Why should a healthcare business need a solid business plan

By Jamie Frew on Jun 16, 2024.
Fact Checked by Ericka Pingol.


Starting a healthcare practice
Starting a healthcare business practice can be a bit of a tricky thing, as there are a lot of aspects involved in its operations. Without a business plan, it can get complicated very quickly, so to avoid becoming entrapped in the common pitfalls of healthcare, it’s best to plan out every process and procedure. Making a plan is essential, and quite simply, is part of healthcare startup 101. With techniques such as, you can have more effective preparations in place to face any challenge posed to you, as well as better understand where to make adjustments, improvements, and allocate your resources. With the right plan implemented, you can take off in no time, and work on expanding and prioritizing growth in addition to your client's needs.
Reasons why your healthcare business must have a strong business plan
There are multiple reasons why your healthcare business should have a strong business plan in place, including the following.
To understand your step-by-step strategy for future
A business plan outlines all the resources you need across business operations and can provide a solid backbone to prepare you for potential future challenges. A plan provides a clear direction for all business areas and allows you to know what steps to take in regard to growth and expansion.
To effectively manage your cash flow
Every healthy business needs a positive cash flow to secure investments and ensure there’s enough to be able to supply resources to meet client needs. A business plan can help you avoid breaking even and allow more transparency when it comes to seeing money flows, and can also improve your receivables and payables. Any delays can be accounted for, and when it comes to external financial services, you can appropriately receive reimbursements on time.
To get additional funding for expansion
Continuing with the theme of finances, if successful, you’re likely to face important investment decisions to promote growth and expansion within your business. Sometimes cash flow isn’t enough, and additional funding is needed to accommodate more resources, such as a data warehouse. Having a detailed, and well-outlined business plan can contribute to a higher likelihood of being awarded the right funds to generate higher cash flows through expansion.
To help identify any potential weaknesses
Plans are a great way to outline all your ideas and resources, and presenting information through this clarified format can often highlight areas that you may need to spare additional attention to. Using plans can identify areas of weakness that you may need external support and advice on, and having everything viewable from one place can allow for more valuable discussion.
To communicate your ideas with stakeholders
Businesses are highly concerned with stakeholders and investors, and having a business plan in healthcare serves as a great communication tool for liaison with important institutions. You can use it to hire additional staff, as well as apply for credit and loans for investment purposes. This doesn’t need to be a complicated plan, but if stakeholders are to have a share in your operations, having an outline of your ideas and plans is the least you could do for their peace of mind.
What should your business plan include?
You may be wondering about what needs to be included in a business plan; after all, they can be very detailed, and serve very different purposes depending on your business. Fortunately, we’re here to help, and every business plan should include the following.
Executive summary
Your executive summary should be a concise description of your plan, including summarized details of every core aspect. This may include short descriptions of your market analysis, your value set, as well as finances. Keep in mind that this is a summary, and so it should be written after the plan is fully completed.
Marketing strategy
Your marketing strategy should focus on answering the four Ps of product, price, promotion, and place. You should clearly describe the product or service that you are selling, in addition to the fees you charge. Promotion should outline all the marketing healthcare strategies that you’ll employ, and the place describing where you’ll be located.
Competitive analysis
One of the most important aspects of a plan is considering your competitors, and how your service offers value that differentiates and sets you apart. Ideally, you should discuss your direct competitors and your indirect competitors, or those who target a different market within the same realm of healthcare.
Description of your healthcare practice
Naturally, you should describe your healthcare practice in terms of its operations, mission, and how you’ll run. It should cover all the basics, so all clients and stakeholders who read it can grasp the essentials of what you’re about.
Financial goals
Because investors and lenders will need to see evidence of your financial plans, it’s absolutely vital that you include this aspect. This is one of the most important sections of any business plan, as information such as income and cash flow statements, as well as balance sheets, all need to be included. Profitability should be emphasized at every point, and in regard to a future exit strategy.
Organization and management policies
You should include details concerning your management teams, or any managerial type staff, as well as outlines concerning how you will manage your business data. Data security solutions are important, and so it’s important to make sure that you have considered this in regard to every operation. Investing in healthcare compliance software can help ensure you have the right organizational policies in place.
Customer analysis
Similar to a target market, you need to crack down on the specifics of your service, and what exact demographic you’re catering to.
Healthcare business plan template
To help you get started, we’ve covered all of the basics and compiled it into one business plan for you to follow and implement in your business practice and overcome revenue. For success in your business, consider expanding on the following aspects.
1. Executive Summary
- Business Overview
- Products Served
- Customer Focus
- Success Factors
- Financial Highlights
2. Company Overview
- Who You Are
- Your History
- Your Products/Services
3. Industry Analysis
4. Customer Analysis
- Demograpic profile of target market
- Customer segmentation
5. Competitive Analysis
- Direct and Indirect Competitors
- Competitive Pricing
- Compeitive Advantage
6. Marketing Plan
- Promotions Strategy
7. Operations Plan
- Functional Roles
8. Management Team
- Management Team
- Hiring Plan
9. Financial Plan
- Revenue and Cost Drivers
- Capital Requirements and Use of Funds
- Key Assumptions
Take home message
Every successful healthcare business must implement a business plan to be held accountable and to have a clear direction for the future of its services. Plans can help you have an outline according to your resources and aids in a better understanding of where to allocate your time and energy in improving business operations. You can identify your strengths and weaknesses, and gain a closer relationship with your business procedures and processes to further growth and expansion in the future. Additionally, having a business plan can help you understand your target market, and prioritize client needs. Plans enable you to do what you do best and capitalize on healthcare technology trends to promote growth and learning in the long term.
Get Carepatron for free today and show us your business plan love!

Further reading:
- How to Start a Healthcare Business: The Ultimate Guide
- Four Reasons Why Your Company Must Have A Strong Business Plan At Any Phase
Related Articles

Join 10,000+ teams using Carepatron to be more productive
How to Create a Profitable Healthcare Business Plan for Your Medical Practice

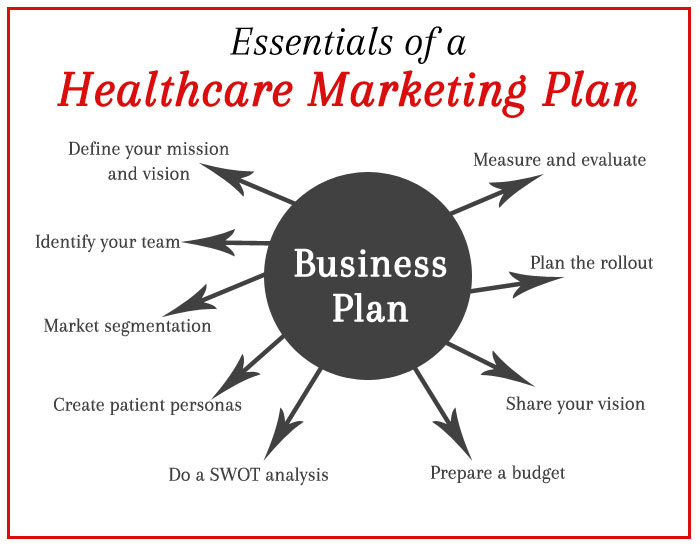
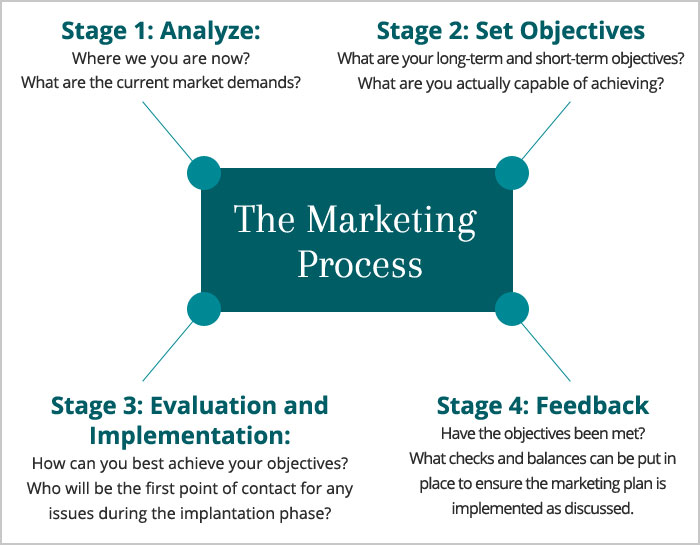
Marketing is crucial for any industry, and healthcare industry is no exception. Whether you are a big hospital or private practice, creating and implementing an effective marketing plan will help to attract new patients, retain the existing ones and maintain relationships with your staff and patients. An effective marketing strategy will play an integral role in increasing revenue, building patient trust, improving online reputation and expanding your reach.
A healthcare business plan can help you define and identify the target audience and key prospects. It can also assist in evaluating and comparing your practice data against your industry. Clearly, a business plan is necessary, so does your practice have one? Here are some more benefits of creating a strategic plan for your medical practice:
- Physician business plan provides clear direction to your marketing initiatives, preventing random activities that may work against each other.
- The process of developing a strategic plan offers an opportunity for everybody involved to collaborate in shaping the future of the practice. Active participation of all the stakeholders ensures the success of projects and priorities.
- A strategic healthcare business plan helps the physician set marketing goals and priorities for the medical practice.
- Clarity of aims and objectives can improve the quality of patient care.
Strategic business planning offers great long-term value. After the initial planning is done, a practice can use it as the benchmark for measuring progress and monitoring areas of improvement.
The process for preparing a strategic business plan is not clear-cut, but it is one of the most important things you should do for the strategic growth of your practice. A well-defined marketing plan will outline how you will retain existing patients and attract new patients, retain staff and communicate your message in the most efficient manner.

You do not need to hire expensive consultants to create a marketing plan for your healthcare practice. All that you need is the willingness to put in time and effort. An ideal healthcare marketing plan should address every aspect related to promoting your practice, and to effectively plan, you must do some research.
Identify your target audience
The first step in any business plan is to figure out who is going to seek your service. If you have a specialty practice, you probably know the answer. According to industry experts, your marketing efforts will be effective only if they are targeted. So to identify your potential patients, start by defining the common characteristics of your current patients. Always remember, your marketing plan is all about reaching your target audience and adjusting your approach to fit their preferences. Beyond demographics, try to learn the reasons why your potential patients will come to your practice, know your competition and understand your competitors’ approach in reaching the target audience. Examine how your competitors market their practice and then compare their approach, services and marketing strategies with yours. You must also determine your unique selling proposition and understand what makes you different from your competition.
Marketing is all about keeping up-to-date. So make sure while doing your research, you stay updated on current affairs. The idea is to keep up-to-date with financial, political and marketing trends that influence the medical community so you can create an effective business plan that responds to changing market conditions.

Time for some brainstorming sessions
After you have identified your potential market and patients, you will need to categorize and address critical operational questions about your medical practice. You may need to set up brainstorming sessions with people you trust, including family, friends, team members or other professionals. During these sessions, try to find answers to these basic but critical questions:
Question: Which marketing platforms will make be most suitable for promoting your services?
Pro tip: You will need to think regarding how to present or sell your services. For instance, consider offering packages that are generic in nature and offer value for money.
Question: What is the best time and frequency of marketing your service?

Pro tip: Too much promotion can create a negative brand image in the minds of potential patients. Too much advertising tends to make patients suspicious. So depending on your target audience, determine the best time for promoting your practice.
Question: What are you trying to achieve from your business plan? How do you plan to measure these goals?
Pro tip: According to experts, your marketing plan should include basic tasks that have short-term goals so that you do not end up compromising on the patient experience. You can consider using big data to evaluate and measure results and their impact on ROI.
Penning the business plan
Now that you have completed the groundwork, it is time to put all your facts and figures into words. Here are some basic steps for creating a business plan for your medical practice:

- Define your mission and vision: This is where you need to determine your goals. You have to understand where you want your practice to be in five to seven years. You will need to prepare a list of all the marketing techniques and tactics and determine what options will work best for your practice. Some of the effective marketing tactics are networking, direct marketing, print advertising, training sessions, media, open houses, social media, blogs, third-party websites and much more.
- Identify your team: In order to build support and generate enthusiasm, you should determine the outgoing personalities in your organization. Find people who will help support your marketing efforts by hosting open houses, patient training sessions, interviews and other public relations initiatives.
- Market segmentation: Consider potential patients think outside the box. Look within your organization first – you may find some of your best customers and marketers there. You must understand where your patients come from and dive deeper into your business model. Is your practice mainly run by physician referrals, or do patients refer directly? You need to create an extensive list of potential patients and categorize them.
- Create patient personas: Patient personas are representations of your ideal patients. You must create patient personas based on your research and reflect on their needs and issues. For instance, if one of your buyer personas is a diabetic, his or her needs will be different from a flu patient.
- SWOT analysis: SWOT matrix is another important component of the business plan. You can use this analysis to assess your practice’s strengths, weaknesses, opportunities and threats. This study will help you understand your market situation better and discover growth opportunities. For a successful SWOT analysis , you must be specific, realistic, compare different situations and keep your business plans and goals updated.
- Prepare a budget: Now that you have all the market information you need and have established the best way to reach your potential patients, focus on your budget to support your marketing campaign. To begin with, it is advisable to stick with the 80/20 rule. According to this rule, 80 percent of your business volume will often come from 20 percent of your patients.
- Share your vision: The first step is to make sure the plan is received and understood by your organization’s leadership. Next, make sure your plan becomes a part of the organizational culture. You must encourage employees to come up with ideas that will support your idea. Always share your plans with physicians, volunteers, employees, board members and top leadership.
- Plan the rollout: To begin with, introduce your campaign internally. Your organization’s leadership and staff are often your best support. If they get the message, your marketing efforts will be successful.
- Measure and evaluate: You should regularly track new patients, physician referrals, leads, website hits and procedure volumes in order to assess the success of your business plan.
Don’t forget the 7Ps
Even the most insightful services, supported by the best business plan, will not survive on the market if they are unable to reach potential patients. That is why practices need to invest in strategies that will bridge the gap between them and the target audience. For your marketing initiatives to be successful, you must address the 7Ps in order to evaluate and measure your business activities. These seven Ps are product, price, promotion, place, packaging, positioning and people. These 7Ps will help you review and define key issues that impact your marketing activities.
- Product: When was the last time you took an unbiased look at your products, service, facility or value proposition? Do your products meet the needs of the patients? Do your products and services deliver value? Is your medical practice properly presented? The ‘product’ for your healthcare practice is the happiness and satisfaction of your patients, which is intangible and cannot be quantified. The only way is to know that customers receive value and comfort by way of your medical practice.
- People: Healthcare is all about people – your current patients, potential patients, staff and management – everyone delivers or receives a service plays a significant part in the product category. Your patients will evaluate the service and satisfaction based on assumptions and interactions. Usually, patients do not have much insight to your medical skills, but they will know if they are pleased based on how you deal with them. Your reputation and your image are not yours alone – it is teamwork.
- Price: It is the amount people pay in exchange for the product received. Therefore, the price must be competitive, enough to generate profit, but may vary when bundled with promotional offers. Sometimes, price is the biggest factor. Therefore, as a practice owner, you must take a serious look at those areas where there is flexibility and be open to adjusting and reducing prices to meet your patients’ needs.
- Promotion: This refers to all the direct and indirect ways of communicating about your product to your people or potential patients. This may include personal and mass interaction. In all instances, promotion should always be carried out in a professional manner. The objective of promoting your practice is to examine how, when, what and where you can offer your service to your target audience.
- Place: This points to presenting your products or services to your target audience in the right place and at the right time. Needless to say, the ‘place’ will be your office where the product will meet the user. However, in healthcare, a change in location can impact the user’s decision to buy.
- Packaging: Take an unbiased look at the appearance of your office, front office, waiting area, brochures and website and the appearance of your medical staff. You might be surprised to see what patients are observing when they walk through your front door.
- Positioning: This refers to the way your brand, products or service are perceived by your target customers. If you could get the opportunity to create the ideal impression in the minds of your patients, what would you want it to be?
For successfully growing their practice and attracting new patients, many practices are working with medical marketing agencies. As a medical marketing agency , Practice Builders knows what is suitable for different medical specialties. We can introduce you to the best marketing tactics that will draw new patients to your practice. Moreover, we know how to develop effective business plans that will lead to significant growth in your medical practice. To find out more, contact us today.
Recent Posts

Sharon Mason Parker
Sharon has spent 25 years building teams and developing people to work together to help improve the client experience in the markets we serve. This ultimately benefits both customers and staff equally. Sharing best practices and ideas helps clients and team members envision new alternatives, which is quite fulfilling when positive change results. Sharon enjoys working closely with clients to understand the true drivers that are affecting their business environment. By engaging clients in meaningful exploration of their goals and challenges, she often discovers that an issue they asked for help in solving is merely a symptom of something else or something greater. Solving the real issue through truly listening and not just addressing the symptoms helps create true partnerships with clients.
Have you Assessed your Practice’s Potential to Acquire more Patients?

Most Popular Posts
- How Medspa Marketing Services Grow Your Medspa Clinic
- Stay Ahead of the Curve with Online Video
- 10 Ways Medical Practices Can Improve Healthcare Access
- How to Respond to Negative Reviews of Your Practice
- How the Right EMR System Can Save Your Practice Money and Time
Thank you for subscribing to our Weekly Tips. We are sure that you will find them very valuable
Mail not sent due to some internal issue. Please try again.
Email already exist. Please try again with diffrent email address.
Animated Modal with Header and Footer
Have you diagnosed your practice health lately, get a complimentary your practice.
Get instant access to detailed competitive research, SWOT analysis, buyer personas, growth opportunities and more for any product or business at the push of a button, so that you can focus more on strategy and execution.
Table of contents, the importance of a well-designed hospital business plan.
- 6 April, 2024
Planning Your Hospital Business
When starting a hospital business, careful planning is essential for long-term success. This section will delve into the importance of annual business plans and the essentials of conducting a market assessment.
Importance of Annual Business Plans
In the ever-evolving healthcare industry, having an annual business plan is crucial for hospital leaders to navigate change and ensure a secure future. Compared to planning at five-year intervals tied to strategic efforts, annual business plans offer greater flexibility and adaptability to the dynamic healthcare environment.
A well-crafted business plan serves as a key tool to achieve financial and operational success in hospitals. It enables growth regionally and prepares hospitals for potential partnerships. By regularly reviewing and updating the business plan, hospitals can stay aligned with their goals and overcome challenges that arise in the healthcare landscape.
Market Assessment Essentials
Conducting a comprehensive market assessment is a crucial step before starting a hospital business plan. This assessment provides invaluable insights into the demographics, patient origin, market share, and competitors in the target area. Understanding these foundational elements is vital for developing a successful hospital business plan.
To conduct a market assessment, hospitals should consider factors such as population demographics, patient needs, and healthcare trends specific to the region. Analyzing the competitive landscape and identifying potential growth opportunities are also essential components of the assessment. By gathering this information, hospitals can better understand the market dynamics and tailor their business strategies accordingly.
By incorporating the findings from the market assessment into the hospital business plan, hospitals can make informed decisions and set realistic goals. This strategic approach allows hospitals to position themselves effectively within the market, anticipate future trends, and meet the needs and expectations of their customers, competitors, regulators, and community.
By recognizing the importance of annual business plans and conducting a thorough market assessment, hospitals can lay a strong foundation for their future success. These strategic planning practices enable hospitals to adapt to the changing healthcare landscape, provide quality care, and achieve their financial and operational objectives.
Crafting a Successful Business Plan
Crafting a well-designed and comprehensive business plan is crucial for the success and sustainability of a hospital. A hospital business plan serves as a roadmap, guiding the development, growth, and operations of the facility. It helps secure funding, attract partnerships, recruit talent, and achieve operational excellence. Let’s explore two key components of a successful hospital business plan: focusing on measurable results and involving stakeholders.
Focus on Measurable Results
A hospital business plan should prioritize measurable results to track progress and ensure accountability. By setting specific and measurable goals, hospitals can track their performance and make informed decisions to drive improvements. The business plan should include a detailed action plan with identified responsible parties, timelines, and specific metrics to track progress. This enables hospital leadership to monitor the effectiveness of their strategies and make adjustments if needed.
Measurable results can encompass various aspects, including financial performance, patient outcomes, operational efficiency, and quality metrics. For example, financial forecasts and projections should be included in the business plan to provide a clear understanding of the hospital’s financial viability and growth potential. These projections should cover revenue, expenses, and profit projections for the initial years of operation. In addition, a SWOT analysis (Strengths, Weaknesses, Opportunities, and Threats) can help identify areas for improvement and competitive advantages within the hospital’s operations. By focusing on measurable results, hospitals can monitor their progress and make data-driven decisions to achieve their goals.
Stakeholder Involvement
Involving key stakeholders in the business planning process is vital for a successful hospital business plan. Stakeholders such as hospital board members, medical staff, and C-suite leaders bring valuable perspectives and expertise to the table. They can provide insights into the hospital’s strategic direction, operational considerations, and community needs. Board representatives, in particular, can offer valuable input during the planning process.
By involving stakeholders, hospitals can foster a sense of ownership and commitment to the business plan. The diverse perspectives and expertise brought by stakeholders can help identify opportunities, address challenges, and ensure that the plan aligns with the hospital’s mission and vision. Collaborative input from stakeholders also enhances the likelihood of successful plan implementation and promotes a shared sense of responsibility for the hospital’s success.
In conclusion, a well-crafted hospital business plan focuses on measurable results and stakeholder involvement. By setting measurable goals and tracking progress, hospitals can make informed decisions and drive improvements. Involving key stakeholders ensures that the plan reflects the hospital’s mission and vision, and benefits from the diverse perspectives and expertise of those involved. A comprehensive and well-executed business plan is a critical tool for hospitals to achieve financial and operational success, enabling growth and sustainability in the ever-evolving healthcare landscape.
Legal Compliance in Healthcare
When it comes to starting and operating a hospital, legal compliance is of utmost importance. Healthcare businesses must adhere to various regulations and implement compliance plans to ensure they operate within the boundaries of the law. In this section, we will discuss the importance of compliance plans and provide an overview of the Stark Law, a crucial legal consideration for healthcare business owners.
Importance of Compliance Plans
Compliance plans play a vital role in the healthcare industry. These plans outline the necessary steps and protocols that healthcare entities must follow to ensure adherence to legal and regulatory requirements. Having a well-designed compliance plan is essential for several reasons:
Avoiding legal troubles : A robust compliance plan helps healthcare businesses identify and address potential legal and regulatory issues proactively. By implementing proper protocols, businesses can minimize the risk of non-compliance and prevent legal complications.
Protecting patients and ensuring quality care : Compliance plans prioritize patient safety and quality care. By following established guidelines, healthcare providers can maintain high standards and ensure that patients receive appropriate and ethical treatment.
Mitigating financial risks : Non-compliance with healthcare regulations can result in severe financial penalties and other consequences. Implementing a compliance plan helps healthcare businesses mitigate financial risks by ensuring adherence to billing and coding requirements and other relevant regulations.
Building trust and reputation : Operating in compliance with healthcare regulations helps build trust with patients, employees, and other stakeholders. It demonstrates a commitment to ethical practices and responsible healthcare management, which can enhance the reputation of the hospital in the community.
To develop a comprehensive compliance plan, healthcare businesses should seek legal assistance from healthcare attorneys who specialize in healthcare regulations and compliance. These attorneys can evaluate the business, identify potential compliance risks, and assist in creating a customized plan tailored to the specific needs of the hospital.
Understanding the Stark Law
The Stark Law is a federal law that prohibits healthcare providers from making referrals for certain designated health services payable by Medicare or Medicaid to entities with which the provider or their immediate family members have a financial relationship. The law aims to prevent potential conflicts of interest and ensure healthcare decisions are based on the best interests of the patients.
Violating the Stark Law can have severe consequences for healthcare business owners. Penalties may include hefty fines, exclusion from Medicare and Medicaid programs, and even potential criminal charges ( Massingill ). It is crucial for hospital owners to familiarize themselves with the Stark Law and take necessary precautions to ensure compliance.
To navigate the complexities of healthcare regulations, healthcare entities, regardless of their size or type of business, need to have a comprehensive medical compliance plan in place and ongoing legal support ( Massingill ). Seeking guidance from experienced healthcare attorneys can help hospital owners understand the intricacies of the law and develop strategies to comply with the Stark Law and other relevant regulations.
In conclusion, legal compliance is a critical aspect of operating a hospital. Implementing a well-designed compliance plan and understanding laws such as the Stark Law are essential for hospital owners to avoid legal troubles, provide quality care, mitigate financial risks, and maintain a trustworthy reputation in the healthcare industry. Seeking legal guidance ensures that healthcare businesses operate within the confines of the law and continue to provide safe and ethical healthcare services.
Healthcare Market Research Insights
In the ever-evolving healthcare landscape, staying informed about health trends and adapting to the needs of patients is crucial for the success of a hospital business. This is where healthcare market research plays a vital role. By conducting thorough market research, hospitals can gain valuable insights into emerging health trends and patient preferences, enabling them to make informed decisions and optimize their healthcare services.
Adapting to Health Trends
Healthcare market research helps identify emerging health trends and patient needs by analyzing data and patient feedback. By understanding evolving health concerns, lifestyle changes, and expectations from healthcare providers, hospitals can adapt their services and treatments to address these trends and meet the changing needs of patients.
For example, market research may reveal a growing demand for alternative therapies or a shift towards holistic healthcare approaches. By recognizing these trends, hospitals can consider incorporating complementary and alternative medicine options or offering wellness programs to cater to the changing preferences of patients.
Furthermore, market research helps pharmaceutical companies develop innovative medications that align with patient expectations. By studying patient demographics, treatment preferences, and unmet medical needs, pharmaceutical companies can design medications that are more effective and better meet patient expectations ( LinkedIn ). This enables hospitals to stay updated with the latest treatment options and provide enhanced healthcare services.
Optimizing Healthcare Services
Market research enables healthcare organizations to optimize their services and operations, ultimately improving the patient experience. By analyzing patient data and feedback, hospitals can make data-driven decisions that enhance healthcare delivery and resource allocation.
For instance, through market research, hospitals can identify areas for improvement in operational efficiency, such as reducing wait times or streamlining administrative processes. By addressing these pain points, hospitals can enhance the overall patient experience and increase patient satisfaction.
Moreover, market research helps assess the adoption rates and preferences of patients and healthcare professionals regarding healthcare technologies. By understanding patient and healthcare provider preferences for telemedicine, wearable devices, and other innovative solutions, hospitals can design and implement technology solutions that seamlessly integrate into the healthcare ecosystem.
By leveraging predictive analytics, healthcare market research can also help hospitals forecast future healthcare needs and challenges. This enables organizations to proactively address issues such as disease outbreaks, resource allocation, and healthcare infrastructure planning. By staying ahead of the curve, hospitals can better prepare for the future and provide high-quality healthcare services to their communities.
In summary, healthcare market research is a valuable tool for hospitals to adapt to health trends and optimize their healthcare services. By staying informed about emerging trends and patient preferences, hospitals can make data-driven decisions, enhance their operations, and provide the best possible care to their patients.
Key Components of a Hospital Business Plan
A hospital business plan is a comprehensive document that outlines the vision, goals, strategies, and financial projections of a hospital. It serves as a roadmap for the development, growth, and sustainability of the hospital. A well-designed hospital business plan is crucial for attracting funding, securing partnerships, recruiting talent, and achieving operational excellence.
Financial Forecasts and Projections
One of the key components of a hospital business plan is the financial plan. This section provides detailed financial forecasts and projections for the hospital, including revenue, expenses, and profit projections for the first few years of operation. These projections help stakeholders assess the financial viability and potential profitability of the hospital. It also enables the hospital to plan its budget, allocate resources, and make informed financial decisions. By presenting realistic and data-driven financial forecasts, a hospital business plan demonstrates the hospital’s financial stability and growth potential.
A typical financial plan includes:
- Revenue Projections: Estimating the sources of revenue, such as patient services, insurance reimbursements, and grants.
- Expense Projections: Anticipating the costs involved in running the hospital, including salaries, supplies, equipment, and facility maintenance.
- Profit and Loss Statement: Summarizing the expected income and expenses to calculate the projected profitability of the hospital.
- Cash Flow Analysis: Assessing the inflow and outflow of cash to ensure sufficient funds are available to meet the hospital’s financial obligations.
- Break-Even Analysis: Determining the point at which the hospital’s revenue equals its expenses, indicating when the hospital will start generating profits.
SWOT Analysis and Strategy
Another crucial component of a hospital business plan is the SWOT analysis. SWOT stands for strengths, weaknesses, opportunities, and threats. Conducting a SWOT analysis allows the hospital to identify and analyze its internal strengths and weaknesses, as well as external opportunities and threats. This analysis helps the hospital adapt to the changing market and environment by capitalizing on its strengths, addressing its weaknesses, leveraging opportunities, and mitigating threats. It enables the hospital to anticipate and respond to the needs and expectations of its customers, competitors, regulators, and the community.
The SWOT analysis is typically followed by the development of a strategy. The strategy outlines the specific actions and initiatives the hospital will undertake to achieve its goals and address the findings of the SWOT analysis. This includes marketing strategies, operational plans, financial strategies, and human resource strategies. The strategy section of a hospital business plan demonstrates the hospital’s ability to navigate challenges, capitalize on opportunities, and differentiate itself in the healthcare industry. It provides a roadmap for success and guides decision-making across all aspects of hospital management ( Quora ).
By including comprehensive financial forecasts and conducting a thorough SWOT analysis with a well-defined strategy, a hospital business plan becomes a powerful tool for guiding the development and success of the hospital. It helps secure funding, attract partners, and ensure the hospital is well-positioned to provide high-quality healthcare services while adapting to the ever-changing healthcare landscape.
Ensuring Effective Staffing in Healthcare
When it comes to running a hospital, ensuring effective staffing is essential to providing quality care and maintaining patient satisfaction. Two key aspects of staffing in healthcare are nursing staffing plans and staffing strategies for optimal care.
Nursing Staffing Plans
A nursing staffing plan is a written document or app used to schedule nurse attendance for every shift in every patient unit. This plan ensures that the right amount of nurses with the right skills are allocated to the appropriate departments. It serves as quality assurance to meet regulatory and safety requirements in healthcare facilities.
The benefits of having a nursing staffing plan are numerous. It helps prevent skills gaps, avoids staffing shortages, and enables effective succession planning. By strategically planning and utilizing existing staff, healthcare facility managers can improve staff supply and efficiency, control recruiting costs, and enhance overall operations.
To create a comprehensive nursing staffing plan, several steps should be followed. These include setting clear business goals, assessing current staffing levels, refining goals for nursing staff, analyzing future staffing needs using ratio analysis and industry-standard rates, and developing a staffing plan by mapping out shifts for at least the next six months ( Dropstat ).
Staffing Strategies for Optimal Care
Effective staffing strategies in healthcare facilities are crucial for ensuring that there is always enough appropriately qualified staff on each shift to provide optimum care. These strategies play a vital role in improving patient outcomes, enhancing nurse-patient relationships, and ultimately elevating the patient experience ( Dropstat ).
When developing staffing strategies, it is essential to consider the unique needs of the hospital and its patient population. The strategies should align with the hospital’s objectives and focus on creating a balanced and skilled workforce. This may involve a combination of hiring permanent staff, utilizing temporary or agency staff, and implementing flexible scheduling options to accommodate peak demand periods.
By adopting effective staffing strategies, hospitals can improve patient care, reduce nurse burnout, and enhance staff satisfaction. These strategies should be continuously evaluated and adjusted based on patient acuity, changes in healthcare regulations, and the evolving needs of the hospital.
In conclusion, effective staffing in healthcare is crucial for delivering quality care and ensuring patient satisfaction. Nursing staffing plans and staffing strategies play a vital role in achieving optimal staffing levels and providing the best possible care. By investing in comprehensive staffing plans and implementing effective strategies, hospitals can enhance their operations, improve patient outcomes, and create a positive work environment for their staff.
Perform Deep Market Research In Seconds
Automate your competitor analysis and get market insights in moments
Create Your Account To Continue!
Automate your competitor analysis and get deep market insights in moments, stay ahead of your competition. discover new ways to unlock 10x growth., just copy and paste any url to instantly access detailed industry insights, swot analysis, buyer personas, sales prospect profiles, growth opportunities, and more for any product or business..

Why Strategic Planning is Important in Healthcare
December 1, 2018
The healthcare industry is sometimes too complex and confusing for most to understand. It’s always changing due to technological advancements or government mandates . It’s becoming more important to plan the success of your healthcare organization. By preparing for the future, your organization can better prepare for the unknown. A strong strategic plan helps all levels of your business, no matter how large or small.
What is Strategic Planning in Healthcare?
Strategic planning in healthcare organizations involves creating objectives and setting goals for where the organization sees itself in the long-term. With these goals and objectives in mind, you can create a plan to achieve them. You can’t just set goals and objectives based on your needs. You also have to set them according to economic trends, government policies, and technological advancements.
Strategic planning in healthcare is critical for healthcare organizations to succeed. Understanding how your organization operates is the key to creating an effective strategic plan for the entire healthcare system to succeed. Sometimes you need to look at the hierarchy of your organization. Determining your company’s goals and setting a path to achieve these goals motivates your staff at every level to succeed with you.

Why Strategic Planning is Important in Healthcare?
Improved communication among all chains.
It’s easy for departments at every level to become confused as to what’s going on. Both your employees and stakeholders want to ensure that your organization will have a long-lasting future. They want to know where your organization is headed and the steps it takes to get there. Effective planning in healthcare management can help you create clarity and improve communication. Your strategic plan should address the key issues, your organization’s vision and goals, and the steps to get there. Your employees and stakeholders will have improved confidence and faith in your organization.
Developing and sharing a vision
With this in mind, you can make an impact on every level of your organization. Employees will be committed and motivated to help achieve your vision. Stakeholders will have the confidence and clarity they need to make sound financial decisions. Strategic planning for healthcare facilities that’s clearly developed, executed, and communicated can help each of your individuals carry out your out vision that can lead to a fulfilling future.
Increased employee motivation and engagement
Each of your employees wants to be recognized and heard. Being recognized by their leaders can greatly impact their productivity, engagement, and safety management. Every employee wants to have the responsibility to make decisions they know will benefit your organization. This also motivates them to perform above the minimum acceptable standards as outlined in the job description or performance evaluation. Employees won’t be motivated to improve themselves for an organization that doesn’t state a clear vision or a well-executed game plan.
Transformational leadership and authority
Transformational leadership is a type of leadership that inspires your employees to work harder and to do better. It incorporates techniques that have been cited in organizational behavior literature. Transformational leaders clearly communicate their organization’s vision, believe in their individual employees, and have the abilities to produce high levels of performance. Helping your employees understand how their roles can contribute your organization’s mission and vision is a crucial part of strategic management.
Increased team cooperation and collaboration
Team collaboration and cooperation is an essential component in delivering high-quality healthcare. Employees must work together to make your organization a success. Teamwork is essential for every healthcare industry in order to improve their performance and service. Effective strategic planning models in healthcare can bring your employees together to deliver quality care, great customer service, and increased performance.
Take the time to work on your strategic plan before sharing it with your employees. A well thought-out and executed strategic plan can increase teamwork, improve performance accountability, and increase employee engagement. With all levels working harmoniously together, you can quickly achieve the long-term goals of your organization.
Writing Business Plans for a Life Science Startup or Clinical Program
Topic Relevance by Timeline
The business plan is an important tool for raising capital, finding strategic partners, recruiting, and providing an internal guide on how to drive a company’s growth.
The plan should include an executive overview, introduction to the management team, market and competitive analyses, value proposition, operating plan, financial projections, and potential risks.
The plan should be concise, well written, and dynamic. Details behind key assumptions should be included.
Common business plan pitfalls include focusing only on the product without framing it in the context of the consumers/patients, the market dynamics, and the ecosystem in which it will be launched, as well as giving financials that are too aggressive and precise given the stage the company is in.
New founders should consider engaging experts to help test assumptions as they develop the key parts of the business plan, including the financial projections.
Many of the same concepts for writing a business plan for a startup apply to creating a business plan for a new clinical program or expanding operations within a health system.
Introduction
Building a life science startup is a long and complex endeavor, and the skills required are very different from the knowledge and training that academic scientists undergo. The process of developing a business plan ensures the team has tested their vision/strategy, and the plan can be used as a roadmap to guide their operations. It also serves as an important communication document when seeking investment in the business. Topics familiar to experienced grant writers—such as the significance, innovation, and approach topics from National Institutes of Health (NIH) grant applications—are relevant and necessary for framing the business plan. The plan also helps to keep the management team accountable, but sage entrepreneurs will recognize that they will often have to revise the original plan over time, based on clinical trial results, regulatory milestones, and market changes. There are several kinds of business plans, generally described as either one-page plans (business model canvas or lean launchpad) and traditional, full-length plans. While one-page business plans are a useful and simple tool for rapid, early iteration, the startup team will ultimately have to write a more detailed plan to secure funding (“ Business Model Canvas ”'; Osterwalder and Pigneur ). In this chapter, we focus on the later and will outline the key elements of a full-length biomedical business plan, highlight the pitfalls to avoid, and provide potential resources for new founders to get their plans started.
It is important to note that developing a sound business plan is also highly relevant for supporting smaller-scale clinical programs, operational investments, and intrapreneurship efforts (see the chapter on " Intrapreneurship: Strategic Approaches for Managing Disruptive Innovation in Your Clinical and Research Projects "). Please see the section at the end of the chapter that outlines the key differences for these types of business plans.
Key Elements of a Business Plan
A) executive s ummary.
The executive summary is a one to four page overview of the existing problem/need in the market and how the new product or service has a unique value proposition that addresses that need (Markowitz) . It is the reader’s first impression of the business, and investors often read only the summary, so it is important for it to be compelling ( Figure 1 ). Consider it a concise but more formal “elevator pitch” that highlights what the company is and why the product or service will win in the market (Cohen) . The remainder of the executive summary should include the short- and long-term goals, key points in the strategic plan, the business model, summary of financial projections, and information about employees and location (Valentin) .
Elements in an Executive Summary.
B) Management team and advisors
This section introduces the management team, their backgrounds, and how their expertise aligns with their particular roles in the business. In addition to the management team, there should be a Scientific Advisory Board (SAB), which helps to guide technology decisions, and a Board of Directors (BoD) which helps to guide all key decisions for the company. SAB and BoD members should be chosen based on their ability to provide industry knowledge and key industry connections that can help the company grow. Having industry experts involved in the company gives assurance—especially to investors—that the technology and operations have been vetted and are supported by those who know the market well.
C) Market Overview
This section should describe the overall landscape of the market, including the size of the market, key segments, historical and expected market growth, and key drivers or trends that may impact the problem the startup is trying to solve.
Market size estimates for life science businesses often include the incidence and prevalence of the disease/condition related to the problem, the estimated medical cost burden—in the U.S. or globally—associated with the condition, and the estimated cost for the consumer/patient with the current available solutions (see the chapter “ Conducting Insightful Market Research ”). It may be useful to describe any relevant preclinical and clinical data that support why this problem exists and highlight the market need. While a large market size is usually viewed positively, it is important that the information provided focus on the market size relevant to the startup’s specific solution. For example, a business plan for an intervention to treat prescription opioid addiction should include details about the global market for opioid drugs, the most recent trends and the expected growth rate of prescribed opioid use and abuse, the morbidity and mortality associated with opioid abuse, and the estimated annual cost for the treatment of opioid abuse and addiction, including the subsequent medical and mental health costs. To demonstrate market size in this example, estimates would include the number of emergency department visits, hospitalizations, intensive care unit admissions, and procedures for overdose or opioid abuse–related complications, as well as the current number, length, and cost of drug rehabilitation admissions.
In terms of the current market, it is useful to describe how the market is divided into customer/patient segments, which may be by geographic region, demographics, psychographic, or customer type (in healthcare, this might be pediatric vs. adult, or inpatient hospital vs. outpatient setting), among others, who are using a certain type of product/service. In the above example of the opioid market, there is segmentation in application (pain relief, anesthesia, cough suppression, diarrhea suppression, or treating addiction) and by geography (North America, Europe, Asia-Pacific, South America, and the Middle East/Africa, which can be further broken down by key countries), which can then be mapped to the types of opioid products with different mechanisms of action (for example, short acting vs. long acting opioids). If the market has clear customer/market segments, there are likely different drivers of demand in each of them, which should be well understood since the startup will want to provide product/service offerings that meet the needs of those segments. Describing the market structure, how this market is segmented, and projected growth rate of target segments will make it easier to determine which segments are the most valuable and to describe how they will be targeted.
As the market data are outlined, it is important to tie back to the product/service offering and how it is uniquely positioned to fulfill the unmet need(s) within the particular target markets (see the chapter “ Identifying Unmet Needs: Problems that Need Solutions ”). Use market research, economic trends, and even patient and provider behaviors, if appropriate, to determine what sector(s) of the market the product fits best. Understand the needs of patients, providers, and hospitals and why the startup’s strategy will meet these needs, in order to better prepare the marketing plan for the product. Moreover, it is important to highlight the attributes of the market that support the offering, such as a large addressable market size, rapid growth in the market segment(s) of interest, and/or the level of competition in these segments. These are dimensions that are critical to stakeholders when they evaluate the business plan.
D) Competitive Landscape
The problem the startup is seeking to solve is one that multiple incumbents are likely already addressing today, either directly or indirectly. This section should provide an overview of the current offerings in the market, where they fall short, and how the new offering fills a current gap in the market. In the above sections, the problem should have been outlined and framed in a way that there would be critical dimensions that matter to stakeholders (patients, physicians, providers, payers). It would be helpful to describe how these competitive offerings compare across these dimensions, which sets up the next section on value proposition.
Understanding the competitors’ product and services, market share, current and past strategies, strengths and weaknesses, the threats they pose to the startup, and the opportunities they make available are integral to a thorough and useful analysis of the competition. This is not just an exercise to learn about other businesses; it will also help identify the strengths and weakness of the startup’s business strategy (see the chapter “ Startup Company Formation and Management ”). Consider developing a basic profile of each of the current direct competitors in the market with these characteristics and include it in the Appendix.
Typical sources of information are company websites and marketing materials (Hisrich et al.) . Academic libraries can also provide a wealth of information through their subscriptions. Other helpful strategies include browsing media outlets for press releases and public relations information, social media, and former customers’ testimonials on how they perceive the competition.
E) Value Proposition
Building off the market need and competitive landscape analysis, the value proposition of the startup’s solution should be articulated in this next section. Against the dimensions that matter to stakeholders, this section of the plan should describe how the new solution will outperform the competition. The value proposition statement is a key way to succinctly demonstrate the measurable benefit that the patient or provider would get from the new product or service, and why patients or health care providers would choose it over existing solutions. Money savings, time, and convenience add to the value of a product. It is important to explain this in a way that can be understood by both scientific and nonscientific audiences. Describe the product/service without revealing too much proprietary information since the business plan may be distributed beyond the intended recipients.
The research results that led to the development of the new product should be shared. This may include pilot data, preclinical/animal model studies, and/or clinical trials, depending on what stage of testing the product has undergone (see the chapter “ Pre-Clinical Animal Models ”). Provide preliminary data and reference specific publications that support the product. In addition, any results of prototype testing should be included.
In the life sciences realm, even if the product solution meets the needs of a patient, ensuring that it fits into the medical ecosystem is imperative. Understanding the infrastructure of a hospital, including the physicians, the administrators, the insurance payers, and whether or not the new offering will improve a patient’s quality of life or improve outcomes such that payers will reimburse the startup for its technology is critical to success. It is also important to articulate (if applicable) whether or not the offering can be dropped into existing treatment algorithms/processes or if changes will need to be made to how work is done to adopt the solution. If a lot of re-training or adjustments around the rest of the ecosystem are required, the value proposition will be more challenging since a lot of changes will need to be made to adopt the solution.
As an update to this chapter, I recommend “The Triple Win Framework” to write a successful value proposition. Here is a quick intro course to using the framework. —
|
|---|
F) Operating Plan
With the market and competitive landscape outlined, and the company’s value proposition defined, this section should describe how the company will execute to capitalize on the opportunity. The operating plan should begin with a thorough explanation of the business model—how the company will work successfully with clients, suppliers, manufacturers, and partners to generate profit. Include here the organizational structure of the company. Next, describe all critical technical, regulatory, and strategic milestones. Finally, outline any functional details about daily execution (Friend and Zehle) .
There are numerous business models, and any one industry may have several examples of successful companies using different approaches. For example, is the company going to adopt an integrator model, where they will build out everything needed to launch the offering, or will they adopt an orchestrator model, where they will partner with people for certain core competencies (e.g., manufacturers) to bring the solution to market? The operating plan should describe the selected model and explain why it is preferable to alternatives. Referencing the leading players highlighted in the competitive landscape section and contrasting against their business models may also be helpful.
Healthcare businesses must deal with reimbursement, fee schedules, billing systems, managed care contracts, and licensing, along with operational issues. The operating plan must address how these challenges will be handled and how the company will get paid, either through insurance reimbursement, by employers, on a fee-for-service basis, or directly by consumer payments. The long sales cycle in most health care businesses is particularly challenging for startups and requires keen long-term planning.
Reimbursement by third-party payers to hospitals and physicians is one of the determinants in whether or not a product will ultimately make it to market, whether it will be used by healthcare providers and patients, and how accessible the product will be. For most technology in healthcare, the payers account for most of the purchasing. Understanding the payers’ reimbursement process, their reimbursement terms, their method for determining the amount to be paid to the provider, and their policy on out-of-pocket cost sharing with the patients is integral as the reimbursement method will impact return on investment for the business (see the chapter “ Reimbursement Strategies and CPT Codes for Device Development ”).
After establishing the business model, it is important to provide an overview of the significant milestones the company foresees. Include any remaining technical development goals, any regulatory approvals the company will face, and other strategic imperatives, such as licenses to related technology, critical partnerships, or protecting intellectual property. Biotechnology and biomedical devices may also need to go through extensive regulatory and legal processes before approval. These processes are outlined elsewhere in this textbook (see the chapter “ FDA Device Regulation: 510(k), PMA ” and, “ FDA Drug Regulation: Investigational New Drug Applications ”).
Each of these milestones should include a description of the task, due date, budget, and responsible person. Due dates and budgets should be ranged since it is difficult to have 100% clarity; milestones function as the management team’s commitment to investors, and the company’s ability to complete these goals will be assessed.
Young businesses should also provide details about the market entry strategy to penetrate the targeted market effectively and to reach revenue and profit expectations. To develop this strategy, engaging with and understanding the ecosystem early on can help improve the design of the new offering and ensure that the solution can be reimbursed. Ideally, during this process one should meet with representatives across the ecosystem to understand what they care about and what the startup will need to deliver in order for them to embrace the new offering.
The technical side of the operating plan should include tactical steps and a timeline for implementing the plan and making the business operational. As a reference point, mention what has been done thus far. Explain how the business will operate, describing the current production process but also the planned process once the company is at scale. Include high-level details about labor, materials, technology, facilities, equipment, manufacturing processes, distribution plan, supply chain, and quality-control measures.
G) Financial Projections
In this section, the team must articulate the financials of the company and show that they have a solid understanding of their expenses, future revenue, and the projected timeline for achieving revenue goals. There will be many assumptions that go into these estimates, so it is important to provide ranges and to explain the assumptions behind the projections. Potential investors will review them to gauge the robustness of an entrepreneur’s understanding of the challenges that lie ahead.
A startup’s financial statements should detail the anticipated financial performance over time (for example: expenses, assets, liabilities, and working capital). Since the financial performance of the startup is dependent on future events (e.g., regulatory approvals or clinical trial partnerships), the financial projections will likely need to be in the format of a ‘pro forma’ budget, which projects future revenues and expenses based on a set of assumptions. Projections of financial statements should go far enough into the future to help readers see where the business can go when it matures or reaches an exit point. Outlined below are the three major parts of the financial plan ( Kolchinsky ; Friend and Zehle ).
The income statement shows the revenue, expenses, and profit for the business over a specific time period. If there are multiple sources of revenue, these may be itemized for future comparisons over time. Early on in the business development, this may be generated monthly and eventually quarterly or annually. An income statement showing earnings before interest, taxes, depreciation, and amortization (EBITDA) acts as a frequent proxy for a cash flow statement.
A statement of cash flow projections shows what the company expects to bring in and how much it will be spending each month. This includes tracking the cash revenues and cash disbursements for the month, and reconciling these two against the opening balance from the previous month. It is important to demonstrate that the startup can adhere to a budget and not overspend consistently. Thus, conservative estimates are preferred; this will increase the level of expenses, but the company should be able to justify why those expenses are needed. Additionally, the statement should show how much working capital the startup needs to pay the bills early on, and how long it will take to have a positive cash flow (bringing in more money than the company is spending). By estimating conservatively, the team can ensure that the company will have enough financial support (i.e., runway) to achieve the milestones without falling short of cash and going bankrupt.
The balance sheet highlights any major working capital requirements and includes assets, liabilities, and equity. Rather than showing trends, the balance sheet reflects these as of a set date.
The additional components of the financial plan detail how the company expects to make money selling the product. These include:
the cost of the product, what factors go into the unit cost, and the plans for bringing these costs down when the company is at scale;
cost estimates for equipment, facilities, inventory, and day-to-day operations, including salaries;
the price the company expects to receive for the product and why it is achievable, especially in the context of reimbursement.
Due to the long process of taking a product to market in healthcare businesses, there should be a section in the financial plan about the capital required for the various regulatory milestones. As outlined in the operating plan, all product development, technical, and regulatory milestones would come with an estimated budget and timeframe for completion. Included in this is the cost of the Food and Drug Administration’s drug review process—a major consideration in the financial projections for life science startups. From preclinical research to the Investigational New Drug application, to clinical trials, to the New Drug Application submission and review, this process is expensive and takes many years to complete. How far along a product is in this process will factor greatly into how much money will be necessary to complete Phase 1, 2, and/or 3 trials, as well as the subsequent regulatory requirements.
Clinical trials can incur substantial costs beyond distributing the study drug/device and the associated study procedures. Site costs, fees for storage, technology solutions, and safety monitoring, core lab fees, and study staff salaries—for scientists, physicians, project managers, data managers, research coordinators, biostatisticians, and site management, including regulatory visits and investigator meetings—all must be budgeted into the cost of each phase, and the timeline to complete the data collection should be considered. In addition, up to 30% of any grant funding may need to go toward administrative overhead to carry out the study, if implemented at an academic medical center. In some cases, academic entrepreneurs can establish sponsored research agreements that allow components of the preclinical or clinical research to occur at their university (see chapters on “Post Alliance Agreements and Sponsored Research Agreements” and “ Understanding Conflict of Interest for Academic Entrepreneurs ”). As mentioned earlier, many of these projections may be pro forma because they will rely on the achievement of other milestones prior to implementation.
H) Risks/Anticipated Problems
All business plans should include a section on anticipated risks/problems and potential alternative strategies. This can demonstrate to investors that the entrepreneur has thought through potential challenges and has plans to either prevent them from occurring, or backup plans to mitigate the consequences. Generally speaking, a balanced approach is helpful here—not hiding or obfuscating major challenges, especially those that have befallen other companies, but at the same time not overwhelming the reader with negativity. At the very least, this can be a thought exercise for the startup and may identify issues that had not previously been considered. While a business plan is not a legal document or binding contract, intentional distortion of facts can come back to haunt a company.
Business Plans for Clinical or Operational Programs
There will be many situations where an idea is not yet at the stage of becoming a company, but requires investment to drive growth or sustain operations. Examples include developing a new clinical program or service (e.g., a novel surveillance protocol postsurgical intervention that will result in diagnostic testing revenue) or expanding operations (e.g., building a new facility to treat patients who have an eating disorder). These situations also call for business plans in order to garner support and investment—in this case, the investment would be coming internally from the health system or institution rather than outside investors.
The key components of these business plans are executive summary, background, proposal description, market and competitive analyses, operating plan, metrics for success, financial projections, and potential risks. Many of the same concepts from earlier apply, but the key differences include: 1) the business plan should specify the dollar amount of the resources needed to make the plan operational; and 2) the proposal description, operating plan, financial projections, and risks should take into account the impact of the plan on the existing operations of the system.
As mentioned earlier, most health systems will have internal strategy and finance teams, which are helpful resources for developing business plans and should be consulted early on to help with the financial projections as well as the anticipated system impacts of the plan. The remainder of this section outlines each part of the business plan and focuses on the key differences from a startup business plan.
Executive summary: In addition to the points covered in the startup executive summary, the executive summary for a new program/service/facility should include the “ask”—what resources (e.g., capital, new full-time employees, or other operating expenses) are being requested to support the new program. The executive summary should also state the expected financial return on the investment from the perspective of the institution (usually in terms of annual steady-state contribution margin or total incremental contribution margin over a period of time, usually seven years).
Background: This section should describe the current state of operations. If the authors are proposing a new clinical program, for example, they should describe the patient population being addressed, how they are currently being served, and the current volumes. It should also describe the limitations of the current state, the unmet need, and what factors necessitate a new solution.
Proposal description: The authors should describe what new program/service/facility is being proposed, and how it addresses the current challenges. This section should also describe how the proposal will lead to growth—will the program reach a new patient population not previously served? Have a greater geographic reach? Result in greater utilization of other services at the institution? This is also an appropriate place to describe other benefits of the plan, including improved quality, safety, patient experience, efficient resource utilization, etc. It is important for this section to align with the institution’s priorities.
Market and competitive analyses: This section should look very much the same as described above in the startup business plan.
Operating plan: This section should build on the proposal description and go into more technical detail. Details should include how the program will be staffed, what type of services will be delivered, where they will be delivered, hours of operation, pricing and reimbursement, and what the impact will be on downstream services and the rest of the institution. Thus, it requires a detailed understanding of how the institution currently operates, so the new proposal can realistically be integrated without excessive disruptions to operant workflow.
Metrics for success: The authors should list two–three measurable metrics that will show the success of the program. These can include volume, financial, patient/staff satisfaction, or other related metrics. Ideally, there should be targets for each metric (e.g., “increase volume by 10% above baseline by year 3”). For plans where measurable impact will not be realized until several years out, milestone-based targets are also acceptable as near-term goals (e.g., “achieve regulatory approval by X date”). It is preferable that these metrics be ones that the institution already monitors, thus enhancing alignment with current priorities and facilitating the ability to add this new project. In some cases, though, it may be necessary to develop new metrics, which should be done in consultation with the institution’s leadership.
Financial projections: This section should include all components outlined above, with the exception of a balance sheet, since the plan is only describing a subset of operations within a larger system. For the pro forma income statement, it is useful to show multiple views: a base case view (if applicable), which shows current operations of the program/facility; an incremental view, which just shows the incremental revenue and expenses associated with the proposed plan; and a strategic view, which is the addition of the base case and incremental. It is also highly recommended to have a separate section outlining the assumptions used to develop the financial projections (e.g., data source, patient population, growth projections, operational start date and ramp-up speed). As these business plans are usually in the context of a large academic institution, it is helpful for planning purposes for the financial statements to specify the organizational entity to which the projected revenues and expenses will accrue (e.g., Hospital vs. Practice Plan vs. Research).
Risks and mitigation: This section should look very much the same as described above in the startup business plan. In addition, the plan should consider potential risks/negative impacts to other parts of the institution. For example, if the plan proposes to build a new facility in a suburban location, will it potentially cannibalize volume from the main location, and if so, what is the plan to mitigate revenue loss?
The same tips on business plan writing apply here. Since clinical and operational programs need to function within the environment of an existing system, socializing the plan early and often is especially critical for gaining support, both for funding the plan and for implementing it. In some cases, this may involve obtaining regulatory approval from internal institutional entities, such as the institutional review board (IRB), legal counsel, or information services (especially if information protected under the Health Insurance Portability and Accountability Act (HIPAA) is involved). Factoring time for these approvals is crucial.
External Resources
In academic entrepreneurship, there are a host of extra challenges that must be considered, including who owns the intellectual property, technology transfer agreements, regulatory procedures, and conflict of interest, among others (Kolchinsky) . At the same time, being part of an academic institution provides many resources not available to non-academic entrepreneurs, including business planning, legal, and funding support. Networking and taking advantage of other schools within the academic system who have experts in these fields will improve the entrepreneur’s knowledge, especially when entrepreneurship is not one’s first career or when this is one’s first experience with developing a product. This can be particularly valuable when estimating costs related to preclinical and clinical research. Many academic centers have clinical research offices that have pre-populated budget templates, which can help to ensure that all aspects of the clinical trial are adequately budgeted. Most academic systems also have corporate Strategy and Finance teams that can help with business analyses as well, such as market/competitive dynamics and projecting future demand (whether that be in terms of patient volume, demand for the product, etc.). In addition, university libraries may provide online access to publications and market research related to the product and the industry. For specific tasks, such as preparing an exit strategy that involves an initial public offering (IPO), extensive external legal and financial consultations are generally required.
Tips on Business Plan Writing
Remember that a business plan is dynamic, changing with the growth of the company and as the company pivots due to unexpected challenges or market trends. The plan should be comprehensive, and key points, data, and strategies should be consistent throughout. Be mindful of including important details without going into excessive minutiae. Lastly, this is a professional document, and it can be the first and lasting impression of the company on potential investors, so appearance matters. To this end, recruit trusted editorial support to make sure the plan is consistent from beginning to end and to check for correct spelling, grammar, and formatting.
Writing a business plan is a process. It requires brainstorming, researching, prewriting, drafting, revising, and editing. The business plan is not only an internal company tool for thinking about the future, it is also about presenting the company’s idea, solution, marketing strategy, financial projections, and long-term vision to prospective investors. It is an introspective exercise that each executive team should utilize to help identify misconceptions before they become costly, to organize and streamline team members’ efforts, to focus on the big picture rather than getting caught up in short-term actions, and to establish performance standards for the company (Valentin) . It is important that all key stakeholders participate in the development and writing of the business plan. As the money at risk increases, the benefits of having a well-developed business plan increase as well.
U.S. Small Business Administration .
BPlans , produced by Palo Alto Software, is a free resource for new entrepreneurs with tools, webinars, and templates for writing a business plan.
Business Plan for Scientists .
Business Plans Handbook : Craft, D. Business Plans Handbook, vol. 42, pp. vii–viii. Gale, 2018. Gale Virtual Reference Library .
The contents of this chapter represent the opinions of the chapter authors and editors. The contents should not be construed as legal advice. The contents do not necessarily represent the official views of any affiliated organizations, partner organizations, or sponsors. For programs or organizations mentioned in this chapter, the authors encourage the reader to directly contact the relevant organization for additional information.
Great article, thank you!
Thanks, that's exactly what I was looking for! I read an article about tech company business plan , everything is quite detailed. But I needed a narrower specialty. Your post is just right!
Author Linda Miller and her colleague Brendon Ardietta recently conducted a CHOP workshop on articulating your idea as a “triple win” in healthcare: value for patients, clinicians/researchers, and financers (e.g. CHOP, grant funders, VCs). See video and handouts

- Content Index
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Successful business planning for new programs in health care organizations
Affiliation.
- 1 University of Florida.
- PMID: 10111952
- DOI: 10.1177/016327879101400104
Health care organizations implement business strategies through programs and services, and success depends on careful program design and execution. A conscientious design requires thorough efforts in organizing the planning process, conducting the decision analysis, and obtaining approval for a program. Weak methods and processes in the management of these efforts can result in faulty assumptions and costly errors in the development of new health care ventures, thus preventing the achievement of financial and operating goals. This article reviews the stages of business planning, and the points at which success may be impaired.
PubMed Disclaimer
Similar articles
- Critical care medicine as a distinct product line with substantial financial profitability: the role of business planning. Bekes CE, Dellinger RP, Brooks D, Edmondson R, Olivia CT, Parrillo JE. Bekes CE, et al. Crit Care Med. 2004 May;32(5):1207-14. doi: 10.1097/01.ccm.0000126152.33719.db. Crit Care Med. 2004. PMID: 15190974
- Vertical integration strategies: more promising than diversification. Fox WL. Fox WL. Health Care Manage Rev. 1989 Summer;14(3):49-56. Health Care Manage Rev. 1989. PMID: 2670833
- Diversification offers new opportunities for health care. Coddington DC, Moore KD. Coddington DC, et al. Healthc Financ Manage. 1987 May;41(5):64-71. Healthc Financ Manage. 1987. PMID: 10301504
- Successful business process design. Business plan development for the occupational health services unit. Kalina CM, Fitko J. Kalina CM, et al. AAOHN J. 1997 Feb;45(2):61-7. AAOHN J. 1997. PMID: 9146105 Review.
- Writing a successful business plan. Haag AB. Haag AB. AAOHN J. 1997 Jan;45(1):25-32; quiz 33-4. AAOHN J. 1997. PMID: 9043231 Review.
- Search in MeSH
LinkOut - more resources
Full text sources.

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

- Pricing Customers Get a Demo
- Platform Data Reporting Analytics Collaboration Security Integrations
- Solutions Strategic Planning Organizational Alignment Business Reporting Dashboards OKRs Project Management
- Industries Local Government Healthcare Banking & Finance Utilities & Energy Higher Education Enterprise

Strategic Planning in Healthcare: An In-Depth Guide for Executives

Tricia Jessee
Tricia manages our implementation and onboarding team to ensure the success of ClearPoint customers.
Explore key strategies for healthcare executives in our in-depth guide on strategic planning, covering essential techniques, phases, and success tips.
Table of Contents
A healthcare organization's strategic plan is designed to identify the necessary actions needed to reach the objectives of the organization. Whether you’re creating a new strategic plan from scratch or you’re trying to breathe life into an old plan, I bet we can both agree that strategic planning and execution are tougher than they seem.
But if you have the right tools at your disposal, the process doesn’t have to be quite so painful.
Below, we present an overview of strategic planning in the healthcare industry , including: an introduction to six strategic planning techniques; the four phases necessary to execute a strategic plan; and two examples of strategic planning in healthcare.
Last but not least, we’ll describe some common pitfalls of strategic planning, so you can avoid them in your own planning.
6 Strategic Planning Techniques for Healthcare Providers
- The Performance Prism Model : The Performance Prism is a performance management framework with five perspectives: stakeholder satisfaction, stakeholder contribution, strategies, processes, and capabilities.
- The EFQM Excellence Model : Like the majority of these six techniques, the EFQM model can be used in conjunction with other frameworks. It combines three elements —Fundamental Concepts of Excellence, Criteria, and RADAR—to help you understand cause-and-effect relationships in your organization.
- The Balanced Scorecard : The Balanced Scorecard (BSC) is a strategy management framework that helps you “balance” four perspectives in your organization: finances, customers, internal processes, and learning and growth. In conjunction with a strategy map , the BSC can help provide an excellent way to manage your strategy.
- Benchmarking : Benchmarking allows you to compare metrics in your organization to either an industry average or your competitors. This is a great targeted solution, but less of a full framework.
- Capability analysis : Conducting this analysis helps you think of your organization as a set of capabilities so you can work on identifying gaps that may represent a competitive weakness (and highlight new capabilities that could be a competitive advantage!)
- Market analysis : Conducting market research will give you a good indication of industry size, growth, and trends to be aware of. This is very helpful input for your strategic plan, but it is not a plan in and of itself.
Claim your FREE 108 healthcare KPI library to improve your organizational performance
For strategic plans in healthcare organizations to work, you need to ensure you’re following a process instead of having a free-for-all. For example, if you don’t take time to analyze what needs to go into your strategic plan, you’ll end up with a handful of pointless (and frustrating) meetings.
Take a look at the following four planning phases—they’ll help you set a solid strategic plan in place.
The 4 Planning Phases of Strategic Planning
1. the analysis & assessment phase.
First, it’s critical to gain a basic understanding of what direction you’re trying to go in (while taking into account your internal organizational structure and any external factors you have to consider). You’ll want to hold the majority of your strategy meetings during this phase. In hospitals specifically, you’ll want to figure out where you need to increase performance and focus in on your plans. This is also a good time to look at areas where you are struggling and determine what direction the regulatory and competitive environment is moving in. This will be the area of the highest and most critical need.
2. The Strategy Formulation Phase
During this phase, you’ll focus on developing your high-level strategy and documenting your organization-level strategic plan. You’ll want to pick out the goals and metrics you want to track. For example, most hospitals track metrics that deal with operations, finances, communication, internal issues, public health, and care.
If you're ready to create a Balanced Scorecard that supports your healthcare strategy, we're here to help.
Also, this is the time to look at your general organizational structure and how it links to the strategy. Do you have the right people in charge of the right aspects of your strategy. This helps create accountability and ensures things don’t fall through the cracks. For example, if you’re using the Balanced Scorecard, we encourage you to name owners and collaborators as well as what each person is responsible for therein.
3. The Strategy Execution Phase
During this phase, you’ll translate your high-level strategic plan into an operational plan by honing in on projects and actions.
The execution phase can be particularly challenging for healthcare organizations because they tend to have lots of moving parts. Performance-wise, this not only complicates seeing the big picture—even if individual departments are tracking their own metrics—but also makes it nearly impossible for strategy teams to keep up with the demands of generating massive amounts of relevant data.
To execute your plan successfully, you’ll need to turn your strategy execution process into a well-oiled machine—hence the growing use of strategy software by healthcare organizations. Advanced software like ClearPoint allows you to track and manage performance using a single cloud-based platform, so that everyone in your organization remains informed and in sync with one another. (See more on this in the next chapter.)
4. The Plan Evaluation Phase
This final phase deals with the management process—which includes refining your plan, evaluating performance, and reporting on your data. For example, if you’re tracking all of your metrics and you see one that doesn’t align well, this is when you’d alter or enhance it to make it more applicable to your strategy. Keep in mind, this phase is ongoing and never-ending. You will always be evaluating and refreshing your plan!
2 Examples Of Strategic Planning In Healthcare
Though good strategic planning is indispensable, it’s arguably less than half the battle; the lion’s share of effort in achieving progress will go toward the execution of your plan. This is where many healthcare organizations stumble. They aren’t prepared for the work involved in follow-through, nor are they ready to commit the time and tools required to improve performance.
ClearPoint , for its part, is an invaluable tool. It was specifically designed to help you visualize strategy, organize strategic data, and track and report on performance.
Below are two examples of healthcare strategic planning that demonstrate the impact strategic planning software can have on strategy execution. In both cases, ClearPoint aided the execution of the plans.
See ClearPoint Strategy in action! Click here to watch a quick DEMO on the software
San juan regional medical center (sjrmc).
SJRMC came to us with a problem: They had always used strategy planning for continuous improvement, but struggled to achieve their goals because their software lacked sufficient data tracking and reporting functionality. In particular:
- They had difficulty organizing their data in a meaningful way. They couldn’t get a big-picture view of important metrics, and had no way to compile individual metrics into a strategically comprehensive profile of the hospital’s performance. This made it hard to see how any single department’s daily work was contributing to (or underserving) SJRMC’s larger goals.
- They spent too much time on reporting. Staff members devoted nearly a full day to compiling reports every month.
- Most managers avoided looking at their data because the software was hard to use. Apart from occasionally entering data for committee meetings, people avoided the tedious chore of data entry as well.
Now that they’re using ClearPoint:
- Managers have a better overall picture of performance. Data is displayed in a clear, logical format that enables users to easily analyze performance and make impactful changes based on data-derived conclusions.
- Staff members can produce reports in minutes. All the hospital’s strategic data is housed in ClearPoint. Where calculations are involved, ClearPoint performs them automatically. Team members simply press the “export to PDF” or “print” buttons and the software generates a report.
- Managers stay on top of their metrics. The first thing SJRMC’s employees noticed about ClearPoint was its simplicity, making them more inclined to use it as an aid to improving performance.
Such improvements expedite and streamline hospital processes, and give managers more opportunities and resources for continuously improving performance. They also help leadership more effectively target strategic goals.
Carilion Clinic
Carilion Clinic has a similar story. Following the Balanced Scorecard framework for strategic planning, the clinic uses leadership and provider scorecards to track and improve performance across all its facilities. While the scorecards themselves are effective, the system Carilion was using to create, manage, and share them was not. It took a significant amount of effort just to create a single scorecard. On top of that, there was no easy way for everyone—from physicians and management to senior leaders and board members—to access the information.
The upshot is that Carilion staff members have found ClearPoint to be much more user-friendly and efficient than the old system. The software automatically collects data from other internal applications, and uses advanced algorithms to calculate and roll up key measurements. These capabilities make scorecard creation quick and easy.
ClearPoint also makes it easier for Carilion’s strategy team to share scorecards, which are now sent on an automated schedule to the clinic’s 1,000-plus providers and its senior leadership. By making performance data widely available, the software clarifies performance expectations and ensures everyone knows the metric targets inherent in the goals. It also promotes an understanding of factors that affect compensation for employees or physicians in a given year.
6 Pitfalls To Avoid In Healthcare Strategic Planning
Part of strategic planning in healthcare involves dealing with any road bumps that come your way. While most companies go through some trials during their strategic planning process, a misstep could have major consequences. For one, it could derail your progress and cause you to waste months of time and energy. Additionally, it could create confusion—or even concern—across your organization. Keep in mind, some people in your organization will always be critical of your strategic plan, and those individuals will be the first to doubt it and wonder why you aren’t headed “full-steam ahead.”
While there’s not much you can do to avoid critics, you can avoid putting yourself in a position to have your strategy (and your strategy office) criticized. Avoiding these six common pitfalls is an important step in that direction.
Pitfall #1: Selecting operational KPIs instead of strategic KPIs
It’s far too simple to fall into the trap of selecting metrics that are important for your operations, but have little to no impact on your strategy . For example, many healthcare centers track the percentage of beds that are occupied in order to get a closer look at ongoing patient capacity. This metric helps you understand where you stand on capacity, and is largely operational. However, if one of your strategic goals is to increase the number of patients who choose your hospital or increase your capacity, then this metric could be strategic. Always be sure your metrics truly tie back to and inform your goals.
Pitfall #2: Having too many metrics
The majority of healthcare providers come from either a business or a science background—which makes it quite easy for them to fall in love with measures. But the caution here is that some may get overzealous about metrics and try to track too many—which is a mistake.
If you have too many metrics—say, anywhere north of 35 at the enterprise level—you won’t be able focus on the metrics that will actually make an impact on your strategy. The list of negatives goes on and on: Your reports will end up being too extensive and leadership will be less likely to read them; your meetings will end up being hours long; and you’ll simply never complete the meeting agenda, etc. All of these issues can be avoided simply by not selecting extra metrics that will distract from the conversations you need to be having.
Pitfall #3: Piling too much on your strategy office
I always recommend that you keep your strategy office as “clean” as possible. Here’s what I mean: It’s important to allow those working in the strategy office to do what they’re meant to do—plan and execute your strategy. We’ve seen many instances where others in the healthcare organization begin to tap the strategy office for little projects here and there that aren’t strategy related. The reason for this is typically that those in the strategy office are close to the leadership and are in-tune to what’s happening around the organization. While this makes them a tempting target for random projects, be sure everyone involved in your strategic planning knows their limits. The best way to ensure your strategic planning and strategy execution are successful is to keep the strategy office focused on its priorities, and nothing else.
Pitfall #4: Not having support lined up
It would be a mistake to think it is easy to get people on board with a strategy whose planning process is already in motion. If you want the buy-in of high-level personnel, you must involve them from day one. Such “zero-base” coordination is critical to setting the stage for successful execution. Without it, you’ll invariably experience a degree of organizational discord that will impede planning, muddy priorities, hamstring the alignment of departmental goals, and hinder access to key resources. To avoid these impediments, you’ll need:
- People who understand where the organization should be going, as well as where performance can be improved
- People who can drive change in the process from start to finish
- People who can get the appropriate resources in place to carry out the strategic plans
Pitfall #5: Making unrealistic or ambiguous plans
Making vague or ambiguous plans is a recipe for failure. You need to be specific about the work to be done if you hope to see improvement.
Similarly, make sure projects and action plans can realistically be achieved (including reasonable schedules). If goals and time frames are unrealistic, a constant sense of frustration will undermine morale. To avoid this pitfall, meet with the teams responsible for carrying out the components of your plan—as well as the department heads—to make sure they are armed with realistic goals and the resources they’ll need to succeed.
Pitfall #6: Hazily defined roles and responsibilities
In non-medical corporations, most measure and project owners are tasked with updating their own measure statuses and project reports. But in healthcare organizations, this isn’t always the case. Healthcare organizations can have an assistant-heavy culture, and department leaders and doctors often task those assistants with updating projects they aren’t involved in.
Therefore, it’s particularly important for those in healthcare to clearly define roles and responsibilities when it comes to strategic planning and execution. Is it acceptable for assistants to make measure updates in an ongoing fashion? If so, do they know how to do this appropriately in your strategic planning software so your leadership is consistently made aware of updates? Simply communicating these details can save you a lot of grief in the long term.
Try ClearPoint Strategy Software for Healthcare Strategic Planning
ClearPoint Strategy Software is here to streamline your planning process, from formulation to execution, ensuring you avoid common pitfalls and achieve your strategic goals efficiently.
Don’t let outdated methods hold you back—experience the power of ClearPoint and watch your organization thrive. Book your FREE demo today and see how ClearPoint can revolutionize your strategic planning!
Book your FREE 1-on-1 DEMO with ClearPoint Strategy
What are strategic planning skills.
Strategic planning skills include the ability to analyze complex situations, think critically, set long-term goals, develop actionable plans, and adapt to changing environments. Skills such as communication, leadership, analytical thinking, and decision-making are essential for effective strategic planning.
What are strategic planning tools?
Strategic planning tools are methodologies and frameworks that help organizations define their strategy and make informed decisions. Examples include SWOT analysis, Balanced Scorecard, and PEST analysis. ClearPoint Strategy offers software that facilitates the use of these tools, enabling organizations to streamline their strategic planning processes.
What are strategic planning models?
Strategic planning models are structured approaches used to develop and implement strategies. Common models include the Balanced Scorecard, Blue Ocean Strategy, and Hoshin Planning. These models help organizations align their activities with their vision and objectives, ensuring a cohesive approach to achieving their goals.
What are strategic planning techniques?
Strategic planning techniques are specific methods used to analyze and plan strategies. Techniques such as SWOT analysis, scenario planning, and stakeholder analysis are commonly used to identify opportunities, assess risks, and develop actionable plans. ClearPoint Strategy supports these techniques through its comprehensive planning software.
What are strategic planning concepts?
Strategic planning concepts are fundamental ideas and principles that underpin the strategic planning process. Key concepts include vision and mission statements, goal setting, environmental scanning, and strategy formulation. Understanding these concepts is crucial for developing effective strategic plans that drive organizational success.

Latest posts

Streamlining Strategic Planning with AI
.webp)
Top 5 Change Management Challenges & How to Navigate Them Successfully
.webp)
Strategic Planning in Times of Change: A Roadmap to Success
How to Write a Business Plan for Healthcare
- Small Business
- Business Planning & Strategy
- Write a Business Plan
- ')" data-event="social share" data-info="Pinterest" aria-label="Share on Pinterest">
- ')" data-event="social share" data-info="Reddit" aria-label="Share on Reddit">
- ')" data-event="social share" data-info="Flipboard" aria-label="Share on Flipboard">
How to Start a Financial Services Business
Example of a medical transportation business plan, how do i start a home business caring for elderly people.
- How to Create an Audit Template for a Client Account Review
- How to Get Federal Funding for a Clinic Start-Up
Writing a business plan for a healthcare involves preparing a document that outlines the services you plan to provide and how you intend to run your company. Health care businesses usually deal with reimbursement, fee schedules, billing systems, managed care contracts and operational issues. By describing how your company handles these challenges, you can prove to potential investors that your business strategy is sound and worthy of their investment.
Available Internet Resources
Use the resources provided by websites, such as the Business.gov and the Small Business Administration Small Business Planner websites, to get started writing your health care business plan. Use the self-assessment tool provided by the Small Business Administration website as well as other resources, such as free online courses, access to online mentoring and templates.
Description of Your Health Care Business
Write a description of your health care business. For example, list how your service offers elderly or disabled clients non-medical support at home. If you plan to purchase and run a franchise operation, the parent company typically provides information and training that describes the business.
For example, urgent care center businesses typically provide care by a certified physician, on-site lab services, prescription services and extended hours. Describe the skills and experience of your staff, such as technicians.
Marketing Strategy and Competitive Analysis
Use resources, such as the Plunkett Research website, to identify the industry outlook and trends in the health care industry. Identify your competitors. Analyze their strengths and weaknesses. Prepare your own promotional campaigns, which could mean describing your plans to develop a website to advertise your services or conduct an email marketing campaign to attract new customers.
Describe your community and how you intend to obtain referrals, such as making connections with doctors and hospital administrative personnel. These health care professionals frequently refer patients requiring home health care to local reputable agencies providing quality service to discharged patients.
Organization and Management
Add a section describing how you intend to organize your health care business. List the software programs you intend to use for charting and billing. Establish a mechanism for receiving payment and obtaining reimbursement for services. List the licenses required to operate a health care business in your state, using the resources provided by the Business.gov website.
Ensure that you meet the guidelines for providing health care services and that your services can be reimbursed by Medicare, Medicaid and private insurance.
Financial and Strategic Goals
Describe how you plan to finance your company and specify a multi-year plan. For example, state the number of patients you hope to serve by the end of the first year. Classify these patients by type, such as home health care or personal injury cases. Set success criteria, such as 80 percent customer satisfaction as reported by follow-up surveys you conduct with clients.
Use the resources provided by the Business.gov website to pay your taxes and ensure you adhere to all the required regulations.
- Bplans.com: Free Medical and Health Care Business Plans
- Applied Health Strategies: Working Draft of the Safety Net ACO Business Plan for the “Next Coalition”
- Entrepreneur: Health and Personal Care
- SCORE: Templates for Your Business
- Small Business Administration: Assessment Tool
Tara Duggan is a Project Management Professional (PMP) specializing in knowledge management and instructional design. For over 25 years she has developed quality training materials for a variety of products and services supporting such companies as Digital Equipment Corporation, Compaq and HP. Her freelance work is published on various websites.
Related Articles
How to start a medical staffing company, an outpatient clinic's organizational structure, how to start a medical staffing company for under $1000, how to start a computer recycling business, how to write a business plan for a spa, how to start a safety training consulting business, how to write a business plan for an errand business, how to start a recruitment business, how to start a customer service business, most popular.
- 1 How to Start a Medical Staffing Company
- 2 An Outpatient Clinic's Organizational Structure
- 3 How to Start a Medical Staffing Company for Under $1000
- 4 How to Start a Computer Recycling Business

Understanding Business Strategy to Facilitate Health Care Success
Published september 26, 2022, courses mentioned in this post: h ealth care strategy, series mentioned in this post: health care leadership.
When you think of health care organizations, do the terms sustainable advantage or strategic differentiation come to mind?
In an industry with increasing competition and innovation, leaders of U.S. healthcare organizations, or those delivering care, need to understand how the success of their business depends on these key principles. This includes understanding the industry you’re in and market dynamics, the forces that make it easy or difficult to capture value, and how you can successfully compete against rivals.
You must go beyond simply creating value to develop the critical thinking and analytical skills to evaluate the needs of your business, and its constituents, in order to optimize business decisions and inform new or innovative health care ventures.

Taught by Harvard Business School Professor Leemore Dafny , our Health Care Strategy course teaches learners to align business strategy with the challenges and structures of the health care industry in the United States.
This 5-week course explores four main concepts of business strategy that can enable leaders to deal with the unique challenges and structures of health care organizations. These concepts include:
Value Creation and Value Capture
Value is only created if purchasers are willing and able to pay an amount that exceeds the cost of producing a product or service. Additionally, value creation does not automatically result in value capture.
In Health Care Strategy , learners will exercise how to apply a framework that illustrates value creation and value capture. With case studies from Statins and Livongo , you’ll learn how to determine how much value a seller can capture by considering the competitive environment and the value created for different stakeholders.
Industry Analysis
Within the Industry Analysis module of Health Care Strategy , learners will perform a “five forces” analysis and assess the strength of different forces in different industries through a case study with Advanced Fertility Care . Identifying the forces that drive industry profits is a critical first step to defining a business strategy. A successful strategy combats the forces that diminish industry profits.
Developing a strategy requires making tradeoffs. Through a case study with Oak Street Health , learners will evaluate the tradeoffs made by an entrant in elder care, and how this informs decisions about their growth. Learners will better understand how positioning can enable you to succeed in an “unattractive” industry.
Value capture is more challenging when the value of a product or service is divided among different stakeholders, making this an extra challenge within the health care sector.
Competition
Competition among health care providers increases quality, reduces prices, and can increase a provider’s reach. Learners will evaluate the results of a “natural experiment” involving the British National Health Service (NHS) and assess opportunities provided by destination medicine for both providers and employers through a case study with Geisinger Health .
Learners will also analyze business and regulatory moves that reduce and enhance competition in different markets through a case study with the Surgical Institute of Reading .
The Boundaries of the Firm
The last module of Health Care Strategy dissects an organization’s decision to vertically integrate by observing consolidation in Eastern Massachusetts. The decision to vertically integrate depends on several factors, such as the necessity for “relationship specific” investments by upstream and downstream parties, and the degree of difficulty in aligning incentives with arms-length relationships.
Vertically integrated firms may find it more profitable to price their products less than they would if they were not integrated, even if there is no change in production cost from integrating. Learners will assess the effects of vertical integration on pricing under different assumptions.
Lastly, learners will examine the effects of provider-insurer integration on competition, prices, and access for patients through a case study with Civica Rx . Integration can deflect or enhance competition, depending on the industry structure and potential efficiencies created by the merger.
Register for an upcoming Health Care Strategy cohort today to learn how to use business strategy to facilitate health care success.
| Demonstrate that you are committed to your growth by specializing further and pursuing a multi-course certificate program.
The health care sector in the United States is one of the most essential and consequential parts of our economy.
|
|
|
Related Courses
Health care strategy.
Learn from HBS Professor Leemore Dafny how to align the principles of business strategy with the unique challenges and structures of health care organizations to capture value, define your mission, and lead your organization to success.
Health Care Economics
Taught by Harvard Medical School faculty, this course provides insights into the interactions between industries in the US health care sector and teaches what economic forces are shaping health care.
Digital Health
Digital technologies and big data offer tremendous opportunities to improve health care.

Build plans, manage results, & achieve more
Learn about the AchieveIt Difference vs other similar tools
We're more than just a software, we're a true partner
- Strategic Planning
- Business Transformation
- Enterprise PMO
- Project + Program Management
- Operational Planning + Execution
- Integrated Plan Management
- Federal Government
- State + Local Government
- Banks + Credit Unions
- Manufacturing
Best practices on strategy, planning, & execution
Real-world examples of organizations that have trusted AchieveIt
Ready-to-use templates to take planning to the next level
Research-driven guides to help your strategy excel
Pre-recorded & upcoming webinars on everything strategy & planning
- *NEW!* Podcast 🎙️
The Complete Guide to Strategic Planning in Healthcare
RELATED TAGS:
supply chain
Healthcare institutions around the world must adapt their strategies to meet current trends and patient preferences. By using reliable and thoughtful planning, healthcare facilities can initiate patient-centric approaches and boost success.
Strategic healthcare planning consists of creating objectives, setting goals and then creating a plan for achievement. In other words, it’s the process of outlining goals and taking the necessary steps to achieve them. Most healthcare plans also consider government policies and technological advancements that could alter health goals and operations.
Read on to learn more about the importance of planning in healthcare.
In This Article
The Importance of Planning in Healthcare
- New Technologies
- Mass Adoption of Virtual Care
- Continued Management of Cybersecurity Risks
- Evolving Coding Requirements
- Population Health Management
The Benefits of Healthcare Strategic Planning
Questions to ask, partner with achieveit today.

Strategic planning is essential for a healthcare facility’s overall success. Planning allows organizations to adjust to the changing demands of the healthcare industry while supporting goal achievement.
You can also see the importance of strategic healthcare planning in other areas, including:
- Adapting to current trends: Having strong plans in place can help your facility adjust to current trends. By strategically thinking about the future of the field, you can avoid surprises later. For example, a significant change facing the healthcare industry is the rise of hybrid and remote work. Many facilities offer telehealth services or remote appointments for patients. With strategic management in healthcare, institutions can take note of these changes and adjust upcoming hiring policies and staff positions.
- Meeting patient needs: Strategic planning can also aid facilities in meeting patient needs. As technological advancements progress and the number of available providers grows, patients are seeking personalized and high-quality options. Facilities can examine patient demands and use these to craft their upcoming strategy in healthcare. In turn, they can create a patient-centric approach that improves the quality of care and sets them apart from competitors.
- Reduc ing supply chain disruption impacts: The COVID-19 pandemic disrupted the supply chain for all industries, including healthcare. Without the proper tools and equipment, healthcare professionals cannot provide care for all patients. Your strategic plan could help you analyze current supply chain trends and alter ordering decisions in response. For instance, if you notice a specific type of equipment is consistently out of stock, you could order extra quantities for your facility.
- Meeting rising hospital numbers: After the COVID-19 pandemic, the healthcare industry experienced a sudden increase in hospitalizations . Strategic planning allows facilities to allocate necessary resources to meet these trends. They can also become more prepared for other potential health crises.
- Helping with public funding: Strong performance helps healthcare facilities receive more funding from public sources. Most donors use various quality metrics to determine how much funding institutions should gain each year. A strategic plan can boost your facility’s performance on many levels, from care quality to maintaining supplies.
Overall, strategic planning in hospitals and other facilities is essential for institutional success and responding to current trends in the healthcare industry.
Top 5 Strategic Challenges in Healthcare
From the Affordable Care Act’s (ACA) influx of insured patients to the increased strain of COVID-19, healthcare facilities have been constantly adapting. Here are some examples of strategic planning in healthcare today.
1. New Technologies

In the medical field, new technologies seem to appear every day. From remote patient monitoring to robust patient portals, healthcare facilities must consider the evolution of the tools used during day-to-day care. These resources may impact workflows, budgets and the patient experience.
Many new technologies offer benefits like improved efficiency and positive experiences, but they can also create healthcare challenges in the form of new requirements for your IT team and staff training. Remaining flexible can help you accommodate these possibilities, stay ahead of the competition and improve care with modern capabilities.
2. Mass Adoption of Virtual Care

From a cost perspective, one shining light for healthcare systems is the rise of virtual care, commonly referred to as telemedicine. Using internet-enabled services, healthcare providers are able to consult with patients virtually and provide diagnoses, thereby saving time and resources associated with an in-person hospital consult.
As this technology continues to proliferate, and patients become more comfortable with interacting with their doctors over virtual systems, healthcare systems will be able to trim significant expenses across departments, helping to control costs. In creating their strategic plans, healthcare leaders should take a deep look at how they continue managing telemedicine technology to help aid in future cost savings.
3. Continued Management of Cybersecurity Risks
Data security has become a significant challenge across industries, but none more so than the healthcare industry. Due to the extensive nature of personal information inherent in healthcare records, insurance companies and healthcare systems should be cautious regarding the security of their patient records.
As regular security breaches always remind us, healthcare entities should pay special attention to the security of their systems to ensure the privacy of subscribers. Healthcare leadership will need to collaborate extensively with IT, in a strategic sense, to ensure the department has the resources and technology necessary to guarantee data security and HIPAA compliance.
4. Evolving Coding Requirements
The next version of the International Classification of Diseases (ICD) is currently under review in the U.S. If you’ve been in the industry for a while, you might remember the transition to ICD-10 back in 2015. Although we may not see ICD-11 for a while, healthcare strategy must consider this eventual implementation and other potential changes to reporting and documentation requirements. To ensure full reimbursement, organizations may need to upgrade existing systems and train employees accordingly.
5. Population Health Management
Healthcare systems across the country are being confronted with a new paradigm of healthcare delivery: Ensuring the overall health of demographic cohorts within their communities.
Shifts toward value-based care only increase the focus on population health, requiring healthcare leaders to design strategic plans and allocate resources to educate the populations they serve on preventative care. This will require the participation of stakeholders across departments and often will necessitate new programs to be established to help further population health interests.

Committing to a strategic plan can bring many benefits to healthcare facilities, including:
- Establishing a shared vision: A plan requires your facility to focus on specific goals. As you develop these objectives, you and your team can establish the overall purpose of your facility. Then, you can create concrete ways to meet this vision . You can also inform employees, shareholders and other crucial team members of this vision, inspiring members at every level. All members can unite around a shared purpose and find more value in their work, improving overall performance.
- Prioritizing critical issues: By focusing on a strategic plan, you can prioritize vital issues. Every healthcare facility has specific areas for improvement, whether it’s improving collaboration or meeting staffing requirements. Strategic management in healthcare allows you to identify these areas and brainstorm specific ways to address them. You can focus on resolving the most significant issues first, instead of getting overwhelmed with secondary problems.
- Improving team communication: Strategic planning also assists with communication across your facility. Your plan should address key issues and goals, then outline the steps you will take to achieve these. You can share these plans with all institutional members, giving everyone a clear idea of future actions. With everyone on the same page, your facility can collaborate more easily and stay on track with goals.
- Enhancing motivation: A clear vision and plan can motivate employees to work harder. They can feel empowered to make decisions that support institutional goals. As they work toward a shared purpose outlined in a healthcare strategy, they feel more motivated by their daily work and can improve their performance.
- Solidifying leadership: All healthcare facilities rely on strong leadership to lead employees and meet goals. Leaders can use strategic plans to clearly identify goals for employees. They can clarify expected behaviors and encourage employees to work toward their personal best. Passionate leaders and hard-working employees can establish your facility as a leading healthcare option.
Because the purpose of strategic planning in healthcare is to work towards improvement, asking questions can help you. Healthcare institutions should ask a few crucial questions during their planning. By thinking about particular circumstances, you can tailor plans for your needs. These questions can also help you identify goals and develop a shared purpose.
Here are a few examples of questions to ask during strategic planning:
- What is the current financial situation of your institution?
- What are your goals for finances moving forward?
- What areas need more help or growth?
- What are the needs of your facility’s typical population?
- How could these needs change over time?
- What current trends in the healthcare industry or government policies could impede these goals?
- Where would you like to see your organization in five years or ten years?
You can use questions like these to establish objectives and an overall vision. Once you have developed these, you can develop steps for achievement. Structures like SMART goals can help you create measurable and timely actions .

At AchieveIt, we understand the importance of well-defined healthcare goals and addressing the challenges of healthcare strategy. You can move directly toward your shared vision with a strategic plan and clear-cut goals.
Our strategic planning software helps healthcare institutions meet their goals. The technology helps you analyze data to identify specific goals and areas for improvement. Then, we can help you form quantifiable and actionable goals that move you toward your overall purpose.
AchieveIt software also features:
- Integrated reports
- Automated reminders for deadlines and goals
- Real-time data updates
- Speedy set-ups and communication processes
Our expert team of specialists can help your facility through each step of the planning process. We can enhance your plans and offer specific suggestions for improvement. Whether you want to improve physician care or reduce waiting room times, our software can help you meet these goals.
Let’s actually do this. Schedule a demo with AchieveIt today.
Meet the Author Chelsea Damon
Chelsea Damon is the Content Strategist at AchieveIt. When she's not publishing content about strategy execution, you'll likely find her outside or baking bread.
Related Posts

Balanced Strategy: Mastering the Art of Zooming In and Out

Everything You Need to Know About Business Mission and Vision Statements

Excel vs. AchieveIt for Strategic Planning
Hear directly from our awesome customers
See first-hand why the world's best leaders use AchieveIt
See AchieveIt in action
Stay in the know. Join our community of subscribers.
Subscribe for plan execution content sent directly to your inbox.

How To Implement Effective Strategic Planning In Healthcare

Are you feeling overwhelmed and uncertain about the future?
According to Deloitte , “The global healthcare sector stands at a crossroads in 2024, poised for profound changes. The future of global healthcare is likely to be shaped by innovation, sustainability, social care integration, cost management, and workforce adaptation.”
If you work in the healthcare industry, you know firsthand how quickly things can change. As technology advances, regulations change, the population ages, and new diseases evolve at lightning speed, it can be tough to keep up.
That's why implementing an effective strategic planning process that is execution-ready is so important. It's a tool that helps healthcare organizations prioritize their goals, anticipate potential roadblocks, and quickly adapt to seize new opportunities.
Whether you’re a manager or a top-level executive, this article will provide valuable insights and guidance to help you develop and execute a successful strategic plan.
We'll also show you how Cascade can help you successfully plan, execute, and track your healthcare strategy in one centralized location. Plus, as a bonus, we'll provide a free strategic planning template prefilled with healthcare examples to help you get started.
So, let's dive in and discover how strategic planning can help you navigate the changing landscape of the healthcare environment and achieve your organization’s goals.

Strategic Planning In Healthcare: What Is It?
Strategic planning in healthcare helps you set business goals and decide how to allocate resources to achieve these goals. It involves looking at your organization’s internal and external environments using established strategic tools .
Doing so lets you develop a strategic plan outlining what you want to achieve and an action plan to get there. Think of it like building a roadmap that helps you get to where you want to go.
With a healthcare strategy, you’ll have a framework for improved decision-making that is aligned with your overarching business objectives . This ensures you’re moving towards your long-term goals and objectives, even when making short-term decisions.
Examples Of Strategic Planning In Healthcare
Strategic planning can significantly enhance the operational efficiency and service quality of healthcare organizations. Here are some specific examples of how you can use strategic planning:
- Boosting Patient Care Quality : Tackle specific challenges like lowering the rates of hospital-acquired infections or enhancing the coordination of patient care. By pinpointing these areas, you can implement targeted improvements that directly benefit patient outcomes.
- Optimizing Staff and Resource Management : Utilize data analytics to make evidence-based decisions regarding staffing and resource distribution. This approach ensures that your workforce is optimally aligned with patient needs, and your resource allocation is efficient, contributing to a more effective healthcare system.
- Exploring New Avenues for Growth : Seize opportunities to expand your services and reach by integrating telehealth, offering home healthcare solutions, or developing specialized programs tailored to unique patient demographics. Such strategic initiatives can open new revenue streams and meet the evolving needs of your community.
- Improving Financial Health : Identify strategies for cost reduction and revenue enhancement, such as streamlining supply chain operations or venturing into untapped markets. These measures can bolster your organization's financial stability, allowing for reinvestment in key areas.
- Fostering Partnerships for Comprehensive Care : Establish collaborations with community organizations, other healthcare providers and facilities, or specialists to broaden your service offerings and improve patient care. Partnerships can lead to a more integrated care model that addresses a wide range of patient needs.
📚 Recommended read: Strategy study: The Ramsay Health Care Growth Study
Healthcare Strategic Planning: Why Is It Important?
Strategic planning in healthcare is more than just setting goals; it's about ensuring your organization is on the right track for success.
These are some of the countless benefits of strategic planning in healthcare:
Boost profitability
Strategic planning helps healthcare leaders improve their organization’s financial performance and achieve long-term sustainability. It's about using resources wisely, cutting costs where possible, and smoothing out inefficiencies by streamlining processes and creating better strategic initiatives to increase patient volume and improve experience.
Additionally, strategic planning plays a crucial role in uncovering new opportunities for revenue, enabling healthcare organizations to diversify their sources of income.
Enhance collaboration and engagement
Strategic planning in healthcare goes beyond identifying operational challenges; it's about bringing to light the issues that affect our teams daily, such as the strain of long work hours. When staff feel overburdened, their motivation dips, leading to decreased engagement and higher turnover rates.
By articulating a clear vision for the organization and actively involving employees in the strategic planning process, we can significantly boost morale. It's about making sure everyone feels seen and heard, understanding that their contributions are valued. This inclusive approach not only enhances team engagement but also encourages stronger retention.
Strategic planning also fosters collaboration across different teams and business units within the healthcare organization. By working together towards common goals, departments can better align their efforts, share insights, and support each other in achieving the organization's objectives. This synergy not only improves efficiency but also builds a more cohesive and motivated workforce.
💡Pro Tip : Ensure your vision statement is crystal clear organization-wide for unified strategic alignment.
Increase efficiency
Strategic planning helps you align your operational activities with the organization’s goals. This ensures that every action contributes toward achieving your business objectives. Strategic planning also empowers healthcare leaders, providing them with the insights needed to make resource allocation decisions wisely in the dynamic healthcare landscape.
Improve communication
A good strategic plan should be shared with all stakeholders so they can form a clear picture of how their actions affect a future outcome. This transparency promotes better communication within the organization, as employees align their efforts towards achieving a common goal. The end result is a more collaborative environment where the collective focus is on attaining shared objectives.
Drive alignment and strategy execution
Involving key stakeholders in the strategic planning process is crucial for aligning your healthcare organization's goals with its overarching strategy. This ensures that everyone, from top management to frontline staff, is aligned and moving in the same direction. Achieving this level of strategic harmony across the organization reduces confusion and clarifies the collective mission, paving the way for successful strategy implementation. This collaborative approach not only fosters a unified effort towards common objectives but also enhances the overall effectiveness of the organization's strategic initiatives.
💡Pro Tip : Ensure you balance a top-down and bottom-up for enhanced vertical and horizontal strategic alignment .
5 Strategic Planning Tools For Your Healthcare Strategy
Here’s a list of strategy tools and frameworks that can help you identify gaps in your healthcare strategy, prioritize strategic initiatives, and develop business goals:
1. Balanced Scorecard (BSC)
The Balanced Scorecard translates strategic goals into measurable indicators or metrics to help you balance four critical organizational perspectives: financial, customer, internal processes, and organizational capacity.
Using this tool ensures that your organization aligns with your strategic objectives and that you’re measuring the right KPIs to track progress toward those objectives.
2. Objectives and key results (OKR)
The OKR framework sets specific and measurable objectives and tracks progress toward them using key results. Objectives should be ambitious and challenging but achievable. Meanwhile, key results should be specific and measurable and have defined target values.
This framework promotes accountability and transparency since everyone works toward the same goals.
3. Political, economic, sociocultural, and technological (PEST) analysis
PEST analysis helps you understand the external factors that may impact your operations. By using this tool, you can identify potential opportunities and threats so you can anticipate and respond to changes in the external environment.
For example, PEST can help you identify a shift toward consumer-driven healthcare. Consequently, this enables you to invest in telemedicine and other digital healthcare technologies to meet patients’ changing needs.
4. Strengths, weaknesses, opportunities, threats (SWOT) analysis
SWOT analysis is a simple yet powerful way to identify the internal and external factors that can impact your organization’s success.
For example, if you discover that staffing levels are a weakness, you may decide to invest in staff training or recruitment programs. Or, if you identify an opportunity to expand into a new service area, you may choose to allocate resources for the expansion.
By leveraging your organization's strengths through this analysis, you can craft targeted strategies that address challenges and capitalize on opportunities for sustained success.
5. Theory of change (TOC)
The theory of change is a framework that helps your organization articulate the desired outcomes and specific steps you need to take to achieve them. This model provides a more structured approach to achieving goals by identifying the inputs required for success.
For example, if you want to reduce hospital readmissions, you may use the theory of change to identify the inputs needed (staff training on patient education), activities needed (discharge planning), and desired outcomes (reduction in hospital readmissions). By mapping out this logic model and continuously evaluating the initiative, your organization can adjust its activities to achieve your desired outcomes and improve the quality of care for your patients.
📚 Recommended read: 26 Best Strategy Tools For Your Organization in 2024
How To Implement A Strategic Plan In Healthcare
Implementing a strategic healthcare plan can be challenging. Follow this step-by-step framework to help you get started.
💡Pro Tip : Streamline your healthcare strategy planning, execution, and tracking with Cascade Strategy Execution Platform . It serves as a centralized hub for enhanced decision-making and accelerated results. Unsure of where to begin? Kickstart your strategic planning process with our complimentary pre-filled healthcare strategy template .
1. Establish goals
The first step is to establish clear and measurable goals. These goals should align with your organization’s mission and vision , and be SMART (specific, measurable, achievable, relevant, and time-bound).
Examples of goals in healthcare include reducing hospital readmission rates, improving patient satisfaction scores, or increasing revenue.
👉🏻How Cascade can help? With Cascade's Planner feature , you can simplify the process of constructing your strategies. It provides a structured approach, making it effortless to break down complex high-level initiatives into actionable outcomes.
2. Set milestones and measure progress
Once you establish goals, it’s important to set milestones and measure progress regularly. This allows your organization to track its progress toward achieving its goals, identify areas for improvement, and make necessary adjustments.
Make sure to establish a timeframe for your milestones, whether it's monthly, quarterly, or yearly, depending on the nature of your goal.
👉🏻How Cascade can help? Cascade's Metrics Library offers a centralized repository for your business metrics, allowing you to seamlessly link these metrics to your plan's Key Performance Indicators (KPIs). Integrating core metrics becomes a breeze, whether they originate from your business systems, data lakes, Business Intelligence (BI) tools, or spreadsheets.
3. Develop an execution plan
To successfully achieve your goals, it is essential to have a comprehensive execution plan . This plan should detail all the necessary activities and strategies that will guide you toward success.
An effective execution plan must include a well-structured timeline, a checklist of required resources, and clearly defined responsibilities for each action or project.
👉🏻How Cascade can help? Cascade's Alignment Maps feature empowers you to monitor the interactions between activities by documenting and examining dependencies, blockers, and risks that might arise during your strategic journey. This ensures a smooth path to successful strategy execution.
4. Monitor performance and adapt as needed
Once the plan is in motion, you should monitor its performance regularly and make necessary adjustments when you notice deviations. You must be flexible and willing to change your execution plan as needed.
For example, if the original plan doesn't turn out to be effective, it's important to quickly reevaluate and come up with an alternative strategy.
👉🏻How Cascade can help? Cascade's Dashboards & Reports allow you to gain accurate, real-time insights into your strategic performance, enabling you to easily share this information with your stakeholders.
5. Communicate regularly
Communication is key in implementing a strategic plan . Each stakeholder should understand their role and how their work fits into the big picture. You must inform them of progress toward the established goals, any changes to the execution plan, and other relevant information. This will help you build trust and get buy-in, which are essential for successful strategy execution.
6. Celebrate successes
Celebrating successes helps maintain motivation and momentum. It shows staff and stakeholders that their hard work is paying off. This can be done in various ways, such as recognizing staff members who have contributed significantly to the plan or sharing positive feedback from patients.
Positive reinforcement will motivate employees to keep striving to achieve your organization’s objectives.
📚 Recommended read: How Parker University uses Cascade to help them hold a position as a leader in Patient-Centric Healthcare
Case Study: Perley Health’s Strategic Ambition
Perley Health, a healthcare organization dedicated to improving care for veterans and seniors, faced some significant challenges in their strategic planning and execution processes. These challenges included making assumptions about the stability of the external environment in their long-term planning, inconsistency in how different departments planned and reported, a lack of clarity in how they measured success, and a somewhat fragmented approach to strategic and departmental plans.
Perley Health's journey toward strategic improvement began with the adoption of Cascade, a pivotal decision for them. Initially, they used Cascade to bring together all their strategic plans and initiatives, which brought about greater transparency and alignment with their organizational priorities. This not only made resource allocation more efficient but also provided a standardized way to measure results, making it easier to discuss return on investment (ROI) and track progress systematically.
Empowered by Cascade's capabilities, the management and various teams could now propose forward-thinking initiatives with a clear view of how they aligned with strategic priorities. This sped up decision-making and made funding allocation more precise.
With the right tools in place, Perley Health is now confidently working towards their goal of doubling senior care and establishing themselves as a center of excellence in frailty-informed care. They keep a close eye on their progress using the Cascade platform.
This case underscores the critical importance of strategic planning in navigating the complexities of healthcare, demonstrating a clear path to achieving and surpassing organizational objectives.
📚 Read the complete Perley Health Case Study!
Execute Your Healthcare Strategy With Cascade 🚀
Take the guesswork out of strategic planning in healthcare. With Cascade , you can easily create an execution plan customized to your goals and objectives, including assigning initiatives and setting deadlines for each team member involved.
Take a look at this example of a healthcare strategic plan in Cascade:

You can also leverage easy-to-use dashboards and visualizations that provide real-time data on your progress toward your goals.
Here’s an example of a real-time dashboard:

Cascade lets you collaborate with your team, assign responsibilities, and communicate progress, ensuring everyone is aligned and working toward the same objectives.
Whether you run a small clinic or a large healthcare organization, Cascade will help you make strategic planning in healthcare a breeze. Learn more about Cascade for healthcare !
Looking for a tailored tour of our platform? Book a demo with one of our Strategy Execution experts.
Popular articles

6 Steps To Successful Strategy Execution & Best Practices
.png)
McKinsey GE Matrix: Importance & How To Use It (2024)
.png)
How To Be More Strategic: 7 Tips & Best Practices For Leaders
.png)
Red Ocean Vs Blue Ocean Strategy Overview + Examples
Your toolkit for strategy success.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Business acumen for nursing leaders, optional or essential in today's health system? A discussion paper
Chris raftery.
a Gold Coast Health, Qld, Australia
Anne-Marie Sassenberg
b School of Business, University of Southern Queensland, Toowoomba, Qld, Australia
Anita Bamford-Wade
Over the last number of years, the healthcare system has become more complex in managing increasing costs and outcomes within a defined budget. To be effective through reform, especially moving forward from the COVID-19 pandemic, healthcare leaders, specifically in nursing, have an increased need for business acumen beyond traditional leadership and management principles.
This paper examines the concept of business acumen in the profession of nursing, specifically for managers and higher nurse leaders, establishing whether these skills are optional or essential.
Nurses learn and develop broad skills in leadership and management, but less specifically about business or the broader system. With a contemporary Australian health system aiming to be more effective, nurses may require a greater level of business acumen to adequately understand the mechanics of business decision making in the system when designing care models, as well as representing the business potential of nursing in balance with clinical outcomes through reform.
The modern nurse, in addition to clinical skills, may need a foundational understanding of business evolving throughout their career, to maximise innovative growth across the system, in meeting the healthcare needs of our community now and into the future. Without a foundation level of business acumen and an understanding of the system across the profession, nurses may not be empowered with their full potential of being a strong voice influencing health system reform.
Summary of relevance
Across the world, including Australia more recently, healthcare has become more of a business than a social enterprise. Clinician leaders including nurses, have skills in leadership and management, but inconsistent business acumen or knowledge of the broader system.
What is already known?
Understanding business principles enable leaders to develop and influence sustainable solutions in balancing system resources with clinical outcomes. While business acumen itself is not a new concept across many industries, these skills are less common for clinicians.
What this paper adds?
Understanding the importance of business acumen for nursing leaders will identify gaps in the profession's current leadership and management skillset, as well as highlighting the enhanced value of nursing leaders consistently possessing these business skills. This discussion may also identify opportunities for future growth through training.
Alt-text: Unlabelled box
1. Introduction
Effective leadership in healthcare has grown in importance as we work through the pandemic ( Dudzic, 2021 ). Healthcare is typically an industry associated with the provision of services that address illness and injury ( Mahoney, 2001 ; Thew, 2020 ; WHO, 2019 ). Historically, there has been less focus on cost containment with this provision of care ( WHO, 2019 ). However, with modern day advances in treatment and technology consuming a greater percentage of government and household spending, the healthcare industry has seen a shift over the last two or more decades from ‘care at any cost’ to sustaining a care delivery system working within a defined budget ( WHO, 2019 ). The COVID-19 pandemic has further highlighted the importance of sustainable budgeting in conjunction with health service delivery ( Dudzic, 2021 ). In nursing however, this potentially introduces a clash of values between two paradigms being care and cost ( Bamford-Wade & Moss, 2010 ).
With the introduction of managerialism through reform in the early 2000s that highlighted the importance of leadership skills beyond the delivery of care, sustainability practices of health service delivery have been now somewhat embedded as normal business across the system ( Bamford‐Wade & Moss, 2010 ; Pierce, 2016 ). However, embedding managerialism raises the question, “are our clinicians sufficiently knowledgeable in terms of business acumen to best perform in this more fiscally focused environment, while at the same time continuing best practice standards in meeting the healthcare needs of our community?” Throughout this paper, the authors will refer to business in the context of acumen, which is defined as a combination of knowledge and skills ( Elgood, 2012 ). While there are many differences and timeframes of change between health systems across the world, when noting the global research, the authors will consider healthcare system consistencies within the Australian context, such as healthcare service delivery, clinical outcomes, budget limitations and the role of the nurse leader.
The health system is a complex industry with many moving parts ( Uhl-Bien, Meyer, & Smith, 2020 ). Understanding the business of healthcare and perspective at a systems level (system thinking) can be important to consider. Frequently, a clinician has a good idea regarding improving service delivery, writes a business case, but then fails to receive a green light to proceed ( Malloch & Porter-O'Grady, 1999 ). The clinician often relies on business case templates, without understanding the full context of the business information required ( Sherman, 2020 ). This can then fall short of including all the relevant details to support the decision-making process, leading to a negative outcome without the clinician understanding as to why, demonstrating a highly inefficient process ( Malloch & Porter-O'Grady, 1999 ; Tally, Thorgrimson & Robinson, 2013 ).
Nursing at all levels has a history of not adequately representing the business detail, subsequently failing to get all business cases across the line in the first instance ( Tally et al. 2013 ). Experienced nurse leaders are not immune to this scenario either. While a leader's understanding of the budgetary process is substantially greater than the frontline clinician, there are still some finer business elements a nurse leader may have a limited grasp on, based on their experience and exposure, such as activity revenue ( Davidson, Elliott & Daly, 2006 ). In Australia, a large proportion of our public health system is funded through the delivery of health activity, known as activity-based funding, or ABF ( IHPA, 2021 ). “Fee for service” around health activity, is also one of the foundations of Medicare and private health insurance funding models ( Australian Government, 2019 ). Most of these funding mechanisms, however, do not directly relate to nursing and therefore can be easily misunderstood or underestimated ( Davidson et al., 2006 ). A knowledge of funding mechanisms would empower nurse leaders to better influence the delivery of quality health services.
The environment of healthcare can be described as less than ideal when it comes to understanding a rational approach to economic decision-making ( Altman, 2012 ). While clinical outcomes and person-centred care is always the priority, economic decision-making can be positively or negatively influenced by emotion and intuition of what may be best for the consumer, sometimes leading to mental short cuts and cognitive biases ( Altman, 2012 ). Having knowledge and a clearer understanding of this, however, through a consistent level of business acumen, can only empower nurse leaders to positively contribute to system level decision-making in the healthcare environment ( Altman, 2012 ). Authentically balancing leadership priorities between the competing paradigms of caring and economics, is symbolic of today's changing and challenging healthcare landscape ( Keselman & Saxe-Braithwaite, 2020 ).
Nursing is known as a profession with strengths related to quality, safety, care and compassion ( Burston, Chaboyer & Gillespie, 2014 ; Roche, Duffield, Dimitrelis, & Frew, 2015 ; Shamian & Ellen, 2016 ). Business acumen however, only appears to be a strength of some ( Graham, Fielding, Rooke, & Keen, 2006 ; Kang et al., 2012 ; Waxman & Massarweh, 2018 ), leading to a question of whether this skillset is an opportunity for the profession to explore more broadly, as we continue to evolve our value as leaders across our health system into the future. Nursing has often been a profession of the health industry, perceived as only supporting other health professionals ( Porter-O'Grady, 1999 ; Shamian & Ellen, 2016 ). Therefore, any broader value of nursing has not always been well understood or represented ( Malloch & Porter-O'Grady, 1999 ; Shamian & Ellen, 2016 ). However, despite increasing mechanisms for nursing roles to independently deliver activity and attract revenue, nursing has continued to undersell its full potential in the health system, due to having a limited grasp of representing business principles ( Rutherford, 2012 ; Waxman & Massarweh, 2018 ). Tapping into recurrent funding streams for own-source revenue through activity is one example of opportunity that is relatively foreign for nursing in general, compared with traditional block funding allocations in Australia ( Davidson et al., 2006 ). Activity and revenue for example, are two key metrics of the health system, that would be highly valuable for today's nurse leader to better understand.
Health systems deliver clinical services for the community. Historically, nurses and other clinician leaders have led teams in the delivery of these services, with many other parts of the organisation being run independently at times by non-clinical staff ( Longmore, 2017 ). With a shortage of adequately prepared nurse leaders with a moderate degree of business acumen, Mahoney (2001) noted in the United States (US) that there was a risk of non-nurses filling nurse administrator roles, potentially diminishing the nursing voice. Over the last two decades however, this risk has not reduced globally, and is an opportunity for nurse leaders in Australia to become increasingly relevant as we reform into the future ( Roche et al., 2015 ).
A review of the literature on nursing leadership, management, and business skills indicates the following descriptions. Leadership is defined as a series of qualities from competence, confidence, creativity and courage, in order to carry out functions such as advocacy, inspiration, guidance and empowerment, to build self-esteem, trust, as well as drive vision and influence positive outcomes ( Heuston & Wolf, 2011 ; Mahoney, 2001 ; Negandhi et al., 2015 ; Thomas et al., 2008 ). Management, in the context of a healthcare leader, is defined as administrative tasks related to overseeing staff, budgets and patient care ( Roche et al., 2015 ). While leadership is a series of qualities and management is a series of learned transactional skills related to managers, business is applying a financial and economic lens over this, as well as understanding the running and performance of a complete organisation ( Mahoney, 2001 ). From the literature, the authors understand management be described as “unit (level) leadership,” and propose business being expressed as “system (level) leadership.” It is with a business lens, that the value of a system level of understanding is clearer. These broad terms are noted in Table 1 .
leadership, management and business skills (glossary at end of paper).
| Leadership skills | Management skills | Business skills |
|---|---|---|
| AdvocacyInspirationEmpowermentInfluenceVision | Human resourcesBudgetsQuality/outcomes(Unit leadership) | Finance/economicsPerformanceOrganisation(System leadership) |
A published example of a nursing leader role that demonstrates inconsistent preparedness of the above knowledge in balance is the nurse manager ( Roche et al., 2015 ). A nurse manager is pivotal in influencing a positive clinical environment, effectively managing change, culture, attitude and direction of staff delivering healthcare ( Mathena, 2002 ; Sherman, Bishop, Eggenberger, & Karden, 2007 ). While an essential role, many nurse managers do not commence with formal leadership or management skills, qualifications or knowledge for success ( Contino, 2004 ; Patrician, Oliver, Miltner, Dawson, & Ladner, 2012 ; Roche et al., 2015 ). Often chosen as an excellent clinical nurse with seniority, a skill deficit is immediately present, leading to often rapid, “on the job” training of transactional activities and forced learning by osmosis, which in most cases leads to a competent transactional leader, but often limits the nurse manager to think and act at the system level ( Roche et al., 2015 ; Sanford, 2011 ). What this rapid training in management and leadership does is often impede the full effectiveness of the nurse manager to actively grow as a transformational leader of their unit in the short term, as well as limit their longer term understanding of, and contribution to, the business of the wider organisation and system ( Roche et al., 2015 ). Learning lessons from critical roles such as the nurse manager could better prepare our future nurse leaders.
Broad leadership and management skills, including business acumen, can evolve through experience, as well as be learned via formal educational pathways through various university and healthcare organisation programs ( Curtis, Sheerin, & de Vries, 2011 ). Nurses, however, typically do not have consistent access to adequate training on the full domains of business and finance, despite often being responsible for budgets ( Waxman & Massarweh, 2018 ). For example, financial practices can be limited to being given a set budget to work within, without understanding the full mechanics of how a budget is determined ( Roche et al., 2015 ). Having appropriate educational preparedness that increases consistent business acumen for nursing leadership roles can enhance professionalism, as well as positively influence the clinical environment and wider organisational clinical and financial outcomes through enhancing a workforce culture of empowerment ( Abraham, 2011 ; Cummings et al., 2008 ). The literature points towards business acumen (often referred to as business management skills) being essential, yet it appears to be a distinct skillset less focused on in nursing leadership development ( Graham et al., 2006 ; Kang et al., 2012 ; Waxman & Massarweh, 2018 ). Furthermore, there appears to be a gap in the research of the impact of this lesser focus on business in nursing across the years, as well as what a minimum standard of business acumen would be ( Abraham 2011 ; Mahoney, 2001 ; Roche et al., 2015 ; Waxman & Massarweh, 2018 ). Further research investigating the value of business acumen as part of nursing leadership is vital to continually evolve our input into future health systems.
2. Discussion
Brown (1983 , p. 52) in the US, set the scene of this discussion globally, by asking “ what is business savvy ?.” She highlighted the importance of nurses requiring socialisation to the corporate culture, that the qualifications required for tomorrow's nurses will be different from today's, and that working with a limited health dollar would demand changes to the educational preparedness of nurses ( Brown, 1983 ). Since then, other international perspectives have included Graham et al., (2006) in the UK, noting weaknesses of nursing management being political acumen and professional business management ( Graham et al., 2006 ). While in Taiwan, Kang (2012) found nursing administrators self-rated themselves as high on integrity but low on financial and business acumen skills ( Kang et al., 2012 ). There are limited publications found on this in the Australian context, possibly reflecting the pace and impetus of international trends on this part of leadership.
Flowing on from Brown's initial work, Sanford (2011) drove the case for nursing leadership development being a collaboration between chief financial and chief nursing officers in developing nursing leaders in the US. While Rishel (2014) went one step further, proposing all nursing levels need business knowledge, not just leaders, noting the imperative of floor nurses having awareness of not only positive clinical patient outcomes, but the financial implications of various chemotherapy agents on maintaining a hospital's solvency ( Rishel, 2014 ). In 2018, Waxman noted a broader recognition of business competence in leadership, with the six key healthcare administrator agencies in the US developing five core competencies for healthcare leaders that included business acumen as one of them ( Waxman & Massarweh, 2018 ). As our local profession evolves leadership capacity, it can be argued these competencies would have high relevance for the Australian context as well.
In addition to the technical skills of nursing, nurse leaders develop strengths in leadership and learn transactional skills in management throughout their careers ( Mahoney, 2001 ). However, the ever-growing importance for all clinician leaders to understand a greater depth of how a health organisation runs highlights business acumen as potentially becoming more essential across clinical professions ( Waxman & Massarweh, 2018 ). Notwithstanding the evidence, a focus of business acumen is still lacking from most learning pathways and programs ( Curtis et al., 2011 ; Fuster Linares et al., 2020 ). It can be argued that business is a subset of both leadership and management, but neither adequately cover the finer details of an organisational or systems level perspective. While nursing has strengths in leadership and management, business acumen may be a focused skillset of value for the profession to consider as we continually advance into the future, with business evolving as an essential skill for contributing to healthcare reform ( Bamford-Wade & Moss, 2010 ; Davidson et al., 2006 ; Waxman & Massarweh, 2018 ). This is demonstrated in Fig. 1 .

(Original concept by authors) – nursing technical skills, leadership, management, and business skills.
Modern nurse leaders need to be consistently skilled and recognised as business savvy and need a broad view of the healthcare system ( Mahoney, 2001 ; Waxman & Messarweh, 2018 ). In a global survey by Roche et al., (2015) , limited exposure to hospital affairs as a nurse leader was one of the main factors that influenced a nurse manager's decision to leave a role. The increasing complexity of the system, without adequate training or inclusion, has also been noted as a factor of increasing nurse leader burnout ( Uhl-Bien et al., 2020 ). Understanding the business side of healthcare can positively impact the bottom line of an organisation and is essential in today's changing healthcare environment ( Dudzic, 2021 ; Sanford, 2011 ; Thomas, Seifert, & Joyner, 2016 ). Nurse leaders are ideally placed to balance the clinical context and business demands of today's financially challenged healthcare system and reform efforts ( Kesselman & Saxe-Braithwaite, 2020 ; Pierce, 2016 ). As we move into a new phase of health system management in Australia post-pandemic and through ongoing system modernisation, nurse leaders need to be at the forefront of reform and should have optimised knowledge and acumen to positively influence change.
Along with nursing leaders, further to Rishel's views in 2014, it can be argued that foundational business competence is of value to all clinicians at all levels (nursing/midwifery, allied health, medicine), to deliver care most effectively in today's health system, from understanding everyone's roles in performance through to cost effectiveness. Nurses at all levels could benefit from having leadership skills ( Dyess & Sherman, 2011 ; Vance & Luis, 2020 ). While new graduate nurses are considered somewhat bedside leaders ( Al-Dossary, Kitsantas, & Maddox, 2014 ), all levels of nursing could benefit from skills that enable better understanding of the bigger picture where an institution's survival is based on core business principles ( Fletchall-Wilmes, 2019 ). With healthcare becoming more corporate, nurses in the future will need to be more business savvy to understand the decision-making process, which underpins the delivery of clinical services ( Castledine, 2006 ).
“Knowledge is power” ( Mahoney, 2001 , p. 270). Embedding leadership education to include foundational business principles across nursing degree programs as a norm of practise for all nurses, not just designated leaders, will develop essential skills and baseline awareness of business, increase leadership capacity across the profession and best prepare our nurses for the future ( Curtis et al., 2011 ; Fuster Linares et al., 2020 ; Negandhi et al., 2015 ; Scott & Miles, 2013 ; Thew, 2020 ). In conjunction with traditional nursing values, this would encourage the growth of business acumen in nursing from passive awareness as a new graduate, through to active understanding and dynamic contribution later in one's nursing career as demonstrated in Fig. 2 .

(Original concept by authors) – growth of business acumen.
These foundation skills are proposed to enhance the long-term ability of nursing to lead and drive innovative health, reform and best practice, delivering sustainable healthcare where it counts.
3. Conclusion
Nursing leadership development is not a new concept in Australia nor around the world. However, over the past couple of decades and more recently through reform, there has been limited specific commentary about the need for nursing leaders to be more business savvy, able to adapt to today's healthcare environment, as well as focused efforts to enhance this skillset for nursing in Australia. The Australian healthcare system is at a point where major change is underway to reform and modernise, thus delivering more efficient and effective services for the community and the health system that is sustainable into the future.
Nurse leaders and all clinician leaders, in being able to lead and drive innovation and reform, would benefit from having a good and consistent understanding of all the moving parts of the system. Understanding the big picture in addition to clinical expertise, would promote positive effort and collaborative dialogue for successful transformation of the health system to occur. With an increased focus on the business side of healthcare, the strength and value of nursing's contribution and influence, can only be enhanced with a consistent approach to business acumen across the profession, in addition to the traditional values of nursing. By representing the business detail in addition to caring, our profession could position ourselves to be acknowledged with greater potential than what may be traditionally understood, opening up new opportunities for nursing at the system level. It is believed that business acumen is therefore essential for advancing nursing and health service delivery in Australia.
Furthermore, with the future direction of healthcare in Australia, there is a strong case for foundational business skills to be a fundamental competency of all clinicians at all levels. In nursing for example, this could likely enhance our profession's input on quality and safety, as well as perspective of promoting the person-centredness of healthcare. The inclusion of core business concepts that underpin our health system as part of the undergraduate curriculum, could be an effective method of delivering this knowledge, with continuous training also a vital part of future reform.
4. Recommendations
Overseas literature highlights business acumen as an essential skillset for nurse leaders to understand and contribute to the broader system ( Graham et al., 2006 ; Kang et al., 2012 ; Shamian & Ellen, 2016 ; Thew, 2020 ; Waxman & Massarweh, 2018 ). While in Australia, although transactional leadership and management development are somewhat described ( Roche et al., 2015 ), there is little acknowledgement of specific business acumen for nurses. There would be substantial value in understanding what the literature identifies as skills of business acumen, what these skills look like in nursing in conjunction with traditional values, and what needs to change in structure and culture of health organisations, to recognise and enhance these skills and therefore business acumen across the profession, without being a competing paradigm for nursing?
Along with reviewing the literature, current global bodies of knowledge on the skills of business acumen for clinicians need to be explored further in the Australian context. Further to this, exploring the skills, education and aspirations of our Australian healthcare workforce, as well as input from prominent healthcare leaders and other non-clinical stakeholders, could identify a focused collection of foundation skills of business acumen that will inform policy and curriculum in the future.
Recognising the value of business acumen for nursing leaders (with potential relevance to all clinician leaders), will enable a better understanding of non-clinical knowledge gaps that may form part of a future foundation skill-base, in addition to traditional clinical values, to best prepare our future clinicians to influence the evolution of our future healthcare system in Australia and globally.
| Term | Definition | Source |
|---|---|---|
| Business acumen | An element of leadership, includes skills of financial literacy, knowledge of organisation and ability to take a ‘big picture’ view of the business. | Retrieved from |
| Entrepreneurship | The capacity and willingness to develop, organise and management a business venture along with any of its risks in order to make a profit. | Retrieved from |
| Leadership | A series of skills that set direction and drive a vision, by motivating and inspiring individuals and teams. | Retrieved from |
| Management | Administrative process of planning, organising, staffing, budgeting, leading and controlling a team. | Retrieved from |
| System (healthcare) | The method by which a service (healthcare) is financed, organised and delivered to a target group or population. | Retrieved from |
Authorship contribution statement
The paper properly credits the meaningful contributions of co-authors and co-researchers.
No funding was received to support the development of this paper.
Ethical statement
An ethical statement is not applicable as this publication did not involve human or animal research as it is a discussion paper.
Conflict of interest
Acknowledgements.
Jasna Romic and Sarah Thorning of Gold Coast Health Library Services for assisting with this background review.
- Abraham P.J. Developing nurse leaders: a program enhancing staff nurse leadership skills and professionalism. Nursing administration quarterly. 2011; 35 (4):306–312. doi: 10.1097/NAQ.0b013e31822ecc6e. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Al-Dossary R., Kitsantas P., Maddox P.J. The impact of residency programs on new nurse graduates' clinical decision-making and leadership skills: A systematic review. Nurse education today. 2014; 34 (6):1024–1028. doi: 10.1016/j.nedt.2013.10.006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Altman M. Implications of behavioural economics for financial literacy and public policy. The Journal of socio-economics. 2012; 41 (5):677–690. doi: 10.1016/j.socec.2012.06.002. [ CrossRef ] [ Google Scholar ]
- Bamford-Wade A., Moss C. Transformational leadership and shared governance: an action study. Journal of nursing management. 2010; 18 (7):815–821. doi: 10.1111/j.1365-2834.2010.01134.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown B.S. What is business savvy? Nursing Economics. 1983; 1 (1):52–72. [ PubMed ] [ Google Scholar ]
- Burston S., Chaboyer W., Gillespie B. Nurse-sensitive indicators suitable to reflect nursing care quality: a review and discussion of issues. Journal of Clinical Nursing. 2014; 23 (13-14):1785–1795. [ PubMed ] [ Google Scholar ]
- Castledine G. The business habits of highly effective nurses. British Journal Of Nursing. 2006; 15 (20):1143. doi: 10.12968/bjon.2006.15.20.22301. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Contino D.S. Leadership competencies: knowledge, skills, and aptitudes nurses need to lead organizations effectively. Critical care nurse. 2004; 24 (3):52–64. doi: 10.4037/ccn2004.24.3.52. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cummings G., Lee H., MacGregor T., Davey M., Wong C., Paul L., Stafford E. Factors contributing to nursing leadership: a systematic review. Journal of health services research & policy. 2008; 13 (4):240–248. doi: 10.1258/jhsrp.2008.007154. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Curtis E.A., Sheerin F.K., de Vries J. Developing leadership in nursing: the impact of education and training. British Journal Of Nursing. 2011; 20 (6):344–352. doi: 10.12968/bjon.2011.20.6.344. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davidson P.M., Elliott D., Daly J. Clinical leadership in contemporary clinical practice: implications for nursing in Australia. Journal of Nursing Management. 2006; 14 :180–187. [ PubMed ] [ Google Scholar ]
- Dudzic M. Healthcare reform in a post-pandemic world. New Labor Forum. 2021 doi: 10.1177/10957960211007128. https://doi.org/ [ CrossRef ] [ Google Scholar ]
- Dyess S., Sherman R. Developing the leadership skills of new graduates to influence practice environments: a novice nurse leadership program. Nursing administration quarterly. 2011; 35 (4):313–322. doi: 10.1097/NAQ.0b013e31822ed1d9. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Elgood, C. (2012). "Business Acumen Definition: Who Needs it and Why." Availale from https://www.chris-elgood.com/business-acumen-definition/ , Accesed 28th February 2021.
- Fletchall-Wilmes, M. A. (2019). Financial acumen for nursing: The great game . Paper presented at the Creating healthy work environments conference, Louisiana. Availale from https://sigma.nursingrepository.org/handle/10755/16729
- Fuster Linares P., Rodriguez Higueras E., Martin-Ferreres M.L., Cerezuela Torre M.Á., Wennberg Capellades L., Gallart Fernández-Puebla A. Dimensions of leadership in undergraduate nursing students. Validation of a tool. Nurse education today. 2020; 95 doi: 10.1016/j.nedt.2020.104576. 104576. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Graham I., Fielding C., Rooke D., Keen S. Practice development ‘without walls’ and the quandary of corporate practice. Journal of clinical nursing. 2006; 15 (8):980–988. doi: 10.1111/j.1365-2702.2006.01400.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Heuston M.M., Wolf G.A. Transformational leadership skills of successful nurse managers. The Journal of nursing administration. 2011; 41 (6):248–251. doi: 10.1097/NNA.0b013e31821c4620. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kang C.M., Chiu H.T., Hu Y.C., Chen H.L., Lee P.H., Chang W.Y. Comparisons of self-ratings on managerial competencies, research capability, time management, executive power, workload and work stress among nurse administrators. Journal of nursing management. 2012; 20 (7):938–947. doi: 10.1111/j.1365-2834.2012.01383.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Keselman D., Saxe-Braithwaite M. Authentic and ethical leadership during a crisis. Healthcare Management Forum. 2020 doi: 10.1177/0840470420973051. https://doi.org/ [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Longmore M. Nursing leadership being eroded. Kai Tiaki Nursing New Zealand. 2017; 23 (6):28–29. [ Google Scholar ]
- Mahoney J. Leadership skills for the 21st century. Journal of nursing management. 2001; 9 (5):269–271. doi: 10.1046/j.1365-2834.2001.00230.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Malloch K., Porter-O'Grady T. Partnership economics: nursing's challenge in the quantum age. Nursing Economics. 1999; 17 (6):299–307. [ PubMed ] [ Google Scholar ]
- Mathena K.A. Nursing manager leadership skills. The Journal of nursing administration. 2002; 32 (3):136–142. doi: 10.1097/00005110-200203000-00006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Negandhi P., Negandhi H., Tiwari R., Sharma K., Zodpey S.P., Quazi Z., et al. Building interdisciplinary leadership skills among health practitioners in the twenty-first century: An innovative training model. Frontiers in public health. 2015; 3 doi: 10.3389/fpubh.2015.00221. 221. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Patrician P.A., Oliver D., Miltner R.S., Dawson M., Ladner K.A. Nurturing charge nurses for future leadership roles. The Journal of nursing administration. 2012; 42 (10):461–466. doi: 10.1097/NNA.0b013e31826a1fdb. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pierce B.R. Speaking up: It requires leadership maturity. Nurse leader. 2016; 14 (6):413–418. doi: 10.1016/j.mnl.2016.08.005. [ CrossRef ] [ Google Scholar ]
- Rishel C.J. Financial savvy: the value of business acumen in oncology nursing. Oncology nursing forum. 2014; 41 (3):324–326. doi: 10.1188/14.ONF.324-326. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roche M., Duffield C., Dimitrelis S., Frew B. Leadership skills for nursing unit managers to decrease intention to leave. Nursing: research and reviews (Auckland, N.Z.) 2015; 5 :57–64. doi: 10.2147/NRR.S46155. [ CrossRef ] [ Google Scholar ]
- Rutherford M.M. Nursing is the room rate. Nursing Economics. 2012; 30 (4):193–199. [ PubMed ] [ Google Scholar ]
- Sanford K.D. The case for nursing leadership development: leadership development for nurses can have a positive impact on an organization’s bottom line, particularly in light of future financial challenges. Healthcare financial management. 2011; 65 (3):104–106. [ PubMed ] [ Google Scholar ]
- Scott E.S., Miles J. Advancing leadership capacity in nursing. Nursing administration quarterly. 2013; 37 (1):77–82. doi: 10.1097/NAQ.0b013e3182751998. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sherman R.O., Bishop M., Eggenberger T., Karden R. Development of a leadership competency model. The Journal of nursing administration. 2007; 37 (2):85–94. doi: 10.1097/00005110-200702000-00011. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shamian J., Ellen M.E. The role of nurses and nurse leaders on realising the clinical, social and economic return on investment of nursing care. Healthcare Management Forum. 2016; 29 (3):99–103. [ PubMed ] [ Google Scholar ]
- Sherman R.O. Learn to manage yourself. American Journal of Nursing. 2020; 120 (2):68–71. [ PubMed ] [ Google Scholar ]
- Tally L.B., Thorgrimson D.H., Robinson N.C. Financial literacy as an essential element in nursing management practice. Nursing Economics. 2013; 31 (2):77–82. [ PubMed ] [ Google Scholar ]
- Thew J. Nurses rise to new levels in the c-suite. HealthLeaders (San Francisco, Calif.) 2020; 23 (2):6–18. [ Google Scholar ]
- Thomas J., Collins A., Collins D., Herrin D., Dafferner D., Gabriel J. The language of business: a key nurse executive competency. Nursing Economics. 2008; 26 (2):122–127. [ PubMed ] [ Google Scholar ]
- Thomas T.W., Seifert P.C., Joyner J.C. Registered nurses leading innovative changes. Online journal of issues in nursing. 2016; 21 (3):3. doi: 10.3912/OJIN.Vol21No03Man03. 3. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Uhl-Bien M., Meyer D., Smith J. Complexity leadership in the nursing context. Nursing administration quarterly. 2020; 44 (2):109–116. doi: 10.1097/NAQ.0000000000000407. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vance C., Luis C. A pandemic crisis: Mentoring, leadership, and the millennial nurse. Nursing Economics. 2020; 38 (3):152. [ Google Scholar ]
- Waxman K.T., Massarweh L.J. Talking the talk: financial skills for nurse leaders. Nurse leader. 2018; 16 (2):101–106. doi: 10.1016/j.mnl.2017.12.008. [ CrossRef ] [ Google Scholar ]
- IHPA (2021). Activity based funding. Available from: https://www.ihpa.gov.au/what-we-do/activity-based-funding , Accesed 28th February 2021.
- Australian Government (2019). The Australian health system. Available from https://www.health.gov.au/about-us/the-australian-health-system . Accesed 28 February 2021.
- WHO. (2019). Universal health coverage. Avaialble from https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc) , Accesed 28th February 2021.
- Business Essentials
- Leadership & Management
- Credential of Leadership, Impact, and Management in Business (CLIMB)
- Entrepreneurship & Innovation
- Digital Transformation
- Finance & Accounting
- Business in Society
- For Organizations
- Support Portal
- Media Coverage
- Founding Donors
- Leadership Team

- Harvard Business School →
- HBS Online →
- Business Insights →
Business Insights
Harvard Business School Online's Business Insights Blog provides the career insights you need to achieve your goals and gain confidence in your business skills.
- Career Development
- Communication
- Decision-Making
- Earning Your MBA
- Negotiation
- News & Events
- Productivity
- Staff Spotlight
- Student Profiles
- Work-Life Balance
- AI Essentials for Business
- Alternative Investments
- Business Analytics
- Business Strategy
- Business and Climate Change
- Creating Brand Value
- Design Thinking and Innovation
- Digital Marketing Strategy
- Disruptive Strategy
- Economics for Managers
- Entrepreneurship Essentials
- Financial Accounting
- Global Business
- Launching Tech Ventures
- Leadership Principles
- Leadership, Ethics, and Corporate Accountability
- Leading Change and Organizational Renewal
- Leading with Finance
- Management Essentials
- Negotiation Mastery
- Organizational Leadership
- Power and Influence for Positive Impact
- Strategy Execution
- Sustainable Business Strategy
- Sustainable Investing
- Winning with Digital Platforms
Why Healthcare Professionals Need Business Skills

- 18 Oct 2018
The healthcare industry is undergoing considerable change. Today’s physicians face economic pressure to reduce costs while improving care—amidst a digital transformation that’s changing how and when patients seek treatment. Consider this: Individuals can now spot symptoms with an activity tracker and then video conference their doctor to more quickly reach a diagnosis.
“The complexities of delivering medical care are rapidly changing,” says Dr. Richard Pitts , vice president of clinically integrated networks and senior medical director at St. Joseph Heritage Healthcare, which is part of an 11-state, 50-hospital health system. “There’s a constant pressure to find more effective ways to deliver healthcare while improving quality and still holding the line on costs.”
But balancing those priorities requires more than just medical know-how. Healthcare professionals also need business skills if they want to deliver a high-quality patient experience while still meeting organizational goals.
“Paying attention to the best treatments, along with the cost of those treatments, requires both business and medical skills,” Pitts says.
It’s why Pitts enrolled in CORe , an online program featuring courses in business analytics , financial accounting , and economics . At the time, he was the chief medical officer at a large teaching hospital in Southern California and wanted to understand the business more broadly, so he could better understand the implications of his decisions and more effectively communicate with colleagues.
“CORe filled in the missing pieces with respect to my business skills,” Pitts says. “I’m now able to make meaningful business comments in meetings. Colleagues appreciate my having a basic understanding of the business world.”

Pitts uses population health—summarized by the Centers for Disease Control and Prevention as “the distribution of health outcomes within a population, and the range of personal, social, economic, and environmental factors that influence the distribution of health outcomes”—as an example of where business and medicine intersect. According to Pitts, there are nine major diagnoses, including diabetes and hypertension, in population health. When they are treated aggressively, it can result in a dramatic decrease in any associated complications.
“This saves unnecessary hospitalizations and billions of dollars of healthcare expense, while dramatically improving the quality of life for patients,” Pitts explains. “The professionals heading up this effort speak the language of business and medicine almost simultaneously.”
That example is just one of many ways healthcare professionals could benefit from having business skills. Here are five other competencies physicians should consider adding to their resume.
Business Skills Every Healthcare Professional Needs
1. analytics.
Analytics can help physicians identify disease outbreaks, track health epidemics in real time, and deliver more personalized care to patients. Achieving those goals requires developing a data mindset, however, and understanding how to recognize trends, analyze relationships between variables, and estimate the accuracy of statistics.
“My business analytics course covered regression analysis and, most importantly, the meaning of statistical significance and hypothesis testing,” Pitts says. “These are essentially the same tools that are used in healthcare to decide the outcomes of various treatments in medicine.”
2. Financial Accounting
Given how focused healthcare organizations are on reducing costs, it’s imperative for physicians to have a basic understanding of financial accounting . Not only can that knowledge lead to more strategic business decisions, but it can also help physicians analyze their team’s performance, measure the impact of their work in terms of revenue, and manage the department’s budget.
3. Ability to Lead Large, Diverse Teams
The health system Pitts works for is composed of 111,000 employees, 38,000 nurses, and 20,000 physicians alone—leading to large, diverse teams. And when faced with statistics like one in four Americans has multiple chronic conditions , it’s becoming more apparent that patients require care from multiple providers for optimal results.
The New England Journal of Medicine notes that physicians who want to lead effectively need to know how to “develop a team culture of feedback to improve patient care.” This includes understanding what motivates the team, regularly soliciting advice and incorporating suggestions, providing ongoing feedback, and acknowledging successes while constructively addressing the team’s weaknesses.
4. Strategic Management
As teams grow, so do departments’ needs and priorities. It’s important for leaders to set an organizational structure and strategy to not only guide their team but also help employees determine what to pursue and what not to pursue.
Physicians should start first with defining their mission—what the organization stands for—and then begin answering the tough questions. Where are revenues coming from? Is money being spent in the right places? How can the team optimize operations to improve the patient experience? With each response will come a clearer picture of where the team should focus their efforts.
5. Effective Communication Skills
Strong communication skills go far in healthcare. Physicians need to practice empathy and know how to properly speak with patients and their family members. Beyond that, they also need to communicate with key stakeholders, including other physicians. The more effective they are, the stronger their operations and more streamlined their processes will be.
The Importance of Business Skills
“It's important for physicians at all levels of leadership to have business skills, in order to be an effective member of ever-forming teams in the modern world of medicine,” Pitts says. “Having business skills helps to cross what often is a ‘chasm of understanding’ between physicians and finance members of the healthcare team.”
Do you want to take your career to the next level? Download our free Guide to Advancing Your Career with Essential Business Skills to learn how enhancing your business knowledge can help you make an impact on your organization and be competitive in the job market.

About the Author

Account Suspended!
Please contact our support team for further assistance.
*If you’re the owner of this website and have questions, reach out to Bluehost. We’re happy to help.
The essentials of healthcare innovation
When the winds of change blow, some people build walls, others build windmills. This Chinese proverb reminds us that crises present choices. Those choices, in turn, shape organizations’ future growth paths. Last fall, we wrote about the healthcare sector’s successful shift from merely sustaining core operations when the COVID-19 crisis hit to driving rapid innovations that saved lives and lessened the pandemic’s impact. But the winds remain strong, with new outbreaks and variants of the virus continuing to destabilize our lives and economies, even as vaccines are rolled out. Maintaining the innovation momentum will be critical to a continued effective response.
Over the past year, the healthcare sector experienced dramatic change, with novel business models, unexpected collaborations, and accelerated timelines requiring organizations to rethink how they operate. Many of these shifts are likely to persist. When we surveyed more than 100 leaders in the industry, from pharmaceutical and medical technology companies to health systems and payers, 1 McKinsey Healthcare Innovation Through Crisis Survey, June 2020. 90 percent agreed that the pandemic will fundamentally change the way they do business, requiring new products, services, processes, and business models.
To better understand how healthcare leaders’ priorities have shifted, we interviewed executives from across the value chain. Specifically, we examined how they plan to position their organizations to deliver on their innovation aspirations and which innovation capabilities they expect to grow in importance. They highlighted two main areas where the COVID-19 pandemic has brought major changes they expect to endure.
Digital acceleration. The healthcare sector has long been a laggard in digital adoption, but the pandemic delivered a massive jolt of urgency to embrace new tools and technologies. Providers rapidly scaled offerings and were seeing 50 to 175 times the number of patients via telehealth a few months into the pandemic compared with what they did before . Providers have also more broadly embraced digital engagement with patients and communities, such as proactively messaging about COVID-19-related protocols. Meanwhile, pharmaceutical and medtech companies have expanded their investments in digitally enabled clinical trials and customer-engagement models.
Workplace of the future. Many parts of healthcare require in-person care, but the pandemic has illuminated the extent to which healthcare can be delivered remotely, such as virtual care and remote patient monitoring, and virtual collaboration for professionals in the pharmaceutical and medtech industries. This model supports greater flexibility and has enabled organizations to draw from a more diverse talent pool. “You can now attract anyone, anywhere,” one executive said in reference to hiring. Healthcare leaders are also reevaluating old workplace norms and introducing new measures, such as offering assistance to help combat videoconferencing fatigue. “COVID-19 has shone a light on culture, good or bad,” another interviewee told us, and it has led healthcare players to reassess work conditions and extend greater flexibility to employees.
Adapting to these shifts, along with myriad others, will require many healthcare organizations to transform their operations—and their mindsets. Past research shows that prioritizing innovation during crises can help unlock growth in the recovery, provided leaders approach it with commitment and establish key capabilities and processes.
The foundation for successful innovation
As we noted in our earlier article, lasting innovation success requires eight essential practices (exhibit). While all eight are important and span the full innovation cycle from strategy to execution, in our latest survey, healthcare leaders identified four that are, and will, remain more critical as a result of the pandemic: choose, evolve, accelerate, and extend .
Choose . In a world of dynamic change and heightened uncertainty, it is more important than ever to actively manage portfolios of innovation initiatives, consciously choosing to invest in innovation during a crisis. “There is so much chaos, it’s like a constantly changing game board,” one healthcare leader said. “We need even more discipline to make sure we don’t miss something or get overly enamored of shiny new things.” By regularly reviewing their innovation pipelines, organizations can identify initiatives that are less likely to succeed based on the latest data and assumptions, while strengthening investments in projects with high potential. Deprioritizing some initiatives will be particularly critical for organizations plagued by staff burnout and resource constraints.
Would you like to learn more about our Strategy & Corporate Finance Practice ?
As focus on areas such as infectious diseases and testing grows, incremental innovation likely will not be enough to stay abreast of competitors. Bold bets are necessary, and multiple executives in our survey cited the value of a “start-up approach” and “scrappy mindset” in seizing opportunities. The respondents also reported a greater willingness to take risks and use agile decision making to determine how best to address new business segments. In fact, several companies have adapted their operating models to purposely select and test multiple ideas quickly rather than committing up front to a single path. One large healthcare provider, for example, has adopted a new decision-making process that includes key stakeholders from across their system, which has allowed the provider to speed up decisions across a broad portfolio of initiatives. The organization has found that this model leads to decisions and outcomes that are as good or better than under the previous model, in which they analyzed reams of data and performed weeks of analysis.
Evolve . Another priority that healthcare executives cited was evolving their business models to address new delivery constraints and client expectations. This finding is in line with our recent analysis of profit pools in the sector, which suggests healthcare players that develop innovative business models will generate disproportionate value. Several digital health companies have embraced virtual healthcare delivery, while wearables players have adapted their offerings to include monitoring for COVID-19 symptoms. Companies are also streamlining their customer support by introducing virtual assistants and using new technologies such as augmented reality. One medical technology firm, recognizing that its customers want more flexibility, made its products available as a service, which led to a surge in demand.
Accelerate . From vaccines to new designs of personal protective equipment (PPE) and ventilators, numerous recent examples demonstrate the healthcare sector’s ability to innovate at previously unimagined speeds. In the United States, the US Food and Drug Administration deployed a range of measures (such as issuing new guidance, establishing new industry engagement models, and issuing emergency use authorizations) designed to support the COVID-19 response across the range of products it regulates. In several instances, the FDA stipulated or requested that manufacturers gather data derived from the real-world use of products in order to better characterize performance, understand supply-chain vulnerability, and support additional development activity, both throughout and beyond the pandemic.
Rapid development and deployment of innovations will continue to be critical in the postpandemic world. One executive noted that healthcare has started to embrace the “beta” mindset and “soft launch” models of releasing test versions (where safety permits) that are improved based on user feedback. Another described his life-sciences company’s shift to a product-as-a-service model in just six months—a change that in the past would have taken up to five years.
Extend . The COVID-19 pandemic has highlighted the benefits of nontraditional and creative partnerships and collaborations in quickly finding creative solutions to urgent problems—from the health and auto industries teaming up to build ventilators, to pharmaceutical sector competitors collaborating to hasten the development of a COVID-19 vaccine, to healthcare providers partnering with technology companies to deliver COVID-19 apps and solutions. Experts expect such extensions of the healthcare ecosystem to be the way of the future, with more partnerships and consortia that pool capital, assets, and capabilities, both to bring operational synergies and drive innovation. “Never in my career have I experienced less politics and a more collaborative work environment,” one healthcare leader told us.
From the rise of the sharing economy in the wake of the financial crisis to airport security measures following the 9/11 attacks, deep crises tend to create shifts that stick. The COVID-19 crisis is likewise bringing changes to the healthcare sector that are here to stay. As past downturns have shown, innovation is a critical part of any recovery and will be necessary for healthcare players to stay abreast of their industry. To succeed, leaders should place particular focus on four of the eight essentials of innovation— choose, evolve, accelerate, and extend —while ensuring that end-to-end fundamentals are in place.
Daniel Cohen is an associate partner in McKinsey’s San Francisco office, where Laura Furstenthal is a senior partner; Leigh Jansen is an associate partner in the Vancouver office.
Explore a career with us
Related articles.

Healthcare innovation: Building on gains made through the crisis

Innovation: Your launchpad out of the COVID-19 crisis
The innovation commitment
Demi Lovato said she's in a 'weird position' in her career because she didn't have a backup plan
- Demi Lovato said she wants her children to have the childhood she "didn't have."
- She added that she wants them to have a "backup plan" in their career, as she wished she had.
- Her comments come as Gen Z prioritizes their health and quitting jobs without a plan.

Demi Lovato knows all too well the struggles of early fame and doesn't want her future children to experience those.
When asked what she would do if her future children wanted to follow in her footsteps, Lovato told The Hollywood Reporter in an interview published on Wednesday that she'd prepare them for it — but only after they turn 18.
"Not because I don't believe in you or love you or want you to be happy, but because I want you to have a childhood, the childhood that I didn't have," she said.
At 15, Lovato shot to childhood stardom after starring in Disney's " Camp Rock " in 2008.
"I was filled with gratitude, and there was this sense of wonder and excitement," she said. "It was very much the honeymoon phase of my career, right before the train got moving in a way where I couldn't pump the brakes."
Lovato, 31, went on to face the struggles of early stardom , from addiction to eating disorders . "I didn't realize that child stardom could be traumatic — and it isn't traumatic for everyone, but for me, it was," she said.
Lovato added that she wants her future child to have a "backup plan."
" [It's] something I wish I'd done because sometimes I think it's time for me to move on, but I'm in this weird position in my career because I still rely on music for my income," said Lovato, who, like other Disney stars — including Britney Spears and Miley Cyrus — had transitioned to a career in music.
The importance of backup plans
Lovato's comments come as more Gen Z workers quit their jobs without backup plans . In 2023, management consulting firm Oliver Wyman spent two years studying more than 10,000 Gen Zers across the US and UK. The study found that this generation was more likely than other generations to quit unfulfilling jobs — even without having other jobs lined up.
Related stories
Basant Shenouda , 27, a LinkedIn creator, previously told Business Insider that she left her toxic job less than a year in to take care of her mental health. Although she didn't regret her decision, she had left during a bad job market, which caused her stress. She advised others to consider their financials and assess their risks before quitting without a backup plan.
Similarly, Amber Smith, who left her corporate job to become a reseller and content creator, told BI that she quit because she wasn't happy. Smith, 27, said having a budget and a backup plan was important. If her self-employment did not work out, she planned to become a waitress or a bartender.
It's important to be well-prepared before quitting , she said. "Have a good idea of your expenses and your income so that you are truly prepared so that you don't find yourself having to go back to that job before you want to, if ever."
A representative for Lovato did not immediately respond to a request for comment sent outside regular business hours.
Watch: Why the retail industry has its eye on Gen Z
- Main content
{{loadingHeading}}
{{loadingSubHeading}}
healthcare financial management association

HFMA empowers healthcare financial professionals with the tools and resources they need to overcome today's toughest challenges.
Already a Member?
- Review Benefits
Connect with your healthcare finance community online or in-person.
- Access online community
- Find my Chapter
- Data + Insights
- MAP Initiative
- Peer Review
- Marketing & Sponsorship Opportunities
- Renew Membership
- Refer a Colleague
- My E-Learning
- Review Subscriptions

Sign up for HFMA`s monthly e-newsletter, The Buzz.
E-Newsletter Subscriptions
Member benefits delivered to your inbox!
Healthcare finance content, event info and membership offers delivered to your inbox.
Check out our specialized e-newsletters for healthcare finance pros.
Member benefits delivered to your inbox! Check out our specialized e-newsletters for healthcare finance pros.

Get trusted analysis and direction from the experts at HFMA.
- Regulatory & Accounting
- Healthcare Dollars & Sense
- Value Project
- Patient Friendly Billing
- Healthcare 2030
- Curing Payment Confusion
- Research & Trends
- Claim Integrity
- TLR Reports
- Healthcare Financial Practices Staff
- Sponsored Resources

All the healthcare finance news and information you need to stay current.
- Accounting & Financial Reporting
- Cost Effectiveness of Health
- Finance & Business Strategy
- Healthcare Blame Game
- Leadership & Professional Development
- Legal & Regulatory Compliance
- Operations Management
- Payment, Reimbursement & Managed Care
- Price Transparency
- Revenue Cycle
- Expert Reviewed
- Sponsored Content
- Press Releases

In-person, online. Professional development designed with you in mind.
- Live Events
- Certifications
- Digital Badging
- Organizational Learning

Supporting your career, every step of the way.
- Compensation Benchmarks
- Career Pathways
- Career Self-Assessment
Successful Healthcare Financial Management Requires Imagination and a Solid Plan
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to email a link to a friend (Opens in new window)
Imagining a better tomorrow is one thing. Making it happen is another.
When it comes to strategic planning, there are many different approaches and schools of thought. Common elements, however, include scanning the environment for threats and opportunities, using the resulting information to determine goals, developing a plan for achieving those goals, and establishing performance indicators. Once all that is done, the plan is implemented, performance is evaluated, and the process begins again.
As healthcare finance leaders, this process is second nature. Most of what we do, after all, requires a strategic approach. The budgeting process is just one example. Another is managing merger and acquisition (M&A) activity—something I was involved with numerous times during my 23 years as CFO at Geisinger. One of the most memorable was the merger of AtlantiCare into Geisinger. A well-articulated strategy, multidisciplinary teams, sound financial plans, and a lot of hard work combined to improve both organizations.
Anyone who has been through the M&A process can attest: it is not for the faint of heart, and a solid plan is crucial to success. HFMA released a report late in 2017 that reinforced this message. The study, conducted in collaboration with the Deloitte Center for Health Solutions, provided helpful insights into the M&A process from the perspectives of both the acquiring and the acquired organizations. Particularly helpful were the strategies and business practices identified as correlating with successful mergers. At the top of the list was the need to develop a strong strategic vision for pursing the transaction. Also cited as key to success were explicit financial and non-financial goals, leadership accountability, clear and up-front decision-making, and implementation of project management best practices.
The list is powerful. It appears basic and simple, but in reality, it isn’t always followed—even by those for whom it is second nature to take a strategic approach to planning and implementation. That is why it is important to regularly revisit the topic, as this issue of hfm does. Learning from the experiences of others and reviewing best practices can help us successfully plan and execute our own initiatives and innovations.
It’s been said that hope is not a strategy. Imagination may not be either. It is, however, an important step in the process. So imagine that better tomorrow, but don’t forget to plan. You need both to make it happen.

Kevin Brennan, FHFMA, CPA
is HFMA's 2018-19 National Chair.
Related Tags
Advertisements
Recent strategic planning, hospitals see a margin advantage as care migrates to the outpatient department, annual conference day 3: unitedhealth, optum executives discuss resilience strategies for healthcare, annual conference day 2: keynote speaker suneel gupta expounds on the importance of recharging, how nonprofit health systems can benefit from post-acute care partnerships, how healthcare providers can streamline a/r through partnerships , not-for-profit health systems need a new enterprise strategy, sign up for the buzz.
Healthcare finance content, event info and membership offers delivered to your inbox. Sign up for HFMA’s monthly e-newslettter, The Buzz.

Tips for Choosing Health Insurance for Small Businesses: A Complete Guide
Introduction to health insurance for small businesses.
Selecting the right health insurance for your small business can be a daunting task. With various options available, it's essential to make informed decisions that benefit both you and your employees.
Health insurance is not just about compliance; it’s a vital tool for attracting and retaining top talent while ensuring the well-being of your team.
In this guide, we'll explore the key factors to consider when choosing health insurance for your small business, from understanding the different types of plans to evaluating your company’s unique needs.
By the end, you'll be equipped with the knowledge to choose a plan that aligns with your business goals and supports your employees' health.
The Importance of Choosing the Right Plan
Choosing the right health insurance plan is crucial for small businesses. A well-chosen plan provides more than just coverage; it can significantly impact employee satisfaction and retention.
Here’s why selecting the right health insurance plan is essential:
- Attracting and Retaining Talent : Offering a comprehensive health insurance package can make your business more appealing to potential hires, giving you a competitive edge in the job market.
- Boosting Employee Morale : Employees are more likely to feel valued and secure when they know their health is taken care of, which can lead to higher productivity and job satisfaction.
- Mitigating Financial Risks : The right plan helps protect both the business and its employees from unexpected medical expenses, ensuring that health-related issues don’t become a financial burden.
- Supporting Long-Term Growth : Investing in your employees' health through insurance can lead to a healthier workforce, which contributes to the overall success and growth of your business.
Understanding the importance of these factors can guide you in making a more informed decision.
{{group-insurance-quote="/web-library/components"}}
How Health Insurance Can Benefit Both Employers and Employees
Health insurance is more than just a safety net; it’s a strategic asset for both employers and employees. Here’s how it benefits each:
For Employers:
- Improved Employee Retention : Offering health insurance can significantly reduce turnover rates, as employees are more likely to stay with a company that cares for their well-being.
- Enhanced Productivity : Healthy employees are more productive. Regular check-ups and preventive care, often covered by insurance, help keep your team in top shape, reducing absenteeism.
- Tax Benefits : In India, providing health insurance can offer tax advantages under the Income Tax Act, helping businesses reduce their taxable income while supporting their employees.
- Cost Control : By providing group health insurance, businesses can negotiate better rates and more comprehensive coverage, managing costs more effectively than with individual plans.
For Employees:
- Financial Security : Health insurance protects employees from the high costs of medical treatment, ensuring they don’t have to dip into their savings or incur debt for healthcare needs.
- Access to Quality Healthcare : Employees gain access to a network of quality healthcare providers, making it easier to receive timely medical attention.
- Peace of Mind : Knowing that they and their families are covered gives employees peace of mind, allowing them to focus on their work without the added stress of potential medical expenses.
- Preventive Care : Insurance plans often include preventive services such as vaccinations, screenings, and wellness checks, helping employees maintain good health and catch potential issues early.
By understanding these benefits, small businesses can see that investing in health insurance is not just an expense but a vital component of a thriving workplace.
Understanding Different Types of Health Insurance Options
Navigating the world of health insurance can be complex, especially with the variety of options available.
Understanding the different types of health insurance plans will help you make the best choice for your small business. Here’s a breakdown of the most common options:
1. Group Health Plans vs Individual Health Insurance Policies
- Group Health Plans : Typically offered by employers, these plans cover all eligible employees under a single policy. They often come with lower premiums per person and more comprehensive coverage, making them a popular choice for small businesses. The cost is usually shared between the employer and the employee, making it more affordable for everyone involved.
- Individual Health Insurance Policies : These are purchased by individuals directly from insurers. While they offer flexibility in choosing coverage, they tend to be more expensive and may not provide the same level of benefits as group plans. For small business owners, offering individual policies may not be as cost-effective or attractive to employees as group health plans.
2. Health Reimbursement Arrangements (HRAs)
- HRAs are employer-funded plans that reimburse employees for medical expenses and, in some cases, insurance premiums. They offer flexibility as the employer can control the amount of reimbursement. This option is particularly beneficial for small businesses that want to provide health benefits without committing to a traditional group health plan.
3. Direct Primary Care (DPC)
- Direct Primary Care (DPC) is a model where businesses pay a flat, monthly fee to primary care providers, offering employees unlimited access to basic healthcare services without the need for insurance claims. DPC can be a cost-effective way for small businesses to ensure that employees have access to essential healthcare without the complexities of insurance. This model is gaining popularity for its simplicity and direct approach to healthcare.
4. Small Business Health Options Program (SHOP Plans)
- SHOP Plans are a government initiative aimed at helping small businesses provide affordable health insurance to their employees. These plans allow businesses to offer a variety of coverage options, giving employees the freedom to choose the plan that best suits their needs. SHOP Plans also come with potential tax credits, making them a viable option for many small businesses.
Understanding these options allows you to tailor your choice to what best fits your business and employees' needs. Each type has its advantages, and the right choice will depend on your specific circumstances.
Evaluating Your Small Business's Specific Health Insurance Needs
Selecting the right health insurance plan requires a thorough evaluation of your small business's specific needs.
This ensures that the plan you choose is both cost-effective and beneficial for your employees. Here’s how you can assess these needs:
1. Assessing Employee Needs and Preferences
- Conduct Surveys : Start by surveying your employees to understand their health needs and preferences. This can include questions about their current health coverage, preferred healthcare providers, and any specific healthcare services they value.
- Consider Demographics : The age, health status, and family situations of your employees can influence the type of coverage that will be most beneficial. For example, younger employees may prefer lower premiums with higher deductibles, while older employees or those with families might prioritise comprehensive coverage.
2. Including Essential Benefits and Understanding Healthcare Requirements
- Identify Essential Benefits : Ensure that the plan covers essential benefits like hospitalisation, maternity care, preventive services, and chronic disease management. In India, it's crucial that these benefits align with the specific needs of your workforce.
- Understand Legal Requirements : Familiarise yourself with the regulations surrounding health insurance for small businesses in India, including the minimum coverage requirements and any mandatory benefits.
Evaluating these factors will help you choose a plan that not only meets legal obligations but also supports the health and well-being of your employees.
Key Factors in Choosing a Health Insurance Plan
When choosing a health insurance plan for your small business, several key factors should guide your decision. These factors will help you balance cost, coverage, and convenience, ensuring that you select a plan that benefits both your business and your employees. Here’s what to consider:
1. Comparing Different Health Insurance Policies
- Coverage Options vs Costs : Begin by comparing the coverage offered by different policies. Look for a plan that provides comprehensive benefits at a reasonable cost. It’s essential to find a balance between premium costs and the level of coverage offered, ensuring that the plan is affordable without compromising on essential benefits.
- Network Hospitals and Inclusions/Exclusions : The insurer's network of hospitals is a critical factor. A wider network offers your employees more options for treatment. Additionally, scrutinise what is included and excluded in the policy. Some plans may exclude certain treatments or have sub-limits on claims, which can be a significant drawback.
2. The Significance of Network Hospitals and Inclusions/Exclusions in Plans
- Network Hospitals : Opt for a plan with an extensive network of hospitals, especially those that are conveniently located for your employees. This ensures that employees have easy access to healthcare services without having to travel far or face out-of-network charges.
- Inclusions/Exclusions : Carefully review the list of inclusions and exclusions in each plan. Understand the sub-limits on specific treatments, waiting periods for certain conditions, and any other restrictions that could affect the overall value of the plan. Being aware of these details helps avoid unexpected costs later on.
Considering these factors will guide you towards a plan that not only fits your budget but also meets the healthcare needs of your employees.
{{group-insurance-quote="/web-library/components"}}
Financial Implications and Advantages for Small Businesses
Providing health insurance for your employees is an investment that offers significant financial benefits for your small business. Understanding these advantages can help you make a well-informed decision that supports both your financial goals and your employees’ well-being.
1. Tax Benefits of Providing Health Insurance to Employees
- Tax Deductions : In India, the premiums paid for employee health insurance can often be deducted as a business expense under the Income Tax Act. This reduces your taxable income, effectively lowering your overall tax liability.
- Potential for Additional Tax Credits : Depending on your business size and the specific insurance plan, you may also qualify for tax credits or other financial incentives designed to encourage small businesses to provide health coverage.
2. How Health Insurance Can Reduce Overall Hiring and Retention Costs
- Attracting Talent : Offering a robust health insurance plan makes your business more attractive to potential hires. In a competitive job market, this can give you an edge in securing top talent without the need to offer higher salaries.
- Employee Retention : Employees are more likely to stay with a company that invests in their health and well-being. This reduces turnover and the associated costs of recruiting, hiring, and training new employees.
- Lower Absenteeism : By promoting regular health check-ups and providing easy access to medical care, health insurance can help reduce absenteeism, keeping your workforce healthier and more productive.
Investing in health insurance is not just about meeting obligations—it’s a strategic move that can lead to long-term financial savings and a more stable, motivated workforce.
Engaging Employees in the Selection Process
Involving your employees in the health insurance selection process can lead to better outcomes for everyone.
By understanding their needs and preferences, you can choose a plan that is more likely to be utilised and appreciated, leading to higher satisfaction and overall well-being.
1. Conducting Surveys to Understand Employee Needs Better
- Gathering Feedback : Use surveys or meetings to gather input from your employees about their healthcare needs and preferences. Ask questions about their preferred healthcare providers, the types of coverage they value most, and any concerns they may have with their current health coverage.
- Customising Coverage : With the feedback you collect, you can tailor the health insurance plan to better fit the needs of your workforce. For example, if a significant portion of your employees has young families, you might prioritise plans with strong maternity and paediatric care options.
2. Coverage for Dependents: Yes or No?
- Evaluating the Need : Consider whether offering coverage for employees' dependents is necessary for your business. Providing this option can be a strong incentive for employees with families, making your company more attractive and reducing turnover rates.
- Weighing Costs : While offering dependent coverage can increase premiums, it can also improve employee satisfaction and loyalty. Weigh the benefits against the costs to determine if this is a viable option for your business.
Engaging your employees in the selection process not only helps you choose a plan that meets their needs but also fosters a sense of inclusion and transparency.
This involvement can lead to higher participation rates in the plan and greater overall satisfaction.
The Step-by-Step Guide to Selecting the Right Plan
Selecting the right health insurance plan for your small business involves a careful and systematic approach. Here’s a step-by-step guide to help you through the process:
1. Understanding Your Business Needs
- Evaluate Your Budget : Start by assessing how much your business can afford to spend on health insurance. Consider both the immediate costs, such as premiums, and long-term financial commitments.
- Analyse Workforce Demographics : Take into account the age, health conditions, and family status of your employees. This will help you identify the type of coverage that would best meet their needs.
2. Exploring Insurance Options – SHOP, HRAs, Group Plans, DPC
- SHOP Plans : Consider enrolling in the Small Business Health Options Program (SHOP) if your business qualifies. SHOP Plans offer a variety of options, allowing employees to choose what works best for them while potentially providing your business with tax credits.
- HRAs : Health Reimbursement Arrangements allow you to reimburse employees for their medical expenses, offering flexibility without the need for a traditional group plan.
- Group Health Plans : These are often the most comprehensive option, providing broad coverage to all employees under one plan.
- Direct Primary Care (DPC) : For businesses seeking a straightforward healthcare solution, DPC allows employees unlimited access to primary care services for a fixed monthly fee, bypassing traditional insurance altogether.
3. Making the Final Decision: A Comprehensive Comparison
- Compare Plans Side by Side : Look at the coverage, costs, network hospitals, and additional benefits each plan offers. Consider what’s included, what’s excluded, and any potential limitations or waiting periods.
- Consult with Experts : If possible, consult with a health insurance broker or financial advisor who can provide professional insights tailored to your business’s unique situation.
4. Implementing the Chosen Plan
- Clear Communication : Once you’ve selected a plan, communicate the details clearly to your employees. Ensure they understand how to enrol, what the plan covers, and how it benefits them.
- Support During Enrollment : Offer assistance during the enrolment process, whether through HR or external consultants, to make it as smooth as possible for your employees.
Following these steps ensures that the health insurance plan you choose is well-suited to your business and employees' needs, providing long-term benefits for both.
Avoiding Common Pitfalls When Choosing a Plan
Selecting the right health insurance plan is a significant decision, and avoiding common pitfalls can save your small business from future complications. Here’s what to watch out for:
1. Neglecting Employee Needs or Feedback
- Ignoring Input : Failing to consider employee needs can lead to dissatisfaction and low participation rates in the health plan. Ensure you gather and act on employee feedback to choose a plan that meets their expectations and requirements.
- Assuming One Size Fits All : Avoid the mistake of assuming that a single plan will suit all employees. Different employees have different healthcare needs, and it’s essential to offer options where possible.
2. Ignoring the Fine Print: Sub-limits, Terms, and Conditions
- Overlooking Sub-limits : Some health insurance policies have sub-limits on specific treatments, such as room rent or surgeries. These sub-limits can lead to unexpected out-of-pocket expenses for your employees, reducing the plan's perceived value.
- Missing Hidden Clauses : Pay close attention to terms and conditions, including exclusions, waiting periods, and co-payment clauses. These details can significantly impact the actual coverage provided and lead to disputes or dissatisfaction later on.
3. Focusing Solely on Premium Costs
- Choosing the Cheapest Option : While it’s important to consider cost, choosing the cheapest plan can often mean inadequate coverage. Balance affordability with the level of coverage to ensure your employees receive the benefits they need.
- Overlooking Long-Term Costs : Consider the long-term financial implications of the plan, including potential premium increases, and whether the plan will remain cost-effective as your business grows.
4. Failing to Maintain Flexibility: Knowing When It's Time to Reevaluate Your Plan
- Sticking to an Outdated Plan : As your business evolves, so do your employees' needs. Regularly review your health insurance plan to ensure it continues to meet those needs and adjust as necessary.
- Ignoring Market Changes : Health insurance products and regulations can change. Stay informed about new options or policy changes that could benefit your business and employees.
By being mindful of these common pitfalls, you can avoid costly mistakes and ensure that the health insurance plan you choose is a good fit for your business in both the short and long term.
Maintaining Flexibility: Knowing When It's Time to Reevaluate Your Plan
The health insurance needs of your small business are likely to change over time. Maintaining flexibility and knowing when to reevaluate your plan ensures that it continues to meet the evolving needs of your employees and business. Here’s how to stay adaptable:
1. Changing Business or Employee Needs
- Growth or Downsizing : If your business grows or downsizes, your health insurance plan might need adjustment. A growing workforce may require broader coverage or additional options, while downsizing could mean looking for more cost-effective solutions.
- Shifts in Employee Demographics : Changes in your workforce, such as an increase in younger employees or more employees with families, might necessitate a reevaluation of the coverage provided. Regularly assess your team’s demographics to ensure your plan still aligns with their needs.
2. New Market Options or Policies
- Stay Informed About New Plans : The health insurance market is continually evolving, with new plans and options frequently introduced. Stay updated on these developments to see if there’s a more suitable or cost-effective plan available.
- Regulatory Changes : Government policies regarding health insurance can change, affecting both costs and available options. Keep an eye on any legislative updates that might impact your current plan or present new opportunities.
3. Regular Plan Reviews
- Annual Reviews : Conduct an annual review of your health insurance plan to evaluate its performance. This includes considering employee feedback, assessing claim rates, and comparing the plan to new offerings on the market.
- Benchmark Against Industry Standards : Compare your plan with what other businesses in your industry are offering. This can help you stay competitive in attracting and retaining talent.
Flexibility in managing your health insurance plan allows you to adapt to changes smoothly, ensuring that your coverage continues to support your business goals and employee well-being.
This proactive approach can help you avoid being caught off-guard by unforeseen changes or missed opportunities.
Conclusion: The Long-Term View on Health Insurance for Small Businesses
Health insurance is more than a necessary expense for small businesses—it's a strategic investment in your company's future.
The right plan not only supports your employees' health but also plays a crucial role in attracting and retaining top talent, enhancing productivity, and fostering long-term business growth.
1. The Role of Health Insurance in Employee Satisfaction and Business Growth
- Employee Well-Being : Offering a comprehensive health insurance plan shows your employees that you value their well-being, leading to higher morale and job satisfaction. This, in turn, translates into increased productivity and loyalty, which are essential for sustaining growth.
- Competitive Advantage : In a competitive job market, health insurance can be a differentiator that sets your business apart. By providing quality coverage, you can attract skilled professionals who are looking for more than just a paycheck.
2. Recap of Steps to Choose the Best Plan
- Assess Your Business Needs : Start by understanding your budget and your employees' demographics.
- Explore Insurance Options : Consider different plans such as SHOP, HRAs, group health plans, and DPC.
- Engage Employees : Involve your employees in the selection process to ensure the plan meets their needs.
- Avoid Pitfalls : Be mindful of common mistakes, such as ignoring employee feedback or focusing solely on cost.
- Stay Flexible : Regularly review and adjust your plan to keep it aligned with your business’s evolving needs.
By following these steps, you can select a health insurance plan that not only meets your immediate needs but also adapts to future challenges and opportunities.
For small businesses, making the right choice in health insurance is an investment in long-term success.
Whether you’re providing essential benefits, boosting employee satisfaction, or managing costs, the right plan will help you build a strong, healthy workforce that drives your business forward.
How to Choose the Right Health Insurance Plans to Help Small Businesses
Choosing the right health insurance plan is a critical decision that impacts both your employees' well-being and your business's financial health. Here’s a concise guide to help you navigate this process effectively:
1. Determine What Your Staff Needs
- Assess Demographics : Evaluate the age, family status, and health conditions of your employees.
- Collect Feedback : Use surveys or direct communication to understand their healthcare priorities.
2. Compare Policies
- Coverage vs Cost : Balance the comprehensiveness of coverage with affordability.
- Network Hospitals : Ensure the plan includes a broad network of hospitals convenient for your employees.
3. Guarantee Maximum Coverage
- Include Essential Benefits : Ensure the plan covers hospitalisation, preventive care, and chronic disease management.
- Understand Exclusions : Be clear on what the policy does not cover to avoid surprises.
4. Verify the Policy Terms
- Review Fine Print : Check for sub-limits, co-payment clauses, and waiting periods.
- Consult Experts : If necessary, seek advice from an insurance broker or financial advisor.
5. Check the Network of Hospitals
- Hospital Proximity : Ensure that the plan includes hospitals that are easily accessible to your employees.
- Quality of Care : Look for plans associated with reputable healthcare providers.
6. Consider Add-On Advantages
- Optional Benefits : Evaluate if adding dental, vision, or maternity cover would be beneficial.
- Employee Preferences : Tailor these add-ons based on what your employees value most.
7. Keep an Eye on the Exclusions
- Understand Limitations : Be aware of specific exclusions that might affect your employees.
- Plan Accordingly : Make sure the exclusions don’t undermine the overall value of the plan.
8. Verify the Sub-Limits
- Check for Caps : Be mindful of sub-limits on room rent, specific treatments, and other key aspects.
- Balance Cost and Coverage : Ensure these limits don’t lead to excessive out-of-pocket expenses for your employees.
By following these steps, you can ensure that the health insurance plan you choose is well-suited to both your business’s and your employees’ needs, providing comprehensive coverage while remaining cost-effective.
Frequently Asked Questions (FAQs)
Choosing the right health insurance plan for your small business can raise several questions. Here are answers to some of the most common queries:
Q. Why should a small business owner buy health insurance?
- Attracting and Retaining Talent : Health insurance is a key benefit that helps attract top talent and reduces employee turnover. It shows that you value your employees' health and well-being, making your business more competitive in the job market.
- Tax Benefits : In India, providing health insurance to employees can offer tax deductions, helping to reduce your taxable income.
- Boosting Productivity : Employees with health insurance are more likely to seek preventive care and maintain their health, leading to fewer sick days and higher productivity.
Q. How to choose health insurance for self?
- Evaluate Your Needs : Start by assessing your healthcare needs, including any existing conditions, your preferred healthcare providers, and the types of coverage you require.
- Compare Plans : Look at different policies, balancing coverage and cost. Make sure the plan covers essential services and fits your budget.
- Check for Exclusions : Be aware of what the policy doesn’t cover and ensure these exclusions won’t affect your access to necessary healthcare.
Q. Is company health insurance enough?
- Coverage Scope : Company health insurance often provides comprehensive coverage, but it may not cover all healthcare needs, such as certain specialised treatments or services.
- Consider Supplementing : Depending on your health needs, you might want to consider supplementing company-provided insurance with a personal health insurance plan or add-ons like critical illness cover.
- Evaluate Regularly : Regularly review your company’s health insurance plan to ensure it still meets your needs, especially if your health situation changes.

More From Forbes
Virtual reality—the universal language in healthcare.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Alon Zuckerman is the President of Surgical Theater , a global leader in XR visualization for healthcare.
Imagine walking into the doctor’s office in constant pain. Your head feels like it is going to burst. You get an MRI scan. It’s cancer. You feel suddenly alone and riddled with fear. What do you do? The doctor shows you these images of your brain, but they look like a black and white Rorschach. You point to a large fragment. “Is that the cancer, Doc?” “No, that is just brain matter. … This is the cancer.” You see him pointing to a speck on the screen so tiny you would have otherwise missed it. You think to yourself, “Seriously, this is cancer? This small dot has the power to take my life?” As your mind races, the doctor starts explaining the various treatment options to you, but she seems to be speaking another language altogether. If only there was a way to translate the words flowing from her into something comprehensible.
Now imagine the confusion if you were in a foreign country speaking to a physician using words that are not even your native language. This would make it infinitely more challenging to cognize the gravity of what is being said. Regardless of the situation, when it comes to understanding your health, there are significant language barriers that prevent patients and families from fully understanding the diagnosis and proposed treatment. However, everything changes with the synergy of virtual reality in healthcare.
With VR, anyone, regardless of race, sex, age or language, can visualize their anatomy and prognosis in a way that is easily grasped. When you take a 3D rendering of a person’s anatomy and show it to them in a virtually created world, they are able to clearly visualize it for themselves. After all, a brain is still a brain regardless of cultural and physical differences!
To this end, virtual reality creates a universal language that even a young child can understand. Instead of showing patients scans that look like faded black and white photographs, an image can be recreated into a full-scale 3D rendering then loaded onto a VR headset. Once the patient lowers the virtual lens over their eyes, they are propelled into an entirely simulated world where they can visualize and fully comprehend their very own anatomy.
Nicolas Cage’s ‘Longlegs’ Gets Digital Streaming Premiere Date
Today’s nyt mini crossword clues and answers for wednesday, august 21, nyt ‘strands’ hints, spangram and answers for wednesday, august 21st, the history of medical imaging.
Before 1895, there was no way to depict what was happening inside the human body. In fact, during the 1500s, a magnifying glass was considered state-of-the-art imaging. It was not until Wilhelm Roentgen discovered the X-ray while experimenting with a Crooks Cathode Ray tube that we were finally able to picture the inside of the human body. This discovery immediately went “viral,” setting in motion what would become the Industrial Revolution of medical imaging. World War II sonar technology would later usher in the use of ultrasound. Then, in the 1970s, MRI, CT and PET scans became available.
However, even with these key advances in imaging, only highly trained healthcare providers specializing in reviewing scans could actually interpret them. Patients remained left in the dark when it came to apprehending them for themselves.
Applying VR In Healthcare Today
Virtual reality, however, is redefining this market, making it the standard of care to be able to fully understand and visualize one’s condition prior to receiving treatment. Myriad VR platforms are joining the race to be competitive in the extended reality space. Companies, such as apoQlar, are offering a medical mixed-reality platform for surgical planning, training and education. Other companies such as eXeX are offering hospital and operating room optimization and efficiency platforms. Their CreatorX program allows hospitals to create a virtual workflow for operating room procedures. My company, SurgicalTheater, is using extended reality for surgical planning, patient education and intraoperative augmented reality (AR). And companies like XRHealth are even offering virtual reality for therapeutic healthcare.
When it comes to implementing these advanced technologies, there are several factors the health system must consider, including: cost, scalability and training. With the influx of inflation and prices at an all-time high, hospitals are having to tighten their belts more than ever. It is obligatory to do a cost-benefit analysis and determine the ROI for any innovative tools they plan to purchase. However, upfront costs can readily be outweighed when factoring in increased efficiencies, improved outcomes and a possible reduction in complications brought about by these latest advancements to patient care.
On the other hand, the health system must consider both scalability and training. The hospital will need to identify the resources necessary for a successful implementation. They will require a project manager to supervise the process. They must determine who and how to train the necessary staff and users. Finally, it is essential to have a surgeon champion driving the overall process. All of these variables must be considered and carefully planned before purchasing the equipment or making a material change to their current operations.
Once the hospital has all of the elements in place, they must consider possible challenges that may arise during launch. Not having compatible equipment or the available footprint can cause increased costs and hidden barriers that prolong timelines. Additionally, not having enough excited surgeon users can stifle utilization. Just because you build it does not mean they will come. … Many physicians have established practices and techniques of operating. Introducing any new tool may seem like a threat to their equilibrium. It is essential to build momentum and excitement among surgeons beforehand while also ensuring they have the necessary training and resources to prepare them for a modification to their routine.
This influx of extended reality companies is creating a fundamental paradigm shift in healthcare that is giving patients the confidence to make informed medical decisions. Healthcare providers now have the tools to truly create a personalized treatment plan while communicating and collaborating with their patients, allowing these individuals to fully take back control of their health.
Imagine once again sitting in the surgeon’s office facing your uncertain future. Only now, you have a clear image of what your anatomy looks like, what to expect during treatment and are an active player in the solution rather than watching helplessly from outside.
Forbes Business Council is the foremost growth and networking organization for business owners and leaders. Do I qualify?

- Editorial Standards
- Reprints & Permissions
State’s Steward exit plan is no sure thing, as landowners, creditors push back
State officials brace for a challenge to their plan to seize st. elizabeth’s property.

The Healey administration’s plan to steer six Steward Health Care hospitals into the hands of new owners just got more complicated.
Administration officials expect Apollo Global Management, a private equity firm that controls the St. Elizabeth’s Medical Center property in Brighton, to contest the state’s move to seize the land and buildings by eminent domain, setting up a trial that could last up to two years.
In bankruptcy court filings, meanwhile, disputes between bankrupt Steward and some of its top creditors over how to divvy up proceeds from the Massachusetts hospital sales threw up new roadblocks to the transactions, which were on track to be finalized Thursday.
The developments created fresh uncertainty for a sales process that began late last year and gained urgency after Dallas-based Steward filed for bankruptcy on May 6. Governor Maura Healey on Friday said the state helped engineer preliminary deals to sell St. Elizabeth’s and five other hospitals to health systems in Massachusetts and Rhode Island, promising the deals would be completed “in short order.”
“It’s unsettling to see these challenges to the hospital sales and eminent domain,” said Paul Hattis, senior fellow at the Lown Institute, a health care think tank. “It’s all about investment firms stopping the transition of the health system in Massachusetts to maximize their profits.”
Advertisement
Healey said last week that state officials were frustrated by the protracted sales talks and planned to take the St. Elizabeth’s property by eminent domain. Sharon Boyle, general counsel for the state Executive Office of Health and Human Services, sent a letter to Apollo saying the governor had determined the continued standoff in the hospital negotiations had created “a crisis that threatens the public health in Massachusetts,” endangering the lives of patients.
The so-called offer letter said the state would pay $4.5 million in compensation for the property, a sum it said was based on the bid of a third-party buyer on St. Elizabeth’s, the flagship Steward hospital. The facility sits on nearly 14 acres in Brighton Center, with an assessed value of more than $200 million, according to property records.
Boyle asked Apollo to respond to the offer by Tuesday at 11 a.m. or “the Commonwealth will assume that the offer has been rejected.” As of early afternoon Tuesday, a state spokesperson said the administration hadn’t received a response from Apollo, indicating state officials were bracing for a legal challenge from the New York-based buyout firm.
A spokesperson for Apollo declined to comment on its plans.
Under state law, the governor or the Governor’s Council must formally approve an “order of taking” and record it with the Suffolk County Registry of Deeds. Once it’s recorded, the property would pass to the state, which could then turn it over to Boston Medical Center to continue operating the hospital, pending a legal challenge.
Apollo would have up to three years to challenge the land-taking and would have the right to a trial by jury, according to legal experts. While the legal challenge would contest the stated reason for taking the land, the case would likely become a valuation dispute in which each side would be required to submit independent appraisals of the property. Even if the case is fast-tracked, it could take 18 to 24 months.
A more immediate obstacle to the hospitals changing hands came from a group of private credit companies that extended $575 million in loans to Steward before and after it filed for bankruptcy. The lenders said they have the right to block the sale of hospitals in Massachusetts and seven other states to ensure that the bulk of the profits don’t go to the property owners, according to its filing in US Bankruptcy Court in Houston.
Steward’s sale of its hospitals’ real estate in 2016 has been seen as the primary obstacle to the sales because it’s required bidders to negotiate with both the for-profit hospital system and the landowners, who have thus far failed to agree on how to divide proceeds from the sales.
The private credit firms, however, said their financial interests must be resolved before any of the hospitals can change hands.
Steward’s lenders weren’t identified in the court filing. But the hospital system said in June that it had obtained bankruptcy financing, enabling it to operate through the summer, from a consortium of five lenders: WhiteHorse Finance, Owl Creek Investments, MidOcean Credit Fund Management, Brigade Capital Management, and One Investment Management. Four of them were previous lenders.
In their filing, the lenders said they have collateral on their loans that includes hospital permits, vendor contracts, furniture, and medical equipment for operating rooms and emergency departments. Because these assets “have significant value” to hospital buyers, the lenders claimed a right to consent to purchase agreements, the filing said.
A spokesperson for Steward declined to comment on the filing.
Separately, in a lawsuit filed in the Houston court, Steward accused Medical Properties Trust , a real estate investment trust that bought its hospitals’ land and buildings eight years ago, of interfering with its efforts to sell the hospitals by speaking directly to bidders during the sales talks — something it said violated the terms of the bankruptcy.
While MPT originally bought the real estate, it later sold a 50 percent interest in its Massachusetts hospital properties to another firm, Macquarie Infrastructure Partners. Earlier this month, the landowners turned the property over to their mortgage lender, Apollo, though MPT continues to own Steward hospital properties in other states.
Steward’s filing said MPT had engaged in “calculated efforts to undermine the debtors’ sales process by attempting to siphon all value from the debtors’ estates and hospitals into its own coffers.”
MPT filed a motion asking the bankruptcy judge to dismiss Steward’s charges, calling them “irrelevant as a legal matter.” The motion said Steward “can be expected to lash out at MPT and try to blame MPT for the poor progress of these cases and the delays in the sale process.”
In a statement, the Alabama real estate firm said, “We categorically reject any accusation that MPT has interfered with Steward’s marketing and sales efforts — on the contrary, we have proactively worked with potential bidders to address real estate-related matters.”
The disputes among parties to the bankruptcy, which had been alluded to in court hearings in recent weeks, surfaced as bidders for the six Massachusetts hospitals worked to finalize asset purchase agreements. Bankruptcy Judge Christopher Lopez has scheduled a hearing Thursday to consider final approval of the sales.
It will be up to Lopez to weigh the merits of Steward’s and MPT’s claims, as well as those of Steward’s lenders, potentially delaying the push to transfer the Steward hospitals to new operators. Final hospital sales hearings have previously been scheduled and delayed five times.
Healey announced agreements in principle had been reached for Boston Medical Center to take over St. Elizabeth’s Medical Center and Good Samaritan Medical Center in Brockton; Lawrence General Hospital to acquire Holy Family Hospital in Methuen and Haverhill; and, Lifespan Health System of Providence to purchase St. Anne’s Hospital in Fall River and Morton Hospital in Taunton.
Two other Steward hospitals, Carney Hospital in Dorchester and Nashoba Valley Medical Center in Ayer, are slated to close at the end of the month because they received no qualified bids, the governor said. Leaders in both communities have been pressing the Healey administration to take steps to save those hospitals.
Robert Weisman can be reached at [email protected] .
We've detected unusual activity from your computer network
To continue, please click the box below to let us know you're not a robot.
Why did this happen?
Please make sure your browser supports JavaScript and cookies and that you are not blocking them from loading. For more information you can review our Terms of Service and Cookie Policy .
For inquiries related to this message please contact our support team and provide the reference ID below.

IMAGES
COMMENTS
To understand your step-by-step strategy for future. A business plan outlines all the resources you need across business operations and can provide a solid backbone to prepare you for potential future challenges. A plan provides a clear direction for all business areas and allows you to know what steps to take in regard to growth and expansion.
A strategic healthcare business plan helps the physician set marketing goals and priorities for the medical practice. Clarity of aims and objectives can improve the quality of patient care. Strategic business planning offers great long-term value. After the initial planning is done, a practice can use it as the benchmark for measuring progress ...
The business plan should include a detailed action plan with identified responsible parties, timelines, and specific metrics to track progress. ... a crucial legal consideration for healthcare business owners. Importance of Compliance Plans. Compliance plans play a vital role in the healthcare industry. These plans outline the necessary steps ...
The Importance of Strategic Business Planning in Healthcare. Strategic business planning in healthcare is essential for navigating the industry's complexities. It ensures organizations can effectively respond to evolving regulations, technological advancements, and changing patient needs. A well-crafted strategic plan aligns an organization's ...
Strategic planning in healthcare is critical for healthcare organizations to succeed. Understanding how your organization operates is the key to creating an effective strategic plan for the entire healthcare system to succeed. Sometimes you need to look at the hierarchy of your organization. Determining your company's goals and setting a path ...
Many of the same concepts for writing a business plan for a startup apply to creating a business plan for a new clinical program or expanding operations within a health system. Introduction Building a life science startup is a long and complex endeavor, and the skills required are very different from the knowledge and training that academic ...
Technological advancements play a significant role in modern healthcare practices and has the power to improve patient outcomes and experiences. [1] To support your expansion goals, invest in advanced healthcare technologies that align with your practice's needs. Evaluate electronic medical record (EMR) systems, telemedicine platforms, and ...
Abstract. Health care organizations implement business strategies through programs and services, and success depends on careful program design and execution. A conscientious design requires thorough efforts in organizing the planning process, conducting the decision analysis, and obtaining approval for a program.
6 Strategic Planning Techniques for Healthcare Providers. The Performance Prism Model: The Performance Prism is a performance management framework with five perspectives: stakeholder satisfaction, stakeholder contribution, strategies, processes, and capabilities.; The EFQM Excellence Model: Like the majority of these six techniques, the EFQM model can be used in conjunction with other frameworks.
By Tara Duggan Updated April 09, 2019. Writing a business plan for a healthcare involves preparing a document that outlines the services you plan to provide and how you intend to run your company ...
Identifying the forces that drive industry profits is a critical first step to defining a business strategy. A successful strategy combats the forces that diminish industry profits. Developing a strategy requires making tradeoffs. Through a case study with Oak Street Health, learners will evaluate the tradeoffs made by an entrant in elder care ...
By using reliable and thoughtful planning, healthcare facilities can initiate patient-centric approaches and boost success. Strategic healthcare planning consists of creating objectives, setting goals and then creating a plan for achievement. In other words, it's the process of outlining goals and taking the necessary steps to achieve them.
Strategic planning in healthcare helps you set business goals and decide how to allocate resources to achieve these goals. It involves looking at your organization's internal and external environments using established strategic tools. Doing so lets you develop a strategic plan outlining what you want to achieve and an action plan to get there.
It needs to be sufficiently granular to enable alignment on key issues, but not so detailed that it becomes an execution or implementation plan. The business plan can also address the most important aspects of governance required to deliver on the value thesis for the partnership, including board structure, critical decision rights, decision ...
Discussion. Nurses learn and develop broad skills in leadership and management, but less specifically about business or the broader system. With a contemporary Australian health system aiming to be more effective, nurses may require a greater level of business acumen to adequately understand the mechanics of business decision making in the system when designing care models, as well as ...
A strategic plan is an action plan or road map you can use to develop your compliance plan, achieve your coding and auditing goals, and protect your bottom line. Creating this plan will help you map out your long-term goals and identify specific metrics, revenue targets, and focus areas in need of improvement. Here are the steps to develop your ...
Business Skills Every Healthcare Professional Needs. 1. Analytics. Analytics can help physicians identify disease outbreaks, track health epidemics in real time, and deliver more personalized care to patients. Achieving those goals requires developing a data mindset, however, and understanding how to recognize trends, analyze relationships ...
Strategic planning can address a broad range of issues, including the patient experience, brand image, and revenue. The second component of healthcare FP&A is, of course, finances. While it is possible to address financial concerns and strategic goals separately, this approach can be impractical. Accomplishing any strategic goals will require a ...
The U.S. Department of Health and Human Services (HHS) has issued a statement on who should be getting vaccinations against COVID-19 ahead of flu season. The guidance was released as part of the ...
Another priority that healthcare executives cited was evolving their business models to address new delivery constraints and client expectations. This finding is in line with our recent analysis of profit pools in the sector, which suggests healthcare players that develop innovative business models will generate disproportionate value. Several ...
Smith, 27, said having a budget and a backup plan was important. If her self-employment did not work out, she planned to become a waitress or a bartender. It's important to be well-prepared before ...
A well-articulated strategy, multidisciplinary teams, sound financial plans, and a lot of hard work combined to improve both organizations. Anyone who has been through the M&A process can attest: it is not for the faint of heart, and a solid plan is crucial to success. HFMA released a report late in 2017 that reinforced this message.
Warner Bros Discovery Inc. agreed to spend at least $8.5 billion on movie and TV production at a new entertainment center in Las Vegas if Nevada approves a proposed subsidy next year.
The Importance of Choosing the Right Plan. Choosing the right health insurance plan is crucial for small businesses. A well-chosen plan provides more than just coverage; it can significantly impact employee satisfaction and retention. ... Attracting Talent: Offering a robust health insurance plan makes your business more attractive to potential ...
Healthcare providers now have the tools to truly create a personalized treatment plan while communicating and collaborating with their patients, allowing these individuals to fully take back ...
Long-running negotiations to steer six Steward Health Care hospitals in Massachusetts into the hands of new owners just got more complicated, with bankruptcy disputes throwing up new roadblocks to ...
Public health officials fighting a lethal outbreak of mpox in Africa are struggling to avoid mistakes that cost lives during the Covid-19 pandemic, starting with the slow acquisition of vaccines.