An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Knowledge, Attitude, and Practice toward Food Poisoning among Food Handlers and Dietetic Students in a Public University in Malaysia
Aimi m mohd yusof, nor a a rahman, mainul haque.
- Author information
- Copyright and License information
Address for correspondence: Dr. Mainul Haque, Faculty of Medicine and Defence Health, Universiti Pertahanan Nasional Malaysia (National Defence University of Malaysia), Kem Perdana Sungai Besi, 57000, Kuala Lumpur, Malaysia. E-mail: [email protected]
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Background:
Food poisoning (FP) commonly occurs because of consuming contaminated food, which can be fatal. Many people are not aware of the dangers of FP. Thus, the purpose of this study is to analyze the knowledge, attitude, and practice (KAP) of FP among dietetic students (DS) and food handlers (FH) in a public university in Malaysia.
Materials and Methods:
A cross-sectional study was designed, and a self-administered questionnaire was distributed to 106 respondents. The survey comprised four sections including sociodemographic, knowledge, attitude, and practice.
Total percentage scores for KAP for FH were 86.06%, 32.40%, and 19.91%, respectively, whereas the KAP scores for DS were 89.36%, 34.26%, and 19.94%, respectively. This study revealed that the respondents had good knowledge but poor attitude and practice toward FP. Total mean percentage of KAP scores for DS was higher than FH. Besides, no significant difference was observed in KAP toward FP across different genders, age, education, and income levels among FH. However, for DS, significant difference ( p = 0.008) was observed in knowledge toward FP between genders. Significant association ( p = 0.048) was also reported in practice toward FP with age among DS. This study also found a significant association between knowledge and attitude ( p = 0.032) and knowledge and practice ( p = 0.017) toward FP among FH.
Conclusion:
Nevertheless, among DS, no significant association was observed between knowledge, attitude and practice toward FP. The findings may help them to plan effective methods to promote better understanding about FP and improving their knowledge and awareness.
K EYWORDS : Knowledge and practice , food poisoning , dietetic students , food handlers
I NTRODUCTION
Food poisoning (FP) refers to a group of illnesses that result from the ingestion of contaminated food that contains infectious organisms.[ 1 ] FP is defined as “illnesses caused by bacteria or other toxins in food, typically with vomiting and diarrhea.”[ 2 ] It was estimated that 76 million illnesses because of foodborne diseases resulted in 325,000 hospitalizations and 5,000 deaths each year in the USA.[ 3 ] Similarly, 1.3 million cases of foodborne illnesses, 21,000 hospitalizations, and 500 deaths were reported in England and Wales yearly.[ 4 ] The incidence of foodborne diseases was reported as 47.79 per 100,000 population in Malaysia in 2009, but had 32% increase in 2010, which is after only one year lapse.[ 5 ] Three deaths had been reported in Malaysia after consuming food served at a wedding ceremony in 2013.[ 6 ] Multiple causes are reported that lead to FP of which the most important is incorrect food safety practices. Most cases of FP were due to poor hygiene practices and usually occur in the school canteens, hostel kitchens, restaurants, and stall markets.[ 7 ]
This study was explicitly conducted among food handlers (FH) and dietetic students (DS) in a public university in Malaysia. The main reason for choosing these two groups was that DS were supposed to be more aware toward FP as they learnt about food safety and nutritional facts, whereas FH should also be mindful regarding this issue. This study also aims to find out the association between sociodemographic data with knowledge, attitude, and practice (KAP) toward FP among DS and FH.
M ATERIALS AND M ETHODS
Study area : This study was carried out in a public university in Malaysia.
Sampling population : This survey involved DS from Year I to IV and FH from the cafeterias in the university campus.
Study design : A cross-sectional study was designed and carried out, which involved the distribution of self-administered questionnaire to DS and FH in the university campus.
Study period : Data were collected from February 17, 2016, to February 26, 2016.
Sampling method
The study respondents were selected by quota sampling where convenient sampling was carried in the groups of DS and FH.
Inclusion criteria
Volunteered to participate in this study
Understood either English or Malay as the questionnaires provided were in these two languages
Aged 18 years or above
Sample size : The sample size ( n ) was 106, calculated using the single proportion formula [ n = ( Z α/2 /Δ)2 p (1 – p )] using Z α/2 = 1.96 for 95% confidence interval, p = 0.50 as proportion in population,[ 8 ] and precision, Δ = 0.10, with the addition of 10% nonresponse rate.
Data collection
The survey was conducted by distributing the self-administered questionnaire to the respondents. Before that, detail briefing was given to them so that they understood the purpose of this study. The data were collected among DS and FH in the public university. The questionnaire contained four sections, section A, B, C, and D, which were sociodemographic, knowledge, attitude, and practice toward FP, respectively. Each section consisted of 15 questions. Section A was designed to determine the sociodemographic information of the respondents, which included age, level of education, sex, and income. Section B contained two parts, the answer choices for part 1 were “yes,” “no,” and “I do not know,” whereas for part 2, they were “true,” “false,” and “not sure.” For section C, “strongly agree” to “strongly disagree” (Likert scale) were the answer choices for attitude, whereas for section D, “never” to “always” were the answer choices. In this questionnaire, the respondents needed to tick the appropriate answer choices. All items were modified from previous studies.[ 7 , 8 ] The questionnaire was validated through two approaches, which were content validity and face validity. The content validity of the questionnaire was validated by experts in this field, whereas face validity was conducted through a pilot study.
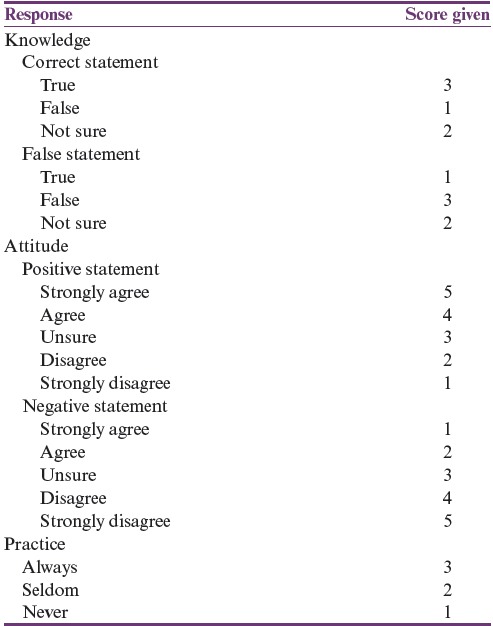
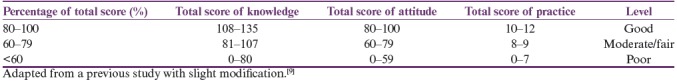
Scoring system
The scoring system for KAP toward FP is shown in Table 1 , whereas the grading of the total scores for the levels of KAP is shown in Table 2 .
Scoring system for knowledge, attitude, and practice
Grading of the total scores for the level of knowledge, attitude, and practice toward food poisoning
Data analysis
Data collected from the questionnaires were analyzed using the SPSS (Statistical Package for Social Scieces) 21, IBM, Armonk, NY, United States of America. Comparison of mean total scores of KAP between two independent groups was analyzed using independent t -test, whereas analysis of variance (ANOVA) was used for the comparison between more than two independent groups after checking for the relevant assumptions of the tests. Association between numerical variables was analyzed using Pearson correlation where the assumptions were satisfied, or otherwise Spearman correlation test was used.
Ethical approval
The study approval was obtained from the university’s postgraduate and research committee (Memo No. IIUM/310/G/13/4/4–179, February 1, 2016). Each respondent’s personal information was confidential, and study participation was voluntary. The study population was informed about the objectives and processes of the study where the data gathered would be anonymized, including for publication. Written consent was then obtained before the questionnaires were distributed.
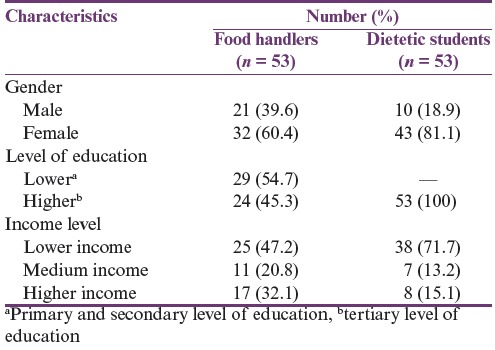
Sociodemographic characteristic of the respondents
In this KAP study, 106 respondents participated involving FH ( n = 53) and DS ( n = 53). The sociodemographic characteristics include age, gender, occupation, and level of education and income. Female respondents were more than male respondents for both the groups [ Table 3 ]. The respondents’ age involved in this study was 18–51 years, and the mean age was 27.14 (standard deviation [SD] = 7.21) years. The details of sociodemographic data are shown in Table 3 .
Sociodemographic data of the respondents ( n = 106)
Scores for knowledge, attitude, and practice toward food poisoning
The total percentage scores for KAP for FH were 86.06%, 32.40%, and 19.91%, respectively, whereas the KAP scores for DS were 89.36%, 34.26%, and 19.94%, respectively. According to the classifications in Table 2 , the respondents had good knowledge but poor attitude and practice toward FP. Generally, the total KAP percentage score for FH was lower than that for DS.
Knowledge toward food poisoning
Most of the respondents (FH = 98.1%, DS = 100%) had heard about FP. Again, most of the respondents (89.6%) knew that FP can lead to death. In addition, 77.4% (41) and 90.6% (48) of FH and DS, respectively, knew the causes of FP. The correct answers for the causes of FP are Salmonella, Staphylococcus aureus , and Listeria spp. In this part, 52.8% of FH and 98.1% of DS identified Salmonella as the cause of FP. Both groups showed positive answers in identifying raw egg (FH = 52.8%, DS = 94.3%), raw milk (FH = 62.3%, DS = 77.4%), and sushi (FH = 30.2%, DS = 62.3%) as the causes of FP. Unfortunately, more than one-third of FH opined that sushi could not cause FP. A total of 58.5% and 98.1% of FH and DS, respectively, answered correctly as Escherichia coli to be associated with FP with raw and undercooked meat. The respondents also identified Campylobacter (FH = 50.9%, DS = 47.2%) as the cause of FP with raw or undercooked poultry. For the next statement, respondents needed to choose the correct symptoms of FP, which were vomiting, diarrhea, and abdominal cramp. All DS and more than 90% of FH answered correctly regarding the symptoms of vomiting and diarrhea for FP, whereas, regarding abdominal cramp, only 88.7% of FH and 79.2% of DS answered correctly. Approximately half of the respondents knew that the slices of honeydew, baked potato, leftover turkey, and chocolate cake kept overnight on the counter and eaten as it is can cause FP. The last question regarding the suitable temperature (74°C) of heating of leftover food was answered precisely by 37.7% and 50.9% of FH and DS, respectively.
Attitude toward food poisoning
Among the respondents, 52.8% FH and 79.3% DS “disagree” to drink raw milk rather than pasteurized milk. In addition, only 30.2% FH and 11.3% DS “disagree” that it is safe to eat fresh raw milk and cheese. On the other hand, 86.8% FH and 92.5% DS “agree” with the statement that they prefer cutting their nails regularly because long nails could contaminate food. Approximately 77.4% of both groups “agree” that wearing gloves is important during the preparation of food. Next, 51% FH and 83% DS respondents “disagree” that half-cooked meat is safe to be eaten. Only 15.1% (8) but 90.5% (48) of FH and DS, respectively, “disagree” that drinking milk from a dented can is safe. Meanwhile, 84.9% (45) and 90.6% (48) of FH and DS, respectively, “disagree” to eating in unclean cafeteria. On next question, 45.3% (24) and 71.7% (38) of FH and DS “agree” that all of us can be a source of FP. Finally, 34% (18) and 66% (35) of FH and DS “disagree” that wiping off the cutting board with a clean paper towel is enough to prevent the spreading of foodborne pathogens.
Practice toward prevention of food poisoning
Among the respondents, 67.9% (36) and 81.1% (43) of FH and DS, respectively, always checked the expiry date before buying foods, whereas 67.9% (36) and 79.2% (42) of FH and DS, respectively, always washed the cutting board before use. On the other hand, 86.8% (46) and 52.8% (28) of FH and DS, respectively, always washed their hands with water and soap after using the toilet. Subsequently, 24.5% (13) and 15.1% (8) of FH and DS, respectively, never kept cooked meat or chicken for more than 4 h at room temperature. Again, 60.4% (32) and 5.7% (3) of FH and DS, respectively, never allow their fingernails to grow long. Finally, 88.7% (47) and 90.6% (48) of FH and DS, respectively, always practiced washing fresh vegetables or fruits before eating.
Association of sociodemographic characteristics with knowledge, attitude, and practice toward food poisoning
Comparing knowledge, attitude, and practice toward food poisoning between food handlers and dietetic students.
Figure 1 shows the comparison of mean total scores of KAP toward FP among FH and DS in the study. DS showed significantly higher mean total percentage score in knowledge ( p = 0.004) and attitude ( p = 0.010) as compared to FH, but the difference was not significant for practice scores.
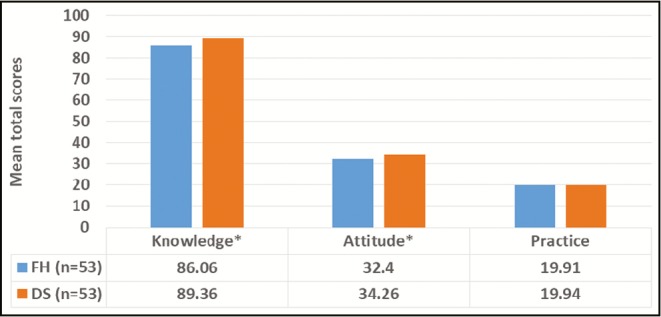
Comparing mean total scores of knowledge, attitude, and practice toward food poisoning between food handlers (FH) and dietetic students (DS). *Significant difference using independent t -test ( p -values of knowledge = 0.004 and attitude = 0.010)
Factors associated with knowledge, attitude, and practice toward food poisoning among food handlers and dietetic students
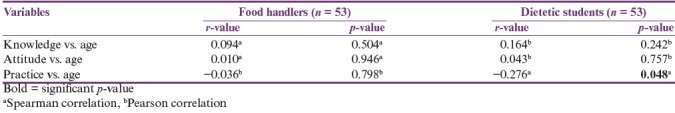
As shown in Table 4 , no significant association was observed between the total scores of KAP toward FP with age among FH and DS, except for between practice and age among DS ( r = −0.276; p = 0.048). The result indicates negative, fair, or little correlation between the variables, meaning the total scores of practice toward FP was lower with older age of DS. On the other hand, comparisons of KAP total scores between different genders, levels of education, and income among FH and DS are shown in Figures 2 – 4 , respectively, with no significant difference found except for the comparison of knowledge between male and female among DS ( p = 0.008) with male DS showing higher scores as compared to female DS.
Correlation between total scores of knowledge, attitude, and practice toward food poisoning with age among food handlers and dietetic students
Comparing mean total scores of knowledge, attitude, and practice toward food poisoning between different genders among food handlers (FH), n (male) = 21; n (female) =32 and dietetic students (DS), n (male) = 10; n (female) = 43. *Significant difference using independent t-test ( p = 0.008)
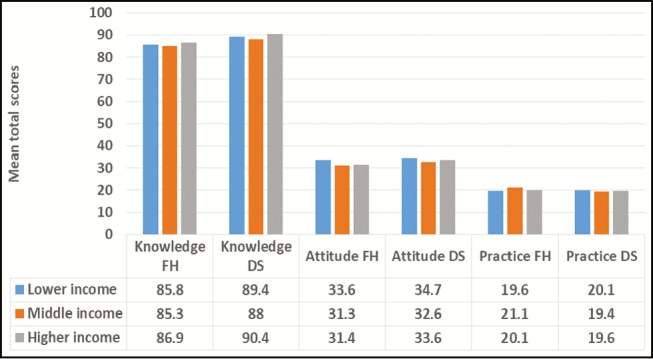
Comparing mean total scores of knowledge, attitude, and practice toward food poisoning between different levels of education among food handlers (FH), n (male) = 21; n (female) = 32. Analysis of variance (ANOVA) test carried out found no significant difference for any of the variables
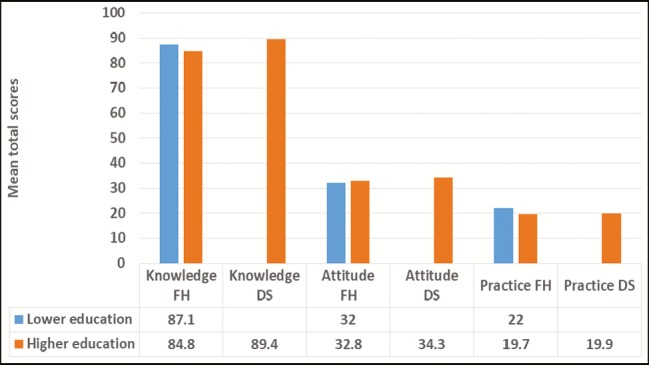
Comparing mean total scores of knowledge, attitude, and practice toward food poisoning between different levels of education among food handlers (FH), n (male) = 21; n (female) = 32. Comparison cannot be made between levels of education among dietetic students (DS), n = 53, because all of them came from the same level of higher education. Independent t -test performed found no significant difference for any of the variables
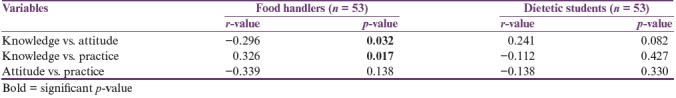
Correlation between knowledge, attitude, and practice toward food poisoning
A significant association ( r = −0.296, p = 0.032) was observed between knowledge and attitude toward FP among FH, also between knowledge and practice ( r = 0.326, p = 0.017) [ Table 5 ]. However, no significant association was observed between attitude and practice among FH, neither was any significant association detected between knowledge, attitude, and practice among DS [ Table 5 ].
Association between total scores of knowledge, attitude, and practice toward food poisoning using Pearson correlation test among food handlers and dietetic students
D ISCUSSION
According to the World Health Organization, 700,000 Asians die each year because of FP.[ 10 ] Hence, it is essential to possess good KAP toward the illness. The respondents in this study had good knowledge but poor attitude and practice toward FP. The total mean KAP score for DS was higher than that for FH.
Sociodemographic characteristics of respondents
A total number of 106 respondents were involved in this study, which consisted of 53 DS and 53 FH. In this study, female respondents outnumbered male respondents. The possible explanation could be that female respondents were more interested toward the dietetic field and worked in the kitchen as FH. The mean age was 27.14 (SD = 7.21) years. In terms of income, most of DS fall in low-income category. Students’ scholarship amount was considered in that category.
The mean percentage knowledge score for DS is higher than that for FH. This correlates with correct answers given by most of DS regarding knowledge about FP. Among the three components, knowledge had the highest percentage score. DS had higher knowledge regarding FP as compared to FH. Both groups were aware that FP could lead to death. Majority of DS knew the cause of FP but more than half of FH were not sure. One study revealed that health science discipline scored higher in food safety knowledge.[ 11 ] DS scored higher because they studied about food safety education.[ 12 ] In addition, both groups answered sushi could cause FP. It has been reported that sushi can promote FP and hepatitis B.[ 13 ] Thus, ensuring the cleanliness and food safety in common dining places in students’ hostels, in cafe and restaurants should be considered as an important public health action.[ 14 ]
The most common pathogens involved in FP are Staphylococcus aureus, Escherichia coli, Salmonella, Listeria spp., Campylobacter , and Clostridium perfringens .[ 15 ] DS had better knowledge regarding this as compared to FH as more than 50% of DS answered correctly. However, more than 18% of both categories of respondents were unsure regarding Legionella , which is consistent to an earlier study.[ 16 ] Legionella is a microorganism, which is actually often responsible for severe pneumonia.[ 17 ] Nevertheless, many of the respondents managed to answer correctly regarding the symptoms of FP, and this is consistent with an earlier finding.[ 15 ] Leftover food should be heated to 74°C to prevent FP. DS scored higher on this matter as 50.9% of them answered correctly, whereas in FH, only 37.7% answered correctly. Moreover, according to the Malaysian Ministry of Health, leftover food should be reheated at least at 74°C to prevent FP.[ 5 ] On the other hand, a previous study reported that FH had a high score in knowledge regarding food temperature control.[ 18 ] This study findings were similar to an earlier study in Turkey where FH had a low score in food temperature control.[ 19 ]
Although the mean percentage attitude scores of DS were higher than FH, the scores indicated that the respondents of both categories had poor attitude toward FP. This finding is similar to a previous study where the mean percentage of attitude scores were poor.[ 8 ] However, both groups “disagree” to drink raw milk rather than pasteurized milk, though this result is not supported by another previous study, which mentioned that the farmer believed that the raw milk is healthier than pasteurized milk.[ 20 ]
It has been reported that most of FH gave the correct statement that the consumption of raw milk and cheese could increase the risk of FP.[ 21 ] Nevertheless, more than half of DS in this study opined that eating raw milk and cheese is safe. This result is similar to another study, which similarly reported that eating raw milk and cheese is safe.[ 8 ] Furthermore, the majority of FH showed a negative attitude toward hygienic statement as compared to DS. This finding was supported by earlier research findings, which reported that more than 50% of FH showed negative attitude in terms of hygiene.[ 22 ] This study also found that FH showed a negative attitude toward the prevention of FP as majority “agree” that washing hand with water only to prevent FP as opposed to washing hand with water and soap. It has been advocated that proper hand washing is essential especially among retail FH to ensure a good standard of food safety and to avoid FP.[ 23 , 24 , 25 ] Besides, most DS opined that drinking from a dented can is harmful, whereas only a minor portion of FH agreed with the earlier notion. This denotes that FH has a negative attitude in preventing FP. This is one of the important facts that FH need to know as they prepare food and drinks for the customer. Drinking from a dented container can lead to a considerable dangerous health hazard.[ 26 ]
It can be considered from the mean percentage practice score that both groups had a poor practice of food hygiene. However, an earlier study revealed that FH showed a positive attitude, which was different from this study.[ 18 ] A few other studies also revealed that FH had a high mean score in hygiene practice and achieved an acceptable level.[ 27 , 28 ] However, an overseas study found that FH showed poor practice of strict food hygiene strategies toward prevention of FP.[ 29 ] On the other hand, it has been reported that food exposed at room temperature for 4 h or more are not safe to be eaten.[ 30 ]
Association between sociodemographic factors with knowledge, attitude, and practice toward food poisoning
In terms of knowledge toward FP, DS scored significantly higher than FH. This could be because DS had a higher education level as compared to FH. This statement is supported by earlier research findings mentioning that those who have high education level tend to have a high mean score in knowledge.[ 17 ] This study also found a significant difference in terms of knowledge toward FP between male and female respondents among DS. The finding denotes that male respondents have higher knowledge level regarding FP as compared to female respondents. This result was different and opposite to another study, which revealed that female students have a high mean score in terms of knowledge.[ 11 ] Furthermore, this study also revealed a significant difference of total attitude toward FP between FH and DS, besides a significant association between the total scores of practice and age among DS. A study found no significant relationship between gender and practice toward FP among FH, which is similar to the findings in this study.[ 22 ]
The results obtained showed a negative correlation between knowledge and attitude among FH. FH in this study showed high scores in knowledge but tend to have negative attitude toward FP. However, a previous study reported a positive correlation between knowledge and attitude among FH.[ 31 ] It has been mentioned that knowledge helps to improve attitude.[ 32 ]
Also, negative correlation was observed between knowledge and practice among DS and attitude and practice among both respondent groups, but the correlation was not statistically significant. These findings were similar to a previous research report, which found negative correlation between attitude and practice among FH.[ 31 ] Another study revealed that having good knowledge and attitude will lead to good practice measures among FH.[ 22 ] However, the results of this study revealed that having good knowledge and attitude does not lead to good practice as reported in a Turkish study.[ 19 ]
Also, a significant association was observed between knowledge and practice toward FP among FH. The r value showed little positive correlation, which means that knowledge leads to positive practice. Nevertheless, another research revealed a negative correlation between knowledge and practice among FH.[ 31 ] However, in this study, a negative correlation was observed between total knowledge and practice among DS, though it was not statistically significant. Finally, no significant association was reported between practice and attitude of FP for both groups. This is a cross-sectional study with its inherent limitation. Moreover, it is a single-center research with limited study because of financial and time constraints.
C ONCLUSION
In conclusion, this study shows that FH and DS had good knowledge but poor attitude and practice, though the total mean percentage score of KAP for DS was higher than that for FH. Besides, no significant difference was observed in KAP toward FP across different genders, age, education, and income levels among FH. However, DS possess significant differences in knowledge toward FP between genders. Also, a significant association was observed between practices toward FP with age among DS. This study also found a significant association between knowledge and attitude and knowledge and practice regarding FP among FH. Nevertheless, among DS, no significant association was observed between knowledge, attitude, and practice toward FP.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
R EFERENCES
- 1. Al-Mazrou YY. Food poisoning in Saudi Arabia. Potential for prevention? Saudi Med J. 2004;25:11–4. [ PubMed ] [ Google Scholar ]
- 2. Hormny AS. Oxford advance learner's dictionary of current English. 7th ed. New York: Oxford University Press; 2007. [ Google Scholar ]
- 3. Mead PS, Slutsker L, Dietz V, McCaig LF, Bresee JS, Shapiro C, et al. Food-related illness and death in the United States. Emerg Infect Dis. 1999;5:607–25. doi: 10.3201/eid0505.990502. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Adak GK, Long SM, O’Brien SJ. Trends in indigenous foodborne disease and deaths, England and Wales: 1992 to 2000. Gut. 2002;51:832–41. doi: 10.1136/gut.51.6.832. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Ministry of Health. Annual Reports. Planning division health informatics center, Ministry of Health, Malaysia. 2014. [Last accessed on 2015 Nov 12]. Available from: http://www.health.gov.bt/publications/annualreports/
- 6. Ramli S, Rattanachot O, Sahir SFM, Osman AR. Tiga Maut Keracunan Makanan, Utusan Malaysia. 2013. [Last accessed on 2018 Oct 9]. Available from: http://www.utusan.com.my/utusan/Jenayah/20131001/je_01/Tiga-maut-keracunanmakanan .
- 7. Norazmir MN, Norazlanshah H, Naqieyah N, Anuar MIK. Understanding and use of food package nutrition label among educated young adults. Food Control. 2012;11:934–40. [ Google Scholar ]
- 8. Sharif L, Al-Malki T. Knowledge, attitude and practice of Taif University students on food poisoning. Food Control. 2010;21:55–60. [ Google Scholar ]
- 9. Tikuye A. South Africa: University of South Africa; 2013. [Last accessed on 2018 Oct 9]. Knowledge, attitude, and practices of health care providers towards isoniazide preventive therapy (IPT) provision in Addis Ababa, Ethiopia [dissertation] Available from: http://uir.unisa.ac.za/bitstream/handle/10500/11916/dissertation_tikuye_am.pdf;sequence=1 . [ Google Scholar ]
- 10. World Health Organization. Food safety: resolution of the executive board of the WHO, 105th Session, EB105. R16 28, Agenda item 3.1. 2000. [Last accessed on 2018 July 16]. Available from: http://apps.who.int/gb/archive/pdf_files/EB105/eer16.pdf .
- 11. Unklesbay N, Sneed J, Toma R. College students’ attitudes, practices, and knowledge of food safety. J Food Prot. 1998;61:1175–80. doi: 10.4315/0362-028x-61.9.1175. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Scheule B. A comparison of the food safety knowledge and attitudes of hospitality and dietetic students. J Hosp Tour Educ. 2002;14:42–50. [ Google Scholar ]
- 13. Ng W-M. Popularization and localization of sushi in Singapore: an ethnographic survey. New Zealand J Asian Stud. 2001;3:7–19. [ Google Scholar ]
- 14. Kwon J, Roberts KR, Sauer K, Cole KB, Shanklin CW. Food safety risks in restaurants and school foodservice establishments: health inspection reports. [Last accessed on 2018 July 15];Food Prot Trends. 2014 34:25–35. Available from: http://www.foodprotection.org/files/food-protection-trends/Jan-Feb-14-kwon.pdf . [ Google Scholar ]
- 15. Sharifa Ezat WP, Netty D, Sangaran G. Paper review of factors, surveillance and burden of foodborne disease outbreak in Malaysia. Malay J Public Health Med. 2013;13:98–105. [ Google Scholar ]
- 16. Mitchell RE, Fraser AM, Bearon LB. Preventing food-borne illness in food service establishments: broadening the framework for intervention and research on safe food handling behaviors. Int J Environ Health Res. 2007;17:9–24. doi: 10.1080/09603120601124371. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Rathore MH. Legionella infection. Drugs and diseases. Pediatrics: general medicine. 2018. [Last accessed on 2018 July 15]. Available from: https://emedicine.medscape.com/article/965492-overview .
- 18. Sharif L, Obaidat MM, Al-Dalalah MR. Food hygiene knowledge, attitudes and practices of the food handlers in the military hospitals. Food Nutr Sci. 2013;4:245–51. [ Google Scholar ]
- 19. Bas M, Ersun AS, Kıvanç G. The evaluation of food hygiene knowledge, attitudes, and practices of food handlers’ in food businesses in Turkey. Food Control. 2006;17:317–22. [ Google Scholar ]
- 20. Hegarty H, O’Sullivan MB, Buckley J, Foley-Nolan C. Continued raw milk consumption on farms: why? Commun Dis Public Health. 2002;5:151–6. [ PubMed ] [ Google Scholar ]
- 21. Osaili TM, Obeidat BA, Jamous DOA, Bawadi HA. Food safety knowledge and practices among college female students in north of Jordan. Food Control. 2011;22:269–76. [ Google Scholar ]
- 22. Abdul-Mutalib NA, Syafiaz AN, Sakai K, Shirai Y. An overview of foodborne illness and food safety in Malaysia. Int Food Res J. 2015;22:896–901. [ Google Scholar ]
- 23. qFood Standards Australia New Zealand. A guide to the food safety standards. Chapter 3. Australia New Zealand Food Standards Code. 3rd ed. 2016. [Last accessed on 2018 July 15]. Available from: http://www.foodstandards.gov.au/publications/Documents/Safe%20Food%20Australia/FSANZ%20Safe%20Food%20Australia_WEB.pdf .
- 24. Mathur P. Hand hygiene: back to the basics of infection control. Indian J Med Res. 2011;134:611–20. doi: 10.4103/0971-5916.90985. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Darko S, Mills-Robertson FC, Wireko-Manu FD. Evaluation of some hotel kitchen staff on their knowledge on food safety and kitchen hygiene in the Kumasi Metropolis. Int Food Res J. 2015;22:2664–9. [ Google Scholar ]
- 26. Byrd-Bredbenner C, Abbot JM, Quick V. Food safety knowledge and beliefs of middle school children: implications for food safety educators. J Food Sci Educ. 2010;9:19–30. [ Google Scholar ]
- 27. Saad M, See TP, Adil MAM. Hygiene practices of food handlers at Malaysian government institutions training centers. Proc Soc Behav Sci. 2013;85:118–27. [ Google Scholar ]
- 28. Rodríguez M, Valero A, Posada-Izquierdo GD, Carrasco E, Zurera G. Evaluation of food handler practices and microbiological status of ready-to-eat foods in long-term care facilities in the Andalusia region of Spain. J Food Prot. 2011;74:1504–12. doi: 10.4315/0362-028X.JFP-10-468. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Akabanda F, Hlortsi EH, Owusu-Kwarteng J. Food safety knowledge, attitudes and practices of institutional food-handlers in Ghana. BMC Public Health. 2017;17:40. doi: 10.1186/s12889-016-3986-9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. United States Department of Agriculture. Food Safety and Inspection Service. Food Safety Information. How temperatures affect food. 2011. [Last accessed on 2018 July 15]. Available from: https://www.fsis.usda.gov/shared/PDF/How_Temperatures_Affect_Food.pdf .
- 31. Ansari-Lari M, Soodbakhsh S, Lakzadeh L. Knowledge, attitudes and practices of workers on food hygienic practices in meat processing plants in Fars, Iran. Food Control. 2010;21:260–3. [ Google Scholar ]
- 32. Acikel CH, Ogur R, Yaren H, Gocgeldi E, Ucar M, Kir T. The hygiene training of food handlers at a teaching hospital. Food Control. 2008;19:186–90. [ Google Scholar ]
- View on publisher site
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Knowledge, Attitude, Practice and Food Poisoning Associated Factors Among Parents in Bench-Sheko Zone, Southwest Ethiopia
Besufekad mekonnen, nahom solomon, tewodros yosef.
- Author information
- Article notes
- Copyright and License information
Correspondence: Besufekad Mekonnen Department of Public Health, Mizan-Tepi University, P.O. Box: 260, Mizan-Aman, Southern Nation Nationality and People Region, Ethiopia Email [email protected]
Received 2021 Jan 22; Accepted 2021 Apr 9; Collection date 2021.
This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License ( http://creativecommons.org/licenses/by-nc/3.0/ ). By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms ( https://www.dovepress.com/terms.php ).
Food poisoning is a food borne disease, mainly resulting from ingestion of food that contains a toxin, chemical or infectious microorganisms like bacteria, virus, parasite, or prion. On the other hand, avoiding food contamination during preparing and feeding is a key factor for reducing the prevalence of food poisoning. This study aimed to assess the knowledge, attitude, self-reported practice and food poisoning associated factors among parents in the selected health centers of Bench-Sheko Zone in Ethiopia.
An institution-based cross-sectional study was conducted among 408 systematically selected parents in Bench-Sheko zone, Ethiopia. The data were collected through face to face interview using a structured questionnaire.
The median knowledge score was 8.0 with an interquartile range (IQR) of 8.0–10.0. The median attitude score was 9.0 with an IQR of 6.0–9.0. The median practice score was 12.0 with an IQR of 10.0–13.0. A positive correlation was seen between knowledge and attitudes of parents with food poisoning (r= 0.321, P < 0.026), between knowledge and practices of parents towards food poisoning (r= 0.312, P < 0.001) and between attitude and practices result towards food poisoning (r= 0.224, p < 0.031). The parents with a higher education level, employed and who live in a city were the factors significantly associated with higher knowledge scores ( p < 0.05). The improved attitude was seen as educational level increased ( p <0.05). The parents with female gender, employed and who live in a city were significantly associated with higher hygienic practices towards the prevention of food poisoning ( p <0.05).
The knowledge, attitude, and self-reported practices of parents regarding food poisoning prevention are associated with each other and are affected by socio-demographic variables. Therefore, adequate emphasis should be given by health sectors to designing strong strategies which address the specific contributing factors for the problem.
Keywords: knowledge, attitude, practices, parents, food poisoning, Ethiopia
Introduction
Food is a known vehicle for many pathogenic and toxigenic agents that cause what are known as food-borne diseases. 1 , 2 Food borne diseases (FBDs) are diseases which are caused by the consumption of contaminated foods or water, with a variety of diseases causing agents ranging from infective organisms, poisonous chemicals, radioactive substances and other harmful substances. 1 , 3 FBDs have increased over the years, and treacherously upset the health and economic well-being of many people in developed and developing countries. 3–5
According to World Health Organization (WHO), contaminated food contributes to 1.5 billion cases of diarrhea in children each year, resulting in over three million premature deaths. 6 , 7 Safe food is defined as not causing harm or illness to the consumer. 8 Food safety is the processes of handling, preparing and storing of food in ways that prevent contamination by toxic chemicals 9 or pathogenic microbes, which result in food-borne illness. 1 , 10
Food poisoning occurs as a result of consuming food contaminated with microorganisms or their toxins; the contamination starting from inadequate preservation methods, unhealthy handling practices, cross-contamination from food contact surfaces, or from persons hiding the microorganisms in their nails and on the skin. 11 The presence of poor hygienic practices during food preparation, handling and storage creates the conditions that allow the proliferation and transmission of disease causing organisms such as bacteria, viruses and other food-borne pathogens. 2 , 15 The signs of toxigenic food poisoning mostly appear within 24 hours after eating of contaminated food. The symptoms include nausea, vomiting, diarrhea, abdominal pain, a headache and fever. The life-threatening neurologic, hepatic and renal syndromes may occur several days after intestinal, and may cause permanent disability or death depending upon which microbe is ingested. 1 , 13–15
The incidence of FBDs depends on the hygienic measures implicated in food production and storage, but they could be ineffective if consumers have unhygienic practices and food handling approaches. 16 It is recommended to apply different precaution techniques to keep safety of foods, including: to wash hands well and often, especially after using the bathroom, before touching food, and after touching raw food by using soap and warm water and scrub for at least 15 seconds; clean all utensils, cutting boards, and surfaces that you use to prepare food with hot, soapy water; wash all raw vegetables and fruits; keep raw foods (especially meat, poultry, and seafood) away from other foods until they are cooked; and cook all food from animal sources to a safe internal temperature. 17 But different studies from Ethiopia have reported that people fail to be concerned of and/or properly apply the prevention techniques. 7 , 17–19
It is known that the KAP of food poisoning are key factors for reducing the prevalence of food-borne diseases in food production and serving area. 7 , 20 In addition, the issue demands more evidence, particularly in southwest Ethiopia. Therefore, this study aimed to assess the knowledge, attitude and self-reported practices related to food poisoning among parents in the selected four health centers of Bench-Sheko zone in southwest Ethiopia. The finding will contribute to devise an intervention of operative, effective and proper health intervention program regarding how to handle food safely and adds evidence in the area of interest.
Study Design, Setting and Period
An institution based cross-sectional study was conducted among parents attending health institutions from September 1 to December 30, 2019, in former Bench-Maji zone which is currently named as Bench-Sheko zone, Ethiopia. Bench-Sheko Zone is one of the 16 zones in Southern Nation Nationalities and Peoples Regional state ( Figure 1 ), which is located at 585 km southwest of Addis Ababa, the capital city of Ethiopia. The zone has an estimated population of 829,493, and the primary health service coverage of the zone is 92.6%, covering a total catchment area of 19,965.8 km 2 with majority (86%, 713,363.98) of the population living in the rural areas. A study was conducted in four randomly selected primary health centers, namely Bire (found in North Bench district), Kite, Debrework (found in South Bench district) and Biftu (found in Guraferda district).
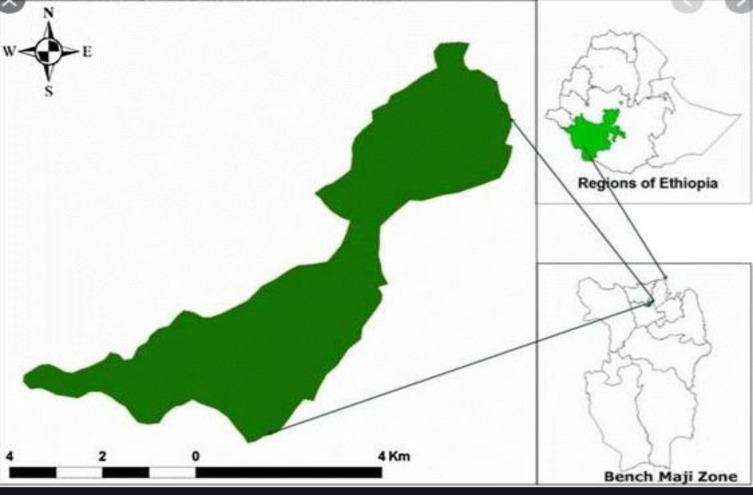
Map of the study area.
The parents who had children aged less than 6 years old and attending the health centers were selected, interviewed and their responses were recorded. The inclusion criteria were age of 18 years old and above and agreed to participate in the study. Exclusion criteria included parents who were not resident in the study area, had not given birth, who had children over 6 years or who had difficulty in communication.
Sample Size Determination and Sampling Technique
Data collection instrument and procedures.
A structured questionnaire, which was adapted from similar studies, 1 , 21–23 was used. The questionnaire was composed of four parts socio-demographic variables (age, gender, educational status, residency, and number of family members including children, their ages, food preparation habit), food poisoning knowledge related questions including general statements about food poisoning causes (15 questions), food poisoning attitude related questions including statements about eating raw food and washing fruits and vegetables (15 questions), and food poisoning practices related questions regarding eating, drinking and washing hands (20 questions). Moreover, in the knowledge and attitude part, the questionnaire entails five options ranging from “strongly agree” to “strongly disagree”. In the practice section, the respondents had five choices: “always yes”; “most of the time”; ‘sometimes’; “rarely”; and “always no”.
The data were collected by BSc nurses and public health officers. Two days’ training was given for data collectors and supervisors about objectives of the study, contents of questionnaire, and approaches to interview. A pre-test was conducted on 5% of the sample in other primary health centers than the study set up, and necessary amendment of the questionnaires based on the result of the pre-test were considered. Finally data were collected through a face-to-face interview.
Ethical Consideration
Data collection was started after obtaining permission from Mizan-Tepi University Institutional Review Boards (MTU-IRB). Again, a support letter was obtained from the Bench Sheko Zone Health Bureau. All study participants were informed about the purpose of the study, their right to deny participation, anonymity, and confidentiality of the information. Moreover, the verbal informed consent was approved by the Mizan-Tepi University Ethical Review Board, and this study was conducted in accordance with the Declaration of Helsinki.
Data Processing and Analysis
The data were entered in to Epi data manager and analyzed using SPSS software version 22. The descriptive statistics (mean, standard deviation, median and interquartile range) were conducted to summarize the results. Some characteristics were consolidated into dichotomous (binary) variables for ease of analysis and interpretation. Normality test was made by using Kolmogorov Smirnov test. In addition, the Mann–Whitney U -test and the Kruskal–Wallis H -test were performed to determine significance difference between the mean values. Moreover, Pearson correlation coefficient was designed to examine a possible correlation between continuous variables (knowledge, attitude and practice scores). The level of significance was declared at p value <0.05.
Socio-Demographic Profiles
Of the 422 sampled populations, 408 were interviewed and completed data were collected, giving a response rate of 96.7%. Almost all respondents were women (97.3%). The mean age of the study participants was 32.5 (SD±5.2) years. One hundred sixty-eight (41.2%) of them have achieved secondary educational level followed by 37% of parents who are able to read and write. Again 88% and 74.3% of participants were unemployed and rural residents respectively. Mothers were found to be the responsible body for preparing food for the family (98.8%) ( Table 1 ).
Socio-Demographic Status of Parents in Bench-Sheko Zone, Ethiopia; 2019 (N= 408)
Knowledge About Food Poisoning
The mean value of knowledge about food poisoning was 9±3.2 SD. When the respondents were asked about the highly risky foods for food poisoning, 42% of the study participants responded that eating raw meat is highly risky for food poisoning, 75% responded that eating raw unwashed vegetables is highly risky for food poisoning and 73.4% responded that drinking raw milk is highly risky for food poisoning. Furthermore, 78%, 74%, 75%, 78.4% and 74.5% of the respondents responded correctly that raw white cheese, unwashed not peeled fruits, uncovered leftover cooked food, untreated surface and rainwater, and raw eggs, respectively, were risky food. The majority of respondents (88%) responded that well cooked food is free from microbes that cause food poisoning and that keeping food in refrigerator will slow down the microbial growth and multiplication, so, prevent food poisoning (52%). Nearly half of the respondents (50.9%) said that there is no risk of food poisoning from eating leftover cooked food reserved in refrigerator for 2–3 days. Regarding hygienic condition of parents, 75% of the respondents said that poor hygienic practice of parents could be the source of food poisoning. Instead, only 38.7% of the respondents agreed that some toxins produced by microbes and cause food poisoning are resistant to heating temperature of food.
Attitude Regarding Food Poisoning
The mean value of attitude regarding food poisoning was 8±4.8 SD. Half of the respondents reported that washing hands with soap before preparing (51.2%) and eating food (50.2%), along with thorough washing of vegetables and fruits (50.4%) are necessary to prevent food poisoning. Concerning raw milk, 58.4% of the respondents correctly disagreed that there is no risk of disease from drinking raw cow milk right after milking, 59.7% disagreed that raw milk is more healthy and nutritious than pasteurized or boiled milk. Regarding raw eggs, half of respondents (51.2%) disagreed that raw eggs are more healthy and nutritious than cooked ones, while 22.7% disagreed that there is no risk of disease from drinking raw eggs. Regarding vegetables and fruits, 50.8% of the respondents disagreed that eating vegetation and fruits directly from the plant without wiping has no risk of disease occurrence. Instead, majority of the respondents agreed that baby feces are free from pathogenic microbes if he/she is not sick. Majority of the respondents (74.5%) agreed that rainwater collected in reservoir is safe to drink without any treatment and 49.6% agreed that there is no risk of disease from eating cooked food reserved at room temperature for 1 day if covered.
Practices About Food Poisoning
The mean practice score was 12±4.8 SD. Regarding practices questions, more than half of the respondents wash their hands with soap and water before eating and preparing food, after contact with animals (55.4%) and after using the toilet (55.6%). In addition, 58% of the respondents wash fresh vegetables and fruits before eating while 57.4% wash their hands with water and soap after handling raw unwashed vegetables. Likewise, 54.4% of the respondents may eat fresh vegetables and fruits after just wiping it, without washing it (56.3%) or pick it up from the plants during a field trip and eat it without washing (59.1%). Half of the respondents do not eat raw eggs and 55% of the respondents do not eat raw or half-cooked meat. Moreover, 60% of the respondents drink raw milk. A high percentage of respondents drink from rainwater collected without any treatment (78.4%) and 75% of parents do not eat foods out of their home (hotels, restaurants and cafeteria), 88% of parents may eat raw white cheese prepared from raw unpasteurized milk. Furthermore, 57.4% of the respondents were cooked food left at room temperature for over 6 h without sufficient heating.
The Kruskal–Wallis test was used to assess the association between socio-demographic variables and knowledge. The result revealed that educational level, residency and employment status were significantly associated with knowledge ( P value < 0.05). However, no significant association was seen between age, gender, number of family member, number of children and food preparation habit with knowledge. It is observed that, parents with relatively highest level of education have good level of knowledge about food poisoning. In addition, respondents who live in urban setting have better knowledge than those who live in rural area ( Table 2 ).
Association Between Socio-Demographic Variable and KAP of Food Poisoning, Among Parents in Bench Sheko Zone, 2019
According to Kruskal–Wallis test, there was significant association between gender, educational level and residency with attitude about food poisoning ( p value < 0.005). On the other hand, age, employment status, number of children, number of family, age of the children and food preparation habit did not show any significant association with attitude ( Table 2 ).
It is observed that gender, education and residency had significant association with practices or taking measures against food poisoning. Other socio-demographic variables such as age, employment status, family number, age of children and food preparation habit did not show any significant association with practice of food poisoning. The result revealed that female parents do have better hygiene practice than males. In addition, the respondents with high level of educational status had better hygienic practices than low educational level. Moreover, parents who live in urban area experience better hygienic practices than those who live in rural setting ( Table 2 ).
The Correlations Between Knowledge, Attitude and Practice Towards Food Poisoning
Pearson’s correlation coefficient was used for testing the existence of any correlation between knowledge, attitude and self-reported practices of parents with food poisoning. Accordingly, positive correlation was seen between knowledge and attitudes of parents with food poisoning ( r = 0.321, P value < 0.026). This shows that parents who had good knowledge were more likely to have good attitude regarding food poisoning. In addition, there was positive correlation between knowledge and practices of parents towards food poisoning ( r = 0.312, P value 0.001). This implies that parents who had good knowledge were more likely to have good hygiene practices towards food poisoning. Moreover, there was positive correlation between attitude and self-reported practices result towards food poisoning ( r = 0.224, p value 0.031). It is well expressed that parents who had good attitude were more likely to have good hygiene practices regarding food poisoning.
This study assessed the knowledge, attitude, and self-reported practice and food poisoning associated factors among parents in the selected health centers of Bench-Sheko zone, southwest Ethiopia. In the developing world, females are more commonly responsible for food preparation; the female carries the responsibility for family care as a wife, from cleaning and arranging the house to preparing the food for all members of the family. In addition, the female, as a mother, takes care of her children. 1 , 24 , 25 This is also clearly found in this study where mothers are the responsible body of preparing food, and since mothers have also other house work burdens, there could be gaps in following necessary precautions for keeping safety of food.
Recent studies asserted that knowledge, attitude and practice are key factors in reducing the prevalence of food-borne diseases in food processing and serving area. 1 , 21 , 22 , 26 On the other hand, they themselves are also influenced by many factors including educational status, gender and age of food handlers. 23 , 27–29 In the current study, it is revealed that educational level, residency and employment status were significantly associated with knowledge. Badrie et al 30 and Zyoud et al 1 have also reported similar findings, in which a significant association between educational level and knowledge was scored. Parents with a high level of education reported higher knowledge scores than those with a lower level. In addition, parents who live in the urban setting reported higher scores than those who live in the rural setting. This consistency might be explained by some close features of study population. Parents, who are educated, employed and who live in towns showed higher knowledge scores and attitude is also improved as educational level increased. Parents with female gender, employed and who live in town had higher hygienic practices towards the prevention of food poisoning. Therefore addressing educational gaps and accessing health information to rural community is demanding.
Educational level, gender and residency were also found to have significant influence on attitude about food poisoning. Although gender was found as one factor affecting parents’ attitude regarding food poisoning, opposing result was reported from a study conducted in Palestine, 1 which revealed there was no significant association between gender and attitude regarding food poisoning. Of course, the difference might happen because in our study majority of respondents were women. Again, men in this study area could pass most of their time at field, and/or may contact many people and as a result may have more exposure to information, on the other hand, those who live in towns and/or who had achieved highest level of education may be influenced to experience good attitude. Parents with a high education level reported a good attitude compared to those with a lower level. Zyoud et al, Altekruse et al, and Ozilgen S. have reported comparably close result. 1 , 31 , 32 Again, influence of health information and education status is found to be the most important factor affecting attitude of parents toward food poisoning, so working in filling these gaps would bring better change.
Regarding practice, again gender, level of education and residency were found to have significant association about taking measures against food poisoning. This result is consistent with a study conducted in Debark town and Palestine. 1 , 7 Similarity may be explained by comparability of study population and setting. Parents who live in a town had better hygienic practice than those who live in rural area. In addition, female parents scored higher than males. A possible explanation for this result may be the lack of adequate experience in food preparation between female parents compared to males. Contrary to this, study reports from Henok et al and Zyoud et al 1 , 7 revealed that female parents and village residences lack hygienic knowledge and practices regarding food poisoning. Whenever people live at a distance from towns where many health services and information are easily accessible, it is clear that health problems may occur and failing to keep safety of food is one of the areas which results in big health impact, mainly resulting in food poisoning.
Significant association was also shown between knowledge, attitude and practice. Accordingly; parents who had good knowledge have also demonstrated a good level of attitude and practice. This result is consistent with a study conducted in Iran, Palestine, China and West Indies. 1 , 22 , 30 This implies knowledge is a primary and a very important potential for securing food safety and enabling people to take measures to reduce occurrence of food poisoning, as a result, it demands interventions targeting specific population group so as to empower them to prevent food poisoning.
Generally it is found that knowledge, attitude and practice towards taking measures against food poisoning are still limited and demands efforts to promote public health through applying different health interventions mainly health education targeting the main associated factors.
Conclusion and Recommendations
Two-thirds of the parents have good knowledge about food poisoning but only half of them have good attitude and experience of taking preventive measures to avoid food poisoning. The study also found that gender; educational status, occupation and place of residence were the main factors which showed significant effect and parents who had good knowledge have also demonstrated a good level of attitude and practice. Therefore, emphasis should be given to fill the gaps by applying necessary interventions which consider the major contributing factors as well. Consequently, health sectors in the local area shall give emphasis in fostering knowledge of parents regarding food poisoning and design strategy to change attitude of parents regarding poisoning, facilitate them to experience a good preventive measures and shall promote for good knowledge, attitude and taking preventive measures about food poisoning. Moreover, academic sectors and other sectors working in the area shall design strategies and implement for fostering knowledge, attitude and preventive measures concerning food poisoning and shall make advanced level study of both qualitative and quantitative method to identify the gaps and associated factors more. This study has come with important results but should be used without forgetting its limitation of social desirability bias.
Acknowledgment
The authors acknowledge Mizan Tepi University for unreserved support. In addition, the authors express their appreciation and thanks to Mizan-Tepi University research and community service directorate for overall facilities during the survey. Lastly, the researchers would like to address their deepest thanks to all staff of College of Health Sciences in MTU for their valuable comments.
Funding Statement
The Authors acknowledged Mizan-Tepi University for financial support.
Abbreviations
FBDs, food born diseases; IRB, internal review board; IQR, inter quartile range; KAP, knowledge, attitude and practice; MTU, Mizan-Tepi University; SD, standard deviation; SPSS, Statistical Package for Social Science; WHO, World Health Organization.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
The authors declare that they have no conflicts of interest for this work.
- 1. Zyoud S, Shalabi J, Imran K, et al. Knowledge, attitude and practices among parents regarding food poisoning: a cross-sectional study from Palestine. BMC Public Health . 2019;19(1):1–10. doi: 10.1186/s12889-019-6955-2 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Zeeshan M, Shah H, Durrani Y, Ayub M, Jan Z, Shah M. A questionnaire-based survey on food safety knowledge during food-handling and food preparation practices among university students. J Clin Nutr Diet . 2017;03(02):1–8. doi: 10.4172/2472-1921.100052 [ DOI ] [ Google Scholar ]
- 3. Ulusoy BH, Çolakoğlu N. What do they know about food safety? A questionnaire survey on food safety knowledge of kitchen employees in Istanbul. Food Health . 2018;4(4):283–292. doi: 10.3153/fh18028 [ DOI ] [ Google Scholar ]
- 4. Ismail KA. Assessment of the knowledge, attitude and practice about food safety among Saudi Population in Taif. Biomed J Sci Tech Res . 2018;8(2):4–10. doi: 10.26717/bjstr.2018.08.001629 [ DOI ] [ Google Scholar ]
- 5. Akabanda F, Hlortsi EH, Owusu-Kwarteng J. Food safety knowledge, attitudes and practices of institutional food-handlers in Ghana. BMC Public Health . 2017;17(1):1–9. doi: 10.1186/s12889-016-3986-9 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Zvenyika F. The knowledge, attitudes and practices, and compliance regarding the basic prerequisite programmes (prps) of food safety management systems of food service workers in boarding schools and restaurants in Masvingo province, Zimbabwe; 2017. (November).
- 7. Dagne H, Raju RP, Andualem Z, Hagos T, Addis K. Food safety practice and its associated factors among mothers in debarq town, Northwest Ethiopia: community-based cross-sectional study. Biomed Res Int . 2019;2019:1–8. doi: 10.1155/2019/1549131 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Mohammed AFH. Food safety knowledge, attitude and self‐reported practices among food handlers in Sohag Governorate, Egypt. East Mediterr Heal J . 2019;25(9):1–5. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Mekonnen B, Siraj J, Negash S. Determination of pesticide residues in food premises using QuECHERS method in Bench-Sheko Zone, Southwest Ethiopia. Biomed Res Int . 2021;2021:1–13. doi: 10.1155/2021/6612096 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Yusuf TA, Chege PM. Awareness of food hygiene practices and practices among street food vendors in Nasarawa State, Nigeria. Int J Health Sci Res . 2019;9(7):156–164. [ Google Scholar ]
- 11. Ngoc T, Thanh C. Food safety behavior, attitudes and practices of street food vendors and consumers in Vietnam; 2015.
- 12. Warner K. Street food vending: vendor food safety practices and consumers’ behaviours, attitudes and perceptions; 2013.
- 13. Sharma S, Sangha JK. Relation between food safety awareness and disease incidence: a study of home food preparers in Punjab. Stud Ethnomed . 2015;9(2):255–261. doi: 10.1080/09735070.2015.11905443 [ DOI ] [ Google Scholar ]
- 14. Malavi DN. Food Safety knowledge, attitude and practices of orange-fleshed sweetpotato puree handlers in Kenya. Food Sci Qual Manag . 2017;67(April2018):54–63. [ Google Scholar ]
- 15. Oladoyinbo CA, Akinbule OO, Awosika IA. Knowledge of food borne infection and food safety practices among local food handlers in Ijebu-Ode Local Government Area of Ogun State. J Public Health Epidemiol . 2015;7(9):268–273. doi: 10.5897/jphe2015.0758 [ DOI ] [ Google Scholar ]
- 16. World Health Organization. Five keys to safer food manual safer food manual. Vol 3, 206AD. Available from: http://www.mdpi.com/1660-4601/6/11/2833/ . Accessed April21, 2021. [ Google Scholar ]
- 17. Eshetu D, Kifle T, Hirigo AT. Knowledge, attitudes, and practices of hand washing among aderash primary schoolchildren in Yirgalem Town, Southern Ethiopia. J Multidiscip Healthc . 2020;13:759–768. doi: 10.2147/JMDH.S257034 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Adane M, Teka B, Gismu Y, Halefom G, Ademe M. Food hygiene and safety measures among food handlers in street food shops and food establishments of Dessie town, Ethiopia: a community-based cross-sectional study. PLoS One . 2018;13(5):1–13. doi: 10.1371/journal.pone.0196919 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Tshipamba ME, Lubanza N, Adetunji MC, Mwanza M. Evaluation of the effect of hygiene practices and attitudes on the microbial quality of street vended meats sold in johannesburg, south- africa journal of food: microbiology, safety & hygiene. J Food Microbiol Saf Hyg . 2018;3(2):1–10. doi: 10.4172/2476-2059.1000137 [ DOI ] [ Google Scholar ]
- 20. Adel HS, Ns M, Sm A-R. Assessment of the knowledge, attitude and practice towards food poisoning of food handlers in some Egyptian worksites. Egypt J Occup Med . 2014;38(1):79–94. doi: 10.21608/ejom.2014.789 [ DOI ] [ Google Scholar ]
- 21. Zolfaghari H, Khezerlou A, Alizadeh-Sani M, Ehsani A. Food-borne diseases knowledge, attitude, and practices of women living in East Azerbaijan, Iran. J Anal Res Clin Med . 2019;7(3):91–99. doi: 10.15171/jarcm.2019.017 [ DOI ] [ Google Scholar ]
- 22. Henson S, Reardon T. Private agri-food standards: implications for food policy and the agri-food system. Food Policy . 2005;30(3):241–253. doi: 10.1016/j.foodpol.2005.05.002 [ DOI ] [ Google Scholar ]
- 23. Patil SR, Cates S, Morales R. Consumer food safety knowledge, practices, and demographic differences: findings from a meta-analysis. J Food Prot . 2005;68(9):1884–1894. doi: 10.4315/0362-028X-68.9.1884 [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Aa MB. Knowledge, attitude and practice of female teachers regarding safe food handling; is it sufficient? An Intervention Study, Zagazig, Egypt. Egypt J Occup Med . 2017;41(2):271–287. [ Google Scholar ]
- 25. Omar BA, Shadia SM, Anas SD, Mohammed AE. Food hygiene knowledge, attitude and practices among hospital food handlers in Elmanagil City, Sudan. African Journal of Microbiology Research . 2020;14(4):106–111. doi: 10.5897/AJMR2020.9323 [ DOI ] [ Google Scholar ]
- 26. Soon JM, Baines R, Seaman P. Meta-analysis of food safety training on hand hygiene knowledge and attitudes among food handlers. J Food Prot . 2012;75(4):793–804. doi: 10.4315/0362-028X.JFP-11-502 [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Zanin LM, Thimoteo D, Vera V; GeQual Study Group of Food Quality. Centro de Desenvolvimento do Ensino SC. Food Res Int . 2017;100(Pt 1):53–62. doi: 10.1016/j.foodres.2017.07.042 [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Barrie D. The provision of food and catering hospital services in. J Hosp Infect . 1996;33(1):13–33. doi: 10.1016/S0195-6701(96)90026-2 [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Badrie N, Gobin A, Dookeran S, Duncan R. Consumer awareness and perception to food safety hazards in Trinidad, West Indies. Food Control . 2006;17(5):370–377. doi: 10.1016/j.foodcont.2005.01.003 [ DOI ] [ Google Scholar ]
- 30. Altekruse SF, Street DA, Fein SB, Levy AS. Consumer knowledge of foodborne microbial hazards and food-handling practices. J Food Prot . 1995;59(3):287–294. doi: 10.4315/0362-028X-59.3.287 [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Ozilgen S. Food safety education makes the difference: food safety perceptions, knowledge, attitudes and practices among Turkish university students. J Verbr Leb . 2011;6(1):25–34. doi: 10.1007/s00003-010-0593-z [ DOI ] [ Google Scholar ]
- 32. Ma L, Chen H, Yan H, Wu L, Zhang W. Food safety knowledge, attitudes, and behavior of street food vendors and consumers in Handan, a third tier city in China. BMC Public Health . 2019;19(1):1–13. doi: 10.1186/s12889-019-7475-9 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (379.9 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Research article
- Open access
- Published: 16 May 2019
Knowledge, attitude and practices among parents regarding food poisoning: a cross-sectional study from Palestine
- Sa’ed Zyoud ORCID: orcid.org/0000-0002-7369-2058 1 , 2 ,
- Jawad Shalabi 3 ,
- Kathem Imran 3 ,
- Lina Ayaseh 3 ,
- Nawras Radwany 3 ,
- Ruba Salameh 3 ,
- Zain Sa’dalden 3 ,
- Labib Sharif 4 ,
- Waleed Sweileh 5 ,
- Rahmat Awang 6 &
- Samah Al-Jabi 2
BMC Public Health volume 19 , Article number: 586 ( 2019 ) Cite this article
12k Accesses
24 Citations
Metrics details
Food serves as a vehicle for many pathogenic and toxigenic agents that cause food-borne diseases. Knowledge, attitude, and practices are key factors in reducing the incidence of food-borne diseases in food service areas. The main objective of this study was to evaluate knowledge, attitude, and practices related to food poisoning among parents of children in Nablus, Palestine.
A cross-sectional study was conducted in primary healthcare centers in Nablus district from May to July 2015. Data were collected using structured questionnaire interviews with parents to collect information on food safety knowledge, attitudes, and practices, alongside sociodemographic characteristics.
Four-hundred and twelve parents were interviewed, 92.7% were mothers. The median knowledge score was 12.0 with an interquartile range (IQR) of 11.0–14.0. The median attitude score was 11.0 with IQR of 10.0–13.0, while the median practice score was 18.0 with IQR of 16.0–19.0. Significant modest positive correlations were found between respondents’ knowledge and attitude scores regarding food poisoning ( r = 0.24, p < 0.001), knowledge and practice scores regarding food poisoning ( r = 0.23, p < 0.001), and attitude and practice scores regarding food poisoning ( r = 0.30, p < 0.001). Respondents with a higher education level and who live in a city were the only factors significantly associated with higher knowledge scores ( p < 0.05). Attitude improved as educational level increased ( p < 0.05) and income level increased ( p < 0.05). Those of female gender and employed were statistically significantly associated with higher satisfactory hygienic practices in relation to the prevention of food poisoning ( p < 0.05).

Conclusions
Knowledge, attitude, and practices regarding food poisoning prevention are associated with each other and are affected by a complex interplay between socio-economic variables. The study highlights the need for health education programmes and general awareness campaigns that intend not only to enhance knowledge but also promote parents to practice food safety measures strictly and further strengthen their awareness level.
Peer Review reports
Food serves as a vehicle for many pathogenic and toxigenic agents that cause what are known as food-borne diseases or food poisoning [ 1 ]. In recent decades, food poisoning has become a growing public health problem worldwide, in both developed and developing countries [ 2 , 3 , 4 , 5 , 6 ]. It is defined as a variety of illnesses acquired by consumption of contaminated foods or water, with a variety of causes ranging from infective organisms (bacteria and viruses), poisonous chemicals, radioactive substances and other harmful substances leading to more than 250 different food-borne diseases (ranging from diarrhoea to cancers) [ 7 ]. Food safety refers to the processes of handling, preparing and storing of food in ways that prevent contamination by toxic chemicals or pathogenic microbes resulting in food-borne illness [ 8 ].
Symptoms of toxigenic food poisoning mostly appear within 24 h after ingestion of contaminated food while foodborne infections may not appear until 2–3 days later. Symptoms can include nausea, vomiting, diarrhea, abdominal pain (which is severe in inflammatory processes), headache and fever. Life-threatening neurologic, hepatic and renal syndromes may occur several days after intestinal symptoms, and may cause permanent disability or death depending upon which microbe is ingested [ 1 , 9 ].
In developing countries, many poisoning cases are due to the consumption of unhygienic foods, pesticide residues in foods or water, and inappropriate food storage conditions. However, food poisoning is not a distinctive phenomenon of these countries only, as it also involves developed countries, due to the increasing demand for low-priced food and lack of ability to provide optimal care under hygienic conditions while preparing and storing food [ 5 , 10 ].
The incidence of food-borne illness depends on the hygienic measures implicated in food production and storage, but they could be ineffective if consumers have poor hygienic practices and food handling approaches [ 11 ]. Approximately 50% of food-borne illness cases are related to improper storage or reheating, with 45% associated with inappropriate food storage and 39% with cross contamination [ 12 ]. Knowledge, attitude and practice are key factors in reducing the incidence of food-borne diseases in foodservice areas [ 13 ]. They are also influenced by various factors like gender (females have a higher level of information than males), age (people younger than 35 years of age need extra food safety education), income level and cultural factors [ 14 , 15 ]. Therefore, evaluation of the baseline of such data (before any food safety education material can be prepared for their use) is an essential first step to inform the development of effective and relevant health education programmers to ensure that food handlers are knowledgeable about and experienced in food safety [ 16 , 17 ].
To the best of our knowledge, there are few studies conducted in Palestine regarding food poisoning or food-borne illnesses [ 18 , 19 , 20 , 21 , 22 ]. Therefore, the main objective of this study was to evaluate knowledge, attitude and practices related to food poisoning among parents in Nablus district, Palestine. However, regarding parents’ practices and knowledge regarding food poisoning in Palestine, our study may be the first one conducted in Palestine.
Study design and sampling strategy
In the current study, a descriptive cross-sectional method was applied. The study was conducted in four primary healthcare centres in Nablus, Palestine: Al-Makhfeyah; Ras-Alain; Al-Wosta; and Balata. Parents attending the centers with children aged less than 6 years were interviewed and their answers were transcribed.
A non-probability convenience sampling technique was used. A sample of 104 parents was selected from each primary healthcare centre. Inclusion criteria included parents 18 years old or older and gave consent to take part in the study. Exclusion criteria included parents who were not resident in the study area or had not given birth or who had children over 6 years or who had difficulty in communication.
Data collection form
A questionnaire in the native Arabic language adapted from a previous study [ 23 ] was used. The questionnaire consisted of four sections (see Additional file 1 ):
The first section included demographic information such as participants’ age, gender, educational level, employment status, residency, income level, number of family members including children, their ages, food preparation, and number of meals consumed away from home.
The second section consisted of 15 questions about food poisoning knowledge including general statements about food poisoning causes.
The third section consisted of 15 questions about food poisoning attitude including statements about eating raw food and washing fruits and vegetables.
In the fourth section, consisted of 20 questions about food poisoning practices regarding eating, drinking and washing hands.
In the knowledge and attitude section, the questionnaire provided five choices ranging from ‘strongly agree’ to ‘strongly disagree’. In the practice section, the respondents had five options: ‘always yes’; ‘most of the time’; ‘sometimes’; ‘rarely’; and ‘always no’. The questionnaire was tested with a pilot sample ( N = 30) before conducting the study and no changes were recommended. Permission to use this instrument to measure parents’ knowledge, attitude and practices regarding food poisoning in this study was obtained from the developers of the questionnaire [ 23 ].
Data collection procedure
Clinical pharmacists, who were well-trained on collecting data for the knowledge, attitude and practices questionnaire, carried out data collection. Parents were asked to complete the questionnaire during a face-to-face interview. Each questionnaire took 10–15 min to administer. Statements in the questionnaire were explained when necessary. A verbal consent form, explaining the purpose of the research and assuring confidentiality was read to participants. The participants had the right to participate or not. The data were collected on weekdays only. The collection process occurred from May to July 2015.
Ethical consideration
The Institutional Review Boards (IRB) of An-Najah National University authorized all aspects of the study protocol before the initiation of the study and approval to conduct the study was obtained from the Ministry of Health. Verbal consent was also obtained from all parents before participation.
Data statistical analysis
All analyses were performed using IBM SPSS statistics, version 20.0. Descriptive statistics were used to describe the sample. The responses were analyzed as correct or incorrect answers (see Additional file 2 ). Each correct answer was given one point while each incorrect answer was given zero point. Regarding knowledge, the five choices that ranged from ‘strongly agree’ to ‘strongly disagree’ were given values of 4 to 0, respectively. A correct answer indicated good knowledge, whereas an incorrect answer indicated poor knowledge. For attitude, this section included a set of negative statements (1–11) and the other four statements were positive (12–15). Negative statement choices had a value of 0 for ‘strongly agree’ and 4 for ‘strongly disagree’ and for positive statements it was the opposite (4 for ‘strongly agree’ and 0 for ‘strongly disagree’). A correct answer indicated a good attitude and an incorrect answer indicated a poor attitude. The practice section included six positive questions (1–6) with an answer choice value of 4 for ‘always yes’ and 0 for ‘always no’. The remaining questions (7–20) were negative with an answer choice value of 0 for ‘always yes’ and 4 for ‘always no’. A correct answer was indicated hygienic practice and a negative answer indicated unhygienic practice. Responses were consolidated into dichotomous (binary) variables for analysis. Previous studies had shown that consolidating a Likert scale to binary formats does not affect the results [ 24 , 25 ]. Data were presented as mean ± standard deviation (SD) or median and interquartile range (IQR) for numerical variables, and frequencies with percentages for nominal variables. All scores were tested for normality using the Kolmogorov–Smirnov test. Because the normality of all scores were not met, the Mann-Whitney U test and the Kruskal-Wallis H test were performed. The Pearson correlation coefficient was calculated to examine a possible correlation between continuous variables (knowledge, attitude and practices scores). In all analyses, a significance level of 5% was used.
Sociodemographic data
Demographic information for the sample is presented in Table 1 . Four-hundred and twelve questionnaires were collected from the primary care centres. Respondents were mostly females (92.7%). The mean age of respondents was 29.62 years (SD ± 6.380) and the median was 29.0 years with an interquartile range of 25.0–34.0. For educational level, the highest percentage was for high educational level followed by secondary level (40.8 and 38.8%, respectively). More than half of the respondents (66.9%) were living in a city and had an average income level of 500–1000 Jordanian Dinar (1 Jordanian Dinar (JD) equals 1.41 US Dollar); (59.2%). The majority was unemployed (78.9%) and reported that the mother is responsible for food preparation (96.3%).
Knowledge about food poisoning
The total knowledge score was 15. The mean knowledge score was 12.0 (SD = 2.2) and the median was 12.0 with an interquartile range of 11.0–14.0. Distribution of responses to each knowledge question is shown in Additional file 2 : Table S1. As shown in Additional file 2 : Table S1, 88.4% of the respondents agreed that pathogenic microbes cause food poisoning. When the respondents were asked about the highly risky foods for food poisoning, 93.2% of the respondents correctly agreed that eating raw or half-cooked meat is highly risky for food poisoning, 91.5% agreed that eating raw unwashed vegetables is highly risky for food poisoning and 87.1% agreed that drinking raw milk is highly risky for food poisoning. Moreover, 84.7, 82.8, 78.3, 74.3 and 70.9% of the respondents agreed correctly that raw white cheese, unwashed not pealed fruits, uncovered leftover cooked food, untreated surface and rainwater, and raw eggs, respectively, were risky food.
The majority of respondents agreed that well cooked food is free from microbes that cause food poisoning (91.3%) and that keeping food at refrigerator will slow down the microbial growth and multiplication, so, prevent food poisoning (90.2%). Approximately two thirds of the respondents agreed that there is no risk of food poisoning from eating leftover cooked food kept in refrigerator for 2-3 days. Eighty three percent of the respondents agreed that unhygienic practice of food handlers could be the source of microbial contamination of the food, which causes food poisoning. On the other hand, only 49.0% of the respondents correctly agreed that some toxins produced by microbes and cause food poisoning are resistant to heating temperature of food. Detailed responses are shown in Additional file 2 : Table S1 and S2.
The Kruskal-Wallis test was used to analyse the association between sociodemographic factors and knowledge. According to that, both educational level and residence area show a significant association with knowledge ( p < 0.05) (Table 2 ). On the other hand, there was no significant association between age and gender with knowledge. Respondents with a high level of education reported good knowledge (median = 13.0), more so than others with secondary or primary level (median = 12.0). As the educational level increased, knowledge increased ( p < 0.05). Respondents who live in a city or village reported good knowledge (median = 13.0), more so than those living in a camp (median = 11.0). Knowledge increased as residency situation improved ( p < 0.05).
Attitude regarding food poisoning
The total attitude score was 15, while the mean attitude score was 11.1 (SD = 2.5) and the median was 11.0 with an interquartile range of 10.0–13.0. Distribution of responses to each attitude question is shown in Additional file 2 : Table S3. As shown in Additional file 2 : Table S3, the majority of the respondents reported that washing hands with soap before preparing (96.4%) and eating food (96.1%) along with thorough washing of vegetables and fruits (95.6%) are necessary to prevent food poisoning. Two thirds of the respondents correctly agreed that food handlers without clinical symptoms could contaminate food with pathogenic microbes, which cause food poisoning. Regarding raw milk, 82.0% of the respondents correctly disagreed that there is no risk of disease from drinking raw goat or cow milk right after milking, 76.7% correctly disagreed that raw milk is more healthy and nutritious than pasteurized or boiled milk and 71.4% disagreed there is no risk of disease from drinking the milk of the camel right after milking. Regarding raw eggs, 68.4% of respondents correctly disagreed that raw eggs are more healthy and nutritious than cooked ones, while 36.2% wrongly agreed that there is no risk of disease from drinking raw eggs. A great percentage of the respondents correctly disagreed the statement that there is no risk of disease from eating raw meat of young animals. Regarding vegetables and fruits, 82.8% of the respondents disagreed that wiping vegetables or fruits make them safe to be eaten and 79.9% disagreed the statement that there is no risk of disease from eating unwashed vegetables and herbs picked up directly from the plant. On the other hand, about two thirds of the respondents wrongly agreed that baby feces are free from pathogenic microbes if he/she is not sick. About forty-six percentage of the respondents wrongly agreed that rainwater collected in reservoir is safe to drink without any treatment and 43.7% agreed that there is no risk of disease from eating cooked food kept at room temperature for 1 day if covered. Detailed responses are shown in Additional file 2 : Table S3 and S4.
Table 3 shows the significant association between attitude and two of the demographics: educational level and income level (Kruskal-Wallis test, p < 0.05). Age, gender, employment status and residency did not show a significant association with attitude. Respondents with a high educational level reported a good attitude (median = 12.0), more than those with lower levels (median = 11.0). As the educational level increased, attitude was improved ( p < 0.05). Respondents who have high-income levels (i.e. 1001–2999 JD (1 JD equals 1.41 US Dollar)) reported a good attitude (median = 12.0), more than those having a lower one (median = 11.0). As income level increased, attitude improved ( p < 0.05).
Practices regarding food safety
The total practice score was 20. The mean practice score was 17.3 (SD = 2.6) and the median was 18.0 with an interquartile range of 16.0–19.0. Distribution of responses to each practices question is shown in Additional file 2 : Table S5. As shown in Additional file 2 : Table S5, parents’ responses suggest that 95.9% of the respondents wash their hands with soap and water before both eating and preparing food, after contact with animals (98.3%) and after using the toilet (99.3%). About 98% of the respondents wash fresh vegetables and fruits before eating and 72.3% wash their hands with water and soap after handling raw unwashed vegetables. On the other hand, more than one third of the respondents may eat fresh vegetables and fruits after just wiping it (35.9%), without washing it (31.8%) or pick up it from the plants during a field trip and eat it without washing (34.7%). The majority of the respondents do not eat raw eggs, but about one quarter of them may eat half-cooked eggs (i.e. egg yolk is soft) (24.8%). Over 90 % of the respondents do not eat raw or half-cooked meat (96.1 and 94.2%, respectively) and do not drink raw cow, goat (94.2%), or camel milk (94.4%). Although that, about 20 % of the respondents may eat raw white cheese prepared from raw un-pasteurized milk. When the respondents were asked about cooked food left at room temperature for over 6 h without sufficient heating, only 28.2% said that they might eat it. A high percentage of respondents don’t eat from a restaurant or cafeteria looks not clean (96.4%), don’t drink from rainwater collected without any treatment (83.3%) and don’t eat food, like meat and rice and soup, by hand from a bowl shared by several people (91.7%). Detailed responses are shown in Additional file 2 : Table S5 and S6.
The results as shown in Table 4 indicate that gender and employment status were significantly associated with practice towards food poisoning with p < 0.05 (Mann-Whitney U test) and residency was significantly associated with it (Kruskal-Wallis test, p < 0.05). Other demographics did not show any significant association with practice towards food poisoning like age, educational level and income level. Female participants reported hygienic practice (median = 18.0) more than male participants (median = 16.0), so, hygienic practice towards food poisoning is higher in females than males ( p < 0.05). Hygienic practice towards food poisoning is higher among non-working consumers than working ones ( p < 0.05). The medians for both were 18.0 and 17.0, respectively. Respondents who live in a village reported hygienic practice towards food poisoning (median = 19.0), more than those living in a city (median = 18.0). Those living in a camp reported the lowest hygienic practice (median = 16.0). Living situation improvement is not necessary to increase hygienic practice towards food poisoning ( p < 0.05).
The correlations between knowledge, attitude and practice scores regarding food poisoning
A significant modest positive correlation was shown between respondents’ knowledge and attitude scores regarding food poisoning ( r = 0.240, p < 0.001). The results mean that respondents who had good knowledge were more likely to have a good attitude towards food poisoning. A significant modest positive correlation was demonstrated between respondents’ knowledge and practice scores regarding food poisoning ( r = 0.227, p < 0.001). Taken together, these results indicate that respondents who had good knowledge were more likely to have hygienic practices towards food poisoning. There was a significant modest positive correlation between respondents’ attitude and practice scores regarding food poisoning ( r = 0.303, p < 0.001), which means that respondents who had a good attitude were more likely to have hygienic practice towards food poisoning.
This study was designed to assess and evaluate the level of knowledge, attitude and practices among Palestinian parents regarding food poisoning and to determine if they have acceptable levels of them. As mentioned in the literature review, there are no studies undertaken to discuss parents’ knowledge, attitude and practices regarding food poisoning in Palestine.
The most obvious note to emerge from the analysis is that the sample has a bias to female participation with n = 382 female participants and n = 30 male participants. Additional factors such as parity, rural/urban status, household wealth status, and spouses’ education level would help to get a more complete view of possible predictive factors related to knowledge, attitude and practices towards food poisoning. However, in Middle Eastern Arab cultures, the female carries the responsibility for family care as a wife, from cleaning and arranging the house to preparing and cooking the food for all members of the family [ 26 , 27 ]. In addition, the female, as a mother, takes care of her children, and being a daughter, she will help her mother. Because of this responsibility, being the housekeeper generally and especially the main food preparer, she always seeks to protect her family members and does not want to cause them any suffering. Food preparers believe that any food prepared outside the home (i.e. in restaurants, cafeterias, hotels... etc.) will make them more susceptible to food poisoning and do not think that food prepared in the home may contribute to food poisoning [ 11 , 28 , 29 , 30 ]. A study that was conducted in the West Indies revealed that consumers think that 20% of food poisoning occurs in the home [ 28 ]. Although Day [ 31 ] found that the percentage of cases arising from food prepared at home may be underestimated in statistics for many reasons. Borneff et al. [ 32 ] reported that food-borne illness caused by food prepared at home is three times that caused by food prepared in cafeterias. The WHO reported that 40% of food-borne outbreaks occur at home [ 33 ]. Alsayeqh [ 34 ] found that insufficient cooking, unsatisfactory storage of food, cross contamination, and unsafe food sources are risks for food poisoning, Williamson et al. [ 35 ] found that 25% of food poisonings are due to inappropriate food handling and preparation, while Redmond & Griffith [ 16 ] estimated that 50–86% of reported food-borne outbreaks are associated with the home.
Several studies have shown that there are many variables that affect food safety knowledge, attitude, behaviours, perception and practice. Age, gender, education level, socio-economic status and employment status were the most important variables [ 15 , 17 , 36 , 37 ]. Food safety knowledge has been found to increase with age and length of practice, and females reported higher scores than males [ 38 ]. Bruhn and Schutz [ 39 ], Byrd-Bredbenner et al. [ 40 ] and Sudershan et al. [ 30 ] found that females have more information about food safety and appropriate food handling methods than males. Many studies that were conducted to examine the food safety knowledge among young adults further support the previous research [ 23 , 41 ].
On the other hand, Badrie et al. [ 28 ] reported that gender has no effect in the responses of consumers, while Unusan [ 42 ] found that males scored higher than females in food safety knowledge. Many studies found that very young or old adults, men, those of low educational and income levels have higher risky behaviours than younger people [ 5 , 43 ]. A possible explanation for low knowledge in young adults may be due to a lack of home economics courses in secondary schools that teach food safety [ 41 , 44 ]. Consumers with college education and those that work in food or nutrition related jobs reported higher knowledge scores than those with a high school degree and who had never worked in this area because of the training classes required of the employee [ 11 ]. Patil et al. [ 26 ] found that consumers with college education reported less safe practices than those without higher education, although they reported higher knowledge scores. Risky behaviours increase with increasing socio-economic status [ 45 ]. This inconsistency may be because safe food handling and consumption practices are developed by preparation experience in food preparing [ 46 ]. In other words, consumers living in higher socio-economic levels do not prepare food as often as those from lower levels.
In this study, the results seem to be consistent with other research which found that there was a significant association between educational level and knowledge score. Respondents with a high level of education reported higher knowledge scores than those with a lower level. In addition, respondents who live in a city or village reported higher scores than those living in camps. Another important finding was that age affects knowledge score, but the association was not significant. Surprisingly, gender affected neither knowledge nor attitude but significantly affected practice. This finding further supports the idea that females are more informed about appropriate food handling behaviours. Respondents with a high education level reported a good attitude compared to those with a lower level. Income level was also found to affect attitude score in that respondents with an income level of 1001–2999 JD (1 JD equals 1.41 US Dollar) scored higher than others. These results support the ideas [ 29 , 44 , 47 ] mentioned previously. In addition to gender, residency and employment status show a significant association with practice. Respondents who live in a village had greater hygienic practice than those living in a city, while those living in a camp reported the lowest hygienic practice. Working respondents scored lower than those who are not working. A possible explanation for this result may be the lack of adequate experience in food preparation between working respondents compared to those not working. These results support the findings of Issa et al. [ 22 ] that camp residents lack hygiene awareness and knowledge regarding food handling.
Redmond and Griffith [ 16 ] and Yarrow et al. [ 48 ] said that knowledge does not always participate in developing a positive attitude and behaviours, and Hogue et al. [ 49 ] reported that consumers have knowledge about food safety, but their knowledge is not always reflected in their food handling behaviours. In contrast to earlier findings, this study showed that there is a significant modest positive correlation between knowledge and both attitude and practice. In addition, there was a significant modest positive correlation between attitude and practice. As long as the consumer had good knowledge, he/she was more likely to have a good attitude and hygienic practice and as long as he/she had a good attitude, he/she had hygienic practice. These findings support those of Al-Shabib and his colleagues [ 50 ]. After analysing the data, it was somewhat encouraging and pleasing that 96.12, 90.77 and 98.30% of the respondents had good knowledge, a good attitude and hygienic practice, respectively.
The present results are significant in that they could be taken as a baseline for educating people about proper practice to reduce food poisoning. However, there are still many questions about this topic (i.e. food poisoning knowledge, attitude and practice in Palestine) and more research is needed to form a correct and clear view.
Strengths and limitations
The major strength of the present study is the relatively large sample size. In addition, a key strength of this study is that it is the first one in Palestine conducted to evaluate knowledge, attitude and practices level regarding food poisoning for parents. The major limitation of this study is that the data were collected by face-to-face interview, so, the respondents may answer in a manner that makes them look well informed, yet it does not give the real answers, thus we only measured and compared the reported practice and did not know if consumers actually did what they report doing. Being limited to Nablus, this study lacks representativeness of all Palestinian parents and represents only those in Nablus district. Another limitation that may affect the generalizability of the study is that the majority of the respondents were female and only 7.3% male. We also found that this analysis involved cross-sectional data so we are unable to determine the direction of the relationship between parents’ factors and levels of knowledge, attitude and practices towards food poisoning.
The main goal of the current study is to evaluate knowledge, attitude and practices regarding food poisoning among Palestinian parents in Nablus. This study shows that the respondents generally have good knowledge, a good attitude and hygienic practices (96.12, 90.77 and 98.30%, respectively). The study also found a significant positive correlation between knowledge, attitude and practice. Highly educated respondents and those who live in cities or villages have better knowledge than others.
Moreover, highly educated respondents and those with high-income levels have better attitudes. Unemployed females, as they have higher chance to prepare food at home, living in villages are more likely to have hygienic practices. In general, it seems that there is an emerging need for appropriate solutions. These findings suggest significant implications to be considered as a baseline for further investigations, and for building and applying awareness campaigns for educating the public on the importance of basic food safety. Educational programmes or campaigns should start with parental awareness regarding the direct hazards to their family health from food poisoning, as by realising their susceptibility to food poisoning, their motivation to change becomes stronger and beneficial, as parents are more likely to change their behaviours as long as it benefits their children.
Abbreviations
Interquartile range
Institutional Review Boards
Standard deviation
World Health Organization. Food safety. 2014. http://www.who.int/mediacentre/factsheets/fs399/en/ . Accessed 11 Apr 2016.
Grace D. Food safety in low and middle income countries. Int J Environ Res Public Health. 2015;12(9):10490–507.
Article CAS Google Scholar
Havelaar AH, Kirk MD, Torgerson PR, Gibb HJ, Hald T, Lake RJ, Praet N, Bellinger DC, de Silva NR, Gargouri N, et al. World health organization global estimates and regional comparisons of the burden of foodborne disease in 2010. PLoS Med. 2015;12(12):e1001923.
Article Google Scholar
Nyachuba DG. Foodborne illness: is it on the rise? Nutr Rev. 2010;68(5):257–69.
Quinlan JJ. Foodborne illness incidence rates and food safety risks for populations of low socioeconomic status and minority race/ethnicity: a review of the literature. Int J Environ Res Public Health. 2013;10(8):3634–52.
Bender JB, Smith KE, Hedberg C, Osterholm MT. Food-borne disease in the 21st century. What challenges await us? Postgrad Med. 1999;106(2):109–12 115–106, 119.
Centers for Disease Control and Prevention. Foodborne Germs and Illnesses. 2015. http://www.cdc.gov/foodsafety/foodborne-germs.html . Accessed 11 Apr 2016.
University of Rhode Island. Causes and prevention of foodborne illness. 2015. https://web.uri.edu/foodsafety/cause-and-prevention-of-foodborne-illness/ . Accessed 14 May 2019.
Acheson DW. Patient information: food poisoning (food-borne illness) (beyond the basics). 2014. http://www.uptodate.com/contents/food-poisoning-foodborne-illness-beyond-the-basics?source=search_result&search=food+poisoning+food+borne+illness+beyond+the+basics&selectedTitle=2~150 . Accessed 11 Apr 2016.
Signs RJ, Darcey VL, Carney TA, Evans AA, Quinlan JJ. Retail food safety risks for populations of different races, ethnicities, and income levels. J Food Prot. 2011;74(10):1717–23.
Meysenburg R, Albrecht JA, Litchfield R, Ritter-Gooder PK. Food safety knowledge, practices and beliefs of primary food preparers in families with young children. A mixed methods study. Appetite. 2014;73(1):121–31.
Bean NH, Griffin PM. Foodborne disease outbreaks in the United States, 1973-1987: pathogens, vehicles, and trends. J Food Prot. 1990;53(9):804–17.
Harun H, Abd Samad N, Mohd Hassan N, Abdul Rahman AW. Relationship between knowledge and practice among food handlers in vocational college Johor state: does lt compliance with food safety standards guide. In: 3d UPL Internitional Conference on Technical and Vocational Education and Training: 13-14 November 2014; Bandung (lndonesia); 2014.
Google Scholar
Odeyemi OA, Sani NA, Obadina AO, Saba CKS, Bamidele FA, Abughoush M, Asghar A, Dongmo FFD, Macer D, Aberoumand A. Food safety knowledge, attitudes and practices among consumers in developing countries: an international survey. Food Res Int. 2019;116:1386–90.
Zanin LM, da Cunha DT, de Rosso VV, Capriles VD, Stedefeldt E. Knowledge, attitudes and practices of food handlers in food safety: an integrative review. Food Res Int. 2017;100(Pt 1:53–62.
Redmond EC, Griffith CJ. Consumer food handling in the home: a review of food safety studies. J Food Prot. 2003;66(1):130–61.
Soon JM, Baines R, Seaman P. Meta-analysis of food safety training on hand hygiene knowledge and attitudes among food handlers. J Food Prot. 2012;75(4):793–804.
Adwan G, Alqarem B, Adwan K. Prevalence of foodborne pathogens in meat samples in Palestine. Int Food Res J. 2015;22(5):1806–12.
Al-Khatib IA, Al-Mitwalli SM. Food sanitation practices in restaurants of Ramallah and Al-Bireh district of Palestine. East Mediterr Health J. 2009;15(4):951–8.
Al-Hindi A, Abdelraouf A, Elmanama AN, Hassan I, Salamah A. Occurrence of intestinal parasites and hygiene characters among food handlers in Gaza strip, Palestine. Ann Alquds Med. 2012;8:2–13.
Hammad OMM. Assessment of microbial quality of food samples in Nablus District (Master's thesis). Nablus: An-Najah National University; 2004.
Issa M, McHenry M, Issa AA, Blackwood RA. Access to safe water and personal hygiene practices in the Kulandia refugee camp (Jerusalem). Infect Dis Rep. 2015;7(4):6040.
Sharif L, Al-Malki T. Knowledge, attitude and practice of Taif University students on food poisoning. Food Control. 2010;21(1):55–60.
Grassi M, Nucera A, Zanolin E, Omenaas E, Anto JM, Leynaert B. Performance comparison of Likert and binary formats of SF-36 version 1.6 across ECRHS II adults populations. Value Health. 2007;10(6):478–88.
Rogith D, Yusuf RA, Hovick SR, Peterson SK, Burton-Chase AM, Li Y, Meric-Bernstam F, Bernstam EV. Attitudes regarding privacy of genomic information in personalized cancer therapy. J Am Med Inform Assoc. 2014;21(e2):e320–5.
Patil SR, Cates S, Morales R. Consumer food safety knowledge, practices, and demographic differences: findings from a meta-analysis. J Food Prot. 2005;68(9):1884–94.
Awad Allah MB, El-Shafei DA, Abdelsalam AE, Sheta SS. Knowledge, attitude and practice of female teachers regarding safe food handling; is it sufficient? An intervention study, Zagazig, Egypt. Egypt J Occup Med. 2017;41(2):271–87.
Badrie N, Gobin A, Dookeran S, Duncan R. Consumer awareness and perception to food safety hazards in Trinidad, West Indies. Food Control. 2006;17(5):370–7.
Subba Rao GM, Sudershan RV, Rao P, Vishnu Vardhana Rao M, Polasa K. Food safety knowledge, attitudes and practices of mothers: findings from focus group studies in South India. Appetite. 2007;49(2):441–9.
Sudershan RV, Rao GMS, Rao P, Rao MVV, Polasa K. Food safety related perceptions and practices of mothers – a case study in Hyderabad, India. Food Control. 2008;19(5):506–13.
Day C. Gastrointestinal disease in the domestic setting: what can we deduce from surveillance data? J Inf Secur. 2001;43(1):30–5.
CAS Google Scholar
Borneff J, Hassinger R, Wittig J, Edenharder R. Effective hygienic measurements in households today. Zbl Bakt Mik Hyg. 1988;187(4–6):404–13.
Food and agriculture organization, World Health Organization. The FAO-WHO Pan European conference on food safety and quality. 2002. http://www.fao.org/3/a-y3696e.pdf . Accessed 13 Apr 2016.
Alsayeqh AF. Foodborne disease risk factors among women in Riyadh, Saudi Arabia. Food Control. 2015;50:85–91.
Williamson DM, Gravani RB, Lawless HT. Correlating food safety knowledge with home food-preparation practices. Food Technol. 1992;46(5):94–100.
Evans EW, Redmond EC. Behavioral risk factors associated with listeriosis in the home: a review of consumer food safety studies. J Food Prot. 2014;77(3):510–21.
Al-Sakkaf A. Domestic food preparation practices: a review of the reasons for poor home hygiene practices. Health Promot Int. 2015;30(3):427–37.
Albrecht JA. Food safety knowledge and practices of consumers in the U.S.a. J Consum Stud Home Econ. 1995;19(2):119–34.
Bruhn CM, Schutz HG. Consumer food safety knowledge and practices. J Food Saf. 1999;19(1):73–87.
Byrd-Bredbenner C, Abbot JM, Wheatley V, Schaffner D, Bruhn C, Blalock L. Risky eating behaviors of young adults-implications for food safety education. J Am Diet Assoc. 2008;108(3):549–52.
Byrd-Bredbenner C, Maurer J, Wheatley V, Schaffner D, Bruhn C, Blalock L. Food safety self-reported behaviors and cognitions of young adults: results of a national study. J Food Prot. 2007;70(8):1917–26.
Unusan N. Consumer food safety knowledge and practices in the home in Turkey. Food Control. 2007;18(1):45–51.
Ayaz WO, Priyadarshini A, Jaiswal AK. Food safety knowledge and practices among Saudi mothers. Foods. 2018;7(12):193.
Altekruse SF, Street DA, Fein SB, Levy AS. Consumer knowledge of foodborne microbial hazards and food-handling practices. J Food Prot. 1996;59(3):287–94.
Klontz KC, Timbo B, Fein S, Levy A. Prevalence of selected food consumption and preparation behaviors associated with increased risks of food-borne disease. J Food Prot. 1995;58(8):927–30.
Altekruse SF. Effectiveness of consumer labels for the safety of foods of animal origin. J Am Vet Med Assoc. 1996;209(12):2056.
CAS PubMed Google Scholar
Ozilgen S. Food safety education makes the difference: food safety perceptions, knowledge, attitudes and practices among Turkish university students. J Verbrauch Lebensm. 2010;6(1):25–34.
Yarrow L, Remig VM, Higgins MM. Food safety educational intervention positively influences college students’ food safety attitudes, beliefs, knowledge, and self-reported practices. J Environ Health. 2009;71(6):30–5.
PubMed Google Scholar
Hogue AT, White PL, Heminover JA. Pathogen reduction and Hazard analysis and critical control point (HACCP) Systems for Meat and Poultry. Vet Clin North Am Food Anim Pract. 1998;14(1):151–64.
Al-Shabib NA, Mosilhey SH, Husain FM. Cross-sectional study on food safety knowledge, attitude and practices of male food handlers employed in restaurants of King Saud University, Saudi Arabia. Food Control. 2016;59:212–7.
Download references
Acknowledgments
Not applicable
No funding was received in preparation of this study.
Availability of data and materials
The raw data supporting the findings presented in this study will be available from the corresponding author upon request.
Author information
Authors and affiliations.
Poison Control and Drug Information Center (PCDIC), College of Medicine and Health Sciences, An-Najah National University, Nablus, 44839, Palestine
Sa’ed Zyoud
Department of Clinical and Community Pharmacy, College of Medicine and Health Sciences, An-Najah National University, Nablus, 44839, Palestine
Sa’ed Zyoud & Samah Al-Jabi
PharmD program, College of Medicine and Health Sciences, An-Najah National University, Nablus, 44839, Palestine
Jawad Shalabi, Kathem Imran, Lina Ayaseh, Nawras Radwany, Ruba Salameh & Zain Sa’dalden
Department of Veterinary Pathology and Public Health, Faculty of Veterinary Medicine, Jordan University of Science and Technology, Irbid, 22110, Jordan
Labib Sharif
Department of Pharmacology and Toxicology, College of Medicine and Health Sciences, An-Najah National University, Nablus, 44839, Palestine
Waleed Sweileh
WHO Collaborating Centre for Drug Information, National Poison Centre, Universiti Sains Malaysia (USM), 11800, Penang, Malaysia
Rahmat Awang
You can also search for this author in PubMed Google Scholar
Contributions
JS, KI, LA, NR, RS, and ZS collected data, performed the analyses and literature search, and drafted the manuscript. SZ conceptualized and designed the study, coordinated, supervised and analyzed the data, and assisted in final write-up of the manuscript. WS, SA, RA, and LS developed the study design and methodology, and helped to interpret and analyse the data and redrafted the manuscript. SZ and SA addressed the reviewers’ comments. Then all read, and approved the final manuscript.
Corresponding author
Correspondence to Sa’ed Zyoud .
Ethics declarations
Ethics approval and consent to participate.
Approval to conduct this study, including verbal consent, was granted by An-Najah National University Institutional Review Board before initiation of this study. Verbal consent was obtained from the parents before starting data collection. Informed verbal consent was granted by all participants rather than written consent because the research did not involve any therapeutic intervention and the participations in the study were clearly below minimal risk.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Study questionnaires. This is the final English version of the questionnaire that was used to obtain data that helps to evaluate knowledge, attitude, and practices related to food poisoning among parents of children in Nablus, Palestine. (DOCX 27 kb)
Additional file 2:
Table S1 . Parents’ knowledge responses with correct answers. Table S2. Distribution of responses to each knowledge question with a five-point Likert scale ranked from 1 to 5 (Strongly disagree, disagree, not sure, agree, and strongly agree). Table S3. Parents’ attitude responses with correct answers. Table S4. Distribution of responses to each attitude question with a five-point Likert scale ranked from 1 to 5 (Strongly disagree, disagree, not sure, agree, and strongly agree). Table S5. Parents’ practice responses with correct answers. Table S6. Distribution of responses to each practice question with a five-point Likert scale ranked from 1 to 5 (Always yes, most of the time, sometimes, rarely, always no). (DOCX 27 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Zyoud, S., Shalabi, J., Imran, K. et al. Knowledge, attitude and practices among parents regarding food poisoning: a cross-sectional study from Palestine. BMC Public Health 19 , 586 (2019). https://doi.org/10.1186/s12889-019-6955-2
Download citation
Received : 16 May 2018
Accepted : 08 May 2019
Published : 16 May 2019
DOI : https://doi.org/10.1186/s12889-019-6955-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Food poisoning
- Food safety
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Bibliography
- More Referencing guides Blog Automated transliteration Relevant bibliographies by topics
- Automated transliteration
- Relevant bibliographies by topics
- Referencing guides
Dissertations / Theses on the topic 'Food poisoning'
Create a spot-on reference in apa, mla, chicago, harvard, and other styles.
Consult the top 50 dissertations / theses for your research on the topic 'Food poisoning.'
Next to every source in the list of references, there is an 'Add to bibliography' button. Press on it, and we will generate automatically the bibliographic reference to the chosen work in the citation style you need: APA, MLA, Harvard, Chicago, Vancouver, etc.
You can also download the full text of the academic publication as pdf and read online its abstract whenever available in the metadata.
Browse dissertations / theses on a wide variety of disciplines and organise your bibliography correctly.
North, Richard Anthony Edward. "The quality of public sector food poisoning surveillance in England and Wales with specific reference to salmonella food poisoning." Thesis, Leeds Beckett University, 1995. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.523484.
Hennekinne, Jacques-Antoine. "Innovative approaches to improve staphylococcal food poisoning characterization." Phd thesis, AgroParisTech, 2009. http://pastel.archives-ouvertes.fr/pastel-00005863.
Worsfold, Denise. "An evaluation of domestic food hygiene and food preparation practices." Thesis, Open University, 1994. http://oro.open.ac.uk/57506/.
Mutsaers, Barbara Rosalia Hillegonda. "Food poisoning and other food hazards : risk perceptions and implications for risk communication." Thesis, University of Reading, 1996. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.306894.
Chan, Hon-wing, and 陳漢榮. "Food poisoning outbreaks in Hong Kong resulting from shellfish contamination." Thesis, The University of Hong Kong (Pokfulam, Hong Kong), 1996. http://hub.hku.hk/bib/B31253349.
Al-Hamami, L. A. A. J. "Evaluation of factors influencing salmonella food-poisoning organisms in meat." Thesis, University of Strathclyde, 1987. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.382280.
Chan, Hon-wing. "Food poisoning outbreaks in Hong Kong resulting from shellfish contamination /." Hong Kong : University of Hong Kong, 1996. http://sunzi.lib.hku.hk/hkuto/record.jsp?B17457762.
Krokos, Fragoulis. "Congener-specific determination of ortho and non-ortho chlorobiphenyls in food." Thesis, University of East Anglia, 1994. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.385867.
Fonseka, Thithalapitige Sunil Gamini. "Molecular typing of food poisoning bacteria isolated from farm shrimp and poultry." Thesis, University of Nottingham, 1993. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.316950.
Ross, Zara M. "Modes of action of antimicrobial garlic derivatives." Thesis, University of Wolverhampton, 1994. http://hdl.handle.net/2436/88279.
McKee, Rosemary. "The occurrence and adherence of verocytotoxin producing Escherichia coli strains in relation to food processing." Thesis, Queen's University Belfast, 2002. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.246523.
Dhir, Vinod Kumar. "The resistance of surface-attached Salmonella enteritidis to inimical processes." Thesis, University of Nottingham, 1995. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.309595.
Amoah, E., and A. S. Sydorchuk. "The Co-Infection Case Study: Could Staphylococcal Food-borne ToxicInfection "Improved" Severity Course of Food-Borne Botulism?" Thesis, "Chyst", 2016. http://dspace.bsmu.edu.ua:8080/xmlui/handle/123456789/10866.
Hancock, Ian. "Studies on the rapid detection of the food-borne pathogen Listeria monocytogenes." Thesis, London Metropolitan University, 1995. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.295022.
Meredith, Lucy Margaret. "The impact of consumer behaviour as a cause of food poisoning in the home." Thesis, University of the West of England, Bristol, 2001. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.365187.
Öberg, Erika. "Livsmedelsäkerhet i förskolan : Vilka rutiner har förskolan och finns det skillnad i livsmedelsäkerheten beroende på personalens utbildning." Thesis, Umeå universitet, Institutionen för ekologi, miljö och geovetenskap, 2015. http://urn.kb.se/resolve?urn=urn:nbn:se:umu:diva-105197.
Haque, Ahwarul. "Characterisation of Bacillus cereus strains in Bangladeshi rice." Thesis, Imperial College London, 2002. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.272635.
Bird, Julie Ann. "Detection of sub-lethally injured salmonellae in foods." Thesis, University of Portsmouth, 1990. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.277229.
Jones, Eleanor. "Osmotic adaptations of Staphylococcus aureus." Thesis, University of Nottingham, 1999. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.310928.
Walker, Athene Jayne. "The use of bioluminescent Listeria monocytogenes for rapid biocide assays." Thesis, University of Nottingham, 1994. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.385244.
Campbell, Kathryn Deirdre. "Molecular inter-relationships of psychrotrophic Clostridium botulinum based on 23S rRNA and BoNT genes." Thesis, University of Reading, 1994. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.262610.
Fowler, Richard Paul. "The acid tolerance response of enteropathogenic Salmonella and Escherichia coli strains : a proteomic characterisation and novel links with motility and virulence." Thesis, University of Southampton, 2000. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.340361.
Seeiso, Tabitha Masentle. "Bacteriological quality of meat in Lesotho." Pretoria : [s.n.], 2010. http://upetd.up.ac.za/thesis/available/etd-02262010-165323/.
Bishop, Simon Shurene Patrice. "Characterisation of Listeria monocytogenes using targeted proteomic analysis." Thesis, Queen Mary, University of London, 2012. http://qmro.qmul.ac.uk/xmlui/handle/123456789/8666.
Docherty, Pauline Fletcher. "The survival during milk processing of bacillus cereus with the potential to cause food-borne illness." Thesis, Glasgow Caledonian University, 2000. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.325996.
Oh, Mi Hwa School of Chemical Engineering & Industrial Chemistry UNSW. "Ecology of toxigenic bacillus species in rice products." Awarded by:University of New South Wales. School of Chemical Engineering and Industrial Chemistry, 2006. http://handle.unsw.edu.au/1959.4/23942.
Wilson, Ian Gerald. "Detection of Staphylococcus aureus by DNA hybridization." Thesis, Queen's University Belfast, 1990. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.335445.
McDermid, Ann Sheena. "The influence of pH on the survival and pathogenicity of Salmonella enteritidis phage-type 4." Thesis, Open University, 1998. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.264476.
Goeksoy, E. O. "Decontamination of poultry meat by intense heat treatment." Thesis, University of Bristol, 1999. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.297810.
Pearson, Susan M. "Studies on microbiological hazards associated with ethnic foods, with particular reference to mycotoxin formation and clostridium perfringens." Thesis, Glasgow Caledonian University, 2000. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.325965.
Lim, Kyungwha. "Reduction of spoilage and pathogenic bacteria on beef products by direct and indirect applications of antimicrobial agents /." free to MU campus, to others for purchase, 2003. http://wwwlib.umi.com/cr/mo/fullcit?p3100061.
Campbell, Penelope Tracy. "Assessing the knowledge, attitudes and practices of street food vendors in the City of Johannesburg regarding food hygiene and safety." Thesis, University of the Western Cape, 2011. http://etd.uwc.ac.za/index.php?module=etd&action=viewtitle&id=gen8Srv25Nme4_1212_1318930550.
Currie, Janet Elizabeth. "Joint modelling of point process and geostatistical measurement data." Thesis, Lancaster University, 1998. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.268124.
Orsburn, Benjamin. "Factors Affecting the Heat Resistance of Clostridium perfringens Spores." Diss., Virginia Tech, 2009. http://hdl.handle.net/10919/27697.
Ting, Wei-tsyi. "Studies on the death, injury, repair of injury, and the detection of Salmonella subjected to freezing and thawing /." The Ohio State University, 1986. http://rave.ohiolink.edu/etdc/view?acc_num=osu1487267546984344.
Juranovic, Lillian Regina 1962. "Determination of the toxic/mutagenic potential of toxins associated with ciguatera dinoflagellates." Thesis, The University of Arizona, 1989. http://hdl.handle.net/10150/277164.
Ghosh, Abhinaba. "Molecular analysis of GerP and spore-associated proteins of Bacillus cereus." Thesis, University of Cambridge, 2018. https://www.repository.cam.ac.uk/handle/1810/273545.
Malherbe, WF. "Die gehalte van ondersoeke en die institusionele oordra van data oor aanmeldbare voedselvergiftigingsuitbrake." Thesis, Cape Technikon, 1997. http://hdl.handle.net/20.500.11838/801.
Harry, Kathryn Helene. "Sporulation and enterotoxin regulation by sigma factors in Clostridium perfringens." Thesis, Virginia Tech, 2008. http://hdl.handle.net/10919/42517.
Amaro, Emerson Clayton 1988. "Avaliação da qualidade microbiológica de alimentos prontos para consumo e ambientes em creches da rede pública de Campinas/SP." [s.n.], 2013. http://repositorio.unicamp.br/jspui/handle/REPOSIP/254591.
Tian, Li, and 田理. "Toxicological effects and mechanisms of selected foodborne toxins in medaka and zebrafish models." Thesis, The University of Hong Kong (Pokfulam, Hong Kong), 2013. http://hdl.handle.net/10722/197111.
Seeiso, Tabitha Masentle. "Bacteriological quality of meat in Lesotho." Diss., University of Pretoria, 2009. http://hdl.handle.net/2263/22861.
Rösemann, G. M. "Analysis of pyrrolizidine alkaloids in Crotalaria species by HPLC-MS/MS in order to evaluate related food health risks." Electronic thesis, 2006. http://upetd.up.ac.za/thesis/available/etd-08032007-170633/.
Sun, Bin. "Essays on environmental economics and resource management." Columbus, Ohio : Ohio State University, 2007. http://rave.ohiolink.edu/etdc/view?acc%5Fnum=osu1180553781.
Coleman, Philip Dennis. "A study of knowledge, attitudes and behaviour with regard to food safety, in the Welsh hospitality and catering industry." Thesis, n.p, 2000. http://ethos.bl.uk/.
Lok, Wai-shing. "The food health policy of Hong Kong SAR Government." Hong Kong : University of Hong Kong, 2001. http://sunzi.lib.hku.hk/hkuto/record.jsp?B23530145.
HAMAJIMA, NOBUYUKI, KOUTARO TOMITA, YUKAKO HINOHARA, and NOBUYUKI KATSUDA. "STRUCTURE AND ROLES OF PUBLIC HEALTH CENTERS (HOKENJO) IN JAPAN." Nagoya University School of Medicine, 2011. http://hdl.handle.net/2237/14916.
Fonte, Ângela Isabel Espinha da. "Queijo de coalho do sertão Alagoano: enterotoxigenicidade de S. aureus pela reacção em cadeia polimerase (PCR)." Master's thesis, ISA/UTL, 2011. http://hdl.handle.net/10400.5/4164.
Mamprim, Filho Adel [UNESP]. "Enterotoxinas de Staphylococus coagulase positiva e negativa isoladas das fossas nasais e mãos de manipuladores de alimentos." Universidade Estadual Paulista (UNESP), 2006. http://hdl.handle.net/11449/98321.
Shivers, Sean Alexander. "Utilizing Food Safety Knowledge in Comprehensive Patient Care Among Harlem Hospital Physicians." ScholarWorks, 2019. https://scholarworks.waldenu.edu/dissertations/7746.
- Patient Care & Health Information
- Diseases & Conditions
- Food poisoning
Food poisoning, a type of foodborne illness, is a sickness people get from something they ate or drank. The causes are germs or other harmful things in the food or beverage.
Symptoms of food poisoning often include upset stomach, diarrhea and vomiting. Symptoms usually start within hours or several days of eating the food. Most people have mild illness and get better without treatment.
Sometimes food poisoning causes severe illness or complications.
Products & Services
- A Book: Mayo Clinic Guide to Home Remedies
Symptoms vary depending on what is causing the illness. They may begin within a few hours or a few weeks depending on the cause.
Common symptoms are:
- Upset stomach.
- Diarrhea with bloody stools.
- Stomach pain and cramps.
Less often food poisoning affects the nervous system and can cause severe disease. Symptoms may include:
- Blurred or double vision.
- Loss of movement in limbs.
- Problems with swallowing.
- Tingling or numbness of skin.
- Changes in sound of the voice.
When to see a doctor
Infants and children.
Vomiting and diarrhea can quickly cause low levels of body fluids, also called dehydration, in infants and children. This can cause serious illness in infants.
Call your child's health care provider if your child's symptoms include vomiting and diarrhea and any of the following:
- Unusual changes in behavior or thinking.
- Excessive thirst.
- Little or no urination.
- Diarrhea that lasts more than a day.
- Vomiting often.
- Stools that have blood or pus.
- Stools that are black or tarry.
- Severe pain in the stomach or rectum.
- Any fever in children under 2 years of age.
- Fever of 102 degrees Fahrenheit (38.9 degrees Celsius) or higher in older children.
- History of other medical problems.
Adults should see a health care provider or get emergency care if the following occur:
- Nervous system symptoms, such as blurry vision, muscle weakness and tingling of skin.
- Changes in thinking or behavior.
- Fever of 103 degrees Fahrenheit (39.4 degrees Celsius).
- Diarrhea that lasts more than three days.
- Symptoms of dehydration — excessive thirst, dry mouth, little or no urination, severe weakness, dizziness, or lightheadedness.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Many germs or harmful things, called contaminants, can cause foodborne illnesses. Food or drink that carries a contaminant is called "contaminated." Food can be contaminated with any of the following:
- Parasites that can live in the intestines.
- Poisons, also called toxins.
- Bacteria that carry or make toxins.
- Molds that make toxins.
Understanding terms
The term "food poisoning" is commonly used to describe all foodborne illnesses. A health care provider might use these terms to be more specific:
- "Foodborne illnesses" means all illnesses from any contaminated food or beverage.
- "Food poisoning" means illness specifically from a toxin in food. Food poisoning is a type of foodborne illness.
How food becomes contaminated
Food can be contaminated at any point from the farm or fishery to the table. The problem can begin during growing, harvesting or catching, processing, storing, shipping, or preparing.
Food can be contaminated any place it's handled, including the home, because of:
- Poor handwashing. Feces that remains on the hands after using the toilet can contaminate food. Other contaminants can be transferred from hands during food preparation or food serving.
- Not disinfecting cooking or eating areas. Unwashed knives, cutting boards or other kitchen tools can spread contaminants.
- Improper storage. Food left out for too long at room temperature can become contaminated. Food stored in the refrigerator for too long can spoil. Also, food stored in a refrigerator or freezer that is too warm can spoil.
Common causes
The following table shows common causes of foodborne illnesses, the time from exposure to the beginning of symptoms and common sources of contamination.
Other sources
Bacteria that cause foodborne illnesses can also be found in swimming pools, lakes, ponds, rivers and seawater. Also, some bacteria, such as E. coli, may be spread by exposure to animals carrying the disease.
Risk factors
Anyone can get food poisoning. Some people are more likely to get sick or have more-serious disease or complications. These people include:
- Infants and children.
- Pregnant people.
- Older adults.
- People with weakened immune systems due to another disease or treatments.
Complications
In most healthy adults, complications are uncommon. They can include the following.
Dehydration
The most common complication is dehydration. This a severe loss of water and salts and minerals. Both vomiting and diarrhea can cause dehydration.
Most healthy adults can drink enough fluids to prevent dehydration. Children, older adults, and people with weakened immune systems or other illnesses may not be able to replace the fluids they've lost. They are more likely to become dehydrated.
People who become dehydrated may need to get fluids directly into the bloodstream at the hospital. Severe dehydration can cause organ damage, other severe disease and death if not treated.
Complications of systemic disease
Some contaminants can cause more widespread disease in the body, also called systemic disease or infection. This is more common in people who are older, have weakened immune systems or other medical conditions. Systemic infections from foodborne bacteria may cause:
- Blood clots in the kidneys. E. coli can result in blood clots that block the kidneys' filtering system. This condition, called hemolytic uremic syndrome, results in the sudden failure of the kidneys to filter waste from the blood. Less often, other bacteria or viruses may cause this condition.
- Bacteria in the bloodstream. Bacteria in the blood can cause disease in the blood itself or spread disease to other parts of the body.
- Meningitis. Meningitis is inflammation that may damage the membranes and fluid surrounding the brain and spinal cord.
- Sepsis. Sepsis is an overreaction of the immune system to systemic disease that damages the body's own tissues.
Pregnancy complications
Illness from the listeria bacteria during pregnancy can result in:
- Miscarriage or stillbirth.
- Sepsis in the newborn.
- Meningitis in the newborn.
Rare complications
Rare complications include conditions that may develop after food poisoning, including:
- Arthritis. Arthritis is swelling, tenderness or pain in joints.
- Irritable bowel syndrome. Irritable bowel syndrome is a lifelong condition of the intestines that causes pain, cramping and irregular bowel movements.
- Guillain-Barre syndrome. Guillain-Barre syndrome is an immune system attack on nerves that can result in tingling, numbness and loss of muscle control.
- Breathing difficulties. Rarely, botulism can damage nerves that control the muscles involved in breathing.
To prevent food poisoning at home:
- Handwashing. Wash your hands with soap and water for at least 20 seconds. Do this after using the toilet, before eating, and before and after handling food.
- Wash fruits and vegetables. Rinse fruits and vegetables under running water before eating, peeling or preparing.
- Wash kitchen utensils thoroughly. Wash cutting boards, knives and other utensils with soapy water after contact with raw meats or unwashed fruits and vegetables.
- Don't eat raw or undercooked meat or fish. Use a meat thermometer to make sure meat is cooked enough. Cook whole meats and fish to at least 145 F (63 C) and let rest for at least three minutes. Cook ground meat to at least 160 F (71 C). Cook whole and ground poultry to at least 165 F (74 C).
- Refrigerate or freeze leftovers. Put leftovers in covered containers in the refrigerator right after your meal. Leftovers can be kept for 3 to 4 days in the refrigerator. If you don't think you'll eat them within four days, freeze them right away.
- Cook leftovers safely. You can safely thaw frozen food three ways. You can microwave it. You can move it to the refrigerator to thaw overnight. Or you can put the frozen food in a leakproof container and put it in cold water on the counter. Reheat leftovers until the internal temperature reaches 165 degrees Fahrenheit (74 degrees Celsius).
- Throw it out when in doubt. If you aren't sure if a food has been prepared, served or stored safely, discard it. Even if it looks and smells fine, it may not be safe to eat.
- Throw out moldy food. Throw out any baked foods with mold. Throw out moldy soft fruits and vegetables, such as tomatoes, berries or peaches. And throw away any nuts or nut products with mold. You can trim away mold from firm foods with low moisture, such as carrots, bell peppers and hard cheeses. Cut away at least 1 inch (2.5 centimeters) around the moldy part of the food.
- Clean your refrigerator. Clean the inside of the refrigerator every few months. Make a cleaning solution of 1 tablespoon (15 milliliters) of baking soda and 1 quart (0.9 liters) of water. Clean visible mold in the refrigerator or on the door seals. Use a solution of 1 tablespoon (15 milliliters) of bleach in 1 quart (0.9 liters) of water.
Safety for at-risk people
Food poisoning is especially serious during pregnancies and for young children, older adults and people with weakened immune systems. These illnesses may be life-threatening. These individuals should avoid the following foods:
- Raw or undercooked meat, poultry, fish, and shellfish.
- Raw or undercooked eggs or foods that may contain them, such as cookie dough and homemade ice cream.
- Raw sprouts, such as alfalfa, bean, clover and radish sprouts.
- Unpasteurized juices and ciders.
- Unpasteurized milk and milk products.
- Soft cheeses, such as feta, brie and Camembert; blue-veined cheese; and unpasteurized cheese.
- Refrigerated pates and meat spreads.
- Uncooked hot dogs, luncheon meats and deli meats.
- Foodborne germs and illnesses. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/foodsafety/foodborne-germs.html. Accessed Nov. 7, 2022.
- Definition & facts of food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/definition-facts. Accessed Nov. 7, 2022.
- Symptoms & causes of food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/symptoms-causes. Accessed Nov. 7, 2022.
- LaRocque R. Causes of acute infectious diarrhea and other foodborne illnesses in resource-rich settings. https://www.uptodate.com/contents/search. Accessed Nov. 7, 2022.
- Bennett JE, et al. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Nov. 7, 2022.
- Schmitt BD. Pediatric Telephone Protocols: Office Version. 17th ed. American Academy of Pediatrics; 2021.
- Fever. American College of Emergency Physicians. https://www.emergencyphysicians.org/article/know-when-to-go/fever. Accessed Nov. 30, 2022.
- Bacteria and viruses. FoodSafety.gov. U.S. Department of Health and Human Services. https://www.foodsafety.gov/food-poisoning/bacteria-and-viruses. Accessed Nov. 16, 2022.
- Kellerman RD, et al. Foodborne illnesses. In: Conn's Current Therapy 2022. Elsevier; 2022. https://www.clinicalkey.com. Accessed Nov. 13, 2022.
- Goldman L, et al., eds. Giardiasis. Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Nov. 13, 2022.
- Diagnosis of food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/diagnosis. Accessed Nov. 7, 2022.
- LaRocque R. Approach to the adult with acute diarrhea in resource-rich settings. https://www.uptodate.com/contents/search. Accessed Nov. 7, 2022.
- Treatment for food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/treatment. Accessed Nov. 7, 2022.
- Eating, diet and nutrition for food poisoning. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/food-poisoning/eating-diet-nutrition. Accessed Nov. 20, 2022.
- Four steps to food safety: Clean, separate, cook, chill. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/foodsafety/keep-food-safe.html. Accessed Nov. 7, 2022.
- Leftovers and food safety. U.S. Department of Agriculture. https://www.fsis.usda.gov/food-safety/safe-food-handling-and-preparation/food-safety-basics/leftovers-and-food-safety. Accessed Nov. 20, 2022.
- Foods that can cause food poisoning. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/foodsafety/foods-linked-illness.html. Accessed Nov. 20, 2022.
- Molds on food: Are they dangerous? Food Safety and Inspection Service. U.S. Department of Agriculture. https://www.fsis.usda.gov/food-safety/safe-food-handling-and-preparation/food-safety-basics/molds-food-are-they-dangerous Accessed Dec. 1, 2022.
News from Mayo Clinic
- Mayo Clinic Minute: Food recalls and sickness Oct. 16, 2024, 01:07 p.m. CDT
- 4 essential food safety tips for summertime gatherings July 04, 2024, 02:00 p.m. CDT
- Mayo Clinic Minute: Tips for safer picnics May 24, 2024, 03:00 p.m. CDT
- Mayo Clinic Minute: Does one moldy berry spoil the whole bunch? March 09, 2023, 03:30 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- NEW: Listen to Health Matters Podcast - Mayo Clinic Press NEW: Listen to Health Matters Podcast
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

IMAGES
COMMENTS
the prevention of food poisoning among respondents. For the practical part, six studies had a good level, two studies showed that there was an average score of food safely towards practices and food poisoning prevention, and one study reported that there were unsatisfactory food safety practices. In the reviewed studies, there was a positive
Food poisoning (FP) refers to a group of illnesses that result from the ingestion of contaminated food that contains infectious organisms. FP is defined as "illnesses caused by bacteria or other toxins in food, typically with vomiting and diarrhea."[ 2 ] It was estimated that 76 million illnesses because of foodborne diseases resulted in ...
Food poisoning is a food borne disease, mainly resulting from ingestion of food that contains a toxin, chemical or infectious microorganisms like bacteria, virus, parasite, or prion. On the other hand, avoiding food contamination during preparing and feeding is a key factor for reducing the prevalence of food poisoning. This study aimed to ...
Food poisoning caused by food import is one of the reasons for the region's low economic growth. The costs of illness and death are high for individuals, families, and countries' health-care systems.
Observance of food safety and security is a critical phase for the food industry, and the safety and moreover the security of food items depends upon the capability to identify and trace pathogenic microbes (Scallan et al., 2011, Yamada et al., 2016).The most significant factors contributing to foodborne poisoning are termed "foodborne illness risk factors" by the US Food and Drug ...
The application of tourism health, such as food safety, is an important matter to pay attention to. Based on the annual report (BPOM, 2019), there are 373 cases of food poisoning in Bali, so Bali ...
Food poisoning is a disease caused by the consumption of food or water contaminated with bac-teria and/or their toxins, chemicals, viruses, or parasites. Improper food or drink handling, pro-duction, or storage usually bring about food contamination [1]. The prevention of food
Abstract. Food poisoning is an illness caused by ingestion of contaminated food or drink. Contamination can be caused by bacteria or viruses, and less often by parasites or chemicals. According to a report released by the Food Standards Agency, the estimated number of food-borne disease-related cases that occurred in 2018 was 2 400 000, costing ...
Background Food serves as a vehicle for many pathogenic and toxigenic agents that cause food-borne diseases. Knowledge, attitude, and practices are key factors in reducing the incidence of food-borne diseases in food service areas. The main objective of this study was to evaluate knowledge, attitude, and practices related to food poisoning among parents of children in Nablus, Palestine ...
Temperature abuse during food transport and storage was exhibited by more than 40% of people. Cooked food was held at ambient temperature for prolonged periods by 19% of the people and was re-heated inadequately by 11%. The standard of personal hygiene of some participants was low.
2005 Malaysia Stall food T yphi 171 Nik and Sharifah, 2005 2004 China Cake/raw egg topping Enteritidis 197 D'Aoust and Maurer , 2007 2004 Great Britain Lettuce Newport >350 Montville and ...
The purpose of this thesis was to conduct a study on food safety risk assessment and suggest methods in managing potential risks in the field of risk management for industry ... or more commonly referred to as food poisoning is usually the consequence of the consumption of contaminated food. Negligence to meet food safety standards can
Food borne diseases are globally important, as they result in considerable morbidity, mortality, and economic costs. Many different sources like bacteria, viruses, parasites, chemicals, and prisons, may be transmitted to humans by contaminated food. Outbreaks and sporadic cases of food borne disease are regular occurrences in all countries of ...
Food poisoning means illness resulting from ingestion of. food w ith microbial o r non-microb ial contamination. [1] The condition is characterized by (a) history of ingestion. of a common foo d ...
Raw food, processes food Ready- to- eat fast foods must be cooked and served to the consumers with all hygienic measures. Keywords: food pathogens, staphylococcus aureus, e. coli, salmonella spp & clostridium spp. Introduction . Food poisoning is a term used to express any type of disease or illness after consuming food. Food poisoning, food
In Palestine, it was observed that poisoning materials are within the reach of children and the most common causes of poisoning were:- 1. Ingesting kerosene, medicine, or spoiled food. 2. Agricultural pesticides and fortunately, in many poisoning cases, the doses were much smaller than the lethal dose, so they resulted in mild poisoning.
Overview. Food poisoning, a type of foodborne illness, is a sickness people get from something they ate or drank. The causes are germs or other harmful things in the food or beverage. Symptoms of food poisoning often include upset stomach, diarrhea and vomiting. Symptoms usually start within hours or several days of eating the food.
Thesis statement: Food poisoning is a national problem, which has a direct impact on health and the economy. 2.0. Background There is a historical overview about food poisoning in Britain, the health care of Britain follows the first indication of food poisoning that is caused by a specific organism in 1880 after that moment food poisoning was ...