. Induced abortion in Iran: prevalence, reasons, and consequences. J Midw Women’s Health. 2012;57(5):482–8.
Erfani A. Determinants of induced abortion in Tehran, Iran: the role of contraceptive failure. Eur J Contracept Reprod Health Care 2021: p. 1–13.
Woldeamanuel BT. Assessment of determinant factors of pregnancy termination among women of reproductive age group in Ethiopia: Evidence from 2016 Ethiopian Demographic and Health Survey. Int J Sex Reprod Health Care. 2019;2(1):010–5.
Mpangile GS, Leshabari MT, Kihwele DJ. Factors associated with induced abortion in public hospitals in Dar es Salaam, Tanzania. Reprod Health Matters. 1993;1(2):21–31.
Download references
Acknowledgements
Our heartfelt thanks go to the Arba Minch general hospital and Wolayita Sodo University teaching and referral hospital administration staff and health care professionals working in the hospital who gave support during data collection, data collectors, and study participants. Finally, yet importantly, we would like to say thank you to all people who gave support us directly or indirectly.
Arba Minch University provided funds for the data collection and stationary materials of this research work with a project grant code of Acct. No GOV-1000021480502. The website of the university is www.amu.edu.et . "The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript."
Author information
Authors and affiliations.
Department of Midwifery, College of Medicine and Health Sciences, Dilla University, Dilla, Ethiopia
Mesfin Abebe & Wondwosen Molla
School of Nursing, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia
Abera Mersha & Nega Degefa
School of Public Health, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia
Feleke Gebremeskel & Etenesh Kefelew
You can also search for this author in PubMed Google Scholar
Contributions
MA designed the study, was involved in data collection, analysis, and interpretation of the result and drafted the paper, and participated in preparing all versions of the manuscript. AM, ND, FG, EK and WM assisted in the design and the proposal development, monitored data collection, assisted during analysis, and revised subsequent drafts of the paper. All authors read and approved the final manuscript.
Authors Information
Mesfin Abebe (BScM, MSc in Maternity and Reproductive Health Nursing), Department of Midwifery, College of Medicine & Health Sciences, Dilla University, Dilla, Ethiopia.
Abera Mersha (BScN, MScN, Assistant Professor in Maternity and Neonatal Nursing), School of Nursing, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia.
Nega Degefa (BScN, MScN, Assistant Professor in Pediatric and Child Health Nursing), School of Nursing, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia.
Feleke Gebremeskel (BScN, MPH, Associate Professor in Reproductive Health), School of Public Health, College of Medicine & Health Sciences, Arba Minch University, Arba Minch, Ethiopia.
Etenesh Kefelew (BSc, MPH in Epidemiology and Biostatistics), School of Public Health, College of Medicine & Health Sciences, Arba Minch University, Arba Minch, Ethiopia.
Wondwosen Molla (BScM, MSc in Maternity Nursing), Department of Midwifery, College of Medicine & Health Sciences, Dilla University, Dilla, Ethiopia.
Corresponding author
Correspondence to Mesfin Abebe .
Ethics declarations
Ethics approval and consent to participate.
Ethical clearance was obtained from the Institutional Research Ethical Review Board (IRB) with reference number (IRB/1108/21), College of Medicine and Health Sciences, Arba Minch University. Permission letters from each hospital's chief executive officer were obtained before data collection began. At the beginning of data collection, informed written consent was obtained from each study participant after the explanation of the purpose and procedures of the study. Any information obtained from respondents would be kept confidential and anonymous. To maintain confidentiality, respondents' names were replaced with code numbers. During data collection, the possible COVID-19 prevention measures were implemented. All necessary methods were carried out in accordance with the guidelines of institutional and declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
All authors assert that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
English version information sheet. Amharic version information sheet and consent form.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Abebe, M., Mersha, A., Degefa, N. et al. Determinants of induced abortion among women received maternal health care services in public hospitals of Arba Minch and Wolayita Sodo town, southern Ethiopia: unmatched case–control study. BMC Women's Health 22 , 107 (2022). https://doi.org/10.1186/s12905-022-01695-0
Download citation
Received : 02 December 2021
Accepted : 29 March 2022
Published : 09 April 2022
DOI : https://doi.org/10.1186/s12905-022-01695-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Induced abortion
- Determinant
- Maternal health care service
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Where Harris stands on Israel, abortion, climate change, education and the economy
[Editor's note: An earlier version of this story misstated Harris' proposed 2019 climate plan investment levels. The correct estimate is nearly seven times more than Biden's current proposal.]
Vice President Kamala Harris has emerged as the Democratic party’s presidential frontrunner after Joe Biden dropped his reelection bid Sunday.
Most Democrats have backed Harris, who announced her 2024 campaign for president shortly after Biden penned a letter explaining his decision to exit the 2024 race. Depending on who you ask, Harris is viewed as a moderate or a progressive reformer.
A former prosecutor, Harris was elected San Francisco’s district attorney with a “tough on crime” message in 2003 and worked in that role for seven years. She became the state’s attorney general in 2011 and served until 2017, when she was elected to represent California in the U.S. Senate.
Text with USA TODAY: Sign-up now and get answers to all your election questions.
More: Election 2024 live updates: Endorsements rush in for Harris; Trump attacks begin
Harris launched her own unsuccessful presidential campaign at a rally in her hometown of Oakland, California in 2019. She dropped her bid for the White House and joined President Joe Biden’s ticket in August the following year. In 2021, she was sworn in as vice president.
Decades in the public spotlight and on the public record, here is what we know about where Harris stands on key issues:
Foreign Policy
As Biden’s second-in-command, Harris has largely stood behind his foreign policy positions, but there are signs she could be tougher on Israel over the war in Gaza than the president.
Harris has not given reason to believe she will deviate much from Biden on issues relating to China , for example. She is also unlikely to sway from supporting Ukraine. Harris said earlier this year that Russia has committed “crimes against humanity” in Ukraine over the last two years.
Harris has not directly opposed Biden’s staunch support for Israel, but has expressed sympathy for the more than 38,000 Palestinian lives lost during the conflict. She was one of the first high-profile members of his administration to call for an immediate temporary cease-fire in March. She acknowledged the “immense scale of suffering” in Gaza and said the Israel-Hamas war is a “humanitarian catastrophe” for innocent civilians.
Harris’ support for women’s access to abortions has been a focal point of her tenure as the country’s first female vice president. She embarked on a nationwide Reproductive Freedoms Tour earlier this year to draw attention to attacks on abortion access following the Dobbs decision . She attended her first stop in Wisconsin on Jan. 22, the 51st anniversary of Roe v. Wade .
Harris proposed federal protections that would limit state abortion restrictions during her first presidential campaign. Under her proposal, states would need to clear laws regulating abortion with the Department of Justice, which would need to confirm they are constitutional before taking effect, she explained in 2019 .
“How dare these elected leaders believe they are in a better position to tell women what they need, to tell women what is in their best interest?” Harris asked during a visit to a Minnesota Planned Parenthood clinic in March. “We have to be a nation that trusts women.”
Harris has traveled on an Economic Opportunity Tour this summer to defend the Biden administration’s economic policy and attack former President Donald Trump’s economic agenda.
While on tour, she touted legislation passed during Biden’s time in office, including the American Rescue Plan and Inflation Reduction Act . Harris has tried to emphasize that wage increases have outpaced inflation since the pandemic and made the case that Trump has plans to give more tax cuts to the rich.
“Donald Trump gave tax cuts to billionaires,” she said in a June social media post . “President Joe Biden and I are investing in the middle class and making sure billionaires and big corporations pay their fair share.”
The vice president has made clear that climate change is a key issue a Harris administration would seek to address.
While running for president in 2019, she proposed a climate plan with a $10 trillion price tag — nearly seven times more than the $1.6 trillion Biden has invested in addressing the issue. She also called for a ban on fracking.
As a senator, she co-sponsored the Green New Deal , which called for a dramatic increase in the production of renewable fuels, including wind, solar, and hydropower sources. The 10-year mobilization plan pushed for a transition to energy systems less reliant on generating greenhouse gases, which are the primary contributors to climate change.
Harris has been an advocate inside the Biden administration pushing for the president to forgive student loan debt , which became a staple of his domestic policy agenda.
As a senator, she co-sponsored Vermont Sen. Bernie Sanders’ legislation to make two-year college free for all students and waive tuition for middle-class students attending four-year public universities.
At a Pride Month event last year, she criticized Florida’s 2022 “Don’t Say Gay” law banning educators from discussing sexual orientation and gender identity in elementary and middle school classrooms. Shortly after she announced her presidential campaign Sunday, the American Federation of Teachers endorsed Harris.
Rachel Barber is a 2024 election fellow at USA TODAY, focusing on politics and education. Follow her on X, formerly Twitter, at @rachelbarber_
- Work & Careers
- Life & Arts
US Elections 2024
Where kamala harris stands on five crucial issues, continue reading and get the indispensable us election countdown newsletter for free..
Want a deeper look?

.css-tw73a9{height:2px;min-width:50px;background-image:repeating-linear-gradient( to right, black, black 2px, transparent 2px, transparent 4px );}.css-tw73a9+.css-tw73a9{margin-top:2px;}@media (min-width: 740px){.css-tw73a9{margin:0;}} We've got you covered

US Election Countdown newsletter

US Presidential Election 2024 hub

Democracy 2024

Expert Opinion & Analysis
Explore more offers., standard digital.
- FT Digital Edition
Premium Digital
Print + premium digital, ft professional, weekend print + standard digital, weekend print + premium digital.
The new FT Digital Edition: today’s FT, cover to cover on any device. This subscription does not include access to ft.com or the FT App.
- Global news & analysis
- Expert opinion
- Special features
- Exclusive FT analysis
- FT App on Android & iOS
- FT Edit app
- FirstFT: the day's biggest stories
- 20+ curated newsletters
- Follow topics & set alerts with myFT
- FT Videos & Podcasts
- 20 monthly gift articles to share
- Lex: FT's flagship investment column
- 15+ Premium newsletters by leading experts
- FT Digital Edition: our digitised print edition
- Weekday Print Edition
- FirstFT newsletter
- Videos & Podcasts
- 10 gift articles per month
- Premium newsletters
- 10 additional gift articles per month
- FT Weekend Print delivery
- Everything in Standard Digital
- Everything in Premium Digital
Essential digital access to quality FT journalism on any device. Pay a year upfront and save 20%.
- 10 monthly gift articles to share
- Everything in Print
- Make and share highlights
- FT Workspace
- Markets data widget
- Subscription Manager
- Workflow integrations
- Occasional readers go free
- Volume discount
Complete digital access to quality FT journalism with expert analysis from industry leaders. Pay a year upfront and save 20%.
Terms & Conditions apply
Explore our full range of subscriptions.
Why the ft.
See why over a million readers pay to read the Financial Times.
- Introduction
- Conclusions
- Article Information
GI indicates gastrointestinal.
Whiskers indicate 95% CIs. GI indicates gastrointestinal.
eTable 1. Categorization of Cancers Within SEER*Stat (Version 8.4.0.1)
eTable 2. Baseline Characteristics of Early-Onset Cancers From 2010 to 2019 a
eTable 3. Incidence of Early-Onset Gastrointestinal Cancers From 2010 and 2019
eTable 4A. Incidence of Early-Onset Gastrointestinal Cancer From 2010 and 2019, Stratified by Sex
eTable 4B. Incidence of Early-Onset Gastrointestinal Cancer From 2010 and 2019, Stratified by Age Group
eTable 4C. Incidence of Early-Onset Gastrointestinal Cancer From 2010 and 2019, Stratified by Race
eTable 5. Incidence of Early-Onset Obesity-Related Cancer From 2010 and 2019
eFigure 1. Incident Early-Onset Cancers From 2010 and 2019
eFigure 2. Age-Standardized Incidence Rate of Early-Onset Cancers From 2010 to 2019, by Race and Ethnicity, Sex, and Age Group
eFigure 3. Annual Percentage Change of Cancers From 2010 to 2019, by Organ System
eFigure 4. Annual Percentage Change of Gastrointestinal Cancers From 2010 to 2019
eFigure 5. Annual Percentage Change of Obesity-Related Cancers, by Age Group
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Koh B , Tan DJH , Ng CH, et al. Patterns in Cancer Incidence Among People Younger Than 50 Years in the US, 2010 to 2019. JAMA Netw Open. 2023;6(8):e2328171. doi:10.1001/jamanetworkopen.2023.28171
Manage citations:
© 2024
- Permissions
Patterns in Cancer Incidence Among People Younger Than 50 Years in the US, 2010 to 2019
- 1 Yong Loo Lin School of Medicine, National University of Singapore, Singapore
- 2 Division of Gastroenterology and Hepatology, Department of Medicine, National University Hospital, Singapore
- 3 National University Centre for Organ Transplantation, National University Health System, Singapore
- 4 Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, University Surgical Cluster, National University Hospital, Singapore
- 5 Cancer Science Institute of Singapore, National University of Singapore, Singapore
- 6 Department of Medicine, Division of Gastroenterology and Hepatology, University of Arizona College of Medicine, Phoenix
- 7 AW Morrow Gastroenterology and Liver Centre, Royal Prince Alfred Hospital, Sydney, Australia
- 8 Ark Surgical Practice, Mount Elizabeth Hospital, Singapore, Singapore
- 9 Division of Cancer Control and Population Sciences, UPMC Hillman Cancer Center, Pittsburgh, Pennsylvania
- 10 Department of Epidemiology, School of Public Health, University of Pittsburgh, Pittsburgh, Pennsylvania
- 11 Department of Gastroenterology, Hepatology and Endocrinology, Hannover Medical School, Hannover, Germany
- 12 Division of Gastroenterology, University of California at San Diego, La Jolla
Question What are the patterns in the incidence of cancers in people younger than 50 years (ie, early-onset cancers)?
Findings In this cohort study of 562 145 people with early-onset cancer in the US from 2010 to 2019, the incidence rates of early-onset cancers increased substantially over the study period. Gastrointestinal cancers had the fastest-growing incidence rates among all early-onset cancers.
Meaning These data may be useful for the development of surveillance strategies and funding priorities.
Importance Emerging data suggest that the incidence of early-onset cancers, defined as cancers diagnosed in people younger than 50 years, is increasing, but updated data are limited.
Objective To characterize the patterns in the incidence of early-onset cancers in the US from 2010 to 2019 and provide granular data on the cancers with the fastest-growing incidence rates.
Design, Setting, and Participants This population-based cohort study analyzed data from 17 National Cancer Institute Surveillance, Epidemiology, and End Results registries from January 1, 2010, to December 31, 2019. Age-standardized incidence rates per 100 000 people were extracted for early-onset cancers, with rates age adjusted to the US standard population. A total of 562 145 patients with early-onset cancer between 2010 and 2019 were identified and included. Data were analyzed from October 16, 2022, to May 23, 2023.
Main Outcomes and Measures Primary outcomes were incidence rates and descriptive epidemiological data for people younger than 50 years with cancer. The annual percentage change (APC) of the age-standardized incidence rate was estimated using the Joinpoint regression program.
Results Among 562 145 patients (324 138 [57.7%] aged 40-49 years; 351 120 [62.5%] female) with early-onset cancer, 4565 (0.8%) were American Indian or Alaska Native, 54 876 (9.8%) were Asian or Pacific Islander, 61 048 (10.9%) were Black, 118 099 (21.0%) were Hispanic, 314 610 (56.0%) were White, and 8947 (1.6%) were of unknown race and/or ethnicity. From 2010 to 2019, the age-standardized incidence rate of early-onset cancers increased overall (APC, 0.28%; 95% CI, 0.09%-0.47%; P = .01) and in female individuals (APC, 0.67%; 95% CI, 0.39%-0.94%; P = .001) but decreased in male individuals (APC, −0.37%; 95% CI, −0.51% to −0.22%; P < .001). In contrast, the age-standardized incidence rate of cancers in individuals aged 50 years and older decreased over the study period (APC, −0.87%; 95% CI, −1.06% to −0.67%; P < .001). In 2019, the highest number of incident cases of early-onset cancer were in the breast (n = 12 649). From 2010 to 2019, gastrointestinal cancers had the fastest-growing incidence rates among all early-onset cancer groups (APC, 2.16%; 95% CI, 1.66%-2.67%; P < .001). Among gastrointestinal cancers, those with the fastest-growing incidence rates were in the appendix (APC, 15.61%; 95% CI, 9.21%-22.38%; P < .001), intrahepatic bile duct (APC, 8.12%; 95% CI, 4.94%-11.39%; P < .001), and pancreas (APC, 2.53%; 95% CI, 1.69%-3.38%; P < .001).
Conclusions and Relevance In this cohort study, the incidence rates of early-onset cancer increased from 2010 to 2019. Although breast cancer had the highest number of incident cases, gastrointestinal cancers had the fastest-growing incidence rates among all early-onset cancers. These data may be useful for the development of surveillance strategies and funding priorities.
Cancer has traditionally been considered a disease of older individuals (defined as adults 50 years and older), 1 but recent data suggest a marked increase in the incidence of cancer of various organs among patients younger than 50 years, collectively known as early-onset cancer. 2 , 3 These cancers affect a variety of organ systems, including the breast, colon and/or rectum, pancreas, head and neck, kidney, and reproductive organs. 2 , 4 - 8 The increase in early-onset cancers is likely associated with the increasing incidence of obesity as well as changes in environmental exposures, such as smoke and gasoline, 9 sleep patterns, physical activity, microbiota, and transient exposure to carcinogenic compounds. 10 - 14
Early-onset cancer is associated with substantial mortality and morbidity. 10 , 15 - 18 Recent efforts have evaluated the incidence patterns of specific types of early-onset cancers. 19 - 23 However, an updated comprehensive overview of recent patterns of early-onset cancer in the US that is not limited to specific organ systems has not been reported. 24 This study used population-based data from the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER) program to characterize temporal patterns in the incidence of early-onset cancers in the US from 2010 to 2019. The primary objective was to characterize the temporal patterns in early-onset cancer overall and by organ system. The secondary objective was to assess temporal patterns in early-onset cancer stratified by sex, age group, and race and ethnicity.
This cohort study was conducted in accordance with the Declaration of Helsinki. 25 The study was exempt from institutional review board review because no confidential patient information was involved per the 2018 Revised Common Rule (45 CFR §46). 26 This study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline for cohort studies.
The National Cancer Institute SEER program collects population-based data on cancer incidence in the US. The SEER database is a network of tumor registries from various geographically distinct regions within the country and contains representative data for the racial and ethnic diversity present within the US. 27 The data in the SEER registry are sourced annually from the US Census Bureau, and the registry is estimated to cover approximately 26.5% of the population in the US. 28 In this study, data from 17 SEER registries (hereinafter, SEER 17 database) were used to estimate the number of incident cancer cases from January 1, 2010, to December 31, 2019, as well as the cross-sectional incidence rates and the 10-year mean annual percentage change (APC) in incidence rates. Race and ethnicity categories were determined per the SEER coding manual, which was predominantly based on self-reported data. Data were analyzed from October 16, 2022, to May 23, 2023.
Demographic data were obtained using SEER*Stat software, version 8.4.0.1 (National Cancer Institute), 29 from incident cases of cancer diagnosed between 2010 and 2019 and collected from the SEER 17 database. Population data were segregated based on age, race and ethnicity, and sex available within SEER*Stat. Incidence rates were calculated using SEER*Stat and were age standardized to the 2000 US standard population. 30 Tiwari et al 31 modification was applied for more efficient calculation of CIs for rates and rate ratios. All cases of cancer were classified according to the World Health Organization 2008 definitions, which were based on the International Classification of Diseases for Oncology , third edition. 32 Cancers were grouped according to organ systems (eTable 1 in Supplement 1 ). The APC of incidence rates was quantified using the Joinpoint regression program, version 5.0.2 (National Cancer Institute). 33 Temporal patterns from 2010 to 2019 were evaluated to identify changes that may have occurred over the study period. Rates and APCs across the strata of sex (male or female), race and ethnicity (Hispanic, non-Hispanic American Indian or Alaska Native, non-Hispanic Asian or Pacific Islander, non-Hispanic Black, non-Hispanic White, or unknown race and/or ethnicity), and age group (0-19 years, 20-29 years, 30-39 years, or 40-49 years) were evaluated to identify populations at risk of developing cancer. Analysis of American Indian or Alaska Native populations was restricted to areas with health care services provided by the Indian Health Services for improved accuracy of racial classification. 34 As a result, 960 persons from outside of purchased or referred care delivery areas were excluded from the analysis. The Monte Carlo permutation method was used to test for significance, 33 and 2-sided P < .05 was considered statistically significant.
Between 2010 and 2019, a total of 562 145 patients with early-onset cancer (324 138 [57.7%] aged 40-49 years; 351 120 [62.5%] female and 211 025 [37.5%] male) were identified over 2 102 085 738 person-years of observation. A total of 4565 patients (0.8%) were American Indian or Alaska Native, 54 876 (9.8%) were Asian or Pacific Islander, 61 048 (10.9%) were Black, 118 099 (21.0%) were Hispanic, 314 610 (56.0%) were White, and 8947 (1.6%) were of unknown race and/or ethnicity (eTable 2 in Supplement 1 ).
The number of incident early-onset cancers was 56 051 in 2010 and 56 468 in 2019, representing an increase of 0.74% during the study period. The number of incident early-onset cancers in male individuals was 21 818 in 2010 and 20 747 in 2019, representing a decrease of 4.91%; the number of incident early-onset cancers in female individuals was 34 233 in 2010 and 35 721 in 2019, representing an increase of 4.35% ( Figure 1 A). By race and ethnicity, the number of incident early-onset cancers in 2010 was 351 among American Indian or Alaska Native people, 4723 among Asian or Pacific Islander people, 6245 among Black people, 10 326 among Hispanic people, and 33 578 among White people; the number of incident early-onset cancers in 2019 was 359 among American Indian or Alaska Native people, 6246 among Asian or Pacific Islander people, 5953 among Black people, 13 177 among Hispanic people, and 29 481 among White people ( Figure 1 B). These values represented an increase of 2.28% among American Indian or Alaska Native people, 32.25% among Asian or Pacific Islander people, and 27.61% among Hispanic people but a decrease of 4.68% among Black people and 12.20% among White people. When stratified by specific age groups, the number of incident early-onset cancers in 2019 was 3983 among individuals aged 0 to 19 years, 5899 among individuals aged 20 to 29 years, 14 762 among individuals aged 30 to 39 years, and 31 824 among individuals aged 40 to 49 years.
The incidence rate of early-onset cancer was 99.96 cases per 100 000 individuals in 2010 and 102.97 cases per 100 000 individuals in 2019. The overall incidence of early-onset cancer increased (APC, 0.28%; 95% CI, 0.09%-0.47%; P = .01) ( Figure 2 A; Table 1 ). In contrast, the incidence of cancer among individuals 50 years and older decreased over the same period (APC, −0.87%; 95% CI, −1.06% to −0.67%; P < .001). During the study period, the age-standardized incidence rates of early-onset cancer increased in female individuals (APC, 0.67%; 95% CI, 0.39%-0.94%; P = .001) but decreased in male individuals (APC, −0.37%; 95% CI, −0.51% to −0.22%; P < .001) (eFigure 2 in Supplement 1 ). The mean APCs increased in American Indian or Alaska Native people (1.97%; 95% CI, 0.69%-3.27%; P < .001), Asian or Pacific Islander people (0.97%; 95% CI, 0.58%-1.35%; P = .007), and Hispanic people (1.43%; 95% CI, 1.05%-1.81%; P < .001); were stable in White people (0.04%; 95% CI, −0.24% to 0.31%; P = .77); and decreased in Black people (−0.47%; 95% CI, −0.77% to −0.17%; P = .007). By age group, the incidence of early-onset cancers increased in individuals aged 30-39 years (APC, 0.91%; 95% CI, 0.44%-1.39%; P = .002) but remained stable in other age groups. The incident rates among populations 50 years and older decreased, with mean APCs of −0.48% (95% CI, −0.69% to −0.26%; P = .001) among those aged 50 to 59 years, −0.75% (95% CI, −1.15% to −0.35%; P = .003) among those aged 60 to 69 years, −1.01% (95% CI, −1.28% to −0.74%; P < .001) among those aged 70 to 79 years, and −1.16% (95% CI, −1.29% to −1.03%; P < .001) among those 80 years and older ( Figure 2 B).
The incidence rates and APCs of the individual cancers are summarized in Table 2 . In 2019, the individual cancers with the highest number of incident early-onset cases were cancers of the breast (n = 12 649), thyroid (n = 5869), and colon and/or rectum (n = 4097). From 2010 to 2019, the cancers with the greatest increase in incident cases were in the appendix (251.89%), intrahepatic bile duct (142.22%), and uterus (76.47%). During the study period, the greatest increase in incidence rates occurred in cancers of the appendix (APC, 15.61%; 95% CI, 9.21%-22.38%; P < .001), intrahepatic bile duct (APC, 8.12%; 95% CI, 4.94%-11.39%; P < .001), and other digestive organs (APC, 6.63%; 95% CI, 1.58%-11.93%; P = .02). The greatest decrease in incidence rates of individual early-onset cancers occurred for cancer in the floor of the mouth (APC, −7.58%; 95% CI, −9.59% to −5.52%; P < .001), acute monocytic leukemia (APC, −6.51%; 95% CI, −8.86% to −4.11%; P < .001), and prostate cancer (APC, −6.12%; 95% CI, −8.16% to −4.04%; P < .001).
The number of incident cases of early-onset cancer in 2010 and 2019 by organ system is shown in Figure 1 C and Table 3 . In 2019, the highest number of incident cases of early-onset cancer were in cancers of the breast (n = 12 649), gastrointestinal system (n = 7383), and hematological system (n = 6960). From 2010 to 2019, the greatest increases in the number of incident cases of early-onset cancer occurred in the gastrointestinal system (14.80%; from 6431 cases to 7383 cases), breast (7.70%; from 11 745 cases to 12 649 cases), and endocrine system (8.69%; from 5659 cases to 6151 cases). The mean APCs of early-onset cancer from 2010 to 2019 by organ system are shown in Figure 2 C and Table 3 . From 2010 to 2019, the greatest increases in incidence rates of early-onset cancers occurred in cancers of the gastrointestinal system (APC, 2.16%; 95% CI, 1.66%-2.67%; P < .001), urinary system (APC, 1.34%; 95% CI, 0.61%-2.07%; P = .003), and female reproductive system (APC, 0.93%; 95% CI, 0.32%-1.55%; P = .008) (eFigure 3 in Supplement 1 ). In contrast, the greatest decreases in incidence rates of early-onset cancers occurred in cancers of the respiratory system (APC, −4.57%; 95% CI, −5.30% to −3.83%; P < .001), male reproductive system (APC, −1.75%; 95% CI, −2.40% to −1.10%; P < .001), and brain and nervous system (APC, −0.99%; 95% CI, −1.67% to −0.32%; P = .01).
Because gastrointestinal cancers had the fastest-growing incidence rates among the organ systems, we further explored the incidence patterns among individual gastrointestinal cancers to identify the specific organs contributing to this pattern. The number of incident cases of early-onset gastrointestinal cancers in 2010 and 2019, by individual organ sites, are shown in eFigure 1 in Supplement 1 , and the incidence rates and patterns of early-onset gastrointestinal cancers are shown in eTable 3 in Supplement 1 . In 2019, the highest number of incident cases of early-onset gastrointestinal cancers occurred in the colon and/or rectum (n = 4097), stomach (n = 773), and pancreas (n = 701). From 2010 to 2019, the greatest increases in the number of incident cases of early-onset cancer were in the appendix (251.89%; from 185 cases to 651 cases), intrahepatic bile duct (142.22%; from 45 cases to 109 cases), and pancreas (18.21%; from 593 cases to 701 cases). The greatest increase in the incidence rates of early-onset gastrointestinal cancers was in the appendix (APC, 15.61%; 95% CI, 9.21%-22.38%; P < .001), intrahepatic bile duct (APC, 8.12%; 95% CI, 4.94%-11.39%; P < .001), and pancreas (APC, 2.53%; 95% CI, 1.69%-3.38%; P < .001) (eTable 3 in Supplement 1 ). In contrast, the incidence rates of cancers of the liver and esophagus decreased, with APCs of −4.67% (95% CI, −5.70% to −3.63%; P < .001) for liver cancer and −0.94% (95% CI, −2.56% to 0.71%; P = .22) for esophageal cancer.
The number of incident cases and the incidence rates of early-onset gastrointestinal cancers by sex, age group, and race and ethnicity are shown in eTable 4A to 4C in Supplement 1 . Among both male and female individuals, the incidence rates of cancers of the appendix and intrahepatic bile duct increased significantly from 2010 to 2019, while the incidence rates of stomach cancers increased only in female individuals, and the incidence rates of gallbladder cancers increased only in male individuals.
By age, the greatest increase in incidence rates of early-onset gastrointestinal cancers occurred in those aged 30 to 39 years, with significant increases in cancers of the esophagus (APC, 6.86%; 95% CI, 1.77%-12.21%; P = .01), small intestine (APC, 4.24%; 95% CI, 1.75%-6.78%; P = .004), appendix (APC, 16.20%; 95% CI, 9.81%-22.96%; P < .001), pancreas (APC, 4.47%; 95% CI, 1.23%-7.80%; P = .01), and intrahepatic bile duct (APC, 8.88%; 95% CI, 2.56%-15.59%; P = .01) (eTable 4B and eFigure 4 in Supplement 1 ).
By race and ethnicity, Hispanic people experienced the greatest increase in incidence rates of gastrointestinal cancers (APC, 3.08%; 95% CI, 2.09%-4.08%; P < .001) followed by American Indian or Alaska Native people (APC, 2.83%; 95% CI, 0.51%-5.19%; P = .02) and White people (APC, 2.45%; 95% CI, 1.75%-3.15%; P < .001) (eTable 4C in Supplement 1 ). There were no significant increases in early-onset gastrointestinal cancers by specific sites among American Indian or Alaska Native people. Asian or Pacific Islander people experienced significant increases in the incidence of early-onset appendiceal cancers. Hispanic people had significant increases in stomach, appendiceal, colorectal, pancreatic, and intrahepatic bile duct cancers. Among Black people, the incidence of appendiceal and biliary cancer significantly increased. White people experienced significant increases in the incidence of appendiceal and intrahepatic bile duct cancers.
We next evaluated patterns in the APCs of early-onset cancer among 12 cancers identified as related to obesity by the Centers for Disease Control and Prevention 35 - 37 to assess the association between increasing obesity rates and the incidence of early-onset cancer (eFigure 5 and eTable 5 in Supplement 1 ). From 2010 to 2019, the APC of obesity-related early-onset cancer was 1.00% (95% CI, 0.69%-1.31%; P < .001). The fastest-growing incidence rates of obesity-related cancers were in the pancreas (APC, 2.53%; 95% CI, 1.69%-3.38%; P < .001), gallbladder (APC, 2.36%; 95% CI, −1.60% to 6.48%; P = .21), and uterus (APC, 2.22%; 95% CI, 1.59%-2.85%; P < .001). Conversely, the fastest-decreasing incidence rates among obesity-related cancers were in the liver (APC, 4.67%; 95% CI, −5.70% to −3.63%; P < .001), ovary (APC, −1.03%; 95% CI, −2.15% to 0.10%; P = .07), and esophagus (APC, −0.94%; 95% CI, −2.56% to 0.71%; P = .22).
In this nationwide cohort study, we found that in 2019, a total of 56 468 early-onset cancers were diagnosed in the US. The overall incidence rate of early-onset cancers increased from 2010 to 2019, while the incidence rate of cancers declined among individuals 50 years and older. During the study period, the incidence rates of early-onset cancers increased in female individuals but declined in male individuals; this increase among female individuals was mainly due to cancers of the uterus and breast. By race and ethnicity, there was an increased incidence of early-onset cancer in American Indian or Alaska Native people, Asian or Pacific Islander people, and Hispanic people. However, the incidence of early-onset cancers remained stable among White people and declined among Black people. By age group, the incidence rate of early-onset cancers increased in individuals aged 30 to 39 years and remained stable in other age groups younger than 50 years.
In 2019, breast cancer had the highest number of incident early-onset cases. By organ system, gastrointestinal cancers had the fastest-growing incidence rates of early-onset cancer, followed by cancers of the urinary system and the female reproductive system. Among gastrointestinal cancers in 2019, the most common types of incident early-onset cancers were in the colon and/or rectum, stomach, and pancreas. During the study period, the gastrointestinal early-onset cancers with the fastest-growing incidence rates were in the appendix, intrahepatic bile duct, and pancreas.
These findings built upon previous US studies that provided data on patterns of early-onset cancer until 2014 24 and 2015. 27 These data are also consistent with a recent Global Burden of Disease Study, 3 which estimated that the highest age-standardized incident rates of early-onset cancer occurred in countries with a high sociodemographic index, such as those in North America. The current study expands on these data by providing granular updated patterns through 2019 by organ system, sex, and race and ethnicity. Several studies 7 , 22 , 38 - 46 have described an increase in specific early-onset cancers, such as those of the colon and/or rectum, breast, kidney, stomach, uterus, endometrium, and pancreas. However, there are limited data that provide a comprehensive updated overview of the latest patterns in early-onset cancer in the US, both overall and by organ system, and the current study fills this knowledge gap.
This nationwide study provides updated evidence that the incidence of early-onset cancers in the US is increasing and highlights several disparities. The increase in early-onset cancer disproportionately occurred among female individuals, American Indian or Alaska Native individuals, Asian or Pacific Islander individuals, and individuals aged 30 to 39 years. Further research is required to fully elucidate the reasons for these disparities. There is a need to inform health care professionals about the increasing incidence of early-onset cancer, and investigations for possible tumors need to be considered when clinically appropriate, even in patients younger than 50 years. These data will be useful for public health specialists and health care policy makers and serve as a call to action for further research into the various environmental factors that may be associated with this concerning pattern.
This study has strengths, including a large sample, data updated through 2019, and detailed subgroup analyses by organ system and individual cancer sites.
The study also has limitations. The generalizability of these findings to populations outside of the US may be unclear. There may have been misclassification, or there could have been underreporting or underdiagnosis among underserved populations, such as Black individuals; hence, these results require cautious interpretation. We recognize that although the Centers for Disease Control and Prevention included ovarian cancer in the group of cancers related to obesity, data regarding the association of body mass index with ovarian cancer are conflicting, with an individual participant data meta-analysis only finding an association between body mass index and ovarian cancer among people who had never used hormonal therapy. 34 , 47
This nationwide cohort study found that the incidence of early-onset cancers continued to increase in the US from 2010 to 2019. While breast cancer had the highest number of incident cases, gastrointestinal cancers had the fastest-growing incidence rates among all early-onset cancers. These data may have implications for the development of surveillance strategies and funding priorities.
Accepted for Publication: June 26, 2023.
Published: August 16, 2023. doi:10.1001/jamanetworkopen.2023.28171
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Koh B et al. JAMA Network Open .
Corresponding Authors: Daniel Q. Huang, MBBS, MMED, Department of Medicine, Yong Loo Lin School of Medicine, National University of Singapore, National University Health System, 1E Kent Ridge Rd, Singapore 119228, Singapore ( [email protected] ); Cheng Han Ng, MBBS, Yong Loo Lin School of Medicine, National University of Singapore, Singapore 10 Medical Dr, Singapore 117597, Singapore ( [email protected] ).
Author Contributions: Mr Koh and Dr Huang had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: B. Koh, Ng, Lim, J. Koh, Syn, Wijarnpreecha, Chong, Muthiah, Yeoh, Loomba, Huang.
Acquisition, analysis, or interpretation of data: B. Koh, Tan, Ng, Fu, Zeng, Yong, Meng, Liu, Luu, Vogel, Singh, Huang.
Drafting of the manuscript: B. Koh, Ng, Fu, Lim, Zeng, J. Koh, Loomba, Huang.
Critical review of the manuscript for important intellectual content: B. Koh, Tan, Ng, Yong, Syn, Meng, Wijarnpreecha, Liu, Chong, Muthiah, Luu, Vogel, Singh, Yeoh, Loomba, Huang.
Statistical analysis: B. Koh, Tan, Ng, Fu, Yong, J. Koh, Luu, Huang.
Obtained funding: Ng, Huang.
Administrative, technical, or material support: Tan, Lim, Zeng, Yong, J. Koh, Muthiah, Huang.
Supervision: Syn, Wijarnpreecha, Liu, Chong, Muthiah, Loomba, Huang.
Conflict of Interest Disclosures: Mr Ng reported receiving personal fees from Boxer Capital outside the submitted work. Dr Muthiah reported receiving grants from the National Medical Research Council (Singapore) during the conduct of the study. Dr Vogel reported receiving personal fees from AstraZeneca, BeiGene, Boehringer Mannheim, Bristol Myers Squibb, Eisai Co, Incyte, MSD, Pierre Fabre, and Roche outside the submitted work. Dr Singh reported receiving grants from AbbVie and Pfizer and personal fees from Pfizer outside the submitted work. Dr Yeoh reported serving as a member of the MiRXES Scientific Advisory Board outside the submitted work. Dr Loomba reported receiving grants from Arrowhead Pharmaceuticals, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Eli Lilly and Company, Galectin Therapeutics, Galmed Pharmaceuticals, Gilead Sciences, Hanmi Pharmaceutical Co, Intercept Pharmaceuticals, Inventiva, Ionis Pharmaceuticals, Janssen Pharmaceuticals, Madrigal Pharmaceuticals, Merck & Co, NGM Biopharmaceuticals, Novo Nordisk, Pfizer, Sonic Incytes, and Terns Pharmaceuticals and serving as a consultant for 89bio, Aardvark Therapeutics, Altimmune, Alnylam/Regeneron, Amgen, Arrowhead Pharmaceuticals, AstraZeneca, Bristol Myers Squibb, CohBar, Eli Lilly and Company, Galmed Pharmaceuticals, Gilead Sciences, Glympse Bio, Hightide Therapeutics, Inipharm, Intercept Pharmaceuticals, Inventiva, Ionis Pharmaceuticals, Janssen Pharmaceuticals, Madrigal Pharmaceuticals, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Merck & Co, Pfizer, Sagimet Biosciences, Theratechnologies, Terns Pharmaceuticals, and Viking Therapeutics during the conduct of the study; owning stock options in 89bio and Sagimet Biosciences and being a cofounder of LipoNexus outside the submitted work. Dr Huang reported receiving personal fees from Gilead Sciences outside the submitted work. No other disclosures were reported.
Funding/Support: This study was supported by grants 5UL1TR001442 from the National Center for Advancing Translational Sciences (Dr Loomba); U01DK061734, U01DK130190, R01DK106419, R01DK121378, R01DK124318, and P30DK120515 from the National Institute of Diabetes and Digestive and Kidney Diseases (Dr Loomba); and MOH-000595-01 from the National Medical Research Council of the Singapore Ministry of Health under its NMRC Research Training Fellowship (Dr Huang).
Role of the Funder/Sponsor: The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Rom J Morphol Embryol
- v.61(1); Jan-Mar 2020

A research on abortion: ethics, legislation and socio-medical outcomes. Case study: Romania
Andreea mihaela niţă.
1 Faculty of Social Sciences, University of Craiova, Romania
Cristina Ilie Goga
This article presents a research study on abortion from a theoretical and empirical point of view. The theoretical part is based on the method of social documents analysis, and presents a complex perspective on abortion, highlighting items of medical, ethical, moral, religious, social, economic and legal elements. The empirical part presents the results of a sociological survey, based on the opinion survey method through the application of the enquiry technique, conducted in Romania, on a sample of 1260 women. The purpose of the survey is to identify Romanians perception on the decision to voluntary interrupt pregnancy, and to determine the core reasons in carrying out an abortion.
The analysis of abortion by means of medical and social documents
Abortion means a pregnancy interruption “before the fetus is viable” [ 1 ] or “before the fetus is able to live independently in the extrauterine environment, usually before the 20 th week of pregnancy” [ 2 ]. “Clinical miscarriage is both a common and distressing complication of early pregnancy with many etiological factors like genetic factors, immune factors, infection factors but also psychological factors” [ 3 ]. Induced abortion is a practice found in all countries, but the decision to interrupt the pregnancy involves a multitude of aspects of medical, ethical, moral, religious, social, economic, and legal order.
In a more simplistic manner, Winston Nagan has classified opinions which have as central element “abortion”, in two major categories: the opinion that the priority element is represented by fetus and his entitlement to life and the second opinion, which focuses around women’s rights [ 4 ].
From the medical point of view, since ancient times there have been four moments, generally accepted, which determine the embryo’s life: ( i ) conception; ( ii ) period of formation; ( iii ) detection moment of fetal movement; ( iv ) time of birth [ 5 ]. Contemporary medicine found the following moments in the evolution of intrauterine fetal: “ 1 . At 18 days of pregnancy, the fetal heartbeat can be perceived and it starts running the circulatory system; 2 . At 5 weeks, they become more clear: the nose, cheeks and fingers of the fetus; 3 . At 6 weeks, they start to function: the nervous system, stomach, kidneys and liver of the fetus, and its skeleton is clearly distinguished; 4 . At 7 weeks (50 days), brain waves are felt. The fetus has all the internal and external organs definitively outlined. 5 . At 10 weeks (70 days), the unborn child has all the features clearly defined as a child after birth (9 months); 6 . At 12 weeks (92 days, 3 months), the fetus has all organs definitely shaped, managing to move, lacking only the breath” [ 6 ]. Even if most of the laws that allow abortion consider the period up to 12 weeks acceptable for such an intervention, according to the above-mentioned steps, there can be defined different moments, which can represent the beginning of life. Nowadays, “abortion is one of the most common gynecological experiences and perhaps the majority of women will undergo an abortion in their lifetimes” [ 7 ]. “Safe abortions carry few health risks, but « every year, close to 20 million women risk their lives and health by undergoing unsafe abortions » and 25% will face a complication with permanent consequences” [ 8 , 9 ].
From the ethical point of view, most of the times, the interruption of pregnancy is on the border between woman’s right over her own body and the child’s (fetus) entitlement to life. Judith Jarvis Thomson supported the supremacy of woman’s right over her own body as a premise of freedom, arguing that we cannot force a person to bear in her womb and give birth to an unwanted child, if for different circumstances, she does not want to do this [ 10 ]. To support his position, the author uses an imaginary experiment, that of a violinist to which we are connected for nine months, in order to save his life. However, Thomson debates the problem of the differentiation between the fetus and the human being, by carrying out a debate on the timing which makes this difference (period of conception, 10 weeks of pregnancy, etc.) and highlighting that for people who support abortion, the fetus is not an alive human being [ 10 ].
Carol Gilligan noted that women undergo a true “moral dilemma”, a “moral conflict” with regards to voluntary interruption of pregnancy, such a decision often takes into account the human relationships, the possibility of not hurting the others, the responsibility towards others [ 11 ]. Gilligan applied qualitative interviews to a number of 29 women from different social classes, which were put in a position to decide whether or not to commit abortion. The interview focused on the woman’s choice, on alternative options, on individuals and existing conflicts. The conclusion was that the central moral issue was the conflict between the self (the pregnant woman) and others who may be hurt as a result of the potential pregnancy [ 12 ].
From the religious point of view, abortion is unacceptable for all religions and a small number of abortions can be seen in deeply religious societies and families. Christianity considers the beginning of human life from conception, and abortion is considered to be a form of homicide [ 13 ]. For Christians, “at the same time, abortion is giving up their faith”, riot and murder, which means that by an abortion we attack Jesus Christ himself and God [ 14 ]. Islam does not approve abortion, relying on the sacral life belief as specified in Chapter 6, Verse 151 of the Koran: “Do not kill a soul which Allah has made sacred (inviolable)” [ 15 ]. Buddhism considers abortion as a negative act, but nevertheless supports for medical reasons [ 16 ]. Judaism disapproves abortion, Tanah considering it to be a mortal sin. Hinduism considers abortion as a crime and also the greatest sin [ 17 ].
From the socio-economic point of view, the decision to carry out an abortion is many times determined by the relations within the social, family or financial frame. Moreover, studies have been conducted, which have linked the legalization of abortions and the decrease of the crime rate: “legalized abortion may lead to reduced crime either through reductions in cohort sizes or through lower per capita offending rates for affected cohorts” [ 18 ].
Legal regulation on abortion establishes conditions of the abortion in every state. In Europe and America, only in the XVIIth century abortion was incriminated and was considered an insignificant misdemeanor or a felony, depending on when was happening. Due to the large number of illegal abortions and deaths, two centuries later, many states have changed legislation within the meaning of legalizing voluntary interruption of pregnancy [ 6 ]. In contemporary society, international organizations like the United Nations or the European Union consider sexual and reproductive rights as fundamental rights [ 19 , 20 ], and promotes the acceptance of abortion as part of those rights. However, not all states have developed permissive legislation in the field of voluntary interruption of pregnancy.
Currently, at national level were established four categories of legislation on pregnancy interruption area:
( i ) Prohibitive legislations , ones that do not allow abortion, most often outlining exceptions in abortion in cases where the pregnant woman’s life is endangered. In some countries, there is a prohibition of abortion in all circumstances, however, resorting to an abortion in the case of an imminent threat to the mother’s life. Same regulation is also found in some countries where abortion is allowed in cases like rape, incest, fetal problems, etc. In this category are 66 states, with 25.5% of world population [ 21 ].
( ii ) Restrictive legislation that allow abortion in cases of health preservation . Loosely, the term “health” should be interpreted according to the World Health Organization (WHO) definition as: “health is a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity” [ 22 ]. This type of legislation is adopted in 59 states populated by 13.8% of the world population [ 21 ].
( iii ) Legislation allowing abortion on a socio-economic motivation . This category includes items such as the woman’s age or ability to care for a child, fetal problems, cases of rape or incest, etc. In this category are 13 countries, where we have 21.3% of the world population [ 21 ].
( iv ) Legislation which do not impose restrictions on abortion . In the case of this legislation, abortion is permitted for any reason up to 12 weeks of pregnancy, with some exceptions (Romania – 14 weeks, Slovenia – 10 weeks, Sweden – 18 weeks), the interruption of pregnancy after this period has some restrictions. This type of legislation is adopted in 61 countries with 39.5% of the world population [21].
The Centre for Reproductive Rights has carried out from 1998 a map of the world’s states, based on the legislation typology of each country (Figure (Figure1 1 ).

The analysis of states according to the legislation regarding abortion. Source: Centre for Reproductive Rights. The World’s Abortion Laws, 2018 [ 23 ]
An unplanned pregnancy, socio-economic context or various medical problems [ 24 ], lead many times to the decision of interrupting pregnancy, regardless the legislative restrictions. In the study “Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008” issued in 2011 by the WHO , it was determined that within the states with restrictive legislation on abortion, we may also encounter a large number of illegal abortions. The illegal abortions may also be resulting in an increased risk of woman’s health and life considering that most of the times inappropriate techniques are being used, the hygienic conditions are precarious and the medical treatments are incorrectly administered [ 25 ]. Although abortions done according to medical guidelines carry very low risk of complications, 1–3 unsafe abortions contribute substantially to maternal morbidity and death worldwide [ 26 ].
WHO has estimated for the year 2008, the fact that worldwide women between the ages of 15 and 44 years carried out 21.6 million “unsafe” abortions, which involved a high degree of risk and were distributed as follows: 0.4 million in the developed regions and a number of 21.2 million in the states in course of development [ 25 ].
Case study: Romania
Legal perspective on abortion
In Romania, abortion was brought under regulation by the first Criminal Code of the United Principalities, from 1864.
The Criminal Code from 1864, provided the abortion infringement in Article 246, on which was regulated as follows: “Any person, who, using means such as food, drinks, pills or any other means, which will consciously help a pregnant woman to commit abortion, will be punished to a minimum reclusion (three years).
The woman who by herself shall use the means of abortion, or would accept to use means of abortion which were shown or given to her for this purpose, will be punished with imprisonment from six months to two years, if the result would be an abortion. In a situation where abortion was carried out on an illegitimate baby by his mother, the punishment will be imprisonment from six months to one year.
Doctors, surgeons, health officers, pharmacists (apothecary) and midwives who will indicate, will give or will facilitate these means, shall be punished with reclusion of at least four years, if the abortion took place. If abortion will cause the death of the mother, the punishment will be much austere of four years” (Art. 246) [ 27 ].
The Criminal Code from 1864, reissued in 1912, amended in part the Article 246 for the purposes of eliminating the abortion of an illegitimate baby case. Furthermore, it was no longer specified the minimum of four years of reclusion, in case of abortion carried out with the help of the medical staff, leaving the punishment to the discretion of the Court (Art. 246) [ 28 ].
The Criminal Code from 1936 regulated abortion in the Articles 482–485. Abortion was defined as an interruption of the normal course of pregnancy, being punished as follows:
“ 1 . When the crime is committed without the consent of the pregnant woman, the punishment was reformatory imprisonment from 2 to 5 years. If it caused the pregnant woman any health injury or a serious infirmity, the punishment was reformatory imprisonment from 3 to 6 years, and if it has caused her death, reformatory imprisonment from 7 to 10 years;
2 . When the crime was committed by the unmarried pregnant woman by herself, or when she agreed that someone else should provoke the abortion, the punishment is reformatory imprisonment from 3 to 6 months, and if the woman is married, the punishment is reformatory imprisonment from 6 months to one year. Same penalty applies also to the person who commits the crime with the woman’s consent. If abortion was committed for the purpose of obtaining a benefit, the punishment increases with another 2 years of reformatory imprisonment.
If it caused the pregnant woman any health injuries or a severe disablement, the punishment will be reformatory imprisonment from one to 3 years, and if it has caused her death, the punishment is reformatory imprisonment from 3 to 5 years” (Art. 482) [ 29 ].
The criminal legislation from 1936 specifies that it is not considered as an abortion the interruption from the normal course of pregnancy, if it was carried out by a doctor “when woman’s life was in imminent danger or when the pregnancy aggravates a woman’s disease, putting her life in danger, which could not be removed by other means and it is obvious that the intervention wasn’t performed with another purpose than that of saving the woman’s life” and “when one of the parents has reached a permanent alienation and it is certain that the child will bear serious mental flaws” (Art. 484, Par. 1 and Par. 2) [ 29 ].
In the event of an imminent danger, the doctor was obliged to notify prosecutor’s office in writing, within 48 hours after the intervention, on the performance of the abortion. “In the other cases, the doctor was able to intervene only with the authorization of the prosecutor’s office, given on the basis of a medical certificate from hospital or a notice given as a result of a consultation between the doctor who will intervene and at least a professor doctor in the disease which caused the intervention. General’s Office Prosecutor, in all cases provided by this Article, shall be obliged to maintain the confidentiality of all communications or authorizations, up to the intercession of any possible complaints” (Art. 484) [ 29 ].
The legislation of 1936 provided a reformatory injunction from one to three years for the abortions committed by doctors, sanitary agents, pharmacists, apothecary or midwives (Art. 485) [ 29 ].
Abortion on demand has been legalized for the first time in Romania in the year 1957 by the Decree No. 463, under the condition that it had to be carried out in a hospital and to be carried out in the first quarter of the pregnancy [ 30 ]. In the year 1966, demographic policy of Romania has dramatically changed by introducing the Decree No. 770 from September 29 th , which prohibited abortion. Thus, the voluntary interruption of pregnancy became a crime, with certain exceptions, namely: endangering the mother’s life, physical or mental serious disability; serious or heritable illness, mother’s age over 45 years, if the pregnancy was a result of rape or incest or if the woman gave birth to at least four children who were still in her care (Art. 2) [ 31 ].
In the Criminal Code from 1968, the abortion crime was governed by Articles 185–188.
The Article 185, “the illegal induced abortion”, stipulated that “the interruption of pregnancy by any means, outside the conditions permitted by law, with the consent of the pregnant woman will be punished with imprisonment from one to 3 years”. The act referred to above, without the prior consent from the pregnant woman, was punished with prison from two to five years. If the abortion carried out with the consent of the pregnant woman caused any serious body injury, the punishment was imprisonment from two to five years, and when it caused the death of the woman, the prison sentence was from five to 10 years. When abortion was carried out without the prior consent of the woman, if it caused her a serious physical injury, the punishment was imprisonment from three to six years, and if it caused the woman’s death, the punishment was imprisonment from seven to 12 years (Art. 185) [ 32 ].
“When abortion was carried out in order to obtain a material benefit, the maximum punishment was increased by two years, and if the abortion was made by a doctor, in addition to the prison punishment could also be applied the prohibition to no longer practice the profession of doctor”.
Article 186, “abortion caused by the woman”, stipulated that “the interruption of the pregnancy course, committed by the pregnant woman, was punished with imprisonment from 6 months to 2 years”, quoting the fact that by the same punishment was also sanctioned “the pregnant woman’s act to consent in interrupting the pregnancy course made out by another person” (Art. 186) [ 26 ].
The Regulations of the Criminal Code in 1968, also provided the crime of “ownership of tools or materials that can cause abortion”, the conditions of this holding being met when these types of instruments were held outside the hospital’s specialized institutions, the infringement shall be punished with imprisonment from three months to one year (Art. 187) [ 32 ].
Furthermore, the doctors who performed an abortion in the event of extreme urgency, without prior legal authorization and if they did not announce the competent authority within the legal deadline, they were punished by imprisonment from one month to three months (Art. 188) [ 32 ].
In the year 1985, it has been issued the Decree No. 411 of December 26 th , by which the conditions imposed by the Decree No. 770 of 1966 have been hardened, meaning that it has increased the number of children, that a woman could have in order to request an abortion, from four to five children [ 33 ].
The Articles 185–188 of the Criminal Code and the Decree No. 770/1966 on the interruption of the pregnancy course have been abrogated by Decree-Law No. 1 from December 26 th , 1989, which was published in the Official Gazette No. 4 of December 27 th , 1989 (Par. 8 and Par. 12) [ 34 ].
The Criminal Code from 1968, reissued in 1997, maintained Article 185 about “the illegal induced abortion”, but drastically modified. Thus, in this case of the Criminal Code, we identify abortion as “the interruption of pregnancy course, by any means, committed in any of the following circumstances: ( a ) outside medical institutions or authorized medical practices for this purpose; ( b ) by a person who does not have the capacity of specialized doctor; ( c ) if age pregnancy has exceeded 14 weeks”, the punishment laid down was the imprisonment from 6 months to 3 years” (Art. 185, Par. 1) [ 35 ]. For the abortion committed without the prior consent of the pregnant woman, the punishment consisted in strict prison conditions from two to seven years and with the prohibition of certain rights (Art. 185, Par. 2) [ 35 ].
For the situation of causing serious physical injury to the pregnant woman, the punishment was strict prison from three to 10 years and the removal of certain rights, and if it had as a result the death of the pregnant woman, the punishment was strict prison from five to 15 years and the prohibition of certain rights (Art. 185, Par. 3) [ 35 ].
The attempt was punished for the crimes specified in the various cases of abortion.
Consideration should also be given in the Criminal Code reissued in 1997 for not punishing the interruption of the pregnancy course carried out by the doctor, if this interruption “was necessary to save the life, health or the physical integrity of the pregnant woman from a grave and imminent danger and that it could not be removed otherwise; in the case of a over fourteen weeks pregnancy, when the interruption of the pregnancy course should take place from therapeutic reasons” and even in a situation of a woman’s lack of consent, when it has not been given the opportunity to express her will, and abortion “was imposed by therapeutic reasons” (Art. 185, Par. 4) [ 35 ].
Criminal Code from 2004 covers abortion in Article 190, defined in the same way as in the prior Criminal Code, with the difference that it affects the limits of the punishment. So, in the event of pregnancy interruption, in accordance with the conditions specified in Paragraph 1, “the penalty provided was prison time from 6 months to one year or days-fine” (Art. 190, Par. 1) [ 36 ].
Nowadays, in Romania, abortion is governed by the criminal law of 2009, which entered into force in 2014, by the section called “aggression against an unborn child”. It should be specified that current criminal law does not punish the woman responsible for carrying out abortion, but only the person who is involved in carrying out the abortion. There is no punishment for the pregnant woman who injures her fetus during pregnancy.
In Article 201, we can find the details on the pregnancy interruption infringement. Thus, the pregnancy interruption can be performed in one of the following circumstances: “outside of medical institutions or medical practices authorized for this purpose; by a person who does not have the capacity of specialist doctor in Obstetrics and Gynecology and the right of free medical practice in this specialty; if gestational age has exceeded 14 weeks”, the punishment is the imprisonment for six months to three years, or fine and the prohibition to exercise certain rights (Art. 201, Par. 1) [ 37 ].
Article 201, Paragraph 2 specifies that “the interruption of the pregnancy committed under any circumstances, without the prior consent of the pregnant woman, can be punished with imprisonment from 2 to 7 years and with the prohibition to exercise some rights” (Art. 201, Par. 1) [ 37 ].
If by facts referred to above (Art. 201, Par. 1 and Par. 2) [ 37 ] “it has caused the pregnant woman’s physical injury, the punishment is the imprisonment from 3 to 10 years and the prohibition to exercise some rights, and if it has had as a result the pregnant woman’s death, the punishment is the imprisonment from 6 to 12 years and the prohibition to exercise some rights” (Art. 201, Par. 3) [ 37 ]. When the facts have been committed by a doctor, “in addition to the imprisonment punishment, it will also be applied the prohibition to exercise the profession of doctor (Art. 201, Par. 4) [ 37 ].
Criminal legislation specifies that “the interruption of pregnancy does not constitute an infringement with the purpose of a treatment carried out by a specialist doctor in Obstetrics and Gynecology, until the pregnancy age of twenty-four weeks is reached, or the subsequent pregnancy interruption, for the purpose of treatment, is in the interests of the mother or the fetus” (Art. 201, Par. 6) [ 37 ]. However, it can all be found in the phrases “therapeutic purposes” and “the interest of the mother and of the unborn child”, which predisposes the text of law to an interpretation, finally the doctors are the only ones in the position to decide what should be done in such cases, assuming direct responsibility [ 38 ].
Article 202 of the Criminal Code defines the crime of harming an unborn child, pointing out the punishments for the various types of injuries that can occur during pregnancy or in the childbirth period and which can be caused by the mother or by the persons who assist the birth, with the specification that the mother who harms her fetus during pregnancy is not punished and does not constitute an infringement if the injury has been committed during pregnancy or during childbirth period if the facts have been “committed by a doctor or by an authorized person to assist the birth or to follow the pregnancy, if they have been committed in the course of the medical act, complying with the specific provisions of his profession and have been made in the interest of the pregnant woman or fetus, as a result of the exercise of an inherent risk in the medical act” (Art. 202, Par. 6) [ 37 ].
The fact situation in Romania
During the period 1948–1955, called “the small baby boom” [ 39 ], Romania registered an average fertility rate of 3.23 children for a woman. Between 1955 and 1962, the fertility rate has been less than three children for a woman, and in 1962, fertility has reached an average of two children for a woman. This phenomenon occurred because of the Decree No. 463/1957 on liberalization of abortion. After the liberalization from 1957, the abortion rate has increased from 220 abortions per 100 born-alive children in the year 1960, to 400 abortions per 100 born-alive children, in the year 1965 [ 40 ].
The application of provisions of Decrees No. 770 of 1966 and No. 411 of 1985 has led to an increase of the birth rate in the first three years (an average of 3.7 children in 1967, and 3.6 children in 1968), followed by a regression until 1989, when it was recorded an average of 2.2 children, but also a maternal death rate caused by illegal abortions, raising up to 85 deaths of 100 000 births in the year of 1965, and 170 deaths in 1983. It was estimated that more than 80% of maternal deaths between 1980–1989 was caused by legal constraints [ 30 ].
After the Romanian Revolution in December 1989 and after the communism fall, with the abrogation of Articles 185–188 of the Criminal Code and of the Decree No. 770/1966, by the Decree of Law No. 1 of December 26 th , 1989, abortion has become legal in Romania and so, in the following years, it has reached the highest rate of abortion in Europe. Subsequently, the number of abortion has dropped gradually, with increasing use of birth control [ 41 ].
Statistical data issued by the Ministry of Health and by the National Institute of Statistics (INS) in Romania show corresponding figures to a legally carried out abortion. The abortion number is much higher, if it would take into account the number of illegal abortion, especially those carried out before 1989, and those carried out in private clinics, after the year 1990. Summing the declared abortions in the period 1958–2014, it is to be noted the number of them, 22 037 747 exceeds the current Romanian population. A detailed statistical research of abortion rate, in terms of years we have exposed in Table Table1 1 .
The number of abortions declared in Romania in the period 1958–2016
|
|
|
|
|
|
|
|
|
|
|
| 1958 | 112 100 | 1970 | 292 410 | 1982 | 468 041 | 1994 | 530 191 | 2006 | 150 246 |
| 1959 | 578 000 | 1971 | 330 000 | 1983 | – | 1995 | 502 840 | 2007 | 137 226 |
| 1960 | 774 000 | 1972 | 381 000 | 1984 | 303 123 | 1996 | 456 221 | 2008 | 137 226 |
| 1961 | 865 000 | 1973 | 376 000 | 1985 | 302 838 | 1997 | 347 126 | 2009 | 115 457 |
| 1962 | 967 000 | 1974 | 335 000 | 1986 | 183 959 | 1998 | 271 496 | 2010 | 101 915 |
| 1963 | 1 037 000 | 1975 | 359 417 | 1987 | 182 442 | 1999 | 259 888 | 2011 | 101 915 |
| 1964 | 1 100 000 | 1976 | 383 000 | 1988 | 185 416 | 2000 | 257 865 | 2012 | 88 135 |
| 1965 | 1 115 000 | 1977 | 379 000 | 1989 | 193 084 | 2001 | 254 855 | 2013 | 86 432 |
| 1966 | 973 000 | 1978 | 394 000 | 1990 | 992 265 | 2002 | 247 608 | 2014 | 78 371 |
| 1967 | 206 000 | 1979 | 404 000 | 1991 | 866 934 | 2003 | 224 807 | 2015 | 70 447 |
| 1968 | 220 000 | 1980 | 413 093 | 1992 | 691 863 | 2004 | 191 038 | 2016 | 63 085 |
| 1969 | 258 000 | 1981 | – | 1993 | 585 761 | 2005 | 163 459 |
|
|
Source: Pro Vita Association (Bucharest, Romania), National Institute of Statistics (INS – Romania), EUROSTAT [ 42 , 43 , 44 ]
Data issued by the United Nations International Children’s Emergency Fund (UNICEF) in June 2016, for the period 1989–2014, in matters of reproductive behavior, indicates a fertility rate for Romania with a continuous decrease, in proportion to the decrease of the number of births, but also a lower number of abortion rate reported to 100 deliveries (Table (Table2 2 ).
Reproductive behavior in Romania in 1989–2014
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Total fertility rate (births per woman) | 2.2 | 1.8 | 1.6 | 1.5 | 1.4 | 1.4 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.2 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.3 | 1.4 | 1.3 | 1.0 | 1.36 | 1.40 | 1.44 |
| Live births (1000s) | 369.5 | 314.7 | 275.3 | 260.4 | 250.0 | 246.7 | 236.6 | 231.3 | 236.9 | 237.3 | 234.6 | 234.5 | 220.4 | 210.5 | 212.5 | 216.3 | 221.0 | 219.5 | 214.7 | 221.9 | 222.4 | 212.2 | 196.2 | 201.1 | 182.3 | 183.7 |
| Abortion rate (legally induced abortions per 100 live births) | – | 315.3 | 314.9 | 265.7 | 234.3 | 214.9 | 212.5 | 197.2 | 146.5 | 114.4 | 110.8 | 110.0 | 115.6 | 117.6 | 105.8 | 88.3 | 73.9 | 68.5 | 63.9 | 57.6 | 52.2 | 48.0 | 52.7 | 43.7 | 47.2 | 42.7 |
Source: United Nations International Children’s Emergency Fund (UNICEF), Transformative Monitoring for Enhanced Equity (TransMonEE) Data. Country profiles: Romania, 1989–2015 [ 45 ].
By analyzing data issued for the period 1990–2015 by the International Organization of Health , UNICEF , United Nations Fund for Population Activity (UNFPA), The World Bank and the United Nations Population Division, it is noticed that maternal mortality rate has currently dropped as compared with 1990 (Table (Table3 3 ).
Maternal mortality estimation in Romania in 1990–2015
|
|
|
|
|
|
| 2015 | 31 [22–44] | 56 | 179 | 1.1 |
| 2010 | 30 [26–35] | 61 | 202 | 1.2 |
| 2005 | 33 [28–38] | 71 | 217 | 1.1 |
| 2000 | 51 [44–58] | 110 | 222 | 1.5 |
| 1995 | 77 [66–88] | 180 | 241 | 2.1 |
| 1990 | 124 [108–141] | 390 | 318 | 5.2 |
Source: World Health Organization (WHO), Global Health Observatory Data. Maternal mortality country profiles: Romania, 2015 [ 46 ].
Opinion survey: women’s opinion on abortion
Argument for choosing the research theme
Although the problematic on abortion in Romania has been extensively investigated and debated, it has not been carried out in an ample sociological study, covering Romanian women’s perception on abortion. We have assumed making a study at national level, in order to identify the opinion on abortion, on the motivation to carry out an abortion, and to identify the correlation between religious convictions and the attitude toward abortion.
Examining the literature field of study
In the conceptual register of the research, we have highlighted items, such as the specialized literature, legislation, statistical documents.
Formulation of hypotheses and objectives
The first hypothesis was that Romanian women accept abortion, having an open attitude towards this act. Thus, the first objective of the research was to identify Romanian women’s attitude towards abortion.
The second hypothesis, from which we started, was that high religious beliefs generate a lower tolerance towards abortion. Thus, the second objective of our research has been to identify the correlation between the religious beliefs and the attitude towards abortion.
The third hypothesis of the survey was that, the main motivation in carrying out an abortion is the fact that a woman does not want a baby, and the main motivation for keeping the pregnancy is that the person wants a baby. In this context, the third objective of the research was to identify main motivation in carrying out an abortion and in maintaining a pregnancy.
Another hypothesis was that modern Romanian legislation on the abortion is considered fair. Based on this hypothesis, we have assumed the fourth objective, which is to identify the degree of satisfaction towards the current regulatory provisions governing the abortion.
Research methodology
The research method is that of a sociological survey by the application of the questionnaire technique. We used the sampling by age and residence looking at representative numbers of population from more developed as well as underdeveloped areas.
Determination of the sample to be studied
Because abortion is a typical women’s experience, we have chosen to make the quantitative research only among women. We have constructed the sample by selecting a number of 1260 women between the ages of 15 and 44 years (the most frequently encountered age among women who give birth to a child). We also used the quota sampling techniques, taking into account the following variables: age group and the residence (urban/rural), so that the persons included in the sample could retain characteristic of the general population.
By the sample of 1260 women, we have made a percentage of investigation of 0.03% of the total population.
The Questionnaires number applied was distributed as follows (Table (Table4 4 ).
The sampling rates based on the age, and the region of residence
|
|
|
|
|
|
|
|
| |
| Women in North-West | Urban | 37 898 | 58 839 | 50 527 | 54 944 | 53 962 | 60 321 | 316 491 |
| Rural | 36 033 | 37 667 | 36 515 | 41 837 | 43 597 | 42 877 | 238 526 | |
| Sample in North-West | Urban | 11 | 18 | 15 | 17 | 16 | 18 | 95 |
| Rural | 11 | 11 | 11 | 13 | 13 | 13 | 72 | |
| Women in the Center | Urban | 32 661 | 46 697 | 46 713 | 54 031 | 52 590 | 59 084 | 291 776 |
| Rural | 29 052 | 31 767 | 29 562 | 34 402 | 35 334 | 35 502 | 195 619 | |
| Sample in the Center | Urban | 10 | 14 | 14 | 16 | 16 | 18 | 88 |
| Rural | 9 | 9 | 9 | 10 | 11 | 11 | 59 | |
| Women in North-East | Urban | 38 243 | 50 228 | 45 924 | 51 818 | 49 959 | 63 157 | 299 329 |
| Rural | 63 466 | 51 814 | 47 524 | 60 495 | 67 009 | 65 717 | 356 025 | |
| Sample in North-East | Urban | 11 | 15 | 14 | 16 | 15 | 19 | 90 |
| Rural | 19 | 16 | 14 | 18 | 20 | 20 | 107 | |
| Women in South-East | Urban | 31 556 | 40 879 | 43 317 | 53 461 | 53 756 | 67 135 | 290 104 |
| Rural | 34 494 | 32 446 | 29 987 | 37 828 | 41 068 | 42 836 | 218 659 | |
| Sample in South-East | Urban | 10 | 12 | 13 | 16 | 16 | 20 | 87 |
| Rural | 10 | 10 | 9 | 11 | 12 | 13 | 65 | |
| Women in South Muntenia | Urban | 30 480 | 38 066 | 40 049 | 47 820 | 49 272 | 64 739 | 270 426 |
| Rural | 52 771 | 55 286 | 49 106 | 60 496 | 67 660 | 74 401 | 359 720 | |
| Sample in South Muntenia | Urban | 9 | 11 | 12 | 14 | 15 | 19 | 80 |
| Rural | 16 | 17 | 15 | 18 | 20 | 22 | 108 | |
| Women in Bucharest–Ilfov | Urban | 41 314 | 83 927 | 90 607 | 102 972 | 86 833 | 98 630 | 504 283 |
| Rural | 5385 | 7448 | 7952 | 9997 | 9400 | 10 096 | 50 278 | |
| Sample in Bucharest–Ilfov | Urban | 12 | 25 | 27 | 31 | 26 | 30 | 151 |
| Rural | 2 | 2 | 2 | 3 | 3 | 3 | 15 | |
| Women in South-West Oltenia | Urban | 26 342 | 31 155 | 33 493 | 39 064 | 39 615 | 50 516 | 220 185 |
| Rural | 31 223 | 29 355 | 26 191 | 32 946 | 36 832 | 40 351 | 196 898 | |
| Sample in South-West Oltenia | Urban | 8 | 9 | 10 | 12 | 12 | 15 | 66 |
| Rural | 9 | 9 | 8 | 10 | 11 | 12 | 59 | |
| Women in West | Urban | 30 258 | 45 687 | 39 583 | 44 808 | 44 834 | 54 155 | 259 325 |
| Rural | 19 205 | 20 761 | 19 351 | 22 788 | 24 333 | 26 792 | 133 230 | |
| Sample in West | Urban | 9 | 14 | 12 | 13 | 14 | 16 | 78 |
| Rural | 6 | 6 | 6 | 7 | 7 | 8 | 40 | |
| Total women | 540 381 | 662 022 | 636 401 | 749 707 | 756 054 | 856 309 | 4 200 874 | |
| Total sample | 162 | 198 | 191 | 225 | 227 | 257 | 1260 | |
Source: Sample built, based on the population data issued by the National Institute of Statistics (INS – Romania) based on population census conducted in 2011 [ 47 ].
Data collection
Data collection was carried out by questionnaires administered by 32 field operators between May 1 st –May 31 st , 2018.
The analysis of the research results
In the next section, we will present the main results of the quantitative research carried out at national level.
Almost three-quarters of women included in the sample agree with carrying out an abortion in certain circumstances (70%) and only 24% have chosen to support the answer “ No, never ”. In modern contemporary society, abortion is the first solution of women for which a pregnancy is not desired. Even if advanced medical techniques are a lot safer, an abortion still carries a health risk. However, 6% of respondents agree with carrying out abortion regardless of circumstances (Table (Table5 5 ).
Opinion on the possibility of carrying out an abortion
|
| |
|
|
|
| Yes, under certain circumstances | 70% |
| No, never | 24% |
| Yes, regardless the situation | 6% |
| Total | 100% |
Although abortions carried out after 14 weeks are illegal, except for medical reasons, more than half of the surveyed women stated they would agree with abortion in certain circumstances. At the opposite pole, 31% have mentioned they would never agree on abortions after 14 weeks. Five percent were totally accepting the idea of abortion made to a pregnancy that has exceeded 14 weeks (Table (Table6 6 ).
Opinion on the possibility of carrying out an abortion after the period of 14 weeks of pregnancy
|
| |
|
|
|
| Yes, under certain circumstances | 64% |
| No, never | 31% |
| Yes, regardless the situation | 5% |
| Total | 100% |
For 53% of respondents, abortion is considered a crime as well as the right of a women. On the other hand, 28% of the women considered abortion as a crime and 16% associate abortion with a woman’s right (Table (Table7 7 ).
Opinion on abortion: at the border between crime and a woman’s right
|
| |
|
|
|
| A crime and a woman’s right | 53% |
| A crime | 28% |
| A woman’s right | 16% |
| I don’t know | 2% |
| I don’t answer | 1% |
| Total | 100% |
Opinions on what women abort at the time of the voluntary pregnancy interruption are split in two: 59% consider that it depends on the time of the abortion, and more specifically on the pregnancy development stage, 24% consider that regardless of the period in which it is carried out, women abort a child, and 14% have opted a fetus (Table (Table8 8 ).
Abortion of a child vs. abortion of a fetus
|
| |
|
|
|
| Both, depending on the moment when the abortion takes place | 59% |
| A child | 24% |
| A fetus | 14% |
| I don’t answer | 3% |
| Total | 100% |
Among respondents who consider that women abort a child or a fetus related to the time of abortion, 37.5% have considered that the difference between a baby and a fetus appears after 14 weeks of pregnancy (the period legally accepted for abortion). Thirty-three percent of them have mentioned that the distinction should be performed at the first few heartbeats; 18.1% think it is about when the child has all the features definitively outlined and can move by himself; 2.8% consider that the difference appears when the first encephalopathy traces are being felt and the child has formed all internal and external organs. A percentage of 1.7% of respondents consider that this difference occurs at the beginning of the central nervous system, and 1.4% when the unborn child has all the features that we can clearly see to a newborn child (Table (Table9 9 ).
The opinion on the moment that makes the difference between a fetus and a child
|
| |
|
|
|
| Over 14 weeks (the period legally accepted for abortion) | 37.5% |
| From the very first heart beat (18 days) | 33.3% |
| When the child has all organs contoured and can move by himself (12 weeks) | 18.1% |
| When the first encephalon traces are being felt and the child has formed all internal and external organs (seven weeks) | 2.8% |
| At the beginning of the central nervous system, liver, kidneys, stomach (six weeks) | 1.7% |
| When the unborn child has all the characteristics that we can clearly observe to a child after birth | 1.4% |
| When you can clearly distinguish his features (nose, cheeks, eyes) (five weeks) | 1.2% |
| Other | 1% |
| I don’t know | 3% |
| Total | 100% |
We noticed that highly religious people make a clear association between abortion and crime. They also consider that at the time of pregnancy interruption it is aborted a child and not a fetus. However, unexpectedly, we noticed that 27% of the women, who declare themselves to be very religious, have also stated that they see abortion as a crime but also as a woman’s right. Thirty-one percent of the women, who also claimed profound religious beliefs, consider that abortion may be associated with the abortion of a child but also of a fetus, this depending on the time of abortion (Tables (Tables10 10 and and11 11 ).
The correlation between the level of religious beliefs and the perspective on abortion seen as a crime or a right
|
| |||||||
|
|
|
| |||||
| A woman’s right | A crime | Both depending on the moment when it took place | Not know | No | |||
| Are you a religious person? | A very religious and practicant person | 1% | 11% | 12% | – | – | 24% |
| A very religious but non practicant person | 4% | 7% | 15% | – | 1% | 27% | |
| A relatively religious and practicant person | 5% | 6% | 13% | – | – | 24% | |
| Relatively religious but non practicant person | 6% | 4% | 13% | 2% | – | 25% | |
| Total | 16% | 28% | 53% | 2% | 1% | 100% | |
The correlation between the level of religious beliefs and the perspective on abortion procedure conducted on a fetus or a child
|
| ||||||
|
|
|
| ||||
| A fetus | A child | Both depending on the time of abortion | Not know | |||
| Are you a religious person? | A very religious and practicant person | 2% | 8% | 14% | – | 24% |
| A very religious but non practicant person | 3% | 7% | 17% | – | 27% | |
| A relatively religious and practicant person | 4% | 5% | 16% | 3% | 28% | |
| Relatively religious but non practicant person | 5% | 4% | 12% | 3% | 24% | |
| Total | 14% | 24% | 59% | 6% | 100% | |
More than half of the respondents have opted for the main reason for abortion the appearance of medical problems to the child. Baby’s health represents the main concern of future mothers, and of each parent, and the birth of a child with serious health issues, is a factor which frightens any future parent, being many times, at least theoretically, one good reason for opting for abortion. At the opposite side, 12% of respondents would not choose abortion under any circumstances. Other reasons for which women would opt for an abortion are: if the woman would have a medical problem (22%) or would not want the child (10%) (Table (Table12 12 ).
Potential reasons for carrying out an abortion
|
| |
|
|
|
| If the child would have a medical problem (genetic or developmental abnormalities of fetus) | 55% |
| If I would have a medical problem | 22% |
| In any of these situations, I would abort | 12% |
| If the child would not be desired | 10% |
| I don’t know | 1% |
| Total | 100% |
Most of the women want to give birth to a child, 56% of the respondents, representing also the reason that would determine them to keep the child. Morality (26%), faith (10%) or legal restrictions (4%), are the three other reasons for which women would not interrupt a pregnancy. Only 2% of the respondents have mentioned other reasons such as health or age.
A percentage of 23% of the surveyed people said that they have done an abortion so far, and 77% did not opted for a surgical intervention either because there was no need, or because they have kept the pregnancy (Table (Table13 13 ).
Rate of abortion among women in the sample
|
| |
|
|
|
| No | 77% |
| Yes | 23% |
| Total | 100% |
Most respondents, 87% specified that they have carried out an abortion during the first 14 weeks – legally accepted limit for abortion: 43.6% have made abortion in the first four weeks, 39.1% between weeks 4–8, and 4.3% between weeks 8–14. It should be noted that 8.7% could not appreciate the pregnancy period in which they carried out abortion, by opting to answer with the option “ I don’t know ”, and a percentage of 4.3% refused to answer to this question.
Performing an abortion is based on many reasons, but the fact that the women have not wanted a child is the main reason mentioned by 47.8% of people surveyed, who have done minimum an abortion so far. Among the reasons for the interruption of pregnancy, it is also included: women with medical problems (13.3%), not the right time to be a mother (10.7%), age motivation (8.7%), due to medical problems of the child (4.3%), the lack of money (4.3%), family pressure (4.3%), partner/spouse did not wanted. A percentage of 3.3% of women had different reasons for abortion, as follows: age difference too large between children, career, marital status, etc. Asked later whether they regretted the abortion, a rate of 69.6% of women who said they had at least one abortion regret it (34.8% opted for “ Yes ”, and 34.8% said “ Yes, partially ”). 26.1% of surveyed women do not regret the choice to interrupted the pregnancy, and 4.3% chose to not answer this question. We noted that, for women who have already experienced abortion, the causes were more diverse than the grounds on which the previous question was asked: “What are the reasons that determined you to have an abortion?” (Table (Table14 14 ).
The reasons that led the women in the sample to have an abortion
|
| |
|
|
|
| I did not desired the child | 47.8% |
| Because of my medical problems | 13.3% |
| It was not the right time | 10.7% |
| I was too young | 8.7% |
| Because the child had health problems (genetic or developmental abnormalities of fetus) | 4.3% |
| Because I did not have financial resources (I couldn’t afford raising a child) | 4.3% |
| Because of the pressure of my family | 4.3% |
| The partner/husband did not wanted | 4.3% |
| Other reasons | 3.3% |
| Total | 100% |
The majority of the respondents (37.5%) considered that “nervous depression” is the main consequence of abortion, followed by “insomnia and nightmares” (24.6%), “disorders in alimentation” and “affective disorders” (each for 7.7% of respondents), “deterioration of interpersonal relationships” and “the feeling of guilt”(for 6.3% of the respondents), “sexual disorders” and “panic attacks” (for 6.3% of the respondents) (Table (Table15 15 ).
Opinion on the consequences of abortion
|
| |
|
|
|
| Nervous depression | 37.5% |
| Insomnia and nightmares | 24.6% |
| Disorders in alimentation | 7.7% |
| Affective disorders | 7.7% |
| Deterioration of interpersonal relationships | 6.3% |
| The feeling of guilt | 6.3% |
| Sexual disorders | 3.3% |
| Panic attacks | 3.3% |
| Other reasons | 3.3% |
| Total | 100% |
Over half of the respondents believe that abortion should be legal in certain circumstances, as currently provided by law, 39% say it should be always legal, and only 6% opted for the illegal option (Table (Table16 16 ).
Opinion on the legal regulation of abortion
|
| |
|
|
|
| Legal in certain terms | 53% |
| Always legal | 39% |
| Illegal | 6% |
| I don’t know | 2% |
| Total | 100% |
Although the current legislation does not punish pregnant women who interrupt pregnancy or intentionally injured their fetus, survey results indicate that 61% of women surveyed believe that the national law should punish the woman and only 28% agree with the current legislation (Table (Table17 17 ).
Opinion on the possibility of punishing the woman who interrupts the course of pregnancy or injures the fetus
|
| |
|
|
|
| Yes | 61% |
| No | 28% |
| I don’t know | 7% |
| I don’t answer | 4% |
| Total | 100% |
For the majority of the respondents (40.6%), the penalty provided by the current legislation, the imprisonment between six months and three years or a fine and deprivation of certain rights for the illegal abortion is considered fair, for a percentage of 39.6% the punishment is too small for 9.5% of the respondents is too high. Imprisonment between two and seven years and deprivation of certain rights for an abortion performed without the consent of the pregnant woman is considered too small for 65% of interviewees. Fourteen percent of them think it is fair and only 19% of respondents consider that Romanian legislation is too severe with people who commit such an act considering the punishment as too much. The imprisonment from three to 10 years and deprivation of certain rights for the facts described above, if an injury was caused to the woman, is considered to be too small for more than half of those included in the survey, 64% and almost 22% for nearly a quarter of them. Only 9% of the respondents mentioned that this legislative measure is too severe for such actions (Table (Table18 18 ).
Opinion on the regulation of abortion of the Romanian Criminal Code (Art. 201)
|
|
|
|
|
|
|
|
| |
| Reasonable | 40.6% | 14% | 22% |
| Too small | 39.6% | 65% | 64% |
| Too big | 9.5% | 19% | 9% |
| I don’t know | 6.6% | 2% | 3% |
| I don’t answer | 3.7% | – | 2% |
| Total | 100% | 100% | 100% |
Conclusions
After analyzing the results of the sociological research regarding abortion undertaken at national level, we see that 76% of the Romanian women accept abortion, indicating that the majority accepts only certain circumstances (a certain period after conception, for medical reasons, etc.). A percentage of 64% of the respondents indicated that they accept the idea of abortion after 14 weeks of pregnancy (for solid reasons or regardless the reason). This study shows that over 50% of Romanian women see abortion as a right of women but also a woman’s crime and believe that in the moment of interruption of a pregnancy, a fetus is aborted. Mostly, the association of abortion with crime and with the idea that a child is aborted is frequently found within very religious people. The main motivation for Romanian women in taking the decision not to perform an abortion is that they would want the child, and the main reason to perform an abortion is the child’s medical problems. However, it is noted that, in real situations, in which women have already done at least one abortion, most women resort to abortion because they did not want the child towards the hypothetical situation in which women felt that the main reason of abortion is a medical problem. Regarding the satisfaction with the current national legislation of the abortion, the situation is rather surprising. A significant percentage (61%) of respondents felt as necessary to punish the woman who performs an illegal abortion, although the legislation does not provide a punishment. On the other hand, satisfaction level to the penalties provided by law for various violations of the legal conditions for conducting abortion is low, on average only 25.5% of respondents are being satisfied with these, the majority (average 56.2%) considering the penalties as unsatisfactory. Understood as a social phenomenon, intensified by human vulnerabilities, of which the most obvious is accepting the comfort [ 48 ], abortion today is no longer, in Romanian society, from a legal or religious perspective, a problem. Perceptions on the legislative sanction, moral and religious will perpetual vary depending on beliefs, environment, education, etc. The only and the biggest social problem of Romania is truly represented by the steadily falling birth rate.
Conflict of interests
The authors declare that they have no conflict of interests.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Coronavirus disease 2019 and first-trimester spontaneous abortion: a case-control study of 225 pregnant patients
Affiliations.
- 1 Division of Gynecology and Obstetrics 1, Department of Surgical Sciences, City of Health and Science, University of Turin, Turin, Italy.
- 2 Division of Gynecology and Obstetrics 1, Department of Surgical Sciences, City of Health and Science, University of Turin, Turin, Italy. Electronic address: [email protected].
- 3 Laboratory of Clinical Pharmacology and Pharmacogenetics, Amedeo di Savoia Hospital, Department of Medical Sciences, University of Turin, Turin, Italy.
- 4 Department of Surgical Sciences, City of Health and Science, University of Turin, Turin, Italy.
- 5 Unit of Infectious Diseases, Amedeo di Savoia Hospital, Department of Medical Sciences, University of Turin, Turin, Italy.
- 6 Laboratory of Microbiology and Virology, Amedeo di Savoia Hospital, ASL Città di Torino, Turin, Italy.
- PMID: 33039396
- PMCID: PMC7543983
- DOI: 10.1016/j.ajog.2020.10.005
Background: The disease caused by the severe acute respiratory syndrome coronavirus 2 was named coronavirus disease 2019 and classified as a global public health emergency. The evidence related to the impact of coronavirus disease 2019 on pregnancy is limited to the second and third trimester of pregnancy, whereas data on the first trimester are scant. Many viral infections can be harmful to the fetus during the first trimester of pregnancy, and whether severe acute respiratory syndrome coronavirus 2 is one of them is still unknown.
Objective: With this study, we evaluated severe acute respiratory syndrome coronavirus 2 infection as a risk factor for early pregnancy loss in the first trimester of pregnancy. Furthermore, coronavirus disease 2019 course in the first trimester was assessed.
Study design: Between February 22 and May 21, 2020, we conducted a case-control study at S. Anna Hospital, Turin, among pregnant women in their first trimester, paired for last menstruation. The cumulative incidence of coronavirus disease 2019 was compared between women with spontaneous abortion (case group, n=100) and those with ongoing pregnancy (control group, n=125). Current or past infection was determined by the detection of severe acute respiratory syndrome coronavirus 2 from nasopharyngeal swab and severe acute respiratory syndrome coronavirus 2 immunoglobulin G and immunoglobulin M antibodies in a blood sample. Patient demographics, coronavirus disease 2019-related symptoms, and the main risk factors for abortion were collected.
Results: Of 225 women, 23 (10.2%) had a positive test result for coronavirus disease 2019. There was no difference in the cumulative incidence of coronavirus disease 2019 between the cases (11/100, 11%) and the controls (12/125, 9.6%) (P=.73). Logistic regression analysis confirmed that coronavirus disease 2019 was not an independent predictor of early pregnancy loss (odds ratio, 1.28; confidence interval, 0.53-3.08). Coronavirus disease 2019-related symptoms in the first trimester were fever, anosmia, ageusia, cough, arthralgia, and diarrhea; no cases of pneumonia or hospital admission owing to coronavirus disease 2019-related symptoms were recorded. No difference in the incidence of symptoms was noted between the 2 groups.
Conclusion: Severe acute respiratory syndrome coronavirus 2 infection during the first trimester of pregnancy does not seem to predispose to early pregnancy loss; its cumulative incidence did not differ between women with spontaneous abortion and women with ongoing pregnancy. Coronavirus disease 2019 appears to have a favorable maternal course at the beginning of pregnancy, consistent with what has been observed during the second and third trimesters.
Keywords: COVID-19; SARS-CoV-2; abortion; coronavirus; fetus; first trimester; miscarriage; pregnancy; pregnancy loss; preterm birth; seroprevalence; severe acute respiratory syndrome; vertical transmission.
Copyright © 2020 Elsevier Inc. All rights reserved.
PubMed Disclaimer
Inclusion criteria and time of…
Inclusion criteria and time of serologic and molecular sampling in the case and…

Time elapsed between spontaneous abortion…
Time elapsed between spontaneous abortion care, diagnostic testing and seromolecular profiles Last menstruation…
- Increased incidence of first-trimester miscarriage during the COVID-19 pandemic. Sacinti KG, Kalafat E, Sukur YE, Koc A. Sacinti KG, et al. Ultrasound Obstet Gynecol. 2021 Jun;57(6):1013-1014. doi: 10.1002/uog.23655. Ultrasound Obstet Gynecol. 2021. PMID: 33880806 Free PMC article. No abstract available.
Similar articles
- SARS-CoV-2 in first trimester pregnancy: a cohort study. la Cour Freiesleben N, Egerup P, Hviid KVR, Severinsen ER, Kolte AM, Westergaard D, Fich Olsen L, Prætorius L, Zedeler A, Christiansen AH, Nielsen JR, Bang D, Berntsen S, Ollé-López J, Ingham A, Bello-Rodríguez J, Storm DM, Ethelberg-Findsen J, Hoffmann ER, Wilken-Jensen C, Jørgensen FS, Westh H, Jørgensen HL, Nielsen HS. la Cour Freiesleben N, et al. Hum Reprod. 2021 Jan 1;36(1):40-47. doi: 10.1093/humrep/deaa311. Hum Reprod. 2021. PMID: 33145598 Free PMC article.
- Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Yan J, Guo J, Fan C, Juan J, Yu X, Li J, Feng L, Li C, Chen H, Qiao Y, Lei D, Wang C, Xiong G, Xiao F, He W, Pang Q, Hu X, Wang S, Chen D, Zhang Y, Poon LC, Yang H. Yan J, et al. Am J Obstet Gynecol. 2020 Jul;223(1):111.e1-111.e14. doi: 10.1016/j.ajog.2020.04.014. Epub 2020 Apr 23. Am J Obstet Gynecol. 2020. PMID: 32335053 Free PMC article.
- SARS-CoV-2 infection in the first trimester and the risk of early miscarriage: a UK population-based prospective cohort study of 3041 pregnancies conceived during the pandemic. Balachandren N, Davies MC, Hall JA, Stephenson JM, David AL, Barrett G, O'Neill HC, Ploubidis GB, Yasmin E, Mavrelos D. Balachandren N, et al. Hum Reprod. 2022 May 30;37(6):1126-1133. doi: 10.1093/humrep/deac062. Hum Reprod. 2022. PMID: 35389480 Free PMC article.
- COVID-19 and miscarriage: From immunopathological mechanisms to actual clinical evidence. Cavalcante MB, de Melo Bezerra Cavalcante CT, Cavalcante ANM, Sarno M, Barini R, Kwak-Kim J. Cavalcante MB, et al. J Reprod Immunol. 2021 Nov;148:103382. doi: 10.1016/j.jri.2021.103382. Epub 2021 Sep 10. J Reprod Immunol. 2021. PMID: 34534878 Free PMC article. Review.
- Maternal and fetal outcomes of COVID-19, SARS, and MERS: a narrative review on the current knowledge. Simsek Y, Ciplak B, Songur S, Kara M, Karahocagil MK. Simsek Y, et al. Eur Rev Med Pharmacol Sci. 2020 Sep;24(18):9748-9752. doi: 10.26355/eurrev_202009_23068. Eur Rev Med Pharmacol Sci. 2020. PMID: 33015821 Review.
- SARS-CoV-2 infection in IVF-conceived early pregnancy and the risk of miscarriage: a matched retrospective cohort study. Xu J, Mao D, Liu C, Sun L. Xu J, et al. Hum Reprod Open. 2024 Apr 23;2024(2):hoae024. doi: 10.1093/hropen/hoae024. eCollection 2024. Hum Reprod Open. 2024. PMID: 38764909 Free PMC article.
- SARS-CoV-2 infection is detrimental to pregnancy outcomes after embryo transfer in IVF/ICSI: a prospective cohort study. Li Y, Zhao Q, Ma S, Tang S, Lu G, Lin G, Gong F. Li Y, et al. BMC Med. 2024 Mar 18;22(1):124. doi: 10.1186/s12916-024-03336-9. BMC Med. 2024. PMID: 38500129 Free PMC article.
- Outcomes of SARS-CoV-2 infection in early pregnancy-A systematic review and meta-analysis. Rodriguez-Wallberg KA, Nilsson HP, Røthe EB, Zhao A, Shah PS, Acharya G. Rodriguez-Wallberg KA, et al. Acta Obstet Gynecol Scand. 2024 May;103(5):786-798. doi: 10.1111/aogs.14764. Epub 2024 Jan 10. Acta Obstet Gynecol Scand. 2024. PMID: 38200686 Free PMC article. Review.
- Maternal COVID-19 Serological Changes-Comparison between Seroconversion Rate in First and Third Trimesters of Pregnancy and Subsequent Obstetric Complications: A Cohort Study. Rayo MN, Aquise A, Fernandez-Buhigas I, Gonzalez-Gea L, Garcia-Gonzalez C, Sanchez-Tudela M, Rodriguez-Fernandez M, Tuñon-Le Poultel D, Santacruz B, Gil MM. Rayo MN, et al. Viruses. 2023 Dec 5;15(12):2386. doi: 10.3390/v15122386. Viruses. 2023. PMID: 38140627 Free PMC article.
- COVID-19 incidence in women of reproductive age: a population-based study in Reggio Emilia, northern Italy. Sileo FG, Bonvicini L, Mancuso P, Vicentini M, Aguzzoli L, Khalil A, Giorgi Rossi P. Sileo FG, et al. BMC Pregnancy Childbirth. 2023 Oct 13;23(1):726. doi: 10.1186/s12884-023-06044-z. BMC Pregnancy Childbirth. 2023. PMID: 37833634 Free PMC article.
- Fehr A.R., Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol Biol. 2015;1282:1–23. - PMC - PubMed
- Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. - PMC - PubMed
- Yan J., Guo J., Fan C., et al. Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Am J Obstet Gynecol. 2020;223:111.e1–111.e14. - PMC - PubMed
- Cao D., Yin H., Chen J., et al. Clinical analysis of ten pregnant women with COVID-19 in Wuhan, China: a retrospective study. Int J Infect Dis. 2020;95:294–300. - PMC - PubMed
- Ferrazzi E., Frigerio L., Savasi V., et al. Vaginal delivery in SARS-CoV-2-infected pregnant women in northern Italy: a retrospective analysis. BJOG. 2020 [Epub ahead of print] - PMC - PubMed
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Elsevier Science
- Europe PubMed Central
- Ovid Technologies, Inc.
- PubMed Central
Other Literature Sources
- scite Smart Citations
- MedlinePlus Health Information
Miscellaneous
- NCI CPTAC Assay Portal
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
Advertisement
Subscriber-only Newsletter
Why Are Democrats Losing Ground Among Nonwhite Voters? 5 Theories.
There’s no shortage of solid hypotheses, and the best explanation may be a combination of them.
- Share full article

By Nate Cohn
Why is President Biden losing ground among Black, Hispanic, Asian American and other nonwhite voters?
There’s no easy answer for this relative weakness that shows up in polling, and there might never be one. After all, we still don’t have a definitive explanation for why Donald J. Trump made big gains among white working-class voters in 2016 or Hispanic voters in 2020 , despite the benefit of years of poll questions, final election results and post-election studies.
While the question may be hard, getting the best possible answer matters. Ro Khanna, a Democratic congressman and co-chair of Bernie Sanders’s 2020 presidential campaign, recently asked me on social media whether the Democratic challenge is the absence of a “compelling economic vision.”
If Democrats believe that’s the answer, Mr. Khanna and his colleagues might approach the election differently than if they believe the answer is crime, the migrant crisis or perceptions of a “woke” left. The choice of approach might not only affect who wins, but also the policies and messages promoted on the campaign trail and perhaps ultimately enacted in government.
A definitive answer to our question may be beyond reach, but there’s no shortage of solid hypotheses. The various theories are not mutually exclusive — the best explanation may synthesize all of them.
Theory 1: It’s about the moment — Biden, his age, the economy and abortion
Why do surveys show President Biden struggling among all voters nowadays, regardless of race? The biggest reasons typically cited are inflation, the economy and his age.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

COMMENTS
Among these 48 areas, for 2019, the abortion rate was 11.4 abortions per 1,000 women aged 15-44 years, and the abortion ratio was 195 abortions per 1,000 live births. From 2018 to 2019, the number of abortions increased 2%, the abortion rate increased 0.9%, and the abortion ratio increased 3%.
Abortion services have been targeted by restrictive policies, and unequal access is further compounded by existing weaknesses in our health care system, as highlighted by the coronavirus disease 2019 (Covid-19) pandemic. 7,8 This already fragmented landscape was further complicated when the U.S. Supreme Court ruled that there was no constitutional right to abortion in its June 24, 2022 ...
Background Rape, unintended pregnancy, and abortion are among the most controversial and stigmatized topics facing sexual and reproductive health researchers, advocates, and the public today. Over the past three decades, public health practicioners and human rights advocates have made great strides to advance our understanding of sexual and reproductive rights and how they should be protected ...
A national study that assessed women's support for and interest in alternative models of abortion provision found that about half of U.S. women are supportive of and nearly one-third are interested in medication abortion (Biggs et al., Citation 2019). The growing interest and practice in this type of abortion provision warrant scholars to ...
We are just starting to quantify and qualify their effects. Two recent studies published in JAMA offer early indications of the effects of draconian bans. In "Association of Texas' 2021 Ban on Abortion in Early Pregnancy with the Number of Facility-Based Abortion in Texas and Surrounding States," White et al. used a large dataset ...
Addressing a Crisis in Abortion Access A Case Study in Advocacy. ... York State's previous abortion law allowed for abortion care for any indication up to 26 weeks of gestation; yet, by 2019, when the Reproductive Health Act was passed, many staff were unaware of the existing legal parameters that regulated abortion, and few health care ...
A potentially landmark battle is in play over abortion rights, and it's headed to the U.S. Supreme Court on Dec. 1. In 2018, the Mississippi legislature passed and the governor signed House Bill 1510, known as the Gestational Age Act, which bans abortions after 15 weeks. There are exceptions if the life of the fetus or parent is at risk—but ...
Studies of medication abortion outcomes have often ex-cluded persons with hemoglobin levels less than 9.5 to 10 g per deciliter,33 and screening for anemia by history is appropriate.28,31,34 A patient's history and symptoms should inform the decision to obtain a hemoglobin or hematocrit level before abortion in early pregnancy. 28,34 Additional
2019 Jun 14;19(1):76. doi: 10.1186/s12905-019-0771-9. Authors ... Case presentation: This case study focuses on the story of a 19-year-old Nicaraguan woman who was raped, became pregnant, and almost died from complications resulting from an unsafe abortion. Her case, detailed under the pseudonym Ana Maria, presents unique challenges related to ...
New York State has been a beacon for abortion access since 1970. Yet, after Roe v Wade was decided, New York State abortion law was not in compliance with federal law, and risk-averse medical institutions hesitated to provide later abortions, forcing patients out of state for care. After years of advocacy, the Reproductive Health Act was passed ...
A country's abortion law is a key component in determining the enabling environment for safe abortion. While restrictive abortion laws still prevail in most low- and middle-income countries (LMICs), many countries have reformed their abortion laws, with the majority of them moving away from an absolute ban.
Supreme Court to hear pivotal abortion case in March 03:09. All statistics measuring abortion in the U.S. — the rate, the ratio to live births, and the absolute number — reached a "historic ...
An institutional-based unmatched case-control study was conducted among 413 women from 15th April to 15th June 2021 in selected public hospitals of Arba Minch and Wolayita Sodo town, Southern Ethiopia. ... Oromia, Ethiopia: Cross-sectional study. 2019. Rasch V, et al. Induced abortion in Denmark: effect of socio-economic situation and country ...
Abstract. Canada decriminalized abortion, uniquely in the world, 30 years ago. We present the timeline of relevant Canadian legal, political, and policy events before and since decriminalization. We assess implications for clinical care, health service and systems decisions, health policy, and the epidemiology of abortion in the absence of ...
Under her proposal, states would need to clear laws regulating abortion with the Department of Justice, which would need to confirm they are constitutional before taking effect, she explained in 2019.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Cite this article as: Cosma S, Carosso AR, Cusato J, et al. Coronavirus disease 2019 and first trimester spontaneous abortion: a case-control study of 225 pregnant patients. Am J Obstet Gynecol 2021;224:391.e1-7.
Abortion was a winning issue for Democrats at the ballot box in the 2022 midterm elections and subsequent off-year elections. As an 81-year-old Catholic man who in the past supported abortion ...
2019). Despite its frequency, abortion remains a highly con-tested and stigmatized biopolitical public health issue in the United States (Altshuler et al., 2017). The historic Roe v. ... abortion, we conducted a case study of the website www. abortionchangesyou.com. We selected this website for sev-eral reasons: it is not openly politicized ...
Objective: The aim of the present study was to evaluate psychological problems in women with recurrent spontaneous abortion (RSA). Materials and methods: In this case-control study, 115 women with RSA were assigned to the case group and 240 non-pregnant women comprised the control group. The revised version of the Symptom Checklist-90 (SCL-90-R) and the Intolerance of Uncertainty scale (IUS ...
In this nationwide cohort study, we found that in 2019, a total of 56 468 early-onset cancers were diagnosed in the US. The overall incidence rate of early-onset cancers increased from 2010 to 2019, while the incidence rate of cancers declined among individuals 50 years and older. During the study period, the incidence rates of early-onset ...
Tensions are on a knife edge after Israel carried out a strike on the Hezbollah leader allegedly behind an attack in the Golan Heights.
Among the 49 reporting areas that provided data for 2019, a total of 629,898 abortions were reported. Of these abortions, 625,346 (99.3%) were from 48 reporting areas that provided data every year during 2010-2019. In 2019, these continuously reporting areas had an abortion rate of 11.4 abortions per 1,000 women aged.
On December 1, 2021, the U.S. Supreme Court heard arguments in a Mississippi case, Dobbs v Jackson. 1 Experts who listened to the arguments and questions from the Justices agree that the current federal protections for abortion established by Roe v Wade (hereinafter "Roe") 2 will be significantly weakened. Access will be particularly restricted for people who need abortions later in ...
Of 225 women, 23 (10.2%) had a positive test result for coronavirus disease 2019. There was no difference in the cumulative incidence of coronavirus disease 2019 between the cases (11/100, 11%) and the controls (12/125, 9.6%) (P=.73).Logistic regression analysis confirmed that coronavirus disease 2019 was not an independent predictor of early pregnancy loss (odds ratio, 1.28; confidence ...
Abstract. This article presents a research study on abortion from a theoretical and empirical point of view. The theoretical part is based on the method of social documents analysis, and presents a complex perspective on abortion, highlighting items of medical, ethical, moral, religious, social, economic and legal elements.
The Surprise Ending to the Mar-a-Lago Documents Case The Sunday Read: 'The Kidnapping I Can't Escape' Fifty years ago, her father's friend was taken at gunpoint on Long Island.
Furthermore, coronavirus disease 2019 course in the first trimester was assessed. Study design: Between February 22 and May 21, 2020, we conducted a case-control study at S. Anna Hospital, Turin, among pregnant women in their first trimester, paired for last menstruation. The cumulative incidence of coronavirus disease 2019 was compared between ...
On the other hand, 63 percent of white voters say abortion should be at least mostly legal, a tally greatly exceeding the usual Democratic support among white voters.