Registered Nurse RN
Registered Nurse, Free Care Plans, Free NCLEX Review, Nurse Salary, and much more. Join the nursing revolution.

Nursing Student Quizzes & Sample Tests | Free Quizzes for Nurses
This page contains all of our free interactive quizzes and sample tests for nursing students and current nurses. This page is designed to help nursing students and current nurses succeed. Whether you want to practice some dosage and calculations problems, practice for HESI or NCLEX, this page can help.
We are constantly adding new quizzes and tests–so make sure to bookmark this page, and check back for updates. Also, please help us spread the word–let your friends know about this page so they can enjoy these quizzes and tests. Consider sharing on your Facebook or other social media.
List of all of Our Videos
View all of RegisteredNurseRN’s YouTube videos (teaching tutorials, NCLEX tips, nursing school questions, career help and more)
Nurse Sarah’s Notes and Merch

“ Fluid and Electrolytes Notes, Mnemonics, and Quizzes by Nurse Sarah “. These notes contain 84 pages of Nurse Sarah’s illustrated, fun notes with mnemonics, worksheets, and 130 test questions with rationales.
-You can get an eBook version here or a physical copy of the book here.
“ ABG Interpretation Notes, Mnemonics, and Workbook by Nurse Sarah “. These notes contain 64 pages of Nurse Sarah’s illustrated, fun notes with mnemonics, and worksheets that include over 90 ABG practice problems and 60 test review questions covering ABG concepts.
NCLEX Practice Test
We have developed NCLEX practice quizzes to help you prepare for the NCLEX exam. These quizzes are designed to test your knowledge on what you may encounter on the NCLEX exam. Each quiz has rationals and you will be able to see what you got right and wrong.
Respiratory System
- Respiratory Sounds (Comprehensive)
- Wheezes (high-pitched) Lung Sounds Quiz
- Rhonchi Lung Sounds Quiz
- Fine Crackles Lung Sounds Quiz
- Stridor Lung Sounds Quiz
- Coarse Crackles Lung Sounds Quiz
- Pleural Friction Rub Quiz
- Lung Sounds Quiz
- ARDS NCLEX Questions
- Tuberculosis NCLEX Questions
- Asthma Quiz
- Pneumothorax Quiz
- Chest Tube Care Quiz
- Chronic Bronchitis vs Emphysema Quiz
- COPD (chronic obstructive pulmonary disease) Quiz
- Lung Anatomy and Physiology Quiz
- Pneumonia Quiz
- Coronavirus (COVID-19) Quiz
EKG/ECG Quizzes
- ECG Identify Rhythms Quiz
- Junctional Tachycardia Rhythm Quiz
- Accelerated Junctional Rhythm Quiz
- Junctional Escape Rhythm Quiz
- Pulseless Electrical Activity (PEA) Quiz
- Asystole Rhythm Quiz
- Ventricular Tachycardia (V-tach) Quiz
- Ventricular Fibrillation (V-fib) Quiz
- Atrial Fibrillation (A-Fib) Quiz
- Atrial Flutter Quiz
- Normal Sinus Rhythm Quiz
- Third-Degree (Complete) Heart Block Quiz
- Second-Degree type II (Mobitz type II) Quiz
- Second-Degree type I (Mobitz type I Wenckebach) Quiz
- First-Degree Heart Block Quiz
- Sinus Tachycardia ECG/EKG Quiz
- Sinus Bradycardia ECG/EKG Quiz
- ECG/EKG Interpretation Basics Quiz
- QRS Complex Measurement Quiz
- PR Interval Measurement on EKG Quiz
- EKG Rhythm Quiz on Heart Blocks
- EKG Rhythm Quiz on Atrial Fibrillation & Atrial Flutter
- EKG Rhythm Strip on PQRST Quiz
- Car Seat Safety NCLEX Questions
- Adolescent Growth Development NCLEX Questions Quiz
- School-age Growth Developmental NCLEX Questions Quiz
- Preschooler Growth Development Milestones NCLEX Questions
- Toddler Developmental Milestones NCLEX Questions
- Infant Developmental Milestones NCLEX Questions
- Newborn (Infant) Reflexes NCLEX Questions
- Truncus Arteriosus NCLEX Questions
- Coarctation of the Aorta NCLEX Questions
- Transposition of the Great Arteries NCLEX Questions
- Atrial Septal Defect NCLEX Questions
- Ventricular Septal Defect NCLEX Questions
- Patent Ductus Arteriosus NCLEX Questions
- Tetralogy of Fallot NCLEX Questions
- Cystic Fibrosis NCLEX Questions
- Epiglottitis
- Immunization Schedule (Ages 0 to 6 years)
- NCLEX Peds Metabolic & Endocrine Disorders
- Safe Dosage Calculations for Pediatrics
- NCLEX Pediatric Nursing Developmental Stages
- Glasgow Coma Scale NCLEX Questions
- Alzheimer’s Disease (dementia) NCLEX Questions
- Autonomic Dysreflexia NCLEX Questions
- Guillain-Barré Syndrome NCLEX Questions
- Seizures NCLEX questions
- Multiple Sclerosis
- How to Calculate Cerebral Perfusion Pressure Quiz
- Increased Intracranial Pressure (ICP) Quiz
- Parkinson’s Disease Quiz
- Stroke (CVA) Quiz
- Cholinergic Crisis vs. Myasthenic Crisis Quiz
- Myasthenia Gravis Quiz
- Sympathetic vs. Parasympathetic Nervous System Quiz
- Cancer Staging and Grading NCLEX Questions
- HIV (AIDS) NCLEX Questions Nursing Quiz
- Metabolic Panel (CMP vs. BMP) Quiz
- PT/INR vs. aPTT Quiz
- Complete Blood Count (CBC) NCLEX Questions
- Labs to Know for NCLEX Quiz
- Sickle Cell Anemia Quiz
- Blood Transfusion Quiz
- Blood Types Quiz
- Pernicious Anemia Quiz
- Iron-deficiency Anemia Quiz
Autoimmune Disorders
- Systemic Lupus Erythematosus NCLEX Questions
Dosage Calculations
Many students struggle in their Dosage Calculations nursing school class. While the math can be difficult to learn at first, it does get much easier in time. Here are some tests you can practice:
- IV Completion and Infusion Time (Flow Rates gtts/min)
- Desired Over Have Practice Questions
- Insulin Drip Calculations Quiz
- How to Read a Medication Label Nursing Quiz
- 24-Hour Clock vs. 12-Hour Clock Practice Quiz
- COMPREHENSIVE: Dosage Calculations
- Body Surface Area Calculations
- Tube Feeding Nursing Calculations
- Dopamine IV Drip Calculation
- Heparin Drip Practice Problems
- IV Infusion Time Quiz
- Celsius and Fahrenheit Conversion Quiz
- Grain Nursing Dosage Calculations Quiz
- Safe Dosage Calculations for Pediatrics Quiz
- Weight-based Calculations Quiz
- Drug Reconstitution Calculation Quiz
- IV Infusion Rates Quiz
- IV Flow Rates Quiz
- IV Bolus Quiz
- Oral Medication Quiz
- Capsules & Tablets Quiz
- Conversions Quiz
Pharmacology
- SSRIs Antidepressant NCLEX Questions
- Rights of Medication Administration
- Barbiturates NCLEX Questions
- Benzodiazepines NCLEX Questions
- Medication Frequencies Time Abbreviation Quiz
- Medication Administration Routes and Abbreviations Quiz
- Statins (HMG-CoA Reductase Inhibitors) NCLEX Questions
- Antidotes for Meds NCLEX Quiz
- Beta Blockers NCLEX Questions
- Calcium Channel Blockers NCLEX Questions
- Potassium-Sparing Diuretic NCLEX Questions
- Thiazide Diuretics NCLEX Questions
- Loop Diuretics NCLEX Questions
- ARBs Angiotensin II Receptor Blockers NCLEX Questions
- ACE Inhibitors NCLEX Questions
- Heparin NCLEX Questions
- Warfarin (Coumadin) NCLEX Questions
- Digoxin NCLEX Questions
- Aminoglycosides (Antibiotics) NCLEX Questions
- Macrolides (Antibiotics) NCLEX Questions
- Fluoroquinolones (Antibiotics) NCLEX Questions
- Cephalosporins (Antibiotics) NCLEX Questions
Eye Disorders
- Glaucoma NCLEX Questions
- Cataracts NCLEX Questions
Anatomy & Physiology Quizzes
These anatomy and physiology quizzes are designed to help you understand exam material in your lecture class. Each quiz is specially made to test your knowledge on anatomy terms, function, and location of material. We tried to compile the most common used test questions asked in an Anatomy and Physiology class.
- Medical Terminology Prefixes Quiz
- Medical Terminology Suffixes Quiz
- Layers of the Heart Wall Quiz
- Regional Terms Anatomy Quiz
- Skin Glands Anatomy Quiz
- Nail Anatomy Quiz
- Tooth Anatomy Quiz (structure and tissues)
- Types of Teeth Quiz
- Biceps Brachii Anatomy Quiz
- Brachialis Anatomy Quiz
- Body Movement Terms Quiz (Comprehensive)
- Flexion and Extension Quiz
- Rotation Quiz
- Gliding Quiz
- Abduction and Adduction Quiz
- Circumduction Quiz
- Elevation and Depression Quiz
- Protrusion, Excursion, Retrusion Quiz
- Protraction vs. Retraction Quiz
- Inversion vs. Eversion Quiz
- Dorsiflexion vs. Plantarflexion Quiz
- Opposition and Reposition Quiz
- Pronation vs. Supination Quiz
- Smooth Muscle Quiz
- Cardiac Muscle Tissue Quiz
- Skeletal Muscle Tissue Quiz
- Muscle Anatomy Quiz
- Vertebral Column Ligaments Quiz
- Vertebral Column Quiz
- Sacrum Anatomy Quiz
- Coccyx Bone Anatomy Quiz
- Rib Bone Anatomy Quiz
- Sternum Quiz
- Female vs. Male Pelvis Quiz
- Pelvis Quiz
- Patella Quiz
- Tibia and Fibula Quiz
- Bone Types Quiz
- Bones of the Foot Quiz
- Clavicle and Scapula Quiz
- Radius Ulna Bone Quiz
- Humerus Bone Quiz
- Hand, Wrist, Arm Bones Quiz
- Skull Bones Quiz (Cranial and Facial)
- Body Cavities and Membranes Quiz
- Abdominal Regions and Quadrants Quiz
- Anatomical Body Planes and Sections Quiz
- Directional Terms Quiz
- Kidney and Nephron Quiz
- Respiratory System Quiz
- Human Bones Quiz
- Cranial Nerves Quiz
- Quiz on the Pelvis
- Anatomy & Physiology of the Spine & Ribs Quiz
- Anatomy & Physiology Neuron Structure Quiz
- Anatomy & Physiology Skin Integumentary System Quiz
- Anatomy & Physiology Cell Structure & Function Quiz
- Electrical Conduction System of the Heart Quiz
- Blood Flow of Heart Quiz
- True vs. False Labor NCLEX Questions
- Preeclampsia and Eclampsia NCLEX Questions
- Fetal Station Quiz
- Presumptive, Probable, Positive Pregnancy Signs Quiz
- Gestational Diabetes NCLEX Questions
- Gravidity and Parity Quiz
- Fetal Circulation Quiz
- Fundal Height NCLEX Questions
- Abruptio Placentae vs. Placenta Previa Quiz
- Stages of Labor Quiz
- APGAR Scoring Quiz
- Menstrual Cycle Quiz
- GTPAL Calculating Quiz
- Naegele’s Rule Quiz
- Fetal Heart Tone Decelerations Quiz
- NCLEX Maternity Nursing OB Assessment Part 1
- NCLEX Maternity Nursing Prenatal Part 2
Nursing Disaster Management
- Disaster Triage NCLEX Questions
Cardiovascular
- Coronary Artery Anatomy Quiz
- Angina NCLEX Questions
- DVT (Deep Vein Thrombosis) NCLEX Questions
- Peripheral Vascular Disease (PVD) NCLEX Questions
- Renin-Angiotensin-Aldosterone System (RAAS) Quiz
- Preload vs. Afterload Nursing Quiz
- Myocardial Infarction (MI) Quiz
- Coronary Artery Disease Quiz
- Pericarditis Quiz
- Endocarditis Quiz
- Heart Failure Quiz
- Heart Sounds Quiz
Gastrointestinal
- T-Tube NCLEX Questions
- Cholecystitis NCLEX Questions
- Hepatitis NCLEX Questions
- Cirrhosis Quiz
- Pancreatitis Quiz
- Celiac Disease Quiz
- Peptic Ulcer Disease Quiz
- Diverticulosis and Diverticulitis Quiz
- Crohn’s Disease vs. Ulcerative Colitis Quiz
- Crohn’s Disease Quiz
- Ulcerative Colitis Quiz
- Appendicitis Quiz
- Ostomy Care Quiz
Musculoskeletal
- Assistive Devices NCLEX Questions (Crutches, Canes, Walkers)
- Walker (Assistive Devices) NCLEX Questions
- Canes (Assistive Devices) NCLEX Questions
- Crutches (Assistive Devices) NCLEX Questions
- Fractures Quiz
- Osteoporosis Quiz
- Osteoarthritis vs. Rheumatoid Arthritis Quiz
- Osteoarthritis Quiz
- Rheumatoid Arthritis Quiz
Integumentary
- Skin Cancer NCLEX Questions
- Parkland Burn Formula
- Rule of Nines for Burns
- Pressure Ulcers
- Neurogenic Shock NCLEX Questions
- Anaphylactic Shock NCLEX Questions
- Septic Shock NCLEX Questions
- Hypovolemic Shock NCLEX Questions
- Cardiogenic Shock NCLEX Questions
- Stages of Shock NCLEX Questions
Fundamentals
- Patient Positioning (New)
- Delegation NCLEX Questions
- Intake and Output Calculation Practice
- Personal Protective Equipment (PPE) Quiz
- Isolation Precautions Quiz
- NCLEX Nursing Fundamentals Perioperative Quiz
- NCLEX Positioning Patients Fundamentals
- Chronic Kidney Disease (End Stage Renal Failure) Quiz
- Acute Kidney Injury (Acute Renal Failure) Quiz
- Nephrotic Syndrome vs Glomerulonephritis Quiz
- Nephrotic Syndrome Quiz
- Acute Glomerulonephritis Quiz
- Renal Calculi (Kidney Stones) Quiz
- Urinary Tract Infection Quiz
- Nephron Function Quiz (Part 2)
- Kidney and Nephron Anatomy Quiz (Part 1)
Endocrine Disorders
- Cushing’s Disease and Syndrome NCLEX Questions
- Pheochromocytoma Quiz
- Hypoparathyroidism vs Hyperparathyroidism Quiz
- Myxedema Coma Quiz
- Grave’s Disease Quiz
- Thyroid Storm Quiz
- Hypothyroidism vs Hyperthyroidism Quiz
- DKA vs HHNS Quiz
- Hyperglycemic Hyperosmolar Nonketotic Syndrome (HHNS) Quiz
- Diabetic Ketoacidosis Quiz
- Diabetes Mellitus NCLEX Part 1 Quiz
- Diabetes Pharmacology & Nursing Management Part 2 Quiz
- Addison’s Disease vs Cushing’s Syndrome/Disease Quiz
- SIADH vs Diabetes Insipidus Quiz
- Adrenal Crisis (Addisonian Crisis) Quiz
Fluid & Electrolytes Quizzes
- Colloids Nursing Solutions Quiz
- Fluid Movement Capillary Wall (Oncotic and Hydrostatic Pressure)
- Cell Membrane Transport Quiz (Diffusion, Osmosis, Active Transport)
- Hormones in Fluid Regulation (RAAS and Thirst Mechanism)
- Fluid Volume Deficit (Hypovolemia)
- Fluid Volume Overload Excess (Hypervolemia)
- IV Fluid Types NCLEX Questions
- Hyperchloremia vs. Hypochloremia NCLEX Questions
- Fluid and Electrolyte Nursing Quiz (Comprehensive)
- Hypophosphatemia vs Hyperphosphatemia Quiz
- Hypomagnesemia vs Hypermagnesemia Quiz
- Hyponatremia vs Hypernatremia Quiz
- Hypocalcemia vs Hypercalcemia Quiz
- Isotonic, Hypotonic, & Hypertonic IV Solution Quiz
- Hypokalemia vs Hyperkalemia Quiz
Arterial Blood Gas Quizzes
- Metabolic Acidosis vs Metabolic Alkalosis Quiz
- Respiratory Acidosis vs Respiratory Alkalosis Quiz
- ABG (arterial blood gas) Quiz
NCLEX Quizzes by Subject
- Hypertension NCLEX Quiz (include pharmacology questions)
- NCLEX Oncological Cancer Disorders
- NCLEX Integumentary Skin System (skin disorders) Part 1
- NCLEX Integumentary System (Pressure Ulcers & Burns) Part 2
- NCLEX Fluids & Electrolytes
- NCLEX Nutrition Quiz
- NCLEX Taking Care of Patients with Tubes
ATI TEAS Math Practice Tests
- Solving Equations with One Unknown Variable Quiz
- Multiplying & Dividing Decimal Numbers Quiz
- Order of Operations Quiz
- Multiplying & Dividing Fractions Quiz
- Subtracting Whole Numbers Quiz
- Adding & Subtracting Fractions Quiz
CPR Quizzes
CPR Quiz for an Adult Victim
Video Teaching Tutorials for NCLEX
Easy Way to Understand Fetal Heart Tone Decelerations
Electrical Conduction System of the Heart
EKG PQRST Rhythm Strip
Easy Way to Memorize Blood Flow of the Heart
How to Analyze ABGs with the Tic Tac Toe Method
What is the Metric Table and How to Use it?
What is Dimensional Analysis and How to Set up a Problem
Video 1: Solving Basic Metric Conversions using Dimensional Analysis
Video 2: Solving IV Bolus Problems using Dimensional Analysis
Video 3: Solving Oral Drug Problems with Dimensional Analysis
Video 4: Solving IV Drip Factors gtt/min
Video 5: Solving IV Infusion Rates mL/hr
We’ll be adding more and more quizzes over time , so make sure to bookmark this page and come back often. Also, we’d really appreciate it if you would share it on Facebook, Twitter, or other social media. Thanks so much!
Please Share:
- Click to print (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Telegram (Opens in new window)
Disclosure and Privacy Policy
Important links, follow us on social media.
- Facebook Nursing
- Instagram Nursing
- TikTok Nurse
- Twitter Nursing
- YouTube Nursing
Copyright Notice
NCLEX Practice Questions & Tests for 2024

- Over 125 Years of Healthcare Expertise: 125+ years of combined healthcare experience with a focus in nursing education.
- Exceptional User Satisfaction: 4.9/5 average rating from 3,500+ reviews across TrustPilot , WorthePenny , Better Business Bureau, and other trusted review sites.
- Proven Success: Over 1 million nurses served since 2012 with a 99% NCLEX pass rate ( 2024 NCLEX average pass rate = 79%).
- Team Composition: Staff includes RNs, MSNs, DHSs, nursing professors, and current/former NCLEX question writers.
NCLEX Practice Questions with Answers by Topic
- Clinical Skills & Concepts
- Fluid & Electrolytes
- Mental Health
- Pathophysiology
- Pediatrics & OBGYN
- Pharmacology
Clinical Skills & Concepts NCLEX Practice Questions
Access comprehensive NCLEX practice questions covering dosage calculations, EKG interpretation, Foley catheter insertion, and more.

Fluid & Electrolytes NCLEX Practice Questions
Master essential concepts with NCLEX practice questions focusing on electrolyte lab values, fluid volume deficit, and fluid-electrolyte balance.

Med Surg NCLEX Practice Questions
Prepare for the NCLEX with targeted practice questions covering a wide range of medical-surgical topics, from acute coronary syndrome to stroke management.

Mental Health NCLEX Practice Questions
Enhance your understanding of psychiatric nursing with NCLEX practice questions on cognitive behavioral therapy, therapeutic communication, and psychiatric disorders.

Pathophysiology NCLEX Practice Questions
Dive deep into disease mechanisms with NCLEX practice questions exploring conditions like neurologic disorders, endocrine disorders, and stress physiology.

Pediatrics & OBGYN NCLEX Practice Questions
Sharpen your knowledge of pediatric and obstetric nursing with NCLEX practice questions on topics such as infant reflexes, stages of labor, and menstrual cycle.

Pharmacology NCLEX Practice Questions
Strengthen your grasp of pharmacological principles with NCLEX practice questions covering a spectrum of medications, including analgesics, antibiotics, antipsychotics, and more.

- 125+ Years of Healthcare Expertise
- Over 1,000,000 nurses served
- 99% NCLEX Pass Rate
- 4.9/5 average rating from 3,500+ reviews
NCLEX-RN Practice Questions for Exam Prep
Are you a nursing student preparing for the NCLEX exam in 2024?
As one of the most important exams in your career, having a comprehensive study plan that includes plenty of NCLEX practice questions is crucial. But finding the right resources can feel as overwhelming as studying for the exam!
So, what should an aspiring nurse do? First, take a deep breath, and rest assured you’ve come to the right place.
We’re here to help you prepare for success!
Empowering Your NCLEX Success in 2024
Unveiling your path to triumph, understanding the nclex-rn exam, the nclex-rn milestone, integrating practice nclex questions into prep, what’s different about the new nclex, evolution of the nclex test, adaptive testing and question variability, nclex exam question types, time limit and structure of the nclex-rn examination, strategic time management, scoring and passing standards for the nclex-rn examination, understanding nclex scoring, aiming for success, nclex-rn examination prep and study strategies, nclex-rn test plan, structured study planning, test-taking tactics, winning strategies, navigating exam day, get test ready with simplenursing.
- NCLEX-RN Exam Frequently Asked Questions
The journey to becoming a registered nurse (RN) is an exciting one!
It’s a field full of opportunities to make a positive impact on people’s lives and further professional growth. But first, you must pass the National Council Licensure Examination for Registered Nurses (NCLEX-RN) — and that’s where we come in.
We designed our NCLEX practice question bank to help you feel confident and prepared to ace the exam in 2024.
When preparing for the NCLEX, every bit of knowledge and practice counts. That’s why you need a comprehensive guide and practice question bank that covers all the key areas you need to know to pass the exam in 2024.
But first, let’s look at what the NCLEX is all about.
The NCLEX-RN is a computer-based exam developed by the National Council of State Boards of Nursing (NCSBN).
It tests your knowledge and skills in four major categories:
- Safe and Effective Care Environment: This category focuses on your understanding of nursing management and safety principles in various healthcare settings. It also includes legal and ethical considerations, as well as infection control protocols.
- Health Promotion and Maintenance: This category tests your knowledge of promoting healthy practices for clients across the lifespan. Topics include disease prevention, health education, and screening.
- Psychosocial Integrity: This category covers your understanding of nursing care’s psychological and social aspects. Topics include therapeutic communication, cultural sensitivity, and mental health disorders.
- Physiological Integrity: Physiological integrity covers your understanding of the basic functions and systems of the human body. This includes topics like oxygenation, nutrition, mobility, and elimination. It also includes medication administration and other nursing interventions to promote physiological well-being.
The NCLEX-RN exam is a critical milestone for nursing professionals.
It’s the final step in becoming a licensed RN , and passing it demonstrates that an individual has the necessary knowledge and skills to provide safe, effective care to clients.
One of the primary reasons why the NCLEX-RN is so significant is because it sets a standard for professional nursing practice. By passing the exam, nurses demonstrate that they have met the minimum level of competency required to work in the field.
Additionally, the NCLEX-RN exam is a key component of ensuring client safety. Its rigorous testing process assesses critical thinking and clinical judgment.
Passing the NCLEX ensures that only competent, eligible individuals are providing care to clients.
Moreover, passing the exam is a personal achievement, representing years of hard work, dedication, and commitment to nursing.
One of the most effective ways to prepare for the NCLEX-RN exam is by practicing with NCLEX-style questions.
These questions mimic the format and style of the actual exam, making them an essential tool for improving test-taking skills and increasing confidence. Integrating practice NCLEX questions into your exam preparation allows you to familiarize yourself with the types of questions and the difficulty level you can expect on exam day.
Practicing with NCLEX-style questions also allows you to identify strengths and weaknesses, helping you focus study efforts on areas that need improvement.
Here are two examples of practice NCLEX questions:
- Place the client in a restraint.
- Encourage independence with activities of daily living.
- Conduct hourly neurovascular checks.
- Place a bed alarm.
Correct answer: D. Place a bed alarm.
Rationale: Placing a bed alarm is an appropriate intervention. It will alert the nurse when the client attempts to get out of bed, preventing falls.
- “I can’t believe I have to give myself insulin shots every day.”
- “I will need to limit my sugar intake and exercise regularly.”
- “I guess I’ll have to switch to a low-carb diet now.”
- “Diabetes is a lifelong condition, but I can cure it with medication.”
Correct answer: B. “I will need to limit my sugar intake and exercise regularly.”
Rationale: This statement indicates understanding the lifestyle changes necessary to manage Type 2 diabetes, including limiting sugar intake and exercising regularly. The other options either demonstrate a need for more understanding or provide incorrect information about the condition.
In addition to understanding the significance of the NCLEX-RN exam and the importance of practicing with NCLEX-style questions, it’s essential to be aware of recent changes to the exam.
In 2023, the NCSBN implemented a new version of the NCLEX-RN exam, the Next Generation NCLEX (NGN) . One key difference between the previous and the latest version is an increased emphasis on clinical judgment and decision-making skills.
The NGN project started in response to the evolving health care landscape and changing roles of nurses.
One significant change is new question types requiring test-takers to make decisions based on client scenarios rather than just recalling information. This shift puts a greater emphasis on critical thinking and decision-making skills, essential abilities for nurses at the bedside.
Another significant change in the NGN exam is the implementation of computerized adaptive testing (CAT).
This format tailors each question to an individual’s ability level, allowing for a more personalized and accurate assessment of their knowledge. In traditional exams, all test-takers receive the same questions, regardless of their abilities.
However, with CAT, individuals will receive different questions based on their previous responses, creating a more efficient and precise evaluation of their knowledge.
The NGN has introduced new NCLEX exam questions to assess higher-level thinking and clinical judgment skills.
These include:
- Drag-and-Drop Cloze: When choosing a response, test-takers can drag an option to the answer box, keeping in mind that multiple answers might be correct. Test-takers can also drag the option back to its original list or eliminate it from the question entirely.
- Drop-Down Cloze: This involves a section that offers a selection of drop-down choices for completing a sentence or paragraph, with each choice presenting three to five potential answers.
- Drag-and-Drop Rational: This query involves a question with either a singular cause and effect or dual causes. Test-takers can select an answer from a list and place it over a specified target. They can easily drag the answer back to the list or remove it if they want to change their choice. This method ensures a dynamic and interactive approach to assessing understanding, allowing for a straightforward and efficient evaluation process.
- Drop Down Rationale and Table: This type of question involves one sentence that outlines a cause and its effects, potentially leading to multiple outcomes. The response might take the form of a dyad, consisting of a single sentence with two options to choose from, or a triad, presenting a single sentence accompanied by three selectable options.
- Matrix Multiple Choice and Response: These inquiries consist of four to ten lines, each offering two or three choices. Participants must select one option per line to proceed. Completing all selections is mandatory before moving on to the subsequent question.
- Multiple Response Select N: This type stands out from other multiple-choice questions because test-takers select only a specified number of options, unlike in other formats where they might be allowed to choose all that apply.
- Multiple Response Grouping: The multiple-choice question format involves a structured table containing two to five categories, each offering two to four choices. All categories feature an equal number of options, requiring test-takers to make at least one selection per category to proceed.
- Highlight Text and Table: Taste-takers select key parts of the text to pinpoint what’s crucial for the task at hand. The type of question features answers broken down into manageable pieces, with a limit of ten options available. Test-takers have the flexibility to choose or remove options as they deem appropriate.
- Trend: This question type explores the NCSBN Clinical Judgement Measurement Model (NCJMM), a series of steps to assess clinical judgment.
Test-takers must answer a minimum of 85 questions and a maximum of 150 questions. They must complete the exam in five hours, including breaks.
The test-taker’s performance determines the length of the exam. It automatically ends when the computer determines that the test-taker has reached or exceeded the passing standard. The recommended time to spend on each question is up to two minutes per question.
It’s essential to have a strategic plan in place to manage time effectively during the NCLEX-RN exam.
This includes practicing time management techniques during preparation, such as timing yourself while taking an NCLEX practice test and setting aside specific study periods for each subject area. On exam day, consider using a watch or timer to keep track of your pace and ensure you don’t spend too much time on a single question.
We also recommend taking breaks during the exam to avoid mental fatigue and keep your mind fresh for each section. Taking advantage of these breaks can help you recharge and refocus, increasing your overall performance on the exam.
Did you know an average of 42% of all NCLEX-RN takers will fail (including first-timers and retakers)?
We don’t say this to scare you but to emphasize the importance of understanding the scoring process and what it takes to pass.
The NCLEX-RN exam uses a CAT system to determine a test-taker’s final score. This adaptive system selects each question based on the test-taker’s previous responses, with the difficulty level increasing or decreasing depending on their performance.
It also allows for a more accurate measure of each individual’s nursing knowledge and clinical judgment.
The final score is determined by a pass/fail system, with the NCSBN establishing a minimum passing standard .
This passing standard is based on analyzing each question’s difficulty level and content to ensure only those who demonstrate a safe level of nursing knowledge and clinical judgment will pass the exam.
Aim for proficiency rather than just the minimum passing standard to increase your chances of passing the NCLEX-RN exam.
This means having a thorough understanding of nursing concepts and being able to apply them in different scenarios. Studying beyond what’s required and practicing with NCLEX sample questions can help you achieve this level of proficiency.
It’s also important to manage test anxiety and maintain a positive mindset during the exam. Remember that you have prepared for this moment.
Lastly, don’t be discouraged if you fail your first attempt. Many successful nurses have taken the NCLEX multiple times before passing.
Use your experience to identify areas of improvement and continue to strive for proficiency in all aspects of nursing.
Preparing for the NCLEX-RN exam can be daunting, but it’s manageable with the right strategies and study programs .
Here are tips to help you prepare.
The NCLEX-RN Test Plan is a detailed outline of the exam’s content and format.
Familiarizing yourself with the test plan early will help you create an effective study plan.
Create a structured study schedule that fits your learning style and personal commitments.
Some prefer studying for shorter periods with more frequent breaks, while others may work better with longer study sessions. Choose a method that works best for you and stick to it.
To supplement your studying, use comprehensive resources like:
- NCLEX-RN practice questions
- Online courses
- Predictor tests
- Review books
Knowing how to approach different types of questions can make a significant difference in your test score.
Three useful techniques include:
- Reading the question and all possible answers carefully before choosing an answer
- Eliminating obviously incorrect answers first to narrow down options
- Ruling out extreme answers or those not supported by nursing principles
Understanding the exam format is crucial for success.
Answer each question to the best of your ability, as unanswered questions and incorrect answers can result in lower scores. Additionally, maintaining confidence during the exam is key.
Don’t let challenging questions discourage you.
On exam day, eat a healthy breakfast.
Stay focused during the exam by taking breaks and managing any test-related stress.
In addition to these general strategies, a comprehensive platform like SimpleNursing can increase your chances of success on the NCLEX exam.
We offer animated videos, cheat sheets , practice questions, colorful study guides, and more specifically designed for nursing students preparing for exams.
Don’t let test anxiety or lack of preparation prevent you from achieving your nursing career goals. Sign up for a free trial today and get one step closer to passing the NCLEX exam!
Frequently asked questions
What makes the nclex test questions so hard.
The NCLEX test questions assess critical thinking skills and the ability to make safe decisions as a nurse.
How many questions are on the NCLEX?
The NCLEX has between 85 and 150 questions, but the number of questions a test-taker receives depends on how they answer the previous questions.
Can I retake the NCLEX if I fail?
Yes. However, it is important to review and improve your study strategies . Using a digital NCLEX remediation tool , like SimpleNursing, can help you pinpoint areas for improvement.
How many times can I take the NCLEX?
You can retake the NCLEX up to eight times per year .
How do I get an NCLEX authorization to test (ATT)?
You’ll receive an ATT from the NCSBN after completing the required education and submitting an application.
How long does it take to get NCLEX results?
You typically receive results in about six weeks . But you can use the Pearson Vue NCLEX trick to get unofficial results.
What are the requirements for taking the NCLEX?
You must have graduated from an accredited nursing program . This requirement ensures that all test-takers have a solid foundation in nursing knowledge and skills . You must also complete clinical hours, have a criminal background check, and provide proof of identity.
What do I need to bring to the NCLEX?
You must bring a valid ID and your ATT. Consider bringing a watch and wearing clothing to help you stay comfortable during the exam. If you need accommodations , make sure to notify the testing center ahead of time.
Can I take the NCLEX at home?
No, the NCLEX is a proctored exam , and you must take it at an authorized testing center. There are no provisions for taking the exam remotely.
How do I schedule my NCLEX exam?
You can schedule your exam through the Pearson Vue website or by phone . You’ll need your ATT and payment information to complete the scheduling process.
Education: Bachelor of Arts in Communications, University of Alabama
These NCLEX Practice Questions are made to mimic the actual exam. As such, some question types are more easily viewed on desktop computers.


Home / NCLEX-RN Practice Test Questions
NCLEX-RN Practice Test Questions
You've learned about the NCLEX-RN exam, studied the sections, and are ready to put your knowledge to the test. Take our practice NCLEX exam below to get ready for the real deal.
Jump to Section
Click on the section names below to jump to a particular section of the RegisteredNursing.org NCLEX-RN Practice Exam.
- The Safe and Effective Care Environment: The Management of Care
- The Safe and Effective Care Environment: Safety and Infection Control
- Health Promotion and Maintenance
- Psychosocial Integrity
- Physiological Integrity: Basic Care and Comfort
- Physiological Integrity: Pharmacological and Parenteral Therapies
- Physiological Integrity: Reduction of Risk Potential
- Physiological Integrity: Physiological Adaptation
The NCLEX-RN Test Plan is organized into four major Client Needs categories. Two of the four categories are divided into subcategories as shown below:
- Management of Care – 17% to 23%
- Safety and Infection Control – 9% to 15%
- Health Promotion and Maintenance – 6% to 12%
- Psychosocial Integrity – 6% to 12%
- Basic Care and Comfort – 6% to 12%
- Pharmacological and Parenteral Therapies – 12% to 18%
- Reduction of Risk Potential – 9% to 15%
- Physiological Adaptation – 11% to 17%
For more practice test questions from professional sources try these .

The Safe & Effective Care Environment: The Management of Care Practice Questions
You should respond to the couple by stating that only unanticipated treatments and procedures that are not included in the advance directive can be made by the legally appointed durable power of attorney for healthcare decisions.
- You should be aware of the fact that the wife of the client has a knowledge deficit relating to advance directives and durable powers of attorney for healthcare decisions and plan an educational activity to meet this learning need.
- You should be aware of the fact that the client has a knowledge deficit relating to advance directives and durable powers of attorney for healthcare decisions and plan an educational activity to meet this learning need.
- You should reinforce the wife’s belief that legally married spouses automatically serve for the other spouse’s durable power of attorney for health care decisions and that others than the spouse cannot be legally appointed while people are married
Correct Response: A
Both the client and the client’s spouse have knowledge deficits relating to advance directives. Legally married spouses do not automatically serve for the other spouse’s durable power of attorney for health care decisions; others than the spouse can be legally appointed while people are married.
- Privacy and to have their medical information confidential unless the client formally approves the sharing of this information with others such as family members.
- Make healthcare decisions and to have these decisions protected and communicated to others when they are no longer competent to do so.
- Be fully informed about all treatments in term of their benefits, risks and alternatives to them so the client can make a knowledgeable and informed decision about whether or not to agree to having it
- Make decisions about who their health care provider is without any coercion or undue influence of others including healthcare providers.
Correct Response: B,D
The Patient Self Determination Act, which was passed by the US Congress in 1990, gives Americans the right to make healthcare decisions and to have these decisions protected and communicated to others when they are no longer competent to do so. These decisions can also include rejections for future care and treatment and these decisions are reflect in advance directives. This Act also supports the rights of the client to be free of any coercion or any undue influence of others including healthcare providers.
The Health Insurance Portability and Accountability Act (HIPAA) supports and upholds the clients’ rights to confidentially and the privacy of their medical related information regardless of its form. It covers hard copy and electronic medical records unless the client has formally approved the sharing of this information with others such as family members.
The elements of informed consent which includes information about possible treatments and procedures in terms of their benefits, risks and alternatives to them so the client can make a knowledgeable and informed decision about whether or not to agree to having it may be part of these advanced directives, but the law that protects these advance directives is the Patient Self Determination Act.
- Call the doctor and advise them that the client’s physical status has significantly changed and that they have just had a cardiopulmonary arrest.
- Begin cardiopulmonary resuscitation other emergency life saving measures.
- Notify the family of the client’s condition and ask them what they should be done for the client.
- Insure that the client is without any distressing signs and symptoms at the end of life.
Correct Response: B
You must immediately begin cardiopulmonary resuscitation and all life saving measures as requested.by the client in their advance directive despite the nurse’s own beliefs and professional opinions. Nurses must uphold the client’s right to accept, choose and reject any and all of treatments, as stated in the client’s advance directive.
You would not call the doctor first; your priority is the sustaining of the client’s life; you would also not immediately notify the family for the same reason and, when you do communicate with the family at a later time, you would not ask them what should or should not be done for the client when they wishes are already contained in the client’s advance directive.
Finally, you would also insure that the client is without pain and all other distressing signs and symptoms at the end of life, but the priority and the first thing that you would do is immediately begin cardiopulmonary resuscitation and all life saving measures as requested by the client in their advance directive, according to the ABCs and Maslow’s Hierarchy of Needs.
- Case manager
- Collaborator
- Coordinator of care
Correct Response: D
The priority role of the nurse is advocacy. The nurse must serve as the advocate for both the fetus and the mother at risk as the result of this ethical dilemma where neither option is desirable. As an advocate, the nurse would seek out resources and people, such as the facility’s ethicist or the ethics committee, to resolve this ethical dilemma.
- Client advocate
- Entrepreneur
A nurse who organizes and establishes a political action committee (PAC) in their local community to address issues relating to the accessibility and affordability of healthcare resources in the community is serving as the client advocate. As you should know, the definition of “client” includes not only individual clients, and families as a unit, but also populations such as the members of the local community.
Although the nurse, as the organizer of this political action committee (PAC), will have to collaborate with members of the community to promote the accessibility and affordability of healthcare resources in the community, this is a secondary role rather than the primary role.
Additionally, although the nurse is serving in a political advocacy effort, the nurse is not necessarily a politician and there is no evidence that this nurse is an entrepreneur.
- The right task, the right circumstances, the right person, the right competency, and the right supervision or feedback
- The right task, the right circumstances, the right person, the right direction or communication, and the right supervision or feedback
- The right competency, the right education and training, the right scope of practice, the right environment and the right client condition
- The right competency, the right person, the right scope of practice, the right environment and the right client condition
The Five Rights of Delegation include the right task, the right circumstances, the right person, the right direction or communication, and the right supervision or feedback.
The right competency is not one of these basic Five Rights, but instead, competency is considered and validated as part of the combination of matching the right task and the right person; the right education and training are functions of the right task and the right person who is able to competently perform the task; the right scope of practice, the right environment and the right client condition are functions of the legal match of the person and the task; and the setting of care which is not a Right of Delegation and the matching of the right person, task and circumstances.
- The American Nurses Association’s Scopes of Practice
- The American Nurses Association’s Standards of Care
- State statutes
- Federal law
Correct Response: C
The registered nurse, prior to the delegation of tasks to other members of the nursing care team, evaluates the ability of staff members to perform assigned tasks for the position as based on state statutes that differentiate among the different types of nurses and unlicensed assistive personnel that are legally able to perform different tasks.
Although the American Nurses Association’s Standards of Care guide nursing practice, these standards are professional rather than legal standards and the American Nurses Association does not have American Nurses Association’s Scopes of Practice, only the states’ laws or statutes do.
Lastly, scopes of practice are within the legal domain of the states and not the federal government.
- Observe the staff member during an entire shift of duty to determine whether or not the nurse has accurately and appropriately established priorities.
- Observe the staff member during an entire shift of duty to determine whether or not the nurse has accurately and appropriately completed priority tasks.
- Ask the staff member how they feel like they have been able to employ their time management skills for the last six months.
- Collect outcome data over time and then aggregate and analyze this data to determine whether or not the staff member has completed reasonable assignments in the allotted time before the end of their shift of duty.
The best way to objectively evaluate the effectiveness of an individual staff member’s time management skills in a longitudinal manner is to collect outcome data over time, and then aggregate and analyze this data to determine whether or not the staff member has completed reasonable assignments in the allotted time before the end of their shift of duty. Another way to perform this longitudinal evaluation is to look at the staff member’s use of over time, like the last six months, when the unit was adequately staffed.
Observing the staff member during an entire shift of duty to determine whether or not the nurse has accurately and appropriately established priorities is a way to evaluate the short term abilities for establishing priorities and not assignment completion and observing the staff member during an entire shift of duty to determine whether or not the nurse has accurately and appropriately completed priority tasks is a way to evaluate the short term abilities for completing established priorities and not a complete assignment which also includes tasks that are not of the highest priority.
Lastly, asking the staff member how they feel like they have been able to employ their time management skills for the last six months is the use of subjective rather than objective evaluation.
- An unlicensed staff member who has been “certified” by the employing agency to monitor telemetry: Monitoring cardiac telemetry
- An unlicensed assistive staff member like a nursing assistant who has been “certified” by the employing agency to insert a urinary catheter: Inserting a urinary catheter
- A licensed practical nurse: The circulating nurse in the perioperative area
- A licensed practical nurse: The first assistant in the perioperative area
An unlicensed staff member who has been “certified” by the employing agency to monitor telemetry can monitor cardiac telemetry; they cannot, however, interpret these cardiac rhythms and initiate interventions when interventions are indicated. Only the nurse can perform these roles.
Unlicensed assistive staff member like a nursing assistant cannot under any circumstances be certified” by the employing agency to insert a urinary catheter or insert a urinary catheter because this is a sterile procedure and, legally, no sterile procedures can be done by an unlicensed assistive staff member like a nursing assistant.
Lastly, the role of the circulating nurse is within the exclusive scope of practice for the registered nurse and the role of the first assistant is assumed only by a registered nurse with the advanced training and education necessary to perform competently in this capacity. Neither of these roles can be delegated to a licensed practical nurse or an unlicensed assistive staff member like a nursing assistant or a surgical technician.
- Only the VA health care services because he is not 65 years of age
- Medicare because he has been deemed permanently disabled for 2 years
- Medicaid because he is permanently disabled and not able to work
- Choices B and C
This client is legally eligible for Medicare because he has been deemed permanently disabled for more than 2 years in addition to the VA health care services. People over the age of 65 and those who are permanently disabled for at least two years, according to the Social Security Administration, are eligible for Medicare.
Based on the information in this scenario, the client is not eligible for Medicaid because has a “substantial” VA disability check on a monthly basis and is not indigent and with a low income.
- The case manager’s role in terms of organization wide performance improvement activities
- The case manager’s role in terms complete, timely and accurate documentation
- The case manager’s role in terms of the clients’ being at the appropriate level of care
- The case manager’s role in terms of contesting denied reimbursements
Registered nurse case managers have a primary case management responsibility associated with reimbursement because they are responsible for insuring that the client is being cared for at the appropriate level of care along the continuum of care that is consistent with medical necessity and the client’s current needs. A failure to insure the appropriate level of care jeopardizes reimbursement. For example, care in an acute care facility will not be reimbursed when the client’s current needs can be met in a subacute or long term care setting.
Nurse case managers do not have organization wide performance improvement activities, the supervision of complete, timely and accurate documentation or challenging denied reimbursements in their role. These roles and responsibilities are typically assumed by quality assurance/performance improvement, supervisory staff and medical billers, respectively.
- The ProACT Model: Registered nurses perform the role of the primary nurse in addition to the related coding and billing functions
- The Collaborative Practice Model: The registered nurse performs the role of the primary nurse in addition to the role of the clinical case manager with administrative, supervisory and fiscal responsibilities
- The Case Manager Model: The management and coordination of care for clients throughout a facility who share the same DRG or medical diagnosis
- The Triad Model of Case Management: The joint collaboration of the social worker, the nursing case manager, and the utilization review team
The Triad Model of case management entails the joint collaboration of the social worker, the nursing case manager, and the utilization review team.
The Professionally Advanced Care Team, referred to as the ProACT Model, which was developed at the Robert Wood Johnson University Hospital, entails registered nurses serving in the role of both the primary nurse the clinical case manager with no billing and coding responsibilities; these highly specialized and technical billing and coding responsibilities are done by the business office, medical billers and medical coders.
The Case Manager Model entails the registered nurses’ role in terms of case management for a particular nursing care unit for a group of clients with the same medical diagnosis or DRG. In contrast to this Case Manager Model of Beth Israel Hospital, the Collaborative Practice Model of case management entails the role of some registered nurses in a particular healthcare facility to manage, coordinate, guide and direct the complex care of a population of clients throughout the entire healthcare facility who share a particular diagnosis or Diagnostic Related Group.
- The Case Manager Model
- The ProACT Model
- The Collaborative Practice Model
- The Triad Model of Case Management
The Case Manager Model and the Collaborative Practice Model of case management are the only models of case management that employ the mandated and intrinsic use of critical pathways which are multidisciplinary plans of care that are based on the client’s current condition, and that reflect interventions and expected outcomes within a pre-established time line.
The ProACT Model, the Collaborative Practice Model and the Triad Model of Case Management do not necessarily employ critical pathways; these models can use any system of medical records and documentation.
- An opt out consent
- An implicit consent
- An explicit consent
- No consent at all is given
The type of legal consent that is indirectly given by the client by the very nature of their voluntary acute care hospitalization is an implicit consent indirectly given by the client by the very nature of their voluntary acute care hospitalization is an implicit consent.
An explicit consent, on the other hand, is the direct and formal consent of the client; and an opt out consent is given when a patient does NOT refuse a treatment; this lack of objections by the patient indicates that the person has consented to the treatment or procedure with an opt out consent.
- Take the photographs because these photographs are part of the holiday tradition at this facility
- Take the photographs because all of the residents are properly attired and in a dignified condition
- Refuse to take the photographs unless you have the consent of all to do so
- Refuse to take the photographs because this is not part of the nurse’s role
You should refuse to take the photographs unless you have the consent of all to do so because to do otherwise is a violation of the residents’ rights to privacy and confidentiality as provided in the Health Insurance Portability and Accountability Act (HIPAA). This, rather than the false belief that this is not part of the nurse’s role, is the reason that you would not automatically take these photographs.
Regardless of whether or not these photographs are part of the holiday tradition at this facility and whether or not the residents are properly attired and in a dignified condition, no photographs can be legally taken without the residents’ permission and consent.
- The Patient Self Determination Act: The client’s right to choose the level of care
- The Patient Self Determination Act: The clients’ right to healthcare insurance coverage for mental health disorders
- The Mental Health Parity Act: The privacy and security of technological psychiatric information
- The Health Insurance Portability and Accountability Act (HIPAA): The privacy and security of technological medical information
The Health Insurance Portability and Accountability Act (HIPAA) protects the client’s legal rights to the privacy, security and confidentiality of all medical information including data and information that is technologically stored and secured.
The Patient Self Determination Act uphold the client’s right to choose and reject care and not the level of care that is driven and decided upon as based on medical necessity and health insurance reimbursement; this Act also does not give client’s the right to any health insurance including healthcare insurance coverage for mental health disorders.
Lastly, the Mental Health Parity and Addiction Equality Act, passed in 2008, mandates insurance coverage for mental health and psychiatric health services in a manner similar to medical and surgical insurance coverage; it does not protect the privacy and security of technological psychiatric information, HIPAA does.
- The physical therapist
- The occupational therapist
- The podiatrist
- The nurse practitioner
The member of the multidisciplinary team that you would most likely collaborate with when the client is at risk for falls due to an impaired gait is a physical therapist. Physical therapists are licensed healthcare professionals who assess, plan, implement and evaluate interventions including those related to the patient’s functional abilities in terms of their gait, strength, mobility, balance, coordination, and joint range of motion. They also provide patients with assistive aids like walkers and canes and exercise regimens.
Occupational therapists assess, plan, implement and evaluate interventions including those that facilitate the patient’s ability to achieve their highest possible level of independence in terms of their activities of daily living such as bathing, grooming, eating and dressing.
Podiatrists care for disorders and diseases of the foot; and nurse practitioners, depending on their area of specialty, may also collaborate with nurses when a client is affected with a disorder in terms of gait, strength, mobility, balance, coordination, and joint range of motion, however the member of the multidisciplinary team that you would most likely collaborate with when the client is at risk for falls due to an impaired gait is a physical therapist.
- The dietician
The member of the multidisciplinary team that you would most likely collaborate with when the client can benefit from the use of adaptive devices for eating is the occupational therapist. Occupational therapists assess, plan, implement and evaluate interventions including those that facilitate the patient’s ability to achieve their highest possible level of independence in terms of their activities of daily living such as bathing, grooming, eating and dressing. Many of these interventions include adaptive devices such as special eating utensils and grooming aids.
Physical therapists are licensed healthcare professionals who assess, plan, implement and evaluate interventions including those related to the patient’s functional abilities in terms of their gait, strength, mobility, balance, coordination, and joint range of motion. They also provide patients with assistive aids like walkers and canes and exercise regimens.
Dieticians assess, plan, implement and evaluate interventions including those relating to dietary needs of those patients who need regular or therapeutic diets. They also provide dietary education and work with other members of the healthcare need when a client has dietary needs secondary to physical disorders such as dysphagia; and podiatrists care for disorders and diseases of the foot.
- To fulfill the nurse’s role in terms of collaboration
- To plan and provide for optimal client outcomes
- To solve complex multidisciplinary patient care problems
- To provide educational experiences for experienced nurses
The primary goal of multidisciplinary case conferences is to plan care that facilitates optimal client outcomes. Other benefits of multidisciplinary case conferences include the fulfillment of the nurse’s role in terms of collaboration and collegiality, to solve complex multidisciplinary patient care problems so that optimal client outcomes can be achieved and also to provide educational experiences for nurses; these things are secondary rather than primary goals.
- A Pedorthist
- A pediatric nurse practitioner
- A trauma certified clinical nurse specialist
- A prosthetist
The member of the multidisciplinary team would you most likely collaborate with when your pediatric client has had a traumatic amputation secondary to a terrorism blast explosion a month ago or more ago is a prosthetist. Prosthetists, in collaboration with other members of the healthcare team, assess patients and then design, fit and supply the patient with an artificial body part such as a leg or arm prosthesis. They also follow-up with patients who have gotten a prosthesis to check and adjust it in terms of proper fit, patient comfort and functioning.
Pedorthists modify and provide corrective footwear and employ supportive devices to address conditions which affect the feet and lower limbs. Lastly, you may collaborate with a trauma certified clinical nurse specialist and a pediatric nurse practitioner but this consultation and collaboration should begin immediately upon arrival to the emergency department, and not a month after the injury.
- Conceptualization conflicts
- Avoidance - Avoidance conflicts
- Approach - Approach conflicts
- Resolvable conflicts
- Unresolvable conflicts
- Double Approach - Avoidance conflicts
- Approach-Avoidance conflicts
Correct Response: B, C, F, G
According to Lewin, the types of conflict are Avoidance-Avoidance conflicts, Approach- Approach conflicts, Double Approach - Avoidance conflicts and Approach-Avoidance conflicts.
- Frustration: The phase of conflict that is characterized with personal agendas and obstruction
- Conceptualization: The phase of conflict that occurs when contending parties have developed a clear and objective understanding of the nature of the conflict and factors that have led to it
- Taking action: The phase of conflict that is characterized with individual responses to and feelings about the conflict
- Resolution: The type of conflict that can be resolved
- Avoidance-Avoidance: A stage of conflict that occurs when there are NO alternatives that are acceptable to the contending parties
- Approach- Approach Conflicts: The type of conflict that occurs when the people involved in the conflict want more than one alternatives or actions that could resolve the conflict.
- Approach-Avoidance Conflicts: The type of conflict that occurs when the people involved in the conflict believe that all of the alternatives are NEITHER completely satisfactory nor completely dissatisfactory.
Correct Response: C, F, G
Taking action is the phase of conflict that is characterized with individual responses to and feelings about the conflict; Approach- Approach conflicts are a type of conflict that occurs when the people involved in the conflict want more than one alternatives or actions that could resolve the conflict; and Approach-Avoidance conflicts are a type of conflict that occurs when the people involved in the conflict believe that all of the alternatives are NEITHER completely satisfactory or completely dissatisfactory.
Frustration is the phase of conflict that occurs when those involved in the conflict believe that their goals and needs are being blocked and not met, and not necessarily characterized with personal agendas and obstruction; conceptualization is the phase of conflict that occurs when those involved in the conflict begin to understand what the conflict is all about and why it has occurred. This understanding often varies from person to person and this personal understanding may or may not be accurate, clear or objective, and not a clear and objective understanding of the nature of the conflict and factors that have led to it; resolution is a phase of conflict resolution, not a type of conflict, that is characterized when the contending parties are able to come to some agreement using mediation, negotiation or another method; an Avoidance-Avoidance conflict is a type of conflict and not a phase of conflict, that occurs when there are NO alternatives that are acceptable to any the contending parties; Approach- Approach conflicts occur when the people involved in the conflict want more than one alternative or action that could resolve the conflict; and lastly, Double Approach - Avoidance is a type of conflict and not a stage of conflict that occurs when the people involved in the conflict are forced to choose among alternatives and actions, all of which have BOTH positive and negative aspects to them.
- Competition
- Accommodating Others
Conflicts can be effectively resolved using a number of different strategies and techniques such as compromise, negotiation, and mediation.
Avoidance of the conflict, withdrawing in addition to other passivity, competition, and accommodating others are not effective and healthy conflict resolution techniques.
- Conceptualization
- Frustration
- Taking action
Correct Response: B, A, D, C
The stages of conflict and conflict resolution in the correct sequential order are frustration, conceptualization, and taking action.
- The Patient Self Determination Act
- The Mental Health Parity Act
- The Health Insurance Portability and Accountability Act
- The Americans with Disabilities Act of 1990
The federal law is most closely associated with the highly restrictive “need to know” is the Health Insurance Portability and Accountability Act. This law restricts access to medical information to only those persons who have the need to know this information in order to provide direct and/or indirect care to the client.
The Mental Health Parity Act passed in 2008, mandates insurance coverage for mental health and psychiatric health services in a manner similar to medical and surgical insurance coverage.
And, lastly the Americans with Disabilities Act of 1990 and the Rehabilitation Act of 1973 forbid and prohibit any discrimination against people with disabilities.
- The facility’s Performance Improvement Director who is not a healthcare person and who has no direct contact with clients
- A nursing student who is caring for a client under the supervision of the nursing instructor
- The facility’s Safety Officer who is not a healthcare person and who has no direct contact with clients
- A department supervisor with no direct or indirect care duties
A department supervisor with no direct or indirect care duties does not have the “right to know” medical information; all of the others have the “right to know” medical information because they provide direct or indirect care to clients.
For example, both the facility’s Performance Improvement Director who is not a healthcare person and who has no direct contact with clients and the facility’s Safety Officer who is not a healthcare person and who has no direct contact with clients provide indirect care to clients. For example, they collect and analyze client data in order to fulfill their role and responsibilities in terms of process improvements and the prevention of incidents and accidents, respectively.
Nursing and other healthcare students also have the “need to know” medical information so that they can provide direct client care to their assigned client(s).
- “A computer in the hallway was left unattended and a client’s medical record was visible to me.”
- “I just saw a nursing student looking at the medical record for a client that they are NOT caring for during this clinical experience.”
- “As I was walking past the nursing station, I saw a dietician reading the progress notes written by members of the laboratory department in addition to other dieticians’ progress notes.”
- “I refused the nursing supervisor’s request to share my electronic password for the new nurse on the unit.”
A staff members comment, “As I was walking past the nursing station, I saw a dietician reading the progress notes written by members of the laboratory department in addition to other dieticians’ progress notes” “indicates the need for the Nurse Manager to provide an educational activity relating to confidentiality and information security because dieticians often have the “need to know” about laboratory data so that they can, for example, assess the client’s nutritional status in terms of their creatinine levels.
The report that the nursing student was “looking at the medical record for a client that they are NOT caring for during this clinical experience” indicates that the reporting staff member is correctly applying the principles for maintaining confidentiality and privacy of information; the report that a “computer in the hallway was left unattended and a client’s medical record was visible to me” indicates that the reporting staff member is correctly applying the principles for maintaining confidentiality and privacy of information; and lastly, “I refused the nursing supervisor’s request to share my electronic password for the new nurse on the unit” also indicates that the staff member is knowledgeable about privacy and confidentiality.
- Case management
- Continuity of care
- Medical necessity
- Critical pathway
The continuity of care is defined as the sound, timely, smooth, unfragmented and seamless transition of a client from one area within the same healthcare facility, from one level of care to a higher and more intense level of care or to a less intense level of care based on the client’s status and level of acuity, from one healthcare facility to another healthcare facility and also any discharges to the home in the client’s community.
Case management and critical pathways may be used to facilitate the continuity of care, but they are not the sound, timely, smooth, unfragmented and seamless transition of the client from one level of acuity to another. Lastly, medical necessity is necessary for reimbursement and it is one of the considerations for moving the client from one level of acuity to another but medical necessity is not the continuity of care.
- The Four P's
The standardized “hand off” change of shift reporting system that you may want to consider for implementation on your nursing care unit is ISBAR. Other standardized change of shift “hand off” reports, as recommended by the Joint Commission on the Accreditation of Healthcare Organization, include:
- SBAR, not IBAR
- The Five Ps not the Four Ps and
Lastly, MAUUAR is a method of priority setting and not a standardized “hand off” change of shift reporting system.
- SBAR: Symptoms, background, assessment and recommendations
- ISBAR: Interventions, symptoms, background, assessment and recommendations
- The Five Ps: The patient, plan, purpose, problems and precautions
- BATON: Background, assessment, timing, ownership and next plans
The Five Ps are the patient, plan, purpose, problems and precautions.
The elements of the other standardized reporting systems are listed below:
SBAR stands for:
- S: Situation: The patient’s diagnosis, complaint, plan of care and the patient's prioritized needs
- B: Background: The patient’s code or DNR status, vital Signs, medications and lab results
- A: Assessment: The current assessment of the situation and the patient’s status and
- R: Recommendations: All unresolved issues including things like pending diagnostic testing results and what has to be done over the next few hours
ISBAR stands for:
- I: Introduction: The introduction of the nurse, the nurse’s role in care and the area or department that you are from
- R: Recommendations: All unresolved issues including things like pending diagnostic testing results and what has to be done over the next few hours
BATON stands for:
- B: Background: Past and current medical history, including medications
- A: Actions: What actions were taken and/or those actions that are currently required
- T: Timing: Priorities and level of urgency
- O: Ownership: Who is responsible for what? and
- N: Next: The future plan of care
IPASS stands for:
- I ntroduction: The introduction of the nurse, the nurse’s role in care and the area or department that you are from
- P: Patient: The patient’s name, age, gender, location and other demographic data
- A: Assessment: The current assessment of the situation and the patient’s status
- S: Situation: The patient’s diagnosis, complaint, plan of care and the patient's prioritized needs and
- S: Safety concerns: Physical, mental and social risks and concerns
- Atrial fibrillation
- First degree heart block
- Shortness of breath upon exertion
- An obstructed airway
- Fluid needs
- Respect and esteem by others
- 3,4,2,1,5,6
- 3,4,5,1,2,6
- 2,3,5,1,4,6
- 3,2,4,1,5,6
Correct Response:
Client needs are prioritized in a number of different ways including Maslow’s Hierarchy of Human Needs and the ABCs. In terms of priorities from # 1 to # 6 the conditions above are prioritized as follows:
The ABCs identifies the airway, breathing and cardiovascular status of the patient as the highest of all priorities in that sequential order; and Maslow’s Hierarchy of Needs identifies the physiological or biological needs, including the ABCs, the safety/psychological/emotional needs, the need for love and belonging, the needs for self-esteem and the esteem by others and the self-actualization needs in that order of priority.
- Understanding level
One of the 2 nd priority needs according to the MAAUAR method of priority setting is risks.
The ABCs / MAAUAR method of priority setting places the ABCs, again, as the highest and greatest priorities which are then followed with the 2 nd and 3 rd priority level needs of the MAAUAR method of priority setting.
The 2 nd priority needs according to the MAAUAR method of priority setting after the ABCs include M-A-A-U-A-R which stands for:
- M ental status changes and alterations
- A cute pain
- A cute urinary elimination concerns
- U naddressed and untreated problems that require immediate priority attention
- A bnormal laboratory and other diagnostic data that are outside of normal limits and
- R isks including those relating to a healthcare problem like safety, skin breakdown, infection and other medical conditions
The 3 rd level priorities include all concerns and problems that are NOT covered under the 2 nd level priority needs and the ABCs. For example, increased levels of self care abilities and skills and enhanced knowledge of a medical condition are considered 2 nd level priority needs.
- Time management skills
- Communication skills
- Collaboration skills
- Supervision skills
Time management skills are most closely related to successfully meeting the established priority needs of a group of clients.
In addition to prioritizing and reprioritizing, the nurse should also have a plan of action to effectively manage their time; they should avoid unnecessary interruptions, time wasters and helping others when this helping others could potentially jeopardize their own priorities of care.
Although good communication skills, collaboration skills and supervision are necessary for the delivery of nursing care, it is time management skills that are most closely related to successfully meeting the established priority needs of a group of clients.
- Client rights
Morals are most closely aligned with ethics. Ethics is a set of beliefs and principles that guide us in terms of the right and wrong thing to do which is the most similar to ethics.
Laws and statutes defined what things are legal and what things are illegal. Lastly, client rights can serve as a factor to consider when ethical decisions are made; but they are not most closely aligned with ethics, but only, one consideration of many that can be used in ethical decision making.
- Deontology: The school of ethical of thought that requires that only the means to the goal must be ethical.
- Utilitarianism: The school of ethical of thought that requires that only the end goal must be ethical.
- Deontology: The school of ethical of thought that requires that only the end goal must be ethical.
- Utilitarianism: The school of ethical of thought that requires that only the means to the goal must be ethical.
The two major classifications of ethical principles and ethical thought are utilitarianism and deontology. Deontology is the ethical school of thought that requires that both the means and the end goal must be moral and ethical; and the utilitarian school of ethical thought states that the end goal justifies the means even when the means are not moral.
- Justice: Equally dividing time and other resources among a group of clients
- Beneficence: Doing no harm during the course of nursing care
- Veracity: Fully answering the client’s questions without any withholding of information
- Fidelity: Upholding the American Nurses Association’s Code of Ethics
Fully answering the client’s questions without any withholding of information is an example of the application of veracity into nursing practice. Veracity is being completely truthful with patients; nurses must not withhold the whole truth from clients even when it may lead to patient distress.
Justice is fairness. Nurses must be fair when they distribute care and resources equitably, which is not always equally among a group of patients. Beneficence is doing good and the right thing for the patient; it is nonmaleficence that is doing no harm.
- Planning a way to evaluate the effectiveness of the class by seeing a decrease in the amount of referrals to the facility’s Ethics Committee
- Establishing educational objectives for the class that reflect the methods and methodology that you will use to present the class content
- The need to exclude case studies from the class because this would violate client privacy and confidentiality
- Some of the most commonly occurring bioethical concerns including genetic engineering into the course content
You would consider including some of the most commonly occurring bioethical concerns including genetic engineering into the course content.
You would also plan how you could evaluate the effectiveness of the class by seeing an increase, not a decrease in the amount of referrals to the facility’s Ethics Committee, because one of the elements of this class should address ethical dilemmas and the role of the Ethics Committee in terms of resolving these.
You would additionally establish educational objectives for the class that reflect specific, measurable learner outcomes and not the methods and methodology that you will use to present the class content; and lastly, there is no need to exclude case studies from the class because “sanitized” medical records can, and should be, used to avoid any violations of client privacy and confidentiality.
- Serve as the witness to the client’s signature on an informed consent.
- Get and witness the client’s signature on an informed consent.
- Get and witness the durable power of attorney for health care decisions’ signature on an informed consent.
- None of the above
One of the roles of the registered nurse in terms of informed consent is to serve as the witness to the client’s signature on an informed consent.
Other roles and responsibilities of the registered nurse in terms of informed consent include identifying the appropriate person to provide informed consent for client, such as the client, parent or legal guardian, to provide written materials in client’s spoken language, when possible, to know and apply the components of informed consent, and to also verify that the client comprehends and consents to care and procedures.
The registered nurse does not get the client’s or durable power of attorney for health care decisions’ signature on an informed consent, this is the role and responsibility of the physician or another licensed independent practitioner.
- Self determination
- Nonmalficence
Self-determination is most closely aligned with the principles and concepts of informed consent. Self-determination supports the client’s right to choose and reject treatments and procedures after they have been informed and fully knowledgeable about the treatment or procedure.
Justice is fairness. Nurses must be fair when they distribute care and resources equitably, which is not always equally among a group of patients; fidelity is the ethical principle that requires nurses to be honest, faithful and true to their professional promises and responsibilities by providing high quality, safe care in a competent manner; and, lastly, nonmaleficence is doing no harm, as stated in the historical Hippocratic Oath.
- The purpose of the proposed treatment or procedure
- The expected outcomes of the proposed treatment or procedure
- Who will perform the treatment or procedure
- When the procedure or treatment will be done
The minimal essential components of the education that occurs prior to getting an informed consent include the purpose of the proposed treatment or procedure, the expected outcomes of the proposed treatment or procedure, and who will perform the treatment or procedure. It is not necessary to include when the treatment or procedure will be done at this time.
Other essential elements include:
- The benefits of the proposed treatment or procedure
- The possible risks associated with the proposed treatment or procedure
- The alternatives to the particular treatment or procedure
- The benefits and risks associated with alternatives to the proposed treatment or procedure
- The client’s right to refuse a proposed treatment or procedure
- The Security Rule
- The American Nurses Association’s Code of Ethics
- The American Hospital’s Patients’ Bill of Rights
- The Autonomy Rule
Prohibitions against sharing passwords are legally based on the Security Rule of HIPAA mandates administrative, physical, and technical safeguards to insure the confidentiality, integrity, and availability of electronic protected health information. This rule relates to electronic information security as well as other forms of information.
The American Nurses Association’s Code of Ethics and the American Hospital’s Patients’ Bill of Rights both address client confidentiality and their rights to privacy, however, these statements are not legal, but instead ethical and regulatory statements; and lastly, there is no autonomy law or rule.
- Social networks and cell phone cameras pose low risk in terms of information technology security and confidentiality.
- The security of technological data and information in healthcare environments is most often violated by those who work there.
- The security of technological data and information in healthcare environments is most often violated by computer hackers.
- Computer data deletion destroys all evidence of the data.
The security of technological data and information in healthcare environments is most often violated by those who work there. The vast majority of these violations occur as the result of inadvertent breaches with carelessness and the lack of thought on the part of employees. Technology is a double edged sword.
Technological advances such as cell phone cameras, social networks like Facebook, telephone answering machines and fax machines pose great risk in terms of the confidentiality and the security of medical information. Computer data deletion does not always destroy all evidence of the data; data remains.
- Assault: Touching a person without their consent
- Battery: Threatening to touch a person without their consent
- Slander: False oral defamatory statements.
- Slander: False written defamatory statements.
Slander is false oral defamatory statements; and libel is written defamation of character using false statements.
Assault, an intentional tort, is threatening to touch a person without their consent; and battery, another intentional tort, is touching a person without their consent.
- Ensured the client’s safety which is a high patient care priority
- Violated Respondeat Superior
- Violated the client’s right to dignity
- Committed a crime
When you loosely apply a bed sheet around your client’s waist to prevent a fall from the chair, you have falsely imprisoned the client with this make shift restraint. False imprisonment is restraining, detaining and/or restricting a person’s freedom of movement. Using a restraint without an order is considered false imprisonment even when it is done to protect the client’s safety.
Respondeat Superior is the legal doctrine or principle that states that employers are legally responsible for the acts and behaviors of its employees. Respondeat Superior does not, however, relieve the nurse of legal responsibility and accountability for their actions. They remain liable.
There is no evidence in this question that you have violated the client’s right to dignity.
- Respondeat Superior does not mean that a nurse cannot be held liable.
- Respondeat Superior does not mean that a nurse cannot be held libel.
- Respondeat Superior is an ethical principle.
- Respondeat Superior is a law.
Respondeat Superior does not mean that a nurse cannot be held liable and not libel which is a written defamation of character using false statements. Liability is legal vulnerability.
Respondeat Superior is the legal doctrine or principle and not a law or ethical principle.
- Causation, foreseeability, damages to the patient, a duty that was owed to the client and this duty was breached, and direct rather than indirect harm to the client.
- Causation, foreseeability, damages to the patient, a duty that was owed to the client and this duty was breached, and direct and/or indirect harm to the client.
- Causation, correlation, damages to the patient, a duty that was owed to the client and this duty was breached, and direct and/or indirect harm to the client.
- Causation, foreseeability, damages to the patient, a duty that was owed to the client and this duty was breached, and a medical license.
The six essential components of malpractice include causation, foreseeability, damages to the patient, a duty that was owed to the client and this duty was breached, and, lastly, this breach of duty led to direct and/or indirect harm to the client.
A medical license is not necessary; nurses and other healthcare professionals can be found guilty of malpractice. Lastly, correlation is the relationship of simultaneously changing variables. For example, a ppositive correlation exists when the two variables both increase or decrease; and a negative occurs when one variable increases and the other decreases.
- Sound structures like policies and procedures
- Processes and how they are being done
- Optimal client outcomes
- Optimal staff performance
The current focus of performance improvement activities is to facilitate and address optimal client outcomes. Throughout the last several decades performance improvement activities have evolved from a focus on structures to a focus on process and now, to a focus on outcomes.
Staff performance is not the focus of performance improvement activities but instead the focus of competency assessment and validation.
- An adverse event
- A root cause
- A healthcare acquired event
- A sentinel event
A sentinel event is an event or occurrence, incident or accident that has led to or may have possibly led to client harm. Even near misses, that have the potential for harm, are considered sentinel events because they have the potential to cause harm in the future.
An adverse event, like an adverse effect of a medication, has actually led to an adverse response; it is not a near miss. A root cause is a factor that has led to a sentinel event; and there is no such thing as a healthcare acquired event.
- Discover a process flaw
- Determine who erred
- Discover environmental hazards
- Determine basic client needs
The primary purpose of root cause analysis is to discover process flaws. Root cause analysis and a blame free environment are essential to a successful performance improvement activity, therefore, root cause analysis does not aim to determine who erred and made a mistake. Root cause analysis explores and digs down to the roots of the problem, its root causes and the things, not people, which are the real reasons why medical errors and mistakes are made.
It is nursing assessment that determines the basic client needs and environmental surveillance that discovers environmental safety hazards, and not root cause analysis.
Root cause analysis activities ask “Why”, rather than “Who”, which would place blame on a person or group of people: and What? and When? Questions are rarely asked.
- Historical data and performance improvement activities focus on current data.
- Current data and performance improvement activities focus on historical data.
- Decreasing financial liability and performance improvement activities focus on process improvements.
- Decreasing falls and performance improvement activities focus on process improvements.
The primary distinguishing characteristic of risk management when compared and contrasted to performance improvement is that risk management activities focus on decreasing financial liability and performance improvement activities focus on process improvements.
Risk management focuses on decreasing and eliminating things that are risky and place the healthcare organization in a position of legal liability. Some examples of risk management activities include preventing hazards and adverse events such as patient falls and infant abduction and the legal liabilities associated with these events.
Referrals complement the healthcare teams’ abilities to provide optimal care to the client.
- Referrals simply allow the client to be discharged into the community with the additional care they need.
- Nurses facilitate referrals to only the resources within the facility.
When clients have assessed needs that cannot be fulfilled and met by the registered nurse in collaboration with other members of the nursing care team, the registered nurse should then seek out resources, as well as utilize and employ different internal or external resources such as a physical therapist, a clergy member or a home health care agency in the community and external to the nurse’s healthcare agency.
The Safe & Effective Care Environment: Safety & Infection Control Practice Questions
- The sensitizing dose of penicillin can lead to anaphylaxis.
- The second dose of penicillin can lead to distributive shock.
- You should be aware of the fact that about 10% of the population has an allergy to both penicillin and latex.
- You should be aware of the fact that about 20% of the population has an allergy to both penicillin and latex.
The second dose of penicillin can lead to anaphylactic shock which is a form of distributive shock.
The first exposure to penicillin, referred to as the “sensitizing dose”, sensitizes and prepares the body to respond to a second exposure or dose. It is then the second exposure or dose that leads to anaphylaxis, or anaphylactic shock.
It is estimated that approximately 10% of people have had a reaction to penicillin. Some of these reactions are an allergic response and others are simply a troublesome side effect. There is no scientific data that indicates that 10% or 20% of the population has an allergy to both penicillin and latex.
- A 77 year old female client in a client room that has low glare floors.
- An 87 year old female client in a client room that has low glare floors.
- A 27 year old sedated male client.
- A 37 year old male client with impaired renal perfusion.
The 27 year old sedated male client is at greatest risk for falls.
Some of the risk factors associated with falls are sedating medications, high glare, not low glare, floors and other environmental factors such as clutter and scatter rugs, not low glare floors, a history of prior falls, a fear of falling, incontinence, confusion, sensory deficits, a decreased level of consciousness, impaired reaction time, advancing age, poor muscular strength, balance, coordination, gait and range of motion and some physical disorders, particularly those that affect the musculoskeletal or neurological systems; falls are not associated with poor and impaired renal perfusion.
- The nurse should advise clients in a smoke filled room to open the windows.
- The first thing that the nurse should do when using a fire extinguisher to put out a small fire is to aim the fire extinguisher at the base of the fire.
- Rapidly lift and move a client away from the source of the fire when their slippers are on fire.
- The home health care nurse should advise the client that the best fire extinguisher to have in the home is an ABC fire extinguisher.
The home health care nurse should advise the client that the best fire extinguisher to have in the home is an ABC fire extinguisher because this one fire extinguisher is a combination of a type A fire extinguisher, a type B and a type C, which put out all types of fires including common household solids like wood, household oils like kitchen grease and electrical fires.
The nurse should advise the client GET LOW AND GO if a room fills with smoke. They should not take any time to open window.
The first thing to do when using a fire extinguisher is to pull the pin and then aim it at the base of the fire. Later, you would squeeze the trigger and sweep the spray over and over again over the base of the fire. The acronym PASS is used to remember these sequential steps.
When a person has clothing that has caught on fire, the person should STOP, DROP AND ROLL. Tell the person, to STOP, DROP, and to not run, and as you also cover the person with a blanket to smother the fire.
- A tornado that has touched down on the healthcare facility
- A severe cyclone that has destroyed nearby homes
- A massive train accident that brings victims to your facility
- An act of bioterrorism in a nearby factory
A tornado that has touched down on the healthcare facility is an example of an internal disaster because this tornado has directly affected the healthcare facility. Tornados, cyclones, hurricanes and other severe weather emergencies can be both an internal disaster when they affect the healthcare facility and also an external disaster when they impact on the lives of those living in the community. Hurricane Katrina is a good example of a weather emergency that affected not only healthcare facilities but also members of the community.
- Use a slide board.
- Use a mechanical lift.
- Use a gait belt.
- Notify the client's doctor that the client cannot be safely transferred by you.
The best and safest way to transfer this paralyzed client when you suspect that you will need the help of another for the client’s first transfer out of bed is to use a mechanical lift. It is not necessary or appropriate to notify the doctor.
Mechanical lifts are used mostly for patients who are obese and cannot be safely moved or transferred by two people, and also for patients who are, for one reason or another, not able to provide any help or assistance with their lifts and transfers, such as a person who is paralyzed.
A gait or transfer belt and slide boards are assistive devices that can be used to assist with transfers and lifting however, they are not appropriate for this client as based on your assessment.
- Advise the nurse that the legs must be close together for stability during lifting and transfers.
- Advise the nurse that the legs should be one in front of the other and not spread apart during a transfer.
- Validate the nurse’s competency in terms of the application of body mechanics principles during a transfer.
- Validate the nurse’s competency in terms of the application of ergonomics principles during a transfer.
You should validate the nurse’s competency in terms of the application of body mechanics principles during a transfer because the nurse had spread her legs apart during the transfer to provide a wide base of support, which is a basic principle of body mechanics and not ergonomics.
Simply defined ergonomics addresses correct bodily alignment such as the lumbar curve accommodation in an ergonomically designed chair; and body mechanics is the safe use of the body using the correct posture, bodily alignment, balance and bodily movements to safely bend, carry, lift and move objects and people.
- The client has refrigerated foods labelled with an expiration date.
- You assess that the home is free of scatter rugs that many use to protect the feet against hard floors.
- The client uses the FIFO method for insuring food safety.
- The client assures you that the smoke alarm batteries are replaced annually to insure that they work.
When the client assures the nurse that they replace their smoke alarm batteries annually to insure that they work, the assessing nurse should immediately know that the client is in need of education relating to the fact that smoke alarm batteries should be changed at least twice a year.
The client has demonstrated that they are knowledgeable about food safety and environmental safety because they have expiration dates on refrigerated foods, they use the FIFO method for food safety and they do not use scatter rugs which can lead to falls.
The FIFO rule is F irst I n is F irst O ut. In other words, the first foods in the pantry or refrigerator are the first foods that should be consumed or discarded.
- It is clear?
- It is damaging to the lungs.
- It is damaging to the spleen and the liver.
- It leads to the over production of hemoglobin.
Carbon monoxide is particularly dangerous because it is clear, invisible and odorless. Carbon monoxide poisoning can occur when a person is exposed to an excessive amount of this odorless and colorless gas; it severely impairs the body to absorb life sustaining oxygen which is the result of this deadly gas and not damage to the lungs. This oxygen absorption deficit can lead to serious tissue damage and death. For these reasons, home carbon monoxide alarms are recommended.
These dangers are associated with deoxygenation and not splenic or hepatic damage or the over production of hemoglobin.
- Sentinel event.
- System variance.
- Adverse effect.
- Provider variance.
The lack of necessary supplies and equipment to adequately and safely care for patients is an example of a system variance.
A variance is defined as a deviation that leads to a quality defect or problem. Variances can be classified as a practitioner variance, a system/institutional variance, a patient variance, a random variance and a specific variance.
A sentinel event is defined as is an event or occurrence, incident or accident that has led to or may possibly lead to client harm. Adverse effects are serious and unanticipated responses to interventions and treatments, including things like medications.
- Notify the doctor.
- Render care.
- Assess the cleint.
- Notify the nurse manager.
The first thing that you should do immediately after a client accident is to assess the client and the second thing you should do is render care after this assessment and not before it.
Lastly, notifications to the doctor and the nurse manager are only done after the client is assessed and emergency care, if any, is rendered.
- Counsel the staff about their need to stop wasting the resources of this department.
- Check the equipment yourself to determine the accuracy of this equipment department.
- Ignore it because everyone can make an innocent mistake.
- Plan an educational activity about determining what equipment to send for repairs.
You should plan an educational activity about determining what equipment should and should not be sent for repairs. This data suggests that the staff members need education and training about the proper functioning of equipment used on the nursing care unit.
Counseling the staff about their need to stop wasting the resources of this department is placing blame and this blame may prevent future valid returns of equipment.
You should not check the equipment yourself to determine the accuracy of this equipment department because they are the experts, not you, with these matters.
You should also not ignore it because everyone can make an innocent mistake. The issue has to be addressed and corrected.
- Education and training on all pieces of equipment
- Pilot testing new equipment
- Reading all the manufacturer’s instructions
- Researching the equipment before recommending its purchase
Education and training on all pieces of equipment is an essential component for insuring that medical equipment is being used safely and properly by those who you supervise. Other essential components include validated and documented competency to use any and all pieces of equipment by a person qualified to do so, preventive maintenance and the prompt removal of all unsafe equipment from service.
Pilot testing new equipment, researching the equipment before recommending its purchase, and reading the entire manufacturer’s instructions are things done prior to the purchase of the equipment and these things do not impact on the safety of the piece of medical equipment.
- A possible vulnerability of the facility’s information technology to hacking
- The assisted suicide of a client in your facility by the spouse of the client
- Vulnerability to computer hacking
- Potential information theft
The assisted suicide of a client in your facility by the spouse of the client is a security concern that is also a sentinel event that must be reported.
A possible vulnerability of the facility’s information technology to hacking, vulnerability to computer hacking and potential information theft is security concerns but they are not sentinel events that must be reported.
- Training all nurses to serve as a part of a security response team
- Training all clerical staff to be a part of a security response team
- The restriction of visitors in a special care area
- Bar coded client identification bands to insure proper identification
The restriction of visitors in a special care area is an effective security plan that you may want to consider for implementation within your facility.
Some of the other security measures that you may want to consider include security alert systems to alert staff to a security breach such as security breach of the newborn nursery, the use of visitor identification badges or stickers that identify people who are authorized to be in a facility, closed circuit monitoring and alarm systems in high risk areas such as the emergency care area, automatically locking security doors, and electronic wristbands for the newborn and the mother to prevent infant abductions.
Special assignments and training for a group of people so that this specially trained group can act when a security breach occurs is also a good idea but it is not necessary to train all nurses or clerical staff; it is sufficient to train a limited group of people, provided an ample number of these team members are assigned and available on all tours of duty around the clock, including on holidays.
- Sterile items ONLY are placed on the sterile field.
- The nurse must keep the sterile field below waist level.
- Coughing or sneezing over the sterile field contaminates the sterile field.
- The nurse must maintain a 1/2 inch border around the sterile field that is not sterile.
- Moisture and wetness contaminate the sterile field.
- Sterile masks are used by staff and the client when a sterile field is being set up and/or maintained
Correct Response: A, C, E
Sterile items ONLY are placed on the sterile field; coughing or sneezing over the sterile field contaminates the sterile field; and all moisture and wetness contaminate the sterile field.
Some of the other principles that are applied to setting up and maintaining a sterile field include keeping the sterile field above the waist level and preventing coughing or sneezing by professional staff and the client during the set up and during the maintenance of the sterile field. If there is a danger that anyone may cough or sneeze over the field, the professional staff and/or the client should don a mask to prevent contamination. Lastly, a one inch border, not a ½ border that is not sterile is maintained around the perimeter of the sterile field.
- A physical restraint: A physical restraint is a manufactured device that is used, when necessary, to prevent falls.
- A physical restraint: A physical restraint is any mechanical device, material, or equipment attached to or adjacent to the resident’s body that the individual cannot remove easily which restricts freedom of movement or normal access to one’s body.
- A chemical restraint: A chemical restraint is a drug used for sedation to prevent falls.
- A chemical restraint: A chemical restraint is a drug used for discipline or convenience and not required to treat medical symptoms.
A chemical restraint: A chemical restraint is a drug used for discipline or convenience and not required to treat medical symptoms, according to the Centers for Medicare and Medicaid Services.
The most complete and accurate definition of a physical restraint is any manual method or physical or mechanical device, material, or equipment attached to or adjacent to the resident’s body that the individual cannot remove easily which restricts freedom of movement or normal access to one’s body and is NOT a safety devices that is routinely used for certain procedures, according to the Centers for Medicare and Medicaid Services.
- Informed consent for the restraint
- The reason for the restraint
- The type of restraint to be used
- Client behaviors that necessitated the restraints
The minimal components of orders for restraint include the reason for and rationale for the use of the restraint, the type of restraint to be used, how long the restraint can be used, the client behaviors that necessitated the use of the restraints, and any special instructions beyond and above those required by the facility’s policies and procedures.
Informed consent is not necessary for the initiation or the use of restraints
- The vascular phase
- The prodromal phase
- The incubation phase
- The initial injury
- The exudate phase
- The convalescence phase
The stages of the inflammatory process in correct sequential order are:
- The initial tissue injury which can result from an infection or a traumatic cause
- The vascular response. The release of histamine, prostaglandins and kinins. These substances lead to vasodilation which increases the necessary blood supply to the injured tissue and the area surrounding
- The exudate response. The release of leukocytes, including macrophages and neutrophils, to the injured area to combat the infection.
The signs of infection such as the incubation, prodromal and convalescence stages, in the correct sequential order are:
- The incubation period
- The illness stage
- The convalescence stage
Health Promotion & Maintenance Practice Questions
- The infant had doubled their birth weight at twelve months.
- The infant had tripled their birth weight at twelve months.
- The mother reports that the infant is drinking 60 mLs per kilogram of its body weight.
- The infant had grown ¼ inch since last month.
The normal assessment data for the infant at 12 months of age is that the infant has doubled their birth weight at 12 months of age.
The mother’s reports that the infant is drinking 60 mLs per kilogram of its body weight and the fact that the infant had grown ¼ inch since last month are not normal assessment data. Infants are fed breast milk or formula every two to four hours with a total daily intake of 80 to 100 mLs per kilogram of body weight.
As the neonate grows, they gain five to seven ounces during the first six months and then they double their birth weight during the first year; the head circumference increases a half inch each month for six months and then two tenths of an inch until the infant is one year of age. Similarly, the height or length of the newborn increases an inch a month for the first 6 months and then 1/2 inch a month until the infant is 1 year of age.
- The Programmed Longevity Theory
- The Immunological Theory of Aging
- The Endocrine Theory
- The Rate of Living Theory
The theory of aging that supports your belief that strict infection control prevention measures are necessary is the Immunological Theory of Aging. The Immunological Theory of Aging states that aging leads to the decline of the person’s defensive immune system and the decreased ability of the antibodies to protect us against infection.
The Programmed Longevity Theory of aging states that genetic instability and changes occur such as some genes turning on and off lead to the aging process; the Endocrine Theory of aging states that aging results from hormonal changes and the biological clock’s ticking; and Rate of Living Theory states that one’s longevity is the result of one’s rate of oxygen basal metabolism.
Other theories of aging are:
- Wear and Tear Theory: This theory describes aging as a function of the simple wearing out of the tissues and cells as one ages.
- Cross Linking Theory: This theory of aging explains that aging results for cell damage and disease from cross linked proteins in the body.
- Free Radicals Theory: This theory is based on the belief that free radicals in the body lead to cellular damage and the eventual cessation of organ functioning.
- Somatic DNA Damage Theory: Somatic DNA Damage theory is based on the belief that aging and death eventually occur because DNA damage, as continuously occurs in the human cells, continues to the point where they can no longer be repaired and replaced and, as a result, they accumulate in the body.
- Increased creatinine clearance.
- Impaired immune system.
- Decreased hepatic metabolism.
- Increased bodily fat.
The elderly population is at risk for more side effects, adverse drug reactions, and toxicity and over dosages of medications because the elderly have a decrease in terms of their hepatic metabolism secondary to the hepatic functioning changes of the elderly secondary to a decreased hepatic blood flow and functioning.
The elderly have decreased rather than increased creatinine clearance; the immune system is also decreased in terms of its functioning, however, this change impacts on the elderly’s ability to resist infection rather than impacting a medication’s side effects, adverse drug reactions, toxicity and over dosages; and, lastly, a decrease in terms of bodily fat, rather than an increase in terms of bodily fat impacts on medications. The distribution of drugs is impaired by decreases in the amount of body water, body fat and serum albumin; drug absorption is decreased with the aged patient’s increases in gastric acid pH and decreases in the surface area of the small intestine which absorbs medications and food nutrients.
The expected date of delivery is calculated using Nagle’s rule which is:
The first day of last menstrual period – 3 months + 7 days = the estimated date of delivery
For example, when the first day of the last menstrual period is 10/20/2016 you would:
- Subtract three months from 10/20/2016 and then you get 7/20/2016 and then
- Add seven days to 7/20/2016 and then get 7/27/2016, after which you would
- Add one year to 7/27/2016 to get the estimated date of delivery for7/27 of the following year which is 7/27/2017.
- You should explain that fetal lie is where the fetus’ presenting part is within the birth canal during labor, among other information about the other assessments.
- You should explain that fetal presentation is the relationship of the fetus’s spine to the mother’s spine, among other information about the other assessments.
- You should explain that fetal attitude is the relationship of the fetus’ presenting part to the anterior, posterior, right or left side of the mother’s pelvis, among other information about the other assessments.
- You should explain that fetal station is the level of the fetus’ presenting part in relationship to the mother’s ischial spines, among other information about the other assessments.
You should explain that fetal station is the level of the fetus’ presenting part in relationship to the mother’s ischial spines. Fetal station is measured in terms of the number of centimeters above or below the mother’s ischial spines. Fetal station is -1 to -5 when the fetus is from 1 to 5 centimeters above the ischial spines and it is from +1 to +5 when the fetus is from 1 to 5 centimeters below the level of the maternal ischial spines.
Fetal lie is defined as the relationship of the fetus’s spine to the mother’s spine. Fetal lie can a longitudinal, transverse or oblique life. Longitudinal lie, the most common and normal lie, occurs when the fetus’ spine is aligned with the mother’s spine in an up and down manner; a transverse lie occurs when the fetus’ spine is at a right ninety degree angle with the maternal spine; and, lastly, an oblique lie occurs when the fetus’ spine is diagonal to the mother’s spine.
Fetal presentation is defined by where the fetus’ presenting part is within the birth canal during labor. The possible fetal presentations are the cephalic presentation, the cephalic vertex presentation, the cephalic sinciput presentation, the cephalic face presentation, the cephalic brow presentation, the breech presentation, the complete breech presentation, the frank breech presentation, the shoulder breech presentation, and the footling presentation.
Fetal attitude is the positioning of the fetus’s body parts in relationship to each other. The normal attitude is general flexion in the “fetal position”. All attitudes, other than the normal attitude, can lead to a more intense and prolonged labor.
Fetal position is the relationship of the fetus’ presenting part to the anterior, posterior, right or left side of the mother’s pelvis.
- You should apply the principles of initiative when caring for preschool children.
- You should apply the principles of sensorimotor thought when caring for preschool children.
- You should apply the principles of intimacy when caring for the adolescent.
- You should apply the principles of concrete operations when caring for the adolescent.
You should apply the principles of initiative when caring for preschool children. The developmental task for preschool children is initiative, according to Eric Erickson.
The other developmental tasks, according to Eric Erickson are:
- Infant: Trust
- Toddler: Autonomy
- School Age Child: Industry
- Adolescent: Identity formation
- Young Adult: Intimacy
- Middle Aged Adult: Generativity
- Older Adults: Ego integrity
In the correct sequential order, Jean Piaget’s levels of cognitive development include:
- Sensorimotor thought: Infancy to About 2 Years of Age
- Preoperational and symbolic functioning: From 2 to 7 Years of Age
- Concrete operations: 7 to 11 Years of Age
- Formal operations: 12 Years of Age
- Childhood immunizations
- Separation anxiety
The expected life transition should you apply into your practice for these pediatric clients as you are caring for pediatric clients of all ages is puberty.
Throughout the life span, there are several significant expected life transitions that require the person to cope and adjust. Some of these expected life transitions include puberty, maternal and paternal attachments and bonding to the neonate, pregnancy, care of the newborn, parenting, and retirement.
Although young children will experience separation anxiety and they will also be maintained on an immunization schedule, these are not expected life changes.
- The Biophysical Dimension
- The Psychological and Emotional Dimension
- The Spiritual Dimension
- The Health Systems Dimension
The Dimensions Model of Health includes six dimensions that impact on the client, including the community. The Spiritual Dimension is not one of these six dimensions.
These dimensions are the:
- Biophysical Dimension
- Psychological and Emotional Dimension
- Health Systems Dimension
- Behavioral Dimension
- Socio-Cultural Dimension
- Physical Environment Dimension
- Mediterranean ethnicity for cystic fibrosis.
- African American ethnicity for Tay Sachs disease.
- British Isles ethnicity for psychiatric mental health disorders.
- Saudi Arabian ethnicity for sickle cell anemia.
You would identify a client who is of Saudi Arabian ethnicity for sickle cell anemia. Other ethnicities at greatest risk for sickle cell anemia include those who are African, Latin Americans, Southern Europeans and some clients from some Mediterranean nations.
Other disorders and diseases and the ethnicities associated with them are listed below
- Thalassemia: Clients with a Mediterranean ethnicity
- Tay Sachs Disease: Ashkenazi Jewish people
- Cystic Fibrosis: Clients with a European ethnicity
- Psychiatric Mental Health Disorders: African Americans and Native Americans
- Hypertension: African Americans, Pacific Islanders , Native Americans, Alaskan natives, Hispanic and Caribbean clients
- Diabetes: African Americans, Caribbeans, Native Americans and clients from India, Pakistan and Bangladesh
- Cancer: Caucasians and clients from Scotland and Ireland
- The need for a targeted assessment is based on the application of the nurse’s knowledge of pathophysiology and the presenting symptoms.
- The need for a targeted assessment is based on the application of the nurse’s knowledge of developmental needs and developmental delays.
- Targeted assessment is done on an annual basis for existing clients rather than a complete assessment that is done for new clients.
- Targeted assessments consist of a brief medical history and a complete assessment consists of a complete health history and a complete physical assessment.
The need for a targeted assessment is based on the application of the nurse’s knowledge of pathophysiology and the presenting symptoms. Targeted assessments and screenings are done in addition to routine and recommended screenings when a particular disorder has a genetic pathophysiological component for risk and when a client is presenting with a particular sign or symptom.
For example, a targeted assessments relating to nutritional status may be indicated when an infant or young child is listless and not gaining weight according the established criteria; an adolescent may be target screened for visual acuity when a high school teacher reports that the teen does not seem to be able to read things on the blackboard; and a toddler may be target screened when the parent reports that the child is not responding to their name.
- Genetic predisposition
- Lifestyle choices
- High risk behaviors
- An external locus of control
Life style choices are the risk factors that are most likely able to be corrected. Poor life style choices place a person at risk and they are often considered also risky behaviors.
As discussed before, some risks are preventable and correctable and others are not. For example, genetics, age and gender are NOT modifiable risks, but the risks associated with life style choices are modifiable, correctable and able to be eliminated when the person changes their behavior in reference to these risky behaviors.
Some risky life style choices include:
- Excessive sun exposure
- The lack of regular exercise
- A poor diet
- Cigarette smoking and the use of other tobacco products
- Alcohol use
- Illicit drug use
- Unprotected sex
- Avocational and hobby choices such as rock climbing
- Inadequate sleep and rest
Genetic predisposition is an innate and not correctable risk factor and an external locus of control can lead to poor life style choices, however, this is not the most likely correctable risk factor.
- A transdermal contraceptive patch
- A diaphragm
- A vaginal contraceptive ring
You would not recommend any of the above methods of contraception for this family.
You would not recommend the use of a transdermal contraceptive patch or a vaginal contraceptive ring for the couple because both of these contraceptive methods are contraindicated when the woman has a history of deep vein thrombosis and cigarette smoking; and you would also not recommend a diaphragm because the compliance of this couple cannot trusted because the couple has a history of the lack of adherence to medical regimens.
- Information about the lack of scientific evidence regarding the effectiveness of all herbs.
- Data to support the fact that magnets can be effective in terms of fibromyalgia pain, and as such, may be a good choice for this client.
- Research that suggests that prayer is an effective alternative method to relieve pain and stress that can be helpful to this client.
- Information that contraindicates the use of biofeedback because this alternative, complementary health practice can interfere with the client’s pacemaker functioning.
Scientific data now indicates that prayer is effective for the relief of stress, anxiety and pain, and as such, may be helpful to this client.
Some herbs, minerals and supplements are scientifically deemed as safe and effective and others are not scientifically effective and they can also lead to harm; at the current time, the National Institutes of Health (NIH) states that magnets are not scientifically effective and they are also not considered safe for clients with a pacemaker or insulin pump because these internally implanted devices can be adversely affected by the magnetic force of the magnet; and, lastly, biofeedback does not interfere with the client’s pacemaker functioning.
- A social worker
- A physical therapist
- An occupational therapist
- A speech therapist
The healthcare professional would you most likely refer this family to in order to address this deficit in terms of their instrumental activities of daily living (ADLs) is a social worker.
The activities of daily living are differentiated in terms of the basic activities of daily living and the instrumental activities of daily living. Examples of basic activities of daily living include things like bathing, mobility, ambulation, toileting, personal care and hygiene, grooming, dressing, and eating. Deficits in terms of the basic activities of daily living are best addressed by a physical and/or occupational therapist.
The instrumental activities of daily living are more advanced than the basic activities of daily living. The instrumental activities of daily living include things like grocery shopping, housework, meal preparation, the communication with others using something like a telephone, and having transportation. Deficits in terms of the instrumental activities of daily living are best addressed by a social worker. For example, the social worker may assist the client in terms of their transportation and they can also teach the client about how to grocery shop, for example.
- Olfactory Cranial Nerve: The sensory nerve that transmits the sense of smell to the olfactory foramina of the nose
- Optic Cranial Nerve: This sensory nerve transmits the sense of vision from the retina to the brain.
- Oculomotor Cranial Nerve: This motor and sensory nerve controls eye movements and visual acuity.
- Trochlear Cranial Nerve: This motor nerve innervates eye ball movement and the superior oblique muscle of the eyes.
- Abducens Cranial Nerve: This motor nerve innervates and controls the abduction of the eye using the lateral rectus muscle.
- Facial Cranial Nerve: This motor nerve controls facial movements, some salivary glands and gustatory sensations from the anterior part of the tongue.
- Glossopharyngeal Cranial Nerve: This sensory nerve This nerve gives us the sense of taste from the posterior tongue, and it also innervates the parotid glands
Correct Response: A,B,D,E
The olfactory cranial nerve is a sensory nerve that transmits the sense of smell to the olfactory foramina of the nose; the optic cranial nerve is also a sensory nerve and it transmits the sense of vision from the retina to the brain.
The trochlear cranial nerve is a motor nerve that innervates eye ball movement and the superior oblique muscle of the eyes; and the abducens cranial nerve is a motor nerve that innervates and controls the abduction of the eye using the lateral rectus muscle.
The oculomotor cranial nerve is a motor nerve controls eye movements, the sphincter of the pupils and the ciliary body muscles; it has no sensory function. The facial cranial nerve is a motor and sensory nerve which controls facial movements, some salivary glands and gustatory sensations from the anterior part of the tongue. And, lastly, the glossopharyngeal cranial nerve is both a motor and sensory nerve that gives us the sense of taste from the posterior tongue, and it also innervates the parotid glands.
- The Taylor test
- The Rinne test
- The Babinski test
- The APGAR test
The sense of hearing is assessed using the Rinne test and the Weber test and a tuning fork.
A Taylor hammer, not a Taylor test, is used to check reflexes like the biceps and triceps reflexes; the Babinski sign occurs when the foot goes into dorsiflexion and the great toe curls up; this sign is an abnormal response to this stimulation and it can indicate the presence of deep vein thrombosis. And lastly, the APGAR test is used to assess the neonate immediately after birth in terms of the infant’s appearance, grimace and reflexes, appearance in terms of skin color, and respiratory rate and effort.
- Light palpation
- Deep palpation
Deep palpation is cautiously done after light palpation when necessary because the client’s responses to deep palpation may include their tightening of the abdominal muscles, for example, which will make the light palpation less effective for this assessment, particularly if an area of pain or tenderness has been palpated.
Inspection is typically the first step and percussion of the abdomen should be done prior to any palpation, particularly deep palpation.
The five types of sounds that are elicited during percussion are flatness, resonance, hyperresonance, tympany and dullness. Dullness is heard when percussion is done over a solid organ like the liver and spleen.
Flatness is normally assessed over muscles and bones; resonance is a hollow sound that is heard, for example, over the air filled lungs; and hyperresonance, which is a booming sound that is heard over abnormal lung tissue, as occurs among clients with chronic obstructive pulmonary disease (COPD); and, lastly, tympany is heard over the stomach with air as a drum like sound.
- A complete medical history, a general survey and a complete physical assessment.
- A complete medical history, a general survey and a focused physical assessment.
- A client interview, a significant other interview, a general survey and a complete physical assessment.
- A client interview, a significant other interview, a general survey and a focused physical assessment.
A comprehensive health assessment includes a complete medical history, a general survey and a complete physical assessment.
Although a complete medical history is done using a client interview and a significant other interview for much data, it is the health history and not the interview that is part of the comprehensive health assessment. A focused assessment is done as based on some pathology, sign or symptom and it is not considered a part of a comprehensive health assessment.
- Tympany: A hollow sound
- Dullness: A thud like sound
- Dullness: A hollow sound
- Resonance: A booming sound
Dullness is a thud like sound and not a hollow sound. Tympany is a drum like sound; and resonance is a hollow sound.
Psychosocial Integrity Practice Questions
- A couple which consists of a husband and wife both of whom are affected with Alzheimer’s disease
- A poverty stricken couple without any healthcare resources in the community
- A pregnant woman and a husband who was physically abused as a young child
- A wealthy couple with feelings that they are immune from punishment and above the law
A pregnant woman and a husband who was physically abused as a young child is the couple is at most risk for domestic violence because pregnancy and a personal prior history of abuse are two commonly occurring risk factors among abused woman and male abusers, respectively.
Current research indicates that abuse and neglect affect all people of all ages and of all socioeconomic classes including the wealthy as well as the poverty stricken.
Other patient populations at risk of abuse and neglect include female gender, infants, children, the cognitively impaired, the developmentally challenged, the elderly and those with physical or mental disabilities; some of the other traits and characteristics associated with abusers include substance related use and abuse, a psychiatric mental health disorder, poor parenting skills, poor anger management skills, poor self-esteem, poor coping skills, poor impulse control, immaturity, and the presence of a current crisis.
- Restrain the client
- Place the client in seclusion
- Get an order for a sedating medication
- Establish trust with the client.
The first thing that you should do to prevent violence towards others is to establish trust with the client. The first step in the nurse-client relationship is to establish trust in this therapeutic relationship. Without trust future collaboration, interventions and client outcomes cannot be accomplished to facilitate appropriate and safe behaviors.
Restraints and seclusion are not indicated until others are in imminent danger because of this client’s current violent behaviors and not a history of it. Lastly, sedating medications to prevent violence are also not the first things that are done.
- Psychological dependence secondary to amphetamine use
- Substance abuse secondary to amphetamine use
- Addiction secondary to amphetamine use
- Physical dependence secondary to amphetamine use
The appropriate nursing diagnosis for this client is “Psychological dependence secondary to amphetamine use”. Psychological dependence is defined as the person’s need to continue the use of the substance to avoid any unpleasant feelings and experiences that can occur when the substance is not taken. Amphetamines and hallucinogenic drugs like LSD are often associated with psychological dependence.
Substance abuse, simply defined, is one’s overindulgence of an addictive substance which can be alcohol, prescription drugs and/or illicit, illegal drugs. Substance abuse does not include prescribed medications, such as narcotic pain medications, that are being used for medical reasons; however, these same medications when used after there is no longer a medical need to use them is considered substance abuse.
Addiction is defined as the unending and constant need for the person to have the chosen substance even when the use of the substance causes the client to have serious physical, psychological, social and/or economic consequences and harm including a loss of control over the substance abuse and use. Contrary to popular opinion, addiction can occur with and without physical dependence.
Physical dependence occurs when the cessation of a drug causes adverse physical effects; these ill effects are typically greater and more intense when the cessation of the drug is rapid and abrupt. Some of the drugs that are most often associated with physical dependence include cocaine, opioid drugs, alcohol and benzodiazepines. As previously stated, physical dependence does not necessarily indicate addiction; addiction can be present with or without any physical dependency.
- Orem’s Self Care Model
- Nagi's Model
- A cognitive model of disability
- A biomedical model of disability
Nagi’s Model of disability model describes disabilities and its limitations are the result of a discrepancy between the client’s abilities and the limitations of the physical and social environment within which the client lives.
Although clients with disabilities should be assessed and have interventions related to their self care abilities, Dorothea Orem’s Self Care Model is not a model of disability. This model describes self care needs and abilities as wholly compensatory, partly compensatory and supportive educative.
Cognitive models of disability focus on the importance of affected client’s ability to remain as independent as possible and ways that the empowered client can exercise their own self-determination, confidence, self efficacy, and control.
Lastly, biomedical models address pathology, impairments and the manifestations of impairments that can be cured or lead to death.
The characteristics of the stages or phases of crisis, in the correct sequential order, are:
- Level 1 Crisis Signs and Symptoms: Patients experiencing a level one crisis typically experience anxiety and they also typically begin to use one or more psychological ego defense mechanisms.
- Level 2 Crisis Signs and Symptoms: Patients experiencing a level two crisis most likely exhibit some loss of their ability to function. They may also try to experiment with alternative methods of coping in order to deal with the crisis that is not being effectively coped with using one’s currently used coping mechanisms.
- Level 3 Crisis Signs and Symptoms: Patients experiencing a level three crisis show the signs and symptoms of the General Adaptation Syndrome which is characterized with fight, flight and panic as discussed above under the section entitled “Coping Mechanisms: Introduction”.
- Level 4 Crisis Signs and Symptoms: Clients experiencing a level four crisis exhibit severe signs and symptoms such as being totally detached and removed from others, feeling overwhelmed, becoming disoriented, and even with thoughts of violence toward self and others.
- Displacement
- Sublimation
- Dissociation
- Reaction formation
Dissociation is the psychological ego defense mechanism occurs when the client detaches and dissociates with person or time to avoid the stress until they are ready to cope with it.
Displacement transforms the target of one’s anger and hostility from one person to another person or object. Displacement allows the person to ventilate and act out on their anger in a less harmful and a more socially acceptable manner.
A client uses the ego defense mechanism of sublimation when they transform and replace unacceptable urges and feelings into a socially acceptable urge or feeling.
A client is using reaction formation when the client acts and behaves in a manner that is completely the polar opposite of their true feelings.
- Jean Watson's
- Martha Rogers'
- Nagi's theory
- Madeleine Leininger’s theory
The theoretical framework that you would recommend that this committee should consider when addressing mutiethnicity and the culturally diverse nature of this facility for this philosophy is Madeleine Leininger’s theory.
Madeleine Leininger’s theory of Transcultural Nursing and her book “Culture Care Diversity and Universality: A Theory of Nursing” “searches for comprehensive and holistic care data relying on social structure, worldview, and multiple factors in a culture in order to get a holistic knowledge base about care” (Leininger, 2006, p. 219)
Jean Watson’s Jean Watson developed the Human Caring Theory which states that caring is the essence of nursing. Watson's theory has the four major concepts of health, nursing, society/environment and human being. Caring consists of the following 10 nursing interventions that demonstrate genuine caring.
Martha Rogers’ theory is the Science of Unitary Human Beings which is based on general systems theory without any focus on multiethnicity and cultural diversity; and lastly, Nagi’s Model of disability model describes disabilities and its limitations are the result of a discrepancy between the client’s abilities and the limitations of the physical and social environment within which the client lives.
- The client will accept impending death
- Guilt related to past transgressions
- Spiritual distress related to guilt
- Pain related to end of life symptoms
“The client will accept impending death” is the client goal would be the most likely appropriate and expected for the vast majority of these clients. In fact, one of the primary goals of hospice and palliative care is to facilitate the client’s and family member’s acceptance.
Other goals are the freedom for guilt, spiritual distress and pain at the end of life; therefore, these diagnoses are not expected.
- The client will be free of constipation
- The client will remain free of pain and distress
- The administration of an antiemetic to prevent vomiting and further dehydration
- The administration of an enema to correct the constipation
Based on this client’s signs and symptoms and the fact that the client is expected to die in a day or two, the appropriate client outcome for this client is that the client will remain free of pain and distress.
“The client will be free of constipation” requires interventions such as an enema which are not indicated when death is imminent unless, of course, the client is adversely affected with pain and discomfort as the result of it which is not the case with this client. Additionally, the administration of an antiemetic to prevent vomiting is not indicated because there is no evidence in this question that the client is actually vomiting.
- “You should try to come to a few sessions at least because they may be very informative to you”.
- “You are probably correct. This really is not your problem”.
- “Despite the fact that it is your grandson’s drug addiction, situations such as this affect all members of the family including grandparents who live in the home.”
- "You should attend because the doctor has ordered family therapy for you as extended family members”.
You should respond to the grandparents’ statement with “Despite the fact that it is your grandson’s drug addiction, situations such as this affect all members of the family including grandparents who live in the home”.
After this statement, you should also educate the grandparents about the fact that group and family therapy is often indicated when the family unit is affected with stressors and dysfunction because family members may not fully understand the need for the entire family unit to participate when only one member of the family is adversely affected with a stressor and poor coping and that all family members are affected when only one member of the family unit is adversely affected.
You would NOT state “You should try to come to a few sessions at least because they may be very informative to you” because these sessions are therapeutic and not educational; you would not state “You are probably correct. This really is not your problem” because this statement is not true; and you should also not state “You should attend because the doctor has ordered family therapy for you as extended family members” because this is not the real reason why attending these sessions is needed.
- Engel's theory
- Kubler Ross' theory
- Lewin's theory
- Warden's theory
The theory of grief and loss would you most likely integrate into your practice as you perform this role is Warden’s Four Tasks of Mourning. This theory has four tasks that people go through after the loss of a loved one. These tasks are accepting the loss, coping with the loss, altering, modifying and changing the environment to cope with and accommodate for the absence of the lost person, and, finally, resuming one’s life while still having a healthy connection with the loved one.
Engel’s Stages of Grieving include stages both prior to and after a loss and these stages are:
- Shock and disbelief
- Developing awareness
- Restitution
- Resolving the loss
- Idealization
Kubler Ross’s Stages of Grieving occur prior to the death and these stages include:
Lastly, Lewin developed theories of change, leadership and conflict and NOT a theory related to grief after the loss of a loved one.
- The concern related to the client’s cultural reluctance to report psychological symptoms because of some possible culturally based stigma associated with psychiatric mental health disorders
- Concerns revolving around the lack of financial and health insurance resources to pay for psychological care
- Concerns related to the compliance with psychological treatment regimens because of the client’s lack of social support systems
- The concern related to the culturally based client apathy about nursing care and nursing assessments
The concern related to the client’s cultural reluctance to report psychological symptoms because of some possible culturally based stigma associated with psychiatric mental health disorders which is a barrier to assessment because the client fears being stigmatized and rejected when divulging psychological data including anxiety and other symptoms.
The lack of financial and health insurance resources to pay for psychological care, the lack of social support systems, and the client’s apathy are barriers to psychological care but these factors are not a barrier to a psychological assessment and these factors are not cultural, but instead social and psychological.
- Cognitive psychotherapy
- Behavioral psychotherapy
- Cognitive behavioral psychotherapy
- Psychoanalysis
Behavioral psychotherapy is particularly useful among clients who are adversely affected with phobias, substance related disorders, and other addictive disorders. Some of the techniques that are used with behavioral therapy include operant conditioning as put forth by Skinner, aversion therapy, desensitization therapy, modeling and complementary and alternative stress management techniques.
Cognitive psychotherapy is most often used to treat clients, including groups of clients, with depression, eating disorders, anxiety, and anxiety disorders to facilitate the altering of the clients’ attitudes and perspectives relating to stressors.
Cognitive behavioral psychotherapy, which is a combination of cognitive psychotherapy and behavioral psychotherapy and also referred to as dialectical behavioral therapy is most often used for clients affected with a personality disorder and those at risk for injury and harm to self and/or others.
Psychoanalysis, in contrast to cognitive behavioral therapy and other individual and group therapies, dives into the client’s subconscious and it often focuses on the past as well as the client’s current issues. This therapy is not conducted by registered nurses but, instead, by experienced psychotherapists.
The client religion that is the most pertinent to the role of the admissions coordinator of hospital who assigns the rooms and beds of clients who will be admitted is the Islam religion which requires that the followers face Mecca for daily prayer, therefore, Islam clients should be placed in a room that faces the holy city of Mecca.
Although most religions impact on the care of the client, only Islam is pertinent to the admissions coordinator. Other religions practices and their impact on health care are shown below:
- Christians: End of life rituals like the Sacrament of the Sick, baptisms for newborns, fasting, and the Eucharist.
- Judaism: Religious based circumcisions, a kosher diet which separates dairy foods from meat based foods, and death rituals called a Shiva.
- Hinduism: Many followers are vegetarian; personal hygiene is paramount and they also have death rituals without the prolongation of life.
- Mormonism: Baptism for the newborn, last rites at the time of death, communion, and burials of the dead. Additionally, the Mormon religion prohibits alcohol, tobacco, and caffeine.
- Jehovah’s Witnesses: Prohibitions against blood transfusions, foods containing blood, homosexuality, sex before marriage, abortion, suicide, gambling, alcoholic beverages, tobacco and illicit drugs.
- Psychotic symptoms related to sensory overload
- Psychotic symptoms related to a previously undiagnosed psychosis
- Visual disturbances related to dementia
- Visual disturbances related to delirium
“Visual disturbances related to delirium” is the most appropriate nursing diagnosis for this client, as based on their signs, symptoms, past history and current medical status.
Delirium is characterized with a sudden and abrupt onset of episodic and intermittent periods of time vacillating between periods of impaired cognition and periods of mental clarity. Visual hallucinations are a sign of delirium and delirium can result from a number of different causes including dehydration and anticholinergic medications.
The signs and symptoms of sensory overload do not include visual hallucinations and a sudden and abrupt onset of episodic and intermittent periods of time vacillating between periods of impaired cognition and periods of mental clarity. Instead, the signs and symptoms of sensory overload include anxiety, restlessness, sleep deprivation, fatigue, poor problem solving and decision making skills, poor performance, and muscular tension.
There is no evidence in this question that the client has psychotic symptoms related to a previously undiagnosed psychosis; all the evidence substantiates the suspicion that the client is affected with delirium.
Lastly, dementia has a gradual and progressive onset rather than an abrupt and sudden onset.
- Collect baseline blood pressure readings prior to the beginning of this educational series and then collect and compare blood pressure data during the series and after the series is completed.
- Collect baseline blood pressure readings prior to the beginning of this educational series and then collect and compare blood pressure data after the series is completed.
- Ask the clients how often they use the stress management techniques that they have learned during this educational series.
- Use a questionnaire at the end of the series that asks the participants how they liked the class and what they learned during this educational series.
The best way to evaluate the effectiveness of this educational series is to collect baseline blood pressure readings prior to the beginning of this educational series and then collect and compare blood pressure data during the series and after the series is completed. This technique entails evaluating the outcomes of the education in terms of changes in the client and it also includes formative evaluation during the series and summative evaluation at the end of the series.
Collecting baseline blood pressure readings prior to the beginning of this educational series and then collecting and comparing blood pressure data after the series is completed gives us only summative evaluation; it does not provide you with formative evaluation.
Because the primary goal of this series is to lower the blood pressures of clients through the use of stress management techniques, asking the clients how often they use the stress management techniques that they have learned during this educational series and using a questionnaire at the end of the series that asks the participants how they liked the class and what they learned during this educational series does not reflect data and information about the effectiveness of the classes in terms of reducing the blood pressures of hypertensive clients.
Tai Chi is a type of a mind body exercise that deeply focuses on breathing, movement and meditation. Yoga is similar to tai chi in that yoga also employs a combination of breathing, movement and meditation.
Reiki is done for the client when the therapist places their hands on or near the person’s body to promote the client’s energy field and its own natural healing processes. Feng shui is an eastern method of decorating using colors, items and the placement of objects in the environment to promote a harmonious relationship of man and its environment; and lastly Jiu Jitsu is a martial art.
- You should advise the couple to move closer to their children so that they can care for their father.
- You should teach the wife about this progressive disease and the need to promote as much independence as possible.
- You should teach the wife about this progressive disease and the need to do all that she can for the husband to avoid his depression and frustration.
- You should advise the couple to decrease their social activities in order to preserve the husband’s dignity and self-esteem.
You should teach the wife about this progressive disease and the need to promote as much independence as possible. Client’s with Alzheimer’s disease and other disabilities, including physical disabilities, should be coached and encouraged to be as independent as possible.
Moving closer to the children may not be appropriate advice particularly if the children are unable or unwilling to care for their father. Lastly, you should advise the couple to continue their social activities and to only avoid those situations where the necessary compassion and understanding about the client and his condition are absent.
- According to the Global Deterioration Scale, clients in the first stage of Alzheimer’s disease tend to cover up their failing abilities
- According to the Reisberg Scale, clients in the first stage of Alzheimer’s disease tend to cover up their failing abilities
- According to the Global Deterioration Scale, clients in the third stage of Alzheimer’s disease tend to cover up their failing abilities
- According to the Reisberg Scale, clients in the fourth stage of Alzheimer’s disease tend to cover up their failing abilities
According to the Global Deterioration Scale, also referred to as the Reisberg Scale, clients in the third stage of Alzheimer’s disease tend to cover up their failing abilities.
The Global Deterioration Scale stages Alzheimer’s according to seven stages. These stages include
- Stage 1: Cognitive abilities are intact.
- Stage 2: Minimal and hardly noticeable forgetfulness occurs.
- Stage 3: Mild changes in terms of cognition occur. The client may have difficulty in terms of their memory, which at times the client may “cover up” to avoid the detection by others. The signs and symptoms of this stage are similar to those of the Early Stage of Alzheimer’s disease, as discussed immediately above.
- Stage 4: This stage is characterized with increasing confusion about recent events and conversations, mild problems with math and some rather routinized sequential tasks such as cooking. The client may withdraw from others and debate the fact that they are having some cognitive issues.
- Stage 5: Early Dementia occurs. Short and long term memory losses, a lack of orientation to place and time, poor judgment, and some of the client’s self care in terms of the activities of daily living become progressively more problematic. The client may need the assistance and supervision of others to promote the client’s highest possible level of independence in the performance of their basic activities of daily living.
- Stage 6: This stage is referred to a Middle Dementia and moderately severe Alzheimer’s disease. There is almost complete short term and long term memory loss, communication is highly limited and it may only consist of nonverbal behavioral responses, and the client needs complete care to manage their activities of daily living. Sundowner’s syndrome is present and hallucinations as well as agitation may occur.
- Stage 7: This stage is referred to as Late or Severe Dementia and Failure to Thrive. The client is in need of complete care; and immobilization, in addition to the hazards of immobility, may affect the client and the family members at this stage.
- Probing for more information from the client
- Sublimation to determine hidden messages
- Providing privacy so the client is comfortable
- Silence to allow contemplation and thought
- A safe environment of care that is conducive to the prevention of medical errors.
- A client care area that provides personal privacy and the confidentiality of medical information.
- A European method of design and color to promote health and wellness.
- The provision of a therapeutic environment of consistency to promote health.
A therapeutic milieu eliminates as many stressors from the environment as possible. The goal of this environment is to facilitate the client’s coping and recovery without the need to cope with these extraneous and avoidable stressors. Some of the elements of a therapeutic milieu environment include consistency, client rules, limitations and boundaries, and client expectations, including contracts, relating to appropriate behavior.
Physiological Integrity: Basic Care & Comfort Practice Questions
- Psychomotor domain: The client will slightly bend their elbows when holding the hand grips.
- Psychomotor domain: The client will rest their weight on the padded areas on the top of the crutches.
- Cognitive domain: The client will slightly bend their elbows when holding the hand grips.
- Cognitive domain: The nurse will tell the client how often the tips on the crutches must be replaced.
The client goal that is paired with its learning domain that should be included in the patient teaching plan for this client and the parents is “The client will slightly bend their elbows when holding the hand grips” which is part of the psychomotor domain and not the cognitive domain. Lastly, the “nurse will” is an intervention and not a client goal or expected outcome which should be learner, not nurse, oriented.
- An aphasia aid
- A button hook
- Honey thickened liquids
- A word board
The basic activity of daily living assistive device can be useful for the client who is affected with poor fine motor coordination is a button hook that would be used for the dressing activity of daily living.
An aphasia aid and a word board are assistive devices to facilitate communication when the client is affected with a communication deficit such as aphasia; and, lastly honey thickened liquids are indicated for clients with a swallowing disorder and they are not indicated for clients with poor fine motor coordination.
- Place the client in a wheelchair to protect their safety in the clinic.
- Remove the cane from the client to protect their safety.
- Teach the client about the proper length of a cane.
- Have the client use a wheelchair rather than the cane.
You should teach the client about the proper length of a cane. The proper length of the cane should be the length that only permits the client’s elbow to be slightly flexed. Some canes like a wooden cane are not adjustable to the client’s height and others can be adjusted to meet the height needs of the client.
You would not place the client in a wheelchair or ask the client to use a wheelchair and you would also not take the cane, which is their personal property, away from them. You would use this observation as a learning need assessment and, as such, you should teach the client about the proper length of a cane and help them to adjust the height of the cane if the client’s cane is a height adjustable one.
- A cleansing enema
- A retention enema
- A return-flow enema
The most likely intervention for this client, after getting a doctor’s order, is a return flow enema. Return-flow enemas, similar to a carminative enema, are used to relieve flatus and stimulate peristalsis which is frequently a problem after a client has received anesthesia.
Cleansing enemas are used to relieve constipation; and a retention enema is used to administer a medication, to soften stool and to lubricate the rectum so that it is easier and more comfortable for the client to defecate.
Finally, the data in this question does not indicate that the client is constipated and in need of a laxative.
- Both can lead to infection.
- Both are invasive procedures.
- Both are considered sentinel.
- Both are the last resort.
The commonality that is shared in terms of both restraints and urinary catheters is that both are the last, not the first, treatment of choice. Both indwelling urinary catheters and restraints pose risks and complication; therefore, both of these interventions must be prevented with the use of preventive measures.
Indwelling urinary catheters are invasive but restraints are not invasive; indwelling urinary catheters can lead to infection but restraints do not. Lastly, neither are sentinel. A sentinel event is an event or occurrence, incident or accident that has led to or may have possibly led to client harm. Even near misses, that have the potential for harm, are considered sentinel events because they have the potential to cause harm in the future.
- Any solid skin barrier
- A hydrocolloid solid skin barrier
- Hollister’s Flextend
- A skin sealant
You would recommend a skin sealant, including products like Bard’s Protective Barrier and Convatec’s Allkare, which are a fast drying polymer transparent film that can be applied relatively simply with a wipe or a spray. These products are easy to use and less expensive than solid skin barriers, including Hollister’s Flextend and others containing hydrocolloids.
- A prolapsed stoma
- A vitamin B12 deficiency
- Nocturnal enuresis
- GI stone formation
Some of the complications associated with a colostomy include a prolapsed stoma, infection, dehiscence, an ischemic ileostomy, a peristomal hernia, stoma stenosis, stomal retraction, necrosis, mucocutaneous separation, stomal trauma, peristomal skin damage as the result of leakage and parastomal hernias.
A vitamin B12 deficiency, nocturnal enuresis and urinary stone formations are complications associated with urinary diversion and not fecal ostomy diversions.
- Bone demineralization: Turning and positioning every 2 hours
- Urinary stasis: The client will consume 1,000 mL of oral fluids per day
- Muscle atrophy: The client will perform range of motion exercises at least 3 times a day
- Hypercalcemia: Maintaining fluid intake of 1,000 mL per day
“The client will perform range of motion exercises at least 3 times a day” is an appropriate expected outcome of care that the nurse provides to prevent this complication.
Urinary stasis and hypercalcemia, both hazards of immobility, can be prevented when the client will consume 2,000 mL of oral fluids per day. Lastly, calcium loss from the bones can be prevented by weight bearing activity, and not turning and positioning in bed.
- 1 on the scale of 1 to 3
- 2 on the scale of 1 to 5
- 3 on the scale of 0 to 5
- 4 on the scale of 0 to 5
You would document this client’s muscular strength as a 3 on a scale of 0 to 5.
Muscular strength is classified on a scale of zero to five, as below.
- Zero: No muscular contraction
- One: No muscular movement, only a quiver is noted
- Two: Muscular movement but only when assisted with gravity
- Three: Muscular movement against gravity but not against resistance
- Four: Muscular movement against resistance
- Five: Full muscular movement and strength
You would document the size of this wound as 24 cm. After the wound is assessed and measured, the wound dimension is calculated by multiplying the length by the width by the depth of the wound. For example when the length of the sound is 3 cm deep, 2 cm long and 4 cm wide, it is calculated with 3 x 2 x 4 = 24 cm.
- Secondary intention healing
- Tertiary intention healing
- Primary prevention healing
- Secondary prevention healing
Secondary intention healing is the most likely type of wound healing for this client because of the risks associated with the deep infection associated with the ruptured appendix and the peritonitis.
Secondary intention healing, also referred to as healing by second intention, is done for contaminated wounds in order to prevent infections, to prevent the formation of abscesses and to promote healing from the bottom up to the outer surface of the skin so that any potential infection is not closed in at the bottom of the wound. These open wounds are irrigated with a sterile solution and then packed to keep them open and, over time, they will heal on their own. The resulting scar is more obvious than those scars that result from primary intention healing.
Primary intention healing is facilitated with wounds without infection. The wound edges are approximated and closed with a closure technique such as suturing, Steri Strips, and surgical glues.
Tertiary intention healing, also referred to as healing by tertiary intention, is a combination of secondary and primary healing. Tertiary intention healing begins with several days of open wound irrigations and packing, which is secondary healing, followed by the closure of the wound edges with approximation and suturing which is primary healing. Some traumatic wounds are healed with tertiary intention.
Primary, secondary and tertiary prevention strategies are prevention, interventions and restorative or rehabilitation care and not methods of wound healing.
- A barrier film
- An alginate dressing
- Surgical laser debridement
- Autolytic debridement
The treatment of pressure ulcers is complex and it often includes a combination of treatments and therapies. The RYB Color Code of Wounds is sometimes used by nurses to guide the treatment options. RYB stands for the colors of red, yellow and black. The rules of treatment for these three colors are:
- Red: Covering with a dressing such as a hydrocolloid film, turning and positioning the client and avoiding pressure, friction and shearing
- Yellow: Using an alginate dressing
- Black: Debridement, including surgical laser debridement, mechanical debridement, autolytic debridement, enzymatic debridement and sharp instrument debridement, of the area to remove the black necrotic eschar.
- Moritz Schiff’s theory of pain
- The Intensive Theory of Pain
- Melzack and Wall’s theory of pain
- The Specificity Theory of Pain
Melzack and Wall’s Gate Control Theory of pain supports the belief that some of the factors that open this “gate” to pain are low endorphins and anxiety and that some of the factors that close this “gate” to pain are decreased anxiety and fear. The substantia gelatinosa is the “gate” that facilitates or blocks the transmission of pain.
The Specificity Theory of Moritz Schiff described pain as a sensation that was different from all the other senses in that pain had its own specific nervous system pathways from the spinal cord that traveled to the brain; the Intensive Theory of pain is based on the belief that pain is an emotional state, rather than a sensory phenomenon; the Peripheral Pattern Theory of pain of Sinclair and Weddell describes pain as the result of an intense stimulus applied to the skin; and the Neuromatrix Theory of Pain supports the fact that pain is a dynamic and multidimensional process with physical, behavioral, perceptual, psychological and social responses and one that can only be described by the person who is experiencing it.
- Pain level, the quality of the pain, the region or area of the pain, the severity of the pain, and the pain triggers
- Precipitating factors, the quality of the pain, relief factors, the severity of the pain, and the pain triggers
- Pain level, the quantitative numerical pain score, the region or area of the pain, the severity of the pain, and the pain triggers
- Precipitating factors, the quality of the pain, the region or area of the pain, the severity of the pain, and the pain triggers
Precipitating factors, the quality of the pain, the region or area of the pain, the severity of the pain, and the pain triggers are the PQRSTs of the PQRST method of pain assessment.
The severity of the pain, which can include a quantitative, numerical pain score from 1 to 10, for example, is the S of the PQRST method of pain assessment.
- Assessment data, biochemical data, clinical data and dietary data
- Ancestral cultural data, biochemical data, clinical data and dietary data
- Anthropometric data, biological data, chemical data and dietary data
- Anthropometric data, biochemical data, clinical data and dietary data
Anthropometric data, biochemical data, clinical data and dietary data are the A, B, C and Ds of a complete and comprehensive nutritional assessment.
The elements of these A, B, C and Ds of nutritional assessment include:
- A: Anthropometric Data: This data includes variables such as height, weight, body mass index and arm measurements such as the mid arm circumference and the triceps skin fold.
- B: Biochemical Data: Laboratory testing data like serum albumin, hemoglobin, urinary creatinine, and serum transferrin.
- C: Clinical Data: The client’s skin condition, level of activity and status of the client’s mucous membranes.
- D: Dietary Data: This data includes the client’s subjective reports of their food and fluid intake over the last 24 hours and the types of foods that are typically eating.
- Constipation: The provision of a high fiber diet
- Urinary pH changes: Encouraging ample oral fluid intake
- Aspiration: Maintaining the client in at least a 30 degree angle
- Aspiration: Maintaining the client in at least a 90 degree angle
Aspiration can be prevented by maintaining the client in at least a 30 degree angle; a 90 degree angle is not only not necessary, this angle places a client at greater risk for the development of a pressure ulcer.
Diarrhea, rather than constipation is a complication of tube feedings; and urinary pH changes are not a commonly occurring complication of tube feedings.
Some of the other complications and preventive measures are:
- Diarrhea: Maintaining a slow rate of infusion whenever possible, changing the ordered rate and formula when necessary
- Abdominal pain: Maintaining a slow rate of infusion whenever possible
- Dehydration: Monitor the client for any signs and symptoms of dehydration, measure intake and output and notify the doctor of any abnormalities
- Nausea and Vomiting: Slowing the rate down, changing the formula and antiemetic medications to stop the vomiting and to prevent any aspiration
- Tube Dislodgment: Secure and monitor the tube
- Locus of control
- Bodily surface area
- Diaphoresis
There are a wide variety of different factors that influence and impact on our clients’ hygiene habits and routines. For example, cultural practices and beliefs, ethnical factors, religious practices and beliefs, the client’s level of growth and development.
Although the locus of control, bodily surface area and diaphoresis in addition to other factors such as economic constraints, the client’s level of energy, the client’s level of cognition, and environmental factors can impact on hygiene, these are not factors that impact on the client’s hygiene and hygiene practices; they do not typically impact on the lifelong developed hygiene and hygiene practices.
- The neonate: 10 to 15 hours a day
- The toddler: 11 to 14 hours a day
- The preschool child: 12 to 15 hours a day
- The school age child: Less than 8 hours a day
The age group that is accurately paired with the normal and recommended hours of sleep each day is the toddler should sleep about 11 to 14 hours per day.
The neonate should sleep 14 to 17 hours per day; the preschool child should sleep 10 to 13 hours per day; and the school age child should sleep 9 to 11 hours per day.
Physiological Integrity: Pharmacological & Parenteral Therapies Practice Questions
- Stop the intravenous flow
- Slow down the intravenous flow
- Notify the doctor
Your first priority intervention is to immediately stop the flow of the intravenous antibiotic because it is highly likely that the signs of anaphylaxis have occurred as the result of the client’s adverse effect to this antibiotic.
The next thing that you would do is assess the client to determine their physical status and to provide necessary emergency measures, including CPR, if it is indicated. Later, you would notify the doctor about this adverse reaction.
- Mix a small amount of the medication in a small amount of the intravenous fluid and then examine this mixture for color changes
- Refer to a compatibility chart
- Call the doctor and ask if the medication is compatible with the particular intravenous fluid
- Mix a small amount of the medication in a small amount of the intravenous fluid and then examine this mixture for any precipitates
The best way to determine whether or not a medication is compatible for a particular intravenous fluid is to refer to a compatibility chart.
Although, at times, incompatibility can be evidenced with changes such as those related to color changes and the formation of a cloudy solution or obvious precipitate, at other times incompatibility may not be noticeable. For this reason, nurses must refer to a compatibility or incompatibility chart before they mix medications or medications and solutions.
Lastly, there is no need to call the doctor for compatibilities when you have, and should use, a compatibility chart.
- Prevent polypharmacy
- Conserve financial resources
- Prevent interactions
- Prevent allergies
The medication reconciliation process to insure that the nurse is aware of all medications that the client is taking, some of which may have been ordered by a physician other than the client’s primary care doctor and some of which are over the counter or alternative therapies that the client has added. The complete and current list of medications is then reviewed by the nurse and possible interactions are identified and addressed with the client.
Although this medication reconciliation process can also save costs by eliminating unnecessary medications, particularly when the client is taking multiple medications (polypharmacy), this is not a primary purpose. Lastly, medications that the client is allergic to should never be given, therefore, these medications should not appear during the medication reconciliation process; they should never have been given to or taken by the client.
- The fact that drugs classified as categories C, D and X are contraindicated for women who are pregnant.
- The fact that drugs classified as categories A, B and C are contraindicated for women who are pregnant.
- The fact that drugs classified as categories C, D and E are contraindicated for women who are pregnant.
- The fact that drugs classified as categories C, D and Z are contraindicated for women who are pregnant.
Drugs classified as categories C, D and X are contraindicated for women who are pregnant because of the risks associated with these categories in terms of the developing fetus when these medications cross the placental barrier.
- The nurse must be knowledgeable about the fact that this client has A and B agglutinins and lacks the Rh factor
- The nurse must be knowledgeable about the fact that this client has B and O agglutinins and lacks the Rh factor
- The nurse must be knowledgeable about the fact that this client has B agglutinins and lacks the Rh factor
- The nurse must be knowledgeable about the fact that this client has A agglutinins and lacks the Rh factor
The nurse must be knowledgeable about the fact that this client has A agglutinins and they lack the Rh factor.
Type A blood has B agglutinins; type B blood has A agglutinins, type AB blood has no antibodies, or agglutinins, and type O blood has both A and B agglutinins.
People also have a rhesus, or Rh, factor antigen or the lack of it. Clients with an Rh positive blood, which is the vast majority of people, have Rh positive blood and people without the Rh factor antigen have Rh negative blood.
- Hemolysis: Typing and cross matching the blood and checking for ABO compatibility prior to administration
- Hemolysis: Insuring that the client does not have a prior history of hemolysis in the past
- Febrile reactions: Insuring that the client does not have a prior history of hemolysis in the past
- Febrile reactions: Typing and cross matching the blood and checking for ABO compatibility prior to administration
Hemolysis can be prevented by typing and cross matching the blood and checking for ABO compatibility prior to administration. This incompatibility can occur as the result of a laboratory error in terms of typing and cross matching and a practitioner error in terms of checking the blood and matching it to the client’s blood type.
Febrile reactions are the most commonly occurring reaction to blood and blood products administration. Although a febrile reaction can occur with all blood transfusions, it is most frequently associated with packed red blood cells and this reaction is not accompanied with hemolysis nor is it associated with its occurrence.
- You must insure that the client has a patent intravenous catheter that is at least 20 gauge.
- You will need the help of another nurse prior to the administration of these packed red blood cells.
- The unit of packed red blood cells should start no more than 1 hour after it is picked up.
- You must remain with and monitor the client for at least 30 minutes after the transfusion begins.
You will need the help of another nurse prior to the administration of these packed red blood cells. Two nurses must check the blood, the doctor’s order, the ABO compatibility and the client’s identity using at least two unique identifiers prior to the administration of this blood.
You must insure that the client has a patent intravenous catheter that is at least 18 gauge and not 20 gauge; you will be using normal saline and a Y infusion set for the administration of the blood because Ringer’s lactate and other intravenous solutions are not compatible with blood; blood should not remain in the client care area for more than 30 minutes so it is important that the nurse is prepared to begin the transfusion shortly after the blood is delivered to the patient care area; and, lastly, the nurse should remain with and monitor the client for at least 15 minutes after the transfusion begins at a slow rate since most serious blood reactions and complications occur shortly after the transfusion begins.
- A percutaneous, non tunneled subclavian catheter
- A peripheral intravenous catheter that is 20 gauge
- A multi lumen implanted tunneled and cuffed central venous catheter
- A peripherally inserted central venous catheter
You would most likely anticipate that this client will be given a multi lumen implanted tunneled and cuffed central venous catheter because this multi trauma client is in need of multiple intravenous therapies such as blood, medications and total parenteral nutrition over an extended period of time.
A percutaneous, non tunneled subclavian catheter would not be the device of preference because percutaneous, non tunneled subclavian catheters are used when short term treatments are anticipated; a peripheral intravenous catheter that is at least 18 gauge is necessary for the administration of blood; and a peripherally inserted central venous catheter would also not be the venous access device of choice for this seriously ill client who will require long term treatments and care.
- 1.5 tablets
- 1.25 tablets
- 1.33 tablets
You have to determine how many tablets the patient will take if the doctor has ordered 200 mg a day and the tablets are manufactured as 150 mg per tablet.
The mathematical rule for this type of calculation is:
Have = Desired Quantity X
This problem is calculated as shown below.
200 mg: X tablets = 150 mg: 1 tablet
200 mg = 150 mg
X tablets 1 tab
You will criss cross multiply the known numbers and then divide this product by the remaining number to solve for X, as below.
200 x 1 = 150 X
200/150 = 1.33 tabs rounded off to 1 1/3 tabs
You have to determine how many mLs the patient will take if the doctor has ordered 10 mg twice a day and there are 12 mg in each mL.
10 mg: X mL = 12 mg: 1 mL
10 mg = 12 mg X mL 1 mL
10 x 1 = 10 X
10/12 = 0.833 mL rounded off to 0.8 mL
You have to determine how many mLs the patient will take if the doctor has ordered 6,500 units of heparin subcutaneously and there are 4,500 units in one mL.
6,500 units: X mL = 4,500 units: 1 mL
6,500 units = 4,500 units X mL 1 mL
6,500 x 1 = 6,500
6,500/4,500 = 1.44 mL which is rounded off to 1.4 mL
To calculate the number of mg that this pediatric client will receive in each dose, you will have to calculate the client’s weight in kg and then determine the total mg for the day after which you will divide the daily dosage by 2 because the order is for two equally divided doses each day.
The steps for this calculation are shown below:
This is how to determine the client’s weight in terms of kg:
48 pounds: x kg = 2.2 pounds: 1 kg
48 pounds = 2.2 pounds x kg 1 kg
48 x 1 = 48
48/2.2 = 21.81 or 21.81 kg
This is how to determine the client’s total daily dosage when the doctor has ordered has ordered 5 mg/kg/day:
21.81 kg x 5 = 109.05 mg per day
This is how to determine the client’s dose for each of the two divided doses:
109.05/2 = 54.53 mg which is rounded off to 55 mg for each of two divided doses.
The first step of this calculation is to calculate the number of mLs, or cc s, per hour and then determine the number of drops per minute. This calculation is done as follows:
1000 ml = 125 mL per hour 8 hrs
The next step is done using this rule that reflects the fact that there are 60 minutes per hour in order to determine the number of mLs per minute .
1 hour = The ordered mL per hour 125 mLs X min 60 min
1 hour = 125 mL X min 60 min
60 x 1 = 60
88/60 = 2.08 mL per minute
Finally, the number of drops per minute is calculated by using the intravenous infusion set’s drop factor by using this rule.
Volume per minute x Drop factor
2.08 x 20 = 41.6 gtts per minute which is rounded off to 42 gtts per minute
With this type of calculation, the amount of normal saline that will be added to a powder in a vial to reconstitute the medication is important, instead, it is the amount of medication that results after the addition of the normal saline. For example, this reconstituted medication yields it is the yield of 12 mg in an mL that is relevant. It is this that will be used in the calculation.
This calculation is done as shown below:
12 mg = 25 mg 1 mL X mL
25 x 1 = 25
25/12 = 2.08 mL which is 2.1 mL rounded off
When the doctor has ordered 1200 mLs of intravenous fluid every 8 hours, you would calculate the number of mLs per hour, as below.
1200/8 = 150 mLs per hour
From 8 am to 12 noon there are 4 hours so:
150 mLs x 4 = 600 mLs
Because you had 600 mLs at 8 am, you should be prepared to hand another intravenous bag because this 600 mLs should all be infused at 12 noon.
- Question the order because Benadryl is an antihistamine and not a sleeping medication.
- Refuse to give the Benadryl because this medication is a stimulant.
- Question the order because Benadryl is contraindicated when the client has a sleep inducement disorder.
- Give the Benadryl because sleep inducement is an accepted off label use of this medication.
You would administer this Benadryl because sleep inducement is an accepted off label use of this medication. When a medication is used for any other than these established and approved uses, this usage is referred to as an “off label use”.
- The “right” verification
- The “right” to refuse
- The “right” documentation
- The “right” client education
The “right verification” is not one of the “Ten Rights of Medication Administration”. The verification of the doctor’s order for a medication is to confirm the right paint, medication, dose, route and time or frequency, it, in itself, is not one of the “10 Rights”.
The “Ten Rights of Medication Administration” are the right, or correct:
- Time or frequency
- Client education
- Documentation
- Right to refuse
- Assessment and
- Gluteus maximus muscle.
- Vastus lateralis muscle.
- Deltoid muscle.
- The sternocledomastoid muscle.
The administration of an intramuscular injection to a neonate should be given in the vastus lateralis, rectus femoris and ventrogluteal muscle sites and not the deltoid or the gluteus maximus muscles because these muscles have not yet developed.
The sternocledomastoid muscle is not an intramuscular injection site.
- A subcutaneous injection site
- The PQRST technique
- The Z track technique
- The sublingual site
You would expect to use to use the Z track technique to administer ferrous sulfate.
Ferrous sulfate IM is given using the Z Track technique to avoid the leakage and dark staining of the injection site with this medication.
Ferrous sulfate is not administered with a subcutaneous injection or using the sublingual route. Lastly, the PQRST method is used to assess pain and not used as a guideline for medication administration.
- 1,5,4,2,3,6
- 4,3,2,6,1,5
- 4,2,5,3,1,6
- 1,5,3,6,4,2
The steps for mixing NPH, the long acting insulin, with regular insulin, the short acting insulin in the correct sequential order are:
- Prep the top of the longer acting insulin vial with an alcohol swab.
- Inject air that is equal to the ordered dosage of the longer acting insulin using the insulin syringe. Do NOT withdraw the longer acting insulin yet.
- Prep the top of the shorter acting insulin with an alcohol swab
- Inject air that is equal to the ordered dosage of the shorter acting insulin using the same insulin syringe.
- Withdraw the ordered dosage of the shorter acting insulin using the same insulin syringe.
- And, then lastly, withdraw the ordered dosage of the longer acting insulin using the same insulin syringe.
- Allow the nurse to administer the injection.
- Ask the nurse to use the vastus lateralis muscle instead.
- Ask the nurse to verify the doctor’s order again.
- Stop the nurse from administering the injection.
You would stop the nurse from administering the injection when you observe that the nurse has palpated the gluteus maximum muscle to determine the correct site. Intramuscular injection sites are determined by using boney landmarks and not by palpating the muscle.
You would not allow the nurse to administer the injection and you would not ask the nurse to use the vastus lateralis muscle instead because nothing indicates the need to do so. Lastly, you would verify the doctor’s order prior to entering the room and preparing to administer the injection and not during the time that the intramuscular site is being identified.
- You have failed to have another nurse witness the 0.8 mLs and the 0.2 mLs of waste.
- You have failed to have another nurse witness the 0.8 mLs of waste.
- You have failed to have another nurse witness the 0.2 mLs of waste.
- You have failed ask another nurse to verify the calculation of the dosage.
You have failed to have another nurse witness the 0.8 mLs and the 0.2 mLs.
All controlled substances are documented on the narcotics record as soon as they are removed, and all controlled substances that are wasted for any reason, either in its entirety or only partially, must be witnessed or documented by the wasting nurse and another nurse. Both nurses document this wasting.
It should not be necessary for you to ask another nurse to verify this calculation; the nurse is accountable and responsible for accurate dosage calculations.
The procedure for this medication reconciliation process is:
2. Compile a list of current medications and other preparations 1. Compile a list of newly prescribed medications 4. Compare the two lists and make note of any discrepancies and inconsistencies 5. Employ critical thinking and professional judgments during the comparisons of the two lists 6. Communicate and document the new list of medications to the appropriate healthcare providers
- The client with heart failure who is receiving Ringer’s lactate
- The client with cancer who is receiving bendamustine
- The client who is receiving potassium supplementation intravenously
- The client who is receiving total parenteral nutrition
The client with cancer who is receiving bendamustine is at greatest risk for extravasation. Extravasation occurs when vesicant and other vein irritating drugs infiltrate into the tissue. In severe cases, extravasation can lead to necrosis and the loss of an affected limb. Bendamustine is a vesicant chemotherapy drug.
Extravasation is not associated with the intravenous administration of Ringers lactate or potassium supplementation intravenously because this solution and medication are not vesicants. These intravenous preparations can lead to infiltration but not extravasation. Lastly, the client who is receiving total parenteral nutrition is at risk for other complications such as infection, but not extravasation.
- Infection: Lowering the limb to promote circulation
- Infiltration: The application of cold to the site
- Extravasation: The aspiration of contents including blood from the IV cannula
- Hematoma: The administration of dexrazonxane
In addition to other interventions, intravenous fluid contents including blood are aspirated from the IV cannula.
Other interventions include immediate cessation of the infusion, elevating the limb, applying warm compresses initially to rid the area of any remaining drug that is in the tissues which is then followed by cool compresses to reduce any swelling, and the administration of an ordered substance specific medication such as dexrazoxane.
One of the interventions for infection include the elevation, not lowering, of the affected limb; infiltration is treated with the application of warm, not cold, compresses and one of the interventions for hematoma is the application of pressure and heat and not the administration of dexrazonxane.
- Assess motor functioning.
- Assess sensory functioning.
- Evaluate responses to a tactile stimulation.
- Evaluate responses to a pain analgesic.
The CRIES scale is used to evaluate the neonate’s response to a pain analgesic; this pain scale is also used to assess pain among neonates.
Observational behavioral pain assessment scales for the pediatric population are used among children less than three years of age. Some of these standardized pediatric pain scales, in addition to the CRIES scale, include the FACES Pain Scale, the Toddler Preschooler Postoperative Pain Scale (TPPPS), the Neonatal Infant Pain Scale (NIPS), the Children's Hospital of Eastern Ontario Pain Scale (CHEOPS), the Faces Legs Activity Cry Consolability Pain Scale (FLACC), the Visual Analog Scale (VASobs) the Observation Scale of Behavioral Distress (OSBD), the COMFORT Pain Scale and the Pre-Verbal Early Verbal Pediatric Pain Scale (PEPPS) that is used with toddlers.
- Opioid Agonist: Dilaudid: Constipation
- Opioid Agonist: Naloxone: Constipation
- Opioid Antagonist: Dilaudid: Anaphylaxis
- Opioid Antagonist: OxyContin: Anaphylaxis
Dilaudid is an opioid agonist that can cause constipation.
Other opioid agonists are codeine, OxyContin, Darvon, Dilaudid, Demerol and Percocet. The side effects and adverse reactions to this classification of drugs include constipation, sedation, nausea, dizziness, pruritus, and sedation, respiratory depression and arrest, hepatic damage, an anaphylactic reaction, circulatory collapse and cardiac arrest.
Opioid antagonists also referred to as opioid receptor antagonists, such as naloxone and naltrexone, can have side effects such as hepatic damage, joint pain, insomnia, vomiting, anxiety, headaches and nervousness.
- Your client may be experiencing a fluid overload.
- Your client may be experiencing an embolus.
- Your client may be hyperglycemic.
- Your client may have an inadvertent pneumothorax.
The client may be experiencing an embolus, which is a complication of total parenteral nutrition. Some of the signs and symptoms of an embolus are chest pain, dyspnea, shortness of breath, coughing, and respiratory distress.
Emboli, secondary to total parenteral nutrition occur when air is permitted to enter this closed system during tubing changes and when a new bottle or bag of hyperalimentation is hung. This complication can be prevented by instructing the client to perform the Valsalva maneuver and the nurse’s rapid changing of tubings and solutions when the closed system is opened to the air.
An inadvertent pneumothorax can occur and become symptomatic during the insertion of the TPN catheter and not four days later.
Other side effects of TPN and their signs and symptoms are listed below.
- Infection: The classical signs of infection including a fever, malaise, swelling and redness at the insertion site, diaphoresis, chilling and pain in the area of the TPN catheter insertion site.
- Fluid overload: Hypertension, edema, adventitious breath sounds like crackles and rales, shortness of breath, and bulging neck veins.
- Hyperglycemia: High blood glucose levels, thirst, excessive urinary output, headache, nausea and fatigue.
- Hypoglycemia: Low blood glucose levels, shakiness, clammy and cool skin, blurry vision, diaphoresis and unconsciousness and seizures.
- Clients are at high risk for infection when they are getting TPN because they are immunocompromised.
- Clients are at high risk for hyperglycemia when they are getting TPN because they are diabetic.
- The client should perform the Valsalva maneuver when the nurse changes the TPN tubing.
- The client should perform the Valsalva maneuver when the nurse changes the TPN dressing.
The client should perform the Valsalva maneuver when the nurse changes the TPN tubing to prevent an embolus which can occur when the tubing is opened to the air while it is being changed.
A mask, not the Valsalva maneuver, is indicated for TPN dressing changes.
Lastly, clients are at risk for infection secondary to TPN because these solutions are high in dextrose and because TPN is an invasive sterile procedure; and clients are at high risk for hyperglycemia when they are getting TPN because these solutions are high in dextrose and not because the client is already a diabetic client.
Physiological Integrity: Reduction of Risk Potential Practice Questions
- Respiratory rate: 32 breaths per minute
- Pulse: 110 beats per minute
- Blood pressure: 55/82
- “The respiratory rate is a little too fast but the other vital signs are normal.”
- “The pulse rate is a little too fast but the other vital signs are normal.”
- “The blood pressure is a little low but the other vital signs are normal.”
- “All of these vital signs are normal for a child that is 2 years of age.”
All of these vital signs are normal for the toddler who is 2 years old. The normal vital signs for the toddler are:
- Respiratory rate: From 20 to 40 per minute
- Pulse rate: From 90 to 140 beats per minute
- Blood pressure: Diastolic from 50 to 80 mm Hg and systolic from 80 to 112 mm Hg
- Pulse: 100 beats per minute
- Blood pressure: 85/55
The respiratory rate is a little too fast for this 5 year old preschool client. The normal respiratory rate for this client should be from 22 to 30 per minute.
The normal pulse rate and blood pressure for the preschool child are from 80 to 110 beats per minute and a diastolic from 50 to 78 mm Hg and a systolic from 82 to 110 mm Hg.
- Pulmonary Artery Systolic Pressure: 22 mm Hg
- Pulmonary Artery Wedge Pressure: 22 mm Hg
- Pulmonary Artery Diastolic Pressure: 10 mm Hg
- Central Venous Pressure: 5 mm Hg
You would report the pulmonary artery wedge pressure of 22 mm Hg because the normal pulmonary artery wedge pressure is from 4 to 12 mm Hg.
The other normal hemodynamic values are:
- Pulmonary Artery Systolic Pressure: 15 to 26 mm Hg
- Pulmonary Artery Diastolic Pressure: 5 to 15 mm Hg
- Central Venous Pressure: 1 to 8 mm Hg
- The need to cleanse the perineal area with circular wipes.
- The need to cleanse the perineal area from the “dirtiest” to the “cleanest”.
- The need to use a new antiseptic wipe for each wipe from the inner to the outer labia.
- The need to use a new antiseptic wipe for each wipe from the outer to the inner labia.
You would instruct your female client to use a new antiseptic wipe for each wipe from the inner to the outer labia.
A principle of asepsis is the cleansing of areas from the cleanest to the dirtiest and NOT the reverse; therefore, the inner labia are cleansed before the outer labia. The female perineal area is prepped with straight strokes and wipes; and the male wipes with a circular pattern around the urinary meatus.
- Turn the finger down so the blood will drop with gravity.
- Wipe off the first drop of blood using sterile gauze.
- Prick the side of the finger using the lancet.
- Prick the pad of the finger using the lancet.
Pricking the pad of the finger using the lancet is NOT a step in the procedure for obtaining a blood glucose sample for testing. Instead, the side of the finger is pricked with the lancet.
The procedure for checking the client’s blood glucose levels in correct sequential order is as follows:
- Verify and confirm that the code strip corresponds to the meter code.
- Disinfect the client’s finger with an alcohol swab.
- Turn the finger down so the blood will drop with gravity.
- Collect the next drop on the test strip.
- Hold the gauze on the client’s finger after the specimen has been obtained.
- Read the client’s blood glucose level on the monitor.
- PaO2: 65 mm Hg
- PaCO2: 40 mm Hg
- Arterial blood pH: 7.39
You would report the client’s PaO2 of 65 mm Hg because it is not within normal parameters and it is also a significant change for the client. The normal partial pressure of oxygen (PaO2) is from 75 to 100 mm Hg.
The other blood gases, above, are within normal limits, as follows:
- Partial pressure of carbon dioxide (PaCO2): 38 - 42 mmHg
- Arterial blood pH: 7.38 - 7.42
- Oxygen saturation (SaO2): 94 - 100%
- Triglycerides: 75 mg/dL
- Total cholesterol: 6.5 mmol/L
- High-density lipoprotein (HDL): 60 mg/dL
- Low-density lipoprotein (LDL): 955 mg/dL
You would report a total cholesterol level of 6.5 mmol/L because this value exceeds the high normal for total cholesterol which is 5.5 mmol/L and the normal range is from 3 to 5.5 mmol/L.
The other lipid levels are normal as follows:
- Triglycerides: 50-150 mg/dL
- High-density lipoprotein (HDL): 40-80 mg/dL
- Low-density lipoprotein (LDL): 85-125 mg/dL
- Albumin: 40 g/L
- Amylase: 40 U/L
- Direct bilirubin: 17 µmol/L
- Total bilirubin: 17 µmol/L
You would report a direct bilirubin level of 17 µmol/L because this value exceeds the high normal for direct bilirubin which is 6 µmol/L and the normal range is from 0-6 µmol/L.
The other gastrointestinal related normal laboratory values are as follows:
- Albumin: 35-50 g/L
- Amylase: 30-125 U/L
- Total bilirubin: 2-20 µmol/L
- A 76 year old female client who has a history of alcohol abuse.
- A 76 year old female client who has a history of radon gas exposure.
- A 64 year old male client who has a history of cigarette smoking.
- A 64 year old male client who has hypotension.
A 64 year old male client who has hypotension is at greatest risk for impaired vascular perfusion.
Other risk factors associated with impaired vascular and tissue perfusion are:
- Hypervolemia
- Hypovolemia
- Low hemoglobin
- An immobilized limb
- Decreased cardiac output
- Impaired oxygen transportation
- Hypoventilation
Alcohol abuse, cigarette smoking and exposures to radon place people at risk for cancer, rather than impaired perfusion.
- A 76 year old female client who has a history of diabetes.
- A 64 year old male client who has a history of impaired oxygen transport.
The client who is at greatest risk for the development of cancer is the 76 year old female client who has a history of alcohol abuse. Data indicates that alcohol abuse can lead to cancer of the liver and other cancers.
Diabetes, a history of impaired oxygen transport and hypotension are risk factors associated with poor tissue perfusion, and not cancer.
- The level of pain among school age children.
- The risk for the impairment of skin integrity.
- Levels of muscular strength.
- Levels of mobility.
The Norton Scale measures the client’s risk for the impairment of skin integrity. The Norton Scale and the Braden Scale are standardized tools to screen clients for their risk of skin breakdown, pressure ulcers and an impairment of skin integrity.
Pain levels among school age children are measured with other standardized pain tools for pediatric clients; and levels of muscular strength and mobility are measured also with other standardized tests and not the Norton Scale.
- Impaired tissue perfusion
Impaired tissue perfusion is an intrinsic, or internal, risk factor that places the client at risk for pressure ulcers.
Pressure, shearing and friction are extrinsic, or external, risk factors that places the client at risk for pressure impaired tissue perfusion.
Other intrinsic risk factors associated with skin breakdown include:
- Poor nutritional status
- A decreased level of consciousness including that which occurs with sedating medications
- Fecal and/or urinary incontinence
- Impaired circulation
- Alterations in terms of the fluid balance
- Altered neurological sensory functioning
- Changes in terms of skin turgor
- Boney prominences
- Inflate the cuff if the cuff is deflated.
- Deflate the cuff if the cuff is inflated.
- Remove the inner cannula of the tube.
- Call the doctor about this airway obstruction.
The first thing that you should do when you insert the suction catheter and you reach a point of resistance is to deflate the cuff when it is inflated and the second thing that you should do is to remove the inner cannula and suction out the mucous plug.
You would not call the doctor because there is an airway obstruction; you should correct this problem with the measures above.
- Maintain the client with NPO status for at least 4 hours prior to this procedure.
- Teach the client about the fact that they may experience muscle flaccidity.
- Teach the client about the fact that they may have a headache after the ECT.
- Maintain the client on continuous hemodynamic monitoring after the ECT.
You would teach the client about the fact that they may have a headache after the ECT. Other components of the teaching about the aftermath of the procedure that the client should know about include the fact that the client may have muscle soreness, not muscle flaccidity, confusion, amnesia and hypertension.
The client should be maintained as NPO for at least 6 hours before ECT; and it is not necessary to maintain the client on continuous hemodynamic monitoring after the ECT, however, the client’s vital signs should be monitored.
- Strnagulation
- Skin breakdown
- Skin pallor
The neurological complication can occur when a vest restraint is too tight around the client’s body is numbness and tingling that, unless corrected, can lead to neurological damage.
Strangulation, skin breakdown and skin pallor can also occur when a restraint is too tight, however, these restraint complications are respiratory, integumentary system and circulatory system complications rather than neurological complications.
- The appearance of petechiae
- Aplastic anemia
- The appearance of thrombophlebitis
- Elevated platelets
The appearance of petechiae is a sign of thrombocytopenia which is a low platelet count. Other signs and symptoms include purpura, easy bruising, epistaxis, and spontaneous hemorrhage and bleeding.
Thrombocytopenia can occur as the result of several disorders and therapeutic treatments and interventions including aplastic anemia, HIV infection, a genetic disorder, cancer, particularly cancer that affects the bones, some viral pathogens like those that cause mononucleosis, as well as from therapeutic radiation therapy, chemotherapy and some medications such as Depakote.
- Pneumothorax
The complication that you should be aware of during the immediate post-operative period of time after a thoracentesis is a pneumothorax.
The signs and symptoms of pneumothorax and hemothorax include dyspnea, chest pain, shortness of breath and pain. The treatment of a pneumothorax includes the correction of the underlying cause whenever possible and the placement of a chest tube to remove the blood and/or air in the pleural space which will re-expand the affected lung and recreate the negative pressure of the pleural space.
Infection would not be evident during the immediate post-operative period; and, aspiration is not a complication of a thoracentesis.
- The client’s posterior tibia pulse is Grade B
- The client’s posterior tibia pulse is Grade C
- The client’s posterior tibia pulse is 1
- The client’s posterior tibia pulse is 2
You would document this finding as “The client’s posterior tibia pulse is 1”.
The strength, volume and fullness of the peripheral pulses are categorized and documented as follows:
- 0: Absent pulses
- 1: Weak pulse
- 2: Normal pulse
- 3: Increased volume
- 4: A bounding pulse
Grades and grading are not used in reference to pulses.
- The Lazarus Cognitive Appraisal Scale
- The Hamilton Rating Scale
- The McGill Scale
- The Rancho Los Amigos Scale
The tool or scale that you would use for a focused neurological assessment of your client is the Rancho Los Amigos Scale.
Levels of consciousness, which is part of a complete focused neurological assessment, can be determined and measured by using the standardized Glasgow Coma Scale for adults and children or the Rancho Los Amigos Scale. The Rancho Los Amigos Scale determines the patient’s level of awareness and functioning which can range from a 1 to an 8 when a 1 is the complete lack of all responsiveness to all stimulation and an 8 is when a patient is fully alert, oriented, appropriate and purposeful.
The McGill Pain Assessment is used to assess pain levels; the Lazarus Cognitive Appraisal Scale is used to assess levels of stress and coping; and the Hamilton Rating Scale is used to measure and assess depression.
- A lack of zinc
- A lack of vitamin E
- High iron levels
- High phosphorous levels
A lack of zinc, copper, iron and vitamins C and A are risks associated with impaired and delayed wound healing.
Other risk factors that impede wound healing are:
- Advancing age
- Nutritional status
- Some poor lifestyle choices
- Some medications
- Some diseases and disorders
- “The client is having anesthesia awareness which is not good.”
- “This often happens during stage 2 of general anesthesia.”
- "The client needs more general anesthesia.”
- “The client is having a seizure.”
You should respond to this student nurse by stating, “This often happens during stage 2 of general anesthesia.”
Stage 2 of general anesthesia, often referred to as the Excitement Stage, is characterized with uncontrollable muscular activity, irregular respirations, an irregular cardiac rhythm, and, at times, vomiting. This stage does not indicate the need for more general anesthesia.
Anesthesia awareness, which is a rare complication of general anesthesia, is the lack of amnesia during surgery when the client remembers events during surgery and, at times, they remember the pain.
Lastly, there is no evidence in this question that the client is having a seizure.
- Surgical site marking
- Medication reconciliation
- A neutral zone for sharps
Medication reconciliation prevents medication errors and other complications associated with medications and not a way to reduce surgical risks.
Surgical marking, time outs that are done after surgical site marking is done, and a neutral zone for sharps do reduce surgical risks such as wrong site surgery, wrong patient surgeries and sharps injuries.
Physiological Integrity: Physiological Adaptation Practice Questions
- Exclude pregnant visitors from the client’s room.
- Place the client in a negative pressure room.
- Have all visitors wear protective masks and boots.
- All of the above
You would exclude all pregnant visitors from the client’s room in order to protect the pregnant woman’s developing fetus. Brachytherapy is internally placed radioactive material to treat clients who are affected with tumor and cancer of the prostate, lungs, esophagus, cervix, endometrium, rectum, breast, head and neck.
Special radiation precautions are initiated when a client is receiving brachytherapy in order to protect visitors and health care staff from the harmful effects of the radiation. Some of the other special internal radiation precautions include:
- The minimization of the duration of time that health care providers are in the client’s room to deliver care and services to the client
- The placement of the client receiving internal radiation in a private room. A negative pressure room is not indicated for this client.
- The prohibition of the client’s activities outside of their room
- The initiation of complete bed rest for the client until the treatment is discontinued
- The provision of education to the family members and other visitors that includes information about their need to limit the time of their visits to at least less than 1 hour, to stay at least 6 feet away from the client
- The need for health care staff to minimize the amount of time spent in the room, to decline to enter the room if they are pregnant, to retain all supplies and equipment including things like bed linens in the client’s room until they are deemed safe for disposal by a person who is competent to make this decision, and how and when to report concerns about the client’s treatment such as when implanted seeds inadvertently leave the client’s body.
- Oral dryness
Fibrosis is an adverse effect to therapeutic radiation therapy.
Radiation fibrosis can affect bones, nerves, ligaments, muscles, blood vessels, tendons, and the heart in addition to the lungs. Fibrosis occurs as the result of abnormal fibrin and protein accumulation within normal irradiated tissue.
Alopecia, and oral dryness which is also referred to as xerostomia, are side effects and complications to radiation, but not adverse effects.
Other side effects, complications and adverse effects associated with therapeutic radiation therapy are:
- Skin damage
- Damage to the mucosa
- Dental caries and oral infections
- Nausea and vomiting
- Bone marrow suppression and immunosuppression
- Radiation pneumonia
- Placing the client in the Trendelenburg position
- Monitoring the color of the stools
- Using a Hoyer lift for patient transfers
- Monitoring the arterial blood gases
You would monitor the color of the stools for the client who is receiving phototherapy. Phototherapy is used to treat psoriasis, but it is most commonly employed for the treatment of neonatal hyperbilirubinemia and jaundice which can occur among both full term and pre term infants.
You would also monitor and document the client’s:
- Skin for changes in color that may indicate an increase or decrease in the amount of bilirubin in the client’s blood
- Laboratory bilirubin levels to determine whether or not the client’s bilirubin levels are decreasing as the result of the phototherapy
- Volume, color and characteristics of the stool because phototherapy can lead to frequent, loose stools as well as a color change to green colored stools
- Hypokalemia: Hypermagnesemia
- Hyponatremia: Dehydration
- Hyperkalemia: Ketoacidosis
- Hypercalcemia: Hypoparathyroidism
Ketoacidosis is a risk factor for hyperkalemia.
The risk factors for the other electrolyte disorders above are listed below.
- Hypokalemia: Diarrhea, vomiting, and diaphoresis as well as some medications like diuretics and laxatives, and with other disorders and diseases such as ketoacidosis. Hypermagnesemia is not a risk factor for hypokalemia.
- Hyponatremia: Thyroid gland disorders, cirrhosis, renal failure, heart failure, pneumonia, diabetes insipidus, Addison’s disease, hypothyroidism, primary polydipsia, severe diarrhea or vomiting cancer, and cerebral disorders. Dehydration is a risk factor associated with hypernatremia, not hyponatremia.
- Hypercalcemia: Hyperparathyroidism, not hyperparathyroidism, some medications such as thiazide diuretics and lithium, some forms of cancer such as breast cancer and cancer of the lungs, with multiple myeloma, Paget’s disease, non weight bearing activity and elevated levels of calcitriol as occurs with sarcoidosis and tuberculosis.
- Hypernatremia: Hepatic failure
- Hypocalcemia: Vitamin A deficiency
- Hypermagnesemia: Cushing’s disease
- Hypomagnesemia: Crohn’s disease
Crohn’s disease is a risk factor for hypomagnesemia.
Other electrolyte disorder risk factors include:
- Hypernatremia: Dehydration, renal failure, hyperglycemia and Cushing’s disease
- Hypocalcemia: Vitamin D deficiency, Crohn’s disease, sepsis and pancreatitis
- Hypermagnesemia: Addison’s disease, renal failure, diabetic ketoacidosis and dehydration
- Phosphate: From 0.81 to 1.45 mmol/L.
- Chloride: From 60 to 110 mEq/L.
- Calcium: From 6.5 - 10.6 mg/dL.
- Potassium: From 3.7 to 7.2 mEq/L.
The normal level of phosphate is from 0.81 to 1.45 mmol/L.
The other normal levels for these electrolytes are:
- Chloride: From 97 to107 mEq/L.
- Calcium: From 8.5 - 10.6 mg/dL.
- Potassium: From 3.7 to 5.2 mEq/L.
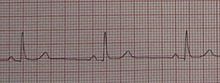
- Idioventricular Rhythm
- Bundle Branch Block
- Sinus bradycardia
- Atrial Flutter
Sinus bradycardia is a sinus rhythm that is like the normal sinus rhythm with the exception of the number of beats per minute. Sinus bradycardia has a cardiac rate less than 60 beats per minute, the atrial and the ventricular rhythms are regular, the P wave occurs prior to each and every QRS complex, the P waves are uniform in shape, the length of the PR interval is form 0.12 to 0.20 seconds, the QRS complexes are uniform and the length of these QRS complexes are from 0.06 to 0.12 seconds.

- Atrial flutter
- Supraventricular Tachycardia
- Premature Atrial Contractions
Atrial flutter, which is a relatively frequently occurring tachyarrhymia; this cardiac rhythm is characterized with an rapid atrial rate of 250 to 400 beats per minute, a variable ventricular rate, a regular atrial rhythm, a possibly irregular ventricular rhythm, the P waves are not normal, the flutter wave has a saw tooth look (f waves), the PR interval is not measurable, QRS complexes are uniform and the length of these QRS complexes are from 0.06 to 0.12 seconds.
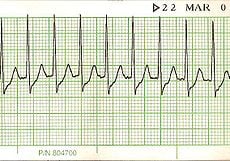
- Torsades de Pointes
- Accelerated Idioventricular Arrhythmia
- First Degree Atrioventricular Heart Block
- Supraventricular tachycardia
Supraventricular tachycardia, simply defined is all tachyarrhythmias with a heart rate of more than 150 beats per minute.
The atrial and ventricular cardiac rates are from 150 to 250 beats per minute, the cardiac rhythm is regular, the p wave may not be visible because it is behind the QRS complex, the PR interval is not discernable, the QRS complexes look alike, and the length of the QRS complexes ranges from 0.06 to 0.12 seconds.
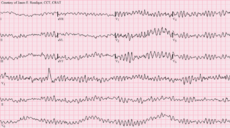
- Third Degree Heart Block
- Second-Degree Atrioventricular Block, Type II
- Ventricular fibrillation
The two types of ventricular fibrillation that can be seen on an ECG strip are fine ventricular fibrillation and coarse ventricular fibrillation; ventricular fibrillation occurs when there are multiple electrical impulses from several ventricular site. This results in erratic and uncoordinated ventricular and/or atrial contractions.
You would instill 250 mLs of irrigating solution after each suctioning of the nasogastric tube. The typical amount of irrigating solution is from 20 mLs to 300 mLs.
- The compression of the renal medulla.
- Syncope and dizziness of unknown origin.
- Pressure on the vena cava which is a major vein in the body.
- Pressure on the vena cava which is the largest artery in the body.
You should explain that superior vena cava syndrome is pressure on the vena cava which is a major vein, not an artery, in the body that carries blood from the systemic circulation to the right atrium of the heart. This pressure on the superior vena cava prevents the normal return of the body’s circulating blood to the heart.
The signs and symptoms of superior vena cava syndrome include tachypnea, dyspnea, venous stasis, a loss of consciousness, edema, seizures, respiratory and/or cardiac arrest and not syncope of unknown origin. This is a life threatening medical emergency.
- Hypovolemic shock
- Septic shock
- A dissected thoracic aortic aneurysm
You would most likely suspect that this client is affected with a dissected thoracic aneurysm. Thoracic aorta rupture and dissections can present with symptoms that can include shortness of breath, dysphagia, dyspnea, coughing, and pain in the chest, arms, jaw, neck, and/or back.
The signs and symptoms of hypovolemic shock vary according to the stage of the shock; some of the signs and symptoms include hypotension, tachycardia, a lack of tissue perfusion, hyperventilation, decreased cardiac output, decreased urinary output, oliguria, anuria, metabolic acidosis, increased blood viscosity, and multisystem failure.
The signs and symptoms of septic shock include the classical signs of infection in addition to hypotension, confusion, metabolic acidosis, respiratory alkalosis, abnormal breath sounds like crackles and rales, a widened pulse pressure, and decreased cardiac output.
- Part of the intestine slides into another part of the intestine.
- The appendix ruptures.
- An ileostomy stoma retracts below the abdominal surface.
- Lungs are infiltrated.
Intussusception occurs when a part of the intestine slides into another part of the intestine. This medical emergency can lead to poor perfusion to the intestine.
The signs and symptoms of intussusception include knee to chest posturing, abdominal pain, bloody stool, fever, constipation, vomiting and diarrhea.
A ruptured appendix occurs when an infected appendix ruptures; a stoma retraction occurs when an ileostomy stoma retracts below the abdominal surface; and pneumonia occurs when the lungs become infiltrated.
- The administration of a thrombolytic medication
- The administration of hyroxyurea
- Placing the client in the lithotomy position
You would expect to administer hydroxyurea which prevents the sickling of the client’s red blood cells. You would not administer a thrombolytic medication; however, you would likely administer analgesic medications for the pain associated with the sickle cell crisis.
The lithotomy position is used for procedures involving the pelvis, including gynecological examinations; and the Trendelenburg position is used when the client is in shock and with significant hypotension.
- Perform the Valsalva maneuver
- Encourage the person to continue coughing
- Perform the Heimlich maneuver
- Begin CPR and prepare for ACLS measures
You would encourage the person to continue coughing because this person has a partial airway obstruction.
You would perform the Heimlich maneuver when the person has a complete airway obstruction. CPR and ACLS may be necessary later, but not now as based on the fact that the person only has a partial airway obstruction. Lastly, the Valsalva maneuver is done when one exerts pressure against resistance.
- Trichomoniasis
- Staphylococcus aureus
- Neisseria gonorrhoeae
Pelvic inflammatory disease is most often caused by the Neisseria gonorrhoeae and Chlamydia trachomatis pathogens; and it most often occurs as the result of untreated salpingitis, pelvic peritonitis, a tubo ovarian abscess and/or endometritis.
Unlike Neisseria gonorrhoeae, trichomoniasis and infections caused by E. coli and Staphylococcus aureus are not associated with the onset of pelvic inflammatory disease which can lead to infertility, increased risk for ectopic pregnancies, sepsis, septic shock and death when left untreated.
- Adaptive immunity
- Passive natural immunity
- Active natural immunity
- Active artificial immunity
The type of immunity occurs when a person has an infectious, communicable disease like the measles is active natural immunity.
Active immunity occurs as the result of our bodily response to the presence of an antigen, with the development of antibodies. Active immunity can be both natural and artificial. Natural active immunity occurs when the body produces antibodies after the client is infected with a pathogen; and artificial active immunity occurs when the body produces antibodies to an immunization vaccine such as those for pneumonia and a wide variety of childhood infectious diseases.
Adaptive immunity is the acquisition of antibodies or activated T cells in the body. Passive immunity occurs when an antibody is introduced into the body by either natural or artificial means. Passive natural immunity occurs when the fetus and neonate receive immunity as a natural process through the placenta; and passive artificial immunity occurs when the client receives an injection of immune globulin.
- The incubation stage
- The prodromal stage
The prodromal stage, or phase, of the infection process is characterized with general malaise, joint and muscular aches and pains, anorexia, and the presence of a headache. The prodromal stage begins with the onset of symptoms and this stage is characterized with the replication and reproduction of the pathogen.
The incubation stage is asymptomatic; the illness stage is the period of time that begins with continuation of the signs and symptoms and it continues until the symptoms are no longer as serious as they were before; and the convalescence stage is the period of recovery during which time the symptoms completely disappear.
- They are not as effective as regular defibrillators.
- They are replacing regular defibrillators in acute care settings.
- Only BLS certified people in the community should use them.
- They can be easily used by people with no healthcare experience.
Automated external defibrillators can be easily used by people with no healthcare experience. Automated external defibrillators are simple to use and there is no need to be able to recognize cardiac arrhythmias or interpret cardiac rhythm strips. Automated external defibrillations are intended to be used by the general public without any healthcare or nursing knowledge of experience; therefore, they are not restricted to only those BLS certified.
Although they are highly effective, they are not replacing the standard defibrillators in the acute care setting.
- Episiotomy extension related to a forceps delivery
- Respiratory depression related to NSAIDs
- Hemothorax related to a latex allergy
Maternal trauma, lacerations, pelvic floor damage, bleeding and an inadvertent extension of the episiotomy to the anus when a forceps delivery of a new born is done.
Respiratory depression can occur as the result of narcotic analgesics such as morphine, and not NSAIDs; pneumothorax and hemothorax can occur as the result of an inadvertent perforation during invasive procedures such as the placement of a total parenteral nutrition catheter and a thoracentesis; and the signs and symptoms of a latex allergy include tachycardia, hypotension, dyspnea, chest pain tremors, and anaphylactic shock, not respiratory depression.
Best Nursing Research Topics for Students
What is a nursing research paper.
- What They Include
- Choosing a Topic
- Best Nursing Research Topics
- Research Paper Writing Tips

Writing a research paper is a massive task that involves careful organization, critical analysis, and a lot of time. Some nursing students are natural writers, while others struggle to select a nursing research topic, let alone write about it.
If you're a nursing student who dreads writing research papers, this article may help ease your anxiety. We'll cover everything you need to know about writing nursing school research papers and the top topics for nursing research.
Continue reading to make your paper-writing jitters a thing of the past.
Popular Online Master of Science in Nursing (MSN) Programs

GCU's College of Nursing and Health Care Professions has a nearly 35-year tradition of preparing students to fill evolving healthcare roles as highly qualified professionals. GCU offers a full spectrum of nursing degrees, from a pre-licensure BSN degree to a Doctor of Nursing Practice (DNP) program.
Enrollment: Nationwide
- MSN - Family NP
- MSN - Adult Gerontology Acute Care NP
- MSN - Nursing Education
- MSN - Health Informatics
- MSN - Public Health Nursing
- MSN - Health Care Quality & Patient Safety
- MBA & MSN - Nursing Leadership in Health Care Systems
- See more GCU nursing programs

WGU's award-winning online programs are created to help you succeed while graduating faster and with less debt. WGU is a CCNE accredited, nonprofit university offering nursing bachelor's and master's degrees.
- BSN-to-MSN - Family NP
- BSN-to-MSN - Psychiatric Mental Health NP
- BSN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Leadership & Management
Enrollment: Nationwide, excluding NY, RI and CT. Certain programs have additional state restrictions. Check with Walden for details.
- MSN - Psychiatric-Mental Health NP
- MSN - Adult/Gerontology Acute Care NP
- MSN - Adult/Gerontology Primary Care NP
- MSN - Pediatric NP - Primary Care
- MSN - Nursing Informatics

As a working RN, you need a flexible, transfer-friendly program to help you save time and money as you take the next step in your nursing career. In our CCNE-accredited4 RN to BSN program, you can transfer in up to 134 credits—which is nearly 75% of program requirements. Your transfer credits can be reviewed in one business day (on average).
Enrollment: FL
- MSN - Adult-Gerontology NP - Primary Care
- MSN - Nursing Leadership & Admin
- MSN - Healthcare Tech, Simulation & Informatics
- See more Rasmussen nursing programs
A nursing research paper is a work of academic writing composed by a nurse or nursing student. The paper may present information on a specific topic or answer a question.
During LPN/LVN and RN programs, most papers you write focus on learning to use research databases, evaluate appropriate resources, and format your writing with APA style. You'll then synthesize your research information to answer a question or analyze a topic.
BSN , MSN , Ph.D., and DNP programs also write nursing research papers. Students in these programs may also participate in conducting original research studies.
Writing papers during your academic program improves and develops many skills, including the ability to:
- Select nursing topics for research
- Conduct effective research
- Analyze published academic literature
- Format and cite sources
- Synthesize data
- Organize and articulate findings
About Nursing Research Papers
When do nursing students write research papers.
You may need to write a research paper for any of the nursing courses you take. Research papers help develop critical thinking and communication skills. They allow you to learn how to conduct research and critically review publications.
That said, not every class will require in-depth, 10-20-page papers. The more advanced your degree path, the more you can expect to write and conduct research. If you're in an associate or bachelor's program, you'll probably write a few papers each semester or term.
Do Nursing Students Conduct Original Research?
Most of the time, you won't be designing, conducting, and evaluating new research. Instead, your projects will focus on learning the research process and the scientific method. You'll achieve these objectives by evaluating existing nursing literature and sources and defending a thesis.
However, many nursing faculty members do conduct original research. So, you may get opportunities to participate in, and publish, research articles.
Example Research Project Scenario:
In your maternal child nursing class, the professor assigns the class a research paper regarding developmentally appropriate nursing interventions for the pediatric population. While that may sound specific, you have almost endless opportunities to narrow down the focus of your writing.
You could choose pain intervention measures in toddlers. Conversely, you can research the effects of prolonged hospitalization on adolescents' social-emotional development.
What Does a Nursing Research Paper Include?
Your professor should provide a thorough guideline of the scope of the paper. In general, an undergraduate nursing research paper will consist of:
Introduction : A brief overview of the research question/thesis statement your paper will discuss. You can include why the topic is relevant.
Body : This section presents your research findings and allows you to synthesize the information and data you collected. You'll have a chance to articulate your evaluation and answer your research question. The length of this section depends on your assignment.
Conclusion : A brief review of the information and analysis you presented throughout the body of the paper. This section is a recap of your paper and another chance to reassert your thesis.
The best advice is to follow your instructor's rubric and guidelines. Remember to ask for help whenever needed, and avoid overcomplicating the assignment!
How to Choose a Nursing Research Topic
The sheer volume of prospective nursing research topics can become overwhelming for students. Additionally, you may get the misconception that all the 'good' research ideas are exhausted. However, a personal approach may help you narrow down a research topic and find a unique angle.
Writing your research paper about a topic you value or connect with makes the task easier. Additionally, you should consider the material's breadth. Topics with plenty of existing literature will make developing a research question and thesis smoother.
Finally, feel free to shift gears if necessary, especially if you're still early in the research process. If you start down one path and have trouble finding published information, ask your professor if you can choose another topic.
The Best Research Topics for Nursing Students
You have endless subject choices for nursing research papers. This non-exhaustive list just scratches the surface of some of the best nursing research topics.
1. Clinical Nursing Research Topics
- Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties.
- Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings.
- Explore the effectiveness of pain management protocols in pediatric patients.

2. Community Health Nursing Research Topics
- Assess the impact of nurse-led diabetes education in Type II Diabetics.
- Analyze the relationship between socioeconomic status and access to healthcare services.
3. Nurse Education Research Topics
- Review the effectiveness of simulation-based learning to improve nursing students' clinical skills.
- Identify methods that best prepare pre-licensure students for clinical practice.
- Investigate factors that influence nurses to pursue advanced degrees.
- Evaluate education methods that enhance cultural competence among nurses.
- Describe the role of mindfulness interventions in reducing stress and burnout among nurses.
4. Mental Health Nursing Research Topics
- Explore patient outcomes related to nurse staffing levels in acute behavioral health settings.
- Assess the effectiveness of mental health education among emergency room nurses .
- Explore de-escalation techniques that result in improved patient outcomes.
- Review the effectiveness of therapeutic communication in improving patient outcomes.
5. Pediatric Nursing Research Topics
- Assess the impact of parental involvement in pediatric asthma treatment adherence.
- Explore challenges related to chronic illness management in pediatric patients.
- Review the role of play therapy and other therapeutic interventions that alleviate anxiety among hospitalized children.
6. The Nursing Profession Research Topics
- Analyze the effects of short staffing on nurse burnout .
- Evaluate factors that facilitate resiliency among nursing professionals.
- Examine predictors of nurse dissatisfaction and burnout.
- Posit how nursing theories influence modern nursing practice.
Tips for Writing a Nursing Research Paper
The best nursing research advice we can provide is to follow your professor's rubric and instructions. However, here are a few study tips for nursing students to make paper writing less painful:
Avoid procrastination: Everyone says it, but few follow this advice. You can significantly lower your stress levels if you avoid procrastinating and start working on your project immediately.
Plan Ahead: Break down the writing process into smaller sections, especially if it seems overwhelming. Give yourself time for each step in the process.
Research: Use your resources and ask for help from the librarian or instructor. The rest should come together quickly once you find high-quality studies to analyze.
Outline: Create an outline to help you organize your thoughts. Then, you can plug in information throughout the research process.
Clear Language: Use plain language as much as possible to get your point across. Jargon is inevitable when writing academic nursing papers, but keep it to a minimum.
Cite Properly: Accurately cite all sources using the appropriate citation style. Nursing research papers will almost always implement APA style. Check out the resources below for some excellent reference management options.
Revise and Edit: Once you finish your first draft, put it away for one to two hours or, preferably, a whole day. Once you've placed some space between you and your paper, read through and edit for clarity, coherence, and grammatical errors. Reading your essay out loud is an excellent way to check for the 'flow' of the paper.
Helpful Nursing Research Writing Resources:
Purdue OWL (Online writing lab) has a robust APA guide covering everything you need about APA style and rules.
Grammarly helps you edit grammar, spelling, and punctuation. Upgrading to a paid plan will get you plagiarism detection, formatting, and engagement suggestions. This tool is excellent to help you simplify complicated sentences.
Mendeley is a free reference management software. It stores, organizes, and cites references. It has a Microsoft plug-in that inserts and correctly formats APA citations.
Don't let nursing research papers scare you away from starting nursing school or furthering your education. Their purpose is to develop skills you'll need to be an effective nurse: critical thinking, communication, and the ability to review published information critically.
Choose a great topic and follow your teacher's instructions; you'll finish that paper in no time.

Joleen Sams is a certified Family Nurse Practitioner based in the Kansas City metro area. During her 10-year RN career, Joleen worked in NICU, inpatient pediatrics, and regulatory compliance. Since graduating with her MSN-FNP in 2019, she has worked in urgent care and nursing administration. Connect with Joleen on LinkedIn or see more of her writing on her website.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

- Request new password
- Create a new account
Essentials of Nursing Practice
Student resources, multiple choice questions.
Consider the questions for each chapter to check your knowledge. Click on the question to reveal the answer.
Chapter 1: What is nursing and what is nursing?
Chapter 2: Being a nursing student
Chapter 3: Core academic skills
Chapter 4: Academic writing and assessment skills
Chapter 5: Ethics
Chapter 6: Law
Chapter 7: Accountability and professionalism
Chapter 8: Resilience
Chapter 9: The role of the student nurse in effecting change
Chapter 10: Delivering effective care
Chapter 12: Value-based, person or family centred care
Chapter 14: Assessment, planning, implementation and evaluation (APIE)
Chapter 15: Core communication skills
Chapter 16: Communication and interpersonal skills in challenging circumstances
Chapter 17: Assessing and managing risk PLUS Clinical governance and quality
Chapter 18: Record-keeping and documentation
Chapter 20: Safeguarding
Chapter 21: Promoting health
Chapter 24: Clinical measurement
Chapter 25: Pain management
Chapter 27: Safer handling of people
Chapter 28: First aid
Chapter 30: Assisting patients with their nutritional needs
Chapter 32: Assisting patients with their hygiene needs
Chapter 33: Last offices
Chapter 35: Introduction to interprofessional working
Chapter 36: Introduction to the psychological contexts of nursing
Chapter 37: Introduction to the sociological contexts of nursing
Chapter 40: Introduction to the global context of nursing
5th Semester (BSc Nursing)
[ bsc nursing ].
5th Semester (BSc Nursing) - Notes, Important Questions, Semester Question paper PDF Download
Nursing - BSc Nursing 5th Semester (BSc Nursing) - Notes, Important Questions, Study Material, Question Bank, Semester Question paper PDF Download. 5th Semester 3rd Year.
Study Material, Notes, Important Questions, Semester Question Paper PDF Download

Nursing Education Topics, Ideas, and Research Paper Examples
James colson dnp, rn.
- May 15, 2024
- Nursing Topics and Ideas
Nursing education plays a pivotal role in shaping the future of healthcare by training competent and compassionate nurses who can provide high-quality care to patients. However, the field of nursing education faces a myriad of challenges that need to be addressed to ensure the continued success of nursing programs and the preparation of future nurses.
Nursing Education Topics
In this article, we will explore Nursing Education topics, ideas for capstone and EBP Projects and give Research Paper Examples. We also explore some of nursing education challenges, propose PICOT questions, suggest evidence-based practice (EBP) and nursing capstone project ideas on nursing education challenges, provide research paper topics and questions, as well as essay topic ideas, all aimed at advancing the field of nursing education.
Working on a Research Paper?
Get your nursing homework and papers crafted by expert writers. Fast delivery, original content, and student-friendly prices guarantee
Nursing Education Challenges
Nursing education faces a host of challenges in the contemporary healthcare landscape. These challenges not only impact the quality of education but also influence the preparedness of future nurses to meet the complex demands of healthcare practice. Some of the key challenges include:
- Faculty Shortages: Nursing programs often struggle to recruit and retain experienced faculty members. The shortage of nurse educators can limit program capacity and affect the quality of instruction.
- Clinical Site Availability: Securing adequate clinical placement sites for nursing students can be a logistical challenge. Competition for clinical placements with other healthcare disciplines can further exacerbate this issue.
- Technological Integration: While technology is essential in modern healthcare, integrating it effectively into nursing education programs can be challenging. Faculty and students need to adapt to rapidly evolving digital tools and resources.
- Balancing Theory and Practice: Finding the right balance between classroom theory and hands-on clinical practice is a perpetual challenge. Nursing educators must ensure that students receive both the knowledge and practical skills necessary for safe and effective patient care.
- Diversity and Inclusion: Nursing education programs must address diversity and inclusion to prepare graduates to care for an increasingly diverse patient population. This includes fostering cultural competence among students.
- Workplace Realities: Preparing students for the realities of healthcare practice, including high patient loads, ethical dilemmas, and interprofessional teamwork, is crucial but can be challenging to simulate in an educational setting.
- Changing Healthcare Landscape: As healthcare delivery models evolve, nursing education must adapt to prepare nurses for new roles and responsibilities, such as telehealth and population health management.
- Evidence-Based Practice: Promoting evidence-based practice within nursing education programs and ensuring that graduates can apply research findings to clinical care is an ongoing challenge.
- Student Diversity: Nursing students come from diverse backgrounds and may have varying learning needs and preferences. Meeting the individual needs of a diverse student body can be a complex undertaking.
- Mental Health and Well-Being: The mental health and well-being of both nursing students and faculty are increasingly recognized as significant concerns. Addressing these issues within the educational environment is vital.
These challenges necessitate ongoing innovation, research, and collaboration within the nursing education community. Addressing these obstacles is essential to ensure that nursing education remains dynamic and responsive to the evolving healthcare landscape and that future nurses are well-equipped to provide safe and effective patient care.
PICOT Questions Examples on Nursing Education Challenges
- In nursing education programs (P), how does the incorporation of virtual simulation (I) compared to traditional clinical experiences (C) affect student clinical competency (O) within a semester (T)?
- In nurse educator training (P), what is the effect of incorporating mindfulness meditation (I) on reducing educator burnout (O) compared with standard training (C) within a year (T)?
- In undergraduate nursing curricula (P), how does the inclusion of cultural competence training (I) compared to no training (C) impact nursing students’ ability to provide culturally sensitive care (O) during their clinical rotations (T)?
- In nursing education programs (P), what is the effect of incorporating interprofessional education (I) on students’ teamwork and collaboration skills (O) compared to programs without such integration (C) within two semesters (T)?
- In nursing faculty development programs (P), how does the use of technology-enhanced teaching strategies (I) compared to traditional teaching methods (C) affect faculty members’ ability to engage and educate students effectively (O) within a year (T)?
- In nursing schools (P), what is the impact of increasing the clinical hours (I) compared to the standard clinical hours (C) on the clinical competence (O) of nursing graduates within their first year of practice (T)?
- In nursing education (P), how does the use of flipped classrooms (I) compared to traditional lecture-based teaching (C) affect students’ critical thinking skills (O) within a semester (T)?
- In graduate nursing programs (P), what is the effect of mentorship programs (I) on improving the transition from student to advanced practice nurse (O) compared to no mentorship (C) within six months (T)?
- In nursing education (P), how does the implementation of evidence-based practice (I) compared to traditional teaching methods (C) influence students’ ability to apply research findings to clinical practice (O) within one academic year (T)?
- In online nursing programs (P), what is the impact of increased faculty-student interaction (I) compared to minimal interaction (C) on student satisfaction and success (O) within a semester (T)?
You can also check out PICOT Questions Examples About Healthcare Technology Privacy and Security Concerns
Evidence-Based Practice (EBP) Project Ideas on Nursing Education Challenges
- Assess the effectiveness of virtual reality simulation in improving nursing students’ clinical skills.
- Implement and evaluate the use of standardized patients to enhance nursing student communication skills.
- Investigate the impact of debriefing techniques in simulation-based learning on students’ reflective practice and critical thinking.
- Examine the effectiveness of flipped classroom approaches in promoting active learning in nursing education.
- Develop and test strategies to address diversity and inclusion in nursing curricula.
- Evaluate the integration of interprofessional education into nursing programs and its impact on collaborative practice.
- Investigate the use of gamification in nursing education to enhance student engagement and learning outcomes.
- Assess the impact of mentorship programs on the professional development and retention of nursing faculty.
- Examine the role of technology-enhanced teaching methods in improving nursing faculty’s instructional effectiveness.
- Evaluate the use of simulation-based education in preparing nursing students for high-acuity clinical settings.
- Investigate the effects of cultural competence training on nursing students’ cultural awareness and competence.
- Develop and implement strategies to reduce educator burnout in nursing faculty.
- Assess the impact of telehealth education and training on nursing students’ readiness for telehealth practice.
- Evaluate the effectiveness of incorporating ethics education into nursing curricula on students’ ethical decision-making.
- Investigate the use of peer mentoring programs to support nursing students’ academic success.
- Examine the effects of incorporating resilience training into nursing education on students’ ability to cope with stress and adversity.
- Assess the impact of increased clinical hours on nursing students’ clinical competency and confidence.
- Investigate the influence of faculty-student interaction on online nursing students’ satisfaction and retention.
- Examine the implementation of evidence-based practice principles in nursing education and its impact on students’ research utilization.
- Evaluate the use of simulation-based education to improve nursing students’ leadership and teamwork skills.

Nursing Capstone Project Ideas on Nursing Education Challenges
- Developing a cultural competence training program for nursing students and evaluating its impact on their practice.
- Implementing and evaluating a peer mentoring program for new nursing students to enhance their transition to the clinical environment.
- Designing a faculty development program focused on incorporating innovative teaching strategies in nursing education.
- Investigating the use of technology-enhanced teaching methods in nursing education and their effects on student learning outcomes.
- Assessing the effectiveness of a standardized patient program in improving nursing students’ communication skills.
- Designing a resilience training program for nursing students and evaluating its impact on their ability to cope with stress.
- Developing a telehealth education curriculum for nursing students and assessing its effectiveness in preparing them for telehealth practice.
- Creating and evaluating an interprofessional education program for nursing and medical students to enhance collaborative practice.
- Investigating the impact of increased clinical hours on nursing students’ clinical competence and confidence.
- Designing and implementing a gamified learning module in nursing education and assessing its impact on student engagement and knowledge retention.
- Developing and evaluating a mentorship program for nursing faculty to support their professional development and well-being.
- Assessing the effects of incorporating ethics education into nursing curricula on students’ ethical decision-making.
- Designing a simulation-based leadership development program for nursing students and evaluating its impact on their leadership skills.
- Investigating the use of debriefing techniques in simulation-based learning and their effects on students’ reflective practice and critical thinking.
- Developing a diversity and inclusion curriculum for nursing programs and assessing its impact on students’ cultural competence.
- Creating and evaluating a flipped classroom approach in nursing education to promote active learning.
- Designing and implementing a tele-ICU training program for critical care nursing students and assessing its effectiveness.
- Investigating the impact of faculty-student interaction in online nursing programs on student satisfaction and retention.
- Developing and evaluating a mentorship program for nursing students to support their academic and clinical success.
- Assessing the influence of evidence-based practice principles in nursing education on students’ research utilization in clinical practice.
Other readers also checked out Nursing Research Paper Topics on Providing Care for LGBTQ Patients
Nursing Research Paper Topics on Nursing Education Challenges
- The Impact of Simulation-Based Education on Nursing Student Clinical Competency.
- Strategies for Enhancing Cultural Competence in Nursing Education.
- Faculty Development in Nursing: Meeting the Challenges of Modern Education.
- The Role of Technology in Nursing Education: Current Trends and Future Directions.
- Interprofessional Education in Nursing: A Pathway to Collaborative Practice.
- Mindfulness Meditation in Nurse Educator Training: Addressing Burnout and Promoting Well-Being.
- Flipped Classrooms in Nursing Education: Advancing Critical Thinking and Engagement.
- The Effects of Increased Clinical Hours on Nursing Student Preparedness for Practice.
- Peer Mentoring Programs in Nursing Education: Impact on Transition and Success.
- Gamification in Nursing Education: A Novel Approach to Learning.
- Strategies for Reducing Educator Burnout in Nursing Faculty.
- Telehealth Education for Nursing Students: Preparing for the Future of Healthcare.
- Ethics Education in Nursing Curricula: Shaping Ethical Decision-Making.
- The Use of Standardized Patients in Nursing Education: Improving Communication Skills.
- Resilience Training for Nursing Students: Enhancing Coping Skills.
- Incorporating Evidence-Based Practice in Nursing Education: Bridging the Research-Practice Gap.
- Tele-ICU Training for Critical Care Nursing Students: Preparing for High-Acuity Settings.
- Faculty-Student Interaction in Online Nursing Programs: Impact on Satisfaction and Retention.
- Mentorship Programs in Nursing Education: Supporting Professional Growth and Development.
- Diversity and Inclusion Initiatives in Nursing Curricula: Fostering Cultural Competence.
Nursing Research Questions on Nursing Education Challenges
- What are the key factors that influence the effectiveness of virtual reality simulation in nursing education?
- How does cultural competence training impact nursing students’ ability to provide culturally sensitive care?
- What teaching strategies are most effective in reducing educator burnout in nursing faculty?
- How can technology-enhanced teaching methods improve nursing faculty’s instructional effectiveness?
- What is the role of standardized patients in enhancing nursing students’ communication skills?
- How does interprofessional education influence collaborative practice among nursing and medical students?
- What is the impact of peer mentoring programs on new nursing students’ transition to clinical practice?
- How does the use of gamification affect student engagement and learning outcomes in nursing education?
- What are the outcomes of resilience training programs for nursing students in terms of stress management and well-being?
- How does telehealth education prepare nursing students for telehealth practice in different healthcare settings?
- What ethical dilemmas do nursing students encounter, and how does ethics education influence their decision-making?
- What are the advantages of flipped classrooms in promoting critical thinking and active learning among nursing students?
- How do increased clinical hours affect nursing students’ clinical competence and confidence?
- What is the impact of faculty-student interaction in online nursing programs on student satisfaction and retention?
- How do mentorship programs benefit nursing faculty in terms of professional development and retention?
- What is the relationship between evidence-based practice principles in nursing education and students’ research utilization in clinical practice?
- How does the use of debriefing techniques in simulation-based learning influence students’ reflective practice and critical thinking?
- What strategies can effectively address diversity and inclusion in nursing curricula to enhance cultural competence?
- What are the outcomes of implementing tele-ICU training for critical care nursing students in terms of preparedness for high-acuity settings?
- How do simulation-based leadership development programs impact nursing students’ leadership skills?
You can also check out Nurse-Patient Ratios Nursing Research Paper Topics Ideas
Nursing Essay Topic Ideas about Nursing Education Challenges
- The Role of Simulation-Based Education in Nursing: Advantages and Challenges.
- Cultural Competence Training in Nursing Education: Necessity and Impact.
- Faculty Development in Nursing: Strategies for Meeting Modern Education Demands.
- The Evolution of Technology in Nursing Education: Current Trends and Future Prospects.
- Interprofessional Education: Fostering Collaboration Among Healthcare Professionals.
- Mindfulness Meditation for Nurse Educators: Combating Burnout and Enhancing Teaching.
- Flipped Classrooms in Nursing Education: A Paradigm Shift in Learning.
- Clinical Competency of Nursing Graduates: The Debate on Increased Clinical Hours.
- Peer Mentoring Programs: Supporting New Nursing Students’ Transition to Clinical Practice.
- Gamification in Nursing Education: Enhancing Engagement and Learning.
- The Burnout Epidemic: Addressing Faculty Burnout in Nursing Schools.
- Telehealth Education: Preparing Nursing Students for the Digital Age of Healthcare.
- Ethics Education in Nursing Curricula: Shaping Ethical Nurses of Tomorrow.
- The Impact of Standardized Patients on Nursing Students’ Communication Skills.
- Resilience Training for Nursing Students: Coping with Stress in the Healthcare Environment.
- Evidence-Based Practice in Nursing Education: Bridging the Research-Practice Gap.
- Debriefing in Simulation-Based Learning: Enhancing Reflective Practice and Critical Thinking.
- Diversity and Inclusion Initiatives in Nursing Education: Fostering Cultural Competence.
- The Flipped Classroom Experience: Student Perspectives and Outcomes.
- Faculty-Student Interaction in Online Nursing Programs: A Catalyst for Success.
- Mentorship Programs for Nursing Faculty: Nurturing Professional Growth.
- The Impact of Increased Clinical Hours on Nursing Students’ Confidence and Competence.
- Simulation-Based Leadership Development: Cultivating Nursing Leaders of Tomorrow.
- Incorporating Mindfulness into Nursing Education: Promoting Well-Being and Resilience.
- Addressing Ethical Challenges in Nursing Practice: The Role of Ethics Education.
- Online Learning in Nursing Education: Advantages, Disadvantages, and Best Practices.
- The Benefits of Interprofessional Education: A Collaborative Approach to Healthcare.
- The Role of Technology in Enhancing Clinical Decision-Making Skills of Nursing Students.
- Cultural Competence in Nursing: A Necessity for Quality Patient Care.
Nursing Education Research Paper Examples
- Pros And Cons Of Mandatory Continuing Nursing Education
- Curriculum Development In Nursing Education
- Readiness as a DNP-Prepared Nurse Leader
- Role of DNP Prepared Nurse as Project Manager
- The Role of the DNP-Prepared Nurse Educator
Nursing education faces a multitude of challenges in preparing future nurses for the dynamic healthcare landscape. Addressing these challenges requires innovative approaches, evidence-based practices, and ongoing research efforts. The PICOT questions, EBP project ideas, capstone project ideas, research paper topics, research questions, and essay topic ideas presented in this article serve as a valuable resource for educators, researchers, and students in the field of nursing education. By focusing on these areas, we can advance nursing education, ultimately ensuring that nurses are well-equipped to provide the highest level of care to patients in an ever-evolving healthcare environment.
1. What is a critical challenge to nursing practice in the 21st century?
The National Advisory Council on Nurse Education and Practice identifies the following critical challenges to nursing practice in the 21st century: A growing population of hospitalized patients who are older and more acutely ill and increasing health care costs.
2. What are the recent trends in nursing research?
Findings: Six themes reflecting the current trends in nursing research were extracted: (a) demographic alterations; (b) increasing diversities and globalization; (c) technology innovation; (d) individualized or personal care and population health initiatives; (e) health policies and regulations;
3. What are the factors affecting nursing students?
Self-efficacy, gender, flipped learning education experience, learning satisfaction, age, and the analysis ability of the flipped learning class.
- Billings, D. M., & Halstead, J. A. (2019). Teaching in nursing: A guide for faculty (6th ed.). Saunders.
- Jeffries, P. R., & Rogers, K. J. (2020). Simulation in nursing education: From conceptualization to evaluation. National League for Nursing.
- Bastable, S. B. (2019). Nurse as educator: Principles of teaching and learning for nursing practice (5th ed.). Jones & Bartlett Learning.
- Harkreader, H., & Hogan, M. A. (2020). Fundamentals of nursing: Caring and clinical judgment (4th ed.). Elsevier.
- Duchscher, J. E. B. (2019). Transition shock: The initial stage of role adaptation for newly graduated registered nurses. Journal of Advanced Nursing, 65(5), 1103-1113.
- Ironside, P. M., & McNelis, A. M. (2017). Clinical education in nursing: Current practices, dilemmas, and challenges. National League for
Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Have a subject expert Write for You Now
Have a subject expert finish your paper for you, edit my paper for me, have an expert write your dissertation's chapter, what you'll learn.
- Nursing Careers
- Nursing Paper Solutions
- Nursing Theories
- Nursing Writing Guides
Related Posts
- Kathleen Masters Nursing Theories: A Framework for Professional Practice
- Rural Nursing Theory: A Guide for Nursing Students
- Barbara Resnick Nursing Theory: A Comprehensive Guide for Nursing Students
Important Links
Knowledge base.
Nursingstudy.org helps students cope with college assignments and write papers on various topics. We deal with academic writing, creative writing, and non-word assignments.
All the materials from our website should be used with proper references. All the work should be used per the appropriate policies and applicable laws.
Our samples and other types of content are meant for research and reference purposes only. We are strongly against plagiarism and academic dishonesty.
Phone: +1 628 261 0844
Mail: [email protected]

We Accept:

@2015-2024, Nursingstudy.org
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Global standards for professional nursing education: The time is now
Cynthia baker.
a Canadian Association of Schools of Nursing (CASN), Queens University, Canadian Association of Schools of Nursing, 1145 Hunt Club Rd, Suite 450, Ottawa K1V 0Y3, Canada
Ann H. Cary
b Marieb College of Health & Human Services, Florida Gulf Coast University, American Association of Colleges of Nursing, United States of America
Maria da Conceicao Bento
c Vocal de Desarrollo Institucional - Assocoación Latino Americana Escuelas y Faculadade de Enfermeria (ALADEFE), Portugal
A well-educated, professional nursing workforce is essential to good health care outcomes. Although nursing education is being strengthened globally, considerable diversity persists in the level and standards of nursing education both within and across countries. An international framework of guidelines for nursing education has, therefore, been developed to promote greater international consistency and high-quality nursing education globally.
The purpose of this paper is to discuss the multinational methodology used to develop a global framework for professional nursing education and the policy implications of this framework in guiding the harmonization of nursing education demanded by the State of the World's Nursing 2020 (WHO, 2020a) call to action. The framework includes the underpinning assumption that nurses be prepared at the baccalaureate level and three pillars of global expectations targeting: a) learning outcomes for graduating preservice nursing students; b) standards for nursing programs, and c) standards for educational institutions delivering nursing programs.
The Global Pillars Framework reflects international best practices, but the guidelines are adaptable across socio-cultural contexts facilitating the integration of locally relevant education. As 2020 has been declared the Year of the Nurse and Midwife globally, the ground has been laid for the next evolution in the education of the nursing workforce globally.
Introduction
The proportion of professionally prepared, baccalaureate nurses is significantly correlated with better health outcomes ( AACN, 2019 ; Aiken et al., 2017 ; Blegen et al., 2013 ). Globally 91% of countries report that standards for duration and content of nursing education exist and 89% of countries indicate they possess accreditation for education institutions ( WHO, 2020a ). However, considerable variation persists in the level and quality of education for registered nurses within the six World Health Organization (WHO) regions. Moreover, often variation exists within a single country ( Shaffer, 2013 ; WHO, 2020a ). The current complexity of health care demands that nursing education respond to a shift to higher levels of decision making, clinical judgement, team leadership, and political acumen enabling nurses to manage care in complex environments and across health care and social sector boundaries. In addition, nurses are an increasingly mobile workforce with one in eight not practicing in the country where they were born or educated ( WHO, 2020b ). Thus, there is an urgent international need for high quality guidelines to direct nursing education and for greater harmonization of entry level nursing education globally.
The Global Alliance for Nursing Education and Sciences (GANES) undertook a multinational methodology to develop global educational guidelines for preservice baccalaureate nursing education. This methodological approach will be described, and the policy implications of the Global Pillars Framework that emerged will be discussed.
Despite advances in health care, the global disease burden has increased. There are more people over 60 than children under five worldwide, which has been associated with a global increase in the prevalence of non-communicable chronic illnesses ( WHO, 2014 ). Communicable diseases however, including the current COVID-19 pandemic, once considered to have been vanquished by medical science, continue to take a devastating toll on communities. In addition, population mobility, armed conflict, and climate change are creating major health crises worldwide ( WHO, 2016 ).
Because nurses fulfill multiple roles in diverse settings and care for all age groups, the quality of their education is crucial to ensure health systems respond effectively to current health challenges ( All-Party Parliamentary Group on Global Health, 2016 ). Nurses are front line responders in health crises and disasters such as the COVID-19 pandemic, provide palliative and end-of-life care, educate and support individuals with chronic illness and their families, monitor patients who are acutely ill, and manage and respond to population health indicators and life threatening conditions in high acuity care settings. In addition, nurses promote population health, and prevent illness and injury among individuals, families, and communities ( GANES, 2019 ).
Level and quality of nursing education
Governments in several countries have undertaken measures to improve health services by enhancing the quality of nursing education. The global challenge facing nursing education programs resides in delivering transformed undergraduate curricula and practice learning opportunities to meet the new paradigms emerging in healthcare.
In response to these demands, an international trend in nursing education has been a shift from vocational training to professional education ( Collins & Hewer, 2014 ). Although some countries continue to provide only vocational training for nurses, an increasing number have instituted the baccalaureate degree as an entry-to-practice requirement for registered nurses ( WHO, 2020a ). For example, China has three entry levels for registered nurses - diploma, advanced diploma, and baccalaureate degree. Chinese policy and regulations recognize that high standards of nursing education are essential to meet the health demands of the population and the numbers of baccalaureate prepared nurses and nurses with graduate degrees have therefore increased ( Wang et al., 2016 ). While a number of countries in the European Union have considered a shift from vocational training to be unnecessary ( Collins & Hewer, 2014 ), the Bologna Accord, prompted a harmonization of educational processes to facilitate the mobility of nurses ( Shaffer, 2013 ), spurring a move to professional education as the requirement for nurses. Further, a national study of nursing education between 2011 and 2013 in South Africa, concluded that top-up, baccalaureate nursing degrees for diploma educated nurses needed to be developed to meet health care demands ( Comiskey et al., 2015 ). A Nursing Qualifications Framework was, therefore, created ( Blauw et al., 2014 ).
The most recent recommendations from the World Health Organization (WHO) and its partners assert that countries must modernize regulatory rules by harmonizing education requirements and standardizing nurses' credentials globally ( WHO, 2020b ). Undoubtedly, the preponderance of evidence demonstrates that the quality of nursing education affects health outcomes. Over the past decade international development aid to optimize health crises outcomes has been directed to nursing education. For example, in 2008 the US Congress made a commitment to enhance nursing education in Africa to achieve UNAIDS 90–90 goals that 90% of HIV positive people know their status, 90% diagnosed are on treatment and 90% on treatment are virally suppressed ( Michaels-Strasser et al., 2018 ). As a result, schools of nursing in the Democratic Republic of the Congo, Ethiopia, Lesotho, Malawi, South Africa, and Zambia were supported with infrastructure improvement, curricular revisions, clinical skill development, in- service training, and faculty development. However, the ground-breaking international study by the Lancet Commission on health professional education for the 21st century, called for curricula that are locally relevant as well as reflective of international best practices ( Frenk et al., 2010 ). Achieving successful implementation of high-quality standards internationally, therefore, is dependent upon ensuring that the standards not only represent best practices but are adaptable to local contexts and cultures.
The aim in creating the Global Pillars Framework was to provide guidelines for professional nursing education that are adaptable to differing sociocultural contexts while representing best practices ( GANES, 2019 ). It is important to recognize that 2020 has been declared by the WHO as the Year of the Nurse and Midwife; therefore the debut of the recommendations in the GANES document is a fitting tribute to enrich the quality of nursing education globally.
International standards for nursing education
Given the diversity in the level and quality of nursing education globally and the importance of well-educated nurses for optimum health care outcomes, strengthened international guidelines for nursing education are essential. As a result, the Global Alliance for Leadership in Nursing Education and Sciences (GANES) developed a Global Framework for Nursing Education to promote high quality, entry-level education for registered nurses worldwide ( GANES, 2019 ). This Global Framework offers guidance for executing recommendations in the State of the World's Nursing 2020 report ( WHO, 2020a )
The global framework specifies expectations for three interrelated pillars ( GANES, 2019 ).
- • Pillar I: Competency expectations for new graduates that are formulated as learning outcomes
- • Pillar II: Expectations for professional nursing education programs that are formulated as guidelines
- • Pillar III: Expectations for educational institutions that provide nursing education programs formulated as guidelines ( GANES, 2019 ).
Methodology
The modified Delphi methodology for developing national, consensus-based guidelines, standards, and competencies ( Schofield et al., 2018 ) was expanded to integrate multi-national engagement. This methodology involves a multi-step, iterative process of formulating and reformulating a knowledge product through input obtained from a wide variety of sources, including multiple stakeholders. This process is led by a panel of experts who come to a final consensus about the knowledge product.
In this initiative, the 12-member, doctoral prepared nursing education leaders of the GANES Board of Directors served as the international panel of experts guiding the development of the Global Pillars Framework. GANES members represented nursing education in South, Central, and North America, Spain, Portugal, and South Africa.
The development process involved 4 phases: 1) environmental scan and literature review; 2) stakeholder consultations; 3) validation survey; and 4) survey analysis and final revisions. The steps of the development process were carried out by a smaller working group of nurse educators in leadership positions from Canada, the United States, and Portugal ( GANES, 2019 ). Each step is described in greater detail.
Phase 1: environmental scan/literature review
The process began with a review of the grey literature on international and national guidelines for nursing education. Grey literature refers to information produced outside dedicated publishing channels such as journals. It includes policy papers, reports, newsletters, government documents, conference proceedings and so on. The following search terms guided the process: nursing education guidelines, and nursing education standards. Documents were retained if they were published by a national or international organization involved in nursing, health care or nursing education. Eighteen documents were reviewed and were supplemented by peer reviewed articles on nursing competencies. This literature informed a first draft of the Global Pillars Framework.
Following draft revisions, peer reviewed literature was retrieved using Medline and CINAHL to examine the research question: “How does the quality of nursing education affect health?” The key words guiding the search strategy were nursing education, global health, and, nursing education standards. The search was restricted to articles published between 2014 and 2019, which yielded 110 articles. We focused on the national and international literature written in English to gain insights. If a review of the abstract indicated a publication was concerned with voluntourism (a form of tourism in which students participate in voluntary work, typically for a charity), graduate level nursing education, or student exchange it was excluded. As a result, 31 articles were retained for analysis.
Drafts of the Global Pillars Framework were created based on the environmental scan and literature review and an initial consensus was reached by the panel of experts on the expectations of the three pillars.
Phase 2: stakeholder consultations
A series of face-to-face consultations with nursing educators were conducted by members of the working group at three international nursing conferences: the first in Miami, United States, the second in Barcelona, Spain, and the third in Lima, Peru ( GANES, 2019 ). At each of these sessions, from 35 to 50 educators who were present reviewed drafts of the pillars and provided feedback. The session in Lima Peru was conducted in Spanish and translated into English by a bilingual research assistant. Each consultation led to further revisions by the working group which were reviewed and, in some cases, modified by the panel of experts. Following the last consultation, a second draft version was adopted by the GANES panel of experts to be validated by an international sample of stakeholders ( GANES, 2019 ).
Phase 3: validation survey
Each of the GANES member organizations sent out a survey electronically to their respective networks in English, French, Spanish, and Portuguese, and a snowball sampling approach was used to reach a wide base of stakeholders ( GANES, 2019 ).
Survey respondents were asked to indicate their level of agreement with:
- a) the two assumptions underpinning the framework (entry-level nursing education must be at the baccalaureate level; and expectations of the framework must be adaptable to local contexts and support local population needs).
- b) each expectation stated in each of the global pillars.
Respondents were also invited to provide input on each of these as well as on the framework in general.
Survey sample
There were 357 respondents of the validation survey from Africa, Asia, Europe, the Middle East, and South, Central, and North America. As displayed in Table 1 , respondents self-identified as educators ( n = 278), employed in not-for-profit nursing roles ( n = 15), engaged in public sector employment (n = 27) or other types of nursing employment ( n = 37) ( GANES, 2019 ).
Respondents by region and type of employment.
| Nursing education employment | Other nursing employment | Total respondents | |
|---|---|---|---|
| Africa | 20 | 3 | 23 |
| Asia | 69 | 17 | 86 |
| Middle East | 1 | 1 | |
| Americas | 163 | 57 | 220 |
| Europe | 25 | 2 | 27 |
Phase 4: survey analysis and final revisions
It was predetermined that if there was less than 75% agreement with any assumption or expectation it would be removed. A descriptive statistical analysis was conducted of the level of agreement with each assumption and each expectation in the framework, and a content analysis of the written, open-ended feedback was carried out. Any further modifications of the framework were to be based on a systematic content analysis of stakeholders' comments.
Level of agreement
There was a very high level of agreement with all components of the framework with none reaching the <75% threshold for removal. More than 90% of respondents indicated that they either strongly agreed or agreed with 39 out of the 42 expectations, and with 1 of the 2 assumptions. Over 80% strongly agreed or agreed with the remaining three expectations in the pillars, and 77% agreed or strongly agreed with the second assumption ( GANES, 2019 ).
Content analysis of feedback
Ninety-nine (28%) of the respondents provided detailed open-ended feedback. All feedback was provided in English despite the diverse sample with native speakers of Spanish, Portuguese, and French who could select to respond to the survey in these languages.
The first step in analyzing their input was to extract all recommendations and categorize them into the following three groups ( GANES, 2019 ):
- 1) Convergent: recommendations from more than one person (20)
- 2) Single participant: recommendations from one person only (25)
- 3) Divergent: contradictory recommendations (5).
The next step was to further sub-categorize comments into the following 4 types of recommendation ( GANES, 2019 ):
- 1) clarify or specify an expectation;
- 2) add an expectation or add to an existing expectation;
- 3) remov e a concept/assumption;
- 4) change an expectation.
For convergent and single participant recommendations, 9 recommended clarification, 28 recommended additions, 3 recommended removal, and 5 recommended modifications. Three of the divergent recommendations were about changing an expectation albeit in opposing directions. Two were about removing or retaining a concept or assumption ( GANES, 2019 ).
Method to address recommendations
Although the application of a given rationale was subjective, an audit trail was kept that included the initial categorizations of the recommendation, whether and how it was addressed, and the specific rationale for the decision. This was submitted to the panel of experts to review along with the proposed modifications made by the working group.
A predetermined set of rationales provided the guidelines for the recommendations. Once the classification and sub-classification of respondents' feedback was completed, the recommendations to either add, clarify, remove, or change an expectation in each of the three categories ( convergent , single participant , divergent ) were reviewed and a decision made as to whether or not the input should be addressed. These were as follows: a) all convergent recommendations to clarify should be addressed; b) recommendations to add an expectation should be addressed if it refers to a broad area of nursing and is supported in current nursing education literature –it should not be addressed if the scope is narrow, the expectation is context dependent, or it applies to medicine rather than nursing; c) recommendations to remove a concept/assumption should be addressed if broadly supported in current nursing education literature; d) recommendations to make a change should be addressed if broadly supported in current nursing education literature ( GANES, 2019 ).
Revisions of convergent recommendations
Based on the guidelines, all convergent comments to clarify were addressed. All but one of the recommendations to add an expectation were addressed. This recommendation was not integrated into the framework because it was judged to be context dependent. In contrast, however, although several respondents recommended that simulation be removed from one expectation because not all countries have the technological capabilities to provide this, it was retained. The group rationalized that the retention of simulation includes non-computerized low fidelity simulation and globally available role-play and therefore, is not context dependent. There was only one convergent recommendation of a minor change: It was to replace knowledge , skills and abilities with knowledge , skills , and attitudes and this modification was made ( GANES, 2019 ).
Single participant recommendations
There were 20 single participant recommendations to add an expectation to standards or learning outcomes. Of these, 11 (55%) were addressed as broad areas of nursing supported by current nursing literature. The remaining 45% were either judged to be a) a narrow and specific concept/theme, b) focused on medicine rather than nursing, or c) not typically found in current nursing literature ( GANES, 2019 ).
Divergent recommendations
Finally, there were five divergent recommendations with contradictory recommendations about changing or removing an assumption or expectation ( GANES, 2019 ):
- 1) Increase level of research expectations/Reduce level of research expectations “Participating” in research was reduced to “using” research to inform practice. The rationale was based on current literature on nursing research and evidence-based practice ( GANES, 2019 ).
- 2) More on nursing theory/remove nursing theory
The term nursing theory was changed to nursing knowledge and the rationale based on current literature related to the discipline of nursing ( GANES, 2019 ).
- 3) Increase level of leadership expectations/reduce level of leadership expectations of students
The expectations related to nursing leadership skills were lowered and the rationale was based on current nursing literature regarding leadership ( GANES, 2019 ).
- 4) Baccalaureate Nursing (BN) unrealistic/BN should be the entry-to-practice qualification (an assumption of the pillars).
With over 75% agreement, the BN as entry-to-practice was retained. In addition, it was specifically supported by all stakeholders at each of the earlier face-to-face consultations ( GANES, 2019 ).
- 5) Internet and library use necessary and important/internet and library access unrealistic
– remove.
Internet and library access were retained despite the influence of context because evidence-informed practice is a key international best practice in nursing education ( GANES, 2019 ).
Rigor, trustworthiness, and limitations
The multilingual and multinational composition of the expert panel and stakeholders who provided input, the expertise and leadership roles of panel members, and the triangulation of data and methods represented integral components of the methodology supporting the credibility and trustworthiness of the findings. Adding to its confirmability and dependability, an audit trail was maintained detailing each step in the process and each revision of the Global Pillars Framework. The audit trail included the documentation of all coding steps, coding decisions, and the rationale for revisions. However, transferability, would have been strengthened if representatives of more linguistic and national groups had been members of the expert panel, and if the validation survey had involved a purposeful sample rather than a snowball sample of respondents. Despite the national diversity of the input obtained, some parts of the world were overrepresented, and others underrepresented or not represented. Similarly, while anglophones, francophones, Spanish and Portuguese speakers contributed to the development of the framework, major linguistic groups such as Mandarin and Arabic were unrepresented.
Global pillars
The collective experience and wisdom of the panel of experts and international stakeholders are reflected in the three pillars with quality expectations for nursing education that emerged from this process (See appendix A). Before discussing policy implications of the framework an overview of each pillar is presented,
Pillar 1: learning outcomes for graduates
The learning outcomes for graduates specified in Pillar l are classified under the following areas: 1) Knowledge and Practice Skills; 2) Communication and Collaboration; 3) Critical Thinking, Clinical Reasoning and Clinical Judgement; and 4) Professionalism and Leadership.
The specific learning outcomes encompassing Knowledge and Practice Skills target cognitive understanding of health sciences, mastery of locally relevant competencies, care of individuals across the life span, care of families and communities, care of clients in stable and unstable conditions, comfort care, pain and symptom management, end-of-life care, psycho- social and spiritual care; social determinants of health; culturally sensitive and culturally safe care; human rights, health equity, social justice and global awareness ( GANES, 2019 ).
The specific learning outcomes focused on Communication and Collaboration incorporate relational skills including empathy and reflection, effective interaction with individuals and families, accurate and timely care documentation, counseling and health education, and interprofessional and intersectoral collaboration ( GANES, 2019 ).
The Clinical Reasoning and Judgement learning outcomes address cognitive skills related to the use of evidence in practice, abilities to identify and interpret observations, and to recognize and respond to rapidly changing situations. Finally, the expectations under Professionalism and Leadership emphasize advocacy, ethical and professional behaviors, leadership, and the ability to influence public policy ( GANES, 2019 ).
Pillar ll: guidelines for educational programs
The guidelines of pillar II are directed at the educational program under the auspices of 1) Curriculum; 2) Admissions; and 3) Learning Experiences. Standards targeting the Curriculum include responsiveness to the local context and to the particular health needs of the population. They also include that key stakeholders provide input into the curriculum and that the curriculum is monitored and updated on a regular basis.
The Admissions construct directs attention to the alignment of student admission standards with resources as well as with academic and practice demands. In addition, it includes that admission policies be reviewed on a regular basis ( GANES, 2019 ).
Learning Experience guidelines include providing nursing students with increasingly complex learning opportunities, interprofessional education, practice through simulation and clinical placements in a variety of settings. They also include that gender and cultural influences be considered.
Pillar lll: guidelines for educational institutions
The guidelines for educational institutions that deliver nursing education programs are classified as: 1) Faculty, Instructors and Preceptors; 2) Resources; 3) Leadership and Administration; and 4) Outcomes.
The guidelines for Faculty, Instructors and Preceptors specify that faculty possess a graduate degree and expertise in the areas in which they teach. Similarly, they also specify that clinical instructors and preceptors possess expertise and experience in the area in which they are teaching and/or mentoring students. In addition, these guidelines specify that the number of students a faculty member, clinical instructor or preceptor is teaching in each classroom or online course, a laboratory course, or a clinical placement fosters optimum learning in accordance with evidence-based quality educational activities ( GANES, 2019 ).
Guidelines targeting the Resources of the educational institution include the need for library and internet resources for students to learn to use evidence to inform their practice and develop critical thinking skills. The institutional expectation necessitating possession of resources (material, pedagogical, and andragogical) needed to support optimum learning is explicit. In addition, the guidelines specify that the institution must have the financial resources to cover both the human and material expenses needed to sustain the educational program ( GANES, 2019 ).
In terms of the Leadership and Administration of the institution, the guidelines specify that the governance and administrative structure must be clearly defined and support a high- quality nursing education program. They also specify that the person responsible for the program must be a registered nurse who has a graduate degree. Guidelines also include that the leadership and administration collaborate effectively with health services to ensure optimum practice opportunities for student learning ( GANES, 2019 ).
The guidelines related to Outcomes focus on the implementation of an ongoing evaluation of the education program, the analysis of evaluation data, and the use of this data analysis to improve the institution, the program, and the student outcomes ( GANES, 2019 ).
Implications for nursing and health policy
Because the quality of nursing education is a critical determinant of the quality of nursing practice, the guidelines for nursing education in the Global Pillars Framework have the potential to execute the call to action to enhance nursing education, nursing care, and nursing services as illustrated in the State of the World's Nursing 2020 report ( WHO, 2020a ). At the policy level, the Global Pillars Framework offers direction to Ministries of Education, Labor, Health and Finance; educational institutions, accreditors, private sector and other funders who have been called to action by the WHO, International Council of Nurses, and Nursing Now to invest in nursing education that produces modernized graduates. The complexity of medicine, science, culture, and delivery systems needed to address population health undergird the tremendous responsibility of nursing education to graduate a well-prepared workforce globally. Policy makers across the globe can be responsive to their constituent and country values by incorporating the voices of nurses and place nurses in policy positions to support the application of this educational standards framework. It is well documented that nurses migrate across regions; therefore, the use of the Global Pillars and research-informed standards can harmonize the education and ultimately practice standards to recognize nurses' credentials globally.
Countries that seek to utilize nurses in specialties, advanced practice, as faculty, and as policy influencers and policy makers will benefit from focusing entry level nursing at the baccalaureate level using the Global Pillars as the initial direction. These Global Pillars ground the preparation of a baccalaureate prepared global workforce- a workforce that has been shown to reduce mortality and length of stay and lower health care costs in countries, predominately in acute care settings where the most expensive resource consumption exists. The science of nursing and nursing care demands clarity in the vision of nurses for the advocacy and policy influence expectations for their roles as they create, educate and influence legislative agenda for health in a country. Well educated nurses reflecting the Global Pillars competency outcomes will play pivotal roles in systems delivery improvements for nursing education globally.
Conclusions
The Global Pillars Framework provides guidelines to strengthen nursing education internationally and is in concert with the WHO State of the World's Nursing 2020 report. “Significant investment in education and training is required to match current and anticipated needs of health systems and meet national and subnational standards” ( WHO, 2020a , recommendation 101). These Pillars are based on a systematic, multinational methodology, reflect an international consensus among national leaders in nursing education, and build on the evidence in support of baccalaureate prepared nurses. They represent, therefore, a first step towards greater harmonization in nursing education internationally through generating discussion and execution among policy makers, nurses, and funders. The State of the World's Nursing 2020 report ( WHO, 2020a ) asserts the imminent challenge to the discipline of professional nursing: we must start now to create a harmonized and modernized nursing education approach to optimize nursing outcomes globally.
CRediT authorship contribution statement
Project design: CB., AC., MdaCB.
Data collection: CB., AC/. MdaCB.
Data analysis: CB.
Manuscript writing: CB., AC.
Critical revisions for important intellectual content: AC., MdaCB.
Declaration of competing interest
Acknowledgment.
The authors acknowledge the editorial review assistance of Dr. Krista Casazza, Associate Dean for Research at Florida Gulf Coast University, Marieb College of Health and Human Services as well as the GANES Board of Directors and the respondents whose input resulted in the final Global Pillars Framework.
Appendix A.
- 1.1.1 Apply nursing knowledge, health sciences including genetics, genomics and epigenetics, behavioral and social sciences, across the continuum of care.
- 1.1.2 Master locally relevant entry-to-practice competencies that reflect evidence-based international best practices.
- 1.1.3 Care for individuals across the lifespan, families, communities, and populations.
- 1.1.4 Manage and monitor complex care of clients in stable and unstable contexts to improve health outcomes.
- 1.1.5 Provide comfort care that addresses pain, symptom management, and psycho-social and spiritual needs throughout the illness trajectory including end-of-life.
- 1.1.6 Provide culturally sensitive, culturally safe, holistic, and person-centered care that integrates the social determinants of health.
- 1.1.7 Apply a global education perspective of human rights, health equity, social justice, global awareness, and the interconnectedness of systems.
- 1.2.1 Implement relational skills including listening, questioning, empathy, reflection, and sensitivity to emotional contexts when providing care.
- 1.2.2 Provide clear, accurate, timely, and appropriate documentation of care.
- 1.2.3 Communicate with empathy and respect in interactions with clients, families, members of the health care team, and others.
- 1.2.4 Counsel and provide information and health teaching to the client, family, and community.
- 1.2.5 Communicate effectively with members of the health care team.
- 1.2.6 Collaborate interprofessionally and intersectorally in the best interest of the client.
- 1.3.1 Systematically seek, interpret, and critically evaluate information, evidence, and practice observations.
- 1.3.2 Use research evidence in providing care.
- 1.3.3 Use clinical reasoning and problem solving to inform decision-making and caregiving in diverse practice settings.
- 1.3.4 Recognize and respond to rapidly changing client conditions and contexts including disasters.
- 1.4.1 Demonstrate a reflective understanding of ethical codes and ethical principles in providing care.
- 1.4.2 Practice within regulatory, legal, and ethical standards and contribute to a culture of patient safety.
- 1.4.3 Demonstrate the ability to analyze and influence public policy related to health.
- 1.4.4 Respond professionally to the needs of the individual, family, and community.
- 1.4.5 Demonstrate leadership skills in promoting health and influencing change.
- • Pillar ll Expectations for professional nursing education programs ( GANES, 2019 , p. 9–10)
- 2.1.1 Faculty teaching and student learning are guided by a curriculum that is systematically developed and reviewed.
- 2.1.2 The curriculum is responsive to the changing health care needs of the local population and the health care system.
- 2.1.3 Key stakeholders including employers, faculty, students, and alumni are consulted and provide input into curriculum development and review.
- 2.1.4 There is a systematic process for ongoing monitoring and improvement of the quality and relevance of the curriculum.
- 2.1.5 There is a systematic process for updating the curriculum as health needs, knowledge, and technology change.
- 2.2.1 Student enrollments are aligned with faculty resources to ensure high-quality education and responsiveness to the health care needs of the community.
- 2.2.2 Admission standards are set in relation to academic and practice demands, communicated clearly to applicants, and are respected.
- 2.2.3 Admission standards are reviewed regularly to ensure they meet current needs.
- 2.3.1 The education program includes practice experience through simulation and placements in a variety of clinical settings and with diverse populations.
- 2.3.2 Practice experiences are organized to provide students with increasingly complex learning opportunities.
- 2.3.3 Gender and cultural influences that may have an impact on learning are considered.
- • Pillar lll: Expectations for educational institutions that provide nursing education programs ( GANES, 2019 , p. 11–12)
- 3.1.1 Nursing faculty with graduate-level education and expertise in the areas in which they teach, ensure optimum delivery of the program in classroom, distance, laboratory, and clinical courses.
- 3.1.2 Nursing instructors and/or preceptors in practice settings possess clinical experience and expertise in the area in which they are instructing or mentoring students.
- 3.1.3 The number of students, in classroom, online/distance, laboratory, and clinical courses fosters optimum learning outcomes.
- 3.2.1 Library and internet resources support the development of evidence-informed practice and critical thinking among students.
- 3.2.2 Material, pedagogical, and andragogical resources support optimum learning outcomes.
- 3.2.3 Financial resources covering the human and material resources needed to deliver the program are sufficient to allow for the continuity of the program.
- 3.3.1 The governance structure is clearly defined and the administration actively supports the delivery of high-quality nursing education.
- 3.3.2 A registered nurse with a graduate degree is responsible for the nursing education program.
- 3.3.3 The leadership and administration of the nursing education program collaborate effectively with health service agencies to provide students with optimum practice learning opportunities.
- 3.4.1 An evaluation plan guides the assessment of the program, the educational institution, and the program outcomes.
- 3.4.2 There is ongoing implementation of the evaluation process and analysis of the evaluation data collected.
- 3.4.3 Evaluation data are used to improve the educational institution, the nursing education program, and student outcomes.
- Aiken L.H., Sloane D.M., McHugh M.D., Griffiths P., Rafferty A.M., Bruyneel L.M.…Sermeus W. Nursing skill mix in European hospitals: Association with mortality, patient ratings, and quality of care. BMJ Quality & Safety. 2017; 26 (7):559–568. doi: 10.1136/bmjqs-2016-005567. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- All-Party Parliamentary Group on Global Health Triple impact: How developing nursing will improve health, promote gender equality, and support economic growth. 2016, October. https://www.who.int/hrh/com-heeg/digital-APPG_triple-impact.pdf?ua=1&ua=1 Retrieved from.
- American Association of Colleges of Nursing Academic progression in nursing: Moving together toward a highly educated nursing workforce. 2019. https://www.aacnnursing.org/News-Information/Position-Statements-White-Papers/Academic-Progression-in-Nursing Retrieved from.
- Blauw W., Ditlopo P., Rispel L. Nursing education reform in South Africa: Lessons from a policy analysis study. Global Health Action. 2014; 7 (1) [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Blegen M.A., Hyde Park S., Goode C.J., Vaughn T.E., Spetz J. Baccalaureate education in nursing and patient outcomes. The Journal of Nursing Administration. 2013; 43 (2):89–94. doi: 10.1097/NNA.0b013e31827f2028. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Collins S., Hewer I. The impact of the Bologna process on nursing higher education in Europe: A review. International Journal of Nursing Studies. 2014; 51 (1):150–156. doi: 10.1016/j.nurstu.2013.07.005. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Comiskey C., Mathews A., Williamson C., Bruce J., Mulaiudzi M., Klopper H. Scaling up nurse education: An evaluation of a national PhD capacity development programme in South Africa in the context of the global shortage of nursing graduates. Nursing Education Today. 2015; 35 (5):647–652. doi: 10.1016/j.nedt.2015.01.003. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frenk J., Chen L., Bhutta Z., Chen J., Crisp N., Evans T.…Serwadda D. Education of health professionals for the 21st century. The Lancet. 2010; 375 https://www.thelancet.com/article/S0140-6736(10)61854-5/fulltext Retrieved from. [ PubMed ] [ Google Scholar ]
- Global Alliance for Leadership in Nursing Education and Science Global pillars for nursing education. 2019, June. https://ganes.info/ Retrieved from.
- Michaels-Strasser S., Smith J., Khanyola J., Sutton R., Price T., El Sadr W. Strengthening the quality and quantity of the nursing and midwifery workforce: Report on eight years of the NEPI Project. Annals of Global Health. 2018; 84 (1):31–35. doi: 10.29024/aogh.6. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schofield R., Chircop A., Baker C., Dietrich L., Duncan M.S., Wotton D. Entry-to-practice public health nursing competencies: A Delphi method and knowledge translation strategy. Nursing Education Today. 2018; 65 :102–107. doi: 10.1016/j.nedt.2018.030001. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shaffer F. Ensuring a global workforce: A challenge and opportunity. Nursing Outlook. 2013; 62 (1):1–4. doi: 10.1016/j.outlook.2013.08.001. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang C., Whitehead L., Byers S. Nursing education in China: Meeting the global demand for quality healthcare. International Journal of Nursing Sciences. 2016; 1 (3):131–136. 10.1016.ijmess.2016.02.009 Retrieved from. [ Google Scholar ]
- World Health Organization “Ageing well” must be a global priority. 2014. http://www.who.int/mediacentre/news/releases/2014/lancet-ageing- series/en/ Retrieved from.
- World Health Organization Global strategy of human resources for health: Workforce. 2016:2030. http://www.who.int/hrh/resources/globstrathrh-203-/en/ Retrieved from. [ Google Scholar ]
- World Health Organization . Author; Geneva, Switzerland: 2020. State of the world’s nursing 2020: Investing in education, jobs, and leadership. [ Google Scholar ]
- World Health Organization WHO and partners call for urgent investment in nurses. 2020. https://www.who.int/news-room/detail/07/04/2020-who-and-partners-call-for urgent-investment-in-nursesJune 26,2020 Retrieved from.
- Login/Register
- Terms and Conditions
- Privacy Policy
M.Sc Nursing 1st Year Question Papers Pdf Download
- Post author: Proudofnurses.com
- Post published: January 23, 2023
- Post category: M.Sc Nursing Question Papers
- Post comments: 0 Comments
M.Sc. Nursing 1st Year Question Papers
Download year-wise m.sc nursing 1st year question papers:.
Our website is proud to offer a wide variety of resources for nursing students, including the latest M.Sc nursing papers available for download. These papers have been carefully selected by experts in the field, and cover a range of topics that are relevant to the current nursing profession. Download your paper today and start exploring the nursing profession worldwide!”

We have listed out the papers year-wise.
[su_heading size=”41″ margin=”40″]M.Sc Nursing 1st Year Question Papers Pdf Download : 2021[/su_heading]
[su_heading size=”26″ margin=”40″]Year 2021 [/su_heading]
M.Sc Nursing 1st Year Question Papers
M.Sc. Nursing 1st Year Question Papers
Our website is the perfect resource for students and professionals looking for high-quality question papers in a variety of subjects & universities. We offer a wide range of question papers that are available for download in PDF format, allowing you to easily access and study them on your computer or mobile device. These question papers cover a wide range of topics and are designed to help you prepare for exams, assessments, and other important academic milestones. Whether you’re a student looking to improve your grades or a professional looking to advance your career, our question papers are the ideal resource for you. Download yours today and start your journey to success!
#Team: www.proudofnuses.com
Please Share This Share this content
- Opens in a new window
You Might Also Like

M.Sc Nursing 2nd Year Question Papers Pdf Download

LNCT – M.Sc Nursing 1st Year Question Papers Pdf Download
Leave a reply cancel reply.
Save my name, email, and website in this browser for the next time I comment.

RGUHS M.Sc Nursing 1st Year Question Papers Last 10 Years 2011-2021 || Rajiv Gandhi University of Health Sciences
- M.Sc Nursing
- Rajiv Gandhi University of Health Sciences
We uploaded RGUHS (Rajiv Gandhi University of Health Sciences) M.Sc Nursing (Master of Science in Nursing) second year (2nd year) 2021, 2020, 2019, 2018, 2017, 2016, 2015, 2014, 2013, 2012, 2011 and 2010 previous question papers. These papers are useful to all the Nursing colleges which are affiliated to Rajiv Gandhi University of Health Sciences.
Rguhs Last 10 Years 2011-2021 Previous Question Papers Download
We will keep on updating this post with latest papers. So, please bookmark this link and please do share this link with your friends
Note: Our team working on M.Sc Nursing 2021, 2018, 2014, and 2012 previous question papers
RGUHS M.Sc Nursing 1st Year (First Year) 2020 Previous Question Papers
9601 Advanced Concepts Of Health And Nursing Paper I Revised Scheme 2 Download 9606 9607 Biostatistics, Research Methodology And Nursing Research Revised Scheme 2 Download 9631 80] Nursing Education Rs3rs4 Download 9631 Nursing Education Rs3 Rs4 Download 9632 Advance Nursing Practice Rs3rs4 Download 9633 Nursing Research Rs3 Rs4 Download 9634 Statistics Rs3rs4 Download 9635 Medical Surgical Nursing Download 9635 Medical Surgical Nursing Rs3rs4 Download 9636 Community Health Nursing I Rs3rs4 Download 9637 Child Health Paediatric Nursing Rs3rs4 Download 9638 Obstetrics And Gynaecological Nursing Rs3rs4 Download 9638 Obstetrics And Gynecological Nursing Rs3rs4 Download 9639 Mental Health Psychiatric Nursing Rs3rs4 Download
2019 October
9601 Advanced Concepts of Health And Nursing Paper I Revised Scheme 2 Download 9606 9607 Biostatistics Research Methodology & Nursing Research Revised Scheme 2 Download 9606 9607 Biostatistics Research Methodology And Nursing Research Revised Scheme 2 Download 9631 Nursing Education Rs–3 And Rs4 Download 9632 Advance Nursing Practice Rs 3 And Rs 4 Download 9633 Nursing Research Rs 3 And Rs 4 Download 9634 Statistics Rs3 And Rs4 Download 9635 Medical Surgical Nursing Rs 3 And Rs 4 Download 9636 Community Health Nursing I Rs3 And Rs4 Download 9637 Child Health Paediatric Nursing Download 9639 Mental Health Psychiatric Nursing Rs3 and Rs4 Download
9613 Administration & Nursing Administration Revised Scheme 2 Download 9620 Paediatric Nursing II Revised Schemes 2 Download 9641 Cardio Vascular And Thoracic Nursing Revised Scheme 3 Download 9642 Critical Care Nursing Rs 3 and Rs 4 Download 9644 Neuro Sciences Nursing Revised Scheme 3 Download 9645 Medical Surgical Nursing Nephro Urology Nursing Rs 3 and Rs 4 Download 9646 Medical Surgical Nursing Ii Orthopaedic Nursing Revised Scheme 3 Download 9647 Gastro Enterology Nursing Rs 3 & Rs 4 Download 9648 Obstetrics And Gynecological Nursing II Revised Scheme 3 Download 9649 Paediatric Nursing Child Health Nursing Rs 3 & Rs 4 Download 9650 Psychiatric Mental Health Download 9651 Community Health Nursing II Rs3 & Rs4 Download
RGUHS M.Sc Nursing 1st Year (First Year) 2019 April Previous Question Papers
9601 Advanced Concepts Of Health And Nursing Paper I Revised Scheme 2 Download 9606 9607 Biostatistics Research Methodology And Nursing Research Revised Scheme 2 Download 9606 Biostatistics Research Methodology And Nursing Research Revised Scheme 2 Download 9631 Nursing Education Rs 3 And Rs4 NE Download 9632 Advance Nursing Practice Rs 3 And Rs 4 ANP Download 9633 Nursing Research Rs 3 And Rs 4 NR Download 9634 Statistics Rs 3 And Rs 4 Download 9635 Medical Surgical Nursing Rs 3 And Rs 4 MSN Download 9636 Community Health Nursing I Rs 3 And Rs 4 CHN Download 9637 RS 3 RS4 Child Health Paediatric Nursing CHPN Download 9638 80 Marks Obstetrics And Gynecological Nursing MOGN Download 9639 Mental Health Psychiatric Nursing Rs3 And Rs4 Download
RGUHS M.Sc Nursing 1st Year (First Year) 2017 May Previous Question Papers
9631 Nursing Education Rs 3 And Rs4 NE Download 9632 Advance Nursing Practice Rs 3 And Rs 4 ANP Download 9633 Nursing Research Revised Scheme 3 Download 9634 Statistics Rs3 And Rs4 Download 9635 Medical Surgical Nursing Rs 3 And Rs 4 MSN Download 9636 Community Health Nursing I Rs3 And Rs4 CHN Download 9637 RS 3 RS4 Child Health Paediatric Nursing CHPN Download 9638 80 Marks Obstetrics And Gynecological Nursing Download 9639 Mental Health Psychiatric Nursing Rs3 And Rs4 Download
RGUHS M.Sc Nursing 1st Year (First Year) 2016 April Previous Question Papers
9606 9607 Biostatistics Research Methodology And Nursing Research Revised Scheme 2 Download 9607-Biostatistics Download 9608 Nursing Speciality I Medical And Surgical Nursing Revised Scheme 2 Download 9609 Nursing Speciality I Community Health Nursing I Revised Scheme 2 Download 9612 Nursing Speciality I Obstetrics And Gynaecological Nursing I Revised Scheme 2 Download 9631 Nursing Education Rs3 AndRs4 NEA Download 9632 Advance Nursing Practice Rs 3 And Rs 4 ANP Download 9633 Nursing Research Revised Scheme 3 Download 9634 Statistics Rs3 And Rs4 Download 9635 Medical Surgical Nursing Rs 3 And Rs 4 MSN Download 9636 Community Health Nursing I Rs3 And Rs4 CHN Download 9637 Child Health Paediatric Nursing Download 9638 80 Marks Obstetrics And Gynecological Nursing Download 9639 Mental Health Psychiatric Nursing Rs3 And Rs4 Download
RGUHS M.Sc Nursing 1st Year (First Year) 2013 May Previous Question Papers
8401 Advanced Concepts Of Health And Nursing Paper I Revised Scheme Download 8421 Medical Surgical Nursing II Revised Scheme Download 9601 Advanced Concepts Of Health And Nursing Paper I Revised Scheme 2 Download 9603 Note Three Hours Given To Complete NTHGC Download 9606 Note Three Hours Given To Complete NTHGC Download 9608 Nursing Speciality I Medical And Surgical Nursing Revised Scheme 2 Download 9609 Nursing Speciality I Community Health Nursing I Revised Scheme 2 Download 9610 Nursing Speciality I Paediatric Nursing Revised Scheme 2 Download 9612 Nursing Speciality I Revised Scheme 2 Download 9631 Nursing Education Rs 3 And Rs 4 NE Download 9632 Advance Nursing Practice Rs 3 And Rs 4 Download 9633 Note Three Hours Given To Complete Download 9634 Note Three Hours Given To Complete Download 9635 Medical Surgical Nursing Rs 3 And Rs 4 MSN Download 9636 Community Health Nursing I Rs 3 And Rs 4 CHN Download 9637 Nursing Speciality I Paediatric Nursing Rs 3 And Rs 4 Download 9638 Obstetrics And Gynaecological Nursing Rs 3 And Rs 4 Download 9639 Mental Health Psychiatric Nursing Rs 3 And Rs 4 Download
If you face trouble opening any of the question paper or if you need any other paper, please drop us a mail to [email protected] with subject, university, semester details. We will send you the papers.
Above question papers are applicable for below affiliated colleges with Rajiv Gandhi University of Health Sciences – RGUHS
KLE College of Pharmacy
BVV Sangha’s Hanagal Shri Kumareshwar College of Pharmacy BVVS Ayurveda Medical College and Hospital Grameen Ayurvedic Medical College P.M. Nadagouda Memorial Dental College and Hospital – PMNMDCH Rural Ayurvedic Medical College and Research Centre S.Nijalingappa Medical College and H.S.K. Hospital and Research Centre Shri BVV Sangha Sajjalashri Institute of Nursing Science College Shri Kalidas Ayurvedic Medical College – SKAMC Shri Vijay Mahantesh Vidya Vardhak Sangha Ayurvedic Medical College and P.G. Center Sidramappa Danigond Ayurvedic College and Research Centre Sri Veer Pulikeshi Rural Ayurvedic Medical College Hospital and Research Centre
Abhaya College of Nursing Academy of Medical Education Dental College and Hospital – AMDC Acharya and BM Reddy College of Pharmacy Acharya Institutes of Health Sciences Aditya Bangalore Institute for Pharmacy Education and Research – ABIPER Aditya College of Nursing Adventist College of Nursing AECS Maaruti College of Dental Sciences and Research Centre AECS Maruthi College of Nursing AJ College of Nursing – AJCN Ambigara Chowdaiah College of Nursing Ambika School and College of Nursing Amrita Institute of Technology and Science Anupama School of Nursing Atreya Ayurvedic Medical College AVK (Adarsha Vidya Kendra) College of Nursing B.V.K.’s Shradha School of Nursing Babu Jagjivan Ram Dental College Banaswadi College of Nursing Bangalore City College of Nursing Bangalore City International College of Nursing Bangalore Medical College and Research Institute Bhagath College of Nursing Bhagawan Buddha Homoeopathic Medical College and Hospital Bhuvan Institute of Nursing Sciences BMS Hospital Nursing College – BMSHNC Brite College of Nursing Brite School of Nursing Capitol College of Nursing Chinai College of Nursing Chinai School of Nursing Chinmaya Institute of Nursing Christian College CMR College of Nursing – CMRCN CNK College of Nursing CNK Reddy College of Pharmacy Colaco Academy of Paramedical Sciences CR College of Pharmacy Dayananda Sagar College of Nursing – DSCN Dayananda Sagar College of Pharmacy Dayananda Sagar College Physiotherapy – DSCPT Diana College of Nursing Divine Grace Nursing Institute Dr. B.R. Ambedkar Institute of Nursing Dr. B.R. Ambedkar Medical College Dr. M.R. Ambedkar Dental College Dr. Syamala Reddy College and School of Nursing Dr. Syamala Reddy Dental College and Research Centre East Point College of Pharmacy – EPCP East West College of Pharmacy Eben-Ezer College of Nursing ESI Post Graduate Institute of Medical Science and Research Faran College and School of Nursing Father Mathews College of Nursing Florence College of Nursing – FCN Florence College of Physiotherapy Fortis Institute of Nursing Frank College of Nursing – FCN Gautham College of Pharmacy Gayathri College of Nursing Gayathri Institute of Nursing Sciences Global College of Nursing Golden College of Nursing Goldfinch College of Nursing Goutham College Gouthami College of Nursing Government College of Pharmacy Government Dental College and Research Institute – GDCRI Government Homoeopathic Medical College and Hospital Government Unani Medical College Harsha College of Pharmacy Harsha School and College of Nursing Hillside College of Nursing Hillside College of Pharmacy Hina College of Nursing Hina School of Nursing Hindustan College of Nursing – HCN Holy Mother Institute of Nursing Ikon Nursing School and College Indian Academy College of Nursing – IACN Indian Institute of Ayurvedic Medicine and Research – IIAMR Indian Institute of Nursing Indo Asian Academy’s Sri Krishna Rukmini College of Nursing Josco College of Nursing Jupiter School and College of Nursing Kamala College of Nursing – KCN, Kamala Krishna Royale Nursing College – KKRNC Karnataka College of Nursing Karnataka College of Pharmacy – KCP Kempegowda College of Nursing Kempegowda Institute of Medical Science Kempegowda Institute of Physiotherapy Kidwai Memorial Institute of Oncology – KMIO KKECS College of Pharmacy KLE Society’s Institute of Dental Sciences KMJ College of Nursing KNN College and School of Nursing Koshys College of Nursing Kote Group of Institutions KR Institute of Nursing Krupanidhi College of Nursing – KCON Krupanidhi College of Pharmacy Krupanidhi College of Physiotherapy KTG College of Nursing KTG College of Physiotherapy KTG Colllege of Nursing Laxmi Memorial College of Physiotherapy – LMCP M.S. Ramaiah College of Pharmacy M.S. Ramaiah Dental College – Faculty of Dental Sciences M.S. Ramaiah Institute of Nursing Education and Research M.S. Ramaiah Medical College Mahalakshmi College of Pharmacy Mahatma Gandhi Professional School of Nursing Mallige College of Pharmacy Mallige Institute of Pharmacy Manjunatha School of Nursing Manjushree College of Nursing Matru School and College of Nursing MES College of Pharmacy Milind Institute of Pharmacy Miranda College of Nursing Mobility India Rehabilitation Research and Training Centre Mother Teresa College of Nursing and School of Nursing MVJ College of Nursing MVM Suma Institute of Nursing Sciences Narayana Hrudayalaya College of Nursing Nargund College of Pharmacy Nargund College of Physiotherapy National Institute of Unani Medicine Navaneetham College of Nursing Nightingale Institute of Nursing Noor School and College of Nursing NU Trust College Oxford Medical College Hospital and Research Centre Padmashree College of Hospital Administration Padmashree College of Nursing Padmashree Institute of Medical Laboratory Technology Padmashree Institute of Nursing Padmashree School of Public Health PES College of Pharmacy PR College of Nursing Pragathi College and Institute of Nursing Prajwal College of Nursing Presidency College and School of Nursing Quality Health Care College of Nursing RajaRajeshwari Dental College and Hospital – RRDCH RajaRajeswari College of Nursing RajaRajeswari College of Physiotherapy RajaRajeswari Dental College and Hospital – RRDCH RajaRajeswari Medical College and Hospital – RRMCH Raman College of Pharmacy – RCP Ranebennur College of Nursing Roohi College and School of Nursing – RCSN RR College of Pharmacy RR Nursing Institutions Rural College of Pharmacy RV College of Nursing RV College of Physiotherapy S.B. School of Nursing S.E.A. College of Nursing Sambhram Institute of Medical Sciences and Research – SIMSAR Sapthagiri Institute of Medical Sciences and Research Centre – SIMSRC Sarojini College of Nursing – SCN Sarvodaya College of Nursing SB College of Nursing SBD Institute of Pharmacy Shantidhama School and College of Nursing Sharadadevi College of Nursing Shekhar College of Nursing Shiv Group of Institutions Shri Sharada Nursing College Shushruti College of Nursing – SCN Smt. Lakshmi Devi College of Nursing – SLDCN Smt. MC Vasantha College of Nursing Smt. Nagarathnamma College of Nursing Smt. Nagarathnamma School of Nursing Sneha College of Nursing Sofia College of Nursing Spurthy College of Nursing Sri Basavaraja Swamy College of Nursing Sri Basavaraja Swamy College of Nursing Sri Kalabyraveshwara Swamy College of Nursing and Hospital Sri Lakshmi College of Nursing Sri Raghavendra College of Nursing Sri Raghavendra College of Pharmacy – SRCP Sri Rajiv Gandhi College of Dental Sciences and Hospital Sri Ramakrishna College of Nursing Sri Sai College of Pharmacy Sri Sathya Sai Institute of Higher Medical Sciences – SSSIHMS Sri Sharada College of Nursing Sri Soubhagya Lalitha College of Nursing Sri Sri College of Ayurvedic Science and Research – SSCASR Sri Vagdevi School and College of Nursing Sri Venkateshwara College of Nursing – SVCN Sri Venkateshwara Dental College and Hospital – AVDCH Sri Vishnu School and College of Nursing St. George College St. John’s College of Nursing St. John’s Medical College St. John’s National Academy of Health Sciences St. John’s Pharmacy College St. John’s Research Institute – SJRI St. Martha’s College of Nursing St. Mary’s Institute of Nursing St. Theresa School of Nursing Subash College of Nursing Sushrutha Institute of Nursing SVN College of Nursing T. John College of Nursing T. John College of Pharmacy T. John School of Nursing The BSE College of Nursing The Oxford College of Nursing The Oxford College of Pharmacy The Oxford College of Physiotherapy The Oxford Dental College and Hospital Trident Educational Society’s Valley College of Pharmacy Universal College and School of Nursing Vagdevi School and College of Nursing Varalakshmi School and College of Nursing Vidyakirana Institute of Nursing Sciences – VINS Vijayanagar College and School of Nursing Visveswarapura Institute of Pharmaceutical Sciences Viswa Sai College of Nursing Viswa Sai School of Nursing Vivekananda College of Pharmacy Vokkaligara Sangha Dental College and Hospital Vydehi Institute of Medical Sciences and Research Centre Vydehi Institute of Pharmacy Wockhardt Institute of Nursing
Jai Narayan Vyas School of Pharmacy Belagavi KLE Society’s Institute of Nursing Sciences
Acharya Deshabhushan Ayurvedic Medical College and Hospital AM Shaikh Homoeopathic Medical College Belgaum Institute of Medical Sciences Bharatesh Homoeopathic Medical College KLE Society’s College of Pharmacy Maratha Mandal’s Dental College and Research Centre Maratha Mandal’s Nathajirao G. Halgekar Institute of Dental Sciences and Research Centre P.G. and Research Centre A.M. Shaikh Homoeopathic Medical College Parshwanath Doddanavar Bharatesh College of Nursing – PDBCN Rani Chennamma College of Pharmacy Rural Ayurveda Medical College Hospital and Research Centre S.B. Shirkoli Homoeopathic Medical College SCSES Shivabasavajyothi Homoeopathic Medical College SGV Ayurvedic Medical College Shree Shiv Basav Jyoti Homoeopathic Medical College, Hospital and Research Centre Shri BM Kankanwadi Ayurved Mahavidyalaya Shri JG Ayurvedic Medical College
Bellary Institute of Nursing Taranath Government Ayurvedic Medical College Togari Veeramallappa Memorial College of Pharmacy Vijayanagar Institute of Medical Sciences – VIMS, Bellary Bhilwara Genius Nursing College
Akkamahadevi College of Nursing Basaveshwar College of Pharmacy Bidar Bidar Institute of Medical Sciences HKDET Dental College Hospital and Research Institute N.K. Jabshetty Ayurvedic Medical College Nida College of Nursing RRK Samithi College of Pharmacy Rural College of Nursing S.B. Patil Dental College and Hospital Shri Veerbhadreshwar Education Trust College of Pharmacy Sri Siddarameshwara Ayurvedic Medical College Suleman College of Nursing – SCN SYE Society Sri Siddalingeshwar College of Pharmacy Vishwapalini College of Nursing
Al – Ameen Dental College Al – Ameen Fathima College of Nursing Al – Ameen Medical College AVS Ayurveda Mahavidyalaya Ayurveda Vidyalaya Samitis Ayurveda Mahavidyalaya BLDE Association’s Sri BM Patil College of Nursing and School of Nursing BLDE Association’s College of Pharmacy Dr. BNM Rural Ayurvedic Medical College Luqman Unani Medical College and Hospital Sushiladevi Nursing School & Siddeshwar College of Nursing Tulza Bhavani College of Nursing Chamarajnagar Manonidhi Institute of Nursing
Government Unani Medical College Chikmagalur Aroor Laxminarayana Rao Memorial Ayurvedic Medical College and PG Centre Chitradurga Amrutha Ayurvedic Medical College and Hospital Amrutha School of Nursing Chitradurga Basaveshwara College of Nursing Basaveshwara Medical College and Hospital SJM College of Pharmacy SJM Dental College and Hospital Sri Jagadguru Murugharajendra College of Pharmacy – SJM Chittoor Sapthagiri School of Nursing Davanagere Bapuji Pharmacy College College of Dental Sciences Kumuda College of Nursing S.S. Institute of Medical Sciences and Research Centre – SSIMS&RC S.S. Institute of Nursing Science SCS College of Pharmacy Shilpa School and College of Nursing SS Institute of Medical Sciences and Research Centre
Dr. B.D. Jatti Homoeopathic Medical College and Hospital Mahaganapati Ayurvedic Medical College Shri C.B. Guttal Ayurvedic Medical College and Hospital Shri CB Guttal Ayurvedic Medical College and Hospital Shri Dharmasthala Manjunatheshwara College of Medical Sciences and Hospital Soniya Education Trust College of Pharmacy Gadag Bhagwan Mahaveer Jain Ayurvedic Medical College DGM Ayurvedic Medical College and Hospital KLE Society’s College of Pharmacy Rajiv Gandhi Education Society’s Ayurvedic Medical College and Hospital Shri D.G. Melmalagi Ayurvedic Medical College and Hospital Shri SB Siddaling Shivacharya Swamigi Ayurvedic Medical College
Al – Badar Rural Dental College and Hospital Al Badar Dental College Al Kareem College of Nursing Al Qamar College of Nursing HKE Society College of Nursing HKE Society’s Dr. Malakreddy Homoeopathic Medical College and Hospital HKE Society’s College of Pharmacy KCT College of Pharmacy Khaja Bandanawaz Institute of Medical Sciences – KBNIMS Luqman College of Pharmacy Mahadevappa Rampure Medical College RME’s College of Pharmacy S. Nijalingappa Institute of Dental Science and Research Tipu Sultan Unani Medical College and Hospital – TSUMCH
DR Karigowda College of Pharmacy Hassan Institute of Medical Sciences Nisarga Institute of Nursing Science Rajeev College of Nursing Rathna College of Nursing Rathna School of Nursing Smt. NDRK College of Nursing Sri Dharmasthala Manjunatheshwara College of Ayurveda and Hospital Sri Hasanamba Dental College and Hospital Hoskote MVJ Medical College and Research Hospital Hubli Karnataka Institute of Medical Sciences – KIMS KLE University’s College of Pharmacy Sana Institute of Health Sciences
Alva’s College of Naturopathy and Yogic Sciences Alva’s Homoeopathic Medical College Karwar Institute of Medical Sciences Prasanna College of Nursing RNS College of Nursing SDM College of Naturopathy and Yogic Sciences Kolar AECS Pavan College of Nursing AECS Pavan College of Pharmacy KGF College of Dental Sciences and Hospital – KGFCDS Noorie College of Nursing Sambhram College and Institute of Nursing Sri Channegowda College of Nursing Sri Devaraj URS Medical College Sri K.V. College of Pharmacy Sri. Devraj URS School of Nursing Koppal Shri Jagadguru Gavisiddeshwara Ayurveda College and Hospital Mandya Adichunchanagiri College of Nursing Adichunchanagiri Institute of Medical Sciences – AIMS Bharathi College of Pharmacy Mandya Institute of Medical Sciences – MIMS Sri Adichunchanagiri College of Pharmacy Mangalore A. Shama Rao Nursing School AB Shetty Memorial Institute of Dental Sciences AJ Institute of Dental Sciences AJ Institute of Medical Sciences and Research Centre Athena College of Nursing City College of Physiotherapy City Hospital Research and Diagnostic Centre Dr. MV Shetty College of Medical Laboratory Technology Dr. MV Shetty College of Nursing Dr. MV Shetty College of Physiotherapy Father Muller College Allied Health Sciences Father Muller College of Nursing – FMCN Father Muller Homoeopathic Medical College Father Muller Medical College Karavali College of Nursing Science Karavali College of Pharmacy – KCOP Karnataka Ayurveda Medical College Kasturba Medical College Mangalore Laxmi Memorial College of Nursing – LMCN Mangalore Institute of Nursing Sciences Masood College of Nursing New Mangala College of Nursing Nitte Institute of Medical Laboratory Sciences Rukmini Shetty Memorial College of Nursing Sahyadri Institute of Health Sciences – SCHS SCS College of Nursing Sciences Shree Devi College of Nursing Shree Devi College of Pharmacy Shree Devi College of Physiotherapy Srinivas College of Pharmacy – SCP Srinivas College of Physiotherapy Srinivas Institute of Medical Sciences and Research Centre Srinivas Institute of Nursing Sciences – SINS Tejasvini Nursing Institute Unity Academy of Education Nursing Institute Unity Nursing Institute Vikas College of Physiotherapy Zulekha Nursing College – ZNC Manipal Krishna Muniyal Ayurvedic Medical College Muniyal Institute of Ayurveda Medical Sciences – MIAMS Udupi College of Nursing Moodbidri Alva’s Ayurvedic Medical College Alva’s College of Physiotherapy Alva’s Institute of Nursing Science – Alva’s College of Nursing
BGS Apollo Nursing College Cauvery College of Nursing and Health Science – Cauvery School of Nursing Farooqia Dental College Gopala Gowda Shanthaveri Memorial School and College of Nursing Government Nature Cure and Yoga College Holdsworth Memorial College of Nursing JSS Ayurveda Medical College and Hospital – JSSAMCH JSS College of Nursing JSS College of Physiotherapy Raman College of Nursing Sarada Vilas College of Pharmacy Sri Jayadeva Institute of Cardiovascular Sciences and Research Suraksha School of Nursing Vidya Vikas College of Nursing Vikram College of Nursing Vikram Institute of Nursing Vishwa Bharathi College of Nursing
Kalmathada Pujya Shri Virupaksha Shivacharya Ayurved Medical College and Hospital Navodaya College of Nursing Navodaya College of Paramedical Sciences Navodaya College of Physiotherapy Navodaya Dental College and Hospital Navodaya Medical College NET Pharmacy College NET Pharmacy College V.L. College of Pharmacy Ramanagara Dr. HLT College of Pharmacy MMU College of Pharmacy Patel College of Nursing Sri Nirvanaswamy College of Nursing – SNCN
Sai Paramedical College Sai Paramedical Institute
Bapuji Ayurvedic Medical College and Hospital Bapuji College of Nursing – BCN Mythri College of Nursing Sharavathi Dental College and Hospital Shimoga Institute of Medical Sciences – SIMS Tadikela Subbaiah College of Nursing TMAE Society’s Ayurvedic Medical College
KVG Ayurveda Medical College and Hospital KVG Dental College and Hospital KVG Medical College and Hospital
Akshaya College of Nursing Akshaya Nursing College Anirudh College of Nursing Aruna College of Nursing Ashwini Ayurvedic Medical College and Research Centre Ashwini Institute of Nursing Bharathi College of Nursing HMS Unani Medical College and Hospital Priyadarshini College of Pharmacy Shridevi Institute of Nursing Shridevi Institute of Para Medical Sciences Siddaganga Institute of Nursing Sciences and Research Centre Sowrabha Institute of Nursing Science Sree Siddaganga College of Pharmacy Sri Ramana Maharshi Institute of Nursing Science Sri Siddhartha Dental College Sri Siddhartha Medical College – SSMC Varadaraja Institute of Nursing Sciences
Canara College of Nursing City School of Nursing New City Hospital and Institution of Health Sciences SDM College of Ayurveda and Hospital Sri Dharmasthala Manjunatheshwara College of Ayurveda and Hospital Udupi Dhanvantari College of Nursing Vidya College of Health Sciences Vidya School of Nursing Vidyarathna College of Nursing
rguhs m.sc nursing 1st year question bank 5 years 2012 to 20 rguhs m.sc nursing 1st year solved question papers pdf m.sc nursing 1st year solved paper pdf m.sc nursing entrance exam solved question papers pdf m.sc nursing entrance exam question paper free download pdf m.sc nursing 1st year question papers first year m.sc nursing question papers rguhs m.sc nursing first year question bank 5 years 2012 to 20
rguhs m.sc nursing question papers
About The Author
FirstRanker.com is an educational site for all the B.Tech, B.E, M.E, B.Sc, M.Sc, B.Pharm, M.Tech, M.Pharm, MBA, MCA, MBBS, BDS, MD, Degree, Nursing students.
Add a Comment Cancel reply
Your email address will not be published. Required fields are marked *
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Nursing Education Research Paper Topics

Nursing education research paper topics are crucial for the development of the nursing profession. The field of nursing education is vast and encompasses a wide range of topics, from teaching and learning strategies to curriculum development and technology integration. Research in this area is essential for the continuous improvement of nursing education practices, which ultimately leads to better-prepared nurses and improved patient outcomes. This article will provide a comprehensive list of research paper topics in nursing education, as well as an in-depth article discussing the significance of nursing education and various aspects of it. Additionally, the article will present iResearchNet’s writing services, offering students the opportunity to order a custom nursing education research paper on any topic.
100 Nursing Education Research Paper Topics
The significance of nursing education cannot be overstated. It is a critical component in the preparation of nursing professionals who are competent, compassionate, and prepared to meet the diverse health needs of populations worldwide. Nursing education encompasses a wide range of topics, from theories and concepts to curriculum development, teaching and learning strategies, assessment and measurement, simulation, technology integration, continuing education, leadership and management, legal and ethical issues, and innovations and future trends. Research in these areas is vital for the continuous improvement and evolution of nursing education, ultimately leading to better-prepared nurses and improved patient outcomes. This section provides a comprehensive list of nursing education research paper topics, divided into ten categories.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code.
Theories and Concepts in Nursing Education
- The role of self-efficacy in nursing education.
- Applying adult learning theories in nursing education.
- The impact of constructivism on nursing education.
- The relevance of social learning theory in nursing education.
- The influence of transformative learning in nursing education.
- Critical thinking development in nursing education.
- The role of reflective practice in nursing education.
- The importance of emotional intelligence in nursing education.
- The impact of experiential learning in nursing education.
- The role of cognitive load theory in nursing education curriculum.
Curriculum Development and Evaluation
- The impact of competency-based education on nursing curriculum.
- Strategies for integrating cultural competence in the nursing curriculum.
- The role of evidence-based practice in nursing curriculum development.
- The impact of interprofessional education on nursing curriculum.
- Strategies for integrating mental health into the nursing curriculum.
- The role of simulation in nursing curriculum development.
- Strategies for integrating community health nursing into the curriculum.
- The impact of global health education on nursing curriculum.
- Strategies for developing a culturally inclusive nursing curriculum.
- The role of accreditation standards in nursing curriculum development.
Teaching and Learning Strategies
- The effectiveness of case-based learning in nursing education.
- The impact of problem-based learning on nursing students’ critical thinking skills.
- The role of team-based learning in nursing education.
- The effectiveness of flipped classroom in nursing education.
- The impact of online learning on nursing education.
- Strategies for promoting active learning in nursing education.
- The role of clinical reasoning in nursing education.
- The effectiveness of peer teaching in nursing education.
- The impact of concept mapping on nursing students’ learning outcomes.
- Strategies for promoting self-directed learning in nursing education.
Assessment and Measurement in Nursing Education
- The effectiveness of formative assessment in nursing education.
- The impact of summative assessment on nursing students’ learning outcomes.
- The role of self-assessment in nursing education.
- The effectiveness of peer assessment in nursing education.
- The impact of objective structured clinical examination (OSCE) in nursing education.
- Strategies for promoting authentic assessment in nursing education.
- The role of portfolio assessment in nursing education.
- The effectiveness of simulation-based assessment in nursing education.
- The impact of written examinations on nursing students’ learning outcomes.
- Strategies for promoting continuous assessment in nursing education.
Simulation in Nursing Education
- The effectiveness of high-fidelity simulation in nursing education.
- The impact of simulation on nursing students’ clinical reasoning skills.
- The role of simulation in developing nursing students’ communication skills.
- The effectiveness of simulation in teaching nursing procedures.
- The impact of simulation on nursing students’ self-confidence.
- Strategies for promoting realism in simulation-based nursing education.
- The role of debriefing in simulation-based nursing education.
- The effectiveness of simulation in interprofessional education.
- The impact of simulation on nursing students’ decision-making skills.
- Strategies for integrating simulation into the nursing curriculum.
Technology Integration in Nursing Education
- The effectiveness of virtual reality in nursing education.
- The impact of mobile applications on nursing education.
- The role of e-learning in nursing education.
- The effectiveness of online discussions in nursing education.
- The impact of electronic health records on nursing education.
- Strategies for promoting digital literacy in nursing education.
- The role of social media in nursing education.
- The effectiveness of computer-based simulations in nursing education.
- The impact of telehealth on nursing education.
- Strategies for integrating technology into the nursing curriculum.
Continuing Education and Lifelong Learning
- The effectiveness of continuing education programs for nurses.
- The impact of lifelong learning on nurses’ professional development.
- The role of continuing education in maintaining nursing competency.
- The effectiveness of online continuing education for nurses.
- The impact of continuing education on nurses’ job satisfaction.
- Strategies for promoting a culture of lifelong learning among nurses.
- The role of professional associations in continuing education for nurses.
- The effectiveness of certification programs in nursing.
- The impact of continuing education on nurses’ clinical practice.
- Strategies for integrating continuing education into nurses’ professional development plans.
Leadership and Management in Nursing Education
- The effectiveness of leadership development programs for nursing students.
- The impact of leadership styles on nursing students’ learning outcomes.
- The role of mentorship in developing nursing leaders.
- The effectiveness of management training for nurse educators.
- The impact of leadership and management education on nurses’ job satisfaction.
- Strategies for promoting a culture of leadership among nursing students.
- The role of leadership in promoting a positive learning environment.
- The effectiveness of leadership in promoting interprofessional collaboration.
- The impact of leadership on nursing students’ clinical practice.
- Strategies for integrating leadership and management education into the nursing curriculum.
Legal and Ethical Issues in Nursing Education
- The effectiveness of ethics education in nursing.
- The impact of legal education on nursing students’ clinical practice.
- The role of ethics and legal education in developing nursing students’ decision-making skills.
- The effectiveness of ethics and legal case studies in nursing education.
- The impact of ethics and legal education on nurses’ professional development.
- Strategies for promoting a culture of ethical practice among nursing students.
- The role of professional codes of ethics in nursing education.
- The effectiveness of ethics and legal education in preventing malpractice.
- The impact of ethics and legal education on nurses’ job satisfaction.
- Strategies for integrating ethics and legal education into the nursing curriculum.
Innovations and Future Trends in Nursing Education
- The effectiveness of innovative teaching strategies in nursing education.
- The impact of emerging technologies on nursing education.
- The role of innovation in promoting a positive learning environment.
- The effectiveness of innovative assessment strategies in nursing education.
- The impact of innovation on nursing students’ learning outcomes.
- Strategies for promoting a culture of innovation among nursing students.
- The role of innovation in promoting interprofessional collaboration.
- The effectiveness of innovation in promoting self-directed learning.
- The impact of innovation on nurses’ professional development.
- Strategies for integrating innovation into the nursing curriculum.
Research in nursing education is essential for the continuous improvement and evolution of nursing education practices. The diverse range of nursing education research paper topics listed above provides a solid foundation for exploring various aspects of nursing education, from theories and concepts to curriculum development, teaching and learning strategies, assessment and measurement, simulation, technology integration, continuing education, leadership and management, legal and ethical issues, and innovations and future trends. It is encouraged that students and researchers explore these topics in-depth to contribute to the body of knowledge in nursing education and ultimately lead to better-prepared nurses and improved patient outcomes.
Rhe Range of Nursing Education Research Paper Topics
Nursing education holds immense significance in the healthcare sector. It serves as the foundation for preparing competent and compassionate nursing professionals who play a pivotal role in ensuring the health and well-being of individuals and communities worldwide. Nursing education involves a comprehensive approach that encompasses various aspects such as curriculum development, teaching and learning strategies, technology integration, assessment and measurement, simulation, continuing education, leadership and management, legal and ethical issues, and innovations and future trends. This article aims to discuss the significance of nursing education and examine various aspects of it, highlighting a range of nursing education research paper topics.
Significance of Nursing Education
Nursing education is the cornerstone of preparing nursing professionals who are equipped with the knowledge, skills, and attitudes necessary to provide high-quality care to patients. It involves not only the transmission of knowledge but also the development of critical thinking, decision-making, communication, and clinical skills. Nursing education prepares nurses to work in various healthcare settings, from hospitals and clinics to community health centers and home care. It also instills a commitment to lifelong learning, professional development, and ethical practice. Moreover, nursing education plays a crucial role in addressing the current and future challenges faced by the healthcare system, such as the increasing prevalence of chronic diseases, aging population, healthcare disparities, and the need for interprofessional collaboration.
Curriculum Development
Curriculum development in nursing education involves the design and organization of educational experiences to achieve the desired learning outcomes. It encompasses the identification of competencies, development of learning objectives, selection of content, organization of learning experiences, and evaluation of learning outcomes. Curriculum development is a dynamic process that requires continuous evaluation and revision to ensure its relevance, effectiveness, and alignment with the needs of the students, healthcare system, and society. Some of the nursing education research paper topics related to curriculum development include:
Teaching and learning strategies in nursing education involve the selection and implementation of methods and activities that facilitate the achievement of learning objectives. These strategies can vary from traditional lectures and discussions to more interactive and innovative approaches such as case-based learning, problem-based learning, team-based learning, flipped classroom, online learning, simulation, and peer teaching. The selection of teaching and learning strategies should consider the characteristics of the learners, the nature of the content, and the context in which the learning occurs. Some of the nursing education research paper topics related to teaching and learning strategies include:
Technology Integration
Technology integration in nursing education involves the use of technology to enhance the teaching and learning process. It encompasses a wide range of tools and applications, from computers and mobile devices to virtual reality, simulation, electronic health records, and telehealth. Technology integration can facilitate access to information, promote interactive and self-directed learning, enhance clinical reasoning and decision-making skills, and prepare nursing students for the technology-rich healthcare environment. However, it also poses challenges related to digital literacy, privacy and security, and equitable access to technology. Some of the nursing education research paper topics related to technology integration include:
In conclusion, nursing education is of paramount importance in preparing competent and compassionate nursing professionals who can address the current and future challenges faced by the healthcare system. It involves various aspects such as curriculum development, teaching and learning strategies, and technology integration, each of which offers a range of nursing education research paper topics for exploration. Conducting research in these areas can contribute to the continuous improvement and evolution of nursing education practices, ultimately leading to better-prepared nurses and improved patient outcomes.
iResearchNet’s Custom Writing Services
In the world of academia, writing research papers is a fundamental and unavoidable task. This is particularly true for nursing students, who must not only master the complex body of knowledge associated with their field but also actively contribute to it through original research. Unfortunately, many students find themselves overwhelmed by the demands of their nursing programs, and struggle to find the time, resources, or expertise needed to complete their research papers to a high standard. That’s where iResearchNet comes in. Our company is dedicated to providing customized writing services to students in need, and we specialize in helping nursing students tackle the vast array of nursing education research paper topics.
- Expert Degree-Holding Writers : Our team is comprised of professional writers, all of whom hold advanced degrees in their fields. This ensures that they have the knowledge and expertise necessary to provide high-quality content on a wide range of nursing education research paper topics.
- Custom Written Works : Each paper we produce is crafted from scratch, according to the specific requirements and guidelines provided by the client. This ensures that the final product is not only of high quality but also entirely original and tailored to the client’s needs.
- In-Depth Research : Our writers are trained to conduct thorough and meticulous research using reliable and up-to-date sources. This ensures that the papers we produce are well-informed and grounded in the latest scientific knowledge and research.
- Custom Formatting : We understand that different institutions and professors have different requirements when it comes to formatting. That’s why we offer custom formatting services to ensure that your paper adheres to the specific formatting guidelines of your institution, whether it be APA, MLA, Chicago/Turabian, or Harvard style.
- Top Quality : We take pride in the quality of the work we produce. Our writers are not only knowledgeable and experienced but also dedicated to producing the highest quality work possible. This means well-researched, well-written, and well-formatted papers that meet or exceed the client’s expectations.
- Customized Solutions : We understand that each client and each research paper is unique. That’s why we offer customized solutions to meet the individual needs of each client. Whether you need help with selecting a topic, conducting research, writing, editing, or formatting, we can provide the support you need.
- Flexible Pricing : We offer flexible pricing options to accommodate the budgetary constraints of our clients. Our pricing is based on the complexity of the project, the level of expertise required, and the deadline for completion.
- Short Deadlines : We understand that sometimes deadlines can creep up on you, and you may find yourself in need of urgent help. That’s why we offer the option to complete orders with a deadline as short as three hours.
- Timely Delivery : We understand the importance of meeting deadlines, and we make it a priority to deliver all orders on time. This ensures that you have ample time to review the work and request any necessary revisions.
- 24/7 Support : Our customer support team is available 24/7 to address any questions, concerns, or issues you may have. Whether you need help with placing an order, have a question about our services, or need assistance with an ongoing project, we are here to help.
- Absolute Privacy : We take your privacy very seriously. All personal and payment information provided by our clients is kept strictly confidential and is never shared with third parties.
- Easy Order Tracking : Our user-friendly online platform allows you to easily track the progress of your order, communicate with your writer, and access all the necessary documents and files.
- Money-Back Guarantee : We are confident in the quality of the work we produce, but we also understand the importance of providing a safety net for our clients. That’s why we offer a money-back guarantee. If you are not satisfied with the final product, and we are unable to rectify the situation, we will provide a full refund.
In conclusion, iResearchNet is your one-stop-shop for all your research paper needs. With our team of expert degree-holding writers, custom written works, in-depth research, and a host of other features, we are equipped to provide top-quality customized solutions for a wide range of nursing education research paper topics. Whether you are struggling to find a topic, conduct research, write, edit, or format your paper, we can provide the support you need. Our flexible pricing, timely delivery, 24/7 support, absolute privacy, easy order tracking, and money-back guarantee ensure that you can place your order with confidence. Don’t hesitate to reach out to us for help with your nursing education research paper. We are here to support you every step of the way.
Unlock Success with iResearchNet
Are you struggling with your nursing education research paper? Overwhelmed by the vast array of topics, the intricacies of research, or the rigors of formatting? Don’t let the stress get to you! iResearchNet is here to help. Our comprehensive writing services are designed to provide support at every stage of the research paper writing process. From selecting a topic to conducting research, from writing to editing, from formatting to final review, our team of expert degree-holding writers is equipped to provide customized solutions to meet your specific needs. With our flexible pricing, timely delivery, 24/7 support, and money-back guarantee, you can place your order with confidence. Don’t miss out on the opportunity to submit a high-quality research paper that will impress your professors and set you on the path to success.
Success is not just about talent or luck; it is about making smart choices and taking control of your destiny. One smart choice you can make is to seek help when you need it. If you are struggling with your nursing education research paper, don’t hesitate to reach out for help. iResearchNet is here to provide the support you need to overcome the challenges you face and achieve your goals. Our comprehensive writing services are designed to provide customized solutions for a wide range of nursing education research paper topics. Whether you need help with selecting a topic, conducting research, writing, editing, or formatting, we have the expertise and resources to help you succeed. Take control of your success by ordering a custom nursing education research paper from iResearchNet today!
ORDER HIGH QUALITY CUSTOM PAPER


IMAGES
VIDEO
COMMENTS
Download M.Sc Nursing question papers for 1st and 2nd year from 2009 to 2021 for various universities in India. Find the links to previous papers, syllabus, and exam pattern for M.Sc Nursing.
Practice your nursing skills with free interactive quizzes and sample tests on various topics, such as dosage calculations, pharmacology, pediatrics, EKG, and more. Find quizzes for nursing students and current nurses to prepare for HESI, NCLEX, or other exams.
Learn about the four major Client Needs categories that organize the content of the NCLEX-RN exam: Safe and Effective Care Environment, Health Promotion and Maintenance, Psychosocial Integrity, and Physiological Integrity. Review free practice questions by category and improve your test preparation.
Psychosocial Integrity. Basic Care and Comfort. Pharmacological and Parenteral Therapies. Reduction of Risk Potential. Physiological Adaptation. Questions Available: 0. Number of Questions. Start Test. Nursing Careers.
Access free NCLEX practice questions by topic, from clinical skills to pharmacology, written by former NCLEX question writers. Prepare for the 2024 NCLEX exam with overviews, study tips, and detailed answers.
Take a practice NCLEX-RN exam with 200+ questions and rationales organized by client needs categories. Test your knowledge and skills in management of care, safety and infection control, health promotion and maintenance, psychosocial integrity, and physiological integrity.
Throughout the coming decade, it will be essential for nursing education to evolve rapidly in order to prepare nurses who can meet the challenges articulated in this report with respect to addressing social determinants of health (SDOH), improving population health, and promoting health equity. Nurses will need to be educated to care for a population that is both aging, with declining mental ...
Find out what a nursing research paper is, how to choose a topic, and what topics are best for nursing students in 2024. Explore clinical, community, education, mental health, pediatric, and nursing profession research topics with examples and tips.
Paper III. Biostatistics and Research Methods (including Nursing Research Methods) 1990-2000. 2001-2011. MASTER OF SCIENCE (M.Sc.) NURSING DEGREE EXAMINATIONS. SECOND YEAR. (Regulations For Candidates Admitted From 2008-2009 Onwards) PAPER. SUBJECT.
Click on the question to reveal the answer. Chapter 1: What is nursing and what is nursing? Chapter 2: Being a nursing student. Chapter 3: Core academic skills. Chapter 4: Academic writing and assessment skills. Chapter 5: Ethics. Chapter 6: Law. Chapter 7: Accountability and professionalism. Chapter 8: Resilience.
This document contains a 20 question multiple choice nursing education assessment. The questions cover topics like Bloom's taxonomy, types of educational assessments, examples of criterion-referenced assessments, influential nursing education theorists, milestones in the development of nursing education in India, characteristics of problem-based learning, types of teaching methods, steps in ...
Download previous question papers of Post Basic B.Sc Nursing (PBB-Sc Nursing) 2nd year exam conducted by various universities in India. Find question papers of Sociology, Community Health Nursing, Mental Health Nursing, Introduction to Nursing Education and Administration.
Nursing - BSc Nursing 5th Semester (BSc Nursing) - Notes, Important Questions, Study Material, Question Bank, Semester Question paper PDF Download. 5th Semester 3rd Year. Child Health Nursing I including Essential Newborn Care (ENBC), FBNC, IMNCI and PLS, modules - N-CHN (I) 301.
Find the question papers of Post Basic B.Sc. Nursing for first and second year from 1990 to 2023. The question bank covers various subjects such as Nursing Foundation, Nutrition and Dietetics, Biochemistry and Biophysics, Psychology, Maternal Nursing, Child Health Nursing, Microbiology, Medical Surgical Nursing, English, Sociology, Community Health Nursing, Mental Health Nursing, Nursing ...
Examine the implementation of evidence-based practice principles in nursing education and its impact on students' research utilization. Evaluate the use of simulation-based education to improve nursing students' leadership and teamwork skills. Nursing Education Topics, Ideas, and Research Paper Examples 1.
The purpose of this paper is to discuss the multinational methodology used to develop a global framework for professional nursing education and the policy implications of this framework in guiding the harmonization of nursing education demanded by the State of the World's Nursing 2020 (WHO, 2020a) call to action.
Find the latest M.Sc nursing papers for various subjects and years on this website. Download the question papers in PDF format and prepare for exams and assessments.
SECTION - A. I. Answer All Questions. Each answer in one or two sentences: (15 x 1 = 15) List out functions of Indian Nursing Council. Mention any four theories of organizational behaviours. Define regulatory bodies. List out the steps of staffing process. Enlist the types of records. Define deployment.
Download previous question papers of RGUHS M.Sc Nursing 1st year exams from 2011 to 2021. Find papers for nursing education, nursing research, nursing practice and more subjects.
First M.Sc. Nursing Examination, Summer 2018 NURSiNG RESEARCH AND STATISTICS — IV Total Duration: Section I + II = 3 Hours Total Marks : 75 SECTION — I and SECTION — II. Instructions : 1) Use blue/black ball point pen only. 2) Do not write anything on the blank portion of the question paper.
Find e-questions for B.Sc. Nursing degree examinations from 2007 to 2016. Browse the papers by year and subject for each semester.
Find a comprehensive list of research paper topics in nursing education, from theories and concepts to curriculum development and technology integration. Learn how to order a custom nursing education research paper on any topic from iResearchNet's writing services.
Basic B.Sc. Nursing II (Second ) Semester Examination 20 21 -22. ination 2021-22Course Code: NNF125/HNIT145Paper ID: 08022245 Applied Nursing Foundation II Including H. t Module /Health Nursing Informatics & TechnologyTime: 3 HoursNote: At. empt. both the Part.