- Research article
- Open access
- Published: 18 August 2020

Prevalence of non-communicable diseases and its risk factors among Ijegun-Isheri Osun residents in Lagos State, Nigeria: a community based cross-sectional study
- Israel Oluwaseyidayo Idris 1 , 2 , 3 , 4 ,
- Ayodipupo Sikiru Oguntade ORCID: orcid.org/0000-0001-8802-8590 2 , 5 , 6 ,
- Ekow Adom Mensah 1 , 2 , 7 &
- Noriko Kitamura 1 , 2 , 8 , 9
BMC Public Health volume 20 , Article number: 1258 ( 2020 ) Cite this article
18k Accesses
12 Citations
12 Altmetric
Metrics details
The rapid epidemiologic transition of diseases has adverse implications for low-and middle-income countries (LMICs) like Nigeria due to their limited healthcare, weaker health systems and the westernization of lifestyle. There is a need to evaluate the enormity or otherwise of non-communicable diseases (NCDs) burden in such low resource settings. We performed this survey to determine the prevalence of NCDs and its risk factors among the Ijegun- Isheri Osun community residents of Lagos, Nigeria.
A community-based cross-sectional survey was performed on 215 respondents recruited consecutively during a population preventive health campaign. Prevalence of three NCDs (hypertension, diabetes and dyslipidaemia) were calculated. Associations between each of these NCDs and selected risk factors were determined using chi square test. Multivariable logistic regression was used to estimate the risk factors of each of the three NCDs.
The prevalence of hypertension was 35.3% (95% CI 29.0–42.1), diabetes 4.6% (95% CI 2.2–8.4) and dyslipidaemia 47.1% (95% CI 41.1–54.8). Among the NCD risk factors, the prevalence of smoking was 41.3% (95% CI 34.2–48.6), alcohol consumption 72.5% (95% CI 65.5–78.7), and physical activity 52.9 (95% CI 45.5–60.2). The independent significant predictors of hypertension were age ≥ 60 years (aOR 4.56; 95% CI: 1.72–12.09) and dyslipidaemia (aOR 5.01; 95% CI: 2.26–11.13). Age ≥ 60 years (aOR 8.83; 95% CI: 1.88–41.55) was an independent predictor of diabetes. Age ≥ 60 years (aOR 29.32; 95% CI: 4.78–179.84), being employed (aOR 11.12; 95% CI: 3.10–39.92), smoking (aOR 2.34; 95% CI: 1.03–5.33) and physical activity (aOR 0.34; 95% CI: 0.15–0.76) were independent predictors of having dyslipidaemia.
Conclusions
The prevalence of hypertension, diabetes and dyslipidaemia and their associated risk factors are high among the respondents of Ijegun-Isheri Osun community of Lagos state, Nigeria. This highlights the need for further implementation research and policy directions to tackle NCD burden in urban communities in Nigeria. These strategies must be community specific, prioritizing the various risk factors and addressing them accordingly.
Peer Review reports
The burden of non-communicable diseases (NCDs) continues to increase globally especially in developing countries, with different risk factors contributing to the surge [ 1 ]. This is a result of rapid urbanisation, and westernisation of lifestyle and dietary habits [ 2 , 3 , 4 , 5 , 6 , 7 ]. Low-and middle-income countries (LMICs) are likely to suffer a greater burden of these diseases compared to the developed nations because of their limited healthcare financing for NCDs, and their relatively weak and unprepared health systems for these diseases [ 7 , 8 , 9 , 10 ].
Africa is expected to have the world’s largest increase in NCD deaths over the next decade due to the epidemiologic transition of disease [ 2 ]. In most countries in Sub Saharan Africa, NCDs are now responsible for more than three-quarters of all deaths and this will continue to increase if urgent and evidence-based policies to curtail the trend are not successfully implemented [ 8 , 9 , 11 ]. Furthermore, there are clear gaps in the evidence for successful implementation of NCD interventions within the primary health care setting in Sub Saharan African countries. Models and approaches to properly inform the design of interventions that address the needs of communities and individuals are often lacking in most developing countries like Nigeria [ 12 ]. For many years, public health policies in Nigeria have focused on the control of infectious diseases, with attendant dearth of necessary data for policy decisions on NCDs [ 13 ]. There is a need to pay attention to NCDs in Nigerian communities because these health challenges contribute to economic losses, household poverty and reduction in productivity [ 14 ].
Many of the surveys on NCDs in Nigeria have been largely hospital-based. The few available community surveys have shown differences in urban and rural communities in terms of the burden of NCD risk factors. Alikor et al. [ 15 ] found that 38% of rural residents in Nigeria had 2 or more NCD risk factors while Odugbemi et al. [ 16 ] have reported hypertension prevalence, diabetes, dyslipidaemia and physical inactivity prevalence of 35, 4.6, 47.1 and 92% respectively in traders in a popular Lagos market.
Prevalence rates from direct enumeration of individuals in a representative community provide credible evidence for healthcare planning, allocation of resources and monitoring trajectory of diseases by government agencies. Lagos being the “de facto” industrial capital of Nigeria is a multi-ethnic society undergoing rapid social and lifestyle dynamics of an industrialised urban society. Measuring the prevalence of NCDs in urban communities in Lagos is attractive and provides opportunities for health promotion and policy formulation as it provides a snapshot of the burden of NCDs in such communities.
We thus, set out in this survey to determine the prevalence of NCDs (hypertension, diabetes and dyslipidaemia) and their behavioural risk factors among the Ijegun-Isheri Osun community residents of Lagos, Nigeria.
Study design and setting
This cross-sectional survey was carried out by the NAIJAHEALTH Initiative, a self-funded Non-Governmental Organisation that engages in health promotion in Lagos, Nigeria. The study respondents were residents of the Ijegun- Isheri Osun community, Lagos State, Nigeria who participated in a population preventive health campaign on the 29th and 30th of June, 2018. The sites for the campaign were the Isheri Osun primary healthcare centre, Isheri Osun community market and the Christ apostolic worship centre, Isheri Osun. Residents of this community who were at least 15 years old were recruited consecutively into the study after giving informed consent. Participants who had severe cognitive impairment that mitigated against remembering past events or giving reliable medical history were excluded from the study.
Sample size
Minimum sample size was calculated using the formula [ 17 ]:
N = the minimum sample size
Z α/2 = the standard normal deviate corresponding to a level of significance of 0.05 is 1.96
p = the prevalence rate of hypertension in Abia communities by Ogah et al [ 18 ] i.e. 31.8%.
d = the desired precision: 10%
Applying the formula, the minimum sample size is:
All the 215 respondents who participated in the survey were included in this analysis.
Data collection
Data collection instrument.
A semi structured interviewer administered questionnaire was developed for this survey (see Additional file 1 ). The questionnaire was based on the modified WHO Stepwise protocol which consists of three steps (screening questionnaire, physical indices measurement and biochemical measurement) [ 19 , 20 ]. This is a recommended protocol for epidemiologic studies as it emphasizes collection of good quality data even if the data is small. The questionnaire was divided into subsections of demographic data, medical history, lifestyle risk factors, presenting symptoms and signs, clinical measurements and laboratory test results (see Additional file 1 for further details). The questionnaire was pre-tested before the main study among 10 respondents. The questionnaire was also translated into the Yoruba language which is the local language spoken by most of the populace in the study community. The responses in Yoruba were then translated back into English language before statistical analyses.
Data collection procedure
The study questionnaire as described was used for data collection. This was administered by trained assistants while medical care and advice was given by clinicians involved in the study.
Blood pressure measurements were obtained with a mercury sphygmomanometer according to standard guidelines [ 21 ]. Systolic and diastolic blood pressures were measured at Korotkoff sounds phase I and V, respectively. Two readings were taken at intervals of at least 2 min, and the average of the readings was used to represent the patient’s blood pressure [ 19 ]. If there was > 5 mmHg difference between the first and second readings, additional reading was obtained, and then the average of these multiple readings was used [ 22 , 23 ]. A participant was considered to have hypertension on the basis of self-reported history of hypertension and/or the use of blood pressure-lowering medication and/or documented blood pressure ≥ 140/90 mmHg [ 18 ]. Blood pressure status was categorized into normal, pre-hypertension and elevated blood pressure readings using the cut-offs of the European Society of Cardiology [ 24 ].
Diagnosis of diabetes was based on self-reported history and/or plasma random glucose reading ≥200 mg/dl with clinical signs of diabetes according to the American Diabetes Association [ 25 ]. Smoking status was categorized in to 3 categories. A ‘never smoker’ was someone who had not smoked cigarette in the last 10 years. Occasional or irregular smoker was someone who had smoked at least once in the last 10 years while a regular smoker was defined as someone who smoked at least once a week in the last 10 years.
Alcohol consumption was categorized into three categories. The category ‘Never’ was someone who had never drunk alcohol. Occasional or irregular consumption was ≤monthly consumption and/or 1–2 drinks per day while regular alcohol consumption was defined as drinking > 2 drinks per day. A drink was defined as a bottle or one glass of wine or a shot of spirit.
Regular physical activity was defined as at least 150 min of moderate intensity exercise per week. Irregular physical activity was defined as 30–149 min of moderate intensity physical activity per week while “never” was defined as < 30 min of moderate intensity physical activity per week [ 26 , 27 ].
Plasma blood glucose and lipids (total cholesterol and LDL) using finger-prick blood sample were measured with point-of-care devices. Normal total plasma cholesterol was defined as < 200 mg/dl while normal LDL was defined as < 130 mg/dl. Dyslipidaemia was defined as plasma cholesterol ≥200 mg/dl and/or LDL cholesterol ≥130 mg/dl.
Those who were diagnosed with the conditions reported were counselled and they were provided with health education. They were then referred to the nearest general hospital for follow up. The NAIJAHEALTH program also has volunteers who followed up these individuals in the community through phone calls and home visitations if required.
Data analysis
Data were analysed using Stata version 15 (StataCorp LLC, Lakeway Drive, College Station, Texas, USA). Normality of data was determined using Shapiro-Wilk test. Proportions were used to summarize categorical data while continuous variables were summarized as means (standard deviations) as appropriate. Prevalence of each of the NCDs and cardiovascular risk factors were then calculated. The NCDs were modelled as dependent variables while the socio-demographic and lifestyle risk factors were independent variables. The associations between each of the NCDs, and socio-demographic and lifestyle risk factors were determined using chi square. The odds ratios of each of the NCDs adjusted for the various socio-demographic and epidemiologic cardiovascular risk factors were determined using multivariable logistic regression models. Interaction terms were tested for, in all regression models but there was no significant interaction between any of the variables in the regression models. Finally, Poisson regression analyses were performed to determine the effects of certain co-variates on the clustering of NCDs among the participants. Multivariate models were built using significant variables in initial univariate analyses (purposive confirmatory method) and these models were similar to results obtained by stepwise regression models. The results of the purposive confirmatory approach are presented in this paper. A p value < 0.05 was considered statistically significant in all analyses.
The baseline characteristics of the respondents are shown in Table 1 below. Of the study participants, 41.9% were males and 58.1% were females, with a mean age of 38.4 years. About 11(5.1%) had previous diagnosis of diabetes while 40 (18.6%) had a previous diagnosis of hypertension. Sixty-five individuals (34.4%) frequently consumed more than 2 drinks of alcohol per day while only 14 respondents (7.4%) smoked cigarettes at least once a week. One-fifth of the respondents reported regular physical activity or exercise per week. More than half of those tested had elevated plasma cholesterol level. Among the 171 individuals with blood pressure readings, 50.9, 8.2 and 40.9% had normal, prehypertension and hypertension readings respectively.
Table 2 shows the prevalence of the NCDs and their major risk factors. Hypertension prevalence was 35.3% and similar in both sexes, 4.6% of the subjects had diabetes with no sex difference while 47.9% had dyslipidaemia with a female preponderance (52% in women vs. 42.2% in men).
Less than half of the respondents smoked cigarettes with male preponderance (56.9% in men vs. 31.6% in women). About three-quarters of the respondents consumed alcohol with slight male preponderance while about half of the respondents engaged in exercise with male preponderance (65.3% in men vs. 45.3% in women).
Bivariate analysis using chi-square (see Table 3 below) showed significant association between hypertension and age-group categories. Those who were employed were more likely to have hypertension ( p < 0.001). There was a strong association between hypertension and diabetes with all those who were diabetic also being hypertensives. Both diabetes and dyslipidaemia also showed increased risk with increasing age-group categories. Hypertension and diabetes were each significantly positively associated with having dyslipidaemia while smoking was also associated with dyslipidaemia ( p = 0.01). Physical activity was negatively associated with dyslipidaemia.
When blood pressure and age were modelled as continuous variables, systolic (SBP) and diastolic (DBP) blood pressure showed strong positive linear relationship as shown figure 1 (see Additional file 2 ). Also, each of SBP and DBP showed strong positive linear relationship with age as shown in figures 2 and 3 respectively (see Additional file 2 ).
Age, being employed and dyslipidaemia were independent predictors of hypertension as shown in Table 4 below. Respondents aged ≥60 years were about 5 times more likely to have hypertension in adjusted analyses. Respondents who were employed were 4 times more likely to have hypertension in unadjusted analysis and this was attenuated to about 2-fold increased odds of hypertension in adjusted analyses. Dyslipidaemia conferred a 10-fold increased likelihood of hypertension in unadjusted analysis, but this was attenuated by half to 5-fold increased likelihood of hypertension in adjusted analyses.
Both age and dyslipidaemia were predictors of diabetes in crude analyses, but in adjusted analyses, only age was an independent predictor of diabetes conferring 8.8-fold increased odds of diabetes.
Age, being employed, dyslipidaemia, smoking and hypertension were adverse predictors for having dyslipidaemia while physical activity was protective of having dyslipidaemia in both crude and adjusted analyses. Individuals aged ≥60 years were 30 times more likely to have dyslipidaemia, those who were employed had 11-fold increased odds of having dyslipidaemia, those who smoked were twice at increased likelihood of dyslipidaemia while those with hypertension had 4-fold increased odds of dyslipidaemia. Individuals who engaged in physical activity were 3 times less likely to have dyslipidaemia.
In multivariable Poisson regression, individuals aged ≥60 years had a mean of 2 NCDs while those employed, smokers and the physically inactive each had a mean of 1 NCD as shown in Table 4 (see Additional file 2 ).
Non-communicable diseases have been projected to be a leading cause of morbidity and mortality in Nigeria by 2030 [ 28 , 29 ]. The surveillance of NCD risk factors is one of the key strategies advocated to tackle these emerging public health concerns, particularly in low and middle income countries. This study investigated the prevalence of NCDs and their association with behavioural risk factors in the busy surburb of the Ijegun- Isheri Osun in Lagos State, Nigeria. We found that most of the participants were aged 40 years and above, more than half were female, and majority were married.
Tobacco use, the leading cause of morbidity and mortality globally that claims about 6 million lives annually, was also highly prevalent in this study [ 1 , 30 ]. This finding corroborates reports in India and Bangladesh where prevalence of tobacco use was found to be 34.4 and 43.2% resepectively [ 31 ]. It is known that unhealthy lifestyle habits are prevalent in urban cities and industrial hubs in Nigeria [ 32 , 33 ]. Conversely, low prevalence rates have been reported among the working class in some other parts of Nigeria [ 29 , 34 , 35 ]. These differences could be as a result of civil servants being the focus of previous studies as against this study which participants were general community residents and traders. The sex differences in smoking in this study is in keeping with similar reports in other parts of the country where more males smoked cigarettes than females. This can be attributed to the risk-taking behaviours of men. There was a significant association between increasing age and smoking, which was similar to other existing reports [ 19 ]. Similarly previous health reports have concluded that majority of adult smokers initiated the habit of smoking before the age of 18 years, a finding which supports calls for the extension of tobacco control programs to young adults in order to curtail the habit of smoking as people get older [ 36 , 37 ].
Alcohol consumption and harmful use of alcohol were reported in 32.8 and 34.4% of the respondents respectively. Approximately 2.3 million die each year from the harmful use of alcohol, accounting for about 3.8% of all deaths in the world. More than half of these deaths occur from NCDs including cancers, cardiovascular disease and liver cirrhosis [ 1 ]. A prevalence of 26.9% for alcohol consumption has been reported in urban communities in Ibadan [ 19 ]. The differences in our findings and that of the earlier studies could be due to differences in study populations, the sampling techniques used, and the prevailing lifestyles present in these different communities. Another reason for inconsistent results with the available literature could be due to differences in assessment methods. Previous studies used questionnaires that were not based on the WHO Stepwise protocol while this study used a pretested questionnaire based on the WHO Stepwise protocol [ 20 ].
In our study, incidence of physical activity among the respondents was high (52.9%), which was consistent with previous studies in Ibadan and Abuja, Nigeria which have reported physical activity of 53.6 and 49% respectively among drivers [ 38 , 39 ]. It is interesting that the commonest occupation among Ijegun-Isheri Osun residents is driving. This is especially in keeping with the higher physical activity observed in males. Also, majority of the female respondents in this study were traders who usually sit in their shops throughout the day as reported also in a study in Tejuosho market in Lagos [ 16 ]. Moreover, Lagos is a boisterous city and residents have to engage in demanding jobs and travel long distance daily in search of their daily means of sustenance. However, lower prevalence of physical activity (37.8%) among civil servants in Ibadan have been reported [ 40 , 41 ]. The differences in the findings could be due to the subjective method of assessment in self-reported questionnaires [ 42 ]. Meanwhile, this study used WHO recommendation to classify participants into physical activity categories [ 43 , 44 ]. One plausible reason for high percentage of physical activity in this study was because most participants were young adults with an average age of 38 years. Also, most of them were employed, even though their occupation were not disclosed but leaving home for work place every day might require walking among most participants. This underscores the importance of workplace interventions that encourage physical activity.
Raised blood pressure, the major risk factor for cardiovascular diseases (CVDs) has become a global concern. This is because CVDs are the leading cause of death globally with an estimated 17.5 million deaths yearly, occurring mostly in low-and-middle income countries [ 1 ]. This fact was buttressed in this study where about a third had hypertension, which supports previous findings in other researches in Nigeria [ 39 , 45 ].This is also in keeping with the landmark meta-analysis by Adeloye et al. [ 46 ] who reported prevalence of 30.6% in urban communities in Nigeria. Increasing age has been shown to be a risk factor for raised blood pressure [ 39 , 45 ]. Participants aged 60 years or above were about nine times more likely to be hypertensive compared to those in age group below 60 years.
As a result of aging, changes occurring within the cardiovascular system like thickening of the arterial wall. Thus, the heart does more work in pushing blood against the thickened arterial wall leading to an increase in arterial blood pressure [ 40 , 47 ].However, our study did not show any significant gender difference in the occurrence of hypertension although a systematic review on the current prevalence and pattern of hypertension in Nigeria reported higher prevalence of hypertension among males compared to females [ 40 , 41 , 48 , 49 ]. Being employed and having dyslipidaemia were other predictors of hypertension in this study. The boisterous and stressful life of Lagos with attendant traffic gridlock may contribute to the increased risk of hypertension seen among the respondents who were employed. Dyslipidaemia contributes to atherosclerosis through endothelial dysfunction, inflammation and insulin resistance.
The low incidence of diabetes in the respondents of the Ijegun-Isheri Osun community at the time of this survey is similar to the finding by Ajayi et al. [ 38 ], Oguoma et al. [ 50 ] and Sani et al. [ 51 ] but lower than the reports by Oluyombo et al [ 52 ] . in Ekiti and Agaba et al [ 53 ] . However, Odugbemi et al. [ 16 ] have reported much lower prevalence of diabetes in Tejuosho market in Lagos. Selection bias in our recruitment strategy may explain the difference between our result and the report by Odugbemi et al. [ 16 ] It appears that diabetes prevalence is much higher in Nigeria compared to her neighbouring sub-Saharan countries [ 54 ].
Dyslipidaemia was prevalent in almost half of the respondents at the time of the survey. In addition, age and the lifestyle risk factors predicted those with dyslipidaemia. Dyslipidaemia usually co-exists with obesity and both are important in the pathway to hypertension and atherosclerotic vascular disease. Ogunbode et al. [ 55 ] have coined a mnemonic termed “WASHED” for NCD lifestyle modification and health education in those with obesity in primary care settings. “WASHED” stands for weight control, alcohol reduction, smoking cessation, health promotion, exercise and diet. We have shown in our study the important role of smoking and physical activity as dominant risk factors of dyslipidaemia. We believe that health promotion and education in the community and primary care settings geared towards smoking cessation, increased physical activity and healthy diet would play critical roles in stemming the tide of atherosclerotic vascular diseases in Nigeria. This will require concerted efforts by stakeholders and policy makers if Nigeria is to achieve the 2025 voluntary targets of the Global NCD Action Plan [ 53 ].
This study is an important contribution to the surveillance of NCD risk factors in Nigeria. Even though it is not a nationally representative survey, an assessment of respondents in one community in one of the largest cities in Nigeria can give a minuscular view and snapshot of the drivers of NCDs within the larger population until the time when nationally representative surveys would be conducted in Nigeria.
The study is not without limitations. This was a cross-sectional study and it is difficult to prove temporal associations and causality between the NCDs and the epidemiologic NCD risk factors. A longitudinal study in the future would be helpful to investigate these relationships. Also, our sample size is modest and may have biased some of the estimates.
Furthermore, the consecutive recruitment method used in this study is an important limitation of the study and may have resulted in the recruitment of more individuals with background health challenges and subsequent overestimation of the prevalence and effect sizes of the NCDs reported. Moreover, the reported incidence of the NCDs in this survey only provides a glimpse into the NCDs among the residents of Ijegun-Isheri Osun community at the time of the survey. The estimates are specific for this sample of respondents only. The estimates may be different on different days of the weeks or even different weekend days if there is a differential participation of individuals with chronic medical ailments at different time points. However, by allowing everyone in the community to participate, we provided equal chance for participation in the survey and the reported estimates are similar to other reports in Lagos. Despite this, caution should be exercised in generalising the reported estimates to the whole of the Ijegun-Isheri Osun community or other communities in Lagos.
We depended on the verbal reports of the respondents to ascertain their smoking status and alcohol consumption. Some of them may have underreported their previous diagnosis of hypertension or diabetes, use of tobacco and alcohol consumption. We however measured their blood pressure and plasma glucose levels which were also used in making diagnosis of hypertension and diabetes. It is difficult in epidemiologic surveys to exclude misclassifications of lifestyle behaviours in totality. Although, obesity is one of the four metabolic risk factors of NCDs, it was not assessed in this study. However, we have measured blood cholesterol levels which are more important in the pathophysiologic pathway to cardiovascular diseases [ 56 , 57 ]. Cross tabulation of behavioural risk factors by socio-demographic factors was not computed which makes it difficult to observe the categories of participants that exhibited one habit more than the other. We perhaps underestimated the level of physical inactivity in our study because of the subjective method of assessment in the use of self-reported questionnaires. For future studies, using more objective means of assessing physical activity like pedometers and accelerometers would give more accurate estimates.
In conclusion, we have shown the prevalence of common NCDs and their risk factors among respondents of the Ijegun-Isheri Osun community in Nigeria’s most busy city at the time of this survey. Many of these risk factors are modifiable and this underscores the importance of health promotion and education in reducing the burden of NCDs in Nigeria. Larger surveys of these nature are needed for policy formulation. We plan to conduct more surveys across Nigeria’s 6 socio-political regions in the future.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Adjusted odds ratio
Cardiovascular Diseases
Diastolic blood pressure
Low- and middle-income countries
Non communicable diseases
Systolic blood pressure
Weight control, alcohol reduction, smoking cessation, health promotion, exercise and diet
World Health Organisation
WHO. Global status report on noncommunicable diseases 2010. Geneva: WHO; 2011.
Islam SMS, et al. Non communicable diseases (NCDs) in developing countries: a symposium report. Glob Health. 2014;10(81):1–7.
Alwan AD, Galea G, Stuckler D. Development at risk: addressing noncommunicable diseases at the United Nations high-level meeting. Bull World Health Organ. 2011;89(8):546–546A.
Crush, Jonathan, Bruce Frayne and Milla McLachlan. “Rapid Urbanization and the Nutrition Transition in Southern African.” Urban Food Security Series No. 7. Queen’s University and AFSUN: Kingston and Cape Town. 2011. .
Khorrami et al. Urbanization and noncommunicable disease (NCD) risk factors: WHO STEPwise Iranian NCD risk factors surveillance in 2011. EMHJ. 2017;23(7):469–79.
Bricas N. Urbanization Issues Affecting Food System Sustainability. in 1–25; 2019. https://doi.org/10.1007/978-3-030-13958-2_1 .
Book Google Scholar
Maher D, Sekajugo J. Research on health transition in Africa: time for action. Health Res Policy Syst. 2011;9:1–4.
Panda R, Mahapatra S, Persai D. Health system preparedness in noncommunicable diseases: findings from two states Odisha and Kerala in India. J Fam Med Prim Care. 2018;7:565.
Article Google Scholar
Kengne AP, Mayosi BM. Readiness of the primary care system for non-communicable diseases in sub-Saharan Africa. Lancet Glob Health. 2014;2(5):e247–8.
Kankeu HT, Saksena P, Xu K, Evans DB. The financial burden from non-communicable diseases in low- and middle-income countries: a literature review. Health Res Policy Syst. 2013;11(31):1–12.
WHO. Noncommunicable Diseases Country Profiles. Geneva; 2014. p. 1–207.
de-Graft Aikins A, et al. Tackling Africa’s chronic disease burden: From the local to the global. Globalization Health. 2010;6(5):1–7.
Gounder CR, Chaisson RE. A diagonal approach to building primary healthcare systems in resource-limited settings: women-centred integration of HIV/AIDS, tuberculosis, malaria, MCH and NCD initiatives. Trop Med Int Health. 2012;17:1426–31.
Article PubMed Google Scholar
Joshi R, et al. Task shifting for non-communicable disease management in low and middle income countries - a systematic review. PLoS One. 2014;9(8):e103754.
Alikor CA, Emem-Chioma P. Clustering of cardiovascular disease risk factors in a rural adult population in Nigeria. Int J Res Med Sci. 2018;6:765–71.
Odugbemi T, Onajole A, Osibogun A. Prevalence of cardiovascular risk factors amongst traders in an urban market in Lagos, Nigeria. Niger Postgr Med J. 2012;19:1–6.
CAS Google Scholar
Lwanga SK, Lemeshow S. Sample size determination in health studies: a practical manual. WHO: WHO; 1991. https://doi.org/10.2307/2290547 .
Ogah OS, et al. Cardiovascular risk factors and non-communicable diseases in Abia state , Nigeria : report of a community- based survey. Int J Med Biomed Res. 2013;2:57–68.
Ajayi I, Sowemimo I, Akpa O, Ossai N. Prevalence of hypertension and associated factors among residents of Ibadan - North LocalGovernment Area of Nigeria. Niger J Cardiol. 2016;13:67–75.
World Health Organization. A framework for surveillance: the WHO STEPwise approach to Surveillance of noncommunicable diseases (STEPS). Geneva: World Health Organization. A framework for surveillance: the WHO STEPwise approach to Surveillance of noncommunicable diseases (STEPS). Geneva: World Health Organization; 2003.
Google Scholar
World Health Organization/ International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension statement on management of hypertension. J Hypertens. 2003;21:1983–92.
American Society of Hypertension. Recommendations for routine blood pressure measurement by indirect cuff sphygmomanometry. Am J Hypertens. 1992;5:207–9.
World Health Organization International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/ International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983–92.
Williams B, et al. 2018 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC). Blood Press. 2018;27(6):314–40.
American Diabetes Association, A. A. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2007;30(Suppl 1):S42–7.
NCDs. Global Strategy on Diet, Physical Activity and Health - 2004. Geneva: WHO; 2018.
Egan BM. Physical Activity and Hypertension Knowing Is Not Enough; We Must Apply. Willing Is Not Enough; We Must Do—von Goethe. Hypertension. 2017;69:404–6.
WHO. Noncommunicable diseases: the slow motion disaster. Geneva: WHO; 2017.
Maiyaki M, Garbati M. The burden of non-communicable diseases in Nigeria; In the context of globalization. Ann Afr Med. 2014;13:1–10.
World Health Organization. Global Status Report On Noncommunicable Diseases 2014. (2014).
Agaku IT, et al. Poly-tobacco use among adults in 44 countries during 2008-2012: evidence for an integrative and comprehensive approach in tobacco control. Drug Alcohol Depend. 2014;139:60–70.
Osalusi B, Uantioje E, Ogun S, Afe T, Adeeko O. The prevalence of hypertension among the adults in a semiurbarn community in south West Nigeria. Int J Med Heal Res. 2017;3:93–9.
Lano-Maduagu AT, Oguntona C, Oguntona E, Agbonlahor M, Onabanjo OO. Prevalence of coronary heart diseases risk factors in adults population living in Nigeria’s largest Urban City. J Nutr Disord Ther. 2015;5:1–5.
Oladimeji AM, Fawole O, Nguku P, Nsubuga P. Prevalence and factors associated with hypertension and obesity among civil servants in Kaduna, Kaduna State, June 2012. Pan Afr Med J. 2014;18:13.
Article PubMed PubMed Central Google Scholar
Ige OK, Owoaje ET, Adebiyi OA. Non communicable disease and risky behaviour in an urban university community Nigeria. Afr Health Sci. 2013;13:62–7.
CAS PubMed PubMed Central Google Scholar
Services, U. S. D. of H. and H., Prevention, C. for D. C. and, Promotion, N. C. for C. D. P. and H. & Health, O. on S. and. Executive Summary (The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General). 2014. 1–36. doi: NBK179276.
Puckrein GA, Egan BM, Howard G. Social and medical determinants of Cardiometabolic health: the big picture. Ethn Dis. 2015;25:521–4.
Odeyinka OT, Ajayi IO. Prevalence of hypertension and diabetes and their determinants among commercial drivers in Ibadan. Niger J Cardiol. 2017;14:75–83.
Ojji D, Stewart S, Ajayi S, Manmak M, Sliwa K. A predominance of hypertensive heart failure in the Abuja Heart Study cohort of urban Nigerians : a prospective clinical registry of 1515 de novo cases. 2013:835–42. https://doi.org/10.1093/eurjhf/hft061 .
Adeoye AM, et al. Early diastolic functional abnormalities in normotensive offspring of Nigerian hypertensives. Cardiovasc J Afr. 2012;23:255–9.
Article CAS PubMed PubMed Central Google Scholar
Zuhlke L, et al. Characteristics, complications, and gaps in evidence-based interventions in rheumatic heart disease: the Global Rheumatic Heart Disease Registry (the REMEDY study). Eur Heart J. 2015;36:1115–22a.
Craig CL, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
WHO. Global recommendations on physical activity for health. Geneva: World Health Organisation; 2010. p. 1–58.
Pacific Physical Activity Guidelines for Adults. Framework for Accelerating the Communication of Physical Activity Guidelines. Manila: World Health Organization Regional Office for the Western Pacific Region; 2009.
Oguoma VM, Nwose EU, Richards RS. Prevalence of cardio-metabolic syndrome in Nigeria: a systematic review. Public Health. 2015;129:413–23.
Article CAS PubMed Google Scholar
Adeloye D, Basquill C, Aderemi AV, Thompson JY, Obi FA. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. J Hypertens. 2015;33:230–42.
Commodore-Mensah Y, et al. The afro-cardiac study: cardiovascular disease risk and acculturation in west African immigrants in the United States: rationale and study design. J Immigr Minor Health. 2016;18:1301–8.
Akinlua JT, Meakin R, Umar AM, Freemantle N. Current prevalence pattern of hypertension in Nigeria : a systematic review. PLoS One. 2015;10:1–18.
Adeoye AM, et al. Circadian blood pressure variation amongst people with chronic kidney diseases: a pilot study in Ibadan. Niger Postgrad Med J. 2017;24:131–6.
Oguoma VM, et al. Prevalence of cardiovascular disease risk factors among a Nigerian adult population : relationship with income level and accessibility to CVD risks screening. BMC Public Health. 2015;15:397–412.
Sani MU, Wahab KW, Yusuf BO, Gbadamosi M, Johnson OV. Modifiable cardiovascular risk factors among apparently healthy adult Nigerian population - a cross sectional study. BMC Res Notes. 2010;3:11–21.
Oluyombo R, Olamoyegun MA, Olaifa O, Iwuala SO, Babatunde OA. Cardiovascular risk factors in semi-urban communities in Southwest Nigeria: patterns and prevalence. J Epidemiol Glob Health. 2015;5:167–74.
Agaba EI, et al. A survey of non-communicable diseases and their risk factors among university employees: a single institutional study. Cardiovasc J Afr. 2017;28:377–84.
Adeloye D, et al. Estimating the prevalence , hospitalisation and mortality from type 2 diabetes mellitus in Nigeria: a systematic review and meta-analysis. BMJ Open. 2017;7:1–16.
Ogunbode A, Owolabi M, Ogunniyi A, Ogunbode O. Weight control, alcohol reduction, smoking cessation, health promotion, exercise and diet ( WASHED )’: a mnemonic for lifestyle modification in obesity. Niger J Clin Pr. 2015;18:831–2.
Article CAS Google Scholar
Upadhyay RK. Emerging Risk Biomarkers in cardiovascular. J Lipids. 2015;2015:1–50.
Addo SA, Nti C, Vuvor F, Adjimani J, Steiner-asiedu M. Impact of successful weight loss maintenance on serum lipids and glucose concentrations of previous participants of a weight loss Programme in Accra , Ghana. J Nutr Metab. 2019;2019:1–12.
Download references
Acknowledgements
We thank the residents of Ijegun-Isheri Osun, Lagos state, who willingly participated in this study to expand the frontiers of knowledge. We thank the research assistants who made the conduct of this work easy.
This work was self-funded by the authors.
Author information
Authors and affiliations.
Department of Population Health, Faculty of Epidemiology and Population Health, London School of Hygiene and Tropical Medicine, University of London, London, UK
Israel Oluwaseyidayo Idris, Ekow Adom Mensah & Noriko Kitamura
Disease Control and Surveillance Team, Department of Primary Health Programmes, NAIJAHEALTH Initiative, Lagos, Nigeria
Israel Oluwaseyidayo Idris, Ayodipupo Sikiru Oguntade, Ekow Adom Mensah & Noriko Kitamura
Department of Social and Preventive Medicine, V. N Karazin Kharkiv National University, Kharkiv, Ukraine
Israel Oluwaseyidayo Idris
Health Policy and Governance Unit, Department of State Management and Public Administration, Kharkiv National University of Economics, Kharkiv, Ukraine
Department of Medicine, University College Hospital, Ibadan, Nigeria
Ayodipupo Sikiru Oguntade
Institute of Cardiovascular Science, University College London, London, UK
Department of Family Medicine, Korle-Bu Polyclinic, Accra, Ghana
Ekow Adom Mensah
Institute of Tropical Medicine, Nagasaki University, Nagasaki, Japan
Noriko Kitamura
Department of Disease Control, Graduate School of Public Health and Tropical Medicine, Tulane University, New Orleans, USA
You can also search for this author in PubMed Google Scholar
Contributions
IOI conceptualised this study, secured funding for the survey, supervised the survey and participated in data analysis and report writing. ASO conceptualised this study, planned the methodology, analysed the data and participated in report writing. EAM conceptualised this study, organised data management, participated in data analysis and report writing. NK involved in study conceptualisation, analysed the data and participated in report writing. All authors read the final draft of the manuscript and take full responsibility for the findings reported. The authors read and approved the final manuscript.
Authors’ information
Israel O. Idris, MD, MPA, MScPH; Ayodipupo S. Oguntade, MBChB, MSc, MSc, MWACP; Ekow A. Mensah, MBChB, MSc; Noriko Kitamura, Bachelor of Medicine, MPH&TM
Corresponding author
Correspondence to Ayodipupo Sikiru Oguntade .
Ethics declarations
Ethics approval and consent to participate.
The study protocol and conduct adhered to the principles laid down in the Declaration of Helsinki. Ethical clearance was obtained from the Lagos State Ministry of Health, Nigeria. Written informed consent was obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Data collection instrument. NAIJAHEALTH survey interviewer administered questionnaire.
Additional file 2.
Supplementary analyses. Supplementary Table and Figures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Idris, I.O., Oguntade, A.S., Mensah, E.A. et al. Prevalence of non-communicable diseases and its risk factors among Ijegun-Isheri Osun residents in Lagos State, Nigeria: a community based cross-sectional study. BMC Public Health 20 , 1258 (2020). https://doi.org/10.1186/s12889-020-09349-2
Download citation
Received : 22 April 2020
Accepted : 04 August 2020
Published : 18 August 2020
DOI : https://doi.org/10.1186/s12889-020-09349-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Non-communicable diseases
- Hypertension
- Dyslipidaemia
- Physical activity
- Risk factors
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Open access
- Published: 20 August 2024
Investigation of non-communicable diseases prevalence, patterns, and patient outcomes in hospitalized populations: a prospective observational study in three tertiary hospitals
- Alemu Belayneh ORCID: orcid.org/0000-0003-0039-4348 1 ,
- Legese Chelkeba ORCID: orcid.org/0000-0002-0323-5011 1 , 2 ,
- Firehiwot Amare MPharm 1 ,
- Henok Fisseha ORCID: orcid.org/0000-0002-6195-1251 5 ,
- Senbeta Guteta Abdissa ORCID: orcid.org/0000-0002-9378-9113 3 ,
- Mirgissa Kaba ORCID: orcid.org/0000-0002-2380-4779 4 ,
- Shivani A. Patel 2 &
- Mohammed K. Ali 2
Journal of Health, Population and Nutrition volume 43 , Article number: 128 ( 2024 ) Cite this article
Metrics details
Non-communicable diseases (NCDs) pose a significant global health challenge, constituting over 80% of mortality and morbidity. This burden is particularly pronounced in low- and middle-income countries (LMICs), including Ethiopia. Despite this, there’s limited research on this issue in Africa. This study aims to investigate the prevalence, patterns, and outcomes of NCDs in hospitalized populations across three tertiary hospitals in Ethiopia.
A hospital-based cohort study (August 2022 - January 2023) included patients aged 14 and older diagnosed with cardiovascular diseases (CVDs), diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), asthma, or cancer at three Ethiopian hospitals. Data on demographics, socio-economic factors, clinical characteristics, and outcomes were collected through medical records and interviews. Logistic regression identified factors independently associated with in-hospital mortality, with p ≤ 0.05 considered statistically significant.
In the study across three tertiary hospitals involving 2,237 patients, we uncovered the impact of NCDs. About 23.4% of patients struggled with NCDs, with cardiovascular diseases (53.3%), cancer (29.6%), diabetes (6.1%), and respiratory diseases (6.5%) being the most prevalent. Notably, among those affected, women comprised a slight majority (55.1%), with the average patient age being 47.2 years. Unfortunately, 15.3% of patients with NCDs faced in-hospital mortality. Our analysis revealed predictors of mortality, including cancer diagnosis (adjusted odds ratio [AOR]:1.6, 95% CI: 1.2–1.8, p = 0.01), medication adherence ( AOR: 0.36, 95% CI: 0.21–0.64, p < 0.001), concurrent infections (AOR: 0.36, 95% CI: 0.16–0.86, p < 0.001), chronic kidney diseases (CKD) (AOR: 0.35, 95% CI: 0.14–0.85, p = 0.02), and complications during hospitalization (AOR: 6.36, 95% CI: 3.45–11.71, p < 0.001).
Our study reveals a substantial prevalence of NCDs among hospitalized patients, affecting approximately one in four individuals, primarily with CVDs and cancer. Alarmingly, a significant proportion of these patients did not survive their hospitalization, emphasizing the urgent need for targeted interventions to enhance outcomes in this population.
Non-communicable diseases (NCDs) have emerged as a pressing global health challenge, imposing a significant burden of morbidity and mortality [ 1 ]. NCDs are the leading cause of death globally, claiming 41 million lives annually, which accounts for 71% of all global fatalities. Four major culprits contribute to over 80% of premature NCD-related deaths: cardiovascular diseases (CVDs), causing 17.9 million deaths annually, cancer (9.0 million), respiratory diseases (3.9 million), and diabetes (1.6 million) [ 2 , 3 ]. They disproportionately affect low- and middle-income countries (LMICs), particularly in Sub-Saharan Africa [ 4 ]. Over the past two decades, NCDs, driven by cardiovascular risk factors like unhealthy diets, inactivity, hypertension, obesity, diabetes, high cholesterol, and air pollution, have surged in this region [ 5 , 6 ]. Projections suggest that NCDs are on a trajectory to surpass the combined impact of communicable, maternal, neonatal, and nutritional (CMNN) diseases, becoming the leading cause of mortality in Sub-Saharan Africa by 2030 [ 7 , 8 ].
The surge in NCDs within LMICs is propelled by population ageing, rapid urbanization, and lifestyle changes [ 9 ]. Additionally, many LMICs, including Ethiopia, face a high incidence of communicable diseases and an overburdened healthcare system, intensifying the impact of NCDs, such as premature mortality [ 10 ]. Approximately 48% of NCDs in LMICs occur in individuals below the age of 70, compared to 28% in high-income countries (HICs) [ 11 ]. Ethiopia, in East Africa, is experiencing significant demographic and epidemiological transformations [ 12 ]. Rapid urbanization, globalization, and climate change are shaping the country’s evolving landscape [ 13 , 14 ].Despite government initiatives like the 2003 health extension program improving life expectancy and reducing infectious, maternal, and child deaths, Ethiopia faces challenges from a shifting population pyramid [ 12 ]. Socio-economic shifts, lifestyle changes, and globalization have initiated a nutrition transition from traditional, healthful diets to processed and fast foods [ 15 , 16 , 17 ]. Consequently, Ethiopia is undergoing an epidemiological shift from communicable diseases to chronic conditions [ 12 ].
Hospitalized populations, dealing with complex health conditions, require intensive medical attention, and the burden of NCDs significantly strains healthcare systems, particularly during hospitalizations. Previous studies using Health Information Management System (HMIS) data have shown rising trends in NCDs among inpatients in developed eastern coastal China [ 18 ], Nepal [ 19 ], Nigeria [ 20 ] and Myanmar [ 21 ].
While considerable research has been conducted on NCDs in Ethiopia [ 9 , 22 , 23 ], there is a gap in understanding the prevalence, patterns, and outcomes associated with these diseases specifically within hospitalized populations. This research aims to address this gap by investigating the prevalence, evolving patterns, and outcomes of NCDs during hospitalization. Identifying such nuanced information is vital for informing targeted interventions, optimizing healthcare resource allocation, and improving the overall quality of care for individuals affected by NCDs in hospital settings.
Methods and materials
The study was conducted at three healthcare facilities in Addis Ababa, Ethiopia: Tikur Anbessa Specialized Hospital (TASH), St. Paul Hospital Millennium Medical College (SPHMMC), and Yekatit 12 Hospital (YH). TASH, established in 1972, is the largest referral hospital in Ethiopia. It serves a diverse population with varying socio-economic and demographic backgrounds and offers a wide range of specialized clinical services. SPHMMC, founded in 1968, operates as a teaching hospital with a bed capacity of 700 and initiated Ethiopia’s first integrated modular and hybrid problem-based curriculum for undergraduate medical education in 2007. YH, established in 1923, is also a tertiary-level referral and teaching hospital that provides comprehensive inpatient and outpatient care, serving a large population from both the city and different parts of the nation, including cancer patients.
Study design and period
This was a prospective observational follow-up focusing on patients admitted to the internal medicine, gynaecology and obstetrics and oncology wards during the follow up period from August 2022 to January 2023. We followed-patients until death or discharged to different area (intensive care unit, home, other institution, and wards).
Study population
The study included all eligible patients admitted to the internal medicine, gynaecology, obstetrics, and oncology wards at TASH, SPHMMC, and YH, covering various NCDs such as heart failure, coronary heart disease, cerebrovascular disease, atrial fibrillation, peripheral arterial disease, rheumatic heart disease, hypertension, deep vein thrombosis, pulmonary embolism, cancer (both solid and liquid tumours), and chronic respiratory diseases (asthma and COPD).
Inclusion criteria and exclusions in patient selection
We included patients aged 14 years and older with confirmed NCDs diagnoses in our study. In our facility, adolescent patients in this age group are admitted to adult wards as there is no separate ward for them, and they receive treatment in a manner similar to adults. We chose to incorporate them into our research due to their willingness to cooperate and respond to interview questionnaires. Patients aged less than 14 years as well as those who declined to participate or had incomplete medical records were excluded from the study.
Study variables
Dependent variables : Proportion of NCDs among hospitalized population during study period = (number of admitted patients with NCDs / total number of admissions) x 100. Other dependent variables included were mortality, length of hospital stay, readmission rate within 30-day of discharge, and complications and prescription patterns of key drugs at discharge. Complication was defined as any conditions the patients developed during hospital stay such as hospital acquired infection, bleeding, adverse reaction to medications, organ failure (e.g. acute renal injury, respiratory failure, delirium, etc…). Independent variables : Age, gender, socio-economic factors (monthly income, education and employment), lifestyle factors (physical activity), behavioural factors (drinking and smoking habits), marital status, residency (urban/rural), family history of NCDs, self-reported adherence to medications and concomitantly occurring conditions.
Data collection tool
The data collection process was carried out using a comprehensive tool specifically designed in accordance with the study objectives and tailored to the local context. This tool was designed to gather detailed demographic information, medical history, lifestyle factors, and clinical outcomes of patients admitted with non-communicable diseases. The instrument was based on established clinical assessment protocols, validated questionnaires (such as the World Health Organization (WHO) STEPS questionnaire for risk factors assessment), and electronic health record data extraction templates. Three trained nurses and 3 pharmacists collected data using standardized procedures, ensuring consistency and reliability. Patients admitted with NCDs, including CVDs, DM, chronic respiratory diseases, and cancers, were included in the data collection process. The quality of the data collection tool was assessed through pilot testing, inter-rarer reliability checks, and on-going monitoring to ensure accuracy and completeness of data. Additionally, regular training sessions and supervision were provided to maintain data collection standards and address any challenges encountered during the study period.
Data analysis
Continuous variables (age, monthly income, length of hospital stay) were presented as mean (SD) or median with interquartile range (IQR), while categorical variables (gender, occupation, marital status, place of residence, family history, current smoking status, alcohol drinking status, physical activity, medication adherence, concomitant infection during admission, CKD, epilepsy, readmission within 30 days of discharge, complication during hospital stay, mortality) were expressed as percentages and frequency. The chi-squared test assessed associations between mortality and different NCDs. Binary and multivariate logistic regression analyses, including variables with p-values < 0.2 in univariate analysis, identified predictors of mortality. Significance was set at p ≤ 0.05, and results were reported with 95% confidence intervals. SPSS version 25 facilitated data analysis.
Ethical clearance
Ethical approval was obtained from the School of Pharmacy, College of Health Sciences at Addis Ababa University Ethical Review Committee. Permissions were also sought from each department involved. Informed consent was obtained from all study participants, who were fully informed about the study objectives and given the option to decline or participate. Patient identification numbers were used instead of names to ensure confidentiality.
Baseline characteristics of the included patients
Our study covered a total of 2,237 inpatient visits across three distinct medical institutions in Ethiopia: Tikur Anbessa Specialized Hospital (TASH, n = 1,111), Yekatit 12 Hospital (YH, n = 671), and St. Paul’s Hospital Millennium Medical College (SPHMMC, n = 455). These data were collected over the period from October 2022 to January 2023. Within this patient cohort, 523 admissions were attributed to a range of NCDs, including (CVDs, n = 279, 53.3%), cancer ( n = 155, 29.6%), (DM, n = 32, 6.1%), respiratory diseases ( n = 34, 6.5%), and a combination of CVDs and DM ( n = 23, 4.4%). Consequently, the proportion of patients with NCD among hospitalized patients within our sample was calculated as 23.4% (523 out of 2,237).
Table 1 presents characteristics of patients hospitalized with NCDs. Admissions were distributed across TASH (49%), SPHMMC (27.5%), and YH (23.5%). Gender leaned slightly female (55.1%), with middle-aged adults (51.1%) being the most common age group. The mean average age of the patients was 47.2 ± 18.1. Most patients were urban (76.9%) and married (66.2%). Education varied, with many completing primary school (33.5%) or college/university (26%). Notably, 36.3% reported monthly incomes exceeding $100, while smaller percentages reported ‘no income’ (1.3%), ‘refused to tell’ (11.3%), or ‘I do not know’ (6.5%), indicating income uncertainty among some respondents. The median range of monthly income of the participants was $88.4 (IQR = $33-$154). Additionally, about 31.5% of patients had a family history of at least one NCD. Few engage in regular physical activity (6.5%). The majority of patients exhibit an extensive disease history, accounting for 97.9% (512 individuals). The median duration since diagnosis stands at 12 months, with an IQR spanning from 2 months to 48 months. In terms of concurrent health conditions accompanying NCDs, it was observed that 28.5% of patients presented with additional medical issues during their hospitalization. Among these co-existing conditions, infections of various types were the most prevalent (27.5%), followed by CKD (24.8%) and tuberculosis (12.6%).
Patterns of NCDs among inpatient by demographic and socio-economic characteristics
Among male participants, the most prevalent NCD among hospitalized patients was CVDs at 52.3%, followed by cancer (31.5%). Similarly, female participants exhibited CVDs as the predominant NCD at 54.5%, followed by cancer (27.8%) (Fig. 1 ).

Patterns of NCD in hospitalized patients by demographic and socioeconomic characteristics. NCD: Non-Communicable Disease, CVD: Cardiovascular Disease, DM: Diabetes Mellitus, RD: Respiratory Disease. *Included patients with no reported income [ 7 ], those who were uncertain (59), and those who refused to disclose their income [ 34 ]
A higher percentage of hospitalized seniors were having CVDs (67.2%), with middle-aged adults also showing a substantial proportion (50.2%), whereas a relatively lower percentage of adolescent and young adults were having CVD (48.6%). Conversely, with cancer a larger percentage comprises adolescent and young adults (42.1%), followed by middle-aged adults (30.3%), with a significantly lower representation among senior adults (12.1%) (Fig. 2 ). Overall, CVDs and cancer comprised 82.9% of NCDs among admitted patients.

Pattern of NCDs by age category. DM: diabetes mellitus, RD: respiratory disease, CVD: cardiovascular disease, NCDs: non-communicable diseases
Regardless of education, CVDs were the most common conditions, ranging from 51.3 to 55.7% in different education groups, followed by cancer. Retired individuals had the highest rate CVDs at 68.0%, while employed and unemployed patients showed similar NCD admission proportions, with more cancer cases among the unemployed. Overall, CVDs affected the majority (53.5%).
In our study, heart failure emerged as the predominant CVD in hospitalized patients, representing 35.1% of cases, followed by stroke at 14.3%. Notably, heart failure combined with chronic rheumatic valvular heart disease contributed to 10.1% cases, while venous thromboembolism and hypertension accounted for 9.7% and 3% of cases, respectively. Additionally, coronary heart diseases were responsible for 2.3% of the total cases (Fig. 3 ). Primary cancer types among the hospitalized patients were predominantly haematological cancers, encompassing approximately 105 cases, which represented 67.7% of all cancer-related admissions. Within this category, acute lymphoblastic leukaemia (ALL) had the highest representation at 27.7%, followed by acute myeloid leukaemia (AML) at 18.7%, and chronic lymphocytic leukaemia (CLL) at 12.9%. In the realm of solid tumours, cervical cancer was the most prevalent at 8.4%, followed by ovarian cancer (8.4%) and breast cancer (3.2%) (Fig. 4 ). Among respiratory disorders, asthma prevailed, affecting 70.6% of respiratory cases, while chronic obstructive lung diseases were present in 29.4% of hospitalized patient population. Furthermore, our analysis revealed the most common combination of CVDs and DM resulting was heart failure with DM, representing 52.2% of cases. Hypertension with DM and coronary heart diseases with DM followed closely at 17.4% each, while peripheral artery disease contributed to 8.7% of the cases. The combination of dyslipidaemia and DM was the least common, accounting for 4.4% of cases.

Frequency of CVDs among hospitalized patients. *Heart failure + atrial fibrillation [ 5 ], Heart failure + coronary heart diseases [ 6 ], Atrial fibrillation [ 2 ], Atrial fibrillation + rheumatic heart disease [ 6 ], Hypertension + stroke [ 9 ], Rheumatic heart disease [ 7 ], Heart failure + venous thromboembolism [ 6 ], Heart failure + asthma [ 1 ], Coronary heart diseases + peripheral artery disease [ 2 ], Heart failure + atrial fibrillation + rheumatic heart disease [ 3 ], Heart failure + hypertension [ 8 ], Peripheral artery disease [ 1 ], Dyslipidemia [ 1 ]

Frequency of cancer types among hospitalized patients
Prescription pattern of discharge medications
In our CVD patient group, diuretics were the most common discharge medications (37.9%, n = 198), followed by anticoagulants (36.5%, n = 191), and statins (24.1%, n = 126). Notably, 9.2% ( n = 48) required insulin for DM management. Among patients with respiratory conditions, the primary choice was short-acting beta-agonists (6.1%, n = 32), followed by inhalation corticosteroids (4.8%, n = 25). Oral corticosteroids were less common, with only 2.7% ( n = 14) of prescriptions (Fig. 5 ).

Number of patients received discharge medications. CVDs: cardiovascular diseases, DM: diabetes mellitus, ACE inhibitors: Angiotensin converting enzyme inhibitors, ARBs: Angiotensin receptor blockers
Outcomes of patients admitted due to NCDs
Eighty individuals ( n = 80, 15.3%) did not survive the hospitalization. For those patients who survived ( n = 443, 84.7%), a significant portion, approximately 405 individuals (77.4%), were discharged and able to return to their homes. A smaller subgroup, comprising around 10 patients (1.9%), necessitated admission to the intensive care unit (ICU) during their hospitalization. Additionally, roughly 16 patients (3.1%) were transferred to other wards within the hospital, while approximately 12 patients (2.3%) were referred to external healthcare institutions for further medical attention. Within the study period, 7.5% of the admitted patients experienced readmission, and 38.8% developed complications during their hospital stay (Fig. 6 ). Furthermore, the analysis revealed that the median duration of hospitalization for all patients in the study was 9 days, with a notable interquartile range of 6–15 days.
Relationship between NCD and mortality among hospitalized patients
Relationship between NCD and mortality in hospitalized patients
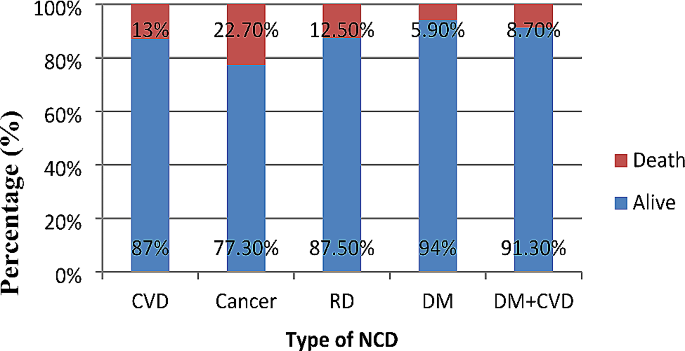
Figure 7 illustrates various patterns of in hospital-mortality among hospitalized patients with NCDs. Among these patterns, cancer exhibited the highest mortality rate at 22.7%, followed by CVDs at 13%, DM at 12.5%, and respiratory disorders with the lowest mortality rate of 5.9%. Statistical analysis indicates a significant association between NCDs related hospital admission and patient mortality (χ2 = 10.8, p = 0.02).

Patterns of in hospital-mortality among hospitalized patients with NCDs
Predictors of mortality in patients with NCDs
Patients with cancer had 50% more mortality compared to patients with CVDs (AOR: 0.5, 95%CI: 0.2–0.8, p = 0.01]. Patients who adhered to their outpatient prescribed medications were 64% less likely to die compared to non-adherent patients (AOR: 0.36, 95% CI: 0.21–0.64, p < 0.001). Patients without infection had a 64% lower risk of mortality compared to those with infection (AOR: 0.36, 95% CI: 0.16–0.86, p < 0.001). Patients without CKD had a 65% lower risk of mortality compared to patients with CKD (AOR: 0.35, 95% CI: 0.14–0.85, p = 0.02). Furthermore, patients with complications during their hospital stay were about 6.4 times more likely to die compared to patients without complications (AOR: 6.36, 95% CI: 3.45–11.71, p < 0.001) (Table 2 ).
In settings where community-based studies and comprehensive data on NCDs are lacking, hospital-based studies serve as vital tools for evaluating the health status of the community served by the hospital. Our study on the patterns of NCDs among hospitalized patients provides valuable insights into the complex interplay of various factors influencing disease prevalence and outcomes.
Our findings highlight that CVDs and cancer collectively constitute a substantial 82.3% of NCD cases among hospitalized patients. This observation is consistent with similar studies conducted in Ethiopia and other African countries [ 22 , 24 , 25 , 26 ]. However, contrasting findings from a study in Nigeria show that CVDs, endocrine, and renal conditions collectively comprise the majority (78%) of NCD cases [ 27 ].The variance in findings underscores the influence of regional and contextual factors on disease prevalence. It is noteworthy that our study encompassed a broader spectrum of specialities, including gynaecology, obstetrics, oncology, and medical wards, which may account for differences in disease rankings compared to studies focused solely on medical wards in Nigeria. This broader scope is particularly significant in countries like Ethiopia, which face dual health challenges of communicable diseases such as HIV, tuberculosis (TB), and malaria alongside a rising burden of NCDs [ 28 ].
The age-specific analysis from our study reveals a higher prevalence of hospital admissions for NCDs among younger cohorts (under 64 years) compared to seniors (aged 65 years and older). This finding aligns with international research trends, such as studies conducted in Sweden, indicating a global pattern where younger adults are more frequently hospitalized for NCDs compared to older adults [ 29 ]. The implications underscore the importance of age-specific healthcare strategies for effective NCD management and prevention.
Regarding specific disease entities, our study found that seniors and middle-aged adults exhibit higher hospitalization rates for CVDs, whereas young adults show a higher prevalence of cancer among admitted patients. This observation reflects the cumulative nature of CVD development with age, influenced by factors such as blood pressure, cholesterol levels, and atherosclerosis, whereas cancers prevalent in younger adults, such as leukaemia and lymphoma, exhibit distinct risk profiles [ 30 , 31 ].
Within the arena of CVDs, heart failure emerges as the predominant condition among hospitalized patients, consistent with findings from studies across diverse geographical regions [ 32 , 33 ]. Stroke also stands out as a significant contributor to cardiovascular-related admissions, underscoring its impact as a leading cause of hospitalization in neurology departments [ 34 ]. Additionally, another study highlights stroke as a notable cause of admission to a tertiary care centre [ 35 ]. These findings emphasize the critical need for interventions addressing heart health, particularly in cases where heart failure coincides with chronic rheumatic valvular heart disease, as noted in prior research [ 36 ]. Similarly, our study underscores the importance of early detection and treatment for primary cancer types, such as ALL, AML, CLL, and cervical cancer. These insights are crucial for guiding targeted healthcare interventions aimed at improving cancer outcomes among hospitalized patients.
Our study also reports an in-hospital mortality rate of 15.3% among patients with NCDs, with cancer exhibiting the highest case fatality rate at 22.7%, followed by CVDs at 13%, and DM at 12.5%. These mortality patterns align with global trends reported by the World Health Organization (WHO), highlighting the substantial burden of NCDs worldwide [ 37 ]. Variations between our findings and WHO data may be attributed to the inclusion of younger individuals in our study, potentially underestimating CVD burdens while highlighting haematological tumours. Comparative studies from Sudan and northern Ethiopia reinforce our findings, indicating high case fatality rates associated with malignancy, sepsis, neurological diseases, and CVDs among hospitalized patients [ 25 , 26 ]. These parallel findings underscore the urgent need for enhanced healthcare strategies to improve patient outcomes and mitigate the impact of NCDs.
These collective results underline the urgency of focusing on NCDs management and prevention strategies to mitigate their impact and improve patient well-being. A distinct set of findings emerged from a retrospective study in Nigeria that involved 2,922 participants. In this study, CVDs were responsible for the highest proportion of NCD-related deaths, constituting 33.5% of the cases [ 25 ]. The divergence in results between our study and the Nigerian study could be attributed to several factors. Notably, our study encompassed a wider range of medical wards, including medical, gynaecology, obstetrics, and oncology wards, while the Nigerian study focused solely on medical wards. This broader scope in our study might have contributed to the variations in the reported causes of NCD-related mortality, emphasizing the impact of the diversity of ward inclusions on the outcomes.
In addressing mortality risks, our study underscores the significance of medication adherence, infection control, and co-morbidity management. Elevated mortality risks associated with infections and chronic kidney disease (CKD) highlight the critical need for proactive infection control measures and comprehensive co-morbidity management strategies. Similar findings have been documented in studies focusing on renal diseases and hospital complications [ 24 , 26 ].
The findings have significant implications.
For clinical practice.
CVDs and cancer collectively accounted for 82.3% of all NCD cases, underscoring their substantial impact in Africa. Younger adults (under 64) exhibited higher hospitalization rates for NCDs compared to older adults, revealing a global health trend. Heart failure predominated among CVDs, while stroke emerged prominently in neurology departments.
Cancer ranked as the second most common NCD among hospitalized patients, highlighting the urgent need for enhanced cancer care. The high case fatality rate of cancer (22.7%) emphasizes the importance of improving treatment outcomes.
From a public health perspective.
It is essential to prioritize preventive health strategies and enhance healthcare infrastructure to effectively manage prevalent NCDs. Health education initiatives can empower communities with knowledge about disease prevention and early detection, potentially reducing disease burden.
Implementing evidence-based policies is crucial for improving clinical care, mitigating the impact of NCDs, and enhancing overall patient outcomes. These efforts aim to foster healthier communities by addressing the root causes and management of NCDs comprehensively.
Strengths and limitations
Despite its strengths, our study has several limitations. Firstly, the study was conducted exclusively in Addis Ababa, Ethiopia, across three healthcare facilities, potentially limiting the generalizability of findings to other regions. Secondly, the inclusion of adolescents in adult wards may influence health profiles and outcomes compared to dedicated paediatric wards. Thirdly, while socio-economic factors like income and education were considered, other factors such as healthcare access and insurance status were not included, which could impact NCD outcomes. Lastly, the exclusion of patients with rare or emerging NCDs or multiple co-morbid conditions may limit the comprehensive understanding of NCD patterns among hospitalized patients. Despite the study limitations, its prospective design, inclusion of diverse wards, and use of established data tools (WHO STEPwise) strengthen its validity and contribute valuable insights into NCD among hospitalized patients and their outcomes in the study area.
In conclusion, our study provides critical insights into predictors of mortality among hospitalized patients with NCDs. By examining a diverse cohort across multiple specialty wards, we have identified significant associations between cancer diagnosis, medication adherence, infections, CKD, and hospital complications with increased mortality risks. These findings underscore the multifaceted nature of NCD management and highlight the importance of targeted interventions to improve patient outcomes in hospital settings. Moving forward, efforts to enhance medication adherence, infection control measures, and co-morbidity management can potentially mitigate mortality rates among individuals with NCDs, thereby advancing healthcare delivery and patient outcomes in hospital settings. Overall, our study contributes to advancing the understanding of NCD epidemiology and clinical management, with implications for improving healthcare practices and policies aimed at combating NCDs globally.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
Non-communicable disease
Cardiovascular disease
Diabetes mellitus
Chronic obstructive pulmonary disease
Chronic kidney disease
Communicable, maternal, neonatal, and nutritional
Tikur Anbessa specialised hospital
St. Paulos hospital Millennium medical college
Yekatit 12 hospital
Intensive care unit
Low- and middle-income countries
Standard deviation
Interquartile range
World health organization
Acute myeloid leukaemia
Chronic lymphoblastic leukaemia
Acute lymphoblastic leukemia
Human immunodeficiency virus
Tuberculosis
Bennett JE, Stevens GA, Mathers CD, Bonita R, Rehm J, Kruk ME et al. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. The Lancet (2018) 22;(392):1072–88.
Ramesh S, Kosalram K. The burden of non-communicable diseases: a scoping review focus on the context of India. J Educ Health Promot. 2023;12:41. https://doi.org/10.4103/jehp.jehp_1113_22 .
Article PubMed PubMed Central Google Scholar
Mohammad HF. 2015. Global, regional, and national comparative risk assessment of 79 behaviournvironmental and occupational, and metabolic. risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (2016);388(10053):1659–724.
Ezzati M, Pearson-Stuttard J, Bennett JE, Mathers CD. Acting on non-communicable diseases in low- and middle-income tropical countries. Nature. 2018;559(7715):507–16.
Article CAS PubMed Google Scholar
Idris IO, Oguntade AS, Mensah EA, Kitamura N. Prevalence of non-communicable diseases and its risk factors among Ijegun-Isheri Osun residents in Lagos State, Nigeria: a community based cross-sectional study. BMC Public Health. 2020;20:1258.
Mudie K, Jin MM, Tan null, Kendall L, Addo J, Dos-Santos-Silva I, et al. Non-communicable diseases in sub-saharan Africa: a scoping review of large cohort studies. J Glob Health. 2019;9(2):020409.
Bigna JJ, Noubiap JJ. The rising burden of non-communicable diseases in sub-saharan Africa. Lancet Glob Health. 2019;7(10):e1295–6.
Article PubMed Google Scholar
WHO. 2023. Non communicable diseases [Internet]. [cited 2023 Oct 17]. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases .
Girum T, Mesfin D, Bedewi J, Shewangizaw M. The Burden of Noncommunicable Diseases in Ethiopia, 2000–2016: Analysis of Evidence from Global Burden of Disease Study 2016 and Global Health Estimates 2016. International Journal of Chronic Diseases (2020) 20;2020:e3679528.
Organization WH. Global status report on noncommunicable diseases 2010. 2011 [cited 2023 Nov 16]; https://iris.who.int/handle/10665/44579 .
WHO. 2014. Global status report on noncommunicable diseases 2014 [Internet]. [cited 2023 Nov 16]. https://www.who.int/publications-detail-redirect/9789241564854 .
Alamnia TT, Sargent GM, Kelly M. Patterns of non-communicable Disease, Multimorbidity, and Population Awareness in Bahir Dar, Northwest Ethiopia: a cross-sectional study. Int J Gen Med. 2023;16:3013–31.
Juma K, Juma PA, Shumba C, Otieno P, Asiki G, Juma K et al. Non-Communicable Diseases and Urbanization in African Cities: A Narrative Review. In: Public Health in Developing Countries - Challenges and Opportunities [Internet]. IntechOpen; 2019 [cited 2023 Nov 16]. https://www.intechopen.com/chapters/69370 .
Misganaw N. Walker, Mirkuzie, Giref, Berheto, et.al. Progress in health among regions of Ethiopia, 1990–2019: a subnational country analysis for the global burden of Disease Study 2019. Lancet. 2022;399(10332):1322–35.
Article Google Scholar
Bosu WK. An overview of the nutrition transition in West Africa: implications for non-communicable diseases. Proc Nutr Soc. 2015;74(4):466–77.
Mbogori T, Kimmel K, Zhang M, Kandiah J, Wang Y. Nutrition transition and double burden of malnutrition in Africa: a case study of four selected countries with different social economic development. AIMS Public Health. 2020;7(3):425–39.
Popkin BM. The Nutrition Transition in the developing World. Dev Policy Rev. 2003;21(5–6):581–97.
Yu D, Shi J, Zhang H, Wang Z, Lu Y, Zhang B, et al. Identifying patterns of non-communicable diseases in developed eastern coastal China: a longitudinal study of electronic health records from 12 public hospitals. BMJ Open. 2017;7(10):e016007.
Amundsen MS, Kirkeby TMG, Giri S, Koju R, Krishna SS, Ystgaard B, et al. Non-communicable diseases at a regional hospital in Nepal: findings of a high burden of alcohol-related disease. Alcohol. 2016;57:9–14.
Sani MU, Mohammed AZ, Bapp A, Borodo MM. A three-year review of mortality patterns in the medical wards of Aminu Kano Teaching Hospital, Kano, Nigeria. Niger Postgrad Med J. 2007;14(4):347–51.
Swe EE, Htet KKK, Thekkur P, Aung LL, Aye LL, Myint T. Increasing trends in admissions due to non-communicable diseases over 2012 to 2017: findings from three large cities in Myanmar. Trop Med Health. 2020;48:24.
Odenigbo CU, Oguejiofor OC. Pattern of medical admissions at the Federal Medical Centre, Asaba-a two year review. Niger J Clin Pract. 2009;12(4):395–7.
CAS PubMed Google Scholar
Memirie ST, Habtemariam MK, Asefa M, Deressa BT, Abayneh G, Tsegaye B, et al. Estimates of Cancer incidence in Ethiopia in 2015 using Population-based Registry Data. J Glob Oncol. 2018;4:1–11.
PubMed Google Scholar
Hailu A, Gidey K, Ebrahim MM, Berhane Y, Gebrehawaria T, Hailemariam T, et al. Patterns of medical admissions and predictors of mortality in Ayder Comprehensive Specialized Hospital, Northern Ethiopia: a prospective observational study. Int J Gen Med. 2023;16:243–57.
Ogunmola OJ, Olamoyegun MA. Patterns and outcomes of medical admissions in the accident and emergency department of a tertiary health center in a rural community of Ekiti, Nigeria. J Emerg Trauma Shock. 2014;7(4):261–7.
Omar SM, Osman OS, Gasim GI, Adam I. Pattern and Trends in Adult Hospitalization/Admission and mortality among Medical Ward inpatients at Gadarif Hospital in Eastern Sudan: A Four-Year Retrospective Study. Int J Gen Med. 2022;15:5879–89.
Akubudike AC, Eze NC. Non communicable Disease admissions in Developing Country as experienced from the Medical Ward of a Tertiary Centre in Nigeria. Cent Afr J Public Health. 2018;4(2):34.
Bygbjerg IC. Double burden of noncommunicable and infectious diseases in developing countries. Science. 2012;337(6101):1499–501.
Gondek D, Ploubidis GB, Hossin MZ, Gao M, Bann D, Koupil I. Inequality in hospitalization due to non-communicable diseases in Sweden: age-cohort analysis of the Uppsala Birth Cohort Multigenerational Study. SSM - Popul Health. 2021;13:100741.
Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, Shah K, et al. Cardiovascular risks Associated with gender and aging. J Cardiovasc Dev Dis. 2019;6(2):19.
CAS PubMed PubMed Central Google Scholar
Zahnreich S, Schmidberger H. Childhood Cancer: Occurrence, Treatment and Risk of Second Primary Malignancies. Cancers (2021);13(11):2607.
Brown JR, Gottlieb SS. Acute decompensated heart failure. Cardiol Clin. 2012;30(4):665–71.
Salah HM, Minhas AMK, Khan MS, Pandey A, Michos ED, Mentz RJ, et al. Causes of hospitalization in the USA between 2005 and 2018. Eur Heart J Open. 2021;1(1):oeab001.
Evelyne AA, Mamadou Z. Current data on the Profile of patients hospitalized for stroke in a Neurology Department in West Africa: Abidjan (Ivory Coast). Am J Psychiatry Neurosci. 2015;3:14.
Kurmi RN, Mandal L, Singh R, Chaudhary PK, Dhungana T, Lamichanne S, et al. Stroke among patients admitted to a Tertiary Care Centre: a descriptive cross-sectional study. JNMA J Nepal Med Assoc. 2023;61(260):305–9.
Limbu YR, Maskey A, MB KC, Malla R, Sharma D, Shrestha NK, A STUDY ON CARDIOVASCULAR DISEASE PATTERN OF ADMITTED CASES IN NEWLY EMERGED NATIONAL HEART CENTRE. J Nepal Med Assoc. 2003;41(141):284–8.
WHO. 2022. World Health Systems Facts. [cited 2023 Oct 17]. https://healthsystemsfacts.org/ . https://healthsystemsfacts.org/.
Download references
Acknowledgements
Research reported in this publication was supported by the Fogarty International Centre of the National Institutes of Health under Award Number D43 TW011404. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
No funding was received for this work.
Author information
Authors and affiliations.
Department of Pharmacology and Clinical Pharmacy, School of Pharmacy, Colleges of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Alemu Belayneh, Legese Chelkeba & Firehiwot Amare MPharm
Hubert Department of Global Health, Rollins School of Public Health, Emory University, Georgia, Atlanta, USA
Legese Chelkeba, Shivani A. Patel & Mohammed K. Ali
Division of Cardiology, Department of Internal Medicine, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Senbeta Guteta Abdissa
Department of Community Health, School of Public Health, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Mirgissa Kaba
Department of Internal Medicine, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
Henok Fisseha
You can also search for this author in PubMed Google Scholar
Contributions
A.B: Conceived the study, designed the study, collected the data, data analysis, and wrote the initial draft of the manuscript. L.C.K: Conceived the study, designed the study, supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. F.A: data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. H.F: supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. S.G: supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. M.K: supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. S.A.P: supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. M.K.A: supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript.
Corresponding author
Correspondence to Legese Chelkeba .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the School of Pharmacy, College of Health Sciences at Addis Ababa University Ethical Review Committee (ERB/SoP/485/14/2022). Permissions were also sought from each department involved. Written informed consent was obtained from all study participants, who were fully informed about the study’s objectives and given the option to decline or participate. Patient identification numbers were used instead of names to ensure confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Belayneh, A., Chelkeba, L., Amare, F. et al. Investigation of non-communicable diseases prevalence, patterns, and patient outcomes in hospitalized populations: a prospective observational study in three tertiary hospitals. J Health Popul Nutr 43 , 128 (2024). https://doi.org/10.1186/s41043-024-00599-z
Download citation
Received : 05 December 2023
Accepted : 18 July 2024
Published : 20 August 2024
DOI : https://doi.org/10.1186/s41043-024-00599-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Non-communicable diseases
- Socio-economic disparities
- Hospital admissions
- Clinical outcomes
Journal of Health, Population and Nutrition
ISSN: 2072-1315
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Loading metrics
Open Access
Peer-reviewed
Research Article
Implementation research on noncommunicable disease prevention and control interventions in low- and middle-income countries: A systematic review
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Global Health and Population, Harvard TH Chan School of Public Health, Boston, Massachusetts, United States of America
Roles Data curation, Writing – review & editing
Affiliation School of Population and Public Health, University of British Columbia, Vancouver, British Columbia, Canada
Affiliation School of Public Health, University of Illinois Chicago, Chicago, Illinois, United States of America
Roles Conceptualization, Investigation, Methodology, Writing – review & editing
Affiliation Alliance for Health Policy and Systems Research, WHO, Geneva, Switzerland
Roles Conceptualization, Investigation, Methodology
Affiliation Department of NCD, WHO, Geneva, Switzerland
Affiliations The George Institute for Global Health, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia, School of Public Health, Harbin Medical University, Harbin, China
Affiliation The George Institute for Global Health, Faculty of Medicine and Health, University of New South Wales, Sydney, Australia
Roles Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing
- Celestin Hategeka,
- Prince Adu,
- Allissa Desloge,
- Robert Marten,
- Ruitai Shao,
- Maoyi Tian,
- Ting Wei,
- Margaret E. Kruk

- Published: July 25, 2022
- https://doi.org/10.1371/journal.pmed.1004055
- Peer Review
- Reader Comments
While the evidence for the clinical effectiveness of most noncommunicable disease (NCD) prevention and treatment interventions is well established, care delivery models and means of scaling these up in a variety of resource-constrained health systems are not. The objective of this review was to synthesize evidence on the current state of implementation research on priority NCD prevention and control interventions provided by health systems in low- and middle-income countries (LMICs).
Methods and findings
On January 20, 2021, we searched MEDLINE and EMBASE databases from 1990 through 2020 to identify implementation research studies that focused on the World Health Organization (WHO) priority NCD prevention and control interventions targeting cardiovascular disease, cancer, diabetes, and chronic respiratory disease and provided within health systems in LMICs. Any empirical and peer-reviewed studies that focused on these interventions and reported implementation outcomes were eligible for inclusion. Given the focus on this review and the heterogeneity in aims and methodologies of included studies, risk of bias assessment to understand how effect size may have been compromised by bias is not applicable. We instead commented on the distribution of research designs and discussed about stronger/weaker designs. We synthesized extracted data using descriptive statistics and following the review protocol registered in PROSPERO (CRD42021252969). Of 9,683 potential studies and 7,419 unique records screened for inclusion, 222 eligible studies evaluated 265 priority NCD prevention and control interventions implemented in 62 countries (6% in low-income countries and 90% in middle-income countries). The number of studies published has been increasing over time. Nearly 40% of all the studies were on cervical cancer. With regards to intervention type, screening accounted for 49%, treatment for 39%, while prevention for 12% (with 80% of the latter focusing on prevention of the NCD behavior risk factors). Feasibility (38%) was the most studied implementation outcome followed by adoption (23%); few studies addressed sustainability. The implementation strategies were not specified well enough. Most studies used quantitative methods (86%). The weakest study design, preexperimental, and the strongest study design, experimental, were respectively employed in 25% and 24% of included studies. Approximately 72% of studies reported funding, with international funding being the predominant source. The majority of studies were proof of concept or pilot (88%) and targeted the micro level of health system (79%). Less than 5% of studies report using implementation research framework.
Conclusions
Despite growth in implementation research on NCDs in LMICs, we found major gaps in the science. Future studies should prioritize implementation at scale, target higher levels health systems (meso and macro levels), and test sustainability of NCD programs. They should employ designs with stronger internal validity, be more conceptually driven, and use mixed methods to understand mechanisms. To maximize impact of the research under limited resources, adding implementation science outcomes to effectiveness research and regional collaborations are promising.
Author summary
Why was the study done.
- While the evidence for the clinical effectiveness of most noncommunicable disease (NCD) prevention and treatment interventions is well established, care delivery models and means of scaling these up to entire populations in need in heterogeneous and resource-constrained health systems are not.
- Implementation research on NCD program delivery can illuminate what does and does not work in preventing NCDs or achieving NCD control. This can promote faster, more efficient, and more effective scale-up of life-saving and health-preserving health system strategies.
- Evidence needed on the current state of implementation research on World Health Organization (WHO) priority NCD prevention and control interventions to help inform research priority.
What did the researchers do and find?
- We performed a systematic review search in MEDLINE and EMBASE databases from 1990 through 2020 to identify implementation research studies that focused on the WHO priority NCD prevention and control interventions targeting cardiovascular disease, cancer, diabetes, and chronic respiratory disease and provided within health systems in low- and middle-income countries (LMICs).
- We identified 222 eligible studies that evaluated 265 priority NCD prevention and control interventions implemented in 62 countries (6% in low-income countries and 90% in middle-income countries). The number of studies published has been increasing over time. The majority of interventions were focused on either screening (49%) or treatment (39%), while prevention accounted for only 12%.
- Reviewed studies emphasized a few health areas, such as cervical cancer, with many other high-burden conditions little researched. The majority of studies were proof of concept or pilot, quantitative using weaker study designs and targeted the micro level of health system.
What do these findings mean?
- While implementation research on priority NCDs has grown substantially, from under 10 studies per year in early 2000s to 51 studies in 2020, this is still vastly incommensurate with the health burden of NCDs.
- Future studies should prioritize implementation at scale, target higher levels health systems (meso and macro levels), and test sustainability of NCD programs. They should employ designs with stronger internal validity, be more conceptually driven, and use mixed methods to understand mechanisms.
- To maximize impact of the research under limited resources, adding implementation science outcomes to effectiveness research and regional collaborations are promising.
Citation: Hategeka C, Adu P, Desloge A, Marten R, Shao R, Tian M, et al. (2022) Implementation research on noncommunicable disease prevention and control interventions in low- and middle-income countries: A systematic review. PLoS Med 19(7): e1004055. https://doi.org/10.1371/journal.pmed.1004055
Academic Editor: Elvin Hsing Geng, Washington University in St Louis School of Medicine, UNITED STATES
Received: December 8, 2021; Accepted: June 21, 2022; Published: July 25, 2022
Copyright: © 2022 Hategeka et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its supporting information files.
Funding: The Alliance for Policy and Health Systems Research and The World Health Organization funded the study. CH received support through a Banting Postdoctoral Fellowship from the Canadian Institutes of Health Research. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: I have read the journal’s policy and the authors of this manuscript have the following competing interests: CH, PA and MEK report personal fees from the funders, during the conduct of the study. MEK is an Academic Editor on PLOS Medicine’s editorial board. RM and RS are employed by the study funders.
Abbreviation: COVID-19, Coronavirus Disease 2019; LIC, low-income country; LMIC, low- and middle-income country; NCD, noncommunicable disease; SDG, Sustainable Development Goal; UMIC, upper middle-income country
Introduction
Noncommunicable diseases (NCDs) have become the leading contributors to morbidity and mortality worldwide. They are now responsible for 74% of all global deaths, 77% of which occur in low- and middle-income countries (LMICs) [ 1 , 2 ]. Approximately 85% of NCD deaths among people aged 30 and 69 years occur in LMICs [ 1 ]. Cardiovascular diseases are the leading causes of NCD mortality, followed by cancers, respiratory diseases, and diabetes [ 1 ]. Together, these 4 NCDs are responsible of over 80% of all premature NCD deaths [ 1 ]. Risk factors such as tobacco and alcohol use, physical inactivity, and unhealthy diets result in significantly greater risk of dying from NCDs. Primary, secondary, and tertiary prevention strategies are vital in addressing NCD burden [ 1 ]. Sustainable Development Goal (SDG) target 3.4 commits countries to reduce premature mortality from NCDs by a third by 2030 relative to 2015 levels. Recent analysis shows that no LMIC is on track to meet this target for both men and women if they maintain their 2010 to 2016 average rates of decline [ 3 ].
NCD prevention and control should not be regarded as a vertical issue separated from other health conditions. The ongoing Coronavirus Disease 2019 (COVID-19) pandemic has put a spotlight on NCDs, as these increased the risk of death for people with COVID infection. Similarly, NCDs increase mortality risk among people with other infectious diseases such as tuberculosis and HIV. It further highlighted the economic and social inequities in who is afflicted with NCDs, in both high-income countries and LMICs. While primary prevention relies on public health, taxation, and other public policy measures, mitigating the health consequences of NCDs also requires strong health systems. Health systems that recognize this challenge and address modifiable risk factors and prioritize the management of NCDs will be better positioned to promote and maintain health. Data from the 2019 World Health Organization (WHO) NCD Country Capacity surveys reveal that only half of 160 countries have national guidelines for NCDs, half have the 6 essential technologies for early detection, diagnosis, and monitoring of NCDs available in primary care facilities of the public health sector, and 20% of countries have 6 (or fewer) of the 11 essential medicines available [ 4 ]. Greater prioritization of NCDs within health systems and high-quality care are essential to achieving SDG 3.4 [ 3 ]. Beyond this lies an important agenda for tackling the cumulatively large group of rarer NCDs that afflict the world’s poorest people [ 5 ].
To support countries in crafting effective NCD strategies, the WHO Assembly endorsed the Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020 (GAP-NCD) in May 2013 together with a set of evidence-based interventions (best-buys) and policy options in its appendix 3 that was updated in 2016 and provides 84 interventions or policy options [ 6 , 7 ]. Furthermore, WHO has developed a compendium including all available health interventions. The list and compendium aim to assist Member States, as appropriate in specific national contexts, in implementing measures to achieve the 9 global voluntary targets for NCDs and Target 3.4 of the SDGs. Despite recent calls for a new commitment to implementation research for NCDs, a mid-point evaluation of the WHO NCD Global Action Plan 2013–2030 (NCD-GAP) found that “research has been the weakest NCD-GAP objective in terms of implementation and that progress in implementing research linked to the NCD-GAP has been slow and incremental” [ 8 , 9 ].
While the evidence for the clinical effectiveness of most NCD prevention and treatment interventions is well established, care delivery models and means of scaling these up to entire populations in need in heterogeneous and resource-constrained health systems are not. Implementation research on NCD program delivery, including cost effectiveness in various regions, can illuminate what does and does not work in achieving NCD control [ 8 , 10 – 12 ]. This can promote faster, more efficient, and more effective scale-up of life-saving and health-preserving health system strategies [ 13 , 14 ]. In this systematic review, we aim to synthesize evidence on the current state of implementation research on WHO priority NCD prevention and control interventions provided within health systems in LMICs [ 6 , 7 , 15 – 17 ].
This systematic review was conducted according to a study protocol registered in PROSPERO (#CRD42021252969) [ 18 ].
Search strategy
Following the Systematic Reviews and Meta-Analyses (PRISMA) checklist [ 19 ], we searched for implementation research studies that focused on relevant NCD prevention and control interventions (Table A in S1 Appendix ) provided within health systems in LMICs and were published in peer-reviewed journals indexed in MEDLINE and EMBASE databases from 1990 to 2020. The databases were last searched on January 20, 2021. Our search terms included medical subject heading (MeSH) terms and/or key words for 4 key themes (implementation research; NCDs; NCD interventions; LMICs) that were adjusted for each database:
- Implementation research (e.g., implementation research, implementation science, diffusion of innovations, implementation strategies, dissemination science, implementation outcomes).
- NCDs (e.g., cardiovascular disease, cancer, diabetes, chronic respiratory disease).
- Interventions (e.g., smoking cessation, management of hypertension, treatment of acute myocardial infarction, cervical and colorectal cancer screening).
- LMICs as defined by the World Bank in 2019 (Table C in S1 Appendix ).
Language restrictions were not applied. Full details of the search strategy are provided in Table B in S1 Appendix .
Inclusion and exclusion criteria
Table 1 summarizes our review’s specific eligibility criteria. This review includes peer-reviewed, empirical quantitative, qualitative, and mixed method study designs conducted in LMICs that described the implementation of relevant NCD preventive and/or control interventions provided within health systems. Using the updated Appendix 3 of the WHO Global NCD Action Plan 2013–2020, we identified the WHO priority NCD prevention and control interventions [ 6 ]. Of these interventions, we selected those that are specifically provided by health systems. This was achieved through discussions and consensus. Table 2 summarizes the intervention categories across eligible NCD risk factors (i.e., tobacco and alcohol use, physical inactivity, and unhealthy diets) and NCDs (i.e., cardiovascular disease, diabetes, cancer, and chronic respiratory disease), and full details are provided in Table A in S1 Appendix . While our search in databases was not restricted to any language, during study screening/review processes, we only retained eligible studies that were in 6 official languages of the United Nations (i.e., Arabic, Chinese, English, French, Russian, and Spanish). We drew on Proctor and colleagues and Glasgow and colleagues to define implementation outcomes eligible for inclusion [ 20 , 21 ]. Nonempirical/primary research studies are not eligible for inclusion ( Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmed.1004055.t001
https://doi.org/10.1371/journal.pmed.1004055.t002
Data extraction and analysis
The titles and abstracts of unique results from the databases were reviewed independently by 2 researchers for potential inclusion using COVIDENCE review software [ 22 ]. The full texts of studies retained at the title and abstract screening stage were retrieved and independently assessed for inclusion. Any discrepancies were resolved through discussion and consensus. Data extraction on each included study was conducted by a single researcher using a data extraction tool, developed and piloted a priori (Table D in S1 Appendix ). Data elements included study characteristics (e.g., publication year, country of implementation, study funding), NCD conditions (risk factors and disease), intervention details (e.g., type of intervention, level of health system), methods (e.g., research approach, study design), implementation outcomes (e.g., fidelity, feasibility), and equity lens (e.g., disaggregated by key SES stratifiers, targeted vulnerable population). We also extracted data on implementation strategies including actor (i.e., who delivered the intervention), action target, and recipients; details of other implementation strategies were not sufficiently described to permit extraction [ 23 ]. The recipients of the action/strategy were further aggregated by demographic subgroup (e.g., people eligible for cancer screening including cervical and colorectal), disease risk subgroup (e.g., patients with myocardial infarction, patients with diabetes or hypertension, people who smoke), general population, healthcare workers (e.g., physicians, nurses, pharmacists, and midwives), and community health workers. We synthesize extracted data using descriptive statistics and following the review protocol registered in PROSPERO. Specifically, we provide an overview of NCD priority intervention implementation study characteristics across NCD conditions to shed light on the current state of implementation research of priority NCD prevention and control interventions in LMICs. Given this review does not focus on effect size of NCD interventions, we did not perform a meta-analysis.
Risk of bias assessment
This review focuses on implementation of multiple interventions across various NCDs, rather than effectiveness of any single set of interventions. Further, studies with heterogenous aims and methodologies (including qualitative methodology) were included. Therefore, risk of bias assessment to understand how effect size may have been compromised by bias is not applicable in this review. We instead commented on the distribution of research designs and discussed about stronger/weaker designs.
Our search strategy implemented in MEDLINE and EMBASE identified 9,683 publications, of which 7,419 unique records were screened for inclusion. Abstract and full-text screening identified 222 studies that met our inclusion criteria (Tables 1 and 2 ) [ 24 – 245 ]. A summary of this process is presented in the PRISMA flow diagram in Fig 1 .
Intervention refers to studies excluded because they studied the implementation of interventions that did not meet the eligible criteria. Study design refers to studies excluded because they used study designs that did not meet eligibility criteria (e.g., nonempirical studies including reviews and commentaries). Outcomes refer to studies excluded based on not having focused on relevant implementation outcomes. Settings refer to studies excluded because they were not conducted in LMICs. Full text means that studies were excluded because full text was not available. Time refers to studies that were excluded because they were published before/conducted before 1990.
https://doi.org/10.1371/journal.pmed.1004055.g001
The 222 studies included in this review evaluated 265 priority NCD prevention and control interventions implemented in 62 countries, of which 6% were in low-income countries (LICs), 45% in LMICs, and 46% in upper middle-income countries (UMICs) ( Table 3 and Figs 2 , 3 , and 4A and Table E in S1 Appendix ). The NCD conditions targeted varied by income groups of countries (Fig A in S1 Appendix ). Eight of the included studies were multicountry studies. The number of studies published has been increasing over time ( Fig 5A ). Overall, the majority of interventions were focused on either screening (49%) or treatment (39%), while prevention accounted for only 12%, with nearly 80% of these tackling prevention of the shared NCD behavioral risk factors—tobacco use, unhealthy diet, physical inactivity, and harmful use of alcohol. The NCD interventions varied by conditions and type (prevention, screening, and treatment) (Figs 2, B, and C in S1 Appendix ). Notably, over one-third of the interventions studied (37%) were for cervical cancer ( Fig 2 ), which accounts for 0.35% of DALYs lost and 0.5% of deaths globally, with similar figures for LMICs ( https://vizhub.healthdata.org/gbd-compare/ ). Diabetes was the focus of nearly one-quarter of the research with hypertension the topic of another 9% ( Fig 2 ). Each of the other recommended interventions represented 5% or less of the implementation research output. Chronic respiratory disease was understudied relative to its prevalence: less than 1% of the studies examined chronic respiratory disease treatment and only 3% smoking cessation programs. The intervention focus appears to vary by income groups of countries (Fig D in S1 Appendix ). Feasibility was the most studied implementation outcome followed by adoption ( Fig 6 ). Most of the actors were researchers, which accounted for 58%; whereas government/ministry of health, providers, and NGOs accounted for 18%, 10%, and 6%, respectively. The majority of intervention targeted improvement in health outcomes (45%) followed by change in behavior (34%).
https://doi.org/10.1371/journal.pmed.1004055.g002
We used country population size in 2020 ( https://data.worldbank.org/indicator/SP.POP.TOTL ) to standardized estimates expressed as number of studies per 1 million population. We used “rworldmap” package ( https://cran.r-project.org/web/packages/rworldmap/rworldmap.pdf ) available in R software to present these standardized estimates across countries where interventions were implemented. Country borders in this package are derived from Natural Earth data. Table E in S1 Appendix shows number of included studies per country.
https://doi.org/10.1371/journal.pmed.1004055.g003
https://doi.org/10.1371/journal.pmed.1004055.g004
Growth of research over time (A) and distributions of NCD interventions by type (B). Fig 5A shows number of studies published each year ( N = 222 studies); Fig 5B shows distributions by type of interventions ( N = 265 NCD interventions evaluated in studied included in the review).
https://doi.org/10.1371/journal.pmed.1004055.g005
https://doi.org/10.1371/journal.pmed.1004055.g006
https://doi.org/10.1371/journal.pmed.1004055.t003
Most studies used quantitative methods, which accounted for 86%, whereas mixed methods and qualitative methods accounted for 9% and 5%, respectively ( Table 2 ). The majority of studies used observational designs, with cross-sectional designs used in 45 studies. Among evaluations, preexperimental studies (such as pre-post without a comparison group or post-only) was the most frequently employed ( n = 56 or 25% of all studies); experimental designs were used in a quarter of studies ( n = 53 or 24% of all studies); quasi-experimental evaluation designs (such as pre-post comparison group or time series) were used in 15 papers (7% of all studies) ( Fig 7 ). Study designs also appear to vary by NCD conditions targeted (Fig E in S1 Appendix ). The sample size among included studies varied, ranging from 11 to 350,581, with median of 658. Most studies were standalone implementation studies (85%), with some variations by NCD conditions (Fig F in S1 Appendix ). Hybrid implementation and effectiveness studies accounted only for 15%. Less than 5% of studies reported they were guided by widely known implementation science framework. Majority of studies were proof of concept or pilot versus scale-up studies (88% versus 12%), with variations by NCD conditions (Fig G in S1 Appendix ). The level of health system targeted most often was micro level, accounting for 79% of studies, with variations by NCD conditions. The meso and macro levels of health systems were targeted by 14% and 7% of studies, respectively (Fig H in S1 Appendix ). Approximately 42% of studies employed an equity lens—i.e., studies disaggregated by SES stratifiers (e.g., age, sex, education, income, and rural versus urban) and/or targeted vulnerable population.
https://doi.org/10.1371/journal.pmed.1004055.g007
A majority of studies (72%) reported funding, with international funding being the predominant source ( Fig 4B ). There seems to be some variations by NCD conditions (Figs I–K in S1 Appendix ). For example, while 78% of studies focused on cervical cancer reported funding, of which 77% were from international sources, those focused on colorectal cancer and treatment of acute myocardial infarction received most of their funding from the countries where implementation research was conducted (Fig K in S1 Appendix ). Majority of reported funding was provided by government/universities (43.6%), 35% reported multiple funders, 16% were foundations/NGOs, and 6% were private funders (e.g., pharmaceutical companies, professional associations) (Fig L in S1 Appendix ). Approximately 62% of corresponding authors were from the country of implementation ( Fig 4C ); however, this varied by funding sources, with studies funded by international funders having the highest number of international corresponding authors.
We conducted a systematic review of implementation research studies on NCD prevention and control strategies in LMICs published between 1990 and 2020. We focused our analysis on WHO-recommended NCD interventions carried out by the health system rather than through policy, legislation, or public health approaches [ 6 , 7 ]. These studies therefore represent the state of the implementation science in prevention and control of NCDs by health systems in the countries bearing the bulk of disease burden from noncommunicable conditions.
Of the 222 implementation science studies included in this review, 94% were conducted in middle-income countries (evenly split between lower- and upper-middle) and 6% in LICs. UMICs were slightly overrepresented compared to their share of the LMIC population (approximately 40%). Only 8 of the studies were multicountry studies, suggesting that cross-national generalizability is not the primary motivation for this type of research. India and China, with 43% of the population of LMICs, comprised one-third of the studies. South Africa, Brazil, Iran, Kenya, and Nigeria, were well represented, each contributing more than 3% of the research.
The studies described 265 different NCD interventions, ranging from screening to prevention to treatment and palliation. Conditions studied varied substantially by region. All 13 of the interventions studied in LICs were for cervical cancer screening. In low-middle income countries, cervical cancer accounted for 37%, diabetes for 29%, and hypertension for 8% of interventions. There was a larger variety of conditions studied in UMICs: while cervical cancer and diabetes comprised half the studies, hypertension, myocardial infarction, colorectal cancer, other cardiovascular diseases, and unhealthy diet each comprised more than 5% of studies. The 2 countries with the largest research output and populations, China and India, differed substantially in focus. In India over 70% of studies were on 2 conditions: diabetes (51%) and cervical cancer (19%), whereas the research was more evenly distributed across the NCDs in China.
Half of all studied interventions in this review evaluated screening for disease, nearly 40% treatment and 12% prevention. Over 70% of all screening studies were for cervical cancer, with less research on other conditions for which screening can be cost effective, such as diabetes, colorectal cancer, and breast cancer. Primary and secondary prevention can reduce incidence of disease and forestall disease progression and disability. We found that only 31 (12%) of the studied interventions addressed prevention with nearly 80% of these tackling prevention of the NCD behavior risk factors (e.g., tobacco use, inactivity, unhealthy diet). Less than 10% of the interventions evaluated in this review focused on management of hypertension (the leading metabolic risk factor worldwide, accounting for approximately 19% of global deaths) [ 246 ]. This suggests a substantial implementation research gap in secondary prevention, a critical function of primary care and other levels of health systems. Primary care services such as hypertension management and glucose control play a major role in reducing mortality, thus insufficient research on their optimal implementation is a major missed opportunity. Recent work shows that treatment and control rates for hypertension were below 25% and 10%, respectively, in many countries in South Asia and sub-Saharan Africa. These countries also showed the slowest rates of improvement from 1990 [ 247 ].
The preponderance of interventions studied was in pilot phase, with fewer than 15% studying large-scale implementation. Along the same lines, feasibility and adoption were the most studied implementation outcomes, suggesting the research is focused on introduction of new approaches. While proof of concept studies is vital with new implementation strategies, arguably WHO-proposed interventions are well established and evidence on (clinical) effectiveness abound. To provide useful guidance to health system planners and realize population health gains, there needs to be a greater investment in large-scale NCD implementation research to promote sustainability of evidence-based interventions. To best scale scarce research resources and accelerate impact, countries could join regional consortia to study interventions and undertake factorial designs that compare locally adapted implementation approaches.
Over three-quarters of the studies were situated at the micro level of the health system—targeting patient, provider, or clinic levels. Nearly 1 in 5 tested a new technology, despite evidence that technology adoption without substantial integration into policies, data, and workflows is typically ineffective in transforming care [ 248 , 249 ]. Education was another common target featuring in 3 of 10 studies; researchers accounted for the majority of the actors. While micro-level approaches are the most “researchable,” as they are easiest to implement and analyze; positive results are difficult to scale and sustain in the absence of systemic health system change. The Lancet Commission on High Quality Health Systems notes that high-quality care results from structures that align system aims and policies with strong governance, management, and appropriately trained workforce [ 250 ]. In this context, micro-level innovation cannot raise quality system wide and is only effective if undertaken as part of a learning health system that can determine whether it offers sufficient benefit over current practice in complexity, cost, and health benefit, and if so, how to best integrate into the health system [ 251 ].
Nearly 9 in 10 studies were stand-alone implementation research. This also points to an opportunity to add implementation research to ongoing effectiveness trials. Integrated or hybrid effectiveness-implementation studies are increasingly being used in high-income countries to shed light on both the outcome and extent and quality of service/program delivery [ 252 ]. Notably, fewer than 5% of studies cited use of an implementation science framework consistent with prior research showing that the use of implementation science framework is substantially lower in LMICs compared with high-income countries [ 253 ]. The use of a tested conceptual framework can improve the rigor of the research and promote comparability of results. Of the studies that reported a funding source, 60% was from international sources, 33% from the country of the research, and the remaining from both local and international sources. This reflects the low spending for health research and especially for health systems and implementation research in LMICs. The lack of domestic support is unlikely to be offset by global funding going forward; a recent analysis showed that NCDs were under prioritized in bilateral agency portfolios relative to their health impacts [ 254 ]. Over 40% of development assistance for health in LICs for NCDs came from NGOs and philanthropies, which are less inclined to support research than operations [ 254 ]. Indeed, we found that only 16% of studies with funding information reviewed were supported by philanthropies or NGOs, while the other remaining studies reported funding sources from government, private, and/or multiple sources.
Scarcity of funding for research is a key constraint to needed implementation research for NCDs. While there are proposals for coordinating and increasing global support, it is unrealistic to expect this to meet the scale of needed research without a substantial increase in countries’ investment in research [ 255 ]. Such an investment is likely to pay off in better health and higher quality, more efficient service delivery [ 256 ]. To make best use of research funds, implementation science should strive to be as generalizable as possible—at minimum at a regional level where health systems share similarities. International and regional institutions can play an important role in supporting research consortia and partnerships to promote efficiency of and accelerate the pace of research and, ultimately its uptake into routine care at scale.
Over 50 of the 222 included studies used an experimental research design. While this is the strongest design to yield causal inference, it is not always feasible to implement. Quasi-experimental designs, such as pretest, posttest comparison group designs, and interrupted time series, which can offer robust information were used in only 15 studies. Preexperimental designs that do not include a comparison group or tracking over time, comprised nearly a quarter of the studies. These designs have very low internal validity and should generally be avoided. The remainder of the studies used cross-sectional descriptions, cohort studies, and qualitative research or multiple study types. Given the disproportionate health harms of NCDs among the poor and other vulnerable groups within countries, disaggregated or stratified analysis is crucial. Forty percent of the assessed studies included stratification by age, sex, education, or urbanicity. Going forward, greater use of quasi-experimental designs, hybrid implementation studies and mixed methods approaches, would benefit the field. An expanded focus on equity of implementation outcomes is also needed.
Strengths and limitations
Our study had several strengths, notably the extensive scope for the search that covered LMICs, a wide range of outcomes and study types, and a large contingent of conditions and health services. We had no language restrictions permitting a comprehensive assessment of the published literature. The review also had several limitations. We focused on WHO-recommended interventions, which at present do not include guidance for some prevalent conditions such as mental health problems and kidney disease [ 6 , 12 ]. Mental health is a major contributor to the global burden of disease and future work should assess the implementation science for the growing range of mental health interventions that appear to be effective in lower-income settings [ 257 , 258 ]. The studies we assessed used differing definitions of implementation outcomes (e.g., acceptability was measured in some studies by self-report and in others by behavior change). This limits direct comparison of study outcomes. Greater use of implementation science frameworks can promote coherence in the research approaches and terminology used to the benefit of end users. Similarly, given the implementation strategies were not specified well enough in the included studies, we elected to focus on actors, action target, and recipients in our description of implementation strategies. Clearly, reporting empirical implementation studies using existing framework to describe implementation strategies would help bolster uptake of implementation research in NCDs.
We also did not search the gray literature and as such, some relevant studies may have been missed. However, studies in gray literature that were not peer reviewed would have not have been eligible for inclusion in this review. Despite using rigorous search strategies without language restrictions, studies published in journals not indexed in MEDLINE and EMBASE were not captured [ 259 – 263 ]. Given the focus on this review and the heterogeneity in aims and methodologies of included studies, risk of bias assessment to understand how effect size may have been compromised by bias is not applicable. As such, we only commented on the distribution of research designs and discussed about stronger/weaker designs. Lastly, we reported year of publication and not time of when study/implementation was conducted.
High-quality implementation science can play a key role in informing effective delivery of health system interventions to mitigate the burden of NCDs and avoiding expensive mistakes. While implementation research on priority NCDs has grown substantially, from under 10 studies per year in early 2000s to 51 studies in 2020, this is still vastly incommensurate with the health importance of the topic. Further, the concentration of studies in a few geographies and a few health areas, such as cervical cancer, highlights the dearth of research for other key conditions. We found a major gap in research on secondary prevention, i.e., management of risk factors or early disease to prevent disease progression and premature death. Research on ways in which health systems can be strengthened, including primary care levels, to provide optimal care for NCDs is critically needed. Future studies should use implementation science frameworks, and, when testing interventions, strong research designs with strong internal validity, including well-designed quasi-experimental studies. Opportunities exist for adding implementation science studies to planned effectiveness research.
Supporting information
S1 prisma checklist. prisma 2020 checklist..
https://doi.org/10.1371/journal.pmed.1004055.s001
S1 Appendix. Appendix tables and figures.
Table A in S1 Appendix. Interventions provided within health systems. Table B in S1 Appendix. Sample of the search strategy used in the MEDLINE database. Table C in S1 Appendix. List of low- and middle-income countries. Table D in S1 Appendix. Data extraction tool. Table E in S1 Appendix. Distribution of studies by countries where they were implemented. Fig A in S1 Appendix. Variation of conditions evaluated by income group. Fig B in S1 Appendix. Priority NCD interventions ( n = 265) identified in 222 studies included in the review. Fig C in S1 Appendix. Distribution of included studies by NCD. Fig D in S1 Appendix. Distribution of intervention type by income group. Fig E in S1 Appendix. Distributions by research designs. Fig F in S1 Appendix. Distributions by standalone implementation studies vs. embedded or hybrid effectiveness-implementation studies. Fig G in S1 Appendix. Distributions by pilot vs. scale-up project. Fig H in S1 Appendix. Variation by level of health system. Fig I in S1 Appendix. Studies that reported funding (vs. those that did not) by NCD conditions. Fig J in S1 Appendix. Distributions by funding type. Fig K in S1 Appendix. Distribution of funding sources by NCDs and their risk factors. Fig L in S1 Appendix. Types of reported funding sources ( N = 222 included studies).
https://doi.org/10.1371/journal.pmed.1004055.s002
- View Article
- Google Scholar
- PubMed/NCBI
- 18. Systematic Review of NCD Implementation Research in Low- and Middle-Income Countries. [Internet]. PROSPERO 2021. [cited 2021 Oct 2]. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021252969 .
- 22. Veritas Health Innovation. Covidence systematic review software. 2020 [cited 2021 Nov 5]. Available from: https://get.covidence.org/systematic-review?campaignid=11343712044&adgroupid=114130876511&gclid=Cj0KCQjwtrSLBhCLARIsACh6RmjH6RwcJalTVCaL76kpSCeqErC2sP8uX4Vj8wZYdEQWQxdXWVwD0eMaAsz1EALw_wcB .
- 264. Beard P, Greenall J, Hoffman C, Nettleton S, Popescu I, Ste-Marie M. Incident Analysis Collaborating Parties. Canadian Incident Analysis Framework. Edmonton, AB: Canadian Patient Safety Institute; 2012.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 18 July 2023
Principles for the prevention and control of non-communicable disease
- Sailesh Mohan 1 nAff5 ,
- Kamlesh Khunti 2 &
- Dorairaj Prabhakaran 3 , 4
Nature Medicine volume 29 , pages 1598–1600 ( 2023 ) Cite this article
1275 Accesses
2 Citations
14 Altmetric
Metrics details
- Epidemiology
- Medical research
Non-communicable diseases in low- and middle-income countries can be tackled with integrated health systems interventions that consider multimorbidity, supported by patient involvement and new technologies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
WHO. Noncommunicable Diseases https://go.nature.com/3N74eoe (2022).
WHO. Noncommunicable Diseases Progress Monitor 2022 https://go.nature.com/3qt6Aov (2022).
NCD Countdown 2030 Collaborators. Lancet 396 , 918–934 (2020).
WHO. Noncommunicable Diseases Progress Monitor 2020 https://go.nature.com/3OSpdwp (2020).
Mendenhall, E. et al. Lancet 389 , 951–963 (2017).
Article PubMed PubMed Central Google Scholar
Allen, L. N. et al. Lancet Glob. Health 11 , e525–e533 (2023).
Article CAS PubMed Google Scholar
The Academy of Medical Sciences. Multimorbidity: a Priority for Global Health Research https://go.nature.com/3N8B8Vs (2018).
The PLOS Medicine Editors. PLoS Med. 20 , e1004229 (2023).
Hurst, J. R. et al. Lancet Glob. Health 6 , e1270–e1271 (2018).
Article PubMed Google Scholar
Sum, G. et al. J. Glob. Health 9 , 020413 (2019).
Mair, F. S. et al. J. Comorb. 10 , 2235042X2096167 (2020).
Article Google Scholar
Russell, C. D. et al. Nat. Med. 29 , 334–343 (2023).
Download references
Acknowledgements
S.M., K.K. and D.P. are supported by the National Institute for Health and Care Research (NIHR) Global Health Research Centre for Multiple Long-Term Conditions using UK aid from the UK Government to support global health research (NIHR203257). The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK government. K.K. is also supported by NIHR Applied Research Collaboration East Midlands and the NIHR Leicester Biomedical Research Centre.
Author information
Sailesh Mohan
Present address: Centre for Chronic Disease Control (CCDC), Delhi, India
Authors and Affiliations
Centre for Chronic Conditions and Injuries (CCCI), Public Health Foundation of India, Delhi, India
Diabetes Research Centre, University of Leicester, Leicester, UK
Kamlesh Khunti
Centre for Digital Health, Public Health Foundation of India, Delhi, India
Dorairaj Prabhakaran
Centre for Chronic Disease Control (CCDC), Delhi, India
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Dorairaj Prabhakaran .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Mohan, S., Khunti, K. & Prabhakaran, D. Principles for the prevention and control of non-communicable disease. Nat Med 29 , 1598–1600 (2023). https://doi.org/10.1038/s41591-023-02368-7
Download citation
Published : 18 July 2023
Issue Date : July 2023
DOI : https://doi.org/10.1038/s41591-023-02368-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Building healthy populations.
Nature Medicine (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Non-communicable disease research
- December 2016
- The Lancet Diabetes & Endocrinology 1(3)
- CC BY-NC-SA

- London School of Hygiene and Tropical Medicine
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- BMC Int Health Hum Right

- Jochen O. Mierau
- MOL BIOL REP

- María Belén Batanero Hernán

- Dan Chisholm

- Walter C. Willett
- Jeffrey P Koplan

- Stephen S Lim
- Jeremy A Lauer
- Cecilia R Sepulveda
- Christopher J L Murray

- Dr David B Evans
- Ruth Roemer
- Prabhat Jha

- David Kessler
- K Srinath Reddy

- Michele Cecchini
- Franco Sassi
- Daniel Chisholm
- Peter Anderson

- Salim Yusuf
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Open access
- Published: 30 October 2020
A research agenda for non-communicable disease prevention and control in India
- Ishu Kataria ORCID: orcid.org/0000-0002-8483-8243 1 ,
- Mariam Siddiqui 1 ,
- Theresa Gillespie 2 ,
- Michael Goodman 3 ,
- Preet K. Dhillon 4 ,
- Carla Bann 5 &
- Linda Squiers 5
Health Research Policy and Systems volume 18 , Article number: 126 ( 2020 ) Cite this article
12k Accesses
12 Citations
13 Altmetric
Metrics details
Non-communicable diseases contribute to 62% of total deaths in India; of concern are the preventable premature deaths, which account for a staggering 48% of mortality. The objective of this study was to establish a consensus research agenda for non-communicable disease prevention and control that has the potential to impact polices, programmes and healthcare delivery in India.
To develop a non-communicable disease research agenda, we engaged our community collaborative board and scientific advisory group in a three-step process using two web-based surveys and one in-person meeting. First, the Delphi methodology was used to generate topics. Second, these ideas were deliberated upon during the in-person meeting, leading to the prioritisation of 23 research questions, which were subjected to Strength, Weakness, Opportunities and Threat analysis by the stakeholders using the Snow Card methodology with the scientific advisory group and community collaborative board. This step resulted in the identification of 15 low effort, high impact priority research questions for various health outcomes across research disciplines based on discussion with the larger group to reach consensus. Finally, the second web-based survey resulted in the identification of 15 key priority research questions by all stakeholders as being the most important using a linear mixed effect regression model.
The final set of 15 priority research questions focused on interventions at the individual, community, systems and policy levels. Research questions focused on identifying interventions that strengthen healthcare systems and healthcare delivery, including models of care and improved access to non-communicable disease screening, diagnosis and treatment, determining the impact of government policies, assessing the effectiveness of prevention programmes (e.g. tobacco, environmental improvements), and testing research tools and resources to monitor non-communicable diseases at the population level.
To produce the evidence base for selecting and implementing non-communicable disease programmes and policies in India, investments are needed. These investments should be guided by a national research agenda for the prevention and control of non-communicable diseases in India. Our findings could form the backbone of a national research agenda for non-communicable diseases in India that could be refined and then adopted by government agencies, the private sector, non-governmental and community-based organisations.
Peer Review reports
Non-communicable diseases (NCDs) account for approximately 41 million deaths each year; 15 million of these deaths are considered premature (before the age of 70 years) [ 1 ] and over 85% occur in low- and middle-income countries [ 2 ]. In India, NCDs contribute to 62% of total deaths; of particular concern are preventable premature deaths, which account for a staggering 48% of the overall mortality [ 3 ]. The leading causes of NCD mortality in 2016 were cardiovascular diseases, chronic respiratory diseases, cancers, diabetes, and urogenital, blood and endocrine diseases [ 4 ]. Findings from the India state-level Disease Burden Initiative reveal dramatic increases in disability-adjusted life year rates between 1990 and 2016 for two specific NCDs – diabetes and ischemic heart disease. The high prevalence of major risk factors, such as tobacco use, harmful consumption of alcohol, poor diet and physical inactivity, are contributing to the rising burden of NCDs [ 5 ]. If the four major NCDs (diabetes, cardiovascular disease, chronic respiratory disease and cancer) are left unaddressed, they could cost India approximately US$ 3.55 trillion in economic losses by 2030 [ 6 ].
In order to effectively address the growing burden of NCDs, there is a need for adequate country level data, which are currently lacking in India [ 7 ]. Comprehensive monitoring of epidemiological trends for NCD risk factors will be crucial to accurately estimate disease burden and inform policy and programme implementation and evaluation [ 8 ]. The Government of India (GoI) has committed to meeting the NCD-related Sustainable Development Goal target, which states that “ by 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being ” [ 9 ]. To achieve this target, GoI has launched the National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS) with a focus on strengthening infrastructure, human resources, health promotion, early diagnosis, treatment and referral [ 10 ]. In July 2017, India presented its Voluntary National Review on the Implementation of Sustainable Development Goals at the High-Level Political Forum held at United Nations Headquarters in New York [ 11 ]. So far, the GoI has established various NCD cells, which are responsible for managing the NPCDCS programme and are tasked to implement and oversee NPCDCS’ programme activities at state, district, community health centre and sub-centre levels. The activities addressed by the NCD cells include health promotion, early diagnosis, treatment and referral, building strong monitoring and evaluation systems through the public health infrastructure, and disease-specific care centres at district and state level across the country [ 11 ].
To address the NCD challenge, India will need to use interventions shown by research to reduce the risk, prevalence and incidence of NCDs. However, the number of well-studied and tested NCD-related interventions, policies, infrastructure investments and changes to health systems in India is relatively small [ 12 ]. Concerted efforts and collaborative research will be required to determine which interventions are most effective for different populations throughout India. However, the research infrastructure to produce these evidence-based interventions is lacking.
To help address this gap in research infrastructure, the National Institutes of Health (NIH) provided Emory University with a 2-year planning grant to develop a Regional Center of Research Excellence (RCRE) in NCDs in India (Planning grant for Regional Centers of Research Excellence in Non-communicable Diseases). Activities under this grant were conducted with support from the Public Health Foundation of India and RTI International and focused on the northern and southern regions of India. A key activity of the RCRE was to develop a comprehensive research agenda for NCD prevention and control in India. At the time the RCRE was formed, an agenda to establish priorities for research to inform NCD prevention and control efforts and guide funding in India did not exist. The purpose of this manuscript is to describe the methods used to develop a consensus-based set of research priorities and share the results. These results can be used as the foundation for the development of a research agenda for NCD prevention and control in India.
To develop an NCD research agenda for India, we engaged a broad range of stakeholders in the fields of NCD policy, public health, research, clinical care and leadership to ensure diverse perspectives were represented during consensus building. We included individuals who served on the community collaborative board (CCB) and the scientific advisory group (SAG) who were a part of the RCRE planning grant. The SAG included scientists with established expertise in NCD research and various aspects of infrastructure development, research, and research enhancement and policy relevant for the region whereas the CCB included national- and state-level stakeholders promoting attention to community interests, strengthening relationships between investigators and stakeholders involved in NCD prevention and treatment. The members covered various disciplines and had a north–south distribution amongst themselves (Table 1 ).
We implemented a three-step process that incorporated both qualitative and quantitative research methods to identify, generate and prioritise research questions that, if answered, had the potential to reduce the incidence of NCDs in India. Table 2 presents an overview of each step, its purpose, the data collection method used and the final product developed.
Step 1. Idea generation
To generate ideas about research that should be conducted to reduce the incidence of NCDs in India, we used the Delphi method, which is a consensus building process that gathers diverse perspectives and organisational agendas from a variety of different experts or stakeholders. Using an iterative approach, stakeholders rate and rank the different ideas that are shared by experts or stakeholders [ 13 ]. To collect stakeholders’ perspectives about what they saw as important research questions that needed to be answered to reduce the incidence of major NCDs in India, we conducted an online survey with all stakeholders from both SAG and CCB ( n = 30). We asked participants to list at least two priority research questions for each of the following health issues: cardiovascular disease, cancer, diabetes, chronic respiratory diseases and mental health. We used these main category descriptors for NCDs to be in line with the new WHO 5 × 5 framework for NCDs [ 14 ]. Next, we asked participants to identify research questions or issues for each of the following research disciplines: epidemiology, clinical research, biostatistics, health systems strengthening, health economics, health promotion, implementation science and health policy. For each research question, we asked participants to share the reason they prioritised the question. A total of 19 participants responded (63.3%), helping generate 165 research questions. After accounting for clustering and duplication, we had 56 unique research questions.
Step 2. Shared prioritisation
To obtain feedback on the 56 unique research questions, we held an in-person meeting where these 19 participants had the opportunity to review and deliberate about the research questions identified in Step 1. The 56 research questions were listed on four large sheets of paper and taped around the room. Each participant was given a set of 10 stickers and asked to place them next to the research question(s) that they felt were most important for the prevention and control of NCDs in India. Participants did this exercise individually, without discussing their selections with other participants. Each participant could either place all 10 stickers on one of the 56 research questions or distribute them among the many research questions based on their relative importance. This resulted in the identification of 23 research questions that were assumed to be most important as they received maximum votes. We then asked participants to perform a small group SWOT (Strength, Weakness, Opportunity and Threat) analysis, which was done using Snow Card methodology – a nominal group technique used to identify and analyse the strengths, weaknesses, opportunities, and challenges in a strategic planning process. Through this method, the diverse ideas expressed in a group of participants can be integrated to represent agreement on a particular issue [ 15 ]. We organised participants into five groups. We assigned each group four or five priority research questions. For every priority research question, each individual in the group listed the Strength(s) and Weakness(s) of the research question, as well as the Opportunities for success that the research question could bring and the Threats, or opposition or challenges in implementing the research question, and what their own organisation could contribute toward addressing the research question. This individual exercise was followed by a small group discussion, in which members discussed the collective assessments of the research questions’ priorities assigned to them until they reached consensus. A volunteer from each group was asked to report the results of the SWOT analysis back to the larger group. The final step was to categorise prioritised research questions within the larger group based on level of effort (low versus high) and potential to impact (low versus high). This categorisation exercise resulted in a set of 15 priority research questions that were deemed by the group as low effort, high impact.
Step 3: Final prioritisation
All the stakeholders who were a part of the in-person meeting were invited to complete a second online survey to rank the final set of 15 research questions. They ranked the research questions in order of importance (1 = most important to 15 = least important). We computed the mean of these rankings across stakeholders for each of the research questions. Because the same individuals ranked each research question, we treated the values as repeated measurements and analysed them using a linear mixed effect regression model. In this model, the outcome was ranking (i.e. 1 to 15), research question was a fixed effect predictor variable and person was a random effect. Within this model, contrast statements were used to compute pairwise comparisons between research questions. A significant difference between a pair of research questions would indicate that stakeholders ranked one research question significantly higher (or lower) than the other.
The least squares mean of ranking for each research question and the main issue the research question addresses are presented in Table 3 . The order in which the questions are listed in the table is the final ranking of the priorities. The lowest mean ranking, which means the topic that was ranked as most important, was for ‘Development of interventions to empower primary physicians and health workers in early diagnosis of NCDs’. The topic that had the lowest mean ranking was understanding the ‘Impact of enabling environment (e.g. green spaces for promotion of physical activity) to prevent and control NCDs’. Priorities focused on identifying interventions that strengthen healthcare systems (Q2) and healthcare delivery, including models of care (Q3) and improved access to NCD screening, diagnosis and treatment (Q1, Q5, Q6, Q8). Research that examines how government policies (Q7) and mandates, such as adding HPV vaccination to the National Immunization Programme (Q12), affect the incidence and prevalence of NCDs were also prioritised by stakeholders. Prevention programmes, such as tobacco prevention (Q9), environmental improvements [ 16 ] and the role of Ayurveda, Yoga & Naturopathy, Unani, Siddha and Homeopathy (Q14), were also proposed as priorities. Finally, research tools (Q4) and resources (Q11) to monitor NCDs at the population level were deemed important as was understanding factors that improve the quality of life of people with NCDs.
Interventions that have been tested regionally and locally are needed to reduce the incidence, prevalence, morbidity and mortality of NCDs. By creating the NPCDCS Programme, the GoI has signalled that reducing NCDs is a priority and research to create the evidence-base for programmatic efforts needs to be funded. An NCD research agenda for India is needed to guide funding and establish research priorities. Our findings represent research questions that (1) have the potential to have a high impact, (2) are relatively feasible to answer in terms of level of effort, and (3) have been vetted by knowledgeable stakeholders representing a variety of different disciplines and fields involved in NCD prevention and control in India. The research questions included identifying and testing interventions at the individual, community, systems, and policy levels and can contribute to a national research agenda for NCD prevention and control in India.
Having an established and promoted research agenda to guide funding and researchers would allow stakeholders, such as GoI, academia, healthcare delivery institutions, healthcare providers and communities, to develop collaborative research that answers the most important research questions that have the potential to reduce the burden of NCDs in India.
It is important that we acknowledge the limitations of our approach and how these may have affected our findings. First, the study participants were recruited as either members of the SAG and CCB developed for the NIH-funded RCRE for NCDs, which focused on two regions of India – New Delhi in the north and Chennai in the south. When we asked participants to share their opinions about the most important research questions that needed to be answered, we did ask participants to focus on the country of India in its entirety. However, because participants worked in predominantly in these two regions, their opinions may have been shaped by their current work and personal experiences in these regions. Second, the wording and framing of the questions we asked participants in all three steps of the prioritisation process likely influenced their responses. For example, when we original solicited research questions participants believed to be important, we asked about the specific health issues, namely cardiovascular disease, cancer, diabetes, chronic respiratory diseases and mental health. We did not include other categories of NCDs (e.g. accidents and injuries) or call out stroke separately from cardiovascular disease as has been done by others [ 16 ]. Our word choice (e.g. using the term chronic respiratory diseases versus lung disease) may have affected the research questions generated by participants. Third, we asked participants to prioritise research questions that would have a high impact and low level of effort so that we ended up with a list of priorities that was feasible to address. As a result, our results do not represent research that could have a high impact and high level of effort. Even with these limitations, these research questions can serve as the beginnings of or as the impetus for a formal research agenda that can support the development and implementation of cost-effective strategies to prevent and control NCDs in India, thereby achieving our NCD targets.
Investments in research are needed to produce the evidence base for selecting and implementing NCD programmes and policies in India. These efforts should be guided by a national research agenda for the prevention and control of NCDs in India. Our findings could form the backbone of a national research agenda for NCDs in India that could be refined and then adopted by government and private, non-governmental and other community-based organisations.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
Community Collaborative Board
Government of India
Non-communicable Diseases
National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Disease and Stroke
Regional Center for Research Excellence
Scientific Advisory Group
Strength, Weakness, Opportunity, and Threat
World Health Organization. Global Action Plan for the prevention and control of noncommunicable diseases 2013–2020. 2012. https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf;jsessionid=52E1B3C677527E0D4DB828DDB046B5A3?sequence=1 . Accessed 21 Jan 2019.
World Health Organization. Noncommunicable diseases factsheet. 2019. http://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases . Accessed 19 Jan 2019.
India State-Level Disease Burden Initiative Collaborators. Nations within a nation: variations in epidemiological transition across the states of India, 1990-2016 in the Global Burden of Disease Study. Lancet. 2017;390(10111):2437–60.
Article Google Scholar
Indian Council of Medical Research, Public Health Foundation of India, Institute for Health Metrics and Evaluation. India: Health of the Nation’s States—The India State-Level Disease Burden Initiative. New Delhi: ICMR, PHFI, and IHME; 2017. https://phfi.org/wp-content/uploads/2018/05/2017-India-State-Level-Disease-Burden-Initiative-Full-Report.pdf . Accessed 20 Jan 2019.
Sinha R, Pati S. Addressing the escalating burden of chronic diseases in India: need for strengthening primary care. J Family Med Prim Care. 2017;6(4):701–8.
Article PubMed Central PubMed Google Scholar
Bloom DE, Cafiero-Fonseca ET, Candeias V, Adashi E, Bloom L, Gurfein L, et al. Economics of Non-Communicable Diseases in India: The Costs and Returns on Investment of Interventions to Promote Healthy Living and Prevent, Treat, and Manage NCDs. Boston: World Economic Forum, Harvard School of Public Health; 2014. http://www3.weforum.org/docs/WEF_EconomicNonCommunicableDiseasesIndia_Report_2014.pdf . Accessed 21 Jan 2019.
Nethan S, Sinha D, Mehrotra R. Non communicable disease risk factors and their trends in India. Asian Pac J Cancer Prev. 2017;18(7):2005–10.
PubMed PubMed Central Google Scholar
Raban MZ, Dandona R, Dandona L. Availability of data for monitoring noncommunicable disease risk factors in India. Bull World Health Organ. 2012;90(1):20–9.
Article PubMed Google Scholar
United Nations. SDG3: Good Health and Wellbeing. https://in.one.un.org/page/sustainable-development-goals/sdg-3-2/#:~:text=By%202030%2C%20end%20the%20epidemics,mental%20health%20and%20well%2Dbeing . Accessed 21 Jan 2019.
Ministry of Health & Family Welfare. National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS). New Delhi: MoHFW; 2013. https://mohfw.gov.in/sites/default/files/Operational%20Guidelines%20of%20NPCDCS%20%28Revised%20-%202013-17%29_1.pdf . Accessed 19 Feb 2019.
Ministry of Health & Family Welfare. Voluntary National Review Report on the Implementation of Sustainable Development Goals. New Delhi: MoHFW; 2017. https://sustainabledevelopment.un.org/content/documents/15836India.pdf . Accessed 19 Feb 2019.
Arokiasamy P. India's escalating burden of non-communicable diseases. Lancet Glob Health. 2018;6(12):e1262–3.
Gilmore GD. Multi-step surveys: the Delphi technique. In: Gilmore G, Campbell D, editors. Needs and Capacity Assessment Strategies for Health Education and Health Promotion. Sudbury: Jones & Bartlett Learning; 2004.
UN General Assembly (73rd session: 2018–2019). Political declaration of the 3rd High-Level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases: resolution / adopted by the General Assembly. New York: UN; 2018. https://www.un.org/en/ga/search/view_doc.asp?symbol=A/RES/73/2 . Accessed 13 Feb 2019.
Rideout C, Gil R, Browne R, et al. Using the Delphi and snow card techniques to build consensus among diverse community and academic stakeholders. Prog Community Health Partnersh. 2013;7(3):331–9.
Upadhyay RP. An overview of the burden of non-communicable diseases in India. Iran J Public Health. 2012;41(3):1–8.
Download references
Acknowledgements
We acknowledge Meera Viswanathan from RTI International and members of the Community Collaborative Board and Scientific Advisory Group for their valuable inputs.
This planning grant for Regional Centers of Research Excellence in Non-communicable Diseases was funded through NIH/National Cancer Institute under award number P20CA210298 to Emory University in partnership with Public Health Foundation of India and RTI International.
Author information
Authors and affiliations.
Center for Global Noncommunicable Diseases, RTI International, New Delhi, India
Ishu Kataria & Mariam Siddiqui
Winship Cancer Institute, Department of Surgery, Emory University, Atlanta, GA, United States of America
Theresa Gillespie
Rollins School of Public Health, Department of Epidemiology, Emory University, Atlanta, GA, United States of America
Michael Goodman
Center for Chronic Disease Control and Public Health Foundation of India, New Delhi, India
Preet K. Dhillon
RTI International, Durham, NC, United States of America
Carla Bann & Linda Squiers
You can also search for this author in PubMed Google Scholar
Contributions
IK and MS conceptualised the research. CB performed the statistical analysis. IK and LS interpreted the results. IK and MS wrote the first draft of the manuscript. IK, MS, TG, MG, PKD and LS reviewed the draft and revised it for important intellectual content. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Ishu Kataria .
Ethics declarations
Ethics approval and consent to participate.
The research was reviewed and approved by the Institutional Review Board of RTI International and Emory University. Written informed consent was obtained from the participants. The consent form is held by RTI International and is available for review by the Editor-in-Chief.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kataria, I., Siddiqui, M., Gillespie, T. et al. A research agenda for non-communicable disease prevention and control in India. Health Res Policy Sys 18 , 126 (2020). https://doi.org/10.1186/s12961-020-00639-0
Download citation
Received : 05 December 2019
Accepted : 30 September 2020
Published : 30 October 2020
DOI : https://doi.org/10.1186/s12961-020-00639-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Non-communicable diseases
- Primary Care
- Universal Health Coverage
- Health System Strengthening
- Integrated Care
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
REVIEW article
Management and prevention strategies for non-communicable diseases (ncds) and their risk factors.

- 1 Panevezys Faculty of Technology and Business, Kaunas Technology University (KTU), Panevezys, Lithuania
- 2 Department of Biochemistry, Faculty of Science, King Abdulaziz University (KAU), Jeddah, Saudi Arabia
- 3 Division of Protein Science, Kungliga Tekniska Högskolan Royal Institute of Technology, Stockholm, Sweden
- 4 Department of Medical Laboratory Science, Charmo University, Chamchamal, Iraq
- 5 Procomcure Biotech, GmbH, Thalgau, Austria
- 6 Prosthetics, Biomechanics and Biomaterial Research, Paracelsus Medical University Salzburg, Salzburg, Austria
- 7 Bioprospecting Departament, Baltic Institute of Advanced Technology, Vilnius, Lithuania
- 8 Faculty of Medicine, Ludwig Maximilian University of Munich (LMU), Munich, Germany
Non-communicable diseases (NCDs) are of increasing concern for society and national governments, as well as globally due to their high mortality rate. The main risk factors of NCDs can be classified into the categories of self-management, genetic factors, environmental factors, factors of medical conditions, and socio-demographic factors. The main focus is on the elements of self-management and to reach a consensus about the influence of food on risk management and actions toward the prevention of NCDs at all stages of life. Nutrition interventions are essential in managing the risk of NCDs. As they are of the utmost importance, this review highlights NCDs and their risk factors and outlines several common prevention strategies. We foresee that the best prevention management strategy will include individual (lifestyle management), societal (awareness management), national (health policy decisions), and global (health strategy) elements, with target actions, such as multi-sectoral partnership, knowledge and information management, and innovations. The most effective preventative strategy is the one that leads to changes in lifestyle with respect to diet, physical activities, cessation of smoking, and the control of metabolic disorders.
Introduction
Non-communicable diseases (NCDs), also known as chronic diseases, are medical conditions that are associated with long durations and slow progress ( Figure 1 ). Most NCDs are non-infectious and are the result of several factors, including genetic, physiological, behavioral, and environmental factors ( 1 ). According to the World Health Organization (WHO), NCDs are the leading cause of death worldwide, responsible for 71% of the total number of deaths each year. The top four killers among NCDs with the highest number of deaths are cardiovascular diseases (17.9 million deaths annually), cancers (9.0 million), respiratory diseases (3.9 million), and diabetes (1.6 million) ( Figure 1 ) ( 1 ). However, the term of NCDs has been extended to cover a wide range of health problems, such as hepatic, renal, and gastroenterological diseases, endocrine, hematological, and neurological disorders, dermatological conditions, genetic disorders, trauma, mental disorders, and disabilities (e.g., blindness and deafness) ( 2 ). The main risk factors contributing to NCDs involve unhealthy diets, physical inactivity, tobacco use, and alcohol misuse. Hence, most of these diseases are preventable as they eventually progress in early life due to lifestyle aspects ( 3 ). There is an increasing concern that poor diet has increased the potential risk, causing chronic diseases, and nutrition problems in the public health sector ( 4 ). Historically, many NCDs have been directly linked to economic growth and were called “diseases of the rich.” Now, the burden of NCDs in developing countries has increased. Further, mortality in low and middle-income countries has doubled the burden of NCDs. The growing interest in population well-being and economic growth, based on Gross National Happiness (GNH), has recently attracted more attention. The epidemic of NCDs hinders the progress of GNH because good health is necessary in order to achieve happiness ( 5 ). Bhutan's experience suggests that strategic opportunities to minimize NCDs and to promote population well-being can be taken advantage of by joining the health sector with other sectors at the individual and organizational levels ( 5 ).
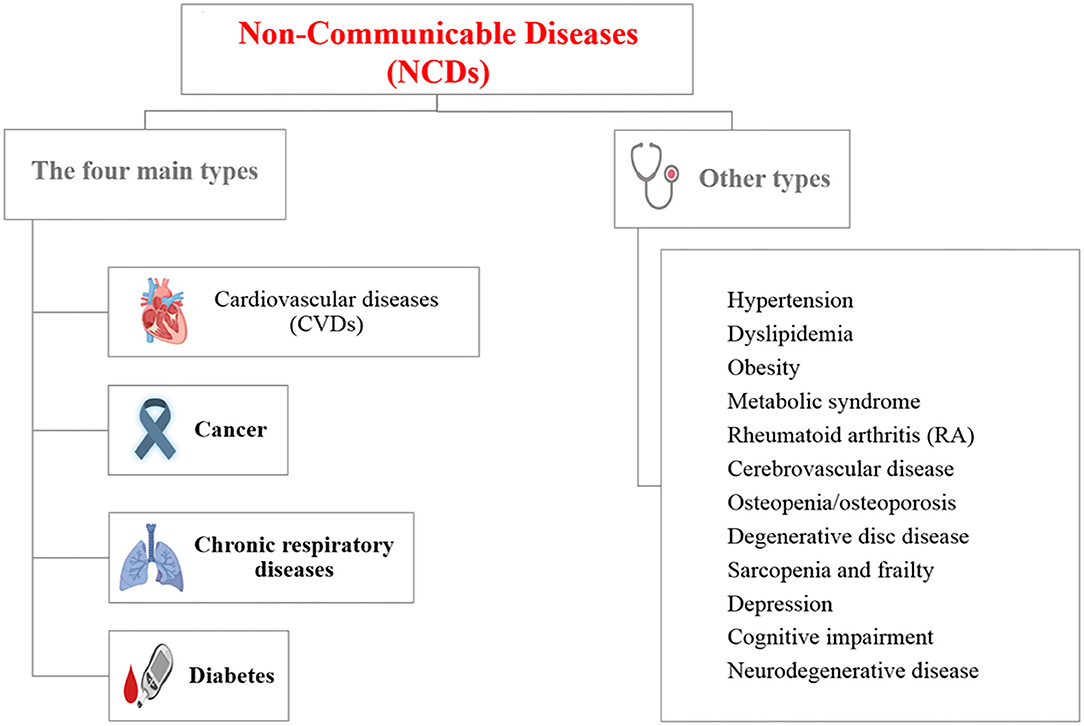
Figure 1 . List of non-communicable diseases (NCDs) [Created with BioRender].
Health and well-being are the primary goals of society in regards to food choice ( 6 ). Researchers have pointed out that the core of the health-conscious lifestyle is directed toward a wellness-oriented lifestyle ( 5 ) and the behavior of people determines their health status ( 7 ). Nutritionists have been reported to be associated with many chronic diseases, but designed studies exploring the association between diet, nutrition, and NCDs are rare ( 8 ). Thus, lifestyle modifications and interventions to reduce the risk of NCDs is the priority in the primary prevention of diseases. Hence, finding answers to the following questions can significantly contribute to a better and healthier society:
• What are NCDs and their risk factors?
• What are the most used interventions in managing the risk of NCDs?
• What are the contemporary prevention strategies for NCDs?
The current review focuses on the answers to the previous questions and highlights several strategic models in the contemporary management of NCDs.
Key Risk Factors of NCDs
Several factors can increase the amount of opportunities to develop NCDs and can be classified in different ways. In one approach, risk factors are classified as modifiable or non-modifiable factors that can have changeable or non-changeable conditions, respectively. The modifiable risk factors involve high blood pressure, smoking, diabetes mellitus, physical inactivity, obesity, and high blood cholesterol, while the non-modifiable risk factors involve age, gender, genetic factors, race, and ethnicity ( 9 – 12 ). Interestingly, although age and gender are non-modifiable factors, most of their associated factors are modifiable. Figure 2 represents a model to classify the risk factors of NCDs. The non-modifiable factors can also be classified into three classes: (i) biological factors, such as being overweight, dyslipidemia, hyper-insulinaemia, and hypertension; (ii) behavioral factors, such as diet, lack physical activity, tobacco smoking, and alcohol consumption; and (iii) societal factors, which involve complex combinations of interacting socioeconomic, cultural and environmental parameters ( 13 ). In the next section, examples of the identified risk factors for NCDs, including age, diet, and economic context, are highlighted.
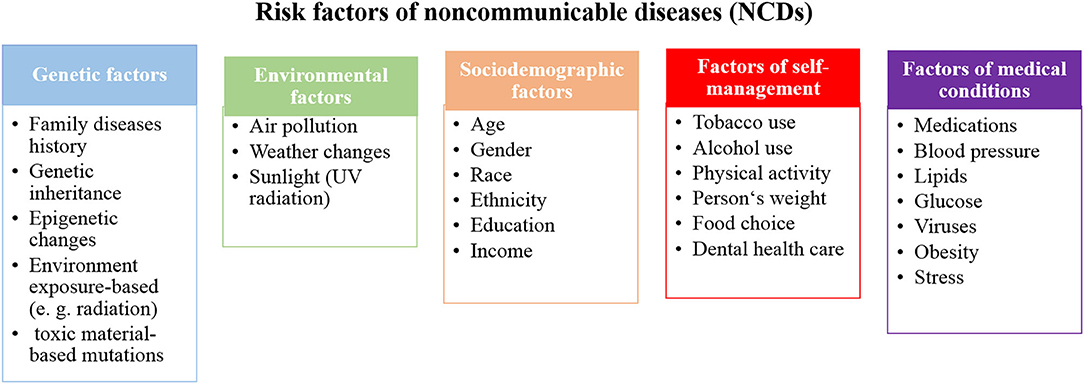
Figure 2 . A proposed model to classify the risk factors of NCDs.
While NCDs are usually associated with elderly people, all ages are at risk, even before birth. These diseases may start in the earliest years of life and keep progressing during childhood, adolescence, and old age ( 14 ). However, 15 million deaths due to NCDs were recorded from people aged between 30 and 69 years of age and more than 82% of these “premature” deaths were from low and middle-income countries ( 15 ). The life-course perspective is evidence of the origin of adult NCDs, which are determined in uterus. Barker ( 16 ) showed that maternal nutrition plays a significant role in adult diseases. He found that adapting human fetuses to a limited supply of nutrients resulted in permanent structure and metabolism changes. Subsequently, such programmed changes may have attributed to several diseases, such as heart disease, diabetes and hypertension in later life ( 16 , 17 ). Moreover, unborn babies are not only negatively influenced by maternal habits, such as diet, drug, stress, alcohol and tobacco consumption during pregnancy, but environmental factors, such as air pollution, also have an effect. These factors influence the fetal and early brain development, for example, a low birth weight is attributable to poor long-term health and poor cognition ( 14 , 18 ).
In the period of childhood, new risks of NCDs may appear due to the easy access to unhealthy food and drinks in kindergartens and schools. Thus, this leads to a high number of overweight and obese children ( 19 ). After that stage of life, young people in the adolescence stage can acquire new and harmful habits, such as smoking and drinking alcohol, which can significantly contribute to NCD risk ( 20 , 21 ). These bad habits may continue during adulthood with additional aspects facing adults in workplaces, including financial stressors, unemployment, unsatisfying careers, and low social engagement, which influence the progress of NCDs ( 20 , 22 ). Retirement and leaving a workplace can provide new challenges among elderly people and influence the development of NCDs. Poor nutrition, lack of physical activity, alcohol and tobacco use, social isolation, and financial stress directly affect older people and strongly promotes NCDs ( 20 ).
The prevention and control of NCDs can be achieved at all ages. The health status of women before and during pregnancy influences the susceptibility of children to NCDs in later life ( 20 , 23 ). This is the most important strategy to control NCDs because it targets the root of the problem. Applying high standards for food and drinks, increased physical activity in schools and workplaces, in addition to monitoring air quality and offering smoke-free zones can largely prevent NCDs at all stages of life. However, taxation and creating restricted policy for the marketing of unhealthy food, sugary drinks, tobacco, and alcohol can largely improve health statistics. Further, as obese children and elderly people are at a high risk of social isolation, it is important, for their mental and physical health, to be involved in social activities ( 20 , 24 ).
Diets and Lifestyle
In the past, infectious and parasitic diseases were the main causes of death, but in the recent decades, NCDs have replaced them and have become the main cause of deaths ( 25 ). This may be attributed to the change of diet habits and lifestyle over the years, which can be classified as a shift of disease patterns in humans. Various dietary factors, such as meat, whole grain products, healthy dietary patterns, sugar-sweetened beverage consumption, and iron-based diets have an obvious relationship with NCDs ( 11 , 12 ). Additionally, the high consumption of processed meat and sugar-sweetened beverages, combined with other unhealthy lifestyle factors, such as a high body mass index (BMI), physical inactivity, and smoking have a marked association with NCDs ( 26 , 27 ). Whole-grain products are independent of the BMI and have protective effects, due to their high fiber contents and ability to slowly release glucose into circulation; subsequently, this reduces the postprandial insulin response and may improve insulin sensitivity ( 26 , 28 – 31 ).
Dietary transition describes the changes in production, processing, availability, dietary consumption, and energy expenditure. Further, the concept becomes wider and involves body composition, anthropometrical parameters, and physical activity ( 32 , 33 ). The use of dietary transition terms arises due to the shift to western diets in developing countries in particular. Traditional food in most countries is healthier, natural, and richer in fiber, and cereal has been replaced by unhealthy processed food that is rich in sugars and fats, animal-source foods, and refined carbohydrates. Hence, low and middle-income countries have seen rapid changes in nutrition transition and rapid increases in NCDs ( 34 ). High food consumption and declining physical activity rates occur simultaneously, resulting in NCDs. The main factor, attributable to physical inactivity, is the rapid and continuous development in technology. The easy access to modern technology and manufacturing in houses and workplaces, including machines, vehicles and labor-saving technology, make life easier but unhealthier from the perspective of reducing the risk of NCDs ( 34 ).
The Economic Context
NCDs are already common in developed countries and rapidly propagate. Spreading western lifestyle in low and middle-income countries, due to global population aging and commercial pressures for unhealthy diets and cigarettes, contributes to the increasing rate of NCDs in these countries ( 35 ). There is a direct relationship between poor health and low-income, which contributes to food poverty, purchasing of cheaper and unhealthy dietary products, and expensive treatments, in addition to psychosocial factors. People with low-incomes have the feeling that they occupy a lower status in society, which prevents them from participating in social life ( 36 ). However, food poverty, poor mobility and lack of physical activity are also serious problems in high-income countries ( 37 ).
There is a growing trend to consider social, political, and economic systems as critical factors that impact NCDs besides individual behavior/lifestyle ( 38 , 39 ). Krieger's Ecosocial theory highlights ecosocial disease distribution which describes how diversity between historical, societal, and ecological conditions significantly contributes to changes in the health outcomes of various social groups ( 39 ). For example, the bad side of economic and health inequality that already exists for many years becomes obvious with the current coronavirus COVID-19 pandemic. According to Krieger's research, the higher number of COVID-19 deaths in African American than whites in the US is attributed to several factors involve living in crowded places, using public transportation to commute to work, working in service jobs in close contact with others, and shortage of protective equipment at workplaces. Furthermore, the lack of access to health care and health insurance, and pre-existing health conditions may be increased the risk from COVID-19 in the African American population ( 40 ).
Key Diseases
Cardiovascular diseases (cvds).
CVDs are the leading contributors to the global burden of disease among the NCDs and account for the most deaths worldwide each year—even more than the number of deaths from cancer and chronic respiratory diseases combined ( 41 , 42 ). CVDs are a group of disorders that are not only related to heart conditions, such as ischaemic heart disease (IHD), stroke, congenital heart disease, coronary heart disease, cerebrovascular disease, peripheral arterial disease, and rheumatic heart disease, but also to blood vessels that involve hypertension, and conditions associated with cerebral, carotid, and peripheral circulation ( 43 ). While CVDs equally affect both sexes, men suffer from higher incidences than women. Still, CVDs are the leading cause of death of women in developed countries ( 44 ). Moreover, many epidemiological studies show the relationship between periodontal disease (PD) and cardiovascular disease. Mild forms of PD affect 75% of adults in the US, and more severe forms affect 20 to 30% of adults. Since PD is common, it is responsible for a significant proportion of proposed infection-associated risks of cardiovascular diseases ( 45 , 46 ).
According to the American Heart Association, there are seven key health factors and behaviors that contribute to the increasing risks of heart disease and stroke: nutrition, smoking, overweight/obesity, physical inactivity, uncontrolled blood pressure, elevated levels of cholesterol, and blood sugar ( 42 ).
Most CVDs can be prevented by addressing the seven risk factors, which involves healthy diets, regular physical activity, avoiding smoking and second-hand smoking, reaching and maintaining a healthy weight, and keeping blood pressure, cholesterol, and blood sugar levels under control ( 42 ).
Cancer is the main public health problem and the second main cause of death globally [who]. It shares the common risk factors with other key diseases of NCDs and several identified and unidentified factors can be attributed to cancer. The causes of cancer can be classified into three categories, including: (i) biological carcinogens (e.g., viral, bacterial, or parasites infections, hormonal and genetics factors); (ii) chemical carcinogens (such as food and water contamination, and tobacco smoking); and (iii) physical carcinogens (such as ultraviolet and ionizing radiation). However, tobacco smoking is considered to be the main cause of cancer, followed by poor diets ( 47 – 49 ). Moreover, together, body weight and lack physical activity are also associated with the most common cancers, including breast (postmenopausal), colon, endometrium, kidney, and esophagus cancers ( 50 ). According to WHO report in 2018, the most common cancers are lung, breast, colorectal, prostate, skin, and stomach, while the most cancer deaths are from cancer of the lung, colorectal, stomach, liver, and breast ( 48 ). A noticeable decrease in the cancer death rates of lung, breast, colon/rectum, and prostate is achieved in high-income countries, but are still high in low and middle-income countries ( 51 ). Further, the incidence of several cancers, including lung, breast, prostate, colon, and rectum, is commonly elevated concurrently with economic development. In contrast, the incidence of stomach cancer declines with economic development ( 48 ). The guidelines for oncological disease prevention and early detection are based on cancer risk assessment, including past medical history, lifestyle factors, family diseases history, and genetic testing ( 10 ).
Lung cancer, which is the most common cancer in the world, is mainly the result of smoking and the risk increases in heavy smokers ( 52 ). Further, several studies reported low intakes of fruits, vegetables and related nutrients in lung cancer patients ( 53 , 54 ). Hence, it is possible to prevent lung cancer by stopping the prevalence of smoking and by increasing fruit and vegetable consumption. Furthermore, dietary habits and physical activity contribute to breast cancer, which is the second most common cancer in the world and the most common cancer among women. Excess adiposity and hormonal mechanisms appeared to play key roles in breast cancer progress, and are effected by dietary intake during childhood and adolescence ( 51 , 55 , 56 ). Hence, maintaining a healthy weight throughout life can minimize the chances of breast cancer. Another type of cancer that is strongly associated with diet is colorectal cancer. High intakes of meat and fat, and low intakes of fruits and vegetables, dietary fiber, vitamins and minerals are related to an increased risk of colorectal cancer ( 57 ). Hence, minimizing or stopping the consumption of meat, especially preserved meats, can reduces the risk of this cancer. Stomach cancer was the main cause of mortality globally, but is currently decreasing in industrialized countries. It is associated with dietary habits and vitamin C intake ( 48 ). Helicobacter pylori infection is considered to be a type I carcinogen and as the strongest known risk factor of gastric cancer ( 58 ). Cancers caused by infections are three times lower in developed countries than in developing ones. It is important to avoid the infection in order to prevent cancer, and that can be achieved by eating food that is properly prepared, drinking water from clean sources, taking vitamins according to the recommended dietary allowance, and avoiding the extensive use of antibiotics in order to reduce antibiotic resistant strains ( 51 ).
Chronic Respiratory Diseases (CRDs)
CRDs cover a wide range of diseases in the airways and the other structures of the lungs. Most of the morbidity and mortality of CRDs is increased with age. CRDs include chronic obstructive pulmonary disease (COPD), occupational lung diseases, asthma and respiratory allergies, sleep apnoea syndrome, and pulmonary hypertension. Asthma and COPD account for most of the deaths among CRDs in low and middle-income countries ( 59 – 61 ). Genetic and environmental factors are the risk factors of CRDs; environmental factors are more dominant. These factors include air pollution exposure, including tobacco smoke and second-hand tobacco smoke, indoor and outdoor air pollution, occupational exposures, and socioeconomic factors ( 62 , 63 ).
CRDs are not fully reversible and are partially preventable ( 64 ). During pregnancy, maternal smoking contributes to lung dysfunction in children at birth. Further, in early life, a child's health affects their subsequent respiratory health. Thus, following a healthy lifestyle in the early ages of life, avoiding respiratory infections, and avoiding environmental and occupational agents can effectively prevent CRDs. Preventing exposure to indoor and outdoor pollutants can be achieved by filtration and ventilation, in addition to the use of natural gas ( 27 ).
Diabetes Mellitus
Diabetes has attracted global attention due to its elevating prevalence and incidence. It is not only a chronic disease, but also an acutely life-threatening condition. Further, it may cause other serious diseases such as heart diseases, kidney failure, and eye damage, which may subsequently lead to blindness, and foot ulcers, which may require limb amputation. The main two types of diabetes are both lead to hyperglycemia. In type 1, the pancreatic β-cells cannot produce a sufficient amount of insulin, while in type 2, the body cells cannot respond properly to insulin ( 64 ). Other types of diabetes involve gestational diabetes mellitus, which occurs in pregnant women with glucose intolerance ( 65 ), and type 3 diabetes, which is associated with Alzheimer's disease, where neurons in the brain cannot respond to insulin ( 66 ). While diabetes can be partially inherited, several lifestyle factors, such as obesity, high sugar consumption, and lack of physical activity can significantly contribute to the progress diabetes. However, lifestyle changes can prevent diabetes and the long-term complications of diabetes. Patients with type 2 diabetes can control or even reverse the diabetes by changing their lifestyle and eating habits. The term “healthy dietary pattern” includes a variety of diets and nutritional factors, for example, reducing the consumption of red and processed meat, sugar-sweetened beverages and alcohol, while increasing the consumption of whole-grain products ( 67 ).
Management of Risk Factors and NCDs
The following sections outline the developed and proposed strategies to manage NCDs and their risk factors from several perspectives.
Management of Risk Factors
The most common causes of NCDs are metabolic and behavioral risk factors and can be largely preventable by several available means. Most global discussions concern the risk factors of self–management (tobacco and alcohol consumption, physical activity, weight, food, and dental health care) and focus on the role of individual responsibility to manage the risk factors of NCDs. Health care specialists should educate patients about their nutrition value and raise the profile of didactics, practicums, and workshops in daily practice ( 68 ). Further, the management of NCDs is the priority of the public health sector in most countries, because management in society is the main direction of NCD prevention strategies. Interventions are used in public health management in an effort to promote good health behavior. For example, India, with its wide sociocultural, economic, and geographical diversity, is implementing multi-sectoral (partnership between different sectors) actions to prevent NCDs, including school health programs, initiatives of National Cancer Control Programme, National Trauma Control program, National Program for Control of Blindness, National Mental Health Programme, the National Tobacco Control Program, and the National Program for Control of Diabetes, Stroke, and Cardiovascular Diseases initiatives ( 69 ). From another approach, researchers also highlight the environmental factors (air pollution, climate changes, sunlight) and their impact on NCD development. Air pollution will be an important challenge in the future and new technologies, such as microchips, will have more of an impact in air monitoring ( 27 ).
Since diet is a common risk factor among most NCDs, it attracts more attention in an effort to find effective strategies to provide healthy food to the community and at all stages of life. Evidence-based nutrition interventions should be a global health priority and the role of the dietary fat studied should be a modifiable variable in the prevention of NCDs ( 29 ). Recent evidence suggests that a diet that is high in healthy fat and rich in unsaturated fatty acids prevents the development of metabolic diseases and reduces cardiovascular events ( 29 ). Many interventions addressing poverty and development have an impact on NCD prevalence and risk ( 69 ). The current evidence is limited to diets, and a positive effect of agricultural-based food security programs on diet indicators has been suggested ( 7 ). A suboptimal diet is the leading risk factor for NCDs and consumption of specific foods, rather than macronutrients or micronutrients; it may be the most significant risk factor for NCDs ( 70 ). Strategic health communication in the population-wide intervention includes engaging the food industry in order to reduce the salt content in foods ( 71 ). The concept of a sustainable diet combines health and environmental concerns and includes the abovementioned risk factors as part of the recommendations to reduce processed meat consumption and to increase whole-grain consumption ( 72 ). Lifestyle activities include healthy diets and focus on limiting the use of salt, sugar, and saturated fats ( 73 ). While our body can synthesize many of the molecules required to function properly, essential nutrients are obtained from food. Carbohydrates, proteins, and fats are the primary components of food. Minerals are inorganic essential nutrients that must be obtained from food. The omega−3 alpha-linolenic and the omega−6 linoleic acids are essential fatty acids that are needed to make some membrane phospholipids. Vitamins (B, C, A, D, E, and K) are the classes of essential organic molecules (such as cofactors) that are required in small quantities for most enzymes to function properly. The absence or low levels of vitamins can have a dramatic effect on health. A focus on the need to meet adequate dietary intakes of essential nutrients ( 74 ) through a healthy diet is considered to be very significant for the aging society ( 74 ). Food supplements are concentrated sources of nutrients (minerals and vitamins) or other substances with a nutritional or physiological effect, which are marketed in the form of pills, capsules, and/or liquids ( Table 1 ). These dietary supplements offer many benefits, including the maintaining of an adequate intake of certain nutrients, to correct nutritional deficiencies, or to support specific physiological functions. Recently, researchers have been looking for new solutions to implement an efficient food production process and to discover the benefits of starch waste on human health.
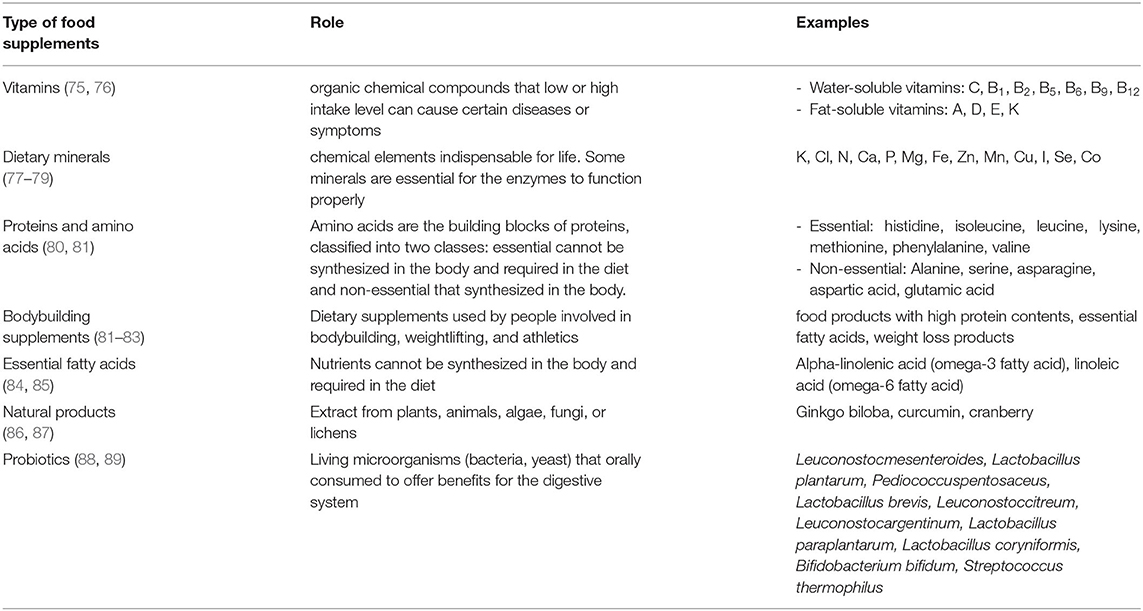
Table 1 . Types of food supplements.
Management of NCDs
NCDs are the silent killers threatening health without showing any symptoms until the problem progresses to an advanced stage. Patients with NCDs, or people with a susceptibility to develop one, need long-term care that is personalized, proactive, and sustainable. Primary health care can organize and deliver healthcare strategies to manage NCDs in each community and to detect diseases at early stages. Thus, they can significantly overcome the challenges linked to a high cost in the health sector. For example, several studies have proved that lifestyle factors have direct links to cancer risk and changing lifestyles, in a positive approach, can considerably minimize the cancer burden. The main risk factors of cancer are age, gender, alcohol, smoking, family disease history, and food ( 90 – 92 ). Cancer can be prevented by changing behavior: dietary improvements, physical activity, weight control, obesity management, tobacco prevention, safe sex and control of oncogenic viruses, sun protection, medications, and lower alcohol consumption ( 26 ).
A dramatic decrease in all cardiovascular disease-related deaths has been recorded in high-income countries, whereas a significant increase was registered in low and middle-income countries ( 93 , 94 ). Checkley et al. reported on NCDs' management in low and middle-income countries ( 95 ). While some people in these countries can access the same treatments that are available in high-income countries, the majority of the population lacks access. The main obstacle causes an increase in the number of patients with NCDs in low and middle-income communities is the absence of a well-designed plan to stop disease occurrence and spreading. Each country needs to prepare its management plan, not just with coping models from high-income countries. Several successful models have been verified, taking into consideration the low-cost strategies to prevent, diagnose and treat NCDs. For example, a cost-effective strategy has been developed in Kenya to diagnose diabetes and hypertension in the early stages of life. While health workers are visiting homes to examine human immunodeficiency virus (HIV) infection, they also measure blood glucose levels and blood pressure. Further, type 2 diabetes is a global pandemic that highly affects human health and global economic development ( 96 ). The International Diabetes Federation reported that there were 415 million people living with type 2 diabetes in 2015, and estimated that the number by 2040 might increase to 642 million, which is attributable to genetic and environmental factors ( 96 ). The genetic–environmental interaction induces insulin resistance and β-cell dysfunction ( 96 ). The epidemic of type 2 diabetes in recent decades has not only attributed to the alteration of the gene pool, but environmental changes also play significant roles in the rapid increase in the prevalence of type 2 diabetes ( 96 ). However, global diabetes mellitus epidemics require the looking for innovative approaches to prevention ( 7 ).
Contemporary Prevention Strategy of NCDs
The prevention strategies of NCDs can include small and large-scale human cooperation ( Figure 3 ). The importance of preventing NCDs arises from the direct impact of NCDs on the decreasing rate of national income. Loss productivity on a large-scale is the result of the inability to work and the frequent absence threats to the national economy. The management strategy to prevent NCDs is based on risk factor management that addresses individual, society, country, and global levels, with actions, such as resource allocation, multi-sectoral partnership, knowledge and information management and innovations. The most critical dimension of the prevention strategy is lifestyle management at the individual level and with a focus on actions, such innovations, which can help the society to increase the awareness of risk factors management, to take health policy decisions at a country level and to develop a health strategy at the global level. The importance of leadership for the change management process is underscored and requires the creation of new approaches to the prevention of NCDs ( 96 , 97 ).
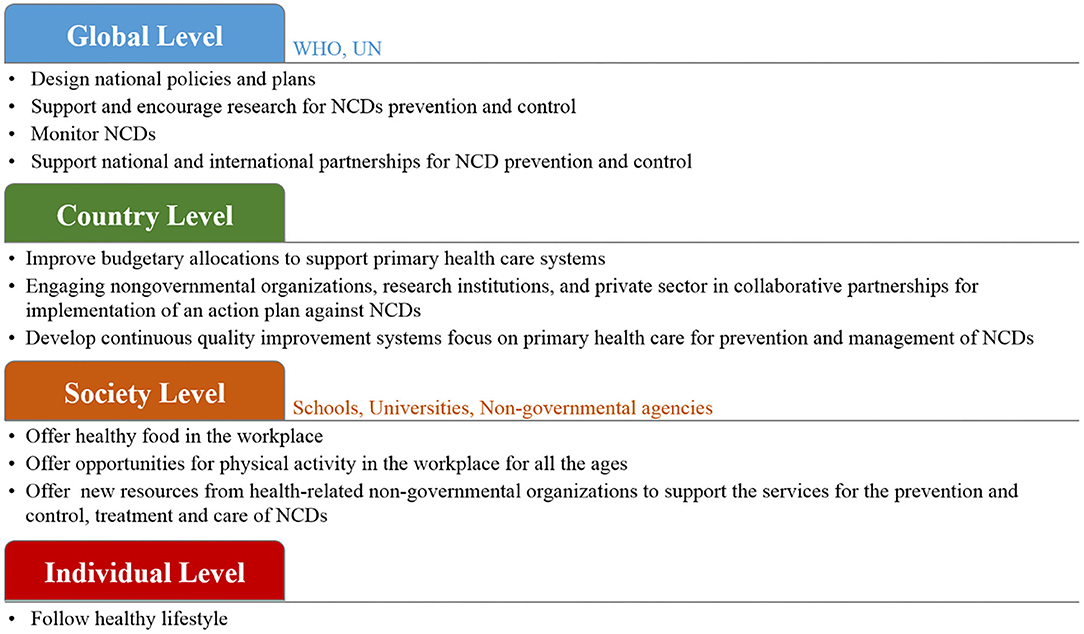
Figure 3 . The proposed prevention management of NCDs with small and large-scale human cooperation.
At the global level, WHO and UN agencies can work together to design policies and strategies to reduce the risk of NCDs ( 98 , 99 ). It is important to monitor NCDs and to assess their progress at the national, regional and global levels. These organization can support research and encourage collaborations among national and international health agencies and academic institutions. Further, tobacco smoke, as a common factor of the four main types of NCDs, must be put under control. The WHO offers help to smokers who have the desire to stop using tobacco products and to implement rules to propose a smoke-free environment. Further, WHO can, by law, protect tobacco control policies from the commercial interests of the tobacco industry. At the country level, each government needs to design its plan based on its economy. Several low-cost and highly effective strategies are available to prevent and manage NCDs ( 100 – 103 ). For example, encouraging people to play sports for physical activity is the most effective factor that can easily influence the prevention of NCDs, and at the same it is time and cost-effective. Moreover, improved budgetary allocations to support primary health care systems should be put in place in order to provide health services to all community members. To achieve large-scale progress, collaboration between governments and various non-governmental organizations, schools, and universities, to provide advice on lifestyle modifications and to warn people about the risks of NCDs, is in high demand. At the society level, research centers and institutes can significantly contribute to the prevention of NCDs by conducting research projects and programs. Focusing research on food biotechnology and agriculture has a direct influence on NCDs risk ( 7 , 104 ). The development of diagnostic tools allows for the rapid detection of NCDs biomarkers with high sensitivity to help detect diseases at their early stages, which subsequently contributes to easier treatment and fast cures ( 105 – 107 ). However, in order to reach the highest attainable standard of health, it is important to encourage individuals and families to follow a healthy lifestyle in order to get an effective response for prevention and the control of NCDs and to improve health outcomes ( 100 , 108 ).
Conclusions
In modern society, NCDs are the main challenge in health systems. Risk factor management is essential in NCDs' management. The management of NCDs requires many strategies from several perspectives and on different levels, including the individual and country levels. Based on the hypotheses that were raised during the above scientific discussion, it can be concluded that modern strategies for the management of NCDs should be oriented toward the individual level, where the individual is responsible for their health by simply following a healthy lifestyle. It is important to combine modern scientific achievements and innovative decisions, with regard to the rationality of nutrition and positive effects on human health. Governments and international organizations should make people aware of their health and their environment to make the world a safe and healthy place. From another perspective, support research to find new techniques to improve food biotechnology is in high demand. Further, finding rapid and sensitive diagnostic platforms to detect NCDs at the point-of-care offers huge benefits to personnel and the healthcare system. The innovations are vital to address the growing crisis of NCDs successfully, and most often use lifestyle projects, the promotion of healthy eating behaviors and smoking cessation. We believe that there is a need to look for further innovations to build better lives in society.
Author Contributions
The manuscript was prepared by AB, SD, and RK. Writing review and editing was done by AB, SD, DS, KO, PS-G, GP, AK, SK, and RK. Final revision and approval was done by RK. All authors contributed to the article and approved the submitted version.
This research was funded by the European Regional Development Fund according to the supported activity Attracting scientists from abroad to carry out research (RK) under Measure No. 01.2.2-LMT-K-718 (project No. 01.2.2-LMT-K-718-02-0012).
Conflict of Interest
KO was employed by the company Procomcure Biotech, GmbH.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. World Health Organization. Noncommunicable Diseases (NCD) . (2019). Available online at: https://www.who.int/gho/ncd/mortality_morbidity/en/ (accessed January 03, 2020).
2. World Health Organization. Global Action Plan: For the Prevention and Control of Non-communicable Diseases . (2013–2020). Available online at: https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf (accessed January 13,2020).
3. Noor NAM, Yap SF, Liew KH, Rajah E. Consumer attitudes toward dietary supplements consumption: implications for pharmaceutical marketing. Int J Pharm Healthc Mark. (2014) 8:6–26. doi: 10.1108/IJPHM-04-2013-0019
CrossRef Full Text | Google Scholar
4. Sithey G, Li M, Thow MA. Strengthening non–communicable disease policy with lessons from Bhutan: linking gross national hapiness and health policy action. J Public Health Policy. (2018) 39:327–42. doi: 10.1057/s41271-018-0135-y
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Goetzke BI, Spiller A. Health-improving lifestyles of organic and functional food consumers. Brit Food J. (2014) 116:510–26. doi: 10.1108/BFJ-03-2012-0073
6. Yang ZY, Yang Z, Zhu L, Qiu C. Human behaviors determine health: strategic thoughts on the prevention of chronic non-communicable diseases in China. Int J Behav Med. (2011) 18:295–301. doi: 10.1007/s12529-011-9187-0
7. Pullar J, Allen L, Townsend N, Williams J, Foster C, Roberts N, et al. The impact of poverty reduction and development interventions on non-communicable diseases and their behavioural risk factors in low and lower-middle income countries. a systematic review. PLoS ONE. (2018) 13:e0193378. doi: 10.1371/journal.pone.0193378
8. Na L, Wu X, Feng R, Li J, Han T, Lin L, et al. The harbin cohort study on diet, nutrition and chronic non communicable diseases: study design and baseline characteristics. PLoS ONE. (2015) 10:e0122598. doi: 10.1371/journal.pone.0122598
9. International Diabetes Federation. IDF Diabetes Atlas . 7th Edn. Brussels: International Diabetes Federation (2015).
Google Scholar
10. Kahn SE, Cooper ME, Del PS. Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet. (2014) 383:1068–83. doi: 10.1016/S0140-6736(13)62154-6
11. Aune D, Ursin G, Veierød MB. Meat consumption and the risk of type 2 diabetes: a systematic review and meta-analysis of cohort studies. Diabetologia . (2009) 52:2277–87. doi: 10.1007/s00125-009-1481-x
12. Imamura F, O'Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ . (2015) 351:h3576. doi: 10.1136/bmj.h3576
13. World Health Organization Technical Report Series. Diet, Nutrition and the Prevention of Chronic Diseases . Geneva: WHO (2003). p. 1–149.
14. Fair Society. Healthy Lives: Strategic Review of Health Inequalities in England Post 2010. London, UK: Marmo Review (2010).
15. World Health Organization. Noncommunicable Diseases: Key Facts . (2018). Available online at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
16. Barker DJP. In utero programming of chronic disease. Clin Sci. (1998) 95:115–28. doi: 10.1042/cs0950115
17. Gluckman PD, Hanson MA. Adult disease: echoes of the past. Euro J Endocrin. (2006) 155 (Suppl. 1):S47–50. doi: 10.1530/eje.1.02233
18. Jefferis BJMH, Power C, Hertzman C. Birth weight, childhood socioeconomic environment, and cognitive development in the 1958 British birth cohort study. BMJ . (2002) 325:305. doi: 10.1136/bmj.325.7359.305
19. Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics . (1998) 101 (Suppl. 2):518–25.
PubMed Abstract | Google Scholar
20. Mikkelsen B, Williams J, Rakovac I, Wickramasinghe K, Hennis A, Shin HR, et al. Life course approach to prevention and control of non-communicable diseases. BMJ . (2019). 364:l257. doi: 10.1136/bmj.l257
21. Pechmann C, Levine L, Loughlin S, Leslie F. Impulsive and self-conscious: adolescents' vulnerability to advertising and promotion. J Public Policy Mark . (2005) 24:202–21. doi: 10.1509/jppm.2005.24.2.202
22. World Health Organization (EURO). The Health and Well-Being of Men in the WHO European Region: Better Health Through a Gender Approach . (2018). Available online at: http://www.euro.who.int/en/health-topics/health-determinants/gender/publications/2018/the-health-and-well-being-of-men-in-the-who-european-region-better-health-through-a-gender-approach-2018 (accessed January 13, 2020).
23. World Health Organization. (2016). Good Maternal Nutrition the Best Start in Life . WHO. Available online at: http://www.euro.who.int/__data/assets/pdf_file/0008/313667/Good-maternal-nutrition-The-best-start-in-life.pdf?ua=1 (accessed January 13, 2020).
24. Billingsley M. New advice on physical activity aims to prevent chronic disease from early years. BMJ . (2016) 343:d4457. doi: 10.1136/bmj.d4457
25. Martorell R, Kettel Khan L, Hughes ML, Grummer-Strawn LM. Overweight and obesity in preschool children from developing countries. Int J Obesity . (2000) 24:959–67. doi: 10.1038/sj.ijo.0801264
26. Stein CJ, Colditz GA. Modifiable risk factors of cancer. Br J Cancer . (2004) 90:299–303. doi: 10.1038/sj.bjc.6601509
27. Schultze F, Gao X, Virzonis D, Damiati S, Schneider MR, Kodzius R. Air quality effects on human health and approaches for its assessment through microfluidic chips. Genes . (2017) 8:244. doi: 10.3390/genes8100244
28. Kumar A. The impact of obesity on cardiovascular disease risk factor. Asian J Med Sci . (2019) 10:21294. doi: 10.3126/ajms.v10i1.21294
29. Billingsley HE, Carbone S, Lavie CJ. Dietary fats and chronic noncommunicable diseases. Nutrients . (2018) 10:1385. doi: 10.3390/nu10101385
30. Katileviciute A, Plakys G, Budreviciute A, Onder K, Damiati S, Kodzius RA. Sight to wheat bran: high value-added products. Biomolecules . (2019) 9:887. doi: 10.3390/biom9120887
31. WHO/FAO. Diet, Nutrition and the Prevention of Chronic Diseases. Draft Joint WHO/FAO Consultation on Diet Nutrition and the Prevention of Chronic Disease . (2003). Available online at: https://www.who.int/dietphysicalactivity/publications/trs916/en/ (accessed January 13, 2020).
32. WHO. (2002). The World Health Report 2002 . Geneva: WHO.
33. Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nut Rev . (1997) 55:31–43. doi: 10.1111/j.1753-4887.1997.tb01593.x
34. Popkin BM. Nutrition transition and the global diabetes epidemic. Curr Diab Rep . (2015) 15:64. doi: 10.1007/s11892-015-0631-4
35. The Lancet Global Health. Getting to the heart of non-communicable diseases. (2018) 6:e933. doi: 10.1016/S2214-109X(18)30362-0
36. Marmot M. Social causes of social inequalities in health. In: Anand S, Fabienne P, Sen A, editors. Public Health, Ethics, and Equity . Oxford: Oxford University Press (2004). p. 37–46.
37. Lundberg O, Åberg YM, Stjärne M, Björk L, Fritzell J. The Nordic Experience: Welfare States and Public Health . Stockholm. Centre for Health Equity Studies (2008). Available online at: https://www.chess.su.se/polopoly_fs/1.54170.1321266667!/menu/standard/file/NEWS_Rapport_080819.pdf
38. Yang JS, Mamudu HM, John R. Incorporating a structural approach to reducing the burden of non-communicable diseases. Global Health . (2018) 14:66. doi: 10.1186/s12992-018-0380-7
39. Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol . (2001) 30:668–77. doi: 10.1093/ije/30.4.668
40. Krieger N. COVID-19 Pandemic Highlights Longstanding Health Inequities in U.S . Harvard T.H. Chan School of Public Health (2020). Available online at: https://www.hsph.harvard.edu/news/hsph-in-the-news/covid-19-pandemic-highlights-longstanding-health-inequities-in-u-s/ (accessed August 11, 2020).
41. Blundell HJ, Hine P. Non-communicable diseases: ditch the label and recapture public awareness. Int Health . (2019) 11:5–6. doi: 10.1093/inthealth/ihy063
42. World Health Organization. Noncommunicable Diseases: Key Facts . (2018). Available online at: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed January 22, 2020).
43. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics−2018 update: a report from the american heart association. Circulation . (2018) 137:e67–492. doi: 10.1161/CIR.0000000000000573
44. Popkin BM, Horton SH, Kim S. The Nutrition Transition and Prevention of Diet-Related Diseases in Asia and the Pacific . Washington, DC: International Food Policy Research Institute (IFPRI) (2001).
45. Brands A, Yach D. NMH Reader. Women and the Rapid Rise of Noncommunicable Diseases . World Health Organization (2002). Available online at: https://apps.who.int/iris/bitstream/handle/10665/67256/WHO_NMH_02.01.pdf;jsessionid=92EE99BB43827D58A0DFDCD7A7E5F5AE?sequence=1 (accessed January 22, 2020).
46. Aune D, Norat T, Romundstad P, Vatten LJ. Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur J Epidem. (2013) 28:845–58. doi: 10.1007/s10654-013-9852-5
47. Fung TT, Hu FB, Pereira MA, Liu S, Stampfer MJ, Colditz GA, et al. Whole-grain intake and the risk of type 2 diabetes: a prospective study in men. Amer J Clin Nutr . (2002) 76:535–40. doi: 10.1093/ajcn/76.3.535
48. Centers for Disease Control and Prevention(US) National Center for Chronic Disease Prevention and Health Promotion(US) Office on Smoking and Health(US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General . Atlanta, GA: Centers for Disease Control and Prevention (2010).
49. Joint WHO/FAO. Expert Consultation on Diet, Nutrition and the Prevention of Chronic Diseases . Geneva, Switzerland (2002). Available online at: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed January 22,2020).
50. Willet MC. Diet, nutrition, and avoidable cancer. Environ Health Perspect . (1995) 103:S165–70. doi: 10.1289/ehp.95103s8165
51. Vainio H, Bianchini F. Weight control and physical activity. In: IARC Handbooks of Cancer Prevention . Vol. 6. Lyon: IARC Press (2002).
52. International Agency for Research on Cancer. Cancer: causes, occurrence and control. In: Thomas L, Aitio O, Day NE, Heseltine E, Kadlor J, Miller AB, Parkin DM, Riboli, editors. Lyon, International Agency for Research on Cancer . Lyon: IARC Scientific Publications (1990).
53. Ferlay J. Globocan 2000: Cancer Incidence, Mortality and Prevalence Worldwide. Version 1.0 . Lyon: International Agency for Research on Cancer (2001).
54. Potter J. Food, Nutrition and the Prevention of Cancer: A Global Perspective . Washington, DC: World Cancer Research Fund/American Institute for Cancer Research (1997).
55. Nutritional Aspects of the Development of Cancer. Report of the working group on diet and cancer of the committee on medical aspects of food and nutrition policy. Rep Health Soc Subj . (1998) 48:i–xiv:1–274.
56. Key TJ, Verkasalo PK, Banks E. Epidemiology of breast cancer. Lancet Oncol . (2001) 2:133–40. doi: 10.1016/S1470-2045(00)00254-0
57. Norat T, Lukanova A, Ferrari P, Riboli E. Meat consumption and colorectal cancer risk: a dose–response meta-analysis of epidemiological studies. Int J Cancer . (2002) 98:241–56. doi: 10.1002/ijc.10126
58. Wroblewski LE, Peek RM J, Wilson KT. Helicobacter pylori and gastric cancer: factors that modulate disease risk. Clin Microbio Rev. (2010) 23:713–39. doi: 10.1128/CMR.00011-10
59. Navarro-Torné A, Vidal M, Trzaska DK, Passante L, Crisafulli A, Laang H, et al. Chronic respiratory diseases and lung cancer research: a perspective from the European Union. Eur Resp J . (2015) 46:1270–80. doi: 10.1183/13993003.00395-2015
60. Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global burden of disease study 2015. Lancet . (2016) 388:1459–544. doi: 10.1016/S0140-6736(16)31012-1
61. de-Graft Aikins A, Unwin N, Agyemang C, Allotey P, Campbell C, Arhinful D. Tackling Africa's chronic disease burden: from the local to the global. Global Health. (2010) 6:5. doi: 10.1186/1744-8603-6-5
62. Bousquet J, Dahl R, Khaltaev N. Global alliance against chronic respiratory diseases. Eur Respir J . (2007) 29:233–9. doi: 10.1183/09031936.00138606
63. Leynaert B, Sunyer J, Garcia-Esteban R, Svanes C, Jarvis D, Cerveri I, et al. Gender differences in prevalence, diagnosis and incidence of allergic and non-allergic asthma: a population-based cohort. Thorax . (2012) 67:625–31. doi: 10.1136/thoraxjnl-2011-201249
64. Bellou V, Belbasis L, Tzoulaki I, Evangelou E. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS ONE . (2018) 13:e0194127. doi: 10.1371/journal.pone.0194127
65. Gilmartin AB, Ural SH, Repke JT. Gestational diabetes mellitus. Rev Obstet Gynecol . (2008) 1:129–34.
66. De la Monte SM, Wands JR. Alzheimer's disease is type 3 diabetes-evidence reviewed. J Diabetes Sci Technol . (2008) 2:1101–13. doi: 10.1177/193229680800200619
67. Esposito K, Chiodini P, Maiorino MI, Bellastella G, Panagiotakos D, Giugliano D. Which diet for prevention of type 2 diabetes? a meta-analysis of prospective studies. Endocrine . (2014) 47:107–16. doi: 10.1007/s12020-014-0264-4
68. Johnston E, Mathews T, Aspry K, Aggarwal M, Gianos E. Strategies to fill the gaps in nutrition education for health professionals through continuing medical education. Curr Atheroscler Rep . (2019) 21:13. doi: 10.1007/s11883-019-0775-9
69. Arora M, Chauhan K, John S, Mukhopadhyay A. Multi-sectoral action for addressing social determinants of noncommunicable diseases and mainstreaming health promotion in national health programmes in India. Indian J Commun Med . (2011) 36:S43–9. doi: 10.4103/0970-0218.94708
70. Mutie PM, Giordano GN, Franks PW. Lifestyle precision medicine: the next generation in type 2 diabetes prevention? BMC Med . (2017) 15:171. doi: 10.1186/s12916-017-0938-x
71. Micha R, Khatibzadeh S, Shi P, Andrews KG, Engell RE, Mozaffarian D. Global, regional and national consumption of major food groups in 1990 and 2010: a systematic analysis including 266 country-specific nutrition surveys worldwide. BMJ Open . (2015) 5:e008705. doi: 10.1136/bmjopen-2015-008705
72. Webster J, Pillay A, Suku A, Gohil P, Santos JA, Schultz J, et al. Process evaluation and costing of a multifaceted population-wide intervention to reduce salt consumption in fiji. Nutrients . (2018) 10:155. doi: 10.3390/nu10020155
73. Springmann M, Wiebe K, Mason-D'Croz D, Sulser TB, Rayner M, Scarborough P. Health and nutritional aspects of sustainable diet strategies and their association with environmental impacts: a global modelling analysis with country-level detail. Lancet Planet Health . (2018) 2:e451–61. doi: 10.1016/S2542-5196(18)30206-7
74. Bruins MJ, van Dael P, Eggersdorfer M. The role of nutrients in reducing the risk for noncommunicable diseases during aging. Nutrients . (2019) 11:85. doi: 10.3390/nu11010085
75. USDA. (2020). U.S.D.o.A. Dietary Guidelines and MyPlate . Available online at: https://www.choosemyplate.gov/dietary-guidelines (accessed Feburary 16, 2020).
76. Fletcher RH, Fairfield KM. Vitamins for chronic disease prevention in adults. JAMA . (2002) 287:3127–9. doi: 10.1001/jama.287.23.3127
77. Castiglione D, Platania A, Conti A, Falla M, D'Urso M, Marranzano M. Dietary micronutrient and mineral intake in the mediterranean healthy eating, ageing, and lifestyle (MEAL) study. Antioxidants . (2018) 7:79. doi: 10.3390/antiox7070079
78. Higdon J. An evidence-based approach to vitamins and minerals: health benefits and intake recommendations. United States: Thieme Medical Publishers (2003). 253p.
79. Huskisson E, Maggini S, Ruf M. The role of vitamins and minerals in energy metabolism and well-being. J Int Med Res . (2007) 5:277–89. doi: 10.1177/147323000703500301
80. Damodaran S Parkin KL Fenema OR. Fennema‘s Food Chemistry . Boca Raton, FL: Taylor and Francis Group (2007). 1144p.
81. Wu G. Amino acids: metabolism, functions, and nutrition. Amino Acids . (2009) 37:1–17. doi: 10.1007/s00726-009-0269-0
82. Applegate EA, Grivetti LE. Search for the competitive edge: a history of dietary fads and supplements. J Nutr . (1997) 127:869–73. doi: 10.1093/jn/127.5.869S
83. Helms ER, Aragon AA, Fitschen PJ. Evidence-based recommendations for natural bodybuilding contest preparation: nutrition and supplementation. J Int Soc Sports Nutr . (2014) 11:20. doi: 10.1186/1550-2783-11-20
84. Simopoulos AP. Essential fatty acids in health and chronic disease. Am Clin Nutr . (1999) 70:560–9. doi: 10.1093/ajcn/70.3.560s
85. Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation . (2002) 106:2747–57. doi: 10.1161/01.CIR.0000038493.65177.94
86. Harvey AL. Natural products in drug discovery. Drug Discov Today . (2008) 13:894–901. doi: 10.1016/j.drudis.2008.07.004
87. Dias DA, Urban S, Roessner U. A historical overview of natural products in drug discovery. Metabolites . (2012) 2:303–36. doi: 10.3390/metabo2020303
88. Kaur IP, Chopra K, Saini A. Probiotics: potential pharmaceutical applications. Eur J Pharm Sci . (2002) 15:1–9. doi: 10.1016/S0928-0987(01)00209-3
89. Parvez S, Malik KA, Kang SA, Kim HY. Probiotics and their fermented food products are beneficial for health. J App Microbiol. (2006) 100:1171–85. doi: 10.1111/j.1365-2672.2006.02963.x
90. Curry S, Byers T, Hewitt M. Fulfilling the Potential of Cancer Prevention and Early Detection . Washington DC: National Academy Press (2003).
91. Jhajharia S, Verma S, Kumar R. Risk factors, susceptibility, and machine learning techniques for cancer prediction. Drug Intervent Today . (2018) 10:580–92.
92. Thun MJ, DeLancey JO, Center MM, Jemal A, Ward EM. The global burden of cancer: priorities for prevention. Carcinogenesis . (2010) 31:100–10. doi: 10.1093/carcin/bgp263
93. Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol . (2017) 70:1–25. doi: 10.1016/j.jacc.2017.04.052
94. Rarau P, Pulford J, Gouda H, Phuanukoonon S, Bullen C, Scragg R, et al. Socio-economic status and behavioural and cardiovascular risk factors in Papua New Guinea: a cross-sectional survey. PLoS ONE . (2019) 14:e0211068. doi: 10.1371/journal.pone.0211068
95. Checkley W, Ghannem H, Irazola V, Kimaiyo S, Levitt NS, Miranda JJ, et al. Management of NCD in low- and middle-income countries. Glob Heart . (2014) 9:431–43. doi: 10.1016/j.gheart.2014.11.003
96. International Diabetes Federation. IDF Diabetes Atlas . 7th ed. Brussels: International Diabetes Federation (2015).
97. World Health Organization (WHO). Global Action Plan for the Prevention and Control of NCDs 2013-2020 . (2013). Available online at: https://www.who.int/nmh/events/ncd_action_plan/en/ (accessed January 22, 2020).
98. Lim J, Chan MM, Alsagoff FZ, Ha D. Innovations in non-communicable diseases management in ASEAN: a case series. Glob Health Action . (2014) 7:25110. doi: 10.3402/gha.v7.25110
99. World Health Organization (WHO). Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-resource Settings . (2010). Available online at: https://www.who.int/nmh/publications/essential_ncd_interventions_lr_settings.pdf (accessed January 22,2020).
100. Rogge J. Statement by Dr Jacques Rogge. In: Proceedings of High-level meeting of the UN General Assembly on the Prevention and Control of Non-communicable Diseases, New York, NY: New York (2018).
101. Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet . (2012) 380:219–29. doi: 10.1016/S0140-6736(12)61031-9
102. Phillips CM, Chen LW, Heude B, Bernard JY, Harvey NC, Duijts L, et al. Dietary inflammatory index and non-communicable disease risk: a narrative review. Nutrients . (2019) 11:1873. doi: 10.3390/nu11081873
103. Zarocostas J. Need to increase focus on non-communicable diseases in global health, says WHO. BMJ . (2010) 341:c7065. doi: 10.1136/bmj.c7065
104. Francesco R, Anna L, Stineke O, Victor A, Gunhild S, Ruth R, et al. Transforming the food system to fight non-communicable diseases. BMJ . (2019) 364:l296. doi: 10.1136/bmj.l296
105. Damiati S, Küpcü S, Peacock M, Eilenberger C, Zamzami M, Qadri I, et al. Acoustic and hybrid 3D-Printed electrochemical biosensors for the real-time immunodetection of liver cancer cells (HepG2). Biosens Bioelectron . (2017) 94:500–6. doi: 10.1016/j.bios.2017.03.045
106. Damiati S, Peacock M, Leonhardt S, Baghdadi MA, Damiati L, Becker H, et al. Embedded disposable functionalized electrochemical biosensor with a 3D-printed flow-cell for detection of hepatic oval cells. Genes . (2018) 9:89. doi: 10.3390/genes9020089
107. Damiati S, Hersman C, Søpstad S, Peacock M, Whitley T, Davey P, et al. Sensitivity comparison of macro- and micro-electrochemical biosensors for human chorionic gonadotropin (hCG) biomarker detection. IEEE Access. (2019) 7:94048–58. doi: 10.1109/ACCESS.2019.2928132
108. Matheson GO, Klugl M, Engebretsen L, Bendiksen F, Blair SN, Borjesson M, et al. Prevention and management of noncommunicable disease: the IOC consensus statement, Lausanne 2013. Clin J Sport Med . (2013) 23:419–29. doi: 10.1097/JSM.0000000000000038
Keywords: risk factors, non-communicable diseases, health policy, prevention strategies, healthcare-management
Citation: Budreviciute A, Damiati S, Sabir DK, Onder K, Schuller-Goetzburg P, Plakys G, Katileviciute A, Khoja S and Kodzius R (2020) Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Front. Public Health 8:574111. doi: 10.3389/fpubh.2020.574111
Received: 18 June 2020; Accepted: 26 October 2020; Published: 26 November 2020.
Reviewed by:
Copyright © 2020 Budreviciute, Damiati, Sabir, Onder, Schuller-Goetzburg, Plakys, Katileviciute, Khoja and Kodzius. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rimantas Kodzius, kodzius@envirola.com
† These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ann Glob Health
- v.89(1); 2023
- PMC10655751

Mitigating the Rising Burden of Non-Communicable Diseases through Locally Generated Evidence-Lessons from Tanzania
Harrieth p. ndumwa.
1 Muhimbili University of Health and Allied Sciences, 9 United Nations Road, Upanga West P O Box 65001, Dar es salaam, Tanzania
Davis E. Amani
Jackline e. ngowi, belinda j. njiro, castory munishi, erick a. mboya, doreen mloka, amani i. kikula, emmanuel balandya, paschal ruggajo.
2 Ministry of Health, P O Box 743, Dodoma, Tanzania
Anna T. Kessy
Emilia kitambala, ntuli kapologwe.
3 President’s Office Regional Administration and Local Government, P O Box, 1923 Dodoma, Tanzania
James T. Kengia
James kiologwe, omary ubuguyu, bakari salum, appolinary kamuhabwa, kaushik ramaiya.
4 Tanzania Non-Communicable Diseases Alliance, P O Box 65201, Dar es salaam, Tanzania
5 Tanzania Diabetes Association, P O Box 65201, Dar es salaam, Tanzania
6 Shree Hindu Mandal Hospital, P O Box 581, Dar es salaam, Tanzania
Bruno F. Sunguya
Background:.
The burden of Non-Communicable Diseases (NCDs) is rapidly increasing globally, and low- and middle-income countries (LMICs) bear the brunt of it. Tanzania is no exception. Addressing the rising burden of NCDs in this context calls for renewed efforts and commitment by various stakeholders. This paper highlights local initiatives and strategies to combat NCDs in Tanzania and provides lessons for countries with similar contexts.
We reviewed published and grey literature and conducted policy analysis on NCDs in Tanzania to examine the burden of NCDs and the national response addressing it. The documents included National NCD strategic plans, NCD research agenda, and reports from the World Diabetes Foundation and the World Health Organization. Moreover, a scoping review of ongoing NCD activities and programs in other countries was also conducted to supplement the evidence gathered.
The rising burden of NCDs as a result of the epidemiological transition in Tanzania called for the launching of a dedicated National NCD Control and Prevention Program. The Ministry of Health collaborates with local, national, and international partners on NCD prevention and curative strategies. This led to the development of important guidelines and policies on NCDs, including strengthening the capacity of health facilities and healthcare workers, increased community engagement and awareness of NCDs, and increased advocacy for more resources in NCD initiatives. Strong governmental commitment has been vital; this is demonstrated by a renewed commitment to the fight through national NCD week and related advocacy activities conducted annually. To ensure multi-stakeholders’ engagement and political commitment, all these activities are coordinated at the Prime Minister’s office and provide strong lessons for countries with contexts similar to Tanzania.
Conclusion:
Multi-stakeholders’ engagement, innovative approaches, and coordinated governmental efforts to address NCDs have shone a light on addressing the burden of NCDs and may be sustainable if aligned with locally available resources. Such initiatives are recommended for adoption by other nations to address the burdens of NCDs.
The burden of Non-Communicable Diseases (NCDs) has rapidly increased globally, making NCDs a leading cause of disability, morbidity, and mortality [ 1 ]. They accounted for about 41 million deaths globally—close to three in every four deaths [ 2 ]. About 17 million people die from NCDs at the most productive age, with eight in ten of such deaths occurring in LMICs [ 2 ]. While NCD mortality is declining in high-income countries, the epidemiological transition seems to take a toll on low- and middle-income countries (LMICs), which now harbor 85% of NCD-related deaths [ 2 ]. Diabetes mellitus, cancers, cardiovascular diseases, and chronic respiratory diseases account for about 80% of these deaths [ 3 , 4 ]. The resulting burden is also associated with nutrition, demographic, and economic transitions in LMICs [ 3 ].
Tanzania, like other LMICs, is experiencing the fast-growing burden of NCDs in the context of persistent communicable diseases and a relatively weak health system. The big four NCDs globally (cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes) contribute to about 40% of the NCD burden in Tanzania [ 5 ]. Different from the global picture, the common four risk factors can only explain less than half of the NCD burden in the country, calling for more local evidence and therefore a tailored approach to NCD prevention. The most common conditions in Tanzania, hypertension and diabetes, were prevalent among 25.9% and 9.1% of the population respectively, as found by a recent nationally representative survey [ 6 ]. Other conditions include cardiovascular diseases, cancers, chronic respiratory diseases, oral diseases, mental illnesses and substance abuse, accidents, and injuries [ 7 ]. While about one-third of all deaths are currently due to NCDs, the burden is projected to overtake all communicable diseases combined [ 7 ].
The rapidly growing burden of NCDs in the context of traditionally persistent communicable disease conditions in Tanzania has weakened health systems, drained the available resources, and put tremendous pressure on individual and national economies [ 8 ]. As a result, access to important preventive, curative, and rehabilitative services has remained a struggle, resulting in higher morbidity and mortality rates, particularly among the under-served younger populations who often lack access to quality health services in relation to their actual health needs [ 9 ]. This calls for evidence-based strategies to inform policies, practice, and members of the community to join efforts to address NCDs.
In responding to the increasing NCD burden, the government of Tanzania has strived to strengthen access to quality health services, policies, and strategies informed by local evidence on NCDs. In collaboration with other stakeholders, the government has established and implemented initiatives to curb this unprecedented threat to national development. Through this process, it is important to take stock of milestones, the evolution of strategies, and the implementation of interventions and initiatives aiming to address the burden of NCDs in Tanzania. This will help to inform the progress of the campaign and draw lessons for other countries with a similar context.
Design and context: As a policy paper, this article mainly involved policy analysis and a desk review of both published and grey literature exploring the evidence available on NCD programs and initiatives in Tanzania. These helped to highlight the initiatives and milestones attained since the launch of the NCD Control and Prevention Program in Tanzania, a first in the region, aiming to coordinate national efforts to address the burden of NCDs.
Review process and data abstraction: We reviewed both published and grey literature that have described the burden of NCDs, National NCD program historical milestones, NCD program mandates and activities, and NCD advocacy activities. A thorough review and documentation of the engagement of civil societies and other stakeholders in the fight against NCDs was conducted. Moreover, we reviewed and documented challenges and opportunities facing the execution of set plans and strategies for NCDs in Tanzania. The documents included: the NCD strategic plan 2016–20; the National NCD Research Agenda 2022; reports from civil societies and the World Diabetes Foundation (WDF); and the Ministry of Health’s reports on various NCD activities in the country. Similar reports by the World Health Organization and other regional and international bodies were also reviewed. The team conducted a narrative synthesis of the gathered literature to compile evidence of the progress and lessons learned that can inform the government and other countries with similar contexts.
Ethical consideration: This evaluation did not require ethical approval owing to the nature of the evidence used. The evaluation team consisted of scientists and researchers from the Muhimbili University of Health and Allied Sciences, the Tanzania Diabetes Association, the Ministry of Health, the President’s Office- Regional Administration and Local Government, and other implementing partners.
Patient and public involvement: No patient was involved.
The burden of NCDs in Tanzania
Evidence shows that in Tanzania, NCDs have the highest contribution to the Disability Adjusted Life Years (DALYs) across all age groups, and the magnitude is higher among the older population [ 5 ]. The burden of NCDs has increased remarkedly over the past 30 years in the country. DALYs as a result of NCDs in Tanzania have doubled from 18.28% in 1990 to 36.39% in 2019 [ 10 ].
In accordance with the available nationally representative survey and isolated evidence from locally conducted studies, the most common NCDs in Tanzania are cardiovascular diseases (25.9%), diabetes (9.1%), chronic respiratory diseases (17.5%), and mental health conditions (11%) [ 5 , 6 , 11 ]. NCDs contribute to nearly a third of all deaths in the country [ 7 ]. Cardiovascular conditions (30–40%), cancers (18.6%), COPDs (18.4%), and injuries (17.9%) account for the largest proportion of all mortalities due to NCDs [ 12 ]. The overall rate of mortality from NCDs has increased by 153.3% between the years 2006 and 2015; four in every ten such deaths occurred at regional referral hospitals, and about a third occurred at primary-level facilities [ 12 ]. Evidence estimates the country has about 40,464 new cases of cancer every year [ 13 ]. In terms of burdens, the most common cancers are cervical (25%), breast (10%), prostate (8.8%), and oesophageal (6.5%) [ 13 ]. Late diagnosis and presentation, as well as a limited number of facilities available for cancer management remain a barrier to addressing the burden of cancer in the country. Despite the increase of NCDs, other conditions such as infectious diseases, neonatal and maternal conditions, and nutritional diseases still remain a challenge, so the country experience a double burden of disease [ 10 ].
The burden of NCDs has also financially strained families and societies. Evidence suggests that the prevalence of catastrophic spending and impoverishment is high among households with NCDs [ 14 ]. The odds of households experiencing catastrophic health spending are 52.7% higher when there is a family member with NCD, as compared to households without one [ 14 ]. The burden of NCDs is also straining the health financing system, as evidenced by the reimbursement of the National Health Insurance Funds (NHIF). The Tanzanian NHIF Report in 2022 shows that only three NCD services—namely haemodialysis, chemotherapy, and care and treatment for cardiovascular diseases—accounted for 20% of all the collected funds in 2021.
NCDs account for most hospitalizations, DALYs, and nearly three-quarters of global mortality [ 15 , 16 ]. The Sustainable Development Goals target 3.4 aims to reduce by one-third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being by 2030 [ 17 ]. High-level meetings of the United Nations General Assembly emphasize the role and importance of multi-stakeholders’ engagement in realizing these targets [ 18 ]. The political declaration of the 2011 United Nations High-Level Meeting (UNHLM) on the prevention and control of NCDs recognized the role of civil societies in supporting national efforts geared to address the burden of these diseases. It called for strengthening the coordination of these stakeholders in order to improve effectiveness.
Evolution of the national NCD program
Tanzania promoted the integration of civil societies (CSOs) and other non-governmental organizations (NGOs) to accelerate the development and execution of plans and strategies geared towards address the rising burden of NCDs. The local response to NCDs in Tanzania began more than three decades ago with the activities of the Adult Morbidity and Mortality Projects (AMMP) and others, such as the essential NCD Health Intervention Project ( Figure 1 ) [ 20 ]. The AMMP was established in 1992 by the then-Muhimbili University College of Health Sciences (MUCHS), the Ministry of Health of Tanzania (MoH), and the University of Newcastle in the United Kingdom. The purpose was to conduct a surveillance system that would provide cause-specific death rates in a three-year duration among adults and to link community-based surveillance to evidence-based planning for health care [ 20 ].

NCD program historical milestones in Tanzania.
The Ministry of Health (MoH) in Tanzania, in collaboration with the Tanzania Non-Communicable Diseases Alliance (TANCDA), Tanzania Diabetes Association (TDA), and other stakeholders, pioneered the development of a National Strategic Plan for NCDs and the development of the National NCD Control and Prevention Program. The program is centrally coordinated at MoH and was launched by Hon. Kasim Majaliwa Majaliwa (MP), the Prime Minister of the United Republic of Tanzania in November 2019 [ 19 ]. This marked the official operationalization of the strategy and the implementation of actions against NCDs, coordinated by the Prime Minister’s office to ensure multi-sectoral engagement.
In 2008, the then-Ministry of Health and Social Welfare established the NCD division to help develop policies and monitor progress in response to NCDs and injuries. The division is currently working to strengthen the capacity for both the prevention and management of NCDs and has a functional National Steering Committee for NCDs ( Figure 1 ) [ 21 ]. The first National NCD Strategy for the prevention of NCDs was launched in 2009, covering the period between 2009 and 2015. It was based on the WHO strategic framework and the Global Strategy on diet and physical activities [ 7 ]. This was subsequently followed by the SECOND NCD MULTI-SECTOR STRATEGY AND ACTION PLAN OF 2016–2020, which expanded to include further preventive and rehabilitative services. In November 2016, the national Non-communicable Diseases and Injury (NCDI) poverty committee was established. The committee was focused on priority setting for NCDs in settings of poverty, and it functions as a sub-group of the existing multisectoral NCD group in the Ministry of Health. The third strategic plan was proposed for the period of 2021–2026 through a participatory process guided by the Ministry of Health. From 17 to 18 September 2019, a framework for multisectoral collaboration, consisting of relevant stakeholders, was initiated in Dar es Salaam, Tanzania; it involved more than 100 stakeholders from the government, NGOs, research institutions, religious associations, law institutions, and academia [ 22 ]. The evolution of the Tanzanian National NCD program over the past three decades has each time made improvements that cut across all aspects of NCDs, from prevention, to treatment and rehabilitation. Multi-stakeholder’s engagement has been consistent throughout all phases and has been vital in ensuring that NCDs are addressed in totality, while affordable and quality care is maintained.
NCDs program mandates and activities
The National NCD prevention and control program under the Ministry of Health is the leading implementing body for NCD-related interventions in Tanzania. The program has been working in line with the guidance provided by the National Policies, Sectoral Strategic Plans, the United Nations Political Declaration on the Prevention and Control of NCDs, and the Global Action Plan for the Prevention and Control of NCDs [ 18 , 23 ]. Since its establishment, the aim has been: to support all issues related to governance and coordination; to identify priority areas for intervention and research; resource mobilization; and the coordination of key stakeholders, as well as service provision, especially at district and regional hospitals in the country. However, efforts are being made to ensure that basic services, such as screening for NCDs, are readily available in primary healthcare facilities—which are noted to have limited basic diagnostic equipment and staff trained to treat NCDs [ 24 , 25 ]. Thus, the National NCD prevention and control program has set out different strategies to address NCDs in the country, as described in Table 1 below.
Strategies and approaches to address NCDs in Tanzania.
| STRATEGY | DESCRIPTION |
|---|---|
| Collaboration with local and international stakeholders: the Non-Communicable Diseases Alliance (TANCDA), Tanzania Diabetes Association (TDA), World Health Organization (WHO), Tanzania Cancer Association (TCA), Tanzania Association for Respiratory Diseases (TARD), Heart Foundation of Tanzania (HFT), World Diabetes Foundation (WDF), and institutions such as the Tanzania Food and Nutrition Centre (TFNC), Tanzania Food and Drug Authority (TFDA), and the Tanzania Bureau of Standards (TBS). | |
| Crossing beyond health systems to engaging other sectors, including education, agriculture, communication, employment, energy, environment, finance, food. Also establishing multisectoral committees at different administrative levels, acknowledging that many determinants of NCDs are outside the health sector. | |
| Working with scientists, policy makers, health personnel, and other partners to develop an NCD strategic plan, which is now being relied upon to develop and implement plans and strategies addressing the burden of NCDs in the country. | |
| Advocacy, treatment, and care guidelines for specific diseases, such as sickle cell disease (SCD), hypertension, stroke, and diabetes mellitus have been developed, used for the routine care of patients with NCDs. | |
| The National NCD Research Agenda has been developed, stipulating the research areas of national interest, also serving as an important guide to scientists and potential funders to select priority areas for NCD research. | |
| In collaboration with TDA and TANCDA, the NCD unit has managed to establish over 150 clinics throughout the country, which are all supplied with diagnostic guidelines and the equipment necessary for the management of NCDs. | |
| Hundreds of healthcare workers from Northern Tanzania, the Lake Zone, and other parts of Tanzania have been trained on NCD prevention, diagnosis, and treatment through support from DANIDA and WDF, in collaboration with the civil society organizations. | |
| Campaigns that focus on prevention and fostering good health-seeking behaviors, which will help ensure timely diagnosis and management of NCDs; these campaigns have been conducted through radio, TV sessions and physical seminars. | |
| One hundred thousand school children have been provided with basic knowledge on risk factors for NCDs and have undergone screening for some of the NCDs. | |
| Over six million individuals were reached by outreach screening and sensitization campaigns conducted in the Lake Zone and Northern Tanzania | |
The National NCD research agenda
WHO recommends high-quality research and development to enable evidence-based NCD responses [ 26 ]. However, only a handful studies on NCDs have been conducted in LMICs, and even fewer are from countries with a fast growing burden of NCDs like Tanzania [ 27 ]. In this regard, the National Strategic Plan for NCDs and the National NCD Prevention and Control Program have highlighted research as one of the core elements of the National NCD response. To further underline the importance of research on NCDs, the first National NCD research agenda was developed by the National NCD Prevention and Control Program, involving research and academic institutions in January 2022. The research agenda aligns with the fourth objective of the Sixty-first World Health Assembly, which endorsed the Global Strategy Action Plan for the Prevention and Control of Non-communicable Diseases. Its aim is to “promote research for the prevention and control of non-communicable diseases.” [ 28 , 29 ]. Other countries have also developed and are operationalizing their own NCD research agendas [ 30 ]. The national research agenda for NCDs aims to prioritize areas where the government and implementing partners need evidence for an NCD response. Moreover, it is used by different local and international stakeholders to increase their understanding of Tanzania’s research context and the elements that should be considered for funding and conducting basic health system, clinical, and implementation research.
NCD advocacy activities
The national NCD week in Tanzania was initiated in 2019, along with other NCD initiatives. To date, three NCD week activities have been implemented, one each year covering all regions. In the first year (2019), the national event for NCD week was commemorated in the capital city, Dodoma. This was followed by Dar es Salaam, the business capital with the biggest burden of NCDs in 2020. In 2021, the national commemorations were held in Arusha, the tourism hub of the country. Apart from the active involvement of the government in the advocacy services for NCDs, the private sector and religious bodies have also assumed active roles in raising awareness of NCDs, alerting populations of the NCD services available, in addition to advocating for multi-stakeholders’ involvement. Main recommendations have been physical activities, such as sports and jogging; NCD exhibitions; awareness and education on NCDs; NCD screening and linkage to care; and NCD advocacy in schools and media [ 31 ]. The NCD weeks have been Climax by the National NCD Scientific Conferences, creating a platform for stakeholders to discuss and disseminate local NCD research findings, analyze the NCD situation, and discuss solutions to address the NCD burden in the country. These efforts are in line with the Global Week for Action on NCDs, which was first organized in 2018; this mainly unites the NCD movement each year under a specific theme to combine efforts in reducing the global burden of NCDs [ 32 ].
Analysis of key policy documents
The policy analysis of non-communicable disease (NCD) documents in Tanzania provides a comprehensive overview of the country’s efforts to address the burden of NCDs. The policy analysis in this paper focus on four key policy documents, including the Tanzania Steps Surveys Report (2013), the Strategic and Action Plan for the Prevention and Control of NCDs in Tanzania 2016–2020, the Tanzania Non-Communicable Diseases and Injuries Poverty Commission (2020), and the National NCD Research Agenda (2022).
The Tanzania Steps Surveys Report (2013) [ 6 ] presents data on NCD risk factors, including tobacco use, physical inactivity, an unhealthy diet, alcohol consumption, and also highlights the prevalence of NCD conditions, such as obesity, high blood pressure, and diabetes. It helps to identify high-risk populations and informs targeted interventions for NCD prevention and control.
The Strategic and Action Plan for the Prevention and Control of NCDs in Tanzania 2016–2020 [ 7 ] serves as a roadmap for NCD prevention and control in Tanzania. It outlines strategic goals, objectives, and interventions aimed at reducing the impact of NCDs on the population. The plan emphasizes the importance of multi-sectoral collaboration, health promotion, and community engagement to tackle NCD risk factors and improve healthcare services for those affected by NCDs.
The Tanzania Non-Communicable Diseases and Injuries Poverty Commission (2020) [ 5 ] focuses on addressing the social and economic impacts of non-communicable diseases and injuries (NCDIs). It provides details on the relationship between poverty and NCDIs and proposes strategies to reduce the burden of NCDIs on vulnerable populations. The report documents an assessment of the readiness of the health system to respond to NCDIs in order to further propose cost-effective interventions for priority NCDI conditions. The report also includes a set of proposed priority NCDI interventions and the proposed estimates of the investment required for implementation.
The National NCD Research Agenda (2022) [ 19 ] highlights research priorities related to NCDs in Tanzania. It involves analyzed evidence from local and global research that have conducted situational analysis and hence, developed NCD research themes. These highlight existing gaps to address the burden of NCDs and propose priority research areas. The six key themes highlighted in this research agenda include: the burden of NCDs; risk factors for NCDs; enabling environments; health systems; innovative and implementation research for NCDs; and multisectoral approaches in addressing NCDs and their related comorbidities. The agenda emphasizes the need for evidence-based interventions and the translation of research findings into policy and practice.
Tanzania represents many of the countries in sub-Saharan Africa with an increasingly growing burden of NCDs—attributed to demographic transition characterized by: an ageing population; economic transition characterized by urbanization, sedentary lifestyles, and the changing nature of economic activities; and nutrition transition characterized by unhealthy dietary patterns, low physical activity thresholds, and therefore overweight and obese populations [ 33 ]. The total DALYs due to NCDs in the sub-Saharan African have increased by about 70% between 1990 and 2009 [ 33 ]. While NCDs have remained the leading cause of morbidity and mortality in high-income countries, they are on a slow decline compared to the situation of LMICs [ 34 ]. The burden is rising fast in Tanzania and is projected to overtake the burdens of traditionally prevalent communicable diseases within a decade. Such a burden has already strained the struggling health system, challenging healthcare financing, and subjecting societies, families, and individuals to poverty.
Addressing the impending NCD threat to national development called for strengthened policies and strategic plans in Tanzania. The development of the NCD National Strategic Plans and the NCD Control and Prevention Program under the Ministries of Health is also seen in other countries such as Kenya [ 35 ], India [ 36 ], Norway [ 37 ] and across different WHO regional offices [ 38 ]. A strong collaboration between Ministries of Health, non-governmental organizations (NGOs) and Civil Society Organizations (CSOs) have added value in addressing the burden of NCDs in Tanzania, similar to other countries with stronger health systems and economies [ 39 ]. Moreover, the WHO recognizes the relevance and value of a sustained and strong civil society organization (CSO) voice in bringing solutions to address NCDs and has created the WHO Civil Society Working Group (CSWG) on Noncommunicable Diseases (NCDs) [ 40 ]. This paper has outlined some of the NCDsprograms and activities in Tanzania, along with their corresponding successes, with the main ones being multi-stakeholders’ engagement, development of guidelines and polices, strengthened capacity for HCWs on NCDs, and increased community engagement and awareness of NCDs. Similar initiatives have been carried out in other countries and have also been shown to have an impact towards addressing NCDs. Multi-stakeholder, multisectoral collaboration is considered as a crucial component in the implementation of NCD policies in every country [ 41 ]. Moreover, countries such as South Africa have also established evidence on the multiple roles of healthcare workers, particularly those working in community levels, in responding to the raising burden of NCDs [ 42 ]. In Mozambique, improved training and supervision for healthcare workers has helped in preventing and controlling cardiovascular diseases at primary healthcare levels, hence improving national NCD care delivery [ 43 ]. In the strategy to achieve universal health coverage, primary healthcare for NCDs is also provided among marginalized populations, such as refugees and healthcare workers that have been on the frontline [ 44 ].
Community engagement and participation are reported to be important elements in strengthening preventive measures towards NCD prevention in LMICs [ 45 , 46 ]. In southeastern Nigeria, community engagement has been demonstrated to contribute towards long-term sustainability in improving the management of NCDs [ 47 ]. With the current emphasis on people-centered health care and universal health coverage [ 26 ], the NCD prevention and control program in Tanzania continues to actively engage community health workers, health management teams at district and referral levels, community leaders, schools, the media, and other stakeholders in NCD prevention, health promotion and awareness activities [ 22 ], a practice that is also noted in many other countries [ 35 , 36 , 37 , 39 , 42 , 47 ].
The implementation of NCD program activities in Tanzania still faces several challenges. Financial constraints limit the scope of these activities and thus threaten the sustainability of the gains made. Human resource for health is still the major outcry in Tanzania for both NCD and communicable disease interventions [ 48 ]. This, in addition to limited availability, affordability, and accessibility of other resources, such as diagnostics and drugs, jeopardize the overall quality of healthcare rendered to patients. Low research output denies policy makers and other stakeholders the evidence necessary to develop and revise policies and strategies for NCDs. Moreover, the double burden of diseases due to coexisting communicable diseases, as well as emerging and re-emerging diseases, including COVID-19. poses a threat to effectively address NCDs in the country [ 49 ].
Despite the challenges, a number of opportunities have been realized to address them. A successful establishment of stakeholders’ framework for NCDs provides the NCD Program with an excellent platform to discuss and implement health promotion and prevention services. The unit can also leverage on the framework to seek and introduce innovative financing models for NCDs, which will help address resource limitations that characterize our health systems. To a great extent, the success of HIV/AIDS and TB programs have been aided by the engagement of community health workers and the introduction of community-based promotion, prevention, testing, and treatment programs [ 50 ]. The integration of NCD advocacy strategies into these existing programs could be a game changer, especially now that a lack of resources, particularly skilled human resources, remain a major health system crisis. Collaborating with the Ministry of Education to increase students’ enrollment into health carders and fostering the development and inclusion of NCD-related teaching programs will contribute to decreasing the human resource for health crises. Advancements in science and technology in many parts of the world have been integral in enhancing the response and resilience of healthcare systems [ 51 ]. Tapping into these developments, especially in a transitioning era of disease epidemiology, is necessary to promote risk communication, and to enhance the efficiency and effectiveness of the strategies being undertaken.
Moreover, a brief analysis of key policy documents, including the Tanzania Steps Surveys Report (2013), the Strategic and Action Plan for the Prevention and Control of NCDs in Tanzania 2016–2020, the Tanzania Non-Communicable Diseases and Injuries Poverty Commission (2020), and the National NCD Research Agenda (2022) provided valuable insights into the strategic direction, research priorities, and the challenges of addressing NCDs in Tanzania. The findings contribute to evidence-informed decision making and serve as a foundation for future research and policy development in the field of NCD prevention and control in Tanzania.
The burden of NCDs is growing at an alarming speed in Tanzania, similar to other LMICs. Despite various challenges, through the Ministry of Health, Tanzania has demonstrated outstanding efforts and commitment to address this growing threat. Various programs and activities have been implemented from the community to national level, including the establishment of NCD units under the Ministry of Health, NCD strategic plans, National NCD research agendas, and a number of NCDs advocacy activities. Understanding that multiple and crosscutting efforts are needed to address NCDs, we call for countries with similar contexts (in terms of NCD burden and characteristics) to implement such efforts, in particular establishing and strengthening NCD units within the Ministries of Health to ensure central and effective coordination of NCD activities. Moreover, the realization of stakeholders’ engagement in addressing the raising burden of NCDs has been key in the success of NCD activities. Collaborations with academic institutions and NGOs to build capacity, strengthen, and generate evidence-based research on NCDs, and developing policies and strategies to address NCDs are of paramount importance. In a short while, these efforts have shown a way to successfully address NCDs and are therefore recommended for adaptation by other nations as an approach to join the global response in tackling NCDs.
Acknowledgements
The authors wish to extend sincere gratitude to the Directorate of Research and Publications of the Muhimbili University and Allied Sciences for providing a conducive environment during conceptualization and manuscript writing. Heartfelt appreciation to the Ministry of Health-National NCD prevention and control program and collaborating partners: the Non-Communicable Diseases Alliance (TANCDA), Tanzania Diabetes Association (TDA), World Health Organization (WHO), Tanzania Cancer Association (TCA), Tanzania Association for Respiratory Diseases (TARD), Heart Foundation of Tanzania (HFT), DANIDA and World Diabetes Foundation (WDF). We thank them for their great efforts to support and implement NCD programs and activities in the country.
Competing Interests
The authors have no competing interests to declare.
Author Contributions
All authors had full access to the data used in this article, and they contributed in either conceptualization, development, data analysis, and/or review of this manuscript.
- Open access
- Published: 19 August 2024
Paper-based and mobile application-based self-monitoring tool for healthy dietary intake, development and applicability: a non-randomized trial
- Janaka Godevithana 1 ,
- Champa Jayalakshmie Wijesinghe 1 &
- Millawage Supun Dilara Wijesinghe 2
BMC Digital Health volume 2 , Article number: 53 ( 2024 ) Cite this article
22 Accesses
Metrics details
Unhealthy diet is a key risk factor for Non-Communicable Diseases (NCDs) that contribute to increased morbidity and premature mortality. With increased computer literacy and mobile phone penetration, there is a high opportunity for mobile application-based interventions. The current study was conducted to develop a mobile application to monitor dietary intake and to assess its acceptability and effectiveness in diet control compared to a similar paper-based intervention.
A mobile application was developed based on research evidence and opinions of local experts. The mobile application was introduced to a selected group of office workers who were in preparation, action, and maintenance stages of the Trans Theoretical Model (TTM) and a paper-based intervention was used as the comparator. Socio-demographic data were collected through a self-administered questionnaire. Participants were followed up for three months for adherence. The effectiveness of interventions was assessed at the end of three months by comparing the progressive change in the stage of change and the change from unhealthy to healthy dietary intake between two groups as primary and secondary outcomes respectively.
Among 123 office workers who participated in the study, 19.5% preferred the mobile intervention over the paper-based intervention. Younger, unmarried office workers and those who do not have children, had a higher acceptance for the mobile intervention ( p < 0.05). There was no difference in adherence (in all three months) or outcomes between the two groups of intervention.
Conclusion and recommendations
Mobile application-based interventions are better accepted among the young age group and further studies are recommended to explore their applicability.
Trial registration
The study was registered in the Sri Lankan Clinical Trial Registry (Registration No. SLCTR/2020/025; Date 15th December 2020).
Peer Review reports
Non-communicable diseases (NCDs) have accounted for 73·4% (95% uncertainty interval [UI] 72·5–74·1) of the deaths around the world to become “the number one killer” in the year 2017 [ 1 ] and cardiovascular and cerebrovascular diseases accounted for 16.1% of the total Disability Adjusted Life Years (DALY) in 2016 [ 2 ]. Alarmingly, major contributions to deaths and DALY were from low- and middle-income countries [ 2 ]. Among four key risk factors (smoking, alcohol consumption, unhealthy diet, and physical inactivity) which have repeatedly shown associations with the development of NCDs, an unhealthy or suboptimal diet has a significant and well-established impact on the development of NCDs as well as its complications. It was highlighted that an unhealthy and suboptimal diet accounted for 11 million deaths and 225 million DALY in 2017 [ 3 ]. Similarly, both mortality and DALY burden are higher in the local context. Ischemic heart disease, stroke, and diabetes are the top three contributors to deaths and DALY due to NCDs among Sri Lankans [ 4 ]. Though alcohol and tobacco use were higher only among males (45.7% and 34.8% respectively), unhealthy diet and physical inactivity were prevalent in both males and females [ 5 ].
Even a small change in risk behaviours for developing NCD will result in a significant impact on the health of an individual or a community [ 6 ]. Hence, it is pivotal to work on behaviour changes to reduce the NCD burden. Human behaviour and its change do not occur at random. There are mechanisms of action that bring about a behaviour change. Behaviour change theories generally describe the mechanisms of action (mediators), moderators of behaviour change, and assumptions regarding behaviour change [ 7 ]. There has been a plethora of behaviour change theories that explain human behaviour and have been used in different types of interventions [ 7 ].
TTM is well-known to be effective in interventions for smoking cessation and its effectiveness in interventions for other behaviour changes has been evident in recent studies. It was shown to be effective in changing dietary behaviour, physical activity, and suicide prevention as well [ 8 , 9 ]. With the recent increase of studies aiming at risk factors for chronic non-communicable diseases, TTM has been widely used in interventions aimed at changing dietary behaviour [ 9 ]. Recent reviews based on newer studies conclude that interventions based on TTM have been successful and effective in changing physical activity, dietary behaviour, smoking and opioid addiction prevention, and dental hygiene improvement [ 10 ]. Dietary interventions targeted at reducing dietary fat intake and improving fruit and vegetable consumption or general healthy dietary intake have been successful according to a very recent review of 14 studies based on TTM [ 11 ].
Behaviour Change Techniques (BCT) are the smallest active ingredient of an intervention, and they are designed based on behaviour change theories [ 12 ]. Several systematic reviews and meta-analyses have been conducted to assess the effectiveness of BCT and concluded that goal setting, self-monitoring and providing information through credible sources (subject specialists) were more effective BCTs among various BCTs used in behaviour change interventions [ 12 , 13 , 14 ].
With the advancement and increased usage of mobile phones and devices, health interventions through such devices have come into the picture. Several studies and reviews have claimed the effectiveness of mobile health interventions over conventional health interventions [ 15 , 16 , 17 ]. Usage of BCT within the mobile application and adopting behaviour change theories or models are associated with the overall application quality and functionality of the application [ 17 ]. Further, BCTs such as providing instructions, feedback on behaviour, contingency rewards and the ability for self-monitoring were commonly used in mobile apps for health interventions [ 18 ]. Among BCTs, self-monitoring was more effective through mobile apps than other methods [ 19 , 20 ].
Workforce participation of the population above 15 years of age in Sri Lanka was 52.3% in 2019 which consists of nearly three-fourths of males (73%) and one-third of females (34.1%) [ 21 ]. Around 25% of the workforce is employed in the public sector (government and semi-government) and it is around 1.1 million excluding tri-forces [ 22 ]. When considering the International Classification of Occupations, 57.6% of the Sri Lankan working population is comprised of professionals, technical and associate workers, and clerks [ 22 ]. Most of them perform office-based duties except in the Departments of Health and Education [ 22 ]. Because of the nature of their work, they are less physically active during working hours and are at a higher risk for developing NCDs. At the same time, a study conducted in public sector offices in the Colombo district showed a higher prevalence of NCD risk factors among office workers such as physical inactivity, excessive carbohydrate and sugar intake, high Body Mass Index (BMI) and high waist to hip ratio [ 23 ]. As a group of individuals with similar risk factors gathered in one place and considering the feasibility of implementation, the office setting is an ideal setting for health promotion interventions and it was found to be effective for such interventions [ 24 ].
While Sri Lanka is claiming high mobile phone penetration [ 25 ] with nearly 47% of smartphone usage among the public [ 26 ], more than 70% of office workers have computer literacy and 56% of them are accessing the internet [ 22 ]. Therefore, there is a higher potential for mobile application-based health interventions in office settings and a higher need for intervention for this population considering their high risk of developing NCDs. Before implementing mobile application-based interventions, their acceptance and effectiveness need to be assessed.
Thus, the current study aimed to develop a mobile application for self-monitoring of dietary intake and assess its acceptability and effectiveness in diet control compared to a paper-based diet monitoring tool. It was hypothesized that mobile application-based interventions are more acceptable and effective than paper-based interventions.
The study was conducted in two phases: design and implementation. During the design phase, an extensive literature survey was conducted to identify appropriate theory/ theories for behaviour change and BCTs to incorporate into diet monitoring tools (mobile application and paper-based tool). It was done through search applications including Google Scholar, Medline, PubMed and Mendeley for studies available online and the Post-Graduate Institute of Medicine (PGIM) library repository for theses and dissertations using keywords diet, dietary intake, behaviour change theory, behaviour change interventions and mobile application-based interventions. Following the literate review, experts in behavioural science, nutrition and mobile health interventions were consulted for their opinion on the layout of diet monitoring tools and operationalisation of dietary portions and servings. Combining findings from the literature review and experts’ opinions the layout for diet monitoring tools was formed and the mobile application was discussed with the software development team. Then the mobile application was developed, and further discussions were conducted with experts on the operationalisation of the application. Upon reaching a consensus, the mobile application was pre-tested at a public sector office (Chief Secretariat – Southern province) which was not included in the proper study and piloted at an office in Matara district (Divisional Secretariat – Welipitiya).
Study design
The implementation phase was conducted as a non-randomized pre-and post-intervention study. Two methods of delivering the intervention (mobile application versus paper-based) were compared for acceptance and effectiveness allowing participants to choose the preferred method as an open-label trial.
Study setting
The study was conducted in 10 selected government offices in Galle districts which were the intervention clusters.
Study population
Development officers (DO), Management assistants (MA) and administrative and management officers were selected for the study. Workers who were involved with any physical exertion during their duty and those who were on special dietary plans were excluded from the study.
Sample size and sampling
The study included participants who were in the preparation, action and maintenance stages of TTM. Therefore, a 100% improvement in the proportion of people consuming the recommended number of fruit and vegetable servings (reported by Steps Survey 2016) [ 5 ] was anticipated in the mobile application-based intervention group. An alpha error of 5% and a beta error of 20% were allowed in sample size calculation. As cluster sampling was done, a design effect 1.58 was also incorporated for the sample size. A 10% dropout rate was also incorporated into the study. Assuming 30% and 60% of participants will have recommended fruits and vegetable intake in the paper- and mobile application-based intervention groups respectively, the minimal sample size for one arm was 42. For both arms, it was 84. After correction for design effect and 10% drop-out rate, the ultimate sample size was 147.
Multistage cluster sampling was used to recruit the participants. A cluster was defined as an office with at least 30 clerical-type workers. Clusters were selected purposefully depending on the number of workers and the nature of work in the office. The participants within the clusters were selected randomly, using a series of random numbers. Participants in preparation, action and maintenance stages of TTM from the intervention clusters were selected using their responses to staging questions (Table 1 ).
Data collection tools and data collection
Two-point data collection was conducted at the baseline and after the intervention. Data collection tools were comprised of three parts which included a self-administered (survey) questionnaire, a staging algorithm and 24-h dietary recall. Self-administered (survey) questionnaire was used to assess basic socio-demographic data, general health status, and dietary behaviours (Supplementary file 1 ). The weight and height of participants were measured according to standard procedures described in the European Health Examination Survey (EHES) [ 27 ]. A four-branching question staging algorithm was used to ascertain the stage of change for healthy behaviour change (Table 1 ). 24-h dietary recall by a trained data collector was used for the assessment of dietary intake. It was assisted with a picture guide (Supplementary file 2 ) to determine the unit of measurement and amount of food that a measuring unit will contain, and it was further assisted with computer software (Supplementary file 3 ) to calculate the number of servings taken from each food group. Basic socio-demographic data and general health status data were collected only at the baseline and the assessment of dietary intake and stage of change were done at the baseline and post-intervention as well.
Intervention
A daily serving counter was introduced to participants who are planning to start or already started a dietary behaviour change (preparation, action and maintenance stage as described in TTM).
Mobile application-based intervention (intervention group)
A simple mobile application was developed to mark daily intake of servings by adding the number of servings from each food group described in Food Based Dietary Guidelines (FBDG) for Sri Lankans [ 28 ]. In the main user interface, the serving counter was displayed for each food group (cereal and cereal-based foods, vegetables, fruits, fish meat and pulses, dairy products, nuts and seeds and unhealthy foods). Recommended numbers of servings were indicated in green colour. When exceeding or not meeting the recommended number, the indicator turns red colour indicating unhealthy eating. A serving guide customized to local foods was included as an additional interface and a link to the serving guide was included in the main interface.
Paper-based intervention (comparison group)
A paper-based serving counter with a serving guide was also prepared with the same colour coding for the numbers of servings in each food group.
The principal investigator introduced a serving counter (both paper-based and mobile application-based) to the participants at the beginning of the intervention and they were allowed to choose the type of serving counter they wanted. The marking of the serving counter was assessed monthly to assess the adherence, by inspecting marked papers and observing the summary of marking of the mobile application-based serving counter. The application was configured to record a summary of markings for the last 30 days. If a participant had missed more than two days of marking per any week, it was considered as poor adherence to the serving counter.
The intervention was conducted for three months, and post-intervention assessments of dietary intake and stage of change were conducted at the end of the third month. Progressive (forward) change in stage of change (defined as ‘a change from a lower stage to a higher stage in one or more stages’) was considered as the primary outcome, whereas a change from an unhealthy diet to a healthy diet was considered as the secondary outcome. A healthy diet was defined as ‘adherence to the number of servings recommended in FBDG for Sri Lankans for more than three food groups including cereal and cereal-based foods, fruits, and vegetables, with the consumption of one or no unhealthy food per day’. The participants, whose diet did not meet the definition of a healthy diet were considered as having an unhealthy diet. If such participant changed to have a healthy diet following the intervention, it was considered as a change from an unhealthy to a healthy diet.
Statistical analysis
Sample characteristics were described in relation to socio-demographic, health and work-related factors. Acceptance rate and adherence to the intervention were described using percentages.
All participants were included in the post-intervention analysis considering the initial group irrespective of their adherence, to perform intention-to-treat analysis. However, it was not possible for the monthly adherence assessment for lost to follow-up participants. Therefore, those who had not turned up for the assessment of adherence were categorized as non-adherent participants.
Pre and post-comparison of the stage of change and dietary intake were done within and between the mobile application and paper-based groups using the Mcnemar test and Wilcoxon Signed Rank test to check the statistical significance. Paired t-test and Mann Whitney U test were used to check differences of means and medians respectively, while a probability level of 0.05 was considered as the cut-off for statistical significance. Intention-to-treat analysis was performed and all participants initially selected for either mobile application or paper-based serving counter were included in the post-intervention assessment.
Ethical and administrative clearance
Ethical approval for the study was obtained from the Ethical Review Committee, Faculty of Medicine, University of Ruhuna (Registration No. 2020/P/105) and the trial was registered in the Sri Lanka Clinical Trial Registry (Registration No. SLCTR/2020/025). Administrative approval was obtained from all relevant authorities (District Secretariat-Galle District, Provincial Ministry of Local Government, Regional Director of Health Services-Galle District). Informed written consent was obtained from all office workers prior to data collection. Workers identified with problems were referred to Teaching Hospital Karapitiya, Base Hospital Udugama, Elpitiya or Balapitiya.
The study was conducted while adhering to the World Medical Association Declaration of Helsinki on ethical principles for medical research involving human subjects.
The following themes were highlighted from the literature review. 1. Need for a behavioural theory as the basis for the intervention, 2. A correct mix of BCT is the key to the success of an intervention, 3. Need for an objective way of assessing the stage of change as the primary outcome, 4. Goal setting, self-monitoring and provision of information through credible sources (subject specialists) were more effective BCT, 5. BCTs such as providing instructions, feedback on behaviour, contingency rewards and the ability for self-monitoring were commonly used in mobile apps for health interventions.
Experts pointed out the following opinions after considering the findings from the literature review. 1. TTM is a good theoretical platform for dietary behaviour change interventions, 2. Goal setting, self-monitoring, and feedback on behaviour (through the mobile app) can be incorporated into the intervention. 3. FBDG Sri Lanka is the best available source to define the recommended levels of food intake as servings. 4. A serving guide can be included in the mobile app.
During the pre-testing and piloting, it was suggested to add a minus option for the serving counter and to add common foods (bread, yams etc.) for the serving guide.
One hundred and twenty-three participants in preparation, action and maintenance stages of TTM were invited to have either the mobile application or paper-based intervention and the response rate at baseline was 100%. However, 26 (21.1%) participants were lost to follow-up.
The mean age of the sample was 40 years (SD 8.04 years). A vast majority were educated up to General Certificate of Education (GCE) Advanced Level or higher, the majority were married and most of them were clerical and supportive workers where the category of DOs and MAs belong. Table 2 summarises the socio-demographic characteristics of the study sample.
Acceptance of the intervention
Most of the sample (80.5%) preferred the paper-based intervention, while 19.5% preferred the mobile application. Figure 1 illustrates the flow of participants at different levels of the intervention. Younger age, being unmarried and not having children were associated with acceptance of the mobile application over the paper-based intervention. Table 3 summarizes factors associated with the acceptance of mobile applications as the method of intervention.

Flow chart of the distribution of participants between paper-based and mobile application-based intervention groups
Dietary intake among participants at pre- and post-intervention
The median number of cereal-based food servings consumed was 5.5 at pre-intervention. It was slightly below the recommended range of servings (6 to 7 servings per day). It remained the same even after the intervention. However, there was a significant change in the variance of cereal-based food intake in pre-and post-intervention. There was a statistically significant improvement in the intake of fruits and vegetables from pre- to post-intervention. Fruit and vegetable intake was below the recommended level (5 servings a day), and it has increased to the recommended level following the intervention in both groups. Unhealthy food (defined as food containing only sugar and starch, deep-fried snacks and processed foods) intake was reduced post-intervention compared to pre-intervention state. Table 4 summarises the median number of servings consumed by all participants and participants in mobile and paper-based intervention groups separately at pre- and post-intervention states.
There were only seven (5.6%) participants had a healthy diet at the baseline (pre-intervention), whereas there were 51 (52.6%) participants having a healthy diet at the post-intervention assessment.
Adherence and outcome of the intervention
Adherence to the intervention was higher in all three months (75.6%, 77.2% and 81.3% respectively). Method of intervention (mobile application or paper-based) was not associated significantly with adherence in any month. More than half of the participants (57.9%) have achieved a progressive change in their stage of change and 46.4% of participants have changed towards a healthy diet. However, neither the adherence nor the outcomes showed a significant association with the mode of intervention. Table 5 summarises associations of adherence and outcomes with the mode of intervention.
Most of the sample characteristics were compatible with data from the labour force data except in the gender distribution. The labour force data report has also highlighted that the composition of the workforce will change from sector to sector as well as office to office [ 22 ]. Further, the gender distribution of the current study is compatible with a previous study conducted in an office setup in Sri Lanka [ 23 ].
Acceptance of the mobile application was low (19.5%) among office workers, despite their higher computer literacy (70%) and internet usage (56%). This might be due to the lack of trust in the mobile application and concerns regarding data safety which have been identified as barriers for acceptance of mobile application-based interventions [ 29 ]. Acceptance of mobile applications was associated with younger age, not having children and unmarried status (Table 3 ). This clearly shows that mobile application was more accepted among young workers who have had experience in mobile applications. Studies have highlighted the higher acceptance of mobile apps among the younger population. Research conducted among American adults has shown higher acceptance of nutrition apps at younger ages [ 29 , 30 ]. A systematic review examining seven studies with different age stratifications and age and acceptability correlations has pointed out the association between the acceptability of mobile application-based intervention and younger ages [ 29 ]. Though similar studies were lacking in the local context, digital literacy was higher among the young population and reduced among the older population [ 31 ]. The adherence was not associated with the mode of intervention (paper-based serving counter or mobile application). This can be due to the selection bias as participants were allowed to use the method of intervention they preferred. As they have chosen the mode of intervention that is more comfortable for them, adherence would have been good.
Dietary intake was suboptimal before the intervention with an adequate median intake of cereal-based foods, and a low median intake of vegetables and fruits and a high median intake of unhealthy foods. Following the intervention, the median consumption of vegetables and fruits had increased and consumption of unhealthy foods had reduced among all participants, particularly in the paper-based intervention group. However, favourable change in vegetable and unhealthy food intake was noted among the mobile application-based intervention group as well (Table 4 ).
There was no significant difference in achieving the primary and secondary outcomes between the paper-based and the mobile application-based intervention groups. This indicates that the intervention was effective in changing the stage of change and subsequent change in dietary behaviour. However, the mode of intervention did not affect the effectiveness of the intervention. Though there were hardly any studies assessing the effectiveness of mobile-based intervention purely in changing the stage of change, several systematic reviews and interventional studies (including randomized controlled trials and non-randomized trials) have assessed the effectiveness of mobile application-based interventions in achieving positive dietary behaviour change. They have provided inconclusive evidence on the effectiveness, some claiming the effectiveness of mobile application-based interventions while others concluding that there is no significant improvement in dietary practices following interventions. A recent systematic review has explored the effectiveness of mobile application-based intervention in achieving dietary behaviour changes. It has shown that both randomized and non-randomized trials were effective in achieving dietary behaviour changes [ 32 ]. Another systematic review highlighted the inconclusive evidence [ 33 ] while three studies concluded no significant improvement in dietary intake following mobile application-based interventions [ 34 , 35 , 36 ]. Several randomised controlled trials have reported a reduction in saturated fat [ 37 ] and sugar-sweetened beverages [ 37 , 38 ] intake following interventions. Increased vegetable and fruit consumption was also noted following mobile application-based interventions [ 38 , 39 , 40 ].
Strengths and limitations
The study sample is representative of the entire district, hence generalization of the study findings would be more accurate. The non-randomized experimental trial design contains its inherent drawbacks as the inability to give a clear comparison between two groups.
Mobile application-based intervention was better accepted among the younger generation, and it can be used to achieve behaviour changes. However, the current study was unable to establish a difference between paper-based interventions and mobile application-based interventions in achieving intended outcomes. Further studies are recommended to explore the feasibility and effectiveness of mobile health interventions in dietary behaviour change in more diverse study settings and populations.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the following link, https://drive.google.com/drive/folders/1LQZnbvIT7uoc0AcTsYi52bO-3FM2v2br?usp=sharing with permission from the corresponding author on request.
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1736.
Article Google Scholar
Hay SI, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, et al. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1260.
Afshin A, Sur PJ, Fay KA, Cornaby L, Ferrara G, Salama JS, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;393(10184):1958.
Institute for Health Metrics and Evaluation. Sri Lanka Institute for Health Metrics and Evaluation. 2020. Available from: https://www.healthdata.org/sri-lanka . Cited 2022 Feb 7
Ministry of Health Nutrition and Indigenous Medicine. Non Communicable Disease Risk Factor Survey Sri Lanka 2015. 1st ed. Colombo: Ministry of Health, Nutrition and Indigeneous Medicine; 2017. Available from: https://www.who.int/ncds/surveillance/steps/STEPS-report-2015-Sri-Lanka.pdf
Swann C, Carmona C, Ryan M, Raynor M, Barış E, Dunsdon S, et al. Health systems and health-related behaviour change: a review of primary and secondary evidence. Citeseer. 2010; Available from: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.302.2422&rep=rep1&type=pdf . Cited 2022 Jul 27
Davis R, Campbell R, Hildon Z, Hobbs L, Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev. 2015;9(3):323.
Article PubMed Google Scholar
Coleman MT, Pasternak RH. Effective strategies for behavior change. Prim Care. 2012;39(2):281–305.
Spahn JM, Reeves RS, Keim KS, Laquatra I, Kellogg M, Jortberg B, et al. State of the evidence regarding behavior change theories and strategies in nutrition counseling to facilitate health and food behavior change. J Am Diet Assoc. 2010;110(6):879–91.
Hashemzadeh M, Rahimi A, Zare-Farashbandi F, Alavi-Naeini A, Daei A. Transtheoretical model of health behavioral change: a systematic review. Iran J Nurs Midwifery Res. 2019;24(2):83.
Article PubMed PubMed Central Google Scholar
Nakabayashi J, Melo GRI, Toral N. Transtheoretical model-based nutritional interventions in adolescents: a systematic review. BMC Public Health. 2020;20(1):1543.
Samdal GB, Eide GE, Barth T, Williams G, Meland E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int J Behav Nutr Phys Act. 2017;14(1):42.
Cradock KA, Ólaighin G, Finucane FM, Gainforth HL, Quinlan LR, Ginis KAM. Behaviour change techniques targeting both diet and physical activity in type 2 diabetes: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14(1):18.
Hartmann-Boyce J, Johns DJ, Jebb SA, Aveyard P, Ogden J, Onakpoya I, et al. Effect of behavioural techniques and delivery mode on effectiveness of weight management: systematic review, meta-analysis and meta-regression. Obes Rev. 2014;15(7):598.
Article CAS PubMed PubMed Central Google Scholar
Lee M, Lee H, Kim Y, Kim J, Cho M, Jang J, et al. Mobile application-based health promotion programs: a systematic review of the literature. Int J Environ Res Public Health. 2018;15(12):2838.
DiFilippo KN, Huang WH, Andrade JE, Chapman-Novakofski KM. The use of mobile apps to improve nutrition outcomes: a systematic literature review. J Telemed Telecare. 2015;21(5):243–53.
Schoeppe S, Alley S, Rebar AL, Hayman M, Bray NA, Van Lippevelde W, et al. Apps to improve diet, physical activity and sedentary behaviour in children and adolescents: a review of quality, features and behaviour change techniques. Int J Behav Nutr Phys Act. 2017;14(1):83.
Patel ML, Hopkins CM, Brooks TL, Bennett GG. Comparing self-monitoring strategies for weight loss in a smartphone app: randomized controlled trial. JMIR Mhealth Uhealth. 2019;7(2):e12209.
Lieffers JRL, Hanning RM. Dietary assessment and self-monitoring with nutrition applications for mobile devices. Can J Diet Pract Res. 2012;73(3):e253.
Department of Census, Statistics. labour force data. Department of Census and Statistics, Battaramulla: Department of Census and Statistics; 2020. Available from: http://www.statistics.gov.lk/samplesurvey/LFS_Annual%20Report_2017.pdf
Department of Census, Statistics. Census of Public and Semi Government Sector Employment – 2016. Colombo, Sri Lanka: Department of Census and Statistics, Ministry of National Policies and Economic Affairs; 2016. [cited 2024 Jun 13]. Available from: https://www.statistics.gov.lk/Resource/en/PublicEmployment/census_reports/FinalReport2016.pdf .
Swarnamali AKSH, Jayasinghe MVTN, Katulanda P. Identification of risk factors for selected non communicable diseases among public sector office employees Sri Lanka. Lijhls. 2017;1(2):12–24.
Chandrasiri A, Dissanayake A, De Silva V. Health promotion in workplaces strategy for modification of risk factors for Non Communicable Diseases (NCDs): a practical example from Sri Lanka. Work. 2016;55(2):281–4.
Telecommunication Regulatory Commission of Sri Lanka. Annual Report 2020. Colombo: Telecommunication Regulatory Commission of Sri Lanka; 2021. [cited 2023 May 3]. Available from: https://www.trc.gov.lk/content/files/reports/AR2020_E.pdf .
Perera A, Wattegama Ch. Seven new facts we learnt about mobile and internet use in Sri Lanka. Daily FT. 2019; Available from: https://www.ft.lk/Columnists/Seven-new-facts-we-learnt-about-mobile-and-internet-use-in-Sri-Lanka/4-681306 . Cited 2023 May 3
Tolonen H, editor. EHES Manual. Part B. Fieldwork procedures. 2nd ed. Helsinki: National Institute for Health and Welfare; 2016.
Nutrition Division Ministry of Health. Food Based Dietary guidelines for Sri Lankans. 2nd ed. Ministry of Health; 2011.
Baer NR, Vietzke J, Schenk L. Middle-aged and older adults’ acceptance of mobile nutrition and fitness apps: a systematic mixed studies review. PLoS ONE. 2022;17(12):0e0278879.
Article CAS Google Scholar
Mackert M, Mabry-Flynn A, Champlin S, Donovan EE, Pounders K. Health literacy and health information technology adoption: the potential for a new digital divide. J Med Internet Res. 2016;18(10):e264.
Department of Census and Statistics. Computer Literacy Statistics 2021. Colombo; 2021. Available from: http://www.statistics.gov.lk/ComputerLiteracy/StaticalInformation/Bulletins/2021-Annual . Cited 2023 May 18
Bonvicini L, Pingani I, Venturelli F, Patrignani N, Bassi MC, Broccoli S, et al. Effectiveness of mobile health interventions targeting parents to prevent and treat childhood obesity: systematic review. Prev Med Rep. 2022;29:101940.
Puig EP, Robles N, Saigí-Rubió F, Zamora A, Moharra M, Paluzie G, et al. Assessment of the efficacy, safety, and effectiveness of weight control and obesity management mobile health interventions: systematic review. JMIR Mhealth Uhealth. 2019;7(10):e12612.
Garcia-Ortiz L, Recio-Rodriguez JI, Agudo-Conde C, Patino-Alonso MC, Maderuelo-Fernandez JA, Gento IR, et al. Long-term effectiveness of a smartphone applicationfor improving healthy lifestyles in general population in primary care: randomized controlled trial (evident ii Study). JMIR Mhealth Uhealth. 2018;6(4):e9218.
Svetkey LP, Batch BC, Lin PH, Intille SS, Corsino L, Tyson CC, et al. Cell phone Intervention for You (CITY): A randomized, controlled trial of behavioral weight loss intervention for young adults using mobile technology. Obesity (Silver Spring). 2015;23(11):2133.
Spook J, Paulussen T, Kok G, Van Empelen P. Evaluation of a serious self-regulation game intervention for overweight-related behaviors (“balance it”): a pilot study. J Med Internet Res. 2016;18(9):e225.
Fukuoka Y, Gay CL, Joiner KL, Vittinghoff E. A novel diabetes prevention intervention using a mobile app: a randomized controlled trial with overweight adults at risk. Am J Prev Med. 2015;49(2):223.
Nollen NL, Mayo MS, Carlson SE, Rapoff MA, Goggin KJ, Ellerbeck EF. Mobile technology for obesity prevention a randomized pilot study in racial and ethnic minority girls. Am J Prev Med. 2014;46(4):404.
Quintiliani LM, Mann DM, Puputti M, Quinn E, Bowen DJ. Pilot and feasibility test of a mobile health-supported behavioral counseling intervention for weight management among breast cancer survivors. JMIR Cancer. 2016;2(1):e4.
Mummah S, Robinson TN, Mathur M, Farzinkhou S, Sutton S, Gardner CD. Effect of a mobile applicationintervention on vegetable consumption in overweight adults: a randomized controlled trial. Int J Behav Nutr Phys Act. 2017;14(1):125.
Download references
Acknowledgements
Authors acknowledge the District Secretary-Galle District and the Chief Secretary-Sothern Province for granting administrative approval for the study and all Divisional Secretaries and Heads of local authorities for supporting the project. Dr. Rajith Hathamuna and Mr. Kasun Vithanage are acknowledged for technical support for computer and mobile application creation and operationalization. Dr. Sithara Kulathunga, Dr. Sulekha Peellage and Dr. Isuri Sandunika are acknowledged for their contribution in data collection.
The study has been self-funded by the corresponding author.
Author information
Authors and affiliations.
Department of Community Medicine, Faculty of Medicine, University of Ruhuna, Galle, Sri Lanka
Janaka Godevithana & Champa Jayalakshmie Wijesinghe
Health Promotion Bureau, Ministry of Health, Nutrition and Indigenous Medicine, Colombo, Sri Lanka
Millawage Supun Dilara Wijesinghe
You can also search for this author in PubMed Google Scholar
Contributions
CJW and MSDW provided technical guidance and supervised the research project while JG did the planning the research project, data collection analysis and report writing.
Corresponding author
Correspondence to Janaka Godevithana .
Ethics declarations
Ethics approval and consent to participate.
Authors declare that Ethical approval for the study was obtained from the Ethical Review Committee, Faculty of Medicine, University of Ruhuna (Registration No. 2020/P/105) and the trial was registered in Sri Lanka Clinical Trial Registry (Registration No. SLCTR/2020/025). Administrative approval was obtained by all relevant authorities (District Secretariat Galle District, Provincial Ministry of Local Government, Regional Director of Health Services-Galle District). Informed written consent was obtained from all office workers prior to data collection. Workers identified with problems were referred to Teaching Hospital Karapitiya, Base Hospital Udugama, Elpitiya or Balapitiya Study was conducted while adhering to the World Medical Association Declaration of Helsinki on ethical principles for medical research involving human subjects.
Consent for publication
In the current study consent for publication is not applicable as no individual level data with identification was included in the manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. survey questionnaire., 44247_2024_109_moesm2_esm.pdf.
Additional file 2. Picture guide used to determine portion sizes using household measurements or food portions on a standard plate.
44247_2024_109_MOESM3_ESM.docx
Additional file 3. Microsoft Excel software used to convert household measurements or portion sizes into numbers of servings.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Godevithana, J., Wijesinghe, C.J. & Wijesinghe, M.S.D. Paper-based and mobile application-based self-monitoring tool for healthy dietary intake, development and applicability: a non-randomized trial. BMC Digit Health 2 , 53 (2024). https://doi.org/10.1186/s44247-024-00109-5
Download citation
Received : 10 September 2023
Accepted : 05 June 2024
Published : 19 August 2024
DOI : https://doi.org/10.1186/s44247-024-00109-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Applicability
- Development
- Dietary intake
- Mobile-based dietary interventions
- Self-monitoring
BMC Digital Health
ISSN: 2731-684X
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
COMMENTS
Introduction. Non-communicable diseases (NCDs), also known as chronic diseases, are medical conditions that are associated with long durations and slow progress (Figure 1).Most NCDs are non-infectious and are the result of several factors, including genetic, physiological, behavioral, and environmental factors ().According to the World Health Organization (WHO), NCDs are the leading cause of ...
Historically, communicable diseases, such as HIV/AIDS, viral hepatitis, malaria, poliomyelitis, tuberculosis, influenza and, more recently, the coronavirus disease 2019, have been at the center of global health concerns and initiatives, as they are transmitted from one person to another with a variety of ways, easily spread across national borders, and threaten the lives of millions of people ...
This study aimed to assess the burden of communicable diseases (CDs) and non-communicable diseases (NCDs) globally, regionally, and nationally from 1990 to 2019, and propose global strategies to ...
The paper reviews the magnitude of NCDs in a detailed way. The global epidemic of NCDs offers a challenge to all countries' health systems, while the challenges differ. The burden of disease in India has changed through the years, with a relatively big decline in communicable diseases and an increase in non-communicable disorders (NCDs).
1. Using a life course approach to addressing the continuum of risk and risk modification throughout the lifespan. 2. Prioritizing national prevention and management strategies for multimorbidity ...
Noncommunicable diseases progress monitor 2020 ISBN 978-92-4-000049- (electronic version) ISBN 978-92-4-000140-4 (print version) ... you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO
Addressing non-communicable disease (NCDs) is a global priority in the Sustainable Development Goals, especially for adolescents. However, existing literature on NCD burden, risk factors and determinants, and effective interventions and policies for targeting these diseases in adolescents, is limited. This study develops an evidence-based conceptual framework, and highlights pathways between ...
The spill-over impact of the novel coronavirus-19 pandemic on medical care and disease outcomes in non-communicable diseases: a narrative review. Public Health Rev. 43 , 1604121 (2022).
In this modelling study, we identified NCDs with established infectious risk factors and infectious diseases with long-term non-communicable sequelae, and did narrative reviews between April 11, 2018, and June 10, 2020, to obtain relative risks (RRs) or population attributable fractions (PAFs) from studies quantifying the contribution of infectious causes to NCDs.
The burden of non-communicable diseases (NCDs) continues to increase globally especially in developing countries, with different risk factors contributing to the surge [].This is a result of rapid urbanisation, and westernisation of lifestyle and dietary habits [2,3,4,5,6,7].Low-and middle-income countries (LMICs) are likely to suffer a greater burden of these diseases compared to the ...
Background Non-communicable diseases (NCDs) pose a significant global health challenge, constituting over 80% of mortality and morbidity. This burden is particularly pronounced in low- and middle-income countries (LMICs), including Ethiopia. Despite this, there's limited research on this issue in Africa. This study aims to investigate the prevalence, patterns, and outcomes of NCDs in ...
Introduction. Non-communicable diseases (NCDs) are the leading causes of disease burden worldwide [].According to World Health Organization (WHO) estimates, NCDs are responsible for 71% of all deaths globally, with around 85% of premature deaths from NCDs occurring in low and middle income countries (LMICs) [].Behavioral risk factors including smoking, alcohol consumption, unhealthy diet and ...
Celestin Hategeka and colleagues evaluate the current state of implementation research on Non-Communicable Disease prevention and control ... quasi-experimental evaluation designs (such as pre-post comparison group or time series) were used in 15 papers ... Wigley S, Holmer H. Implementation of non-communicable disease policies from 2015 to ...
In The Lancet, David Watkins and colleagues explore how countries can get back on track to reach the Sustainable Development Goal (SDG) 3.4 target of reducing premature mortality from cancers, cardiovascular diseases, chronic respiratory diseases, and diabetes by a third by 2030. Drawing on the Disease Control Priorities Project and what WHO considers the "best buys", they synthesise the ...
Globally, non-communicable diseases (NCDs) are the leading causes of mortality, accounting for 41 million deaths annually, with 77% of ... of this scientific evidence is based on research and ...
Non communicable diseases (NCDs) contribute to around 5.87 million (60%) of all deaths in India. Hence, the objectives of this paper are to find baseline information on different NCD risk factors coverage and to determine their trends in India. ... Indian council of medical research (ICMR) IDSP non-communicable disease risk factors survey ...
Summary. 1. This paper is for policy makers that are involved in making investments to tackle the main. non-communicable diseases (NCDs), namely cardiova scular disease, cancers, diabetes and ...
Non-communicable diseases contribute to 62% of total deaths in India; of concern are the preventable premature deaths, which account for a staggering 48% of mortality. The objective of this study was to establish a consensus research agenda for non-communicable disease prevention and control that has the potential to impact polices, programmes and healthcare delivery in India.
1.9 Genetics for prevention and control of noncommunicable diseases. Paper 9. Geneva, World Health Organization, 2011. 1.10 Promoting use of research findings to policies and practice for prevention and control of noncommunicable diseases in low- and middle-income countries. Paper 10. Geneva, World Health Organization, 2011. 2.
Introduction. Non-communicable diseases (NCDs), also known as chronic diseases, are medical conditions that are associated with long durations and slow progress ().Most NCDs are non-infectious and are the result of several factors, including genetic, physiological, behavioral, and environmental factors ().According to the World Health Organization (WHO), NCDs are the leading cause of death ...
Paper context. Deaths due to non-communicable diseases are increasing rapidly in South Africa. They are predicated to be the leading cause of death by 2030. There is a significant shortage of data on vital events due to underfunded and incomplete CRVS systems.
Non-communicable diseases (NCDs) have emerged as the major cause of global mortality, increasing from being responsible for 61% of mortality in 2000, to 74% in 2019, and constitute a major public health challenge for the 21st century. 1 The bulk of the global NCD burden is now borne by low-income and middle-income countries (LMICs) undergoing ...
People living with HIV have a high prevalence of NCDs and their risk factors including hypertension, depression, overweight/obesity, hypercholesterolemia, metabolic syndrome and alcohol consumption. We recommend strengthening of health systems to allow for improved integration of NCDs and HIV services in public health facilities in SSA. NCD risk factors such as obesity, hypercholesterolemia ...
The policy analysis in this paper focus on four key policy documents, including the Tanzania Steps Surveys Report (2013), the Strategic and Action Plan for the Prevention and Control of NCDs in Tanzania 2016-2020, the Tanzania Non-Communicable Diseases and Injuries Poverty Commission (2020), and the National NCD Research Agenda (2022).
Unhealthy diet is a key risk factor for Non-Communicable Diseases (NCDs) that contribute to increased morbidity and premature mortality. With increased computer literacy and mobile phone penetration, there is a high opportunity for mobile application-based interventions. The current study was conducted to develop a mobile application to monitor dietary intake and to assess its acceptability ...
In the south Asian region, delivering non-communicable disease (NCD) prevention and control services through existing primary health-care (PHC) facilities is urgently required yet currently challenging. As the first point of contact with the health-care system, PHC offers an ideal window for prevention and continuity of care over the life course, yet the implementation of PHC to address NCDs ...