

4.2 Basic Concepts
Open Resources for Nursing (Open RN)
Before learning how to use the nursing process, it is important to understand basic concepts concerning how critical thinking relates to nursing practice. Let’s take a deeper look at how nurses think.
Critical Thinking and Clinical Reasoning
Nurses make decisions while providing client care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes “reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.” [1] Using critical thinking means that nurses take extra steps to maintain client safety and don’t just “follow orders.” It also means the accuracy of client information is validated and plans for caring for clients are based on their needs, current clinical practice, and research.
“Critical thinkers” possess certain attitudes that foster rational thinking. These attitudes are as follows:
- Independence of thought: Thinking on your own
- Fair-mindedness: Treating every viewpoint in an unbiased, unprejudiced way
- Insight into egocentricity and sociocentricity: Thinking of the greater good and not just thinking of yourself. Knowing when you are thinking of yourself (egocentricity) and when you are thinking or acting for the greater good (sociocentricity)
- Intellectual humility: Recognizing your intellectual limitations and abilities
- Nonjudgmental: Using professional ethical standards and not basing your judgments on your own personal or moral standards
- Integrity: Being honest and demonstrating strong moral principles
- Perseverance: Persisting in doing something despite it being difficult
- Confidence: Believing in yourself to complete a task or activity
- Interest in exploring thoughts and feelings: Wanting to explore different ways of knowing
- Curiosity: Asking “why” and wanting to know more
Clinical reasoning is defined as, “A complex cognitive process that uses formal and informal thinking strategies to gather and analyze client information, evaluate the significance of this information, and weigh alternative actions.” [2] To make sound judgments about client care, nurses must generate alternatives, weigh them against the evidence, and choose the best course of action. The ability to clinically reason develops over time and is based on knowledge and experience. [3]
Inductive and Deductive Reasoning and Clinical Judgment
Inductive and deductive reasoning are important critical thinking skills. They help the nurse use clinical judgment when implementing the nursing process.
Inductive reasoning involves noticing cues, making generalizations, and creating hypotheses based on specific information or incidents. Cues are data that fall outside of expected findings that give the nurse a hint or indication of a client’s potential problem or condition. The nurse organizes these cues into patterns and creates a generalization. A generalization is a judgment formed from a set of facts, cues, and observations and is similar to gathering pieces of a jigsaw puzzle into patterns until the whole picture becomes more clear. Based on generalizations created from patterns of data, the nurse creates a hypothesis regarding a client problem. A hypothesis is a proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring. If a “why” is identified, then a solution can begin to be explored.
No one can draw conclusions without first noticing cues. Paying close attention to a client, the environment, and interactions with family members is critical for inductive reasoning. As you work to improve your inductive reasoning, begin by first noticing details about the things around you. A nurse is similar to the detective looking for cues in Figure 4.1. [4] Be mindful of your five primary senses: the things that you hear, feel, smell, taste, and see. Nurses need strong inductive reasoning patterns and be able to take action quickly, especially in emergency situations. They can see how certain objects or events form a pattern (i.e., generalization) that indicates a common problem (i.e., hypothesis).
Example: A nurse assesses a client and finds the surgical incision site is red, warm, and tender to the touch. The nurse recognizes these cues form a pattern of signs of infection and creates a hypothesis that the incision has become infected. The provider is notified of the client’s change in condition, and a new prescription is received for an antibiotic. This is an example of the use of inductive reasoning in nursing practice.

Deductive reasoning is another type of critical thinking that is referred to as “top-down thinking.” Deductive reasoning relies on using a general standard or rule to create a strategy. Deductive reasoning relies on a general statement or hypothesis – sometimes called a premise or standard – that is held to be true. The premise is used to reach a specific, logical conclusion. Nurses use standards set by their state’s Nurse Practice Act, federal regulations, the American Nursing Association, professional organizations, and their employer to make decisions about client care and solve problems.
Example: Based on research findings, hospital leaders determine clients recover more quickly if they receive adequate rest. The hospital creates a policy for quiet zones at night by initiating no overhead paging, promoting low-speaking voices by staff, and reducing lighting in the hallways. (See Figure 4.2). [5] The nurse further implements this policy by organizing care for clients that promotes periods of uninterrupted rest at night. This is an example of deductive thinking because the intervention is applied to all clients regardless if they have difficulty sleeping or not.
Clinical judgment is the result of critical thinking and clinical reasoning using inductive and deductive reasoning. Clinical judgment is defined by the National Council of State Boards of Nursing (NCSBN) as, “The observed outcome of critical thinking and decision-making. It uses nursing knowledge to observe and assess presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.” [6] The NCSBN administers the national licensure exam (NCLEX) that evaluates the decision-making ability of nursing graduates and sets a minimum standard for safe, competent nursing care by entry-level licensed nurses. The NCLEX uses the NCSBN Clinical Judgment Measurement Model (NCJMM) to measure clinical judgment.
Evidence-based practice (EBP) is defined by the American Nurses Association (ANA) as, “A lifelong problem-solving approach that integrates the best evidence from well-designed research studies and evidence-based theories; clinical expertise and evidence from assessment of the health care consumer’s history and condition, as well as health care resources; and client, family, group, community, and population preferences and values.” [7]
Nursing Process
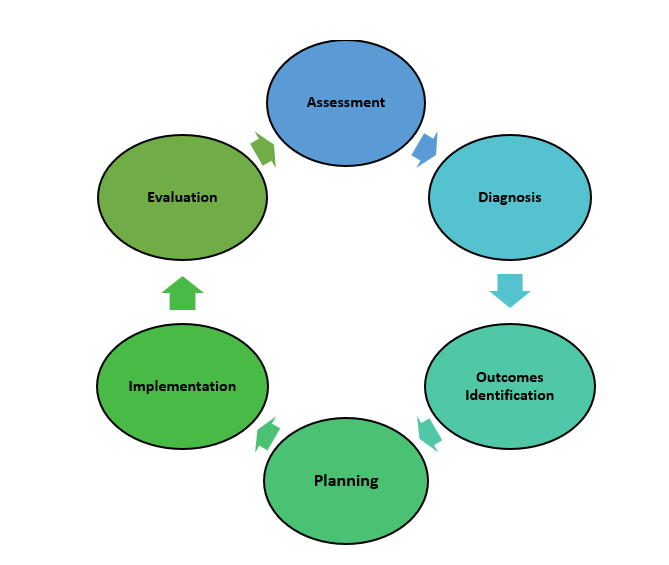
The nursing process is a critical thinking model based on a systematic approach to client-centered care. Nurses use the nursing process to perform clinical reasoning and make clinical judgments when providing client care. The nursing process is based on the Standards of Professional Nursing Practice established by the American Nurses Association (ANA). These standards are authoritative statements of the actions and behaviors that all registered nurses (RNs), regardless of role, population, specialty, and setting, are expected to perform competently. [8] The mnemonic ADOPIE is an easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: A ssessment, D iagnosis, O utcomes Identification, P lanning, I mplementation, and E valuation.
The nursing process is a continuous, cyclical process that is constantly adapting to the client’s current health status. See Figure 4.3a [9] for an illustration of the nursing process.
The ANA’s Standards of Professional Nursing Practice associated with each component of the nursing process are described below.
The “Assessment” Standard of Practice is defined as, “The registered nurse collects pertinent data and information relative to the health care consumer’s health or the situation.” [10] A registered nurse uses a systematic method to collect and analyze client data. Assessment includes physiological data, as well as psychological, sociocultural, spiritual, economic, and lifestyle data. For example, a nurse’s assessment of a hospitalized client in pain includes recognizing cues such as the client’s response to pain, such as the inability to get out of bed, refusal to eat, withdrawal from family members, or anger directed at hospital staff. [11]
Licensed practical/vocational nurses (LPN/VNs) assist with gathering data according to their state’s scope of practice, but do not analyze data because this is outside their scope of practice. The “Assessment” component of the nursing process is further described in the “ Assessment ” section of this chapter.
The “Diagnosis” Standard of Practice is defined as, “The registered nurse analyzes the assessment data to determine actual or potential diagnoses, problems, and issues.” [12] A nursing diagnosis is the nurse’s clinical judgment about the response from the client to actual or potential health conditions or needs. Nursing diagnoses are the bases for the nurse’s care plan and are different than medical diagnoses. [13]
Analyzing assessment data and formulating a nursing diagnosis is outside the scope of practice for LPN/VNs, and as such, they do not assist with this phase of the nursing process. The “Diagnosis” component of the nursing process is further described in the “ Diagnosis ” section of this chapter.
Outcome Identification
The “Outcome Identification” Standard of Practice is defined as, “The registered nurse identifies expected outcomes for a plan individualized to the health care consumer or the situation.” [14] The nurse sets measurable and achievable short- and long-term goals and specific outcomes in collaboration with the client based on their assessment data and nursing diagnoses.
Outcome identification is outside the scope of practice of LPN/VNs, and as such, they do not assist with this phase of the nursing process. The “Outcome Identification” component of the nursing process is further described in the “ Outcome Identification ” section of this chapter.
The “Planning” Standard of Practice is defined as, “The registered nurse develops a collaborative plan encompassing strategies to achieve expected outcomes.” [15] Assessment data, diagnoses, and goals are used to select evidence-based nursing interventions customized to each client’s needs in order to achieve their previously established goals and outcomes. Nursing interventions are planned and documented by RNs in the client’s nursing care plan so that nurses, as well as other health professionals, can refer to it for continuity of care. [16]
The “Planning” component of the nursing process is further described in the “ Planning ” section of this chapter.
Nursing Care Plans
Creating nursing care plans is a part of the “Planning” step of the nursing process. A nursing care plan is a type of documentation that demonstrates the individualized planning and delivery of nursing care for each specific client using the nursing process. RNs create nursing care plans so that the care provided to the client across shifts is consistent among health care personnel. Some interventions can be delegated to LPN/VNs or trained Unlicensed Assistive Personnel (UAPs) with RN supervision.
Creating the nursing care plan is outside the scope of practice, and as such, the LPN/VNs do not perform this task, although they may contribute to it. Developing nursing care plans and implementing appropriate delegation are further discussed under the “ Planning ” and “ Implementation of Interventions ” sections of this chapter.
Implementation
The “Implementation” Standard of Practice is defined as, “The nurse implements the identified plan.” [17] Nursing interventions are implemented or delegated with supervision according to the care plan to assure continuity of care across multiple nurses and health professionals caring for the client. Interventions are documented in the client’s electronic medical record as they are completed. [18] LPN/VNs implement interventions contained in the nursing care plan, provided they are within their scope of practice. The LPN/VN is responsible for documenting the interventions they perform in the client’s medical record.
The “Implementation” Standard of Professional Practice also includes the subcategories “Coordination of Care” and “Health Teaching and Health Promotion” to promote health and a safe environment. [19]
The “Implementation” component of the nursing process is further described in the “ Implementation of Interventions ” section of this chapter.
The “Evaluation” Standard of Practice is defined as, “The registered nurse evaluates progress toward attainment of goals and outcomes.” [20] During evaluation, nurses reassess the client and compare the findings against established outcomes to determine the effectiveness of the interventions and overall nursing care plan. During this phase, RNs ask, “Were outcomes met? Are any modifications required for the nursing care plan?” Both the client’s status and the effectiveness of the nursing care plan are continuously evaluated and modified as needed. [21]
Evaluating and modifying the nursing care plan is outside the scope of practice of LPN/VNs, although they can assist in gathering assessment data to assist the RN in performing this step of the nursing process. The “Evaluation” component of the nursing process is further described in the “ Evaluation ” section of this chapter.
Benefits of Using the Nursing Process
Using the nursing process has many benefits for nurses, clients, and other members of the health care team. The benefits of using the nursing process include the following:
- Promotes quality client care
- Decreases omissions and duplications
- Provides a guide for all staff involved to provide consistent and responsive care
- Encourages collaborative management of a client’s health care problems
- Improves client safety
- Improves client satisfaction
- Identifies a client’s goals and strategies to attain them
- Increases the likelihood of achieving positive client outcomes
- Saves time, energy, and frustration by creating a care plan that is accessible to all staff caring for a client
By using these components of the nursing process as a critical thinking model, nurses plan outcomes and interventions that are customized to the client’s specific needs, ensure the interventions are evidence-based, and evaluate the effectiveness of interventions in meeting the client’s needs.
NCSBN Clinical Judgment Measurement Model
The NCSBN Clinical Judgment Measurement Model (NCJMM) complements the nursing process, but it is a model that assesses an NCLEX candidate’s clinical judgment. Terminology used by this model includes recognize cues, analyze cues, prioritize hypotheses, generate solutions, take action, and evaluate outcomes. See Figure 4.3b [22] and Table 4.2 for comparisons of NCJMM terms and the nursing process. [23] , [24] , [25]
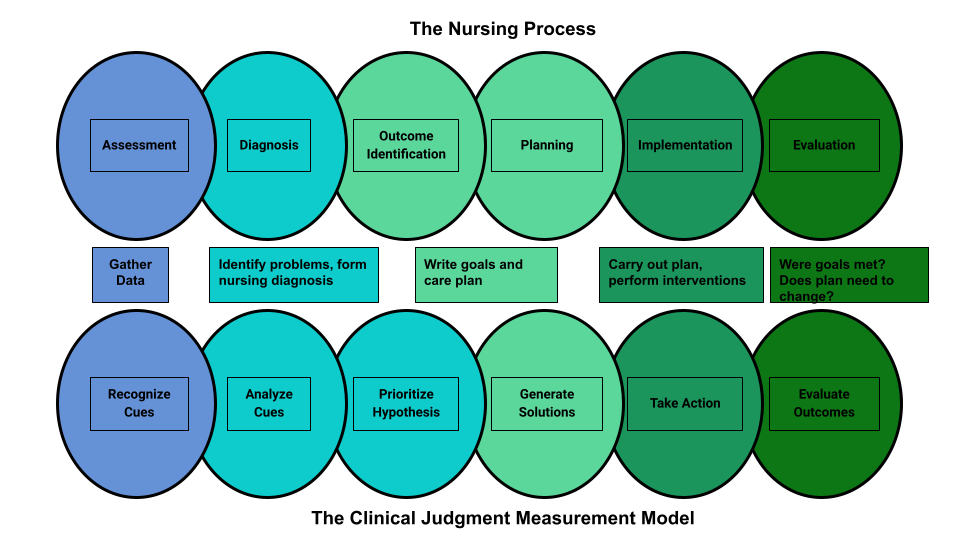
Table 4.2 Comparison of the NCJMM to the Nursing Process
| Determining what client findings are significant, most important, and of immediate concern to the nurse (i.e., identifying “relevant cues”). | ||
| Analyzing data to determine if it is “expected” or “unexpected” or “normal” or “abnormal” for this client at this time according to their age, development, and clinical status. Making a clinical judgment concerning the client’s “human response to health conditions/life processes, or a vulnerability for that response”; also referred to as “forming a hypothesis.” | (Analysis of Data) | |
| Ranking client conditions and problems according to urgency, complexity, and time. | ||
| Planning individualized interventions that meet the desired outcomes for the client; may include gathering additional assessment data. | ||
| Implementing interventions that are safe and most appropriate for the client’s current priority conditions and problems. | ||
| Comparing actual client outcomes with desired client outcomes to determine effectiveness of care and making appropriate revisions to the nursing care plan. |
Learning activities are incorporated throughout this book to help students practice answering NCLEX Next Generation-style test questions.
Review Scenario A in the following box for an example of a nurse using the nursing process and NCJMM skills while providing client care.
Client Scenario A : Using the Nursing Process [26]

A nurse is caring for a hospitalized client with a medical diagnosis of heart failure who has a prescription to receive furosemide 80mg IV every morning. The nurse uses critical thinking according to the nursing process and the NCJMM before administering the prescribed medication:
Assessment/Recognize Cues: During the morning assessment, the nurse notes that the client has a blood pressure of 98/60, heart rate of 100, respirations of 18, and a temperature of 98.7F.
Diagnosis/Analyze Cues: The nurse reviews the medical record for the client’s vital signs baseline and observes the blood pressure trend is around 110/70 and the heart rate in the 80s.
Planning/Prioritize Hypothesis: The nurse recognizes cues (assessment data) that form a pattern related to fluid imbalance and hypothesizes that the client may be dehydrated.
Planning/Generate Solutions: The nurse gathers additional information and notes the client’s weight has decreased four pounds since yesterday. The nurse talks with the client and validates the hypothesis when the client reports that their mouth feels like cotton, and they feel light-headed. By using critical thinking and clinical judgment, the nurse diagnoses the client with the nursing diagnosis Fluid Volume Deficit and plans interventions for reestablishing fluid balance.
Implementation/Take Action: The nurse withholds the administration of IV furosemide and contacts the health care provider to discuss the client’s current fluid status. After contacting the provider, the nurse initiates additional nursing interventions to promote oral intake and closely monitors hydration status.
Evaluation/Evaluate Outcomes: By the end of the shift, the nurse evaluates the client status and determines that fluid balance has been restored.
In Scenario A, the nurse is using clinical judgment and not just “following orders” to administer the Lasix as scheduled. The nurse assesses the client, recognizes and analyzes cues, creates a hypothesis regarding the fluid status, plans and implements nursing interventions, and evaluates outcomes. While performing these steps, the nurse promotes client safety by contacting the provider before administering a medication that could cause harm to the client at this time.
Holistic Nursing Care
Using the nursing process and clinical judgment while implementing evidence-based practices is referred to as the “science of nursing.” Before getting deeper into the science of nursing in the remainder of this chapter, it is important to discuss the “art of nursing” that relies on holistic care provided in a compassionate and caring manner using the nursing process.
The American Nurses Association (ANA) defines nursing as, “Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in the recognition of the connection of all humanity.” [27]
The ANA further describes nursing as a learned profession built on a core body of knowledge that integrates both the art and science of nursing. The art of nursing is defined as, “Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care.” [28]
Nurses care for individuals holistically, including their emotional, spiritual, psychosocial, cultural, and physical needs. They consider problems, issues, and needs that the person experiences as a part of a family and a community as they use the nursing process. Review a scenario illustrating holistic nursing care provided to a client and their family in the following box.
Holistic Nursing Care Scenario
A single mother brings her child to the emergency room for ear pain and a fever. The physician diagnoses the child with an ear infection and prescribes an antibiotic. The mother is advised to make a follow-up appointment with their primary provider in two weeks. While providing discharge teaching, the nurse discovers that the family is unable to afford the expensive antibiotic prescribed and cannot find a primary care provider in their community they can reach by a bus route. The nurse asks a social worker to speak with the mother about affordable health insurance options and available providers in her community and follows up with the prescribing physician to obtain a prescription for a less expensive generic antibiotic. In this manner, the nurse provides holistic care and advocates for improved health for the child and their family.
Caring and the Nursing Process
The American Nurses Association (ANA) states, “The act of caring is foundational to the practice of nursing.” [29] Successful use of the nursing process requires the development of a care relationship with the client. A care relationship is a mutual relationship that requires the development of trust between both parties. This trust is often referred to as the development of rapport and underlies the art of nursing. While establishing a caring relationship, the whole person is assessed, including the individual’s beliefs, values, and attitudes, while also acknowledging the vulnerability and dignity of the client and family. Assessing and caring for the whole person takes into account the physical, mental, emotional, and spiritual aspects of being a human being. [30] Caring interventions can be demonstrated in simple gestures such as active listening, making eye contact, using therapeutic touch, and providing emotional support while respecting their cultural beliefs associated with caring behaviors. [31] See Figure 4.4 [32] for an image of a nurse using touch as a therapeutic communication technique to communicate caring.
Dr. Jean Watson is a nurse theorist who has published many works on the art and science of caring in the nursing profession. Her theory of human caring sought to balance the cure orientation of medicine, giving nursing its unique disciplinary, scientific, and professional standing with itself and the public. Dr. Watson’s caring philosophy encourages nurses to be authentically present with their clients while creating a healing environment. [33]

Now that we have discussed basic concepts related to the nursing process, as well as the science and art of nursing, let’s look more deeply at each component of the nursing process in the following sections.
- Klenke-Borgmann, L., Cantrell, M. A., & Mariani, B. (2020). Nurse educator’s guide to clinical judgment: A review of conceptualization, measurement, and development. Nursing Education Perspectives, 41 (4), 215-221. ↵
- Powers, L., Pagel, J., & Herron, E. (2020). Nurse preceptors and new graduate success. American Nurse Journal, 15 (7), 37-39. ↵
- “ The Detective ” by paurian is licensed under CC BY 2.0 ↵
- “ In the Quiet Zone… ” by C.O.D. Library is licensed under CC BY-NC-SA 2.0 ↵
- NCSBN. (n.d.). NCSBN clinical judgment measurement model . https://www.ncsbn.org/14798.htm ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (4th ed.). American Nurses Association. ↵
- “ The Nursing Process ” by Kim Ernstmeyer at Chippewa Valley Technical College is licensed under CC BY 4.0 ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (n.d.). The nursing process . https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/ ↵
- American Nurses Association. (2021). Nursing: Scope and standards of practice (3rd ed.). American Nurses Association. ↵
- American Nurses Association. (n.d.) The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process / ↵
- American Nurses Association. (n.d.). The nursing process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process / ↵
- “ Nursing Process and NCJMM ” by Tami Davis is licensed under CC BY 4.0 ↵
- NCSBN (n.d.) NCSBN Clinical Judgment Measurement Model. https://www.ncsbn.org/14798.htm ↵
- Ignativicius, V., & Silvestri, L. (2022). Preparing for the Next-Generation NCLEX (NGN): A “how-to” step-by-step faculty resource manual. Elsevier. https://evolve.elsevier.com/education/wp-content/uploads/sites/2/NGN_FacultyGuide_Final.pdf ↵
- “Patient Image in LTC.JPG” by ARISE project is licensed under CC BY 4.0 ↵
- Walivaara, B., Savenstedt, S., & Axelsson, K. (2013). Caring relationships in home-based nursing care - registered nurses’ experiences. The Open Journal of Nursing, 7 , 89-95. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3722540/pdf/TONURSJ-7-89.pdf ↵
- “ hospice-1793998_1280.jpg ” by truthseeker08 is licensed under CC0 ↵
- Watson Caring Science Institute. (n.d.). Watson Caring Science Institute. Jean Watson, PHD, RN, AHN-BC, FAAN, (LL-AAN) . https://www.watsoncaringscience.org/jean-bio/ ↵
Reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow.
A complex cognitive process that uses formal and informal thinking strategies to gather and analyze patient information, evaluate the significance of this information, and weigh alternative actions.
A type of reasoning that involves forming generalizations based on specific incidents.
Subjective or objective data that gives the nurse a hint or indication of a potential problem, process, or disorder.
A judgment formed from a set of facts, cues, and observations.
A proposed explanation for a situation. It attempts to explain the “why” behind the problem that is occurring.
“Top-down thinking” or moving from the general to the specific. Deductive reasoning relies on a general statement or hypothesis—sometimes called a premise or standard—that is held to be true. The premise is used to reach a specific, logical conclusion.
The observed outcome of critical thinking and decision-making. It is an iterative process that uses nursing knowledge to observe and access presenting situations, identify a prioritized client concern, and generate the best possible evidence-based solutions in order to deliver safe client care.
A lifelong problem-solving approach that integrates the best evidence from well-designed research studies, theories, clinical expertise, health care resources, and patient preferences and values.
An easy way to remember the ANA Standards and the nursing process. Each letter refers to the six components of the nursing process: Assessment, Diagnosis, Outcomes Identification, Planning, Implementation, and Evaluation.
Individual, family, or group which includes significant others and populations.
Specific documentation of the planning and delivery of nursing care that is required by the Joint Commission.
Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of individuals, families, groups, communities, and populations in recognition of the connection of all humanity.
Defined as, "Unconditionally accepting the humanity of others, respecting their need for dignity and worth, while providing compassionate, comforting care."
A relationship described as one in which the whole person is assessed while balancing the vulnerability and dignity of the patient and family.
Developing a relationship of mutual trust and understanding.
Nursing Fundamentals 2e Copyright © by Open Resources for Nursing (Open RN) is licensed under a Creative Commons Attribution 4.0 International License , except where otherwise noted.
- Call to +1 844 889-9952
Henderson’s Nursing Theory: The Summary of 14 Basic Needs and Practical Application
| 📄 Words: | 935 |
|---|---|
| 📝 Subject: | |
| 📑 Pages: | 5 |
| 📚 Topics: |
- Introduction: Virginia Henderson Theory
Henderson’s 14 Basic Needs
Henderson’s nursing need theory: origins, henderson’s nursing theory: practical applications, henderson’s theory of nursing: the use in research, conclusion: evaluation of virginia henderson’s theory, video voice-over, introduction: virginia henderson’s theory.
Proposed by Virginia Henderson, the Nursing Need Theory is one of the most crucial theories since it laid the foundation for other nursing care approaches in the 20th century. Henderson’s nursing theory focuses on the nursing staff’s attention to the physiological, psychological, and social needs met through nursing care. One of the prerequisites and assumptions of this model is the patient’s participation in the planning and implementation of care. Henderson’s theory of nursing also posits that there are 14 basic needs that are the same for all people and are based on the model of A. Maslow (Henderson’s nursing need theory,” n.d.). According to this model’s assumption, a healthy person does not have difficulty meeting these needs. This paper will explore Virginia Henderson’s theory, its origins, and its 14 basic needs. It will also explain how Henderson’s nursing need theory is used in practice and research and discuss its strengths and limitations.
The needs in the Nursing Need Theory are the essential daily activities every person has to perform to support their lives. According to this model, nurses should assist patients in performing these activities if they cannot do them themselves. Henderson’s 14 basic needs include the following:
- Normal breathing.
- Drinking and eating enough food.
- Isolation of waste products from the body.
- Maintaining the necessary body position and movement.
- Sleep and rest.
- Selecting clothes, dressing, and undressing.
- Maintain body temperature by choosing clothes and modifying the environment.
- Cleaning the body and grooming.
- Avoiding dangers and avoiding injuring others.
- Communicating with others.
- Worshipping according to one’s faith.
- Working to get a sense of accomplishment.
- Participating in recreational activities.
- Learning and satisfying curiosity.
The four main concepts addressed by Henderson are the individual, the environment, health, and nursing (Henderson’s nursing need theory,” n.d.). All the concepts are dependent on one another and have a direct relationship with each other. One Virginia Henderson’s Nursing Need theory example is as follows: when individuals lack food or sleep, their health state might deteriorate substantially. The entire nursing process by Henderson is aimed at restoring the patient’s independence.
Until the beginning of the 20th century, the concept of “professional nurse” did not exist. At best, some nurses were hired as servants in affluent homes to care for the dying (Alligood, 2014). Nurses at this time had to dress the wounded and take care of them in local hospitals. Before Henderson’s theory, it was common to focus nursing care for the patient, depending on the stated diagnosis. In 1937, Henderson became a member of the team of authors who created a new nursing training program with a patient-centered approach focused on patient care problems, not on their diagnosis.
Henderson used Abraham Maslow’s hierarchy of needs to define and characterize some of the needs of individuals in the Nursing Need Theory. Virginia was one of the most famous nurses of the twentieth century, and the urgency to specialize the nursing theory came to Virginia from the professional society. The International Council of Nurses in 1958 asked her to define the term “nursing” (Gonzalo, 2019). Thus, Henderson’s theoretical approach was based on her practice, education, and existing definitions of Florence Nightingale, who began conceptualizing the nursing definition.
Henderson’s nursing needs theory is useful in practice and many nursing disciplines with different practice directions. The approach is practical because it is based on individuals’ core needs and assumptions of the necessity to be healthy and care for patients from the nurses’ side (Gonzalo, 2019). The application of this theory in practice can be adaptable and flexible and allows professionals to reflect on their nursing competency when helping a patient maintain health and independence.
Henderson’s concept of utilizing the best practice approaches, including evidence-based research and advanced practice knowledge, can be seen as a foundation for any nursing process (Masters, 2015). It is assumed that patient-focused care based on an individual’s needs will help a person recover and maintain a decent health state. Nevertheless, the predicting outcomes cannot be fully drawn from Henderson’s theory that focuses on specific patient’s needs.
The example where this theory could be used is a situation when a patient is being treated in the therapeutic department, and his sleep has been disturbed for three days. The nurse should find out the cause of a sleep disorder and, with the patient, establish activities that would allow a patient to achieve as much independence as possible and pursue actions that would be the most appropriate, such as relaxation exercises or airing the room before going to bed.
The nursing need theory was tested by various researchers, generating different studies. There are numerous researches based on the approach with quantitative and qualitative study methods (Huitzi-Egilegor et al., 2014). One example of the recent research done using the theory was made by Ahtisham et al. (2015) when analysts aimed to develop the nursing theory application into clinical settings to deliver nursing care. The propositions of authors include statements, such as “one of the most contentious and enduring problems in nursing is the poor clinical observation,” “Henderson used the concepts of fundamental human needs, bio physiology…which give the theory a dynamic coverage regarding patients need” (Ahtisham et al., 2015, p. 449).
The theory is comprehensive and quite specific concerning primary needs that a patient has regarding illnesses. However, one can state that the theory tends to be more general than specific as it generalizes different patients and their needs without considering the particular care setting. The strengths of the theory are its broad application to all individuals of all ages, good interrelation of the main concepts, and the ability to add other ideas based on the discussed model. The models’ weaknesses are the lack of conceptual relationship between physiological and other human characteristics, exclusion of the holistic nature of an individual, and lack of an interconnection diagram that connects all needs.
I would use the nursing need theory in the advanced practice to base the approach on the individual’s needs and empathetically establish necessary activities with the patient. However, the advanced practice might require more recent models and theories that would reflect the patient’s behavior and positive outcomes that should be achieved. Nevertheless, Virginia Henderson’s approach is one of the first attempts to describe nursing as an independent profession. She offered a framework for working with the patient that later models of care used.
Ahtisham, Y & Sommer. J. (2015). Case study integrating nursing theory and process into practice; Virginia’s Henderson Need Theory. International Journal of Caring Sciences, 8 (2), 443-450. Web.
Alligood, M. (2014). Nursing theorists and their work (8 th ed.). Elsevier.
Gonzalo, A. (2019). Virginia Henderson: Nursing need theory. Nurses Labs. Web.
Henderson’s nursing need theory. (n.d.). Nursing Theory. Web.
Huitzi-Egilegor, J. X., Elorza-Puyadena, M. I., Urkia-Etxabe, J. M., & Asurabarrena-Iraola, C. (2014). Implementation of the nursing process in a health area: models and assessment structures used. Revista latino-americana de enfermagem, 22 (5), 772–777. Web.
Masters, K. (2015). Models and theories focused on nursing goals and functions. In J. B. Butts, & K. L. Rich (Eds.), Philosophies and theories for advanced nursing practice (2nd ed., pp. 377-407). Burlington, MA: Jones & Bartlett Learning.
Cite this paper
Select style
- Chicago (A-D)
- Chicago (N-B)
NursingBird. (2024, January 26). Henderson’s Nursing Theory: The Summary of 14 Basic Needs and Practical Application. https://nursingbird.com/the-nursing-need-theory-meaning-and-origins/
"Henderson’s Nursing Theory: The Summary of 14 Basic Needs and Practical Application." NursingBird , 26 Jan. 2024, nursingbird.com/the-nursing-need-theory-meaning-and-origins/.
NursingBird . (2024) 'Henderson’s Nursing Theory: The Summary of 14 Basic Needs and Practical Application'. 26 January.
NursingBird . 2024. "Henderson’s Nursing Theory: The Summary of 14 Basic Needs and Practical Application." January 26, 2024. https://nursingbird.com/the-nursing-need-theory-meaning-and-origins/.
1. NursingBird . "Henderson’s Nursing Theory: The Summary of 14 Basic Needs and Practical Application." January 26, 2024. https://nursingbird.com/the-nursing-need-theory-meaning-and-origins/.
Bibliography
NursingBird . "Henderson’s Nursing Theory: The Summary of 14 Basic Needs and Practical Application." January 26, 2024. https://nursingbird.com/the-nursing-need-theory-meaning-and-origins/.
- Personal Nursing Philosophy and Metaparadigms
- A Common Clinical Problem Is Pressure Ulcers
- Effective Care of Exit Sites for Peritoneal Dialysis Catheters
- PIC0 for Pressure Ulcers Literature Review
- Evidence-Based Practice Beliefs and Implementation. Article Critique
- Issue of Stress in Nursing Practice
- Limitations and Solutions Related to Diseases
- Healthcare Policy: Impact of Health Legislation on Nursing
- The Implementation of a New Staffing Matrix in Hospital
- Master’s Education for American Nurses
The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Effective decision-making: applying the theories to nursing practice.
Samantha Watkins
Emergency Department Staff Nurse, Frimley Health NHS Foundation Trust, Frimley
View articles · Email Samantha
Many theories have been proposed for the decision-making conducted by nurses across all practices and disciplines. These theories are fundamental to consider when reflecting on our decision-making processes to inform future practice. In this article three of these theories are juxtaposed with a case study of a patient presenting with an ST-segment elevation myocardial infarction (STEMI). These theories are descriptive, normative and prescriptive, and will be used to analyse and interpret the process of decision-making within the context of patient assessment.
Decision-making is a fundamental concept of nursing practice that conforms to a systematic trajectory involving the assessment, interpretation, evaluation and management of patient-specific situations ( Dougherty et al, 2015 ). Shared decision-making is vital to consider in terms of patient autonomy and professional duty of care as set out in the Nursing and Midwifery Council (NMC) (2018) Code, which underpins nursing practice. Consequently, the following assessment and decision-making processes were conducted within the remits of practice as a student nurse. Decision-making is a dynamic process in nursing practice, and the theories emphasise the importance of adaptability and reflective practice to identify factors that impact on patient care ( Pearson, 2013 ). Three decision-making theories will be explored within the context of a decision made in practice. To abide by confidentiality requirements, the pseudonym ‘Linda’ will be used throughout. Patient consent was obtained prior to writing.
Linda was a 71-year-old who had been admitted to the cardiac ward following an episode of unstable angina. She was on continuous cardiac monitoring as recommended by the National Institute for Health and Care Excellence (NICE) (2016) guideline for chest pain of recent onset. During her stay on the ward, the tracing on the cardiac monitor indicated possible ST-segment elevation ( Thygesen et al, 2018 ). It was initially hypothesised that she might be experiencing an ACS ( Box 1 ) and could be haemodynamically unstable.
Box 1. Acute coronary syndrome
- Acute coronary syndrome is an umbrella term that includes three cardiac conditions that result from a reduction of oxygenated blood through the coronary arteries, causing myocardial ischaemia. An ST-segment elevation myocardial infarction (STEMI) connotes the complete occlusion of one or more of the coronary arteries, which is demonstrated by patient symptoms and ST-segment elevation seen on an electrocardiogram (ECG)
- A non-ST-segment elevation myocardial infarction (NSTEMI) results from a partial occlusion of a coronary artery. Patient symptoms often present alongside dynamic ST-segment depression, T-wave inversion or a normal ECG
- Unstable angina is a result of a transient occlusion of the coronary arteries causing symptoms at rest or on minimal exertion, which may be eased/resolved with rest with or without glyceryl trinitrate (GTN)
- Signs and symptoms of ischaemia experienced by patient include: chest pain with or without radiation to jaw, neck, back, shoulders or arms, which is described as squeezing or crushing. Associated symptoms of lethargy, syncope, pre-syncopal episodes, diaphoresis, dyspnoea, nausea or vomiting, anxiety or a feeling of impending doom often also prevail
Source: Deen, 2018
The possibility that Linda was experiencing ST-segment elevation myocardial infarction (STEMI) meant that she needed rapid assessment of her condition. Stephens (2019) recommended the use of the ABCDE assessment as a timely and effective tool to identify physiological deterioration in patients with chest pain. The student nurse's ABCDE assessment of Linda is shown in Box 2 .
Box 2. ABCDE assessment * of ‘Linda’
- Airway: patent, no audible sounds of obstruction; however, unable to speak in full sentences due to dyspnoea
- Breathing: dyspnoeic, respiratory rate of 27, saturations of 85% on room air—with guidance from the senior charge nurse, 80% oxygen via non-rebreathe mask was administered ( O'Driscoll et al, 2017 )
- Circulation: tachycardia of 112 beats per minute, hypotensive at 92/50 mmHg, oliguric, diaphoretic, and with cool peripherals and a thready radial pulse
- Disability: She was alert on the AVPU scale, but anxious and feeling lethargic. Blood glucose was 5.7 mmol/litre
- Exposure: no erythema or wounds noted. She stated she had central chest pain, which was radiating to her jaw and back, described as ‘pressure’, and rated as a seven out of ten
* in line with Resuscitation Council (2015)
NICE (2016) recommends that the first investigation for patients with chest pain is to conduct an ECG as a rapid and non-invasive assessment for a cardiac cause of the pain. This was carried out and 2 mm ST-segment elevation in the precordial leads V1-V3 was noted, indicating a possible anterior STEMI ( Amsterdam et al, 2014 ). The student nurse had had basic ECG interpretation training as part of the nursing degree undertaken, but had also received informal teaching from registered nursing staff in cardiology. The ECG findings were confirmed by the senior charge nurse after they were alerted to Linda's condition, symptoms, and National Early Warning Score 2 (NEWS 2) ( Royal College of Physicians, 2017 ). The senior charge nurse escalated her care to the cardiology team. A diagnosis of STEMI was made by the cardiology team using the ECG findings and her physiological signs of deterioration from their assessment, within the context of her initial presentation to hospital for unstable angina. This diagnosis, coupled with the deterioration in her condition, meant that she required primary percutaneous coronary intervention (PCI). The NICE (2014) quality standard for acute coronary syndromes and the clinical guideline on STEMI ( NICE, 2013a ) recommend that primary PCI is initiated within 120 minutes to reperfuse the myocardium and prevent further myocardial cellular necrosis. This improves long-term patient outcomes ( Thygesen et al, 2018 ).
Decision-making theories
The recognition of an evolving STEMI on the cardiac monitor corresponds with the model of hypothetico-deductive reasoning ( Pearson, 2013 ) within the descriptive and normative theories ( Box 3 ). Thompson and Dowding (2009) highlighted that this model recognises that decision-making comprises four stages, beginning with cue acquisition. The specific pre-counter cues can be identified as the recognition of the abnormal tracing on the cardiac monitor ( Pearson, 2013 ), suggestive of ST-segment elevation, that indicated Linda might be experiencing haemodynamic deterioration with a cardiac cause. Subsequently, the decision to assess Linda formed the hypothesis generation phase of the decision and the recognition of the clinical signs as indicating STEMI ( Nickerson, 1998 ; Johansen and O'Brien, 2016 ). This hypothesis focused the assessment to identify and examine pertinent factors that supported this conjecture ( Pearson, 2013 ). However, the student nurse required more data to formulate a robust hypothesis thereby initiating the cue interpretation phase by conducting an ABCDE systematic assessment, including ECG. Lindsey (2013) argued that during cue interpretation, the health professional uses prescriptive guidelines to direct the assessment process and provide a rationale.
Box 3. Decision-making theories considered
- Descriptive theory: is concerned with each individuals’ moral beliefs regarding a particular decision
- Normative theory: connotes what decisions individuals should make logically
- Prescriptive theory: encompasses the policies that govern the remits of a decision within the evidence base that informs practice
Source: Pearson, 2013
Arguably, however, clinical knowledge of the pathophysiology of ACS is fundamental to effective cue interpretation, not simply the individual's knowledge of the NICE guidance ( NICE, 2013a ; 2013b ; 2014 ; 2016 ). The student nurse's existing knowledge of the symptoms of ACS supported the cue interpretation with assessing Linda's condition and possible diagnosis of ACS. This knowledge enriched the student nurse's understanding of the guidance, which could then effectively be applied as the central aspect of cue interpretation ( Deen, 2018 ).
Elstein and Schwartz (2002) conceded that the prescriptive theory knowledge synthesised for the decision must be accurate and evidence-based for hypothetico-deductive reasoning to be effective. Courtney and McCutcheon (2009) argued that reliance solely on clinical guidelines can limit decision-making and result in erroneous outcomes and should consequently be used in collaboration with the evidence base. By combining normative theory with prescriptive guidance, clinical decisions can be enriched and validated. Stevens (2013) highlighted that it is vital that the guidance used in corroboration with decision-making models is valid and reliable and therefore prescriptive theory must be critically evaluated against the evidence-base. The guidance published by NICE (2013a) is supported by the American College of Cardiology ( O'Gara et al, 2013 ), European Resuscitation Council ( Nikolaou et al, 2015 ), European Society of Cardiology ( Steg et al, 2012 ) and Cardiac Society of Australia and New Zealand ( Chew et al, 2016 ). Accordingly, these guidelines highlight the clinical signs of STEMI and the diagnostic investigations pertinent to this condition. Within the remits of practice as a student nurse, this evidence supported the decision to escalate Linda's condition.
Antithetically, during cue interpretation and the hypothesis generation phases, Pearson (2013) emphasised the importance of considering multiple hypotheses extrapolated from the clinical data, resulting in the selection of the most appropriate hypothesis when more data are obtained. Despite this, during the interpretation of the cues for the hypothesis, the student nurse failed to consider differential diagnoses, such as pneumothorax or pulmonary embolism, which have similar presentations to STEMI ( Deen, 2018 ). Consequently, this hypothesis generation had an element of uncertainty ( Bjørk and Hamilton, 2011 ), which could have impeded Linda's care by erroneously considering only one potential diagnosis and therefore focusing the assessment on that diagnosis. Student nurses can be considered ‘novice’ health professionals, demonstrating limitations in knowledge regarding differential diagnoses and therefore in potential hypotheses. Pearson (2013) argued that this is because student nurses lack the requisite experience to cluster information as effectively as an ‘expert’ health professional. Consequently, the presentation of one hypothesis is permissible within the remits of practice as a student nurse.
Assessment tools such as ABCDE ( Resuscitation Council UK, 2015 ) ensure that all factors indicative of deterioration are recognised. Consequently, by using a systematic assessment, any potential erroneous hypothesis can be precluded. Therefore, as Carayon and Wood (2010) state, the assessment tool was a barrier to active failure to recognise alternative diagnoses thus circumventing any serious consequences, highlighting the importance of comprehensive assessment to avoid error and safeguard the ethical principle of non-maleficence ( Beauchamp and Childress, 2013 ) fundamental to nursing. Antithetically, Benner et al (2008) argued that even the novice nurse should be able to consider multiple hypotheses within a situation, although they may not be able to reflect on these decisions within the moment. However, as Keller (2009) noted, the hypothetico-deductive model is based on presuppositions recognised by the health professional, such as the evolving cardiac tracing and history of pain, indicating that STEMI was the higher probable cause ( Deen, 2018 ). Consequently, a limitation of hypothetico-deductive reasoning is sufficient experience to aid in generating hypotheses.
Thereafter, in the hypothesis generation phase, the decision-making process evolved to include elements of pattern recognition theory ( Croskerry, 2002 ). The clinical decision that focuses on a single hypothesis can be compared to the use of pattern recognition ( Pearson, 2013 ) where existing knowledge is used to establish the hypothesis. Pearson (2013) commented that hypothetico-deductive reasoning is based on the synthesising and analysing of information whereas the formulation of one hypothesis is suggestive of pattern recognition, where the nurse uses previous experience to evaluate the situation. Consequently, the student nurse's previous experience of assessing a patient in acute STEMI may have guided practice to recognise ST-segment elevation on the telemetry, and then subsequently to conduct an ECG, and to recognise the associated clinical signs of STEMI and to gather a history of the pain using NICE (2013b) guidance on unstable angina, in line with Linda's initial presentation. Croskerry (2002) identified that health professionals who rely on pattern recognition initially recognise visual cues that are then supplemented with more in-depth data, often using assessment tools such as NEWS (and now NEWS 2) and ABCDE. Arguably, the recognition of similarities in clinical presentation, past medical history, and cardiac monitoring tracing of Linda's case to the previous case and use of ABCDE and NEWS 2 to further assess her condition and extrapolate data, identifies that previous experience can facilitate decision-making outcomes.
Finally, in the last phase of the decision-making in the hypothetico-deductive model, the student nurse evaluated the hypothesis and by using the merits from the cues ( Banning, 2008 ) established that STEMI was the most probable cause of Linda's deterioration and could escalate her care appropriately using the prescriptive theory tools described above.
Arguably, by using previous experience to guide practice, an element of confirmation bias may have affected the selection of data ( Thompson and Dowding, 2009 ) and consequently the student may have neglected other important data ( Croskerry, 2003 ). For instance, student nurses are inexperienced with chest auscultation and consequently could not have ruled out differential respiratory diagnoses. Stanovich et al (2013) acknowledged that confirmation bias can be circumvented when evidence is assimilated with hypothesis generation. The consideration that Linda may have been at an increased risk of myocardial infarction due to her age, history of smoking and admission to hospital for unstable angina ( Piepoli et al, 2016 ), indicated that the cause of her deterioration would most likely be cardiac. Thus, an evidence-based approach could inform practice and consequently, any limitations as a ‘novice’ would be minimised through rationalisation and critical thinking. Indeed, Stanovich et al (2013) argued that rationalising and critical thinking are markedly more important than existing knowledge. This is because even an ‘expert’ in a specific field does not have completely comprehensive knowledge, and therefore relies on a critical thought process to make rational decisions.
Conclusively, health professionals must be able to rationalise their decisions ( Johansen and O'Brien, 2016 ) and justify these decisions within the context of each presentation as a central concept of nursing ( NMC, 2018 ).
Communication is vital to establishing consent to treatment where the patient is regarded as having capacity under the Mental Capacity Act 2005. This is particularly significant when conducting investigations and escalating care to ensure that the patient's wishes are respected, and that the patient is empowered with knowledge regarding their condition and care ( Coultier and Collins, 2011 ). Linda was informed that her care required escalation to the appropriate clinical team, and then subsequently recommended to have PCI intervention as the most effective treatment for STEMI ( NICE, 2013a ; 2014 ). Presenting a default decision and using choice architecture can be construed as methods of liberal paternalism used to avoid impeded decision-making from choice overload ( Rosenbaum, 2015 ) or irrational decision bias ( Marewski and Gigerenzer, 2012 ). To escalate Linda's care within the recommended timeframe ( NICE, 2013a ; 2014 ), it was important to use elements of liberal paternalism ( Beauchamp and Childress, 2013 ) while preserving Linda's autonomy of choice ( Kemmerer et al, 2017 ). Linda had a right to make a decision against medical advice as per Re B (Adult, refusal of medical treatment) [2002] and these choices were presented to her by the cardiology team. As a health professional, a duty of care was owed to the patient to escalate concerns regarding her condition under the Code ( NMC, 2018 ).
Conclusively, all three theories of decision-making pertained to this patient's effective care. Nurses must be accountable for their decisions and act within the remits of the NMC (2018) Code. Patient care must consequently be effective, evidence-based and patient-centred. Accountability requires the health professional to act within the remits of their role to ensure safe care is delivered to the patient. This is a fundamental aspect of patient-centric care and principal to effective decision making. Demonstrably, the use of descriptive and normative theories can be interchangeable, however, the use of prescriptive theory is pivotal to validate clinical decision-making. The decision-making process can be further facilitated by use of structured assessment tools to reduce margin of error and improve outcome. Collaborative decision making is pivotal to advancing patient autonomy and empowerment but certain decisions require elements of paternalism to improve the process and uphold the ethical principles of beneficence and non-maleficence. Nevertheless, health professionals have a duty of care to adhere to decisions made by patients established to have capacity to give informed consent, irrespective of the personal beliefs of the professional.
- This article is a reflection on a case scenario where decisions were made in the care of a patient admitted for cardiac monitoring
- Nursing decision making is complex and involves a multitude of processes based on experience, knowledge and skill.
- Understanding the importance of decision-making theory and how these theories apply to practice can be effective in reflecting on practice, and the application of theory to practice can inform patient care
CPD reflective questions
- Consider the three different theories of decision making outlined here—which theory do you deem the most important to your practice? How does this affect your practice?
- Consider how reflecting on your own decision making can improve practice
- What can you do to enrich your own knowledge regarding patients with chest pain?

- History & Society
- Science & Tech
- Biographies
- Animals & Nature
- Geography & Travel
- Arts & Culture
- Games & Quizzes
- On This Day
- One Good Fact
- New Articles
- Lifestyles & Social Issues
- Philosophy & Religion
- Politics, Law & Government
- World History
- Health & Medicine
- Browse Biographies
- Birds, Reptiles & Other Vertebrates
- Bugs, Mollusks & Other Invertebrates
- Environment
- Fossils & Geologic Time
- Entertainment & Pop Culture
- Sports & Recreation
- Visual Arts
- Demystified
- Image Galleries
- Infographics
- Top Questions
- Britannica Kids
- Saving Earth
- Space Next 50
- Student Center
- Introduction
History of nursing
- Scope of nursing practice
- Education for nursing practice
- Hospital-based nursing practice
- Community health nursing practice
- Mental health nursing practice
- The care of children
- The care of women
- Geriatric nursing practice
- Nurse practitioners
- Clinical nursing specialists
- Nurse midwives
- Nurse anesthetists
- National organizations
- International organizations

Our editors will review what you’ve submitted and determine whether to revise the article.
- American Nurses Association - What Is Nursing?
- British Medical Journal - How the nursing profession should adapt for a digital future
- International Council of Nurses - Nursing definitions
- University of Pennsylvania - Penn Nursing - American Nursing: An Introduction to the Past
- National Center for Biotechnology Information - Nursing Practice
- nursing - Children's Encyclopedia (Ages 8-11)
- nursing - Student Encyclopedia (Ages 11 and up)
- Table Of Contents

Recent News
nursing , profession that assumes responsibility for the continuous care of the sick, the injured, the disabled, and the dying. Nursing is also responsible for encouraging the health of individuals, families, and communities in medical and community settings. Nurses are actively involved in health care research, management, policy deliberations, and patient advocacy . Nurses with postbaccalaureate preparation assume independent responsibility for providing primary health care and specialty services to individuals, families, and communities.
Professional nurses work both independently and in collaboration with other health care professionals such as physicians. Professional nurses supervise the work of nurses who have limited licenses, such as licensed practical nurses (LPNs) in the United States and enrolled nurses (ENs) in Australia. Professional nurses also oversee the work of nursing assistants in various settings.
Nursing is the largest, the most diverse , and one of the most respected of all the health care professions. There are more than 2.9 million registered nurses in the United States alone, and many more millions worldwide. While true demographic representation remains an elusive goal, nursing does have a higher proportional representation of racial and ethnic minorities than other health care professions. In some countries, however, men still remain significantly underrepresented.
The demand for nursing remains high, and projections suggest that such demand will substantively increase. Advances in health care technology, rising expectations of people seeking care, and reorganization of health care systems require a greater number of highly educated professionals. Demographic changes, such as large aging populations in many countries of the world, also fuel this demand.
Although the origins of nursing predate the mid-19th century, the history of professional nursing traditionally begins with Florence Nightingale . Nightingale, the well-educated daughter of wealthy British parents, defied social conventions and decided to become a nurse. The nursing of strangers, either in hospitals or in their homes, was not then seen as a respectable career for well-bred ladies, who, if they wished to nurse, were expected to do so only for sick family and intimate friends. In a radical departure from these views, Nightingale believed that well-educated women, using scientific principles and informed education about healthy lifestyles, could dramatically improve the care of sick patients. Moreover, she believed that nursing provided an ideal independent calling full of intellectual and social freedom for women, who at that time had few other career options.

In 1854 Nightingale had the opportunity to test her beliefs during Britain’s Crimean War . Newspaper stories reporting that sick and wounded Russian soldiers nursed by religious orders fared much better than British soldiers inflamed public opinion . In response, the British government asked Nightingale to take a small group of nurses to the military hospital at Scutari (modern-day Üsküdar, Turk.). Within days of their arrival, Nightingale and her nurses had reorganized the barracks hospital in accordance with 19th-century science: walls were scrubbed for sanitation, windows opened for ventilation, nourishing food prepared and served, and medications and treatments efficiently administered. Within weeks death rates plummeted, and soldiers were no longer sickened by infectious diseases arising from poor sanitary conditions. Within months a grateful public knew of the work of the “Lady with the Lamp,” who made nightly rounds comforting the sick and wounded. By the end of the 19th century, the entire Western world shared Nightingale’s belief in the worth of educated nurses.

Nightingale’s achievements overshadowed other ways to nurse the sick. For centuries, most nursing of the sick had taken place at home and had been the responsibility of families, friends, and respected community members with reputations as effective healers. During epidemics , such as cholera , typhus , and smallpox , men took on active nursing roles. For example, Stephen Girard , a wealthy French-born banker, won the hearts of citizens of his adopted city of Philadelphia for his courageous and compassionate nursing of the victims of the 1793 yellow fever epidemic .
As urbanization and industrialization spread, those without families to care for them found themselves in hospitals where the quality of nursing care varied enormously. Some patients received excellent care. Women from religious nursing orders were particularly known for the quality of the nursing care they provided in the hospitals they established. Other hospitals depended on recovering patients or hired men and women for the nursing care of patients. Sometimes this care was excellent; other times it was deplorable, and the unreliability of hospital-based nursing care became a particular problem by the late 19th century, when changes in medical practices and treatments required competent nurses. The convergence of hospitals’ needs, physicians’ wishes, and women’s desire for meaningful work led to a new health care professional: the trained nurse.
Hospitals established their own training schools for nurses. In exchange for lectures and clinical instructions, students provided the hospital with two or three years of skilled free nursing care. This hospital-based educational model had significant long-term implications . It bound the education of nurses to hospitals rather than colleges, a tie that was not definitively broken until the latter half of the 20th century. The hospital-based training model also reinforced segregation in society and in the health care system. For instance, African American student nurses were barred from almost all American hospitals and training schools. They could seek training only in schools established by African American hospitals. Most of all, the hospital-based training model strengthened the cultural stereotyping of nursing as women’s work. Only a few hospitals provided training to maintain men’s traditional roles within nursing.
Still, nurses transformed hospitals. In addition to the skilled, compassionate care they gave to patients, they established an orderly, routine, and systemized environment within which patients healed. They administered increasingly complicated treatments and medication regimes. They maintained the aseptic and infection-control protocols that allowed more complex and invasive surgeries to proceed. In addition, they experimented with different models of nursing interventions that humanized increasingly technical and impersonal medical procedures.

Outside hospitals, trained nurses quickly became critical in the fight against infectious diseases . In the early 20th century, the newly discovered “ germ theory ” of disease (the knowledge that many illnesses were caused by bacteria ) caused considerable alarm in countries around the world. Teaching methods of preventing the spread of diseases, such as tuberculosis , pneumonia , and influenza , became the domain of the visiting nurses in the United States and the district nurses in the United Kingdom and Europe. These nurses cared for infected patients in the patients’ homes and taught families and communities the measures necessary to prevent spreading the infection. They were particularly committed to working with poor and immigrant communities, which often had little access to other health care services. The work of these nurses contributed to a dramatic decline in the mortality and morbidity rates from infectious diseases for children and adults.
At the same time, independent contractors called private-duty nurses cared for sick individuals in their homes. These nurses performed important clinical work and supported families who had the financial resources to afford care, but the unregulated health care labour market left them vulnerable to competition from both untrained nurses and each year’s class of newly graduated trained nurses. Very soon, the supply of private-duty nurses was greater than the demand from families. At the turn of the 20th century, nurses in industrialized countries began to establish professional associations to set standards that differentiated the work of trained nurses from both assistive-nursing personnel and untrained nurses. More important, they successfully sought licensing protection for the practice of registered nursing. Later on, nurses in some countries turned to collective bargaining and labour organizations to assist them in asserting their and their patients’ rights to improve conditions and make quality nursing care possible.
By the mid-1930s the increasing technological and clinical demands of patient care, the escalating needs of patients for intensive nursing, and the resulting movement of such care out of homes and into hospitals demanded hospital staffs of trained rather than student nurses. By the mid-1950s hospitals were the largest single employer of registered nurses. This trend continues, although as changes in health care systems have reemphasized care at home, a proportionately greater number of nurses work in outpatient clinics, home care , public health , and other community-based health care organizations.

Other important changes in nursing occurred during the latter half of the 20th century. The profession grew more diverse. For example, in the United States, the National Organization of Coloured Graduate Nurses (NOCGN) capitalized on the acute shortage of nurses during World War II and successfully pushed for the desegregation of both the military nursing corps and the nursing associations. The American Nurses Association (ANA) desegregated in 1949, one of the first national professional associations to do so. As a result, in 1951, feeling its goals fulfilled, the NOCGN dissolved. But by the late 1960s some African American nurses felt that the ANA had neither the time nor the resources to adequately address all their concerns. The National Black Nurses Association (NBNA) formed in 1971 as a parallel organization to the ANA.
Nursing’s educational structure also changed. Dependence on hospital-based training schools declined, and those schools were replaced with collegiate programs either in community or technical colleges or in universities. In addition, more systematic and widespread programs of graduate education began to emerge. These programs prepare nurses not only for roles in management and education but also for roles as clinical specialists and nurse practitioners. Nurses no longer had to seek doctoral degrees in fields other than nursing. By the 1970s nurses were establishing their own doctoral programs, emphasizing the nursing knowledge and science and research needed to address pressing nursing care and care-delivery issues.
During the second half of the 20th century, nurses responded to rising numbers of sick patients with innovative reorganizations of their patterns of care. For example, critical care units in hospitals began when nurses started grouping their most critically ill patients together to provide more effective use of modern technology. In addition, experiments with models of progressive patient care and primary nursing reemphasized the responsibility of one nurse for one patient in spite of the often-overwhelming bureaucratic demands by hospitals on nurses’ time.
The nursing profession also has been strengthened by its increasing emphasis on national and international work in developing countries and by its advocacy of healthy and safe environments . The international scope of nursing is supported by the World Health Organization (WHO), which recognizes nursing as the backbone of most health care systems around the world.
Scope of Practice
Scope of practice describes the services that a qualified health professional is deemed competent to perform, and permitted to undertake – in keeping with the terms of their professional license.
Scope of practice defined in nursing
The Nursing Scope and Standards of Practice describe the “who,” “what,” “where,” “when,” “why,” and “how” of nursing practice:
- Who: Registered Nurses (RN) and Advanced Practice Registered Nurses (APRN) comprise the “who” constituency and have been educated, titled, and maintain active licensure to practice nursing.
- What: Nursing is the protection, promotion, and optimization of health and abilities; prevention of illness and injury; facilitation of healing; alleviation of suffering through the diagnosis and treatment of human response; and advocacy in the care of individuals, families, groups, communities, and populations.
- Where: Wherever there is a patient in need of care.
- When: Whenever there is a need for nursing knowledge, compassion, and expertise.
- Why: The profession exists to achieve the most positive patient outcomes in keeping with nursing’s social contract and obligation to society.
When each of these questions is answered, the complex considerations in scope of practice become clear. In a profession as dynamic as nursing, and with evolving health care demands, changes in scope of practice and overlapping responsibilities are inevitable in our current and future health care system.

Newly-Revised: Nursing: Scope and Standards of Practice, 4th Edition
This resource informs and guides nurses in their vital work providing safe, quality, and competent care.
Purchase your copy now »
Nursing Specialty Recognition, Scope and Standards Review, Affirmation of Competencies
The American Nurses Association has an established review program for recognition of a nursing specialty, approval of a specialty nursing scope of practice statement, acknowledgment of specialty nursing standards of practice, and affirmation of focused practice competencies. Details about each component of this program, specialty characteristics, review criteria, and submission process are described here .
Health care licensure
Currently, all health care licensure is state-based, and there is some variability between the qualifications for licensure and re-licensure for each state.
Defining scope of practice is generally a two-step process:
- Step 1: The state legislature passes a law, known as a “nurse practice act.”
- Step 2: Regulatory bodies then create and implement rules and regulations, intended to protect the public.
Choice in health care providers
The American Nurses Association (ANA) believes that patients’ interests are best served by a health care system in which many different types of qualified professionals are available, accessible, and working together – collaboratively. Therefore, it is important for scope of practice to reflect a professional’s true expertise.
ANA is a founding member of the Coalition for Patient’s Rights (CPR) , which was established to improve patients’ access to the health care providers of their choice, and the range of services those providers offer. The CPR consists of more than 35 organizations representing a variety of licensed health care professionals, each providing a diverse array of safe, effective, and affordable care.
Protecting and advancing scope of practice
Protecting and advancing scope of practice for nurses is a major initiative for ANA. In the fast-moving world of health care, it is vital that nurses are able to practice to the full extent of their education and abilities, in order to deliver the most efficient, quality care to patients.
There is a growing body of evidence to support the safe and cost-effective provision of care by APRNs, and a national call to remove all barriers to full practice authority. ANA remains committed to monitoring and advocating for legislative and regulatory changes relating to scope of practice, with the aim of removing practice barriers for nurses and improving access to care.
Certifying Bodies
- Acute Care NP
- Adult Psychiatric & Mental Health NP
- Diabetes Management – Advanced
- Family Psych & Mental Health NP
- Gerontological NP
- Pediatric NP
- Adult Health CNS
- Adult Psychiatric & Mental Health CNS
- Child/Adolescent Psych & Mental Health CNS
- Gerontological CNS
- Home Health CNS
- Pediatric CNS
- Acute Care Nurse Practitioner (ACNPC)
- Gerontologic NP
- Certified Nurse-Midwife (CNM)
- Certified Midwife (CM)
- Certified Registered Nurse Anesthetists (CRNA)
- Certified Pediatric Nurse (CPN)
- Primary Care Pediatric Nurse Practitioner (CPNP-PC)
- Acute Care Certified Pediatric Nurse Practitioner (CPNP-AC)
- Pediatric Primary Care Mental Health Specialist (PMHS)
- Oncology Nursing Certification Corporation (ONCC)
Specialty-Specific Resources
Other organizations, including many specialty organizations, publish a number of documents that can be helpful in defining scope of practice, from Scope & Standards documents to position statements.
The American Academy of Nurse Practitioners publishes Standards of Practice for Nurse Practitioners .
Anesthesia The American Association of Nurse Anesthetists (AANA) publishes Scope and Standards for Nurse Anesthesia Practice as well as a number of position statements that serve to define scope of practice.
Critical Care The American Association of Critical Care Nurses (AACN) publishes a number of practice resources .
Midwifery The American College of Nurse-Midwives (ACNM) publishes Core Competencies for Basic Midwifery Practice and Standards for the Practice of Midwifery .
Oncology The Oncology Nursing Society ( ONS ) publishes Oncology Nurse Practitioner Competencies . This document outlines specialty entry-level competencies for Oncology Nurse Practitioners (ONPs) who care for adult and late adolescent patients throughout the continuum of cancer care.
Pediatrics National Association of Pediatric Nurse Practitioners (NAPNAP) Pediatric Nursing: Scope and Standards of Practice is a collaborative effort of the ANA, the Society for Pediatric Nurses (SPN), and NAPNAP.
Psych/Mental Health The American Psychiatric Nurses Association (APNA) Web site provides information about the role of the advanced practice psychiatric nurse organized by topic, workplace setting, and/or specialty.
- Advanced Practice Registered Nurses (APRNs)
- Community Paramedics
- Medication Aides / Assistants / Technicians
The Scope of Nursing Practice describes the “who,” “what,” “where,” “when,” and “why” of nursing practice.
You May Also Like
Faith Community Nursing: Scope and Standards of Practice, 3rd Edition
Pain Management Nursing: Scope and Standards of Practice, 2nd Edition
Pediatric Nursing: Scope and Standards of Practice, 2nd Ed
Item(s) added to cart.
50 Nursing Philosophy Examples + How To Write Your Own

From the first semester of nursing school, aspiring nurses learn about the ethics and values associated with becoming a nurse. However, there comes a time when each nursing student or nurse must decide what they value most and how to incorporate those things into their roles as nurses. This important step is often referred to as establishing a personal philosophy of nursing. Perhaps you have heard of nursing philosophies but are unsure how to develop your personal philosophy. Have you wondered or asked, "What are some good personal philosophy of nursing examples?" If this sounds like you, keep reading! In this article, I will share some insight about nursing philosophies and provide you with information about 50 nursing philosophy examples + how to write your own.
What is a Personal Philosophy of Nursing?
Does every nurse have a personal nursing philosophy, what are the key components of a personal nursing philosophy, • knowledge:, 7 reasons why having a personal nursing philosophy is so important for your career, what are some good personal philosophy of nursing examples.
| Nursing Philosophy Examples For Nursing Students |
| “I believe it is important for everyone to strive to demonstrate the characteristics of honesty, persistence, and compassion. My philosophy on nursing is that if I use those characteristics, coupled with a desire for lifelong learning and a willingness to represent others in need, I can make a difference in the life of my patients and their families and become a strong member of the profession." “As an aspiring nurse, I feel like it is my responsibility to develop an attitude of life-long learning and take advantage of every opportunity to develop skills that will benefit my patients. If I were to articulate my own philosophy of nursing, I would say I believe nursing is one of the most selfless jobs a person can have, and I intend to put everything I have into this pursuit so I can make a difference in the lives of others.” “My nursing philosophy is that nursing is more than a career. It is a privilege accepted by people who are passionate about using their skills and knowledge to help others who cannot help themselves. I vow to be the best nurse I can be and dedicate my professional life to making the lives of others better." |
| Nursing Philosophy Examples For New Grad Nurses |
| “My philosophy about nursing is that it takes diverse people with strong skills and dedication to help impact and improve the lives of patients. I intend to use the education and skills I've obtained in nursing school to establish myself in this profession. I believe if I dedicate myself to a lifelong pursuit of knowledge and personal growth, I can influence the profession of nursing and help improve outcomes for my patients and their loved ones." "I believe in taking a holistic approach to nursing care, respecting my patients' cultural beliefs, ethnic background, and personal preferences. My philosophy of nursing is based on a desire to uphold the values and codes established by the American Nurses Association and to promote a sense of self-value in my patients as I help them reach their healthcare goals.” “My personal philosophy of nursing is that all nurses, whether we are new graduates or nurses with years of experience, have something of value to offer to patients and nursing as a profession. My sincere desire is to develop strong clinical skills and be open to new opportunities to learn and grow so I may contribute to the well-being of my patients and the further development of this profession." |
| Nursing Philosophy Examples For Registered Nurses |
| “As a registered nurse, I believe the care I provide should involve more than giving medicines or changing bandages. I want to treat my patients with the best care, making them feel respected, comfortable, and confident about the care they receive from my service.” “My philosophy as a registered nurse is quite simple. I want to serve everyone I can by giving my best as a nurse and decent human being. I believe all patients, families, and colleagues are unique individuals with unique needs, and I aim to offer my best to them in service as a registered nurse.” “I believe it is important for all nurses to provide safe, high-quality, patient-centered care. My personal philosophy of nursing is driven by a desire to recognize my patients as more than a medical diagnosis or room number. Instead, I desire to be the nurse who promotes the well-being of patients and helps improve outcomes, which will help support and further our profession.” “I chose to become a nurse because I have a deep-rooted desire to help people in need. My personal philosophy of nursing is that I will use my education and clinical experiences to care for my clients and act as an advocate for them, encouraging them to be actively involved in their own care, which increases their feelings of self-worth and results in improved outcomes." “I believe nursing is the truest version of living art a person can demonstrate. As I consider what I feel about my nursing philosophy, I realize the important role I have in improving the lives of others. I want my practice to reflect a genuine concern for every person entrusted to my care and to be a source of hope and encouragement." “For me, there was never any doubt I would become a nurse. I love people and feel most fulfilled when I can do something to help others. I believe nurses are in a unique position to make significant differences in the lives of others. I have made it my personal philosophy to embrace every opportunity to enrich my patients' lives and contribute to this wonderful profession." “My philosophy of nursing is based on the belief that, as a registered nurse, I am an educator, patient advocate, and promoter of good health practices. I feel being a nurse is an honor and privilege, and I desire to fulfill my role with the highest level of integrity and best practices, with the hope that I can contribute positive things to the lives of my patients and their families.” “It is my strong belief that my job involves much more than performing a nursing assessment or administering medications. I exercise my role within the personal nursing philosophy that all clients are unique in their own right and deserve to have care as unique as they are. By viewing each client as an individual and providing care with a holistic approach, I hope to positively impact their healthcare experiences and outcomes." |
| Nursing Philosophy Examples For Pediatric Nurses |
| “I always knew I wanted to become a nurse and had a strong desire to care for children, which is why I chose to specialize in pediatric nursing. I believe by combining compassionate and relational care that is centered around my patients and their family units, I can impact their lives and health outcomes.” “To me, there is no greater joy than being involved in the care of pediatric patients and their families. My personal philosophy of nursing is based on the understanding that open communication, as well as respect and appreciation for the importance of family and each family member's role, can significantly improve my patients' outcomes and help me be a strong member of the pediatric nursing community." “My philosophy of nursing may seem simple, but I truly believe it is possible to impact patient lives by using the power of human touch and emotional connections. I believe, as a pediatric nurse, it is especially important to develop trusting relationships with patients and their families so we can work together to reach positive patient outcomes.” |
| Nursing Philosophy Examples For Psychiatric Nurses |
| “I originally chose to pursue a career as a psychiatric nurse because of my personal experiences with major depression and anxiety. The more I learned, the more I realized how important it is to have competent nurses willing to be transparent enough that patients can relate and feel comfortable seeking help. My nursing philosophy stems from a strong belief that by being the type of nurse I needed when dealing with mental health issues, I can and will help my patients learn ways to manage and overcome obstacles that impact their well-being.” “My philosophy of nursing centers around a sincere desire to help others realize and obtain their desired health goals. Psychiatric nursing is a specialty that is truly personal for me, as I have experienced the loss of a close loved one due to mental illness. I believe nursing should incorporate a holistic approach that honors patient values and promotes positive outcomes." "I can't remember a time when I did not feel a longing to care for others in need, which I believe is what led me to choose nursing as a career. Psychiatric nursing is important to me because I feel as a society, we are just now beginning to realize the true impact mental health and wellness has on every other aspect of our lives. I feel happy when I serve others, and my personal philosophy of nursing is centered on the desire to serve and be compassionate toward others.” |
| Nursing Philosophy Examples For Neonatal Nurses |
| “I believe being trusted with the care of someone else’s child is a gift. As a neonatal nurse, I want to serve my patients and their families by using my skills to be actively involved in their journey of healing so they can recover and grow up to live healthy lives.” “I feel like anyone would be hard-pressed to try and simplify nursing in just a phrase or two. Just like nursing is a complex system made up of many people, I believe our personal philosophies of nursing are often multi-faceted. For me, my nursing philosophy centers around a longing to care for others and help them realize their potential. As a neonatal nurse, that philosophy encompasses patients, families, and everyone involved in care.” “I have a deep desire to care for neonatal patients and their families. My philosophy related to neonatal nursing is that it is my ethical duty to advocate for these patients who do not yet have a voice of their own. I intend to use every resource possible to learn and develop skills that will benefit my patients, comfort and educate their families, and be a strong partner in the neonatal nursing team.” |
| Nursing Philosophy Examples For ICU Nurses |
| "I chose to become an ICU nurse because I feel patients with intensive care needs should have the highest levels of quality care and compassion possible. My belief and personal philosophy of nursing is that all patients, regardless of their prognosis, should be cared for by nurses with a heart for healing. I desire to bring that type of care and compassion to my patients and their families." "Loved ones and I have received care from extraordinary nurses, which solidified my belief in the goodness of others, leading me to choose to pursue this role. Although I chose to become a nurse, I believe nursing is more of a calling, one I am glad I headed. My philosophy related to nursing is that if I can help make the life of one patient better, I will have achieved more than most." “I feel honored to be a nurse, and I have intentionally developed a personal nursing philosophy that reflects the privilege. My philosophy as an intensive care nurse is that I will offer the highest quality in nursing care to my patients and deliver it with compassion as if they were my own family. After all, we all want to feel wanted and cared for, especially when we are unable to care for ourselves." |
| Nursing Philosophy Examples For School Nurses |
| “I believe that school nurses can play a significant role in the lives of those we serve. My nursing philosophy is that I can positively influence those I meet and serve daily and that I will do everything I can to encourage their understanding of what it takes to be physically and mentally well. I feel strongly that when children learn the importance of health and wellness at an early age, they are more likely to make smart decisions about their health later. My personal goal in nursing is to have a positive impact on every client who crosses my path." "I believe it is important for nurses to emphasize the value of every patient for whom we provide care. I understand a student's health can directly impact his ability to learn. My philosophy of nursing, especially as I practice as a school nurse, is to be a source of education and guidance to help students realize their physical and academic potential and to help them strive to achieve their attainable goals.” “My personal nursing philosophy is built upon the belief that addressing the mental, physical, and social health needs of students is a responsibility that rests largely upon my shoulders. The job of a school nurse can be challenging but rewarding, and I am dedicated to always performing with the best interest of each student in mind. |
| Nursing Philosophy Examples For Labor And Delivery Nurses |
| “My philosophy is that nurses have an obligation to provide safe, patient-centered care in a manner that supports individual patient choices, values, and beliefs. I feel, as a labor and delivery nurse, it is crucial to understand the concept of holistic nursing care and to implement it with each patient and family." “I believe nursing is much more than treating illness or disease. Instead, my philosophy of nursing is that it should be focused on providing high-quality patient care tailored to the patient's individual needs. Working in labor and delivery means offering the same care and compassion to the patient's spouse or other loved ones and ensuring everyone's needs are met." "My nursing philosophy is based on my knowledge of what it feels like to need a competent nurse to coach and support me as I labored and delivered my children. I remind myself daily what it meant to have someone in my corner, and I intend to be the same professional, compassionate supporter for all my clients.” |
| Nursing Philosophy Examples For Home Health Nurses |
| “As a provider of nursing care with the privilege of serving in clients’ homes, I realize I am simply a guest who happens to have skills that could enrich my patients’ lives. Although some parts of my personal philosophy may change over time, the core of my personal philosophy on nursing is that I have a great responsibility to provide care for those unable to care for themselves. Knowing this, I am both grateful and extremely humbled." "My beliefs about nursing and the philosophy I try to live by include acknowledging that all patient care should be based on respect for the value and dignity of the patient as an individual with rights. I desire to have a strong work ethic and demonstrate genuine compassion for those entrusted to my care." “I believe effective nursing requires nurses to develop and adhere to strong personal and professional philosophies. My philosophy of nursing is that all patients, whether they are cared for in hospitals, nursing homes, another type of healthcare facility, or their own homes, deserve to feel respected and have their voices heard. I work hard to make sure my clients know their thoughts and feelings are important and promote an atmosphere of care conducive to positive outcomes." |
| Nursing Philosophy Examples For Charge Nurses |
| “As a nurse with several years of experience seeking to work as a charge nurse, my nursing philosophy is based on my duty to provide compassionate, competent nursing care and to lead others in doing the same. I am committed to providing exceptional nursing care and being a role model for other nurses to follow.” “My philosophy of nursing is firmly rooted in beliefs instilled in me as a child. The values and beliefs taught to me by family and others include the need for respect, trustworthiness, and compassion. These beliefs led me to choose nursing as a profession and why I now desire to work as a charge nurse. It is my hope to pass these values onto other nurses for generations to come.” “I feel strongly that all nurses have a responsibility to provide personalized care to patients, regardless of the patient's background or beliefs, and respect the patient's right to autonomy. My philosophy as a charge nurse is to demonstrate the work ethic and professional values I want to see in my team and to support them as they pursue professional goals and strive to provide exceptional patient care." |
| Nursing Philosophy Examples For Nurse Managers |
| "From the time I was in junior high school, I knew I would become a nurse. I love serving others and feel most successful when I help others succeed. My philosophy of nursing includes a belief that a few of the main factors in being a good nurse manager are the ability to effectively communicate with others and a desire to build solid teams, instead of promoting myself.” “I have always believed nurses have a way of touching lives that others do not. As I embraced my career and began considering what is important to me, I began to develop a personal nursing philosophy based on the characteristics I value in others and how I can apply them to my life. To succeed as a nurse manager, I must treat every nurse with respect and appreciation and model the type of behavior I want for my patients, so my team has a strong leader to follow." “I believe one of the most important jobs a nurse can do is be a strong support for patients and families. My nursing philosophy is grounded in the belief that by being a supportive advocate and giving clients a safe person to talk with and trust to provide their care, we can transform their healthcare experiences. I desire to become the kind of nurse manager who leads teams of nurses equipped to handle even the most delicate situations and who are viewed as assets to patient care." |
| Nursing Philosophy Examples For Directors Of Nursing |
| “I feel being a competent Director of Nursing requires active participation with the nurses on my team and the patients we provide care for. As a registered nurse serving as a nursing director, I believe in establishing an atmosphere of collaboration that fosters growth and a renewed commitment to our common goal of patient care" "I sincerely believe nursing is the most rewarding career I could have chosen. I have a strong philosophy based on the idea that by exerting positive influence, promoting quality nursing care, and facilitating collaborative communication among the disciplinary team, we can be a strong nursing force. As a Director of Nursing, I intend to put those ideas into practice every day." “My personal philosophy of nursing is that we all have the power to significantly impact and improve patient outcomes and promote the furtherance of our profession. I believe a solid education and continued learning are essential for the success of nurses. I also believe any nurse in a directorship position should promote the growth of every nurse on her team. That is something I vow to do." |
| Nursing Philosophy Examples For Nurse Practitioners |
| “As a nurse practitioner, my philosophy of nursing is to provide individualized care to my clients by acknowledging their unique situations, educating patients and their families, and providing unconditionally compassionate, high-quality care. I believe my success as a nurse practitioner requires me to accept accountability for being a strong advocate for my patients and their loved ones, as well as being a strong representative of advanced practice nursing." “My personal nursing philosophy is grounded in a conviction that I am in a unique position to positively impact my patients and help improve their outcomes. I believe in the importance of creating an atmosphere that supports strong provider and patient relationships based on respect for my patient’s beliefs and desires for their health and their freedom of choice.” "To me, being a nurse practitioner is more than prescribing medications or treating a specific illness. If I could describe my personal philosophy of nursing from the perspective of a nurse practitioner, I would say it is my duty to promote a healthcare environment that is respectful of and therapeutic for all patients and their families. I will take the role of being a nurse practitioner, representing my patients and the nursing profession to the best of my ability.” |
| Nursing Philosophy Examples For Nursing Educators |
| “As a nurse educator, I value the opportunity to pour into the lives of student nurses. I believe being a nurse educator is a true calling, and if I serve in my role to the best of my ability, I can help change the trajectory of my students' lives and the lives of every patient they ever encounter." “I have based my personal philosophy of nursing on the belief that one of the greatest gifts I can give to my profession is a willingness to impart knowledge to, and encourage learning among, aspiring nurses. I have dedicated my life to improving the lives of others and will continue to do so as a nurse educator, with the hopes of impacting student nurses, the patients we care for, and this profession." “My philosophy of nursing is that we all have a role to play in the health and wellness of ourselves, our families, and our communities. I experienced some of the greatest influence in my life from nursing educators who prepared me for this career. I now intend to give back to the profession and society by demonstrating a strong work ethic and providing patient-centered care, with the hope of helping patients achieve wellness and students achieve professional goals." |
How to Write Your Own Personal Philosophy of Nursing Statement?
1. define what nursing means in your perspective., 2. ask yourself what personal experience relates to your passion for nursing., 3. consider how you want to impact patients, families, and communities through your role as a nurse., 4. highlight your skills., 5. define your personal and professional values., 8 questions to ask yourself when developing your own personal philosophy of nursing, question #1: why did i choose to become a nurse, how to find an answer to this question:, question #2: what are my personal beliefs about nursing, question #3: what qualities make someone a great nurse, question #4: what skills should all nurses have, question #5: why is nursing important to me, question #6: what theories do i have about nursing, question #7: what values should nurses consider important, question #8: would i choose this career again, useful online resources to learn more about nursing philosophy, blogs/websites, youtube videos, bonus 5 important things to keep in mind when writing your personal philosophy of nursing statement, 1. keep it simple., 2. show you are prepared for action., 3. be yourself., 4. be open to change if needed., 5. make a copy for yourself and keep it visible., my final thoughts, frequently asked questions asked by our expert, 1. what was florence nightingale's philosophy of nursing, 2. is there a set format or right way to write a personal philosophy of nursing statement, 3. how do i start my nursing philosophy statement, 4. how can a nurse determine whether her nursing philosophy is good, 5. how long should a personal nursing philosophy statement be, 6. when should i write my nursing philosophy, 7. can i change my nursing philosophy from time to time, 8. how to write the introduction of my personal nursing philosophy, 9. should nursing students have a personal philosophy of nursing, 10. does an informatics nurse have a personal philosophy of nursing, 11. do nursing organizations have their own philosophy of nursing, 12. how does nursing philosophy influence nursing practice, 13. is it required for every nurse to have a personal nursing philosophy, 14. what happens if a nurse does not have a personal philosophy of nursing, 15. what are some famous personal philosophy of nursing quotes.

Nursing Theories and Theorists: The Definitive Guide for Nurses
In this guide for nursing theories and nursing theorists , we aim to help you understand what comprises a nursing theory and its importance, purpose, history, types, or classifications, and give you an overview through summaries of selected nursing theories.
Table of Contents
- What are Nursing Theories?
Defining Terms
History of nursing theories, environment, definitions, relational statements, assumptions, why are nursing theories important, in academic discipline, in research, in the profession, grand nursing theories, middle-range nursing theories, practice-level nursing theories, factor-isolating theory, explanatory theory, prescriptive theories, other ways of classifying nursing theories, florence nightingale, hildegard e. peplau, virginia henderson, faye glenn abdellah, ernestine wiedenbach, lydia e. hall, joyce travelbee, kathryn e. barnard, evelyn adam, nancy roper, winifred logan, and alison j. tierney, ida jean orlando, jean watson.
- Marilyn Anne Ray
Patricia Benner
Kari martinsen, katie eriksson, myra estrin levine, martha e. rogers, dorothea e. orem, imogene m. king, betty neuman, sister callista roy, dorothy e. johnson, anne boykin and savina o. schoenhofer, afaf ibrahim meleis, nola j. pender, madeleine m. leininger, margaret a. newman, rosemarie rizzo parse, helen c. erickson, evelyn m. tomlin, and mary ann p. swain, gladys l. husted and james h. husted, ramona t. mercer, merle h. mishel, pamela g. reed, carolyn l. wiener and marylin j. dodd, georgene gaskill eakes, mary lermann burke, and margaret a. hainsworth, phil barker, katharine kolcaba, cheryl tatano beck, kristen m. swanson, cornelia m. ruland and shirley m. moore, wanda de aguiar horta, recommended resources, what are nursing theories.
Nursing theories are organized bodies of knowledge to define what nursing is, what nurses do, and why they do it. Nursing theories provide a way to define nursing as a unique discipline that is separate from other disciplines (e.g., medicine). It is a framework of concepts and purposes intended to guide nursing practice at a more concrete and specific level.
Nursing, as a profession, is committed to recognizing its own unparalleled body of knowledge vital to nursing practice—nursing science. To distinguish this foundation of knowledge, nurses need to identify, develop, and understand concepts and theories in line with nursing. As a science, nursing is based on the theory of what nursing is, what nurses do, and why. Nursing is a unique discipline and is separate from medicine. It has its own body of knowledge on which delivery of care is based.
The development of nursing theory demands an understanding of selected terminologies, definitions, and assumptions.
- Philosophy. These are beliefs and values that define a way of thinking and are generally known and understood by a group or discipline.
- Theory . A belief, policy, or procedure proposed or followed as the basis of action. It refers to a logical group of general propositions used as principles of explanation. Theories are also used to describe, predict, or control phenomena.
- Concept. Concepts are often called the building blocks of theories. They are primarily the vehicles of thought that involve images.
- Models. Models are representations of the interaction among and between the concepts showing patterns. They present an overview of the theory’s thinking and may demonstrate how theory can be introduced into practice.
- Conceptual framework. A conceptual framework is a group of related ideas, statements, or concepts. It is often used interchangeably with the conceptual model and with grand theories .
- Proposition. Propositions are statements that describe the relationship between the concepts.
- Domain . The domain is the perspective or territory of a profession or discipline.
- Process. Processes are organized steps, changes, or functions intended to bring about the desired result.
- Paradigm. A paradigm refers to a pattern of shared understanding and assumptions about reality and the world, worldview, or widely accepted value system.
- Metaparadigm. A metaparadigm is the most general statement of discipline and functions as a framework in which the more restricted structures of conceptual models develop. Much of the theoretical work in nursing focused on articulating relationships among four major concepts: person, environment, health, and nursing.
The first nursing theories appeared in the late 1800s when a strong emphasis was placed on nursing education.
- In 1860, Florence Nightingale defined nursing in her “ Environmental Theory ” as “the act of utilizing the patient’s environment to assist him in his recovery.”
- In the 1950s, there is a consensus among nursing scholars that nursing needed to validate itself through the production of its own scientifically tested body of knowledge.
- In 1952, Hildegard Peplau introduced her Theory of Interpersonal Relations that emphasizes the nurse -client relationship as the foundation of nursing practice.
- In 1955, Virginia Henderson conceptualized the nurse’s role as assisting sick or healthy individuals to gain independence in meeting 14 fundamental needs. Thus her Nursing Need Theory was developed.
- In 1960, Faye Abdellah published her work “Typology of 21 Nursing Problems,” which shifted the focus of nursing from a disease-centered approach to a patient-centered approach.
- In 1962, Ida Jean Orlando emphasized the reciprocal relationship between patient and nurse and viewed nursing’s professional function as finding out and meeting the patient’s immediate need for help.
- In 1968, Dorothy Johnson pioneered the Behavioral System Model and upheld the fostering of efficient and effective behavioral functioning in the patient to prevent illness.
- In 1970, Martha Rogers viewed nursing as both a science and an art as it provides a way to view the unitary human being, who is integral with the universe.
- In 1971, Dorothea Orem stated in her theory that nursing care is required if the client is unable to fulfill biological, psychological, developmental, or social needs.
- In 1971, Imogene King ‘s Theory of Goal attainment stated that the nurse is considered part of the patient’s environment and the nurse-patient relationship is for meeting goals towards good health.
- In 1972, Betty Neuman , in her theory, states that many needs exist, and each may disrupt client balance or stability. Stress reduction is the goal of the system model of nursing practice.
- In 1979, Sr. Callista Roy viewed the individual as a set of interrelated systems that maintain the balance between these various stimuli.
- In 1979, Jean Watson developed the philosophy of caring, highlighted humanistic aspects of nursing as they intertwine with scientific knowledge and nursing practice.
The Nursing Metaparadigm
Four major concepts are frequently interrelated and fundamental to nursing theory: person, environment, health, and nursing. These four are collectively referred to as metaparadigm for nursing .

Person (also referred to as Client or Human Beings) is the recipient of nursing care and may include individuals, patients, groups, families, and communities.
Environment (or situation) is defined as the internal and external surroundings that affect the client. It includes all positive or negative conditions that affect the patient, the physical environment, such as families, friends, and significant others, and the setting for where they go for their healthcare.
Health is defined as the degree of wellness or well-being that the client experiences. It may have different meanings for each patient, the clinical setting, and the health care provider.
The nurse’s attributes, characteristics, and actions provide care on behalf of or in conjunction with the client. There are numerous definitions of nursing, though nursing scholars may have difficulty agreeing on its exact definition. The ultimate goal of nursing theories is to improve patient care .
You’ll find that these four concepts are used frequently and defined differently throughout different nursing theories. Each nurse theorist’s definition varies by their orientation, nursing experience , and different factors that affect the theorist’s nursing view. The person is the main focus, but how each theorist defines the nursing metaparadigm gives a unique take specific to a particular theory. To give you an example, below are the different definitions of various theorists on the nursing metaparadigm:
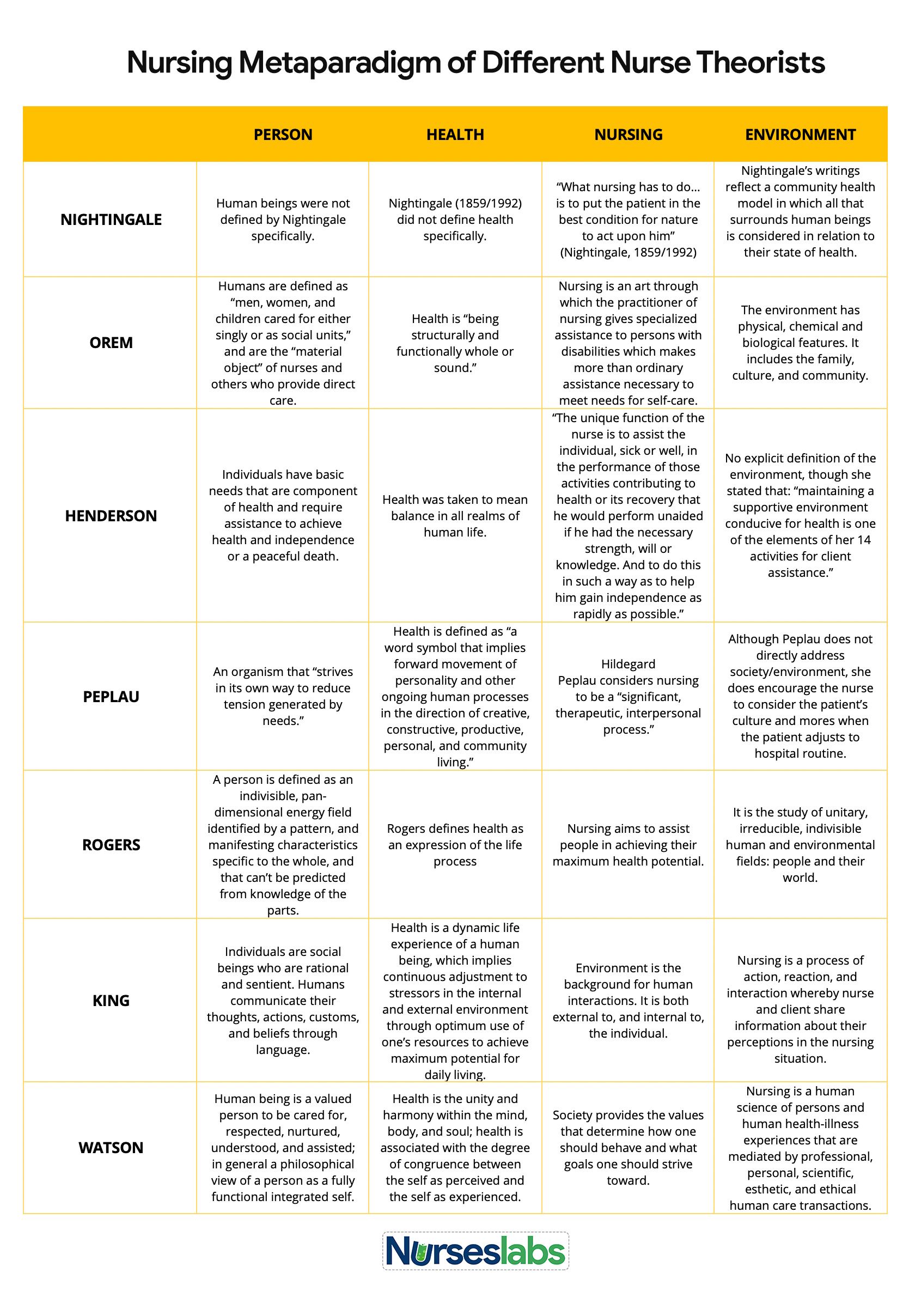
Components of Nursing Theories
For a theory to be a theory, it has to contain concepts, definitions, relational statements, and assumptions that explain a phenomenon. It should also explain how these components relate to each other.
A term given to describe an idea or response about an event, a situation, a process, a group of events, or a group of situations. Phenomena may be temporary or permanent. Nursing theories focus on the phenomena of nursing.
Interrelated concepts define a theory. Concepts are used to help describe or label a phenomenon. They are words or phrases that identify, define, and establish structure and boundaries for ideas generated about a particular phenomenon. Concepts may be abstract or concrete.
- Abstract Concepts . Defined as mentally constructed independently of a specific time or place.
- Concrete Concepts . Are directly experienced and related to a particular time or place.
Definitions are used to convey the general meaning of the concepts of the theory. Definitions can be theoretical or operational.
- Theoretical Definitions . Define a particular concept based on the theorist’s perspective.
- Operational Definitions . States how concepts are measured.
Relational statements define the relationships between two or more concepts. They are the chains that link concepts to one another.
Assumptions are accepted as truths and are based on values and beliefs. These statements explain the nature of concepts, definitions, purpose, relationships, and structure of a theory.
Nursing theories are the basis of nursing practice today. In many cases, nursing theory guides knowledge development and directs education, research, and practice. Historically, nursing was not recognized as an academic discipline or as a profession we view today. Before nursing theories were developed, nursing was considered to be a task-oriented occupation. The training and function of nurses were under the direction and control of the medical profession. Let’s take a look at the importance of nursing theory and its significance to nursing practice:
- Nursing theories help recognize what should set the foundation of practice by explicitly describing nursing.
- By defining nursing, a nursing theory also helps nurses understand their purpose and role in the healthcare setting.
- Theories serve as a rationale or scientific reasons for nursing interventions and give nurses the knowledge base necessary for acting and responding appropriately in nursing care situations.
- Nursing theories provide the foundations of nursing practice, generate further knowledge, and indicate which direction nursing should develop in the future (Brown, 1964).
- By providing nurses a sense of identity, nursing theory can help patients, managers, and other healthcare professionals to acknowledge and understand the unique contribution that nurses make to the healthcare service (Draper, 1990).
- Nursing theories prepare the nurses to reflect on the assumptions and question the nursing values, thus further defining nursing and increasing the knowledge base.
- Nursing theories aim to define, predict, and demonstrate nursing phenomenon (Chinn and Jacobs, 1978).
- It can be regarded as an attempt by the nursing profession to maintain and preserve its professional limits and boundaries.
- Nursing theories can help guide research and informing evidence-based practice.
- Provide a common language and terminology for nurses to use in communication and practice.
- Serves as a basis for the development of nursing education and training programs.
- In many cases, nursing theories guide knowledge development and directs education, research, and practice, although each influences the others. (Fitzpatrick and Whall, 2005).
Purposes of Nursing Theories
The primary purpose of theory in nursing is to improve practice by positively influencing the health and quality of life of patients. Nursing theories are essential for the development and advancement of the nursing profession. Nursing theories are also developed to define and describe nursing care, guide nursing practice, and provide a basis for clinical decision-making . In the past, the accomplishments of nursing led to the recognition of nursing in an academic discipline, research, and profession.
Much of the earlier nursing programs identified the major concepts in one or two nursing models, organized the concepts, and build an entire nursing curriculum around the created framework. These models’ unique language was typically introduced into program objectives, course objectives, course descriptions, and clinical performance criteria. The purpose was to explain the fundamental implications of the profession and enhance the profession’s status.
The development of theory is fundamental to the research process, where it is necessary to use theory as a framework to provide perspective and guidance to the research study. Theory can also be used to guide the research process by creating and testing phenomena of interest. To improve the nursing profession’s ability to meet societal duties and responsibilities, there needs to be a continuous reciprocal and cyclical connection with theory, practice, and research. This will help connect the perceived “gap” between theory and practice and promote the theory-guided practice.
Clinical practice generates research questions and knowledge for theory. In a clinical setting, its primary contribution has been the facilitation of reflecting, questioning, and thinking about what nurses do. Because nurses and nursing practice are often subordinate to powerful institutional forces and traditions, introducing any framework that encourages nurses to reflect on, question, and think about what they do provide an invaluable service.
Classification of Nursing Theories
There are different ways to categorize nursing theories. They are classified depending on their function, levels of abstraction, or goal orientation.
By Abstraction
There are three major categories when classifying nursing theories based on their level of abstraction: grand theory, middle-range theory, and practice-level theory.

- Grand theories are abstract, broad in scope, and complex, therefore requiring further research for clarification.
- Grand nursing theories do not guide specific nursing interventions but rather provide a general framework and nursing ideas.
- Grand nursing theorists develop their works based on their own experiences and their time, explaining why there is so much variation among theories.
- Address the nursing metaparadigm components of person, nursing, health, and environment.
- More limited in scope (compared to grand theories) and present concepts and propositions at a lower level of abstraction. They address a specific phenomenon in nursing.
- Due to the difficulty of testing grand theories, nursing scholars proposed using this level of theory.
- Most middle-range theories are based on a grand theorist’s works, but they can be conceived from research, nursing practice, or the theories of other disciplines.
- Practice nursing theories are situation-specific theories that are narrow in scope and focuses on a specific patient population at a specific time.
- Practice-level nursing theories provide frameworks for nursing interventions and suggest outcomes or the effect of nursing practice.
- Theories developed at this level have a more direct effect on nursing practice than more abstract theories.
- These theories are interrelated with concepts from middle-range theories or grand theories.
By Goal Orientation
Theories can also be classified based on their goals. They can be descriptive or prescriptive .
Descriptive Theories
- Descriptive theories are the first level of theory development. They describe the phenomena and identify its properties and components in which it occurs.
- Descriptive theories are not action-oriented or attempt to produce or change a situation.
- There are two types of descriptive theories: factor-isolating theory and explanatory theory .
- Also known as category-formulating or labeling theory.
- Theories under this category describe the properties and dimensions of phenomena.
- Explanatory theories describe and explain the nature of relationships of certain phenomena to other phenomena.
- Address the nursing interventions for a phenomenon, guide practice change, and predict consequences.
- Includes propositions that call for change.
- In nursing, prescriptive theories are used to anticipate the outcomes of nursing interventions.
Classification According to Meleis
Afaf Ibrahim Meleis (2011), in her book Theoretical Nursing: Development and Progress , organizes the major nurse theories and models using the following headings: needs theories, interaction theories, and outcome theories. These categories indicate the basic philosophical underpinnings of the theories.
- Needs-Based Theories. The needs theorists were the first group of nurses who thought of giving nursing care a conceptual order. Theories under this group are based on helping individuals to fulfill their physical and mental needs. Theories of Orem, Henderson, and Abdella are categorized under this group. Need theories are criticized for relying too much on the medical model of health and placing the patient in an overtly dependent position.
- Interaction Theories. These theories emphasized nursing on the establishment and maintenance of relationships. They highlighted the impact of nursing on patients and how they interact with the environment, people, and situations. Theories of King, Orlando, and Travelbee are grouped under this category.
- Outcome Theories . These theories describe the nurse as controlling and directing patient care using their knowledge of the human physiological and behavioral systems. The nursing theories of Johnson , Levine , Rogers , and Roy belong to this group.
Classification According to Alligood
In her book, Nursing Theorists and Their Work, Raile Alligood (2017) categorized nursing theories into four headings: nursing philosophy, nursing conceptual models, nursing theories and grand theories, and middle-range nursing theories.
- Nursing Philosophy . It is the most abstract type and sets forth the meaning of nursing phenomena through analysis, reasoning, and logical presentation. Works of Nightingale, Watson, Ray, and Benner are categorized under this group.
- Nursing Conceptual Models . These are comprehensive nursing theories that are regarded by some as pioneers in nursing. These theories address the nursing metaparadigm and explain the relationship between them. Conceptual models of Levine, Rogers, Roy, King, and Orem are under this group.
- Grand Nursing Theories. Are works derived from nursing philosophies, conceptual models, and other grand theories that are generally not as specific as middle-range theories. Works of Levine, Rogers, Orem, and King are some of the theories under this category.
- Middle-Range Theories. Are precise and answer specific nursing practice questions . They address the specifics of nursing situations within the model’s perspective or theory from which they are derived. Examples of Middle-Range theories are that of Mercer, Reed, Mishel, and Barker.
List of Nursing Theories and Theorists
You’ve learned from the previous sections the definition of nursing theory, its significance in nursing, and its purpose in generating a nursing knowledge base. This section will give you an overview and summary of the various published works in nursing theory (in chronological order). Deep dive into learning about the theory by clicking on the links provided for their biography and comprehensive review of their work.
See Also: Florence Nightingale: Environmental Theory and Biography
- Founder of Modern Nursing and Pioneer of the Environmental Theory.
- Defined Nursing as “the act of utilizing the environment of the patient to assist him in his recovery.”
- Stated that nursing “ought to signify the proper use of fresh air, light, warmth, cleanliness, quiet, and the proper selection and administration of diet – all at the least expense of vital power to the patient.”
- Identified five (5) environmental factors: fresh air, pure water, efficient drainage, cleanliness or sanitation, and light or direct sunlight.
See Also: Hildegard Peplau: Interpersonal Relations Theory
- Pioneered the Theory of Interpersonal Relations
- Peplau’s theory defined Nursing as “An interpersonal process of therapeutic interactions between an individual who is sick or in need of health services and a nurse specially educated to recognize, respond to the need for help.”
- Her work is influenced by Henry Stack Sullivan, Percival Symonds, Abraham Maslow , and Neal Elgar Miller.
- It helps nurses and healthcare providers develop more therapeutic interventions in the clinical setting.
See Also: Virginia Henderson: Nursing Need Theory
- Developed the Nursing Need Theory
- Focuses on the importance of increasing the patient’s independence to hasten their progress in the hospital.
- Emphasizes the basic human needs and how nurses can assist in meeting those needs.
- “The nurse is expected to carry out a physician’s therapeutic plan, but individualized care is the result of the nurse’s creativity in planning for care.”
See Also: Faye Glenn Abdellah: 21 Nursing Problems Theory
- Developed the 21 Nursing Problems Theory
- “Nursing is based on an art and science that molds the attitudes, intellectual competencies, and technical skills of the individual nurse into the desire and ability to help people, sick or well, cope with their health needs.”
- Changed the focus of nursing from disease-centered to patient-centered and began to include families and the elderly in nursing care.
- The nursing model is intended to guide care in hospital institutions but can also be applied to community health nursing, as well.
- Developed The Helping Art of Clinical Nursing conceptual model.
- Definition of nursing reflects on nurse-midwife experience as “People may differ in their concept of nursing, but few would disagree that nursing is nurturing or caring for someone in a motherly fashion.”
- Guides the nurse action in the art of nursing and specified four elements of clinical nursing: philosophy, purpose, practice, and art.
- Clinical nursing is focused on meeting the patient’s perceived need for help in a vision of nursing that indicates considerable importance on the art of nursing.
See Also: Lydia Hall: Care, Cure, Core Theory
- Developed the Care, Cure, Core Theory is also known as the “ Three Cs of Lydia Hall . “
- Hall defined Nursing as the “participation in care, core and cure aspects of patient care , where CARE is the sole function of nurses, whereas the CORE and CURE are shared with other members of the health team.”
- The major purpose of care is to achieve an interpersonal relationship with the individual to facilitate the development of the core.
- The “care” circle defines a professional nurse’s primary role, such as providing bodily care for the patient. The “core” is the patient receiving nursing care. The “cure” is the aspect of nursing that involves the administration of medications and treatments.
- States in her Human-to-Human Relationship Model that the purpose of nursing was to help and support an individual, family, or community to prevent or cope with the struggles of illness and suffering and, if necessary, to find significance in these occurrences, with the ultimate goal being the presence of hope.
- Nursing was accomplished through human-to-human relationships.
- Extended the interpersonal relationship theories of Peplau and Orlando.
- Developed the Child Health Assessment Model .
- Concerns improving the health of infants and their families.
- Her findings on parent-child interaction as an important predictor of cognitive development helped shape public policy.
- She is the founder of the Nursing Child Assessment Satellite Training Project (NCAST), which produces and develops research-based products, assessment , and training programs to teach professionals, parents, and other caregivers the skills to provide nurturing environments for young children.
- Borrows from psychology and human development and focuses on mother-infant interaction with the environment.
- Contributed a close link to practice that has modified the way health care providers assess children in light of the parent-child relationship.
- Focuses on the development of models and theories on the concept of nursing.
- Includes the profession’s goal, the beneficiary of the professional service, the role of the professional, the source of the beneficiary’s difficulty, the intervention of the professional, and the consequences.
- A good example of using a unique basis of nursing for further expansion.
- A Model for Nursing Based on a Model of Living
- Logan produced a simple theory, “which actually helped bedside nurses.”
- The trio collaborated in the fourth edition of The Elements of Nursing: A Model for Nursing Based on a Model of Living and prepared a monograph entitled The Roper-Logan-Tierney Model of Nursing: Based on Activities of Daily Living.
- Includes maintaining a safe environment, communicating, breathing, eating and drinking, eliminating, personal cleansing and dressing , controlling body temperature, mobilizing, working and playing, expressing sexuality, sleeping , and dying .
See Also: Ida Jean Orlando: Nursing Process Theory
- She developed the Nursing Process Theory.
- “Patients have their own meanings and interpretations of situations, and therefore nurses must validate their inferences and analyses with patients before drawing conclusions.”
- Allows nurses to formulate an effective nursing care plan that can also be easily adapted when and if any complexity comes up with the patient.
- According to her, persons become patients requiring nursing care when they have needs for help that cannot be met independently because of their physical limitations, negative reactions to an environment, or experience that prevents them from communicating their needs.
- The role of the nurse is to find out and meet the patient’s immediate needs for help.
See Also: Jean Watson: Theory of Human Caring
- She pioneered the Philosophy and Theory of Transpersonal Caring .
- “Nursing is concerned with promoting health, preventing illness, caring for the sick, and restoring health.”
- Mainly concerns with how nurses care for their patients and how that caring progresses into better plans to promote health and wellness, prevent illness and restore health.
- Focuses on health promotion , as well as the treatment of diseases.
- Caring is central to nursing practice and promotes health better than a simple medical cure.
Marilyn Anne Ray
- Developed the Theory of Bureaucratic Caring
- “Improved patient safety , infection control, reduction in medication errors , and overall quality of care in complex bureaucratic health care systems cannot occur without knowledge and understanding of complex organizations, such as the political and economic systems, and spiritual-ethical caring, compassion and right action for all patients and professionals.”
- Challenges participants in nursing to think beyond their usual frame of reference and envision the world holistically while considering the universe as a hologram.
- Presents a different view of how health care organizations and nursing phenomena interrelate as wholes and parts in the system.
- Caring, Clinical Wisdom, and Ethics in Nursing Practice
- “The nurse-patient relationship is not a uniform, professionalized blueprint but rather a kaleidoscope of intimacy and distance in some of the most dramatic, poignant, and mundane moments of life.”
- Attempts to assert and reestablish nurses’ caring practices when nurses are rewarded more for efficiency, technical skills, and measurable outcomes.
- States that caring practices are instilled with knowledge and skill regarding everyday human needs.
- Philosophy of Caring
- “Nursing is founded on caring for life, on neighborly love, […]At the same time, the nurse must be professionally educated.”
- Human beings are created and are beings for whom we may have administrative responsibility.
- Caring, solidarity, and moral practice are unavoidable realities.
- Theory of Carative Caring
- “Caritative nursing means that we take ‘caritas’ into use when caring for the human being in health and suffering […] Caritative caring is a manifestation of the love that ‘just exists’ […] Caring communion, true caring, occurs when the one caring in a spirit of caritas alleviates the suffering of the patient.”
- The ultimate goal of caring is to lighten suffering and serve life and health.
- Inspired many in the Nordic countries and used it as the basis of research, education, and clinical practice.
See Also: Myra Estrin Levine: Conservation Model for Nursing
- According to the Conservation Model , “Nursing is human interaction.”
- Provides a framework within which to teach beginning nursing students.
- Logically congruent, externally and internally consistent, has breadth and depth, and is understood, with few exceptions, by professionals and consumers of health care.
See Also: Martha Rogers: Theory of Unitary Human Beings
- In Roger’s Theory of Human Beings , she defined Nursing as “an art and science that is humanistic and humanitarian.
- The Science of Unitary Human Beings contains two dimensions: the science of nursing, which is the knowledge specific to the field of nursing that comes from scientific research; and the art of nursing, which involves using nursing creatively to help better the lives of the patient.
- A patient can’t be separated from his or her environment when addressing health and treatment.
See Also: Dorothea E. Orem: Self-Care Theory
- In her Self-Care Theory , she defined Nursing as “The act of assisting others in the provision and management of self-care to maintain or improve human functioning at the home level of effectiveness.”
- Focuses on each individual’s ability to perform self-care .
- Composed of three interrelated theories: (1) the theory of self-care , (2) the self-care deficit theory, and (3) the theory of nursing systems, which is further classified into wholly compensatory, partially compensatory, and supportive-educative.
See Also: Imogene M. King: Theory of Goal Attainment
- Conceptual System and Middle-Range Theory of Goal Attainment
- “Nursing is a process of action, reaction and interaction by which nurse and client share information about their perception in a nursing situation” and “a process of human interactions between nurse and client whereby each perceives the other and the situation, and through communication , they set goals, explore means, and agree on means to achieve goals.”
- Focuses on this process to guide and direct nurses in the nurse-patient relationship, going hand-in-hand with their patients to meet good health goals.
- Explains that the nurse and patient go hand-in-hand in communicating information, set goals together, and then take actions to achieve those goals.
See Also: Betty Neuman: Neuman’s Systems Model
- In Neuman’s System Model , she defined nursing as a “unique profession in that is concerned with all of the variables affecting an individual’s response to stress.”
- The focus is on the client as a system (which may be an individual, family, group, or community) and on the client’s responses to stressors.
- The client system includes five variables (physiological, psychological, sociocultural, developmental, and spiritual). It is conceptualized as an inner core (basic energy resources) surrounded by concentric circles that include lines of resistance, a normal defense line, and a flexible line of defense.
See Also: Sister Callista Roy: Adaptation Model of Nursing
- In Adaptation Model , Roy defined nursing as a “health care profession that focuses on human life processes and patterns and emphasizes the promotion of health for individuals, families, groups, and society as a whole.”
- Views the individual as a set of interrelated systems that strives to maintain a balance between various stimuli.
- Inspired the development of many middle-range nursing theories and adaptation instruments.
See Also: Dorothy E. Johnson: Behavioral Systems Model
- The Behavioral System Model defined Nursing as “an external regulatory force that acts to preserve the organization and integrate the patients’ behaviors at an optimum level under those conditions in which the behavior constitutes a threat to the physical or social health or in which illness is found.”
- Advocates to foster efficient and effective behavioral functioning in the patient to prevent illness and stresses the importance of research-based knowledge about the effect of nursing care on patients.
- Describes the person as a behavioral system with seven subsystems: the achievement, attachment-affiliative, aggressive-protective, dependency, ingestive, eliminative, and sexual subsystems.
- The Theory of Nursing as Caring: A Model for Transforming Practice
- Nursing is an “exquisitely interwoven” unity of aspects of the discipline and profession of nursing.
- Nursing’s focus and aim as a discipline of knowledge and a professional service are “nurturing persons living to care and growing in caring.”
- Caring in nursing is “an altruistic, active expression of love, and is the intentional and embodied recognition of value and connectedness.”
- Transitions Theory
- It began with observations of experiences faced as people deal with changes related to health, well-being, and the ability to care for themselves.
- Types of transitions include developmental, health and illness, situational, and organizational.
- Acknowledges the role of nurses as they help people go through health/illness and life transitions.
- Focuses on assisting nurses in facilitating patients’, families’, and communities’ healthy transitions.
See Also: Nola Pender: Health Promotion Model
- Health Promotion Model
- Describes the interaction between the nurse and the consumer while considering the role of the health promotion environment.
- It focuses on three areas: individual characteristics and experiences, behavior-specific cognitions and affect, and behavioral outcomes.
- Describes the multidimensional nature of persons as they interact within their environment to pursue health.
See Also: Madeleine M. Leininger: Transcultural Nursing Theory
- Culture Care Theory of Diversity and Universality
- Defined transcultural nursing as “a substantive area of study and practice focused on comparative cultural care (caring) values, beliefs, and practices of individuals or groups of similar or different cultures to provide culture-specific and universal nursing care practices in promoting health or well-being or to help people to face unfavorable human conditions, illness, or death in culturally meaningful ways.”
- Involves learning and understanding various cultures regarding nursing and health-illness caring practices, beliefs, and values to implement significant and efficient nursing care services to people according to their cultural values and health-illness context.
- It focuses on the fact that various cultures have different and unique caring behaviors and different health and illness values, beliefs, and patterns of behaviors.
- Health as Expanding Consciousness
- “Nursing is the process of recognizing the patient in relation to the environment, and it is the process of the understanding of consciousness.”
- “The theory of health as expanding consciousness was stimulated by concern for those for whom health as the absence of disease or disability is not possible . . . “
- Nursing is regarded as a connection between the nurse and patient, and both grow in the sense of higher levels of consciousness.
- Human Becoming Theory
- “Nursing is a science, and the performing art of nursing is practiced in relationships with persons (individuals, groups, and communities) in their processes of becoming.”
- Explains that a person is more than the sum of the parts, the environment, and the person is inseparable and that nursing is a human science and art that uses an abstract body of knowledge to help people.
- It centered around three themes: meaning, rhythmicity, and transcendence.
- Modeling and Role-Modeling
- “Nursing is the holistic helping of persons with their self-care activities in relation to their health . . . The goal is to achieve a state of perceived optimum health and contentment.”
- Modeling is a process that allows nurses to understand the unique perspective of a client and learn to appreciate its importance.
- Role-modeling occurs when the nurse plans and implements interventions that are unique for the client.
- Created the Symphonological Bioethical Theory
- “Symphonology (from ‘ symphonia ,’ a Greek word meaning agreement) is a system of ethics based on the terms and preconditions of an agreement.”
- Nursing cannot occur without both nurse and patient. “A nurse takes no actions that are not interactions.”
- Founded on the singular concept of human rights, the essential agreement of non-aggression among rational people forms the foundation of all human interaction.
- Maternal Role Attainment—Becoming a Mother
- “Nursing is a dynamic profession with three major foci: health promotion and prevention of illness, providing care for those who need professional assistance to achieve their optimal level of health and functioning, and research to enhance the knowledge base for providing excellent nursing care.”
- “Nurses are the health professionals having the most sustained and intense interaction with women in the maternity cycle.”
- Maternal role attainment is an interactional and developmental process occurring over time. The mother becomes attached to her infant, acquires competence in the caretaking tasks involved in the role, and expresses pleasure and gratification. (Mercer, 1986).
- Provides proper health care interventions for nontraditional mothers for them to favorably adopt a strong maternal identity.
- Uncertainty in Illness Theory
- Presents a comprehensive structure to view the experience of acute and chronic illness and organize nursing interventions to promote optimal adjustment.
- Describes how individuals form meaning from illness-related situations.
- The original theory’s concepts were organized in a linear model around the following three major themes: Antecedents of uncertainty, Process of uncertainty appraisal, and Coping with uncertainty.
- Self-Transcendence Theory
- Self-transcendence refers to the fluctuation of perceived boundaries that extend the person (or self) beyond the immediate and constricted views of self and the world (Reed, 1997).
- Has three basic concepts: vulnerability, self-transcendence, and well-being.
- Gives insight into the developmental nature of humans associated with health circumstances connected to nursing care.
- Theory of Illness Trajectory
- “The uncertainty surrounding a chronic illness like cancer is the uncertainty of life writ large. By listening to those who are tolerating this exaggerated uncertainty, we can learn much about the trajectory of living.”
- Provides a framework for nurses to understand how cancer patients stand uncertainty manifested as a loss of control.
- Provides new knowledge on how patients and families endure uncertainty and work strategically to reduce uncertainty through a dynamic flow of illness events, treatment situations, and varied players involved in care organization.
- Theory of Chronic Sorrow
- “Chronic sorrow is the presence of pervasive grief -related feelings that have been found to occur periodically throughout the lives of individuals with chronic health conditions, their family caregivers and the bereaved.”
- This middle-range theory defines the aspect of chronic sorrow as a normal response to the ongoing disparity created by the loss.
- Barker’s Tidal Model of Mental Health Recovery is widely used in mental health nursing.
- It focuses on nursing’s fundamental care processes, is universally applicable, and is a practical guide for psychiatry and mental health nursing.
- Draws on values about relating to people and help others in their moments of distress. The values of the Tidal Model are revealed in the Ten Commitments: Value the voice, Respect the language, Develop genuine curiosity, Become the apprentice, Use the available toolkit, Craft the step beyond, Give the gift of time, Reveal personal wisdom, Know that change is constant, and Be transparent.
- Theory of Comfort
- “Comfort is an antidote to the stressors inherent in health care situations today, and when comfort is enhanced, patients and families are strengthened for the tasks ahead. Also, nurses feel more satisfied with the care they are giving.”
- Patient comfort exists in three forms: relief, ease, and transcendence. These comforts can occur in four contexts: physical, psychospiritual, environmental, and sociocultural.
- As a patient’s comfort needs change, the nurse’s interventions change, as well.
- Postpartum Depression Theory
- “The birth of a baby is an occasion for joy—or so the saying goes […] But for some women, joy is not an option.”
- Described nursing as a caring profession with caring obligations to persons we care for, students, and each other.
- Provides evidence to understand and prevent postpartum depression .
- Theory of Caring
- “Caring is a nurturing way of relating to a valued other toward whom one feels a personal sense of commitment and responsibility.”
- Defines nursing as informed caring for the well-being of others.
- Offers a structure for improving up-to-date nursing practice, education, and research while bringing the discipline to its traditional values and caring-healing roots.
- Peaceful End-of-Life Theory
- The focus was not on death itself but on providing a peaceful and meaningful living in the time that remained for patients and their significant others.
- The purpose was to reflect the complexity involved in caring for terminally ill patients.
- Also known as Wanda Horta, she introduced the concepts of nursing that are accepted in Brazil.
- Wrote the book Nursing Process which presents relevance to the various fields of Nursing practice for providing a holistic view of the patient.
- Her work was recognized in all the teaching institutions called the Theory of Basic Human Needs . It is based on Maslow’s Theory of Human Motivation, whose primary concept is the hierarchy of Basic Human Needs (BHN).
- Horta’s Theory of Basic Human Needs is considered the highest point of her work, and the summary of all her research concludes sickness as a science and art of assisting a human being in meeting basic human needs, making the patient independent of this assistance through education in recovery, maintenance, and health promotion .
- Classified basic human needs into three main dimensions – psychobiological, psychosocial and psychospiritual – and establishes a relationship between the concepts of human being, environment, and nursing.
- The theory describes nursing as an element of a healthcare team and states that it can function efficiently through a scientific method. Horta referred this method as the nursing process .
- She defined the nursing process as the dynamics of systematic and interrelated actions to assist human beings. It is characterized by six phases: nursing history, nursing diagnosis , assistance plan, care plan or nursing prescription, evolution, and prognosis.
Recommended books and resources to learn more about nursing theory:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
- Nursing Theorists and Their Work (10th Edition) by Alligood Nursing Theorists and Their Work, 10th Edition provides a clear, in-depth look at nursing theories of historical and international significance. Each chapter presents a key nursing theory or philosophy, showing how systematic theoretical evidence can enhance decision making, professionalism, and quality of care.
- Knowledge Development in Nursing: Theory and Process (11th Edition) Use the five patterns of knowing to help you develop sound clinical judgment. This edition reflects the latest thinking in nursing knowledge development and adds emphasis to real-world application. The content in this edition aligns with the new 2021 AACN Essentials for Nursing Education.
- Nursing Knowledge and Theory Innovation, Second Edition: Advancing the Science of Practice (2nd Edition) This text for graduate-level nursing students focuses on the science and philosophy of nursing knowledge development. It is distinguished by its focus on practical applications of theory for scholarly, evidence-based approaches. The second edition features important updates and a reorganization of information to better highlight the roles of theory and major philosophical perspectives.
- Nursing Theories and Nursing Practice (5th Edition) The only nursing research and theory book with primary works by the original theorists. Explore the historical and contemporary theories that are the foundation of nursing practice today. The 5th Edition, continues to meet the needs of today’s students with an expanded focus on the middle range theories and practice models.
- Strategies for Theory Construction in Nursing (6th Edition) The clearest, most useful introduction to theory development methods. Reflecting vast changes in nursing practice, it covers advances both in theory development and in strategies for concept, statement, and theory development. It also builds further connections between nursing theory and evidence-based practice.
- Middle Range Theory for Nursing (4th Edition) This nursing book’s ability to break down complex ideas is part of what made this book a three-time recipient of the AJN Book of the Year award. This edition includes five completely new chapters of content essential for nursing books. New exemplars linking middle range theory to advanced nursing practice make it even more useful and expand the content to make it better.
- Nursing Research: Methods and Critical Appraisal for Evidence-Based Practice This book offers balanced coverage of both qualitative and quantitative research methodologies. This edition features new content on trending topics, including the Next-Generation NCLEX® Exam (NGN).
- Nursing Research (11th Edition) AJN award-winning authors Denise Polit and Cheryl Beck detail the latest methodologic innovations in nursing, medicine, and the social sciences. The updated 11th Edition adds two new chapters designed to help students ensure the accuracy and effectiveness of research methods. Extensively revised content throughout strengthens students’ ability to locate and rank clinical evidence.
Recommended site resources related to nursing theory:
- Nursing Theories and Theorists: The Definitive Guide for Nurses MUST READ! In this guide for nursing theories, we aim to help you understand what comprises a nursing theory and its importance, purpose, history, types or classifications, and give you an overview through summaries of selected nursing theories.
Other resources related to nursing theory:
- Betty Neuman: Neuman Systems Model
- Dorothea Orem: Self-Care Deficit Theory
- Dorothy Johnson: Behavioral System Model
- Faye Abdellah: 21 Nursing Problems Theory
- Florence Nightingale: Environmental Theory
- Hildegard Peplau: Interpersonal Relations Theory
- Ida Jean Orlando: Deliberative Nursing Process Theory
- Imogene King: Theory of Goal Attainment
- Jean Watson: Theory of Human Caring
- Lydia Hall: Care, Cure, Core Nursing Theory
- Madeleine Leininger: Transcultural Nursing Theory
- Martha Rogers: Science of Unitary Human Beings
- Myra Estrin Levine: The Conservation Model of Nursing
- Nola Pender: Health Promotion Model
- Sister Callista Roy: Adaptation Model of Nursing
- Virginia Henderson: Nursing Need Theory
Suggested readings and resources for this study guide :
- Alligood, M., & Tomey, A. (2010). Nursing theorists and their work, seventh edition (No ed.). Maryland Heights: Mosby-Elsevier.
- Alligood, M. R. (2017). Nursing Theorists and Their Work-E-Book . Elsevier Health Sciences.
- Barnard, K. E. (1984). Nursing research related to infants and young children. In Annual review of nursing research (pp. 3-25). Springer, Berlin, Heidelberg.
- Brown, H. I. (1979). Perception, theory, and commitment: The new philosophy of science . University of Chicago Press. [ Link ]
- Brown M (1964) Research in the development of nursing theory: the importance of a theoretical framework in nursing research. Nursing Research.
- Camacho, A. C. L. F., & Joaquim, F. L. (2017). Reflections based on Wanda Horta on the basic instruments of nursing. Rev Enferm UFPE [Internet], 11(12), 5432-8.
- Chinn, P. L., & Jacobs, M. K. (1978). A model for theory development in nursing. Advances in Nursing Science , 1 (1), 1-12. [ Link ]
- Colley, S. (2003). Nursing theory: its importance to practice. Nursing Standard (through 2013), 17(46), 33. [ Link ]
- Fawcett, J. (2005). Criteria for evaluation of theory. Nursing science quarterly, 18(2), 131-135. [ Link ]
- Fitzpatrick, J. J., & Whall, A. L. (Eds.). (1996). Conceptual models of nursing: Analysis and application . Connecticut, Norwalk: Appleton & Lange.
- Kaplan, A. (2017). The conduct of inquiry: Methodology for behavioural science . Routledge. [ Link ]
- Meleis, A. I. (2011). Theoretical nursing: Development and progress . Lippincott Williams & Wilkins.
- Neuman, B. M., & Fawcett, J. (2002). The Neuman systems model .
- Nightingale F (1860) Notes on Nursing. New York NY, Appleton.
- Perão, O. F., Zandonadi, G. C., Rodríguez, A. H., Fontes, M. S., Nascimento, E. L. P., & Santos, E. K. A. (2017). Patient safety in an intensive care unit according to Wanda Horta’s theory. Cogitare Enfermagem, 22(3), e45657.
- Peplau H (1988) The art and science of nursing: similarities, differences, and relations. Nursing Science Quarterly
- Rogers M (1970) An Introduction to the Theoretical Basis of Nursing. Philadelphia PA, FA Davis.
52 thoughts on “Nursing Theories and Theorists: The Definitive Guide for Nurses”
Great work indeed
Amazing and simple post I have ever come across about nursing theories.
Thank you for the simplicity
where do i find the reference page in apa format?
The reference listed below the article is in APA format.
i love this. insightful. Comprehensive ,Well researched .
Thank you for these theories they are a life saver and simplified. My school require us to write about 2 nursing theorist from memory for a Comprehensive exam in which if you do not pass it you are required to wait for a year to retake the exam.
Merci beaucoup, puisque je suis très satisfait.
I’m pleased to congratulate you about your work! I really appreciate it! From: Cameroon
An entire’s semester worth of a nursing theory class, expertly and succinctly summarized in one paper. I wish my instructor were as easy to understand. Good work.
I thought this was in a chronological order based on their published works date? Then why Orlando’s theory comes at the later part? Can someone englighten me please because I am making a timeline for our project.
Great job. Very clear and succinct.
I like it. Well explained!
easy to understand and very helpful
thankyou very much.
The article was beneficial to me to understand nursing theories
This is amazing and I love it so enriching!
Thanks for the article may God bless you more Plus More Power and Protection
Thanks so much
Please can someone help me with a nursing theory related to “teamwork” please
Thank you so much !
I loved the text and saw that the nursing theorist Wanda Aguiar Horta, a Brazilian nurse and great theorist regarding basic human needs, was not included.
I suggest reviewing and including it to be more complete.
If you need, I can help with inclusion!
Best Regards
Hi João Carlos, we’d love to hear about her work. Please send us the details via our contact page: https://nurseslabs.com/contact/
Excellent study guide! Detailed, Informative and Valued! Thank you!
hi can someone help me which theorist can relate in Ear, Nose, Throat nursing care.
Wonderful contribution of shared knowledge- now how do we get the word out for nurses that are not able to afford a BSN?
Thanks for the work. It’s very helpful
This has helped me understand theories a bit better, however, there is one that is eluding me. Where does the normative theory fit in?
very educative.I have understood theories more than before.Thanks
hard work. great work in deed
I love reading your material, plain concise and easy
Very informative, more knowledgeable about the theorist
Thank you for your information. This material is great and when I have looked for material for nursing theory. I got is material with complete
A big hand of applause 👏🏿 This is a treasure for nurses of the world. Thank you so much
Hi G. ALex,
Wow, thanks for the awesome feedback! 😊 Super glad you found it to be a treasure. Just curious, was there a particular section that stood out to you or something you’d love to see more of? Always keen to hear what resonates with fellow nurses!
This is really hard work put together in a very easy to understand way.Thank you so much.It came handy
Hi Sigala, Thanks a ton for noticing the effort! 😊 Super happy to hear it came in handy for you. If you ever have suggestions or topics you’d like to see, give me a shout. Cheers to making things understandable!
Absolutely helpful. Thank you.
So glad to hear the nursing theories guide was a hit for you! 😊 If you have any other topics or questions in mind, just give a shout. Always here to help. Keep rocking your studies! Thanks Ishe!
Am happy, to read these theories, very educating. Am going to make use of it when caring for my patients. GREAT NURSES GREAT! I LOVE YOU ALL.
Hi Eboh, I’m thrilled to hear you’re excited about applying these nursing theories in practice! They can really enhance the care we provide. It’s all about putting that knowledge to good use. By the way, which theory resonated with you the most, or which do you see being most applicable in your day-to-day patient care?
How do I relate one of the theories to effective management of intravenous lines? Which theory and how to relate to the above?
Hi wanted to ask you who wrote this page who is the autor because i need to write them on footnotes and i can’t find autor of the page,neither the year it was published. Thank you. Btw this article was really helpful i never understood nursing theories this good.
Hey there Innaya, I’m glad to hear the article on nursing theories was so helpful to you! Here’s how you can cite it in APA format:
Vera, M. (2019, September 11). Nursing Theories and Theorists: The Definitive Guide for Nurses Nurseslabs. https://nurseslabs.com/nursing-theories/
If you need any more help with citations or have other questions, feel free to ask. Happy to assist!
Please is there an app I could download all these from?
Hi Felicia, Thanks for your interest! As of now, we don’t have a dedicated app for downloading our content. However, our website is mobile-friendly, so you can easily access all our resources from your smartphone or tablet browser.
wonderful insights, and very precise and easy to understand, I even got to know and learn about other new theorists of Nursing I didn’t know before.
Thank you so much for this wonderful work.
Its so amazing and very helpful. Please how can I cite any of these theory using Vancouver?
thanls for good informatiom need to explain example
Great!. Useful information to the lecturers, and educators toward delivery info to our young generation nursing.
So detailed 👌🏽 I love it
Leave a Comment Cancel reply
How to Conclude a nursing essay [Nursing Essay Conclusion + Examples]
- Dr. Wilson MN
- August 11, 2022
- Essay Topics and Ideas , Nursing
What You'll Learn
Nursing Essay Conclusion
Writing a Nursing essay conclusion can be one of the most daunting tasks for a nursing student, but with the right format and structure, it can be easily completed.
As you continue, thestudycorp.com has the top and most qualified writers to help with any of your assignments. All you need to do is place an order with us.
There are a few things to keep in mind when writing the conclusion of your nursing essay. First and foremost, you want to make sure that your essay is well-written and engaging; second, you want to make sure that your conclusions reflect the main points of your essay.nnHere are a few tips for writing an effective conclusion: – Be concise: The conclusion of your Nursing Essay should be a concise summary of the key points made in the body of your essay. – Use strong verbs: Conclusions should be written in active, compelling language that grabs readers’ attention. Use strong verbs to capture the reader’s attention and ensure that they stay engaged throughout the essay.
Here’s how to How to Start a Nursing Essay [Nursing Essay Introduction] – Focus on key ideas: The conclusion should focus on key ideas introduced in the body of your essay . Keep your conclusions short and to the point, so that readers can quickly understand what you’ve been saying.
– Tie everything together: The conclusion of your Nursing Essay should provide a clear, cohesive narrative that ties everything together. Try to use a few key images or examples to illustrate your points.
Here are 100+ Excellent Nursing Informatics essay Topics [+Outline]
By following these tips, you can write an effective conclusion to your Nursing Essay .
In order to write a conclusion that is both engaging and informative, follow these tips.
- Tie your key points together. Summarize your main points and how they support your thesis statement .
- Be concise. A good conclusion should not be wordy or overwhelming. Keep it to around 150 words.
- Move the reader forward. Use strong verbs and images to convey your point of view and move the reader forward in the essay by providing a sense of closure or hope for the future.
- Keep it simple. Use concrete examples and analogies to help explain complex concepts.
- End with a hook. Leave readers wanting more, whether that means offering solutions or recommending resources for further learning.
- Proofread and edit your work. Make sure that all grammar and spelling are correct, and that the flow of your essay is clear.
- Here are 100+ Strong Persuasive Nursing Essay Topics Ideas [+Outline]
Nursing Essay Conclusion Example
Concept analysis is a crucial tool for evaluating and determining essential healthcare concepts. Through concept analysis , the study defines CHC as a healthcare agency actively engaging in healthcare services and collaborating with the host community to provide comprehensive and integrated health services founded on primary healthcare principles that mitigate existing health issues, addressing the causal factors for the community. The study uses the 8-step process developed by Walker and Avant to define and characterize community health centers, providing meaning and attributes crucial for scientific research, policymaking, and healthcare interventions.
Nursing Essay Examples
The introduction of university education for nurses has enabled nurses to keep up to date with medical advances. It has changed their roles both in the hospital and community settings and has led to the increase in power they now enjoy. Their working conditions and wages have improved as they have been seen in this more professional standing. Nurses’ ability to assess and evaluate patients has also improved but their ability to provide empathetic and understanding care has diminished as a result to the strong theory base that university education is centred on.
The conclusion could also be improved by ending with a broad summary of the impacts in the same order as in the Body. It could also suggest where university education is taking nursing as a profession.
Here’s an example of a Family Health Assessment Part 2 Paper
Clinical Action Plan: Community Health Plan (Health Education Action Plan)
Start by filling this short order form order.studyinghq.com
And then follow the progressive flow.
Having an issue, chat with us here
Cathy, CS.
New Concept ? Let a subject expert write your paper for You
Yet to start your paper have a subject expert write for you now, already began delegate the remaining part to our professional writers, need some edits and proofreading, test our paper writing service for less.
📕 Studying HQ
Typically replies within minutes
Hey! 👋 Need help with an assignment?
🟢 Online | Privacy policy
WhatsApp us
What is the Nursing Code of Ethics?
- 4 Ethical Principles in Nursing
Nursing Code of Ethics Interpretive Statements
Making ethical decisions as a nurse, history of the nursing code of ethics, how nurses use the nursing code of ethics.

According to the American Nurses Association (ANA) , the nursing code of ethics is a guide for “carrying out nursing responsibilities in a manner consistent with quality in nursing care and the ethical obligations of the profession.”
Ethics, in general, are the moral principles that dictate how a person will conduct themselves. Ethical values are essential for ALL healthcare workers, but ethical principles in nursing are particularly important given their role as caregivers.
There are 4 main principles of the nursing code of ethics:
- Beneficence
- Non-maleficence
These principles are ideally what every nurse should be aware of in their daily nursing practice. While ethical principles are sometimes confusing and often taught briefly during undergraduate nursing -- they should be constants in nursing practice in order to provide the best, safest, and most humane care to all patients.
Popular Online Master of Science in Nursing (MSN) Programs

GCU's College of Nursing and Health Care Professions has a nearly 35-year tradition of preparing students to fill evolving healthcare roles as highly qualified professionals. GCU offers a full spectrum of nursing degrees, from a pre-licensure BSN degree to a Doctor of Nursing Practice (DNP) program.
Enrollment: Nationwide
- MSN - Family NP
- MSN - Adult Gerontology Acute Care NP
- MSN - Nursing Education
- MSN - Health Informatics
- MSN - Public Health Nursing
- MSN - Health Care Quality & Patient Safety
- MBA & MSN - Nursing Leadership in Health Care Systems
- See more GCU nursing programs

WGU's award-winning online programs are created to help you succeed while graduating faster and with less debt. WGU is a CCNE accredited, nonprofit university offering nursing bachelor's and master's degrees.
- BSN-to-MSN - Family NP
- BSN-to-MSN - Psychiatric Mental Health NP
- BSN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Education
- RN-to-MSN - Nursing Leadership & Management
Enrollment: Nationwide, excluding NY, RI and CT. Certain programs have additional state restrictions. Check with Walden for details.
- MSN - Psychiatric-Mental Health NP
- MSN - Adult/Gerontology Acute Care NP
- MSN - Adult/Gerontology Primary Care NP
- MSN - Pediatric NP - Primary Care
- MSN - Nursing Informatics

As a working RN, you need a flexible, transfer-friendly program to help you save time and money as you take the next step in your nursing career. In our CCNE-accredited4 RN to BSN program, you can transfer in up to 134 credits—which is nearly 75% of program requirements. Your transfer credits can be reviewed in one business day (on average).
Enrollment: FL
- MSN - Adult-Gerontology NP - Primary Care
- MSN - Nursing Leadership & Admin
- MSN - Healthcare Tech, Simulation & Informatics
- See more Rasmussen nursing programs
4 Ethical Principles in Nursing
1. autonomy .
Autonomy in nursing is recognizing each individual patient’s right to self-determination and decision-making. As patient advocates, it is imperative that nurses ensure that patients receive all medical information, education, and options in order to choose the option that is best for them. This includes all potential risks, benefits, and complications to make well-informed decisions.
Once the patient has all the relevant information, the medical and nursing team can make a plan of care in compliance with the medical wishes of the patient.
It is important that nurses support the patient in their medical wishes and ensure that the medical team is remembering those wishes. Sometimes, nurses will need to continue to advocate for a patient despite the wishes being verbalized because the medical team might not agree with those wishes.
Many factors may influence a patient's acceptance or refusal of medical treatment, such as culture, age, gender, sexual orientation, general health, and social support system.
2. Beneficence
Beneficence in nursing is acting for the good and welfare of others and including such attributes as kindness and charity. The American Nurses Association defines this as “actions guided by compassion.”
Justice is that there should be an element of fairness in all medical and nursing decisions and care. Nurses must care for all patients with the same level of fairness despite the individual's financial abilities, race, religion, gender, and/or sexual orientation.
An example of this is when working at a free flu clinic or diabetes screening clinic. These are open to all individuals in the community regardless of the previously mentioned factors.
4. Nonmaleficence
Nonmaleficence is to do no harm. This is the most well-known of the main principles of nursing ethics. More specifically, it is selecting interventions and care that will cause the least amount of harm to achieve a beneficial outcome
The principle of nonmaleficence ensures the safety of the patient and community in all care delivery. Nurses are also responsible for reporting treatment options that are causing significant harm to a patient, which may include suicidal or homicidal ideations.
Popular Online RN-to-BSN Programs

At Purdue Global, discover a faster, more affordable way to earn your Nursing degree. Purdue Global is committed to keeping your tuition costs as low as possible and helping you find the most efficient path to your degree.
Enrollment: Nationwide, but certain programs have state restrictions. Check with Purdue for details.
- RN-to-BSN - ExcelTrack
Revised in 2015 to include 9 provisions, the ANA’s nursing code of ethics now includes interpretative statements that can provide more specific guidance for nursing practice.
9 Provisions of the Nursing Code of Ethics
Currently, the nurse’s code of ethics contains 9 main provisions:
- The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
- The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population.
- The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
- The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes action consistent with the obligation to provide optimal patient care.
- The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
- The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
- The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
- The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
- The profession of nursing, collectively through its professional organization, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
The nine provisions were implemented to help guide nurses in ethical decision-making throughout their practice.
Unfortunately, nurses are often unable to make complex ethical decisions based solely on the four principles and nine provisions. In these instances, it is important to consult the ethics committee before making any major decisions. Often, other resources are needed when making major ethical decisions.
Interestingly, the nursing code of ethics is suggested to have been founded in 1893 and named the “Nightingale Pledge” after Florence Nightingale , the founder of modern nursing. As a modification of the Hippocratic Oath, taken by medical doctors, the Nightingale Pledge has been recited by nursing students at graduations with little changes since inception.
The formal code of ethics was developed in the 1950s by the American Nurses Association (ANA) and has undergone numerous modifications since. The most significant recent change was in 2015 when 9 interpretative statements or provisions were added to the code of ethics to help guide nursing practice in a more definitive way.
Many states include the ANA’s nursing code of ethics in their practice statements. Even though the code of ethics is primarily ethics-related, it also has legal implications. Given the importance of the code to the nursing profession, revisions continue on a regular basis.
Knowing the nursing code of ethics is essential for nurses because it will help guide everyday practice and navigate the daily complexities of the healthcare profession. Nurses often use the four major ethical principles throughout a shift, even if not fully aware of them.
This may include,
- Providing pain medication to a post-operative hip replacement
- Holding the hand of a dying patient who is alone
- Advocating for the patient that wants to end chemotherapy and enter hospice care
Nursing is consistently regarded as the most honest and ethical profession and practicing with the nursing code of ethics is essential to ensuring that patients and their families receive the care they have come to know and expect. Utilizing the ethical codes of justice, nonmaleficence, autonomy, and beneficence on a daily basis allows nurses to provide the safest and most compassionate care for their patients.
What are the five codes of ethics in nursing?
- The 5 nursing ethic codes are: nonmaleficence, beneficence, autonomy, justice, and privacy/confidentiality.

What is the Professional Code of Ethics for Nurses?
- The Professional Code of Ethics for Nurses is the guiding outline for how nurses should behave ethically within their profession and how they should decide to act if they encounter barriers that prevent them from fulfilling their professional obligations.
Why is the code of ethics important in nursing?
- It can guide nurses’ professional behavior, provide a framework for decision-making when faced with challenges, and provide support and help prevent moral distress.
What is the code of ethics in healthcare?
- There is not one board ethical code for every healthcare professional, although it has been proposed. Instead, each branch of healthcare, from quality control to medical directors to physicians to nursing, has its own ethical codes.
What is scholarly ethics in nursing?
Find nursing programs.

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.45(1); 2022

Interpretation of the concept ‘nursing’: Utilisation in nursing education and practice
Sundira d. mottian.
1 Department of Health Studies, College of Human Sciences, University of South Africa, Pretoria, South Africa
Lizeth Roets
Kefiloe a. maboe, associated data.
The raw data is available from the corresponding author at moc.liamg@tcellocatadasinu .
Nursing developed over centuries. Changing practice and education influenced its interpretation and understanding. Its meaning and interpretation may differ amongst education institutions, nurse educators and nurses, particularly student nurses.
The objective was to develop a visual concept map of the concept of ‘nursing’, allowing nursing education institutions to have a similar approach and understanding in teaching the concept to student nurses.
The research design was qualitative, explorative, descriptive and contextual. A self-designed, pretested online questionnaire collected data from various categories of nurse participants. An integrative review viewed literature sources published between 2006 and 2016 accessing definitions of ‘nursing’. Data analysis involved thematic analysis of narrative data, data coding processes, interpretation and synthesis of data and further analysis using a systematic concept analysis process. The combined analysed data merged, developing a visual concept map of ‘nursing’. Expert nurse educators validated the visual concept map of ‘nursing’ by e-Delphi technique, using an assessment rubric.
Various definitions of ‘nursing’ revealed identified themes and categories underpinning the concept. After formulation of connotative, denotative definitions and empirical referents, a visual concept map of ‘nursing’ was developed and validated to be an educational tool to facilitate the teaching of the concept of ‘nursing’, enhancing a similar understanding and interpretation thereof.
A visual concept map of ‘nursing’, a tool facilitating teaching the concept and promoting similar understanding of its meaning is valuable in an evolving digital era, where visual stimulation enhances teaching and learning.
Contribution
The primary contribution of the manuscript provided a developed visual concept map of ‘nursing’, to use as a tool to stimulate critical thinking and integrate the various aspects outlined in the map. The visual concept map of ‘nursing’ assists in the education and training of all categories of nurses in the profession, especially student nurses, aiming to support better patient outcomes when the concept of nursing is understood and interpreted in the same way.
Introduction
Literature sources express various definitions of the concept of ‘nursing’. Florence Nightingale in the 19th century defined nursing as: ‘putting the patient in the best condition for nature to act upon him’ (Nightingale 1860 :133). In the 20th century, other definitions were: ‘nursing is a process that was serial and goal-directed demanding certain steps, actions, operations or performances that occurred between the nurse and the person who was nursed’ (Peplau 1952 ). Nursing was also defined as ‘to assist the individual, sick or well, in the performance of those activities contributing to health or its recovery (or a peaceful death)’ (Henderson 1964 ).
More recent definitions of ‘nursing’ are:
The use of clinical judgment in the provision of care to enable people to improve, maintain, or recover health, to cope with health problems, and to achieve the best possible quality of life, in the case of disease or disability, until death. (Royal College of Nursing 2003 :3)
The South African nursing regulatory body, namely the South African Nursing Council (SANC), define nursing as:
[ A ] caring profession practiced by a person registered with the SANC, who supports, cares for and treats a healthcare user to achieve or maintain health. Where this is not possible, a nursing professional cares for a healthcare user so that they live in comfort and with dignity until death. (SANC Nursing Act 2005 :6)
The International Council of Nurses ( 2002 ) expresses nursing as:
[ N ]ursing includes the promotion of health, prevention of illness, and care of the sick, disabled and dying people, advocacy, promotion of a safe environment, research, participation in shaping health policy and in patient and health systems’ management. Nursing is about the privilege of being able to share in the joys and sorrows of people’s lives and making a difference. It is empowering people to make decisions about their health, birth and death and supporting them in their choices. Nursing is about talking, teaching, touching, smiling and crying. Nursing is caring. (Howie & Robertson 2017 :i)
Over the years, with the evolution of nursing, the definitions of nursing have transformed. The definition expanded with advancement in technology and science. In view of this, the SANC, a statutory body governing the practice of nursing in South Africa, provides a definition of nursing encompassed in Act No. 33 of 2005 : Nursing Act, 2005 . It can be suggested that since nurses and nurse educators are being guided by legislative entities, revisiting the definition should be considered, taking into account the radical evolution of nursing practice. However, on the contrary, arguably the definition of nursing provided by the SANC may be considered a standardising definition, as nursing will always require basic care rendered to the healthcare user despite all the advancement in technology and science. Therapeutic care is required despite working with complex technology. Much of the nurses’ work still involves everyday domestic tasks, emotional support and environmental control. Nurses have to feed patients, bathe them, ensure beds are made with fresh linen, open windows for fresh air and comfort those who need reassurance (Keeling, Hehman & Kirchgessner 2018 :160).
The various definitions of ‘nursing’ create an opening for individual nurses and nurse educators to have a different understanding and interpretation of the concept. The different interpretations of the concept of ‘nursing’ influence the way in which nurses think about what nursing actually entails and seemingly affects the outcome of nursing care provided to the healthcare consumers. The foundation of how nursing is practised stems from the interpretation and understanding of what nursing means. A similar understanding and interpretation of the concept ultimately reduces the healthcare consumer’s exposure to risk of harm when under the care of nurses. The concept map of ‘nursing’ will be a guideline, utilised by nurse educators when teaching the concept of ‘nursing’. This tool will facilitate a common interpretation and understanding of the concept, thus promoting the practice of nursing in the same way to benefit all healthcare consumers when the key attributes of the concept are implemented clinically.
The study aimed to develop a visual concept map of ‘nursing’, a tool to facilitate nurse educators during the teaching of the concept of ‘nursing’. The concept map is a benchmark to promote the similar understanding, meaning and interpretation of ‘nursing’, thereby ensuring the practice of nursing in the same way when the key attributes of the concept are expressed when in contact with the healthcare consumers.
Theoretical framework
The theoretical framework adopted was Wilson’s method of concept analysis (1963), which was revised to an eight-step concept analysis process by Walker and Avant ( 2011 ). Concept analysis is a strategy that identifies a set of characteristics essential to defining the connotative meaning of a concept (Gray & Grove 2020 :173). The eight steps of the concept analysis process were: (1) select a concept, (2) determine the aims or purposes of analysis, (3) identify all uses of the concept, (4) determine the defining attributes, (5) identify a model case, (6) identify a contrary case, (7) identify antecedents and consequence and (8) define empirical referents. These systematic steps facilitated the critical analysis of the meaning and interpretation of the concept of ‘nursing’ and promoted clarification of its meaning.
Research methods and design
The objectives of the study were to: (1) explain the meaning and interpretation of the definition of ‘nursing’ from different categories of nurses registered with SANC and as members of Democratic Nursing Organisation of South Africa (DENOSA); (2) provide evidence for the development of a visual concept map that can be utilised by nursing education institutions in teaching the concept.
Research design
A qualitative, explorative, descriptive and contextual approach facilitated detailed analysis of the concept of ‘nursing’ and the development of the visual concept map of ‘nursing’. Figure 1 illustrates the research phases.

Research phases.
Setting and population
The study was conducted in four phases. The setting and population for each phase were as follows: Phase 1 included nurse participants from various categories who were registered with SANC and were members of DENOSA, a total of 84 000 (DENOSA 2022 :1). In Phase 2, the integrative review, the population comprised any online or hard copies of English books, encyclopaedias, journals, newspaper articles, published and unpublished theses and articles, from any discipline containing the definition of ‘nursing’, published between 2006 and 2016. Phase 3 included gathered data from Phases 1 and 2, and finally in Phase 4, the nurse educators inaugurated in Sigma Theta Tau International (STTI), the Africa Region Chapters (Tau Lambda at-Large, Chi Omicron at-Large and Chi Xi at-Large Chapters), formed the setting and the population.
The study followed a nonrandom sampling approach. A selected heterogeneous sample (nurses), n = 415, formed the sample for Phase 1, in which participants took an online survey. Various literature sources specifically chosen with publication from 2006 to 2016 were the sample in Phase 2. An all-inclusive sampling during Phase 3 developed the concept map of ‘nursing’ using all data collected from Phases 1 and 2. Phase 4 sampling included specifically chosen nurse educators, directly involved in updating and improving nursing and nursing education within Africa and teaching the concept of ‘nursing’ to student nurses.
Data collection
Data were collected from 19 March 2017 to 19 June 2017. An online pretested questionnaire via SurveyMonkey™ (Momentive, Inc., San Mateo, California, United States) facilitated data collection in Phase 1. An invitation recruitment letter, including a web link address ( https://forms.gle/oovijxebU2ueAp7X6 ) to access the online questionnaire was sent to all nurses registered on the DENOSA database. Participants voluntarily clicked on the web link address accessing the online questionnaire, and on clicking the ‘NEXT’ button, they voluntarily agreed to participation to the study. Questionnaire completion was over a period of three months, with reminder e-mails sent fortnightly. All ethical considerations related to informed consent, participation, confidentiality and anonymity were applied. During Phase 2, an integrative review pursued consulting related literature sources from 2006 to 2016, with definitions of ‘nursing’. The merged data from Phases 1 and 2 resulted in the development of a visual concept map of nursing in Phase 3. Finally, in Phase 4, the heads of department of schools of nursing of universities belonging to Africa Region Chapters of STTI were e-mailed, requesting three randomly selected nurse educators inaugurated in STTI to participate in the validation process of the visual concept map of ‘nursing’. Participants responded to the e-mail request and invitation, implying acceptance to participation. The visual concept map of nursing, the assessment rubric (see Figure 2 ) and instructions for its use were accessed by participants via a web link address.

Validation assessment rubric (Bartels 1995 :545).
Data analysis
Data from 415 questionnaires were analysed using the SurveyMonkey™ data analysis software. Participants’ demographic data were not fundamental to the study; however, their context could enhance transferability of data to similar context. Data from the open-ended questions related to participants’ input on the concept of ‘nursing’ followed thematic analysis of the narrative data, which was coded according to Tesch’s ( 1992 ) coding guidelines.
The integrative review and data analysis used step 4 of integrative reviews, interpretation and synthesis of the data, outlined by Whittemore and Knafl ( 2005 :550–551). Further analysis of the data included the adapted eight-step concept analysis process by Walker and Avant ( 2011 ).
The combined analysed data from Phases 1 and 2 formulated a visual concept map of nursing arranged in a spider map style, following Novak and Canas’s ( 2006 :1–2) steps to develop a concept map.
Finally, the developed visual concept map of nursing was validated by seven experts in nursing education, using an e-Delphi technique during two rounds of validation when over 75% consensus was reached between participants. An assessment rubric by Bartels ( 1995 :545), outlined in Figure 2 , facilitated the validation process.
Ethical considerations
Ethical approval to conduct this study was obtained from the University of South Africa Health Studies Higher Degrees Committee College of Human Sciences (ref. no. HSHDC/486/2015, REC-012714-039).
After data coding and analysis, emerged categories were (1) ‘altruism’, (2) ‘caring holistically’, (3) ‘cognitive abilities’, (4) ‘collaboration’, (5) ‘compassionate’, (6) ‘dedication’, (7) ‘dignity’, (8) ‘dynamism’, (9) ‘health promotion’, (10) ‘legislature’, (11) ‘meeting needs’, (12) ‘noble’, (13) ‘profession’, (14) ‘research’, (15) ‘support’ and (16) ‘unbiased’. The exposed themes were (1) affective, (2) cognitive and (3) social and behaviour.
In the developed concept map, the concept of ‘nursing’ was the main point of focus. The categories identified were the key attributes of the concept of ‘nursing’, and hierarchical relations between concepts were illustrated. The spider map style reveals the concept of ‘nursing’ at the centre of the spider map, with the themes and categories and subcategories branching towards the centre expressing the importance of the main concept. The linking arrows connect key attributes (categories) of nursing, depicting the relationships between the themes: affective, cognitive and social aspects (see Figure 3 ).

Visual concept map of nursing.
Participants expressed suggestions to enhance the concept map during rounds of validation. There was uncertainty about the term ‘dynamism’ and deficiency in terms of the behaviour aspect; the psychomotor skills aspect had shortfalls, and ‘meeting needs’ should have been included in the social and cognitive parts of the concept map; finally, the ethical code of conduct needed to be addressed.
All participants’ comments were viewed and qualitatively analysed according to the guidelines by Tesch ( 1992 ), with necessary amendments to the visual concept map. The raw data were reviewed to facilitate amendments, and the final concept map of nursing (see Figure 4 ) was accepted as validation was completed, after a consensus of 86% was reached between the panellists.

Final concept map of nursing.
The concept map of nursing contributes a visual presentation to facilitate the teaching of the concept of ‘nursing’. The visual map was designed to assist student nurses to learn in a more meaningful way with the aim of having a similar interpretation and understanding of the concept of ‘nursing’. The layout of the concept map is visual and clear to facilitate understanding of the structure of the concept of ‘nursing’. Teaching becomes highly interactive when student nurses have the opportunity to engage with key attributes in the visual concept map to stimulate critical thinking that can progress into a discussion of the meaning of ‘nursing’. Nurse educators can direct the student nurse’s attention to the inter-relationships of the different aspects of the concept as depicted by the linking arrows. Concerns and expressions about the definition are encouraged to assist with clarity, ensuring a similar interpretation and understanding of the concept of ‘nursing’.
Possibly, pre-exposure to the definition of nursing as outlined by the SANC could have influenced nurses to tailor their definition of the concept of ‘nursing’. Many times, more effort is required for new thoughts and ideas about a topic, a new definition or understanding of a concept as opposed to relying on the familiar. A visual concept map to facilitate the understanding of the concept of nursing can therefore contribute to similar understanding and new insights to the concept.
A tool was developed to teach the concept of nursing to students so that it can be interpreted and understood in the same way. The visual concept map of nursing was developed after analysing various definitions of the concept provided by nurses as well as various literature sources. The concept map is an asset to the education process as visual concept maps stimulate critical thinking and participation of students in their learning.
Acknowledgements
The authors would like to acknowledge the Department of Health Studies, College of Human Sciences, University of South Africa (UNISA) for affording them the opportunity to conduct this research study.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors’ contributions
The contributions made by each author are as follows: S.D.M. is the corresponding author and contributed to the conception and design of the study, the data collection, analysis and interpretation of the data and writing the original draft of the manuscript.
L.R. and K.A.M. made supervisory contribution to the work outlined in the manuscript in the conception and design of the study, data collection, analysis and interpretation of the data; K.A.M. and L.R. also critically revised the manuscript prepared by the corresponding author and offered administrative, technical or material support and supervision and gave the final approval of the manuscript submitted.
Funding information
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors; however, this research received a bursary from UNISA’S Student Funding Directorate (DSF). The article processing charges will be covered by UNISA.
Data availability
The views and opinions expressed in this manuscript are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
How to cite this article: Mottian, S.D., Roets, L. & Maboe, K.A., 2022, ‘Interpretation of the concept “nursing”: Utilisation in nursing education and practice’, Curationis 45(1), a2351. https://doi.org/10.4102/curationis.v45i1.2351
- Bartels, B.H., 1995, ‘ Promoting mathematics connections with concept mapping ’, Mathematics Teaching in the Middle School 1 ( 7 ), 542–549. 10.5951/MTMS.1.7.0542 [ CrossRef ] [ Google Scholar ]
- Democratic Nursing Organisation of South Africa , 2022, About us , n.d., viewed 21 March 2022, from https://www.denosa.org.za/About.php?id=339 . [ Google Scholar ]
- Gray, J.R. & Grove, S.K., 2020, Burns and Grove’s the practice of nursing research: Appraisal, synthesis, and generation of evidence , 9th edn., Elsevier Health Sciences, Missouri, MO. [ Google Scholar ]
- Henderson, V., 1964, ‘ The nature of nursing ’, The American Journal of Nursing 64 ( 8 ), 62–68. 10.1097/00000446-196408000-00029 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Howie, L. & Robertson, A., 2017, Island nurses stories of birth, life and death on remote Great Barrier Island , Allen & Unwin, Auckland. [ Google Scholar ]
- International Council of Nurses (ICN) , 2002, Nursing definitions , viewed 20 May 2022, from https://www.icn.ch/nursing-policy/nursing-definitions . [ Google Scholar ]
- Keeling, A.W., Hehman, M.C. & Kirchgessner, J.C., 2018, History of professional nursing in the United States: A culture of health , Springer Publishing Company, New York, NY. [ Google Scholar ]
- Nightingale, F., 1860, Notes on nursing, what it is, what it’s not , D. Appleton, New York, NY. [ Google Scholar ]
- Novak, J.D. & Canas, A.L., 2006, The theory underlying concept maps and how to construct them , Technical Report IHMC Cmaps Tools, pp. 1–31, Florida Institute for Human and Machine: Pensacola, viewed 30 March 2022, from http://cmap.ihmc.us/Publications/ResearchPapers/TheoryUnderlyingConceptMaps.pdf . [ Google Scholar ]
- Peplau, H.E., 1952, Interpersonal relations in nursing: A conceptual frame of reference for psychodynamic nursing , 3rd edn., Putnam Sons, New York, NY. [ Google Scholar ]
- Royal College of Nursing (RCN) , 2003, Defining nursing , viewed 28 October 2022, from http://anaesthesiaconference.kiev.ua/downloads/defining%20nursing_2003.pdf . [ Google Scholar ]
- South African Nursing Council , 2005, Nursing Act No. 33 of 2005 , viewed 03 August 2021, from https://www.sanc.co.za/wp-content/uploads/2020/06/Nursing-Act-2005.pdf . [ Google Scholar ]
- Tesch, R., 1992, Qualitative research analysis types and software tools , Falmer, New York, NY. [ Google Scholar ]
- Walker, L.O. & Avant, K.C., 2011, Strategies for theory construction in nursing , 5th edn., Prentice-Hall, Boston, MA. [ Google Scholar ]
- Whittemore, R. & Knafl, K., 2005, ‘ The integrative review update methodology ’, Journal of Advanced Nursing 52 ( 5 ), 546–553. 10.1111/j.1365-2648.2005.03621.x [ PubMed ] [ CrossRef ] [ Google Scholar ]

University Administration
- Careers @ USA
- For Current Students
- Request Information
- Master of Occupational Therapy (MOT)
- Doctor of Occupational Therapy (OTD)
- Post-Professional Doctor of Occupational Therapy (PPOTD)
- Master of Health Administration (MHA)
- Doctor of Education (EdD)
- Graduate Certificates
- Clinical Orthopedic Residency (OCS)
- Orthopaedic Manual Physical Therapy Fellowship (OMPT)
- Continuing Professional Education (CPE)
- Doctor of Physical Therapy (DPT)
- Non-Degree Physical Therapy Online Courses
- Master of Science in Speech-Language Pathology (MS-SLP)
- Post-Graduate Nursing Certificates
- Master of Science in Nursing (MSN)
- Doctor of Nursing Practice (DNP)
- Browse All Degree-Programs
- Admissions & Aid Home
- Scholarships & Grants
- How to Apply
- Cost of Attendance
- Financial Aid
- Application Deadlines
- Academic Calendar
- Financial Aid FAQ
- Admissions FAQs
- Catalog/Handbook
- Our History
- Accreditation
- B Corp Certified
- Change of Ownership
- Student Achievement Data
- Institutional Learning Outcomes (ILOs)
- Diversity & Inclusion
- San Marcos, California
- St. Augustine, Florida
- Miami, Florida
- Austin, Texas
- Dallas, Texas
- Our Faculty
- Board of Directors

Nursing MSN & DNP
| 20 May 2024
The Importance of Effective Communication in Nursing

To be a successful healthcare provider, clinical nurse or nurse leader, you need exceptional communication skills—and you need to be able to use them during high-stress situations.
Why Is Communication Important in Nursing?
Having good communication skills is essential to collaborating on teams with your fellow nurses and colleagues from other disciplines. It’s also important to patient-centered care.
Nurses who take the time to listen and understand the concerns of each of their patients are better prepared to address issues as they arise, resulting in better patient outcomes.
On the other hand, poor communication, or lack of communication in healthcare , can lead to patients misunderstanding directions and failing to follow treatment protocols. It can also lead to workflow breakdowns on the team, resulting in a medical error . A report by the Joint Commission found that poor communication in healthcare during patient transfers contributed to 80% of serious medical errors.
Additionally, patients who have established an open and secure dialogue with a nurse or healthcare provider are more likely to disclose the true extent of their symptoms. According to the book Interpersonal Relationships: Professional Communication for Nurses by Arnold and Boggs , healthcare communication competency offers a primary means for establishing a trusting, collaborative relationship with patients and families. Interpersonal communication skills influence the quality of decisions made, as well as the level of patient motivation to follow treatment protocols and achieve desired clinical outcomes.
10 Effective Communication Skills for Nurses

For nurses, good communication in healthcare means approaching every patient interaction with the intention to understand the patient’s concerns, experiences, and opinions. This includes using verbal and nonverbal communication skills, along with active listening and patient teach-back techniques. Below, we explore 10 communication skills that are important for nurses.
1. Verbal Communication
Excellent verbal communication is key. Aim to always speak with clarity, accuracy, and honesty. It’s also important to know your audience and speak appropriately according to the person’s age, culture, and level of health literacy. If you are feeling stressed out or frustrated, be aware of your tone of voice and don’t let these emotions leak into your patient interaction. You can:
- Encourage patients to communicate by asking open questions like, “Can you tell me a bit more about that?”
- Avoid condescending pet names like “honey” or “sweetie” and instead use the patient’s first name or name of choice.
- Speak in clear, complete sentences and avoid technical jargon.
2. Nonverbal Communication
Using elements of nonverbal communication—such as facial expressions, eye contact, body language, gestures, posture, and tone of voice—is also essential in creating rapport. Simply smiling can go a long way. You can also:
- Show interest in what the patient is saying by maintaining eye contact and nodding your head.
- Smile, but don’t stare.
- Sit down when you can, and lean forward to show you’re engaged.
- Use nonthreatening body language that conveys openness.
3. Active Listening
“Active listening” means listening in order to understand the other person’s experience. The highest and most effective form of listening requires complete attention and engagement. This skill is important not only for clinical nurses but also for nurse executives and other healthcare providers as a tool for building trust and commitment with their staff. Active listening includes both verbal and nonverbal communication skills. For example:
- Nod your head, but never interrupt.
- Lean forward and maintain eye contact to let the person know you’re engaged.
- Include minimal verbal encouragement, such as “I understand,” and “go on.”
4. Written Communication
Written communication skills are also essential for effective nurse-to-nurse communication. As a nurse, you will be responsible for creating and updating the patient ’s medical record . It is critical that the medical record is accurate and current so your patients can receive the best care possible. Also, remember to protect patient confidentiality. Some tips:
- Make notes immediately following patient care so you do not forget anything.
- Write legibly and clearly, using simple language.
- Be sure to note accurate dates and times.
5. Presentation Skills
Effective presentation skills are most applicable during “handover”—when you are transferring patient care to another nurse or other healthcare providers . These skills will also help you demonstrate your knowledge and expertise clearly in a variety of workplace settings, such as presenting at conferences, participating in job interviews, giving case reports to physicians, and more. It’s a good idea to:
- Plan out your presentation and practice.
- Pay attention to both your verbal communication and body language.
- Add visuals to your presentation for a better explanation.
- Understand your audience and know what they want and need from the presentation.
6. Patient Education (Patient Teach-Back)
Nurses are in charge of most of the communication between the healthcare team and patients. This includes informing patients and family members of health conditions, diagnoses, treatment plans, and medication protocols. This skill is especially important for family nurse practitioners who work with patients and families to provide health and education counseling.
Patient teach-back is an effective communication strategy where providers ask patients to repeat the information back to them. This method improves patient understanding and encourages adherence to care instructions. Poor understanding of information can cause patients and their family members to feel anxious or become defensive. For example, you can say:
- “We’ve gone over a lot of information. Now I’d like you to repeat it back to me to make sure you remember everything.”
- “Can you repeat the instructions for taking this medicine back to me?”
- “Let’s review what we just discussed. Can you explain it to me in your own words?”
7. Making Personal Connections
It’s important to get to know the person behind the patient. Patient-centered relationships are critical in helping patients feel safe and comfortable. Creating meaningful connections with patients can improve outcomes and trust. Some ideas:
- Spend a couple of extra minutes every day with each patient getting to know them.
- Find out a fun fact about each patient.
- Show interest in their lives and share stories of your own.
It’s important for healthcare professionals to inspire trust in patients by listening actively and taking every complaint and concern seriously. Building trust takes time. Healthcare settings are scary for some patients. It’s important to make them feel as comfortable as possible.
Trust is something that nurse educators and leaders should also cultivate as they work to develop the next generation of nurses. To inspire trust, nurse leaders and educators should:
- Always tell the truth.
- Share information openly.
- Be willing to admit mistakes.
9. Cultural Awareness
You will likely work with people every day who come from a wide range of social, cultural, and educational backgrounds. Every patient and coworker is unique, and it’s important to be aware and sensitive. For example, gauge the patient’s fluency with English and grade your vocabulary accordingly or bring in a translator if necessary and possible. With trans and gender nonbinary patients, be sure to use their preferred name and pronoun.
10. Compassion
Conveying compassion is an essential communication skill in healthcare. According to the Journal of Compassionate Healthcare , “studies show that compassion can assist in prompting fast recovery from acute illness, enhancing the management of chronic illness, and relieving anxiety.” You can deliver compassionate nursing care by putting yourself in the patient’s shoes and understanding their needs and expectations.
How to Overcome Communication Barriers in Nursing
Sometimes the message sent is not always received the way it was desired. Communication barriers in nursing result in weak patient-nurse interactions and relationships. To overcome these, we must first understand the types of communication barriers that nurses face. In the article “ Communication and Language Needs ,” Dawn Weaver identifies three common communication barriers in nursing: physical, social, and psychological.
Physical Barriers
The environment in which you communicate with a patient can make a huge difference in effective communication. Busy, loud, and distracting settings can increase patient stress. To create a safe and comfortable environment, try closing doors, opening blinds, and mitigating outside noises whenever you can.
Social Barriers
Social barriers include differences in language, religion, culture, age, and customs. Understanding each patient’s cultural background can help nurses avoid prejudice and communicate clearly. It’s a good idea to tailor your communication strategies depending on the patient’s age, as well: A 12-year-old and a 70-year-old will have very different ideas of what health and healthcare mean to them.
Psychological Barriers
For many patients, a trip to the doctor is anxiety-inducing. Anxiety and stress are psychological barriers, as are dementia and other cognitive conditions. To help reduce their influence, it helps to take extra time to listen, empathize, and be supportive. Such psychosocial care has been proven to improve patient health outcomes and quality of life.
Nurses may also need to overcome their own psychological barriers. Speaking to patients and family members about death, disease, and other sensitive topics can be distressing. A study in the Journal of Advanced Nursing explored the fact that many nurses experience feelings of anxiety when discussing patient medical needs and conditions.
Get Started Developing Crucial Communication Skills Today
Learning these and other communication skills should be part of your education, whether you’re enrolled in undergraduate nursing school or a graduate nursing program . They are also easy to practice on the job, as you will get plenty of opportunities for communicating with patients and your colleagues. Put your favorite idea into practice today!
The University of St. Augustine for Health Sciences (USAHS) offers Master of Science in Nursing (MSN), Doctor of Nursing Practice (DNP), and Post-Graduate Nursing Certificates designed for working nurses. Our degrees are offered online, with optional on-campus immersions* and an annual interprofessional trip abroad. Role specialties include Family Nurse Practitioner (FNP), Nurse Educator (MSN only) , and Nurse Executive . The MSN has several options to accelerate your time to degree completion. Complete coursework when and where you want—and earn your advanced nursing degree while keeping your work and life in balance.
*The FNP track includes two required hands-on clinical intensives as part of the curriculum.
The Joint Commission. “Joint Commission Center for Transforming Healthcare Releases Targeted Solutions Tool for Hand-Off Communications.” Joint Commission Perspectives 32, no. 8 (August 2012): 1, 3. https://pubmed.ncbi.nlm.nih.gov/22928243/. Accessed: January 26, 2022
Agency for Healthcare Research and Quality. “Use the Teach-Back Method: Tool #5.” Last reviewed September 2020. https://www.ahrq.gov/health-literacy/quality-resources/tools/literacy-toolkit/healthlittoolkit2-tool5.html. Accessed: January 26, 2022
Chen, Cassandra Siyun, Sally Wai-Chi Chan, Moon Fai Chan, Suk Foon Yap, Wenru Wang, and Yanika Kowitlawakul. “Nurses’ Perceptions of Psychosocial Care and Barriers to Its Provision: A Qualitative Study.” The Journal of Nursing Research 25, no. 6 (2017): 411–418. doi:10.1097/JNR.0000000000000185.
ARE YOU INSPIRED?
There could be an article about you here one day. Take charge of your own life-story!
Take charge of your own life-story
More Nursing MSN & DNP Articles

Dr. Elisabeth McGee Discusses USAHS’ Driving Role in Future-Focused Healthcare

Nurse Practitioner vs. Physician Assistant: Key Differences
85 Nursing Quotes: Words of Wisdom for Nurses
Upcoming nursing msn & dnp events.

Post Professional Doctor of Occupational Therapy (OTD) Webinar - September 10 | USAHS

Occupational Therapy Programs (OTD, OTD Flex, MOT, & MOT Flex) - Admissions Webinar - September 16 | USAHS

Doctor of Physical Therapy (DPT) - Admissions Webinar - September 17 @ 4:00 pm PDT
- Click here - to use the wp menu builder

- Privacy Policy
- Refund Policy
- Terms Of Service
- Nursing notes PDF
- Nursing Foundations
- Medical Surgical Nursing
- Maternal Nursing
- Pediatric Nursing
- Behavioural sciences
- BSC NURSING
- GNM NURSING
- MSC NURSING
- PC BSC NURSING
- HPSSB AND HPSSC
- Nursing Assignment
Nursing Implications Definition and Importance
Nursing Implications Definition – Nursing implications are the potential effects of a patient’s condition or treatment on their care. Nurses use their knowledge and skills to assess these implications and develop care plans that minimize risks and promote optimal outcomes. Learn more about nursing implications and their importance in patient care. In the world of healthcare, nursing is a vital profession that plays a critical role in patient care and recovery. Nurses are not just healthcare providers; they are also educators, advocates, and caregivers. To fully appreciate the significance of nursing in healthcare, it’s essential to understand nursing implications. In this Nursing Implications Definition and Importance article, we will delve into the definition of nursing implications and explore why they are crucial in the healthcare landscape.
Table of Contents
What Are Nursing Implications?
Nursing implications refer to the responsibilities and actions that nurses take based on their clinical judgment and assessment of a patient’s condition. These implications are an integral part of nursing care plans and guide nurses in providing safe and effective patient care. Nursing implications encompass a wide range of activities and decisions that nurses make during their interactions with patients.
The Role of Nursing Implications
Nursing implications serve several essential functions within the healthcare system:
1. Individualized Care
Nurses use their clinical judgment to tailor care plans to each patient’s unique needs. This individualized approach ensures that patients receive care that is specifically designed to address their health issues.
2. Monitoring and Evaluation
Nurses continuously monitor patients’ conditions and evaluate the effectiveness of treatments and interventions. This helps in making real-time adjustments to the care plan to ensure optimal outcomes.
3. Patient Advocacy
Nurses advocate for their patients’ rights and well-being. They ensure that patients receive the best possible care and that their voices are heard in the healthcare decision-making process.
4. Communication
Effective communication is key to successful patient care. Nurses use their assessment findings and clinical judgment to communicate with other healthcare team members , ensuring that everyone is on the same page regarding the patient’s condition and treatment plan.
The Importance of Nursing Implications
Understanding the significance of nursing implications is crucial for both healthcare professionals and patients. Here’s why nursing implications are so important:
1. Patient Safety
Nursing implications prioritize patient safety. Nurses are trained to recognize potential risks and take preventive measures to ensure that patients are not harmed during their hospital stay or treatment.
2. Quality of Care
By tailoring care plans to individual patient needs, nursing implications contribute to the overall quality of care. This personalized approach results in better patient outcomes and satisfaction.
3. Timely Interventions
Nurses play a vital role in early detection and intervention. Their ability to assess and make informed decisions can lead to timely interventions that prevent complications and improve patient recovery rates.
4. Coordination of Care
Nursing implications facilitate effective communication and coordination among healthcare team members. This ensures that everyone involved in patient care is well-informed and working towards common goals.
Examples of Nursing Implications
Examples of nursing implications include:
- The risk of getting an infection in a patient with a wound.
- The chance of falling in a patient who has trouble moving around.
- The possibility of not getting enough nutrients in a patient who feels sick and throws up.
- The chance of feeling lonely in a patient who has to stay in the hospital for a long time.
- The risk of medicines not working well together in a patient taking many different drugs.
Types of Nursing Implications
Nursing implications come in two primary types: direct and indirect.
- Direct Implications: These are the immediate or short-term consequences of a patient’s condition or treatment. For instance, a direct implication of a wound is the possibility of getting an infection.
- Indirect Implications: These are the long-term or delayed consequences of a patient’s condition or treatment. For example, an indirect implication of a stroke is the chance of experiencing depression later on.
Identifying and Assessing Nursing Implications
Nurses employ a structured approach known as the nursing process to recognize and evaluate nursing implications. This process consists of four key steps:
- Assessment: This involves collecting information about the patient’s overall health, both physical and mental, their social support system, and the environment they’re in.
- Diagnosis: Here, nurses analyze the gathered data to pinpoint the patient’s nursing diagnoses, which are essentially their health problems or concerns.
- Planning: In this step, nurses establish specific goals and desired outcomes for the patient’s care. They also devise strategies and actions to reach these objectives.
- Evaluation: Finally, nurses assess how the patient responds to the implemented interventions and make any necessary adjustments to the care plan to ensure it remains effective.
Developing and Implementing Nursing Care Plans
Nursing care plans serve as comprehensive documents detailing a patient’s nursing diagnoses, objectives, expected results, interventions, and criteria for assessment. These plans are crafted and put into action through the collective efforts of nurses, alongside fellow healthcare professionals like physicians, dietitians, and physical therapists.
Challenges and Opportunities in Nursing Implications
| 1. Increasing Healthcare Complexity | 1. Innovative Technologies and Treatments |
| 2. Rising | 2. Emphasis on |
| 3. Nursing Shortages | 3. Patient-Centered Care |
| 4. Demands of an Aging Population | 4. Interdisciplinary Collaboration |
| 5. Educational Advancements | |
| 6. Advocacy and Leadership Roles |
Conclusion -Nursing Implications Definition and Importance
Nursing implications are the backbone of patient-centered care. They empower nurses to provide individualized, safe, and high-quality care while advocating for the well-being of their patients. In the ever-evolving healthcare landscape, nursing implications remain a fundamental aspect of nursing practice.
FAQs (Nursing Implications Definition and Importance)
How do nurses determine nursing implications.
Nurses determine nursing implications through a combination of clinical judgment, patient assessment, and evidence-based practice.
Can nursing implications change during a patient’s treatment?
Yes, nursing implications can change based on the patient’s response to treatment or new clinical findings. Nurses regularly reassess and adapt care plans accordingly.
Are nursing implications only relevant in hospital settings?
No, nursing implications are relevant in various healthcare settings, including hospitals, clinics, home care, and long-term care facilities.
What happens if nursing implications are not followed?
Not following nursing implications can lead to compromised patient safety, suboptimal care, and potential harm to the patient.
Please note that this article is for informational purposes only and should not substitute professional medical advice.
Leave a Reply Cancel reply
Recent articles, types of therapeutic communication in nursing, antibiotic injection list: a comprehensive guide, best 11 types and purpose of injections, understanding sexually deviant behavior and examples, top 10 duties of a nurse, benefits and types of convalescent care, download nursing notes pdf, human excretory system pdf, human physiology digestion and absorption, human body digestive system bsc nursing notes pdf, aiims recruitment question with answers, reproductive system nursing notes pdf, staff nurse syllabus and exam pattern question bank -ii, sensory system and sense organs pdf, human respiratory system nursing pdf, more like this, gifts for nursing home residents, gift ideas for nursing students, crystalloid and colloid: differences and when to use each, how to insert a catheter in a female patient -female catheterization, mental health nursing diagnosis care plan pdf, child pediatric health nursing notes -bsc nursing, mid-wifery pdf notes for nursing students, national health programmes in india pdf, primary health care nursing notes pdf, psychology note nursing pdf, nursingenotes.com.
- STUDY NOTES
- SUBJECT NOTES
A Digital Platform For Nursing Study Materials
Latest Articles
Most popular.
© Nursingenotes.com | All rights reserved |
How to Write a Nursing Essay Quickly and Effortlessly?

Samuel Gorbold
In the demanding field of nursing career, efficient and effective writing is a valuable skill that can greatly enhance academic success. Whether faced with looming deadlines or seeking to streamline the writing process, understanding how to compose a nursing essay quickly and effortlessly is crucial. This article serves as a comprehensive guide, offering practical tips, proven strategies, and insightful techniques tailored to the unique demands of nursing essays. From effective planning and nursing essay examples to honing research and writing skills, this article will teach you how to master the essay-writing process seamlessly, ensuring both academic excellence and time management in the dynamic world of healthcare education.
What Is a Nursing Essay?
A nursing essay is a written academic assignment that provides students in nursing programs with the opportunity to articulate their understanding of a particular topic, concept, or clinical experience. Nurse essay creation often requires students to explore and analyze nursing theories, healthcare practices, or case studies, demonstrating a deep comprehension of the subject matter. Additionally, nursing essays may involve critical reflection on personal experiences in clinical settings, allowing students to integrate theoretical knowledge with practical application.
The structure of a nursing essay typically includes an introduction, where the topic is introduced, and the thesis is stated, followed by the body paragraphs that elaborate on key points, provide evidence, and analyze the topic in depth. The conclusion summarizes the main arguments and reinforces the thesis, highlighting the significance of the discussed writing concepts in the context of nursing practice. Throughout the essay, students are encouraged to incorporate evidence-based information, uphold ethical considerations, and adhere to academic writing standards. Use our nursing essay writing service to get a better grip on structure and argumentation.
Medical essays play a crucial role in the educational journey to a nursing career, fostering critical thinking, effective communication skills, and a deeper understanding of the complexities within the healthcare field. These written works not only contribute to academic assessments but also serve as a means for students to articulate their perspectives, share insights gained from clinical experiences, and engage with the ongoing discourse in nursing practice and theory.

How to Start a Nursing Essay?
Starting essays on nursing effectively involves capturing the reader's attention, clearly stating your thesis or main idea, and providing a roadmap for what the essay will cover. Here are some steps to help you begin your nursing essay:
- Start with a Compelling Introduction
Begin your nursing essay with a strong and engaging introduction. You can use a thought-provoking question, a relevant anecdote, or a compelling statistic to grab the reader's attention. Clearly state the purpose of your essay and provide a concise overview of what you will discuss.
- State Your Thesis
In the introduction, clearly state your thesis or main argument. This is the central point that your essay will revolve around. Make sure it is concise, specific, and reflective of the main theme of your essay.
- Provide Context
Write some background or context related to the topic of your essay. This helps the reader understand the significance of the subject matter and sets the stage for the detailed discussions in the body of the essay.
- Outline the Structure
Briefly outline the structure of your essay in the introduction. This provides the reader with a roadmap of what to expect. Mention the main points or sections you will cover in the essay's body.
- Maintain Clarity and Conciseness
Write your introduction clearly and concisely. Avoid unnecessary details or information that does not directly contribute to the main theme. Aim for a balance between providing context and maintaining brevity. In the next section, you will discover a nursing essay introduction example, as well as instructions on how to structure the main body and conclusion.

How to Structure a Nursing Essay?
Essay creationing is an inalienable part of nursing education. A compelling paper parallels a meticulously executed performance, requiring a carefully crafted script and a narrative that unfolds effortlessly, captivating the audience throughout. This script manifests as a thoughtfully organized structure. Let's explore the components that guide the transformation of a nursing essay from a mere assortment of words into a captivating journey filled with valuable insights.
Introduction
The nursing essay introduction should serve as a captivating gateway, enticing the reader to delve into the complexities of the topic. Start with a compelling hook that relates to the subject matter. For instance, you might begin with a thought-provoking question, such as, "How do nurses navigate the delicate balance between empathy and professionalism in patient care?" Following the hook, write a brief overview of the paper's focus, culminating in a clear and concise thesis statement. For example, "This nursing essay will explore the nuanced challenges nurses face in maintaining empathetic connections with patients while upholding the standards of professional healthcare."
The body of your nursing essay should unfold like a well-organized narrative, with each paragraph contributing to the overall storyline. Write each paragraph with a topic sentence that encapsulates a key aspect of your argument. Substantiate your points with relevant examples, drawing from nursing theories, personal experiences, or real-life case studies. For instance, if discussing the importance of effective communication in nursing, narrate a scenario where clear communication positively impacts patient outcomes. Ensure a logical flow between paragraphs, allowing ideas to transition seamlessly. Address counterarguments and demonstrate a comprehensive understanding of the topic, supporting your claims with scholarly references and evidence.
Conclude your nursing essay by summarizing the key points and reinforcing the significance of your thesis. Avoid writing new information but rather synthesize the insights presented in the main body. Reflect on the broader implications of your findings for nursing practice or education. For example, if your essay explored the role of technology in modern healthcare, discuss the potential impact on patient outcomes and the evolving responsibilities of nurses. Conclude with a thought-provoking statement that leaves a lasting impression on the reader, prompting them to contemplate the complexities you've unraveled in your essay.
Nursing Essay Outline
Within the framework of nursing essay composition, the outline serves as a vital architectural blueprint. This section delves into the key elements constituting an effective nursing essay outline, offering a structured foundation for insightful and well-articulated academic discourse.
I. Introduction
- Engaging question or relevant anecdote.
Background:
- Brief context on the significance of the topic.
Thesis Statement:
- A clear and concise statement of the main argument.
Paragraph 1:
- Topic Sentence: Introduction of the first key aspect.
- Example: Real-life scenario, personal experience, or case study.
- Explanation: Analyze the example and relate it to the thesis.
Paragraph 2:
- Topic Sentence: Introduction of the second key aspect.
- Example: Another relevant illustration or supporting evidence.
- Explanation: Elaborate on the connection to the overall argument.
Paragraph 3:
- Topic Sentence: Introduction of the third key aspect.
- Example: Additional supporting evidence or nursing theory application.
- Explanation: Discuss the implications and significance.
Counterarguments:
- Acknowledge opposing views and counter with supporting evidence.
Integration:
- Demonstrate connections between the discussed aspects.
- Showcase a comprehensive understanding of the topic.
III. Conclusion
Summary of Key Points:
- Recap the main points discussed in the body.
Thesis Reinforcement:
- Reiterate the thesis and its significance.
Broader Implications:
- Discuss the broader impact on nursing practice or education.
Thought-Provoking Statement:
- Conclude with a memorable and reflective statement.

How to Write a Nursing Essay Step-by-Step?
Before the writing process begins, remember to adhere to academic standards, cite your sources appropriately, and proofread your essay for clarity, coherence, and grammatical accuracy before submission.
Step 1 – Understand the Assignment
Begin by thoroughly understanding the essay prompt or assignment requirements. Identify the specific topic, guidelines, and any key components that must be addressed in your essay.
Step 2 – Research and Gather Information
Conduct thorough research on the chosen topic. Utilize reputable nursing sources, including academic journals, textbooks, and evidence-based literature. Collect relevant information to support your arguments and enhance the credibility of your essay.
Step 3 – Develop a Strong Thesis Statement
Craft a clear and concise thesis statement that encapsulates the main argument or purpose of your nursing essay. Ensure that your thesis is specific, debatable, and reflective of the key themes you will explore.
Step 4 – Create an Outline
Organize your thoughts and structure your essay by creating an outline. Divide your essay into an introduction, body paragraphs, and conclusion. Outline the main points you want to cover in each section, ensuring a logical flow of ideas.
Step 5 – Write a Compelling Introduction
Capture the reader's attention with a compelling introduction. Start with a hook, provide background information on the nursing topic, and end with a strong thesis statement that outlines the main focus of your essay.
Step 6 – Develop the Body Paragraphs
Dedicate each body paragraph to a specific aspect or key point related to your thesis. Start each paragraph with a topic sentence, support it with relevant examples or evidence, and provide analysis. Ensure a smooth transition between paragraphs to maintain the coherence of your nursing paper.
Step 7 – Craft a Thoughtful Conclusion
Summarize the main points discussed in the body of your essay and restate your thesis in the conclusion. Reflect on the broader implications of your findings, and end with a thought-provoking statement that leaves a lasting impression on the nursing readers.
How to End a Nursing Essay?
In concluding a nursing essay, the primary goal is to reinforce the key points made throughout the essay and leave a lasting impression on the reader. Begin by summarizing the main arguments and findings presented in the essay's body. This recap should concisely revisit the critical aspects of your discussion, emphasizing their significance in the context of nursing practice or theory. By summarizing, you provide a quick reference to the essential takeaways, ensuring clarity and reinforcing the coherence of your essay.
Following the summary, re-write your nursing thesis in a slightly different manner, connecting it back to the broader implications of your study. Discuss how the insights gained from your exploration contribute to the nursing field or address real-world challenges. In this section, it's essential to avoid introducing new information; rather, focus on synthesizing the information presented and showcasing the broader relevance of your work. Finally, leave the reader with a thought-provoking statement or a call to action that encourages further contemplation of the discussed concepts and their impact on the dynamic landscape of nursing. This concluding touch ensures that your nursing essay concludes on a strong and memorable note. Hire long essay writer on EssayHub to get a proper assistance with all academic struggles you have.
15 Nursing Essay Writing Tips
- Clarify the essay requirements and ensure a precise understanding of the topic.
- Craft a clear and focused thesis statement to guide your essay.
- Utilize reputable sources and evidence-based nursing education literature for robust arguments.
- Break down tasks to manage time effectively and avoid last-minute stress.
- Create a well-organized outline to maintain a logical flow in your essay.
- ECapture attention with a compelling hook and clearly state your thesis.
- Dedicate each paragraph to a specific point supported by evidence.
- Move beyond description; analyze and reflect on the significance of your points.
- Use clear, concise, and professional language in your writing.
- Check for grammar, spelling, and coherence errors before submitting.
- Keep your essay focused on the main theme, avoiding unnecessary details.
- Properly cite all sources to uphold nursing integrity.
- Seek feedback from peers or instructors to gain valuable insights.
- Summarize key points and discuss broader implications in your conclusion.
- Review your essay with a fresh perspective, making targeted revisions for improvement.
Nursing Essay Example
It’s a well-known fact that a writing example packed with practical insights into how to produce a certain type of academic document helps students cope with such an assignment faster. That’s why we’ve prepared a nursing essay example for your inspirational and consulting needs.

Samuel Gorbold , a seasoned professor with over 30 years of experience, guides students across disciplines such as English, psychology, political science, and many more. Together with EssayHub, he is dedicated to enhancing student understanding and success through comprehensive academic support.

- Plagiarism Report
- Unlimited Revisions
- 24/7 Support

IMAGES
VIDEO
COMMENTS
Critical Thinking and Clinical Reasoning. Nurses make decisions while providing patient care by using critical thinking and clinical reasoning. Critical thinking is a broad term used in nursing that includes "reasoning about clinical issues such as teamwork, collaboration, and streamlining workflow." [1] Using critical thinking means that nurses take extra steps to maintain patient safety ...
Each letter refers to the six components of the nursing process: A ssessment, D iagnosis, O utcomes Identification, P lanning, I mplementation, and E valuation. The nursing process is a continuous, cyclical process that is constantly adapting to the client's current health status.
The nursing process is defined as a systematic, rational method of planning that guides all nursing actions in delivering holistic and patient-focused care. The nursing process is a form of scientific reasoning and requires the nurse's critical thinking to provide the best care possible to the client.
A contemporary definition of clinical judgement, within the context of nursing, was developed from the analysis and is articulated as Clinical judgement is a reflective and reasoning process that draws upon all available data, is informed by an extensive knowledge base and results in the formation of a clinical conclusion.
Henderson's nursing needs theory is useful in practice and many nursing disciplines with different practice directions. The approach is practical because it is based on individuals' core needs and assumptions of the necessity to be healthy and care for patients from the nurses' side (Gonzalo, 2019). The application of this theory in ...
Conclusion. Nursing professionalism is one of the important foundations of clinical nursing. It is multidimensional, dynamic, and culture oriented. Based on the analysis, nursing professionalism has been defined as providing people care based on principles of professionalism, caring, and altruism.
Nursing integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence. Nursing is the diagnosis and treatment of human responses and advocacy in the care of ...
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood ...
2. CRITICAL THINKING SKILLS. Nurses in their efforts to implement critical thinking should develop some methods as well as cognitive skills required in analysis, problem solving and decision making ().These skills include critical analysis, introductory and concluding justification, valid conclusion, distinguishing facts and opinions to assess the credibility of sources of information ...
Decision-making is a fundamental concept of nursing practice that conforms to a systematic trajectory involving the assessment, interpretation, evaluation and management of patient-specific situations (Dougherty et al, 2015).Shared decision-making is vital to consider in terms of patient autonomy and professional duty of care as set out in the Nursing and Midwifery Council (NMC) (2018)Code ...
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
nursing, profession that assumes responsibility for the continuous care of the sick, the injured, the disabled, and the dying.Nursing is also responsible for encouraging the health of individuals, families, and communities in medical and community settings. Nurses are actively involved in health care research, management, policy deliberations, and patient advocacy.
Pediatric Nursing: Scope and Standards of Practice is a collaborative effort of the ANA, the Society for Pediatric Nurses (SPN), and NAPNAP. The American Psychiatric Nurses Association (APNA) Web site provides information about the role of the advanced practice psychiatric nurse organized by topic, workplace setting, and/or specialty.
1. A personal nursing philosophy serves as a guideline to help nurses live by standards they have set for themselves. 2. Having a personal philosophy of nursing can improve how you interact with patients, their loved ones, and your peers. 3. Personal nursing philosophies help guide ethical, competent, evidence-based, and science-driven nursing ...
Autonomy in nursing is the ability of nurses to understand their patient's right to medical information and care while independently making decisions without consulting the healthcare provider. Autonomy also includes properly advocating for your patient.
Nursing theories aim to define, predict, and demonstrate nursing phenomenon (Chinn and Jacobs, 1978). It can be regarded as an attempt by the nursing profession to maintain and preserve its professional limits and boundaries. Nursing theories can help guide research and informing evidence-based practice.
Keep it to around 150 words. Move the reader forward. Use strong verbs and images to convey your point of view and move the reader forward in the essay by providing a sense of closure or hope for the future. Keep it simple. Use concrete examples and analogies to help explain complex concepts. End with a hook.
According to the American Nurses Association (ANA), the nursing code of ethics is a guide for "carrying out nursing responsibilities in a manner consistent with quality in nursing care and the ethical obligations of the profession.". Ethics, in general, are the moral principles that dictate how a person will conduct themselves.
Conclusion. A visual concept map of 'nursing', a tool facilitating teaching the concept and promoting similar understanding of its meaning is valuable in an evolving digital era, where visual stimulation enhances teaching and learning. ... However, on the contrary, arguably the definition of nursing provided by the SANC may be considered a ...
A philosophy of nursing is a statement that outlines a nurse's values, ethics, and beliefs, as well as their motivation for being part of the profession. It covers a nurse's perspective regarding their education, practice, and patient care ethics. A philosophy of nursing helps you identify the beliefs and theories that shape the choices you ...
For example: Nod your head, but never interrupt. Lean forward and maintain eye contact to let the person know you're engaged. Include minimal verbal encouragement, such as "I understand," and "go on.". 4. Written Communication. Written communication skills are also essential for effective nurse-to-nurse communication.
Conclusion -Nursing Implications Definition and Importance. Nursing implications are the backbone of patient-centered care. They empower nurses to provide individualized, safe, and high-quality care while advocating for the well-being of their patients. In the ever-evolving healthcare landscape, nursing implications remain a fundamental aspect ...
Conclusion. Conclude your nursing essay by summarizing the key points and reinforcing the significance of your thesis. Avoid writing new information but rather synthesize the insights presented in the main body. Reflect on the broader implications of your findings for nursing practice or education. For example, if your essay explored the role ...